Abstract
Introduction
Korean Americans are one of the most underserved ethnic/linguistic minority groups owing to cultural and institutional barriers; there is an urgent need for culturally competent diabetes management programs in the Korean American community for those with type 2 diabetes. The purpose of this study was to test the effectiveness of a community-based, culturally tailored, multimodal behavioral intervention program in an ethnic/linguistic minority group with type 2 diabetes.
Design
A RCT with waitlist comparison based on the Predisposing, Reinforcing, and Enabling Constructs in Education/environmental Diagnosis and Evaluation (PRECEDE)–Policy, Regulatory, and Organizational Constructs in Educational and Environmental Development (PROCEED) and self-help models. Data were collected between September 2010 and June 2013 and were analyzed in August–December 2014. Statistical significance was set at p<0.05.
Setting/participants
In a naturally occurring community setting, a total of 250 Korean Americans with type 2 diabetes were randomized into an intervention group (n=120) or a control group (n=130).
Intervention
The intervention consisted of key self-management skill-building activities through 12 hours of group education sessions, followed by integrated counseling and behavioral coaching by a team of RNs and community health workers.
Main outcome measures
Primary (clinical) outcomes were hemoglobin A1c, glucose, total cholesterol, and low-density lipoprotein at baseline and 3, 6, 9, and 12 months. Secondary (psychosocial and behavioral) outcomes included diabetes-related quality of life, self-efficacy, adherence to diabetes management regimen, and health literacy.
Results
During the 12-month project, the intervention group demonstrated 1.0%–1.3% (10.9–14.2 mmol/mol) reductions in hemoglobin A1c, whereas the control group achieved reductions of 0.5%–0.7% (5.5–7.7 mmol/mol). The differences between the two groups were statistically significant. The intervention group showed statistically significant improvement in diabetes-related self-efficacy and quality of life when compared with the control group.
Conclusions
RN/community health worker teams equipped with culturally tailored training can be effective in helping an ethnic/linguistic minority group manage diabetes in the community.
Introduction
While the increasing incidence and prevalence of type 2 diabetes mellitus (DM) are serious problems in the U.S. and worldwide,1,2 there is growing evidence that racial and ethnic minorities in the U.S. experience a disproportionally high prevalence of DM-related morbidity and mortality.3 A number of individual, group, and systems factors are embedded in ethnic minority communities, including economic inequalities, low access to health care, and certain cultural practices, which are detrimental to achieving optimal DM management. Asian Americans, including Korean Americans (KAs), are one of these ethnic minorities.4
KAs are one of the most underserved minority populations in the U.S. and are at particularly high risk of developing DM, a problem that is exacerbated by the drastic lifestyle changes that KA immigrants face upon arrival in the U.S. These changes affect all areas of life, including SES, diet, living arrangements, physical activities, social relationships, and mental status, all of which in turn influence health status.5 These health risks are further compounded by low health literacy levels: Today’s KAs are predominantly first-generation immigrants and monolingual (Korean only), and more than 70% report having trouble understanding medical terminology, even when using materials that have been translated into Korean.6 In addition, a scarcity of personal and community resources (e.g., lack of health insurance coverage), coupled with institutional and cultural barriers (e.g., language),7 is likely to deter KAs from seeking timely diagnosis or receiving proper treatment. Like other immigrant ethnic minorities, they often have limited access to care and health information.6,7 As a result, KAs with asymptomatic chronic conditions like DM are not receiving timely diagnosis or adequate treatment.
In an effort to close DM-related health disparity gaps and reduce the burden of DM among underserved ethnic minority populations, a culturally tailored behavioral intervention has been recommended, for which collaboration between the ethnic community and health system is essential.3,8,9 Therefore, a community-based, multimodal behavioral self-help intervention program was designed for diabetes management (SHIP-DM) in first-generation KA immigrants with DM. The goal of SHIP-DM was to help KAs achieve better glycemic control and restore their self-confidence with regard to DM management, thereby reducing DM-related mortality and morbidity and improving their quality of life.
Methods
Conceptual Framework and Study Design
SHIP-DM was based on the Predisposing, Reinforcing, and Enabling Constructs in Education/environmental Diagnosis and Evaluation (PRECEDE)–Policy, Regulatory, and Organizational Constructs in Educational and Environmental Development (PROCEED) model10 as the main theoretic framework, incorporating several theoretic premises from the self-help model.11 The modified model enabled researchers and stakeholders to easily connect the predisposing, enabling, and reinforcing factors into measurable indicators or action items. The model has been useful in studies designed to promote chronic condition management skills, including our previous studies for KA immigrants.12-14 The theoretic framework provided ways of directly assessing the intervention effects by looking at distal outcomes (e.g., glucose control) as well as proximal outcomes (e.g., self-efficacy). Based on the model, it was hypothesized that the intervention would empower KAs with DM through the following:
an increase in participants’ DM-related knowledge;
an improvement in participants’ self-care skills;
an increase in participants’ confidence and self-efficacy to deal with DM; and
enabling participants to care for themselves and adhere to treatment regimens.
In order to apply the theoretic framework, the principles of community-based participatory research15,16 were employed for the operational protocols.
SHIP-DM proceeded in two phases: formative refinement and summative evaluation. The details of the formative processes, including our efforts to improve cultural sensitivity with community participation, have been published elsewhere.13 The summative evaluation utilized a community-based, open-label, RCT with a waitlist control group. All intervention protocols were approved by the Johns Hopkins Medicine IRB.
Study Sample
SHIP-DM was for first-generation KA immigrants who have DM and are in need of culturally sensitive behavioral education to improve their self-management skills. Eligibility criteria for our study were purposely broad in order to improve the external validity. They were as follows: self-identification as a KA immigrant; age ≥35 years; physician-diagnosed DM; difficulty in managing glucose levels, as demonstrated by hemoglobin A1c (A1c) ≥7.0% (53 mmol/mol); and ability to stay in the program for at least 1 year.
Study participants were recruited in a natural community setting through media campaigns, outreach to places populated or frequented by KAs (e.g., ethnic churches, supermarkets, festivals), and referrals by Korean healthcare providers. A detailed account of our creative outreach efforts, as members of a linguistic and ethnic minority community, to address major barriers to study participation has been published elsewhere.16,17 Most research activities took place at a community site, the Korean Resource Center (KRC), where our community–academic team members worked together to enroll participants, provide interventions, and collect data, including blood samples for a year-long follow-up period. Trained staff from the Johns Hopkins Institute for Clinical and Translational Research (ICTR) were dispatched to the KRC and obtained blood specimens from participants.
Recruitment, Randomization, and Retention
The study was designed to detect meaningful changes in the primary endpoint of A1c level from baseline to a 12-month follow-up. Using a conservative effect size of 0.5% reduction in A1c with type I error of 0.05 and 90% power with an assumed correlation of 0.80 between measurement points, the sample size was 105 subjects per group.
