Abstract
Youth with autism spectrum disorders frequently experience significant symptoms of anxiety. Empirically supported psychosocial interventions exist, yet access is limited, especially for families in rural areas. Telehealth (i.e. videoconferencing) has potential to reduce barriers to access to care; however, little is known about the feasibility or efficacy of directly intervening with youth with autism spectrum disorders through this modality. This study details the pilot testing of a telehealth version of an empirically supported intervention targeting anxiety in youth with autism spectrum disorders. The primary focus of this study is on feasibility, with evaluation of outcomes as a starting point for future randomized trials. In all, 33 families of youth with autism spectrum disorders and significant anxiety symptoms participated in this study (Telehealth Facing Your Fears (FYF) Intervention: n = 17; Wait-list control: n = 16). Youth of all functioning levels were included. Acceptability was strong; however, the usability of the technology was problematic for some families and impeded some sessions significantly. Fidelity of the telehealth version to the critical elements of the original, in vivo version was excellent. More work is needed to improve delivery of exposure practices and parent coaching. Preliminary efficacy analyses are promising, with improvements observed in youth anxiety over time (relative to a comparison group waiting for live intervention) and parent sense of competence (within group). Clearly, stronger designs are necessary to evaluate efficacy sufficiently; however, this study does provide support for further investigation of clinic-to-home videoconferencing as a direct intervention tool for youth with autism spectrum disorders and their parents.
Keywords: autism, co-occurring anxiety, intervention, feasibility, telehealth
Introduction
Youth with autism spectrum disorders (ASD) frequently experience clinically significant symptoms of anxiety, which can interfere with adaptive functioning at home, at school, and in the community (Van Steensel et al., 2012). Over the past decade, several research groups have presented evidence supporting modified cognitive-behavioral treatment (CBT) as a promising intervention for youth with ASD (Reaven et al., 2012; White et al., 2010; Wood et al., 2009). In a recent Agency for Healthcare Research and Quality (AHRQ) comparative effectiveness report on interventions for youth with ASD, the strength of evidence supporting CBT approaches to treating anxiety in verbal youth with ASD was described as “High” (i.e. “high confidence that the evidence reflects the true effect, AHRQ, 2014: 15). Outcomes reported in several randomized controlled trials of short-term cognitive-behavioral interventions include clinically significant reductions in anxiety symptom severity, loss of anxiety diagnoses, increased participation in school, family and community activities, as well as gains in overall psychological well-being (Chalfant et al., 2007; Reaven et al., 2012; Sofronoff et al., 2005; Storch et al., 2013; White et al., 2010; Wood et al., 2009). There is also growing evidence that parents and family members experience positive outcomes associated with improved coping in the family member with ASD (Weiss et al., 2012).
Unfortunately, there are many obstacles that impact access to evidence-based mental health supports for youth with ASD. First, there is a workforce shortage, complicated, perhaps, by a lack of specialized training programs that prepare mental health providers to treat individuals with intellectual and/or developmental disorders (National Institutes of Health (NIH) Workshop on Mental Health in Intellectual/Developmental Disabilities: Research Challenges and Opportunities, 2014). Similarly, the majority of professionals who specialize in autism intervention (such as behavior analysts) are trained in education, not psychology (Shook, 2005). Second, many youth with ASD—particularly as they reach adolescence—resist attending intervention sessions in clinic settings, resulting in transition difficulties that some parents report significantly hamper treatment participation (Sofronoff et al., 2005). For youth who are anxious, leaving a familiar environment for treatment may be particularly aversive (Albano and Barlow, 1996). Third, for many families, traveling to and from a clinic on a school day can be stressful, time-consuming, and expensive, particularly if there are other children in the home who will need supervision (Reed et al., 2007). For families in rural areas—or those who live far away from specialty clinics—access to health care (both physical and mental) is significantly lacking (Liptak et al., 2008; Kogan et al., 2008; Mandell et al., 2010).
One promising strategy for overcoming these obstacles to mental health treatment is telehealth, specifically clinic-to-home videoconferencing, which allows for both synchronous (i.e. real-time) and asynchronous (i.e. recorded) clinician–patient interactions through the use of web cameras on personal computers. Within the general pediatric literature on the use of videoconferencing, cognitive-behavioral approaches are strongly represented, possibly due to the portability and structure of the critical elements inherent to this therapeutic approach (Richardson et al., 2009). Clinical researchers in community mental health settings have reported significant treatment effects of telehealth delivery of psychosocial interventions to children and teens, across a variety of mental health conditions, including anxiety and depression (Nelson and Palsbo, 2006), attention deficit disorder (Myers, Vander Stoep and Lobdell, 2013), psychosis (Yellowlees et al., 2008), and mood disorder (Pignatiello et al., 2011).
Telehealth delivery of psychosocial interventions may fit particularly well with the social style, interests, and learning strengths of persons with ASD. Videoconferencing could be viewed as preferable to a “face-to-face” encounter with a therapist for many youth, particularly those who are shy or resist changes in their environment (Boydell et al., 2010). Incorporation of technologically based interventions into educational activities has been shown to increase task engagement in persons with ASD, including those with moderate to severe symptoms (Goodwin, 2008; Kimball and Smith, 2007). Videoconferencing is thought to be appealing to visual learners (Pacifici et al., 2006), a style characterizing many persons with ASD (Cohen and Sloan, 2007). Parents, especially those from rural areas, may appreciate the relative convenience and efficiency of accessing specialized clinical care without leaving home.
In autism research, telehealth interventions have been shown to be both feasible and potentially efficacious across a variety of practice encounters, including early intervention (Rule et al., 2006), parent training (Kobak et al., 2011), parent coaching (Vismara et al., 2009), provider preparation (Brookman-Frazee et al., 2012; Gibson et al., 2010; Machalicek et al., 2010; Vismara et al., 2009), diagnostic assessment (Savin et al., 2006), and functional behavior assessment (Barretto et al., 2006; Machalicek et al., 2009). See Boisvert et al. (2010) for review. As of this writing, there are no published studies of the feasibility or efficacy of using videoconferencing to deliver cognitive-behavioral treatment directly to youth with ASD.
