Abstract
AIM: To study changes in characteristics of colorectal carcinoma during the metastatic process and to investigate the correlation between cell proliferation activity and metastatic ability of patients with Dukes’ stage C or D.
METHODS: Formalin fixed and paraffin embedded materials of primary tumors and corresponding lymph node metastases resected from 56 patients with Dukes' stage C or D of colorectal carcinoma were stained immunohistochemically with proliferating cell nuclear antigen (PCNA) and CD44 variant exon 6 (CD44v6).
RESULTS: Thirty-one of 56 patients (55.4%) expressed PCNA in the primary sites and 36 of 56 patients (64.3%) expressed PCNA in the metastatic lymph nodes. A significant relation in PCNA expression was observed between the primary site and the metastatic lymph node (0.010 < P < 0.025). Forty-one of 56 patients (73.2%) expressed CD44v6 in the primary site and 39 of 56 patients (69.6%) expressed CD44v6 in the metastatic lymph node. There was also an significant relationship of CD44v6 between the primary site and the metastatic lymph node (0.005 < P < 0.010). No difference was observed between expression of CD44v6 and PCNA in the primary site (0.250 < P < 0.500).
CONCLUSION: This study partially demonstrates that tumor cells in metastatic lymph node of colorectal carcinoma still possess cell proliferation activity and metastatic ability of tumor cells in primary site. There may be no association between cell proliferation activity and metastatic ability in colorectal carcinoma.
INTRODUCTION
Colorectal carcinoma appears to be increasing in Chinese populations and is characterised by an aggressive course and frequent metastases resulting in death. To reduce morbidity and mortality, identification of those patients with a high propensity to develop distant metastases is of great importance, since they might benefit from adjuvant chemotherapy and/or radiotherapy[1,2]. Although Dukes’ classification is still considered as the most accurate predictor of prognosis after resection, even within a group of tumors of a specified stage, tumor behaviour and prognosis of the disease is not uniform[3-5]. For this reason, additional markers that predict tumor metastatic behaviour are needed[6-9]. At present, PCNA has been described as a significant factor in the prognosis of colorectal carcinoma in several studies[10-12]. On the other hand, many studies demonstrated that expression of CD44v6 correlated with poor survival and was an independent prognosticator in patients who underwent radical surgery[13-17]. However, to our knowledge questions concerning metastases, characteristic changes that occur during the metastatic process, and the correlation between tumor characteristics have to be clarified in detail[18-20]. To our knowledge, there has been neither any study regarding patients with Dukes’ stage C or D analyzing both primary sites and corresponding metastatic lymph nodes genetically or immunohistologically nor a study assessing their relationship.
We examined the expression of these two factors in both primary sites and metastatic lymph nodes to elucidate the characteristic changes of the tumor during metastases and to evaluate the correlation between cell proliferation activity and metastatic ability of the tumor in patients with Dukes’ stage C or D of colorectal carcinoma.
MATERIALS AND METHODS
Materials
175 consecutive patients with colorectal carcinoma admitted to our department underwent resection between 1989 and 1996. The total rate of lymph node metastasis was 33.7%, 77.2%, of which lymph node metastasis next to the colorectum was, 17.9% and 4.9% mesentery and mesenteric artery ligation point respectively. Of these 175 patients, 62 (35.8%) were diagnosed with Dukes’ stage C or D. Among these 62 patients, 56 whose primary site and metastatic node tissues were immunohistochemically evaluable were enrolled in the study. They were comprised of 30 males and 26 females with a mean age of 51.3 ± 14.2 years. Forty nine patients with Dukes’ stage C underwent a complete tumor resection with lymph node dissectioned and 7 patients with Dukes’ stage D underwent a palliative tumor resection with lymph node dissectioned in the Department of Gastroenterology, Shannxi Provincial Cancer Hospital in Xi’an, China. The patients had not been treated before. Their respective clinical data were collected through the review of their medical records. Histologic typing revealed 12 papillary adenocarcinomas, 27 tubular adenocarcinomas, 10 mucinous adenocarcinomas, 5 signet-ring cell carcinomas and 2 undifferentiated carcinomas. Of these patients, there were 49 patients with Dukes’ stage C, whose average number of metastatic lymph nodes was 5.3 ± 2.1 and 7 patients with Dukes’ stage D, whose average number of metastatic sites including lymph node, liver, greater omentum and peritoneum was 8.7 ± 2.6. The paraffin-embedded blocks and histological slides were taken from the Department of Pathology, Shaanxi Provincial Cancer Hospital (Table 1).
Table 1.