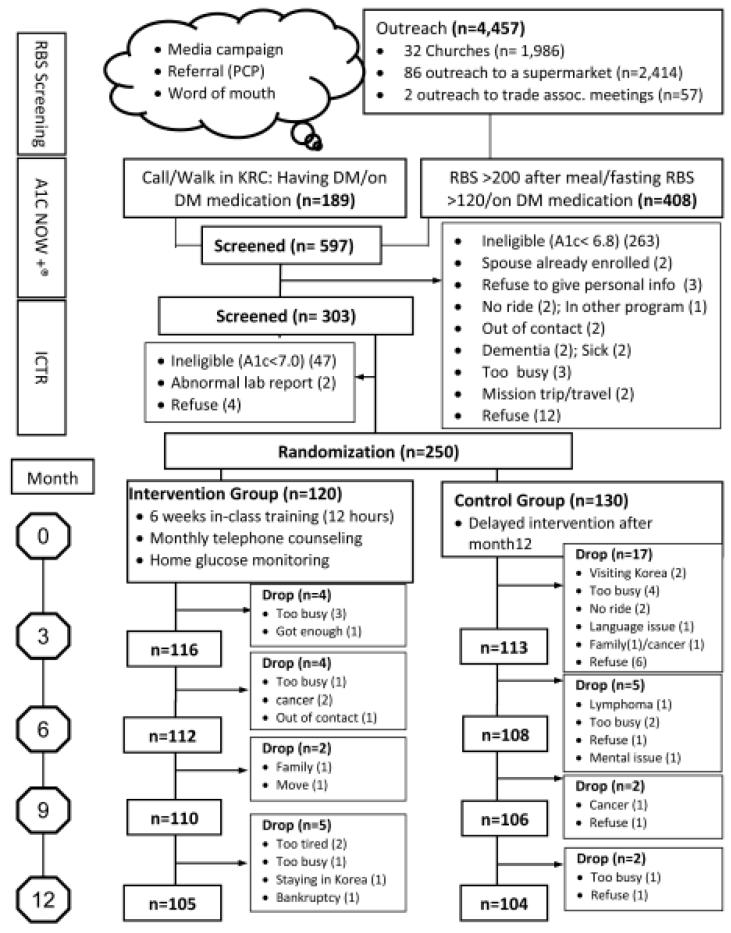
In order to efficiently identify the KAs who had difficulty in managing their DM, a three-step screening process was used. First, a spot check assessed glucose level with a portable glucometer (LifeScan One Touch Ultra*2). When a subject’s glucose level exceeded a predetermined level (200 mg/dL), or if the subject had a physician diagnosis of DM, they visited the study site for further testing with a point-of-care product to assess A1c levels using the dry blood method (A1c Now+ test kit). The third and final stage was to refer participants with A1c Now+ results of ≥6.8% (51 mmol/mol) to the Johns Hopkins ICRT laboratory. At baseline, 250 KAs who met the eligibility criteria were randomized to the intervention group (n=120) or the waitlist control group (n=130), which was oversampled for its lower retention rate. A total of 105 remained in the program in the intervention and 104 in the control group, yielding a total of 209 completers, with a retention rate of 83.6% (CONSORT chart provided in Figure 1).
Figure 1.
CONSORT diagram.
RBS, Random blood sugar; PCP, primary care provider; KRC, Korean Resource Center; ICTR, Johns Hopkins Institute for Clinical and Translational Research lab; DM, Diabetes Miletus
Intervention
SHIP-DM consisted of three main intervention modes:
a series of structured behavioral education programs delivered in a group education format;
ongoing self-monitoring of glucose; and
individualized counseling using a motivational interviewing method.
As a whole, this intervention was aimed at behavioral modification by empowering participants, equipping them with better knowledge and skills about DM and its management, facilitating better communication with their healthcare providers, encouraging better healthcare utilization, and enhancing their general problem-solving skills. These processes were expected to improve glucose control and quality of life.
The group education involved weekly 2-hour sessions over the course of 6 weeks. It included three subcomponents: The educational and behavioral education component was aimed at enhancing the patient’s knowledge of DM and its treatment, while reducing risk factors; and advancing KAs’ coping/enabling capacities through improved problem-solving skills, cognitive reframing, and belief in self. The psychological education component was designed to assist KAs in reframing life adversity within a more positive perspective (i.e., challenge rather than threat). The health literacy–enhancing component addressed the strong need to enhance essential health literacy skills (e.g., reading food labels, understanding essential medical terminology, following instructions to access available healthcare resources). We employed various techniques to encourage participants’ active engagement, including multimedia presentations, teach-back, role play, and group discussions.
Self-monitoring of glucose is an integral part of DM management. Participants in the intervention group were provided with a glucose monitor, strips, and lancet(s) for 12 months, along with detailed instructions about how to accurately take measurements and record them in a DM diary. They were asked to measure twice a day, in the morning and the afternoon, for 12 months.
A team of bilingual nurses/community health workers (CHWs) who had extensive training in DM management provided motivational counseling once a month for 12 months. Calls were recorded and charted according to the implementation protocols. The goal of this telephone counseling was to assist each participant in reaching an individualized treatment goal and to maintain acquired self-care skills and a healthy lifestyle. Overall, treatment goals were guided by the American Diabetes Association clinical guidelines and the Diabetes Prevention Program recommendations.18,19
The counseling team included 4 RNs and 3 CHWs. The RNs counseled 38 participants; the CHWs counseled 67 participants. CHWs were responsible for conducting counseling for participants with relatively stable glucose control and no comorbidities, whereas RNs were responsible for participants with unstable glucose control or complications of DM. The RN–CHW counseling team met weekly to review the progress of all participants. These meetings focused especially on discussing participants with challenges and on strategies to help them overcome barriers to achieve adequate glucose control. In addition, the Principal Investigators and clinical counseling team chose to review one of every 10 counseling records (about 10%) to assess intervention fidelity.
Participants in the control group received a brief educational brochure at baseline that highlighted the critical self-management principles of SHIP-DM. The brochure also contained available care and educational resources in the community. An abbreviated educational session was offered to the control group members after all data were collected at 12 months.
Measures
In addition to the screening questionnaire concerning demographic information and the blood tests for enrollment at baseline, blood specimens were collected from both groups at 3, 6, 9, and 12 months. Other indicators were collected for factors and constructs derived from the theoretic model at baseline and at 3, 6, and 12 months. Data were collected from September 2010 through June 2013, and were analyzed in August–December 2014.