Therefore, the purpose of the present pilot study is to examine the feasibility and preliminary efficacy of a tele-health version of an evidence-based approach to anxiety intervention for youth with ASD, in preparation for a randomized controlled trial. Specifically, the research team modified a manualized, family-focused, cognitive-behavioral group intervention for anxiety for youth with ASD (Facing Your Fears: Group Therapy for Managing Anxiety in Children with High-Functioning Autism; Reaven et al., 2011) for delivery via clinic-to-home videoconferencing. We hypothesized that telehealth delivery of the FYF Intervention would be feasible and potentially efficacious in reducing anxiety symptoms and fears in youth with ASD.
Method
This is a pilot study of the feasibility and potential efficacy of a telehealth version of FYF (Reaven et al., 2011), a manualized, evidenced-based psychosocial intervention for anxiety in youth with ASD. Treatment is delivered in a small group format, comprised of four to six parent–youth dyads. The group format, as described in Reaven et al. (2011), provides social support as well as social learning and generalization opportunities for both parents and youth with ASD. Thus, the telehealth version was also designed for delivery in a small, multi-family group format.
Feasibility variables studied in this pilot include acceptability of intervention to parents and youth with ASD (i.e. recruitment and enrollment rates, treatment completion, session attendance, satisfaction ratings), usability of technology (i.e. frequency of technical problems), and therapist fidelity to critical elements of the original intervention. Pre- and post-measures of youth and parent functioning were also collected to obtain preliminary assessments of efficacy (e.g. youth anxiety symptoms, parent self-efficacy).
Participants
Telehealth FYF sample
In all, 17 families (i.e. each represented by one parent and one youth with ASD and anxiety) from rural and frontier communities in a western state participated in the Telehealth FYF pilot study. All data on feasibility and parent outcomes are based on this sample. Participants were recruited through community workshops, webinars, focus groups, and regional conference presentations in rural parts of the state. Information about project activities was disseminated through electronic newsletters published by JFK Partners, the University Center for Excellence in Developmental Disabilities at the University of Colorado School of Medicine, and several statewide parent groups. Families interested in participating were asked to contact project staff by phone or email. Staff conducted a brief screening for eligibility for the project and participants were engaged in treatment in the order of referral.
Inclusion/exclusion criteria
Inclusion criteria for the youth were as follows: (1) males and females between the ages of 7 and 19 years; (2) current clinical diagnosis of ASD, as documented in an evaluation report that included the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000), administered within the past 5 years by a reliable administrator, or confirmed in a live evaluation by one of the study psychologists on an outreach visit; (3) current scores on the Social Responsiveness Scale (Constantino and Gruber, 2002) that are indicative of moderate risk of autism or greater; (4) indication of clinically significant symptoms of anxiety, as operationalized as obtaining a score of 25 or higher by parent report on the Screening for Childhood Anxiety and Related Emotional Disorders (SCARED; Birmaher et al., 1999); and (5) currently residing more than a 45-min drive from a specialty medical center where intervention was available clinically, and also within state lines (due to licensing requirements). Because the over-arching goal of this study is to examine ways to reduce barriers to psychosocial intervention, we decided to include youth of all functioning levels into this feasibility study. See “Intervention” for information on how the treatment was individualized to meet the needs of participants with impaired/disordered language skills.
Exclusion criteria were as follows: (1) primary mental health diagnosis of a mood disorder, thought disorder, or other psychiatric condition that a study psychologist determined was a more critical target for intervention than anxiety symptoms and (2) severity of mental health conditions that warranted more intensive or more individualized treatment than provided by the experimental intervention.
Inclusion criteria for the parents were as follows: (1) parent or primary caregiver of a youth with ASD and anxiety (as described above); (2) willingness to participate actively in a 10-week, 1-h per week, interactive, multi-family therapy group facilitated by a licensed clinical psychologist or postdoctoral fellow and delivered via videoconferencing; (3) access to a personal computer and internet services with consent to allow the project to supplement hardware, memory, internet connection, and/or processing speed in order to support videoconferencing, or willingness to borrow a project computer equipped to support the project; and (4) willingness to refrain from simultaneously participating in psychological treatment specifically focused on reducing anxiety symptoms in the youth with ASD. Exclusion criteria for parents were: (1) inability to speak and understand English fluently; (2) parent did not reside with the youth with ASD at least 50% of the time; and (3) parent and youth did not reside in Colorado (as required by licensing board).
Comparison group
In order to evaluate the preliminary efficacy of the telehealth version of FYF, secondary data from a companion project were utilized to comprise a comparison group. It is important to note that this was not a pure “wait-list” group, in the sense that participants were not recruited simultaneously with those in the active treatment group reported here. Rather, the comparison group includes youth with ASD and anxiety who qualified for inclusion into the intervention studies of the FYF program, and who entered a wait-list and completed a second set of measures 3 months into their waiting period. Thus, at the time of these analyses, there were 37 youth for whom a parent completed the SCARED at pre-intervention and 3 months later, which is roughly equivalent with the time between the telehealth FYF pre- and post-measures (mean number of days between pre- and post-testing = 104.2, SD = 16.4). A pairwise matching procedure was conducted by a research assistant not affiliated with this study to create a comparison group matched by gender, age (in years), verbal fluency (based on ADOS module). Preliminary tests showed that there were no significant differences between the Comparison Group and Telehealth FYF in intellectual functioning (i.e. IQ categories, see Table 1: χ2(3, 30) = 0.78, p = 0.85) or severity of anxiety symptoms before treatment: F(1, 32) = 0.52, p = 0.48. Recruitment procedures were similar. All inclusion–exclusion criteria applied to the Comparison Group except for the requirement to live a certain distance from specialty autism clinics. Thus, the two groups differ on community type, χ2(2, 31) = 13.27, p = 0.001. Families in the Comparison Group were much less likely to live in rural-non-metropolitan communities. See Table 1 for participant characteristics.
Table 1.
Participant characteristics.
| Telehealth FYF (n = 17)
|
Wait-list FYF (n = 16)
|
|
|---|---|---|
| Mean (SD) or n (%) | Mean (SD) or n (%) | |
| Youth characteristics | ||
| Age (in years) | 11.53 (2.67) | 12.12 (1.96) |
| Sex | ||
| Males | 14 (82.4%) | 13 (81.3%) |
| Females | 3 (17.6%) | 3 (18.8%) |
| Ethnicity | ||
| Hispanic | 2 (11.8%) | 5 (31.3%) |
| Race | ||
| Caucasian | 15 (88.2%) | 14 (87.5%) |
| African American | 1 (5.9%) | 2 (12.5%) |
| Asian | 0 | 0 |
| Native American | 1 (5.9%) | 0 |
| Intellectual functioning (IQ categories derived from nonverbal IQ) | ||
| High (≥ 115) | 2 (11.8%) | 1 (6.3%) |
| Average (85–114) | 10 (58.8%) | 10 (62.5%) |
| Borderline (70–84) | 4 (23.5%) | 4 (25%) |
| Impaired (<70) | 1 (5.9%) | 1 (6.3%) |
| Verbal ability | ||
| Verbally fluent | 13 (76.5%) | 14 (87.5%) |
| Mixed spontaneous/stereotyped | 3 (17.6%) | 1 (6.3%) |
| Primarily stereotyped | 1 (5.9%) | 1 (6.3%) |
| No vocal attempts | 0 | 0 |
| Educational placement | ||
| Homebound | 3 (17.6%) | 1 (6.3%) |
| Primarily self-contained | 0 | 2 (12.5%) |
| General and special education/direct | 9 (52.9%) | 11 (68.8%) |
| General and special education/consult | 5 (29.4%) | 2 (12.5%) |
| General education only | 0 | 0 |
| Anxiety symptoms at baseline | 30.94 (9.34) | 28.25 (11.96) |
| Family characteristics | Telehealth FYF (n = 17) | Wait-list FYF (n = 16) |
| Mother’s education | ||
| High school graduate | 2 (11.8%) | 4 (25%) |
| Some college | 9 (52.4%) | 4 (25%) |
| College degree | 4 (23.5%) | 5 (31.3%) |
| Post-graduate work | 2 (11.8%) | 3 (18.8%) |
| Community type | ||
| Urban | 0 | 5 (31.3%) |
| Rural/metropolitan | 5 (29.4%) | 9 (56.3%) |
| Rural/non-metropolitan | 12 (70.6) | 2 (12.5%) |
FYF: Facing Your Fears; SD: standard deviation.
Intervention
The telehealth version of the FYF intervention was designed to include the critical elements of the FYF intervention, with modifications for delivery over videoconferencing. FYF is usually delivered in a clinic or school setting, in a multi-family group format, for 12 1.5-h sessions across a 3- to -4-month period. Each session is supported by a chapter in a Facilitator’s Manual, a Parent’s Manual, and a Youth Workbook. The first six sessions focus on psychoeducational aspects of anxiety (i.e. recognizing that different people have different worries/fears, anxiety is experienced on a continuum of severity, anxiety impacts how your body feels and what your brain thinks about, etc.). The second six sessions build upon the psychoeducational curricula by promoting the development and implementation of youth-specific anxiety reduction strategies, with the goal of reducing the interference of anxiety and supporting the youth’s ability to cope with small amounts of physiological and cognitive distress. Each parent and youth dyad creates an exposure hierarchy for a specific fear, identifies specific tools the youth finds useful for coping, and practices facing the targeted fears in small, frequent exposure opportunities. Parents are active intervention agents in the FYF approach and are encouraged to serve as coaches for the youth as they practice managing and facing fears in “real-life” situations, and subsequently share their progress with the group. The group format is important for addressing the social aspect of many worries and fears presented by youth with ASD, as well as to decrease isolation and generate a sense of social support among participants. FYF incorporates evidence-based cognitive-behavioral elements, such as psycho-education about anxiety and the mind–body connection, somatic management, cognitive strategies (e.g. “helpful” thoughts), emotion regulation, and graded exposure or facing fears a little at a time (Connolly et al., 2007). Modifications for youth with ASD are integrated throughout the FYF intervention and include provision of visual supports, predictable session routines, video modeling activities, and repetition of key concepts. See Reaven et al. (2011) for more information on the original intervention. See Table 2 for a comparison of the live and telehealth versions of the intervention.
Table 2.
Modifications to live version of FYF for delivery via Telehealth.
| Intervention feature | FYF (Original) approach | Telehealth modification |
|---|---|---|
| Number of sessions | 14 + 1 booster | 10 + 1 booster |
| Length of sessions | 1.5 hours (for both youth and parents) | 1.0 hour (some time spent with only parents) |
| Group size | 4–6 families | 2–4 families |
| Intervention targets | Separation anxiety, generalized anxiety, specific, and social phobia | Same targets |
| Expectations for child vs. parent participation | Parents and youth participate in same dosage of intervention | Parents engage in larger dose of intervention relative to youth |
| Session format | Varies; includes large group discussion, parent–youth dyads, parent only, and youth only | Similar to FYF, but briefer parent–youth activities; no youth only activities |
| Session elements | Visual schedule | Visual schedule |
| Weekly “check-in” | Weekly “check-in” | |
| Mini lesson w/activity | Mini lesson w/activity | |
| Homework | Homework | |
| Therapeutic tools | Video Project: Youth collaborate to create “Face Your Fears” videos and show to parents at end of intervention | Video Project: Parent and youth collaborate to film the youth either facing fears in real time or role-playing an exposure to show to peers at end intervention |
FYF: Facing Your Fears.
The telehealth intervention was individualized to fit the needs of each small group, as is accepted practice in “real-life” implementation of manualized treatments (Kendall and Beidas, 2007). Of the six multi-family groups in this study, one 2-family group required more individualization and modification than the others, due to the markedly disordered language skills noted in both adolescent male participants. Practice exercises and homework activities were modified to meet the needs of these families. Although these youth did not demonstrate the communicative competence to engage in all of the activities that were presented to the other cohorts in the pilot study, their mothers did complete all of the content areas and fidelity assessment supported the finding that the critical elements of the intervention were in practice.