Predisposing factors included several indicators:
demographic information (age, gender, education, income, occupation, marital status, family composition, living arrangement, length of residency in the U.S., and English fluency);
lifestyle-related DM risk factors (smoking, alcohol consumption, physical activity, and dietary intake measured by the 24-hour recall method);
medical history (history of DM and other chronic conditions including hypertension, coronary heart disease, congestive heart failure, and cancer; medications; and the use of Oriental medicine); and
depression, measured by the Korean version of the Personal Health Questionnaire 9 (PHQ-9K).20
Enabling factors included DM knowledge, self-efficacy, and accessibility; attitudes and beliefs related to DM management; effective therapeutic communication with care providers; and healthcare access and utilization for DM management. We tested DM knowledge using the Diabetes Knowledge Test (DKT),21 which has two sets of questionnaires: a 14-item general test and a 9-item insulin-use subscale. In our pilot study, the DKT proved to be reliable, with a Cronbach’s α of 0.70 at baseline.13
Self-efficacy in DM management was measured by a scale adapted from the Stanford Chronic Disease Self-Efficacy scale.22 The modified scale consisted of eight 10-point Likert-type items asking how confident the individual was in managing DM in the areas of diet, exercise, and general self-management behaviors. Our previous study demonstrated the modified scale’s construction validity and reliability (internal consistency coefficient alpha of 0.85 and a test–retest validity of 0.80).13
For primary outcome measures, A1c was measured using the agar electrophoresis assay method, which measured the amount of glucose bound to the hemoglobin in red blood cells. The fraction of A1c when compared with normal hemoglobin was taken as the measure of overall glycemic control during the past 3 months.
Both lipid profiles and A1c were analyzed at the Johns Hopkins ICTR, and blood pressure was measured at the KRC by trained staff using the A&D UA-767 (A&D Company, Tokyo), which has been shown to be reliable.23 The average of the second and third readings taken after the participant had been at rest for 5 minutes was used in the analysis.
For secondary outcome measures, the Diabetes Quality of Life Measure (DQOL; 15 items)24 assessed the participants’ personal experience of DM care and treatment, including the following four dimensions: concern about future effects of DM, concern about social and vocational issues, the impact of treatment, and personal satisfaction with treatment. The DQOL and its four scales had high degrees of internal consistency (Cronbach’s α=0.66–0.92) and excellent test–retest reliability (r =0.78–0.92). Self-care activity was measured by medication adherence, diet, self-monitoring of blood glucose, exercise, foot care, and daily decision making, using the Summary of Diabetes Self-Care Activities scale.25
Intervention Fidelity
A total of 109 intervention group participants (90.8%) attended all six classes; overall, participants attended two to six classes. The average attendance rate was 96.1%. Each participant was scheduled to receive 11 counseling sessions, ranging from 15 to 45 minutes; on average, they received 7.8 counseling sessions, with a range of one to 11 sessions. DM diary recording was not mandatory but recommended, and 110 participants (91.6%) followed the recommendations for the first 6 weeks.
Statistical Analysis
Group differences between the intervention and control groups at baseline were assessed using parametric tests (e.g., t-tests, chi-square tests). Comparison of the two groups with regard to the primary and the secondary outcomes at each data collection point was made using t-tests, and those who completed the program were included in the analysis. Also, the proportions of participants who showed up and sustained the ≥0.5% reduction in A1c level during the project period were compared using chi-square tests. Finally, effects of the intervention were tested using the mixed model of panel data to compare the changes in the primary outcomes over time (i.e., slopes) between the two groups. All analyses were conducted using STATA, version 12, setting the level of statistical significance at p<0.05. The research protocol was approved by the Johns Hopkins Medical Institutions IRB, and written consent was obtained from all study participants.
Results
Table 1 summarizes participants’ baseline characteristics. The intervention and control groups were not statistically different in major demographic characteristics. The participants had a mean age of 58.7 (SD=8.4) years, there were more men (56.9%) than women, and most (89.5%) were married. About two thirds (63.2%) lived in their own home, with an average of one child and an average monthly income of $3,780, with which about two thirds (67.7%) reported maintaining a comfortable life. On average, the KAs in the study had completed about 13.4 years of education (mostly in their homeland, Korea) and had resided in the U.S. for 23.8 years. Almost two thirds (59.3%) were working full/part time.
Table 1.
Sample Characteristics at Baseline
| Indicators | Intervention Group (I) (n=105) |
control Group (C) (n=104) |
Diff (I-C) |
Total (n=209) |
|---|---|---|---|---|
| Age, years (SD) | 59.1 (8.4) | 58.3 (8.5) | 0.8 | 58.7 (8.4) |
| Male, n (%) | 62 (59.1%) | 57 (54.8%) | 4.3% | 119 (56.9%) |
| Married, n (%) | 95 (90.1%) | 92 (88.5%) | 1.6% | 187 (89.5%) |
| Family size, persons (SD) | 3.1 (1.2) | 3.0 (1.1) | 0.1 | 3.0 (1.2) |
| Working: full/part time, n (%) | 56 (53.3%) | 68 (65.4%) | −12.1% | 124 (59.3%) |
| Years in USA, years (SD) | 24.8 (10.8) | 22.8 (11.1) | 2.0 | 23.8 (11.0) |
| Education, years (SD) | 13.5 (3.1) | 13.3 (2.9) | 0.2 | 13.4 (3.0) |
| Housing own, n (%) | 70 (66.7%) | 62 (59.6%) | 7.1% | 132 (63.2%) |
| Comfortable living, n (%) | 62 (62.0%) | 74 (73.3%) | −11.3% | 136 (67.7%) |
| Monthly income, $ (SD) | $3,807 ($3,216) | $3,754 ($3,599) | $53 | $3,780 ($3,411) |
| No health insurance, n (%) | 47 (44.8%) | 57 (54.8%) | −10.0% | 104 (49.8%) |
| Have a primary doctor, n (%) | ||||
| Not have one | 30 (28.6%) | 33 (31.7%) | −3.1% | 63 (30.1%) |
| Korean speaking doctor | 64 (61.0%) | 61 (58.7%) | 2.3% | 125 (59.8%) |
| Non-Korean speaking doctor | 11 (10.5%) | 10 (9.6%) | 0.9% | 21 (10.1%) |
| Known having DM, (mon) (SD)a | 105.3 (87.6) | 99.3 (84.8) | 6.0 | 102.4 (86.0) |
| Get treatment for DM, n (%) | 76 (72.4%) | 73 (70.2%) | 2.2% | 149 (71.3%) |
| Insulin only, n (%) | 5 (4.8%) | 3 (2.9%) | 1.9% | 8 (3.8%) |
| Oral medication only, n (%) | 64 (61.5%) | 67 (64.4%) | −2.9% | 131 (63.0%) |
| Both, n (%) | 7 (6.7%) | 3 (2.9%) | 3.8% | 10 (4.8%) |
| Seriousness of DM impact on work (range 0 (none)–10(severe), mean (SD)b |
2.1 (2.6) | 1.9 (25) | 0.2 | 2.0 (2.5) |
| Seriousness of DM impact on daily activity (range, 0 [none] – 10 [severe]), mean (SD) |
2.8 (3.2) | 2.2 (2.6) | 0.6 | 2.6 (2.9) |
| Overweight (BMI: 25-29.9), n (%) | 46 (43.8%) | 50(48.1%) | −4.3% | 96 (45.9%) |
| Obese (BMI≥ 30), n (%) | 10 (9.5%) | 4 (3.9%) | 5.6% | 14 (6.7%) |
| Waist-hip ratio, mean (SD) | 0.9 (0.1) | 0.9 (0.1) | 0.0 | 0.9 (0.1) |
| Hypertension diagnosed, n (%) | 43 (41.4%) | 57 (54.3%) | − 12.9% | 100 (47.9%) |
n (I)=99, n (C)=92. The remaining 18 realized they had DM less than a month ago.
excluding retired, housewives, unemployed
Note: Boldface indicates statistical significance (p<0.05).
On average, the participants had been aware of their DM or had a physician diagnosis for 8 years and 6 months, but nearly three quarters (71.3%) were currently receiving either oral or insulin treatment, or both. The rates of treatment in the two groups were not statistically different. The majority of them (59.8%) were receiving medical care from a Korean-speaking doctor, but about a third (30.1%) did not have a primary care doctor at all. It should be noted that 18 participants (8.6%) first learned through our screening process that they were diabetic. In addition, the control group reported a higher rate of diagnosed high blood pressure (54.3%) than the intervention group (41.4%), and the difference was statistically significant.
Table 2 shows the differential effects of the intervention on the primary outcome, the A1c level, as an important clinical parameter of diabetic control. At baseline, the two groups were similar— that is, statistically not different from each other—in terms of clinical parameters. A dropout analysis indicated that there was no statistically significant difference in the baseline A1c levels between those who remained in the program and those who dropped out.
Table 2.
Physiological Outcomes in Intervention (I, n=105) and Control Group (C, n=104)
| Outcomes | Baseline | Month 3 | Month 6 | Month 9 | Month 12 |
|---|---|---|---|---|---|
| HbAlc, % (SE) | |||||
| Intervention | 8.9 (0.2) | 7.9 (0.2) | 7.7 (0.1) | 7.8 (0.1) | 7.6 (0.1) |
| Control | 8.8 (0.2) | 8.3 (0.2) | 8.3 (0.2) | 8.2 (0.1) | 8.1 (0.1) |
| Diff (I-C) | 0.1 (0.3) | −0.4 (0.2) | − 0.6 (0.2) ** | − 0.4 (0.2) * | − 0.5 (0.2) ** |
| Changes from baseline, % (SE) | |||||
| Intervention | - | − 1.0 (0.1) *** | − 1.2 (0.1) *** | − 1.1 (0.1) *** | − 1.3 (0.1) *** |
| Control | - | − 0.5 (0.1) *** | − 0.5 (0.1) *** | − 0.6 (0.1) *** | − 0.7 (0.1) *** |
| Diff (I-C) | - | − 0.5 (0.2) ** | − 0.7 (0.2) *** | − 0.6 (0.2) ** | − 0.6 (0.2) *** |
| HbA1c ≥ 0.5% reduction from baseline, n (%) | |||||
| Intervention | 64 (61.0%) | 69 (65.7%) | 66 (62.9%) | 69 (65.7%) | |
| Control | 45 (43.3%) | 40 (38.5%) | 46 (44.2%) | 50 (48.1%) | |
| Diff (I-C) | 17.7% ** | 27.2% *** | 18.7% ** | 17.6% ** | |
| Glucose, mg/dL (SE) | |||||
| Intervention | 160.1 (6.3) | 128.5 (4.5) | 127.9 (4.6) | 131.6 (4.7) | 124.8 (4.3) |
| Control group | 158.3 (5.3) | 143.5 (5.3) | 151.9 (5.2) | 148.9 (4.8) | 147.1 (4.9) |
| Diff (I-C) | 1.8 (8.2) | − 15.0 (6.8) * | − 24.0 (6.9) *** | − 17.3 (6.7) ** | − 22.3 (6.6) *** |
| Changes from baseline, mg/dL (SE) | |||||
| Intervention | - | − 31.6 (5.0) *** | − 32.1 (5.0) *** | − 28.5 (5.0) *** | − 35.2 (5.0) *** |
| Control group | - | − 14.8 (5.1) ** | −6.3 (5.1) | −9.4 (5.1) | − 11.1 (5.1) * |
| Diff (I-C) | - | − 16.8 (7.1) * | − 25.8 (7.1) *** | − 19.1 (7.1) ** | − 24.1 (7.1) ** |
| Triglyceride, mg/dL (SE) | |||||
| Intervention | 177.3 (11.2) | 159.5 ( 9.8) | 163.0 ( 9.9) | 169.4 (10.1) | 167.6 (10.3) |
| Control group | 180.6 (12.6) | 174.9 (11.4) | 178.9 (11.5) | 172.1 (11.3) | 174.7 (12.3) |
| Diff (I-C) | −3.3 (16.8) | −15.4 (15.0) | −16 (15.1) | −2.7 (15.2) | −7.1 (16.0) |
| Changes from baseline, mg/dL (SE) | |||||
| Intervention |
−
17.8 ( *
8.8) |
−14.3 ( 8.8) | −7.9 (8.8) | −9.7 ( 8.8) | |
| Control group | −5.8 ( 8.8) | −1.7 ( 8.8) | −8.5 ( 8.8) | −5.9 ( 8.8) | |
| Diff (I-C) | −12.1 (12.4) |
−12.6 (12.4) | 0.6 (12.4) | −3.8 (12.4) | |
| Total Cholesterol, mg/dL (SE) | |||||
| Intervention | 188.5 (4.2) | 178.2 (3.9) | 176.2 (3.7) | 178.5 (3.8) | 178.8 (3.7) |
| Control group | 201.1 (5.1) | 190.7 (4.1) | 190.6 (3.9) | 188.4 (4.0) | 193.6 (4.7) |
| Diff (I-C) | −12.6 (6.6) | − 12.5 (5.7) * | − 14.4 (5.4) ** | −9.9 (5.5) | − 14.8 (6.0) * |
| Changes from baseline, mg/dL (SE) | |||||
| Intervention | - | − 10.3 (3.3) *** | − 12.3 (3.3) *** | − 10.0 (3.3) ** | − 9.7 (3.3) ** |
| Control group | - | − 10.4 (3.3) *** | − 10.5 (3.3) *** | − 12.7 (3.3) *** | − 7.5 (3.3) * |
| Diff (I-C) | - | −0.1 (4.6) | −1.8 (4.6) | 2.7 (4.6) | −2.2 (4.6) |
| HDL, mg/dL (SE) | |||||
| Intervention | 49.8 (1.2) | 49.8 (1.2) | 49.6 (1.2) | 48.9 (1.2) | 49.0 (1.2) |