Videoconferencing platform
The over-arching goal of this project is to improve access to mental health services; therefore, it was important that the videoconferencing program used in the study be affordable and commercially available for home use. In order to implement the multi-family treatment model of the original FYF program, a platform that allowed for up to six simultaneous users was necessary. Confidentiality and security of transmissions was also a high priority. The program that met our needs was OoVoo (http://www.oovoo.com). The screen configuration included a window for each of the participating families and therapists; thus, if four families were interacting in a group with a therapist, five equally sized windows were visible to all participants. Using webcams and either headsets or built-in microphones, each parent and child at each participating home could hear and see every other dyad. The therapist was always on camera as well. Families were encouraged to mute their microphones when others were talking; otherwise, the interactions were dynamic and involved rotating participation and discussion, along with brief didactics (“lessons”) delivered by therapists. In order to provide additional time to support the parents in their challenging role as coaches, the youth usually left the session approximately 20–30 min before the parents and therapists.
Measures
Participant characterization
Demographic form
This is a 3-page form completed by participating parents and includes demographic information, such as the youth’s age, gender, school placement, medical history, family constellation, parent education, and income.
Documentation of diagnosis of autism spectrum disorder
Participating families in the Telehealth FYF group provided a copy of a clinical evaluation to document the youth’s clinical diagnosis of ASD. One of the study psychologists reviewed the report and determined if the evaluation had been conducted by a qualified professional, included a measure of parent report of symptoms, and provided algorithm scores for an ADOS that was administered within the past 3 years by a trained and reliable administrator. If these criteria were not met, a study psychologist administered the missing measure. Two parents completed an Autism Diagnostic Interview–Revised (ADI-R) with a trained clinician via videoconferencing to supplement the ADOS data that already existed and three youth completed an ADOS with a trained clinician during a home visit. All participants in the Comparison Group completed the diagnostic battery with a research clinician at the University of Colorado as part of their enrollment in the FYF intervention studies.
Current autism symptoms
Parents completed the Social Responsiveness Scale (SRS; Constantino and Gruber, 2002) on their son or daughter to report current autism symptoms. The SRS provides a total score, several sub-scale scores, and a diagnostic risk classification which has been shown to be concordant with the findings of more labor-intensive diagnostic instruments, such as the ADI–R (Bruni, 2014).
Cognitive and adaptive functioning
For youth in the Telehealth FYF Group, standard scores from cognitive testing and adaptive behavior interviews were abstracted from the evaluation reports and educational records shared by the families with the research team. Standardized cognitive data were available for 16 youth. Specific measures were: Wechsler Intelligence Scales for Children (WISC; Wechsler, 2003; n = 2); Wechsler Abbreviated Scales of Intelligence (WASI; Wechsler, 1999; n = 6); Stanford–Binet Intelligence Scales—5th Edition (Roid, 2003; n= 5); Leiter–Revised (Roid and Miller, 2002; n = 3). These data were used to match participants by age, gender, and overall functioning level in order to promote group cohesion. All youth participants in the Comparison Group completed the WASI as part of the FYF intervention trials.
Feasibility measures (Telehealth FYF only; n = 17)
Participant monitoring form
Project staff maintained a written log of each family’s attendance, completion of treatment, and completion of study measures. Information concerning other interventions, medication changes, and significant events impacting the family were also noted during the duration of the intervention and wait-list period.
Parent and youth satisfaction ratings
Parents and youth independently completed a web-based satisfaction measure during Sessions 4 and 9. The 12-item scale incorporates a Likert rating from 1 to 5 (higher indicating greater satisfaction), and was modified from the satisfaction form used in the “live” version of FYF.
Treatment fidelity checklist
The therapist team developed a Fidelity Checklist based upon the critical elements of the original FYF intervention (adapted from Reaven and Blakeley-Smith, 2009). Therapist fidelity was coded via videotape by a project therapist and research assistant (neither of whom delivered the intervention for the sessions being coded). Items were scored on a 3-point scale, in a manner adapted from the Research Units on Pediatric Psychopharmacology (RUPP) Autism Network studies (2007). Endorsements of “0” indicated that the critical element was not present in the session: a “1” indicated partial adherence to intervention guidelines and a “2” indicated full implementation of the intervention guidelines. All intervention sessions were recorded digitally by the Oovoo program and saved to a secure server. A random sample of four sessions from each of the six cohorts (for a total of 24 sessions) was coded for fidelity to key elements of the FYF intervention program by a psychologist and research assistant. Of these 24 samples, 6 (25%) were coded independently by two raters to assess inter-observer reliability (which exceeded 85% across all double-coded samples). Therapist fidelity was calculated as a percentage of possible points (such that ratings of all “2’s” = 100%).
Log of technical difficulties
A research team member completed a log for each session and noted the duration of the session, the number of disconnections or significant technical glitches in picture and sound, and the number of participants affected.
Analytic plan for assessing feasibility
Variables were evaluated by examining raw data by therapist, by session, and by group cohort. Percentages were summarized for each variable and were comparable across therapists and cohorts, thus are presented for the sample as a whole. We set an a priori goal of 80% as the criteria for all feasibility variables.
Analytic plan for assessing acceptability
Acceptability of the telehealth intervention was evaluated by examining recruitment and enrollment rates, treatment completion, attendance, and youth–parent report on satisfaction questionnaires.
Outcome measures
Primary outcome: youth anxiety symptoms
Parent report of the youth’s anxiety was assessed before and after treatment (3 months), using a web-based portal for self-administration of the Screen for Anxiety and Related Emotional Disorders in Children (SCARED; Birmaher et al., 1999). The SCARED is a 41-item checklist that is used to assess risk of anxiety for school-aged youth and adolescents. It provides a total score, as well as domain scores for Panic, Social Phobia, Generalized Anxiety, Separation Anxiety, and School Phobia with associated cutoffs indicating risk of clinically significant concerns. The SCARED has been documented to be a “potentially appropriate” tool for use in clinical trials (Lecavalier et al., 2013) and studies of psychosocial intervention with youth with ASD (Stern et al., 2014).
Analytic plan
Repeated measures ANOVA (two-way, mixed design) was used to examine whether there is a significant change in youth anxiety symptoms over time (3 months) between youth who participated in Telehealth FYF and youth who were on the wait-list for FYF intervention (Comparison Group). The dependent variable was the total score on parent report version of the SCARED.
Secondary outcomes: parenting sense of competence
The secondary outcome targeted for this study was the parent’s perception of efficacy in the parenting role, as measured by the Parenting Sense of Competence Scale (PSOC; Johnston and Mash, 1989). This brief parent checklist includes an Efficacy Subscale, which measures the degree to which a parent perceives himself or herself as competent in parenting a child in challenging situations. This scale has been used in other family-focused interventions and is sensitive to change (Jones and Prinz, 2005).
Analytic plan
Repeated measures ANOVA (oneway within subjects) was used to examine whether there is a significant change in parenting sense of competence between pre-treatment and post-treatment of the Telehealth FYF intervention. Data were not available for this variable for the Comparison Group.
Results
Feasibility (acceptability, usability, and fidelity; examined on subsample: Telehealth FYF; n = 17)
Recruitment and enrollment
In all, 52 parents contacted the research team within a 6-month period to express interest in the study. Of these, the majority did not meet the inclusion criteria for the study (i.e. 18 did not live within the specified geographic area, 6 youth did not meet criteria for ASD, 6 youth did not present with clinically significant anxiety, 3 were older than 19 years). These families were referred to community-based services. Of the 19 families who met inclusion criteria, 17 consented to participate. Multi-family groups were formed in two cohorts of four families (total n = 8 families), one cohort of three families (total n = 3), and three cohorts of two families (total n = 6 families) based upon the youth’s characteristics (i.e. age, gender, functioning level) and the family’s availability. Given the response from the community within a relatively short time frame, recruitment was feasible. Several parents (n = 16) inquired about the program and readily acknowledged that they lived fairly close to the clinic (and thus did not meet study criteria), but were interested in seeing how their child would respond to intervention through a computer. It is important to note that as a research project, the intervention was provided to families without cost, which may impact recruitment rates in real-life practice settings.
Treatment completion
Of the 17 families, 16 who consented to the study completed the 10-session treatment course (attrition: 5.9%).1
Attendance
Overall attendance was approximately 94%. Of the 16 families who participated fully, 8 attended 100% of sessions, 2 missed 2 sessions, and 6 missed 1 session. Additional therapist time was required to deliver the content in an additional telephone or videoconferencing session.
Satisfaction
Sixteen parents and 14 youth completed the satisfaction measures at the 4th and 9th session. The mean Satisfaction score for parents was 92.9%, suggesting high parent satisfaction with the intervention content, delivery method, and alliance with therapist. When asked if they would recommend the program to a friend, 100% of parents responded affirmatively.
The mean Satisfaction score for youth was 88.8%. Younger children tended to report higher levels of enjoyment in the activities than most of the participating adolescents. When asked if they would recommend the program to a friend, 11 of 14 (79%) of participating youth said “yes.” (note: The three who said “no” were all 16–17 years old, with strong verbal skills and ongoing conflicts with their parents regarding rules and responsibilities. Therapist logs for these three families suggested that individual family sessions may have been more helpful than the small group modality, due to the active conflict between the parent and the youth.)
When parents were asked to provide suggestions for improvement in the intervention, responses included focus on sound quality and take steps to enhance for all users; provide all written materials in advance instead of week-by-week; and increase time for parents to talk to therapists without the youth present. Finding ways for therapists to provide live coaching to parents in real-life situations—perhaps through a “bug-in-the-ear” approach was suggested by several parents. Expanding the program to include more parent-to-parent supports was also a common theme in the parent feedback.
Usability of technology
Of the 138 videoconferencing sessions conducted to consent, complete assessments or engage in intervention, 8 (5.8%) were significantly impacted by technical glitches, resulting in one or more families calling in by telephone in order to participate. Examination of technical log data suggests that most glitches occurred early in the course of treatment. Most glitches were thought by the technical team to be caused by “fixable” issues, such as: limited bandwidth, poor sound quality, and audio feedback issues due to equipment settings across users, use of laptops with wireless connections instead of hardwired connections, and background software (including virus protection programs) inhibiting use of the videoconferencing features.
Moderate technical glitches (defined as a brief disconnection with successful re-joining within a few minutes) were more common, with an average occurrence rate of .87/session. Of 17 families, 7 (41%) were disconnected at least one time during the 10-session intervention; 2 families experienced recurrent connection problems during the first five sessions. These disruptions to sessions could be frustrating to families and therapists. Providing families with clear guidelines on how to handle lost connections was an important implementation issue. Some therapists reported that developing a routine where the youth joined the session approximately 10 min in also helped to alleviate frustration. Having ongoing access to a technical support person was also extremely helpful in solving problems in real time.
Fidelity of implementation
Therapist fidelity to the critical elements of the FYF approach was 92.1%. Sessions involving graded exposure tended to be less faithful to the manualized FYF protocol.
Preliminary efficacy (n = 33; entire sample)
Pre- and post-intervention means and standard deviations of parent report of youth anxiety symptoms are reported in Table 3 for the intent-to-treat sample of Telehealth FYF (n = 17, last observation carried forward for 1 youth who dropped out) and the Comparison Group.
Table 3.
Means and standard deviations on the youth- and parent-completed measures for Telehealth FYF and Comparison Group (modified Wait-list).
| Measure | Telehealth FYF (n = 17)
|
Wait-list comparison (n = 16)
|
D | ||
|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | Pre-treatment | Post-wait | ||
| SCARED | .74a | ||||
| M | 30.94 | 26.76 | 28.25 | 32.13 | |
| SD | 9.35 | 8.50 | 11.95 | 12.99 | |
| PSOC | .38b | ||||
| M | 70.44 | 66.44 | N/A | N/A | |
| SD | 10.45 | 10.44 | N/A | N/A | |
SD: standard deviation; FYF: Facing Your Fears; SCARED: Screen for Child Anxiety-Related Emotional Disorders (Birmaher et al., 1999); PSOC: Parent Sense of Competence (Johnston and Mash, 1989).
For both measures, higher scores indicate more problems.
dcorr (Morris, 2007) effect size for mean differences of groups with unequal sample size within a pre- post design.
Cohen’s d (Cohen, 1988).