| Control group | 48.7 (1.1) | 49.6 (1.2) | 49.5 (1.6) | 52.1 (3.8) | 49.7 (1.2) |
| Diff (I-C) | 1.1 (1.5) | 0.2 (1.7) | 0.1 (2.0) | −3.2 (3.9) | −0.7 (1.7) |
| Changes from baseline, mg/dL (SE) | |||||
| Intervention | - | 0.0 (1.7) | −0.2 (1.7) | −0.9 (1.7) | −0.8 (1.7) |
| Control group | - | 0.9 (1.7) | 0.8 (1.7) | 3.5 (1.7) * | 1.1 (1.7) |
| Diff (I-C) | - | −0.9 (2.4) | −1.0 (2.4) | −4.4 (2.4) | −1.9 (2.4) |
| LDL, mg/dL (SE) | |||||
| Intervention | 104.6 (3.3) | 97.7 (3.0) | 94.8 (2.9) | 96.3 (3.0) | 97.6 (3.1) |
| Control group | 115.6 (4.0) | 107.4 (3.5) | 107.6 (3.3) | 105.2 (3.4) | 109.1 (3.5) |
| Diff (I-C) | − 11.0 (5.2)** | − 9.7 (4.6) * | − 12.8 (4.3) ** | − 8.9 (4.5) * | − 11.5 (4.6) * |
| Changes from baseline, mg/dL (SE) | |||||
| Intervention | - | − 6.9 (2.8) ** | − 9.8 (2.8) *** | − 8.3 (2.8) ** | − 7.0 (2.8) * |
| Control group | - | − 8.2 (2.8) ** | − 8.0 (2.8) ** | − 10.4 (2.8) *** | − 6.5 (2.8) * |
| Diff (I-C) | - | 1.3 (3.9) | −1.8 (3.9) | 2.1 (3.9) | −0.5 (3.9) |
| Systolic BP, mg/dL (SE) | |||||
| Intervention | 134.7 (1.8) | 133.1 (1.8) | 131.2 (1.8) | na | 134.3 (1.5) |
| Control group | 133.1 (2.0) | 134.4 (2.0) | 132.1 (1.7) | na | 136.2 (1.9) |
| Diff (I-C) | 1.6 (2.7) | −1.3 (2.6) | −0.9 (2.4) | - | −1.9 (2.4) |
| Diastolic BP, mg/dL (SE) | |||||
| Intervention | 78.9 (1.0) | 78.8 (1.0) | 77.5 (0.9) | na | 79.0 (0.9) |
| Control group | 78.5 (1.1) | 80.3 (1.0) | 79.5 (1.1) | na | 81.2 (0.9) |
| Diff (I-C) | 0.4 (1.5) * | −1.5 (1.4) | −2.0 (1.4) | - | −2.2 (1.2) |
| BP controlled (Systolic/Diastolic BP<130/80), n (%) | |||||
| Intervention | 37 (35.2%) | 37 (35.2%) | 40 (38.1%) | na | 31 (29.5%) |
| Control group | 38 (36.5%) | 34 (32.7%) | 38 (36.5%) | na | 25 (24.0%) |
| Diff (I-C) | −1.3% | 2.5% | 2.6% | - | 5.5% |
Note: Boldface indicates statistical significance (*p<0.05, **p<0.01, ***p<0.001). na, not measured
At baseline, the average A1c level in the intervention group was 0.1% (1.1 mmol/mol) higher than that in control group, a difference that was not statistically significant. Beyond the baseline measures, the A1c levels of both groups were reduced and sustained at a reduced level for the rest of the project period.
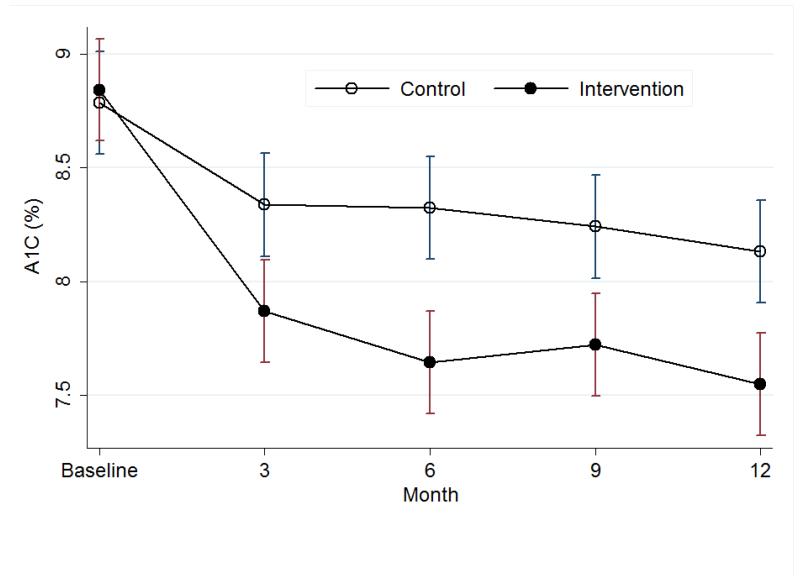
However, the reductions in the intervention group were greater than those in the control group: The differences were on average −0.5% (−5.5 mmol/mol), −0.7% (−7.7 mmol/mol), −0.6% (−6.6 mmol/mol), and −0.6% (−6.6 mmol/mol) at 3, 6, 9, and 12 months, respectively. These differences were all statistically significant (Table 2, Figure 2). In addition, the A1c changes in the intervention group from baseline were −1.0% (−10.9 mmol/mol), −1.2% (−13.1 mmol/mol), − 1.1% (−12.0 mmol/mol), and −1.3% (−14.2 mmol/mol) at 3, 6, 9, and 12 months, respectively. The comparable changes in the control group were −0.5% (−5.5 mmol/mol), −0.5% (−5.5 mmol/mol), −0.6% (−6.6 mmol/mol), and −0.7% (−7.7 mmol/mol), respectively. These differences between the two groups were all statistically significant. In addition, clinically significant reductions of ≥0.5% (5.5 mmol/mol) from baseline were observed to a greater extent in the intervention group (61.0%, 65.7%, 62.9%, and 65.7% at 3, 6, 9, and 12 months, respectively) than in the control group (43.3%, 38.5%, 44.2%, and 48.1% at 3, 6, 9, and 12 months, respectively), and the differences were all statistically significant (Table 2, Figure 2). An additional analysis using the mixed effects model of panel data with random coefficients (intercepts and slopes) was performed. The dependent variable was the level of A1c (expressed in %), and the independent variables were the treatment (0=control, 1=intervention), period (baseline and 3, 6, 9, and 12 months), and their interaction and A1c at baseline. The grouping variables were subject’s ID and group (0=control, 1=intervention). The analysis confirmed that the A1c reductions over time were statistically significant both in the intervention group (b= −0.091, SE=0.010, p<0.001) and the control group (b= −0.047, SE=0.010, p<0.001), and that the reduction in the intervention group was greater than that in the control group (χ2=10.07, p=0.002). The statistically significant reductions in both the intervention and control groups occurred in the first 3 months.