Primary outcome: youth anxiety symptoms
There was a statistically significant difference between the Telehealth FYF and Comparison Group over time on parent report of youth anxiety, F(1, 31) = 8.73; p = 0.006; Eta squared = .22 (see Figure 1).
Figure 1.
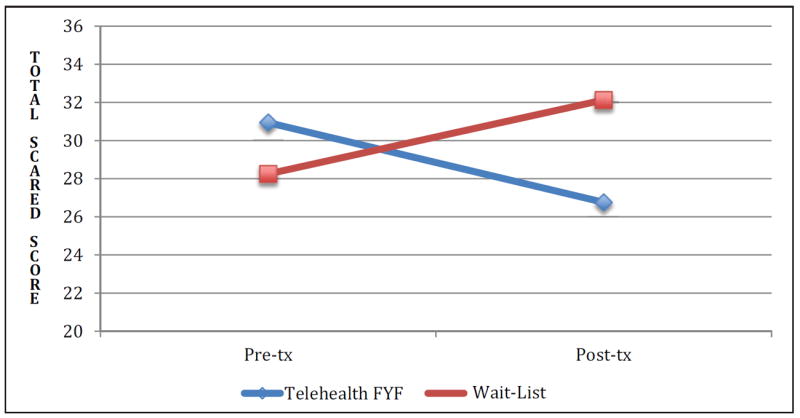
Change in youth anxiety symptoms over time by treatment condition (n = 33).
Secondary outcome: parent sense of competence
There was a statistically significant change in parenting sense of competence between pre- and post-treatment: F(2, 14) = 5.08, p = 0.03. However, this finding should be interpreted cautiously, as participating parents had invested time and effort into the intervention, so may be inclined to report in a positive manner).
Discussion
Results from this pilot study support the feasibility and preliminary efficacy of delivering a modified version of a manualized, CBT multi-family group intervention (i.e. “Facing Your Fears”) to youth with ASD and co-occurring anxiety through commercially available videoconferencing technology. As reflected in the high number of families who expressed interest in the project, there is a great need for the delivery of psychiatric supports for youth in rural areas, particularly those with complex profiles that include ASD. Findings suggest that all parents, most school-aged youth, and some teens found the intervention acceptable. Treatment completion was 93%, session attendance was 94%, and the mean satisfaction ratings for parents and youth 93% and 89%, respectively. Technical problems compromised a small number of sessions and most issues were preventable or fixable. However, having a plan on how to handle these technical problems was clearly essential (e.g. if a family lost a connection and could not immediately reconnect, they called in to the group and participated on a speaker phone rather than further sacrificing session time and content in attempting to reconnect). Therapist fidelity to the key elements of the original FYF manualized intervention was very strong.
Although this study is quasi-experimental and was not designed to test efficacy in a rigorous manner, the preliminary efficacy results reported here demonstrate that the telehealth version of FYF has the potential to impact anxiety and excessive fears in youth with ASD.
Limitations
There are several limitations that must be considered when interpreting the results of this study. The sample size was quite small, and though representative of rural Colorado, was not diverse with regard to race or ethnicity, and most of our participating families were middle class. It is important to note that the group sizes in the Telehealth FYF intervention were limited to four participating families and some groups included only two, due to challenges matching schedules and youth characteristics (e.g. age, interests) for peer cohesion. In contrast, FYF live groups usually include —five to six families. Thus, delivery of the interventions differed on dimensions beyond mode of communication. Further study is necessary to evaluate the impact of these modifications for real-world implementation. Participants were highly motivated and a selection bias may have operated in the recruitment strategy (i.e. obtaining participants through parent groups and community workshops). Generalization of findings is thus limited by the relatively narrow range of participant characteristics described here. The child and family outcomes reported here need to be interpreted cautiously, as these data were collected to inform the design of future efficacy studies, and not to be a rigorous test of intervention impact. The limitations of the design (quasi-experimental, comparison group of convenience, reliance upon subjective data collected from participants in treatment, without blinding) compromise the generalizability of these findings. However, as a pilot study, the data support ongoing investigations with larger, better characterized samples.
Implications for practice
There were some challenges in delivering mental health services via telehealth that are worth noting. From the therapists’ perspective, face-to-face sessions clearly provide more opportunities for behavioral observation, modeling of behavioral techniques to both children and parents, and increased support in completing exposure activities. Creativity was required to implement these techniques via telehealth. For example, video modeling was used to highlight relaxation techniques and exposure completion. In addition, to ensure that families were conducting exposure hierarchies and using coping techniques, families were sent flip cameras and were asked to videotape their exposure tasks and upload their data. Clinicians were able to view the exposure practice, share the videos with the group, and offer praise as well as provide corrective feedback for improving the exposure activity. It has been our experience that watching each group member “face fears” is a critically important component of the group treatment, as it allows each child to take pride in his or her success, and promotes brave behavior among group members. A group context provides an opportunity for parents to coach each other and share their own experiences. Improving the current methods for promoting family-to-family as well as therapist-to-family coaching is an important next step.
Another significant challenge in conducting the FYF intervention via telehealth involves observing and addressing the nuances within parent–child interactions. For example, in an in-person FYF Group, tense parent–child interactions are observed frequently and become an important learning opportunity to practice new strategies. Similar parent–child dynamics occurred during the telehealth groups, but at times these interactions occurred off-camera, making it difficult for the clinicians to directly address the interaction. When the parent–child interactions were observed on screen, the clinicians struggled to coach the parents in a manner that felt dignified to all involved. Whereas in a live session, the therapist can take a parent aside and confidentially impart a few ideas on how to help the child participate, this individual “sidebar” was not viable through our telehealth set-up. It is important to note that additional time was required to address these issues with the parents directly, suggesting that future versions of the telehealth intervention may need to devote more time to this aspect of treatment.
Finally, careful planning on both the clinician’s and the parent’s part was needed and could potentially be improved upon in future research. While the convenience of conducting a session from home was hugely important for the families we served, it may be helpful for future telehealth activities to include discussions with families about how to address the competing demands of other household activities that can occur during session time (e.g. addressing the needs of other children in the home, multitasking). Despite these limitations, overall, with preparation, planning, and practice, telehealth delivery of direct intervention to youth with ASD and anxiety (and their parents) is feasible and has potential to improve access to specialized interventions that may not be available in all communities.
Future directions
Carefully designed studies, using appropriate controls and randomized assignment to intervention condition, are needed. Clear delineation of inclusion criteria, careful identification of appropriate outcome measures, and comprehensive descriptions of study procedure methods (i.e. in enough detail to support independent replication) are necessary for this body of research to move forward. Future studies can compare efficacy of manualized interventions by delivery modality (“live” vs “telehealth”). It will also be important to consider how individual differences in learning style, culture, and familiarity with technology influence one’s comfort with this intervention modality. As with any intervention, telehealth applications are likely to be a better fit for some youth, parents, and therapists than others. It would be helpful to identify the characteristics of youth and parents who appreciate this therapeutic medium, and to examine strategies for promoting therapist comfort and competence communicating in this manner.
Acknowledgments
The authors thank Larry Edelman and Dina Johnson for technological support, Kristen Kaiser for her family leadership and communications expertise, and Mary Hetrick, Angela Turner, Devin Sharp, and Jessica Stern for administrative assistance. Finally, the authors appreciate the efforts and input of the families who collaborated with us on this project.
Funding
This work was supported by the Health Resources and Services Administration (HRSA; R40MC15593-01-00). We are grateful to Autism Speaks, Aspen Extreme Sports Camp, Autism Society of Colorado, Roaring Fork Parent Network, and Moms on the Spectrum, who assisted us with recruiting interested families in rural parts of our state. Database support was provided by NIH/NCATS Colorado CTSI Grant Number UL1 TR001082. Infrastructure and trainee support was provided by ACF/DHHS (University Center of Excellence in Developmental Disabilities Grant # 90DD0699-03-00).
Footnotes
One youth experienced an acute psychiatric crisis and was hospitalized during the second week of his involvement in the study.
References
- Albano AM, Barlow DH. Breaking the vicious cycle: cognitive-behavioral group treatment for socially anxious youth. In: Hibbs ED, Jensen PS, editors. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. Washington, DC: American Psychological Association; 1996. pp. 43–62. [Google Scholar]
- Barretto A, Wacker DP, Harding J, et al. Using telemedicine to conduct behavioral assessments. Journal of Applied Behavior Analysis. 2006;39(3):333–340. doi: 10.1901/jaba.2006.173-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, et al. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Boisvert M, Lang R, Andrianopoulos M, et al. Telepractice in the assessment and treatment of individuals with autism spectrum disorders: a systematic review. Developmental Neurorehabilitation. 2010;13(6):423–432. doi: 10.3109/17518423.2010.499889. [DOI] [PubMed] [Google Scholar]
- Boydell KM, Volpe T, Pignatiello A. A qualitative study of young people’s perspectives on receiving psychiatric services via televideo. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2010;19(1):5–11. [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L, Stahmer AC, Lewis K, et al. Building a research community collaborative to improve community care for infants and toddlers at-risk for Autism Spectrum Disorders. Journal of Community Psychology. 2012;40(6):715–734. doi: 10.1002/jcop.21501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni TP. Test review: social Responsiveness Scale—Second Edition (SRS-2) Journal of Psychoeducational Assessment. 2014;32(4):365–369. [Google Scholar]
- Chalfant AM, Rapee R, Carroll L. Treating anxiety disorders in children with high-functioning autism spectrum disorders: a controlled trial. Journal of Autism and Developmental Disorders. 2007;37(10):1842–1857. doi: 10.1007/s10803-006-0318-4. [DOI] [PubMed] [Google Scholar]
- Cohen J. Set correlation and contingency tables. Applied Psychological Measurement. 1988;12(4):425–434. [Google Scholar]
- Cohen MJ, Sloan DL. Visual Supports for People with Autism: A Guide for Parents and Professionals. Bethesda, MD: Woodbine House; 2007. [Google Scholar]
- Connolly SD, Bernstein GA Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(2):267–283. doi: 10.1097/01.chi.0000246070.23695.06. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. The Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services; 2002. [Google Scholar]
- Gibson JL, Pennington RC, Stenhoff DM, et al. Using desktop videoconferencing to deliver interventions to a preschool student with autism. Topics in Early Childhood Special Education. 2010;29(4):214–225. [Google Scholar]
- Goodwin MS. Enhancing and accelerating the pace of autism research and treatment. Focus on Autism & Other Developmental Disabilities. 2008;23(2):125–128. [Google Scholar]
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. Journal of Clinical Child Psychology. 1989;18(2):167–175. [Google Scholar]
- Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clinical Psychology Review. 2005;25(3):341–363. doi: 10.1016/j.cpr.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Beidas RS. Smoothing the trail for dissemination of evidence-based practices for youth: flexibility within fidelity. Professional Psychology: Research and Practice. 2007;38:13–19. [Google Scholar]
- Kimball JW, Smith K. Crossing the bridge: from best practices to software packages. Focus on Autism & Other Developmental Disabilities. 2007;22(2):131–134. [Google Scholar]
- Kobak KA, Stone WL, Wallace E, et al. A web-based tutorial for parents of young children with autism: results from a pilot study. Telemedicine Journal and E-Health. 2011;17(10):804–808. doi: 10.1089/tmj.2011.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Strickland BB, Blumberg SJ, et al. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Wood JJ, Halladay AK, et al. Measuring anxiety as a treatment endpoint in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;44:1128–1143. doi: 10.1007/s10803-013-1974-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, et al. Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children’s Health. Journal of Developmental and Behavioral Pediatrics. 2008;29(3):152–160. doi: 10.1097/DBP.0b013e318165c7a0. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30(5):205–223. [PubMed] [Google Scholar]
- Machalicek W, O’Reilly M, Chan JM, et al. Using vide-oconferencing to conduct functional analysis of challenging behavior and develop classroom behavioral support plans for students with autism. Education and Training in Developmental Disabilities. 2009;44(2):207–215. [Google Scholar]