Figure 2.
A1C changes over time with 95% CIs.
A similar pattern of reduction was observed in blood glucose level; both the intervention and the control groups started at baseline with similar levels of blood glucose, 160.1 and 158.3 mg/dL, respectively (not statistically different), but they were both sharply reduced (intervention group, 128.5 mg/dL; control group, 143.5 mg/dL) at 3 months, and the reduction was sustained for the rest of the project period. Blood glucose levels for the intervention group were much lower than those for the control group in months 3–12, and these differences were statistically significant (Table 2).
Similarly, the total cholesterol and low-density lipoprotein (LDL) levels of both groups were significantly reduced in the first 3 months, although the differences between the two groups were not statistically significant, but the reductions were sustained for the rest of the project period. The triglyceride levels in both groups were reduced, but only the reduction in the intervention group at 3 months was statistically significant. No statistically significant improvement was observed in high-density lipoprotein, except for in the control group at 9 months. The blood pressure in both groups was stable during the project period, and no statistically significant difference was found between groups and time. The intervention group showed an increase in the proportion of those with optimal blood pressure control (systolic/diastolic blood pressure <130/80), but the increase was not statistically significant (Table 2).
Table 3 demonstrates the effects of the intervention on DM-related psychobehavioral outcomes. During the 12 months of the intervention, there were statistically significant improvements in DM-related self-efficacy, DM knowledge, quality of life, and attitudes toward DM in the intervention group when compared with the control group. The depression experience measured by the PHQ-9K was reduced in both groups during the project period, but only the reductions in the control group were statistically significant.
Table 3.
Psychobehavioral Outcomes in Intervention Group (I=105) and Control Group (C=104)
| Outcomes | Baseline | Month 3 | Month 6 | Month 12 |
|---|---|---|---|---|
| Diabetes self-efficacy (range: 0-80), mean (SE) | ||||
| Intervention | 49.1 (1.3) | 57.5 (1.2) | 57.9 (1.2) | 58.6 (1.2) |
| Control | 44.7 (1.5) | 46.6 (1.5) | 47.2 (1.6) | 46.5 (1.6) |
| Diff (I-C) | 4.4 (2.0) * | 10.9 (1.9) *** | 10.7 (2.0) *** | 12.1 (2.0) *** |
| Changes from baseline, mean (SE) | ||||
| Intervention | - | 8.4 (1.2) *** | 8.7 (1.2) *** | 9.5 (1.2) *** |
| Control | - | 1.9 (1.2) | 2.5 (1.2) * | 1.8 (1.3) |
| Diff (I-C) | - | 6.5 (1.7) *** | 6.2 (1.7) *** | 7.7 (1.7) *** |
| Diabetes knowledge (range: 0-14), mean (SE) | ||||
| Intervention | 7.6 (0.3) | 10.0 (0.2) | 9.9 (0.3) | 10.3 (0.2) |
| Control | 7.8 (0.3) | 8.2 (0.3) | 8.5 (0.3) | 8.3 (0.3) |
| Diff (I-C) | −0.2 (0.4) | 1.8 (0.4) *** | 1.4 (0.4) *** | 1.9 (0.3) *** |
| Changes from baseline, mean (SE) | ||||
| Intervention | - | 2.4 (0.2) *** | 2.3 (0.2) *** | 2.7 (0.2) *** |
| Control | - | 0.4 (0.2) | 0.7 (0.2) ** | 0.5 (0.2) * |
| Diff (I-C) | - | 2.0 (0.3) *** | 1.6 (0.3) *** | 2.1 (0.3) *** |
| DM Quality of Life (range: 0-75), mean (SE) | ||||
| Intervention | 50.1 (1.1) | 55.8 (0.9) | 56.2 (1.0) | 57.6 (1.0) |
| Control | 51.0 (1.1) | 51.0 (1.0) | 51.8 (1.0) | 49.9 (1.0) |
| Diff (I-C) | −0.9 (1.5) | 4.8 (1.3) *** | 4.4 (1.4) ** | 7.7 (1.3) *** |
| Changes from baseline, mean (SE) | ||||
| Intervention | - | 5.7 (0.9) *** | 6.1 (0.9) *** | 7.5 (0.9) *** |
| Control | - | −0.0 (0.9) | 0.8 (0.9) | −1.1 (0.9) |
| Diff (I-C) | 5.8 (1.3) *** | 5.3 (1.3) *** | 8.6 (1.3) *** | |
| Attitudes toward diabetes (range: 10-50), mean (SE) | ||||
| Intervention | 32.7 (0.7) | 33.9 (0.7) | 34.7 (0.7) | 34.7 (0.8) |
| Control | 34.4 (0.7) | 33.1 (0.6) | 33.7 (0.6) | 32.8 (0.7) |
| Diff (I-C) | −1.7 (1.0) | 0.8 (1.0) | 1.0 (1.0) | 1.9 (1.0) |
| Changes from baseline, mean (SE) | ||||
| Intervention | - | 1.2 (0.6) * | 2.0 (0.6) ** | 2.0 (0.7) ** |
| Control | - | − 1.4 (0.6) * | −0.8 (0.6) | − 1.6 (0.7) * |
| Diff (I-C) | - | 2.6 (0.9) ** | 2.7 (0.9) ** | 3.6 (0.9) *** |
| Depression: PRQ-9K (range: 0-27), mean (SE) | ||||
| Intervention | 5.3 (0.5) | 5.2 (0.5) | 4.6 (0.4) | 4.8 (0.5) |
| Control | 5.4 (0.5) | 4.2 (0.4) | 4.6 (0.5) | 4.1 (0.4) |
| Diff (I-C) | −0.1 (0.7) | 1.0 (0.6) | 0.0 (0.6) | 0.7 (0.6) |
| Changes from baseline, mean (SE) | ||||
| Intervention | - | −0.1 (0.4) | −0.6 (0.4) | −0.5 (0.5) |
| Control | - | − 1.2 (0.3) *** | − 0.8 (0.4) * | − 1.3 (0.4) ** |
| Diff (I-C) | - | 1.1 (0.5) * | 0.2 (0.5) | 0.8 (0.6) |
Note: Boldface indicates statistical significance (*p<0.05, **p<0.01, ***p<0.001).
Discussion
SHIP-DM is effective in improving DM control among members of a linguistically isolated ethnic minority immigrant group. Although both groups showed a reduction in A1c during the 12-month study, the intervention group reduction rates were especially noteworthy. First, the magnitudes of reduction in A1c in the intervention group were on a par with or greater than those seen in other clinical trials.26-33 Second, in addition to the significant differences between the intervention and control groups, the reductions in both groups were sustained over the course of 1 year, with evidence of further potential reductions if the intervention continued beyond the study period, although the effects would not be as substantial as those observed within the first 3 months. Finally, the A1c reductions in the intervention group were not only statistically significant but also clinically significant,34 as were the reductions in the control group. Furthermore, the intervention demonstrated significant improvement in important clinical indicators of cardiovascular health, such as reductions in blood glucose, total cholesterol, and LDL levels. Altogether, these improvements are known (based on population-level data) to reduce DM-related morbidity and mortality35-37 by reducing the overall cardiovascular risks of people with DM.
SHIP-DM also improved DM-related psychobehavioral outcomes, including self-efficacy of DM self-management and DM knowledge. Consequently, the DM-related quality of life score was significantly improved, and, more importantly, these statistically significant improvements were sustained for 12 months.
When compared with previous studies of behavioral interventions for DM, our study is unique in several aspects. First, to the best of our knowledge, it is the first full-scale DM management and control trial to follow the spirit and principles of community-based participatory research in their truest sense. The study center is an independent nonprofit community agency and is not affiliated with any academic or healthcare institution, nor does it provide healthcare services other than wellness education. The center works closely with local primary healthcare providers, community/faith-based organizations, local/ethnic mass media, and local health departments to promote health in the community. Through this rapport, it was possible to design health promotion programs to address the unique needs of the KA community, to reach out to KAs for recruitment and enrollment in natural community settings, and to mobilize participants’ commitment to improving their wellness and that of their family and community.
Second, at the core of the intervention delivery consisted of the RN–CHW teams, who were themselves part of the KA community. RNs were in charge of education and counseling of participants with complex problems, and they were the participants’ main contact with the primary care providers; the CHWs were in charge of outreach/recruitment and counseling of other participants. Because the investigators and the RN–CHW teams were bilingual in English and Korean, and because the educational materials were available in both languages, all stakeholders, including researchers, staff, participants, and community leaders, were able to engage in effective communication without the assistance of interpreters, resulting in efficient and timely decision making by consensus. Furthermore, because of the slim-lined operational structure at the KRC, a relatively low-cost but effective and client-centered intervention program for DM management and control became very feasible in the KA community.
Finally, it is noteworthy that the control group also showed reductions in A1c and other DM-related outcome indicators, implying that program participation alone, without intense intervention, had some beneficial effects. We speculate that many of study activities such as handing out a brief educational brochure and having A1c tested every 3 months raised the awareness and maintenance of desirable behaviors in glucose control in general. Similar improvements have been published in many previous clinical trials of behavioral interventions, including our recent blood pressure control study involving KA seniors.38
Limitations
It should be noted that SHIP-DM has several limitations for making inferences from the findings. First, it was a single-center program targeting only one ethnic minority group. Expansion to multiple centers, including other ethnic groups, is warranted. Second, insufficient information is provided in terms of evaluating the cost effectiveness of the intervention.
Conclusions
The positive clinical and psychobehavioral outcomes of this community-partnered intervention underscore its potential as a model for best practices in the Korean and other linguistically isolated underserved ethnic communities.
Acknowledgments
The study was supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R18 DK083936), with material support from LifeScan, including devices (OneTouch glucometer, OneTouch UltraSoft test strips, and OneTouch UltraSoft lancets) for study participants. In addition, the Johns Hopkins Institute for Clinical and Translational Research supported the cost of blood serum lab tests. The authors are grateful for substantial editorial assistance provided by Dr. Deborah McClellan and Ms. Juyoung Lee at the University of Texas at Austin, School of Nursing. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH and other supporters. Clinical Trials Registration: identifier NCT01264796.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Fonseca VA, Kirkman MS, Darsow T, Ratner RE. The American Diabetes Association diabetes research perspective. Diabetes Care. 2012;35(6):1380–1387. doi: 10.2337/dc12-9001. http://dx.doi.org/10.2337/dc12-9001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. http://dx.doi.org/10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Chow EA, Foster H, Gonzalez V, McIver L. The disparate impact of diabetes on racial/ethnic minority populations. Clinical Diabetes. 2012;30(3):130–133. http://dx.doi.org/10.2337/diaclin.30.3.130. [Google Scholar]
- 4.Peek ME, Ferguson M, Bergeron N, Maltby D, Chin MH. Integrated community-healthcare diabetes interventions to reduce disparities. Curr Diabetes Rep. 2014;14(3):467–474. doi: 10.1007/s11892-013-0467-8. http://dx.doi.org/10.1007/s11892-013-0467-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pistulka GM, Winch PJ, Park HJ, Han HR, Kim MT. Maintaining an outward image: a Korean immigrant’s life with type 2 diabetes mellitus and hypertension. Qual Health Res. 2012;22(6):825–834. doi: 10.1177/1049732312438778. http://dx.doi.org/10.1177/1049732312438778. [DOI] [PubMed] [Google Scholar]
- 6.Han HR, Kim JY, Kim MT, Kim KB. Measuring health literacy among immigrants with a phonetic primary language: a case of Korean American women. J Immigr Minor Health. 2011;13(2):253–259. doi: 10.1007/s10903-010-9366-0. http://dx.doi.org/10.1007/s10903-010-9366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Pub Health. 2004;25(1):357–376. doi: 10.1146/annurev.publhealth.25.101802.123107. http://dx.doi.org/10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- 8.Chin MH, Clarke AR, Nocon RS, et al. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med. 2012;27(8):992–1000. doi: 10.1007/s11606-012-2082-9. http://dx.doi.org/10.1007/s11606-012-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Betancourt JR, Duong JV, Bondaryk MR. Strategies to reduce diabetes disparities: an update. Curr Diabetes Rep. 2012;12(6):762–768. doi: 10.1007/s11892-012-0324-1. http://dx.doi.org/10.1007/s11892-012-0324-1. [DOI] [PubMed] [Google Scholar]