- Machalicek W, O’Reilly MF, Rispoli M, et al. Training teachers to assess the challenging behaviors of students with autism using video tele-conferencing. Education and Training in Autism and Developmental Disabilities. 2010;45(2):203–215. [Google Scholar]
- Mandell DS, Morales KH, Xie M, et al. Age of diagnosis among medicaid-enrolled children with autism, 2001–2004. Psychiatric Services. 2010;61(8):822–829. doi: 10.1176/appi.ps.61.8.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB. Estimating effect sizes from the pretest–posttest-control group designs. Organizational Research Methods. 2007;11(2):364–386. [Google Scholar]
- Myers K, Vander Stoep A, Lobdell C. Feasibility of conducting a randomized controlled trial of telemental health with children diagnosed with attention-deficit/hyperactivity disorder in underserved communities. Journal of Child and Adolescent Psychopharmacology. 2013;23(6):372–378. doi: 10.1089/cap.2013.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Health. National Institutes of Health Workshop on Mental Health in Intellectual and Developmental Disabilities: Research Challenges and Opportunities; Bethesda, MD. NIH; 2014. [Google Scholar]
- Nelson E, Palsbo S. Challenges in telemedicine equivalence studies. Evaluation and Program Planning. 2006;29(4):419–425. doi: 10.1016/j.evalprogplan.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Pacifici C, Delaney R, White L, et al. Web-based training for foster, adoptive, and kinship parents. Children and Youth Services Review. 2006;28(11):1329–1343. [Google Scholar]
- Pignatiello A, Teshima J, Boydell KM, et al. Child and youth telepsychiatry in rural and remote primary care. In: Grady BJ, Nelson EL, editors. Telepsychiatry and Telemental Health: Child and Adolescent Psychiatric Clinics of North America. Vol. 20. Philadelphia, PA: Saunders; 2011. pp. 13–28. [DOI] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A. Fidelity checklist for “Facing Your Fears”. University of Colorado; Boulder, CO: 2009. Unpublished. [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K, et al. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: a randomized trial. Journal of Child Psychology and Psychiatry. 2012;53(4):410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven J, Blakeley-Smith A, Nichols S, et al. Facing Your Fears: Group Therapy for Managing Anxiety in Children with High-Functioning Autism Spectrum Disorders. Baltimore, MD: Paul Brookes Publishing; 2011. [Google Scholar]
- Reed P, Osborne LA, Corness M. Relative effectiveness of different home based behavioral approaches to early teaching intervention. Journal of Autism and Developmental Disorders. 2007;37:1815–1821. doi: 10.1007/s10803-006-0306-8. [DOI] [PubMed] [Google Scholar]
- Research Units on Pediatric Psychopharmacology (RUPP) Autism Network. Parent training for children with pervasive developmental disorders: a multi-site feasibility trial. Behavioral Interventions. 2007;22:179–199. [Google Scholar]
- Richardson LK, Frueh BC, Grubaugh AL, et al. Current directions in videoconferencing mental health research. Clinical Psychology: Science and Practice. 2009;16(3):323–338. doi: 10.1111/j.1468-2850.2009.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roid GH. Stanford-Binet Intelligence Scales: SB5. Rolling Meadows, IL: Riverside; 2003. [Google Scholar]
- Roid GH, Miller LJ. Leiter International Performance Scale—Revised (Leiter-R) Wood Dale, IL: Riverside; 2002. [Google Scholar]
- Rule S, Salzberg C, Higbee T, et al. Technology-mediated consultation to assist rural students: a case study. Rural Special Education Quarterly. 2006;25(2):37–45. [Google Scholar]
- Savin D, Garry MT, Zuccaro P, et al. Telepsychiatry for treating rural American Indian youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(4):484–488. doi: 10.1097/01.chi.0000198594.68820.59. [DOI] [PubMed] [Google Scholar]
- Shook GL. An examination of the integrity and future of the behavior analysis certification Board credentials. Behavior Modification. 2005;29:562–574. doi: 10.1177/0145445504274203. [DOI] [PubMed] [Google Scholar]
- Sofronoff K. Counseling youth with Asperger syndrome. In: Baker LJ, Welkowitz LA, editors. Asperger’s Syndrome: Intervening in Schools, Clinics and Communities. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2005. pp. 135–153. [Google Scholar]
- Stern JA, Gadgil MS, Blakeley-Smith A, et al. Psychometric properties of the SCARED in youth with autism spectrum disorders. Research in Autism Spectrum Disorders. 2014;8:1225–1234. doi: 10.1016/j.rasd.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch EA, Arnold EB, Lewin AB, et al. The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(2):132–142. doi: 10.1016/j.jaac.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Van Steensel FJA, Bögels SM, Dirksen CD. Anxiety and quality of life: clinically anxious children with and without autism spectrum disorders compared. Journal of Clinical Child and Adolescent Psychology. 2012;41(6):731–738. doi: 10.1080/15374416.2012.698725. [DOI] [PubMed] [Google Scholar]
- Vismara LA, Young GS, Stahmer AC, et al. Dissemination of evidence-based practice: can we train therapists from a distance? Journal of Autism and Developmental Disorders. 2009;39(12):1636–1651. doi: 10.1007/s10803-009-0796-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio TX: Psychological Corporation; 1999. [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children–Fourth Edition (WISC-IV) San Antonio, TX: Psychological Corporation; 2003. [Google Scholar]
- Weiss JA, Cappadocia MC, MacMullin JA, et al. The impact of child problem behaviors of children with ASD on parent mental health: the mediating role of acceptance and empowerment. Autism. 2012;16(3):261–274. doi: 10.1177/1362361311422708. [DOI] [PubMed] [Google Scholar]
- Weitlauf AS, McPheeters ML, Peters B, et al. Therapies for children with autism spectrum disorder: behavioral interventions update. Rockville, MD: Agency for Healthcare Research and Quality; 2014. Aug, Comparative Effectiveness Review No. 137. AHRQ Publication No. 14-EHC036-EF. Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed] [Google Scholar]
- White SW, Albano AM, Johnson CR, et al. Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clinical Child and Family Psychology Review. 2010;13(1):77–90. doi: 10.1007/s10567-009-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Drahota A, Sze K, et al. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yellowlees PM, Hilty DM, Marks SL. A retrospective analysis of a child and adolescent eMental Health Program. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;41(1):103–107. doi: 10.1097/chi.0b013e31815a56a7. [DOI] [PubMed] [Google Scholar]