- 10.Green LW, Kreuter MW. Health promotion planning: an educational and environmental approach. 2nd ed Mayfield Publishing; Mountainview, CA: 1991. [Google Scholar]
- 11.Braden CJ. Learned self-help response to chronic illness experience: a test of three alternative learning theories. Sch Inq Nurs Pract. 1990;4(1):23–41. [PubMed] [Google Scholar]
- 12.Kim MT, Han HR, Hedlin HK, Kim JY, Kim KB, Hill MN. Tele-transmitted monitoring of blood pressure and bilingual nurse counseling-sustained improvements in blood pressure control during 12 months in hypertensive Korean Americans. J Clin Hypertens (Greenwich, Conn) 2011;13(8):605–612. doi: 10.1111/j.1751-7176.2011.00479.x. http://dx.doi.org/10.1111/j.1751-7176.2011.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim MT, Han HR, Song HJ, et al. A community-based, culturally tailored behavioral intervention for Korean Americans with type 2 diabetes. Diabetes Educ. 2009;35(6):986–994. doi: 10.1177/0145721709345774. http://dx.doi.org/10.1177/0145721709345774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song HJ, Han HR, Lee JE, et al. Translating current dietary guidelines into a culturally tailored nutrition education program for Korean American immigrants with type 2 diabetes. Diabetes Educ. 2010;36(5):752–761. doi: 10.1177/0145721710376328. http://dx.doi.org/10.1177/0145721710376328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merzel C, D’Afflitti J. Reconsidering community-based health promotion: promise, performance, and potential. Am J Public Health. 2003;93(4):557–574. doi: 10.2105/ajph.93.4.557. http://dx.doi.org/10.2105/AJPH.93.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Israel BA, Coombe CM, Cheezum RR, et al. Community-based participatry research: a capacity- building approach for policy advocacy aimed at eliminating health disparties. Am J Public Health. 2010;100(11):2094–2102. doi: 10.2105/AJPH.2009.170506. http://dx.doi.org/10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han HR, Kang JH, Kim KB, Ryu JP, Kim MT. Barriers to and strategies of recruiting Korean Americans for community-partnered health promotion research. J Immigr Minor Health. 2007;9(2):137–146. doi: 10.1007/s10903-006-9022-x. http://dx.doi.org/10.1007/s10903-006-9022-x. [DOI] [PubMed] [Google Scholar]
- 18.American Diabetes Association Standards of medical care in diabetes-2010. Diabetes Care. 2010;33(Suppl. 1):S11–S61. doi: 10.2337/dc10-S011. http://dx.doi.org/10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diabetes Prevention Program (DPP) Research Group The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2000;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han CS, Jo SA, Kwak JH, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008;49(2):218–223. doi: 10.1016/j.comppsych.2007.08.006. http://dx.doi.org/10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21(5):706–710. doi: 10.2337/diacare.21.5.706. http://dx.doi.org/10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 22.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256–262. [PubMed] [Google Scholar]
- 23.Davis PD, Dennis JL, Railton R. Evaluation of the A&D UA-767 and Welch Allyn Spot Vital Signs noninvasive blood pressure monitors using a blood pressure simulator. J Human Hypertens. 2005;19(3):197–203. doi: 10.1038/sj.jhh.1001804. [DOI] [PubMed] [Google Scholar]
- 24.Jacobson A, Barofsky I, Cleary P, Rand L, The DCCT Research Group Reliability and validity of a diabetes quality-of-life measure for the diabetes control and complications trial (DCCT) Diabetes Care. 1988;11(9):725–732. doi: 10.2337/diacare.11.9.725. http://dx.doi.org/10.2337/diacare.11.9.725. [DOI] [PubMed] [Google Scholar]
- 25.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. http://dx.doi.org/10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 26.Thom DH, Ghorob A, Hessler D, De Vore D, Chen E, Bodenheimer TA. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013;11(2):137–144. doi: 10.1370/afm.1443. http://dx.doi.org/10.1370/afm.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sevick MA, Korytkowski M, Stone RA, et al. Biophysiologic outcomes of the enhancing adherence in type 2 diabetes (ENHANCE) trial. J Acad Nutr Diet. 2012;112(2):1147–1157. doi: 10.1016/j.jand.2012.05.008. http://dx.doi.org/10.1016/j.jand.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwartz AV, Johnson KC, Kahn SE, et al. Effect of 1 year of an intentional weight loss intervention on bone mineral density in type 2 diabetes: results from the Look AHEAD randomized trial. J Bone Miner Res. 2012;27(3):619–627. doi: 10.1002/jbmr.1483. http://dx.doi.org/10.1002/jbmr.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schillinger D, Handley M, Wang F, Hammer H. Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: a three-arm practical clinical trial. Diabetes Care. 2009;32(4):559–566. doi: 10.2337/dc08-0787. http://dx.doi.org/10.2337/dc08-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009;35(4):641–651. doi: 10.1177/0145721709335006. http://dx.doi.org/10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- 31.Krein SL, Klamerus ML, Vijan S, et al. Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med. 2004;116(11):732–739. doi: 10.1016/j.amjmed.2003.11.028. http://dx.doi.org/10.1016/j.amjmed.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 32.Hill-Briggs F, Lazo M, Peyrot M, et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med. 2011;26(9):972–978. doi: 10.1007/s11606-011-1689-6. http://dx.doi.org/10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DePue JD, Dunsiger S, Seiden AD, et al. Nurse-community health worker team improves diabetes care in American Samoa: results of a randomized controlled trial. Diabetes Care. 2013;36(7):1947–1953. doi: 10.2337/dc12-1969. http://dx.doi.org/10.2337/dc12-1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu PC, Bosnyak Z, Ceriello A. The importance of glycated hemoglobin (HbA1c) and postprandial glucose (PPG) control on cardiovascular outcomes in patients with type 2 diabetes. Diabetes Res Clin Pract. 2010;89(1):1–9. doi: 10.1016/j.diabres.2009.12.009. http://dx.doi.org/10.1016/j.diabres.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Brinke RT, Dekker N, de Groot M, Ikkersheim D. Lowering HbA1c in type 2 diabetics results in reduced risk of coronary heart disease and all-cause mortality. Prim Care Diabetes. 2008;2(1):45–49. doi: 10.1016/j.pcd.2007.12.004. http://dx.doi.org/10.1016/j.pcd.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 36.Xu L, Chan WM, Hui YF, Lam TH. Association between HbA1c and cardiovascular disease mortality in older Hong Kong Chinese with diabetes. Diabetes Med. 2012;29(3):393–398. doi: 10.1111/j.1464-5491.2011.03456.x. http://dx.doi.org/10.1111/j.1464-5491.2011.03456.x. [DOI] [PubMed] [Google Scholar]
- 37.Gary TL, Batts-Turner M, Yeh HC, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2009;169(19):1788–1794. doi: 10.1001/archinternmed.2009.338. http://dx.doi.org/10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim KB, Han HR, Huh BY, Nguyen T, Lee HB, Kim MT. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27(9):1199–1208. doi: 10.1093/ajh/hpu041. http://dx.doi.org/10.1093/ajh/hpu041. [DOI] [PMC free article] [PubMed] [Google Scholar]