Characteristics of patients with Dukes’ stage C or D colorectal carcinoma
| Gender | Male | 30 |
| Female | 26 | |
| Age(yrs) (mean ± SD) | 51.3 ± 14.2 | |
| Histology | Papillary adenocarcinoma | 12 |
| Tubular adenocarcinoma | 27 | |
| Mucinous adenocarcinoma | 10 | |
| Signet-ring cell carcinoma | 5 | |
| Undifferentiated carcinoma | 2 | |
| Dukes’ classification | Stage C | 49 |
| Stage D | 7 |
Methods
Formalin fixed, paraffin embedded sections of samples were stained immunohistochemically with labeled streptavidin-biotin (LSAB) using a LSAB Kit (Doctor Biotechnology Company, Wuhan, Hubei Province, China). The samples were thinly sectioned (4 μm thick). After deparaffinization, the sections were hydrolyzed with ethanol and endogenous peroxidase activity was inhibited with 0.3% hydrogen peroxide-containing methanol at room temperature for 15 min. For antigen retrieval, the sections were mounted in 300 mL 0.01 M sodium citrate buffer (pH6.0) in a container and microwaved for 15 min at maximum power in a Sharp microwave oven (850 W). Nonspecific binding sites were blocked with 10% nonimmune goat serum. For PCNA, PC10 (Zymed Laboratories, California) whose optimal dilution was 1:150 was used for the first antibody and allowed to react at 4 °C for 12 h. For CD44v6, CD44 variant exon 6 (VFF-18; Bender Co.) whose optimal dilution was 1:100 was used for the first antibody and allowed to react at 4 °C for 12 h. After the second antibody was made to react, peroxidase-labeled streptoavidin was finally allowed to react as an enzyme reagent. Diaminobenzidine was used for coloring. Sections of human tonsils and submucosal lymphoid follicles were used as positive control for PCNA. Positive control of CD44v6 was normal human stratified squamous epithelium which could be strongly stained by anti-CD44v6 antibodies[15]. Sections stained by omitting the primary antibody were used as their negative controls. At least 5 visual fields of the immunohistochemically stained sample were observed at random at × 100 or × 400 magnification. More than 1000 tumor cells were counted by two investigators who were blinded to the clinical outcome. The number of positive cells was counted and expressed as percentage. For PCNA, when the percentage of positive cells was ≤ 50%, the specimen was diagnosed as negative, and when > 50%, the specimen was diagnosed as positive. We also determined the percentage of cells positively stained for CD44v6, as well as the intensity of this staining. Negative, ≤ 10% of cells were positively stained, and positive, > 10% cells were positively stained[21]. The data were analyzed using χ2 text and a P value < 0.05 was considered significant.
RESULTS
Immunohistochemical staining with PCNA showed a selective nuclear pattern (Figure 1, Figure 2). Thirty-one of 56 patients (55.4%) expressed PCNA in the primary site and 36 of 56 patients (64.3%) expressed PCNA in the metastatic lymph node. Among these 56 patients, twenty-four expressed PCNA in both the primary site and metastatic lymph node, seven patients expressed PCNA in the primary site but did not express it in the metastatic lymph node, whereas twelve patients did not express PCNA in the primary site but expressed it in the metastatic lymph node, thirteen patients expressed PCNA in neither the primary site nor metastatic lymph node (Table 2). For expression of PCNA in these 56 patients, a significant relation was observed between the primary site and the metastatic lymph node (0.010 < P < 0.025).
Figure 1.
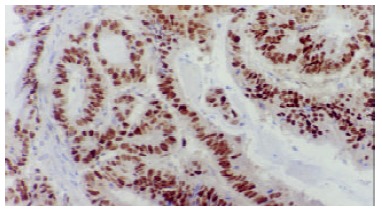
Positive expression of PCNA in primary colorectal carcinoma tissue (LSAB × 100).
Figure 2.
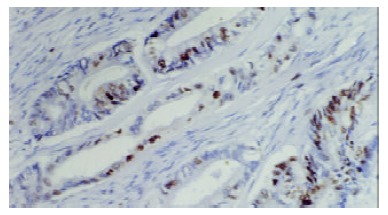
Negative expression of PCNA in primary site (LSAB × 100).
Table 2.
Expression of PCNA in colorectal carcinoma at primary sites and metastatic lymph nodes
| Metastatic lymph nodes |
Primary sites |
|
| - | + | |
| - | 13 | 7 |
| + | 12 | 24 |
Note: χ2 = 5.21, 0.010 < P < 0.025.
Intensely positive staining with CD44v6 mainly occurred on the cell membrane surface of tumor cells (Figure 3). Forty-one of 56 patients (73.2%) expressed CD44v6 in the primary site and 39 of 56 patients (69.6%) expressed CD44v6 in the metastatic lymph node (Figure 4). Among these 56 patients, thirty-three expressed CD44v6 in both the primary site and metastatic lymph node, eight expressed CD44v6 in the primary site but did not express it in the metastatic lymph node, whereas six did not express CD44v6 in the primary site but expressed it in the metastatic lymph node, nine expressed CD44v6 in neither primary site nor metastatic lymph node (Table 3). For expression of CD44v6 in these 56 patients, there was also an significant relationship between the primary site and the metastatic lymph node (0.005 < P < 0.010).
Figure 3.
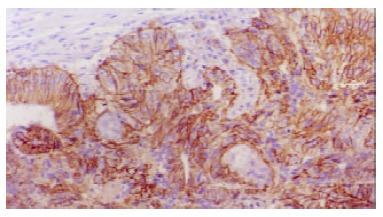
CD44v6 was observed on the cell membrane of tumor cells (LSAB × 100).
Figure 4.
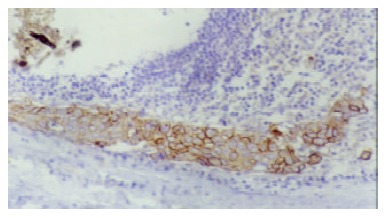
Expression of CD44v6 in corresponding metastatic lymph node, showing that tumor cells were invading lymph node from periphery. (LSAB × 100).
Table 3.
Expression of CD44v6 in colorectal carcinoma at primary sites and metastatic lymph nodes
| Metastatic lymph nodes |
Primary sites |
|
| - | + | |
| - | 9 | 8 |
| + | 6 | 33 |
Note: χ2 = 6.71, 0.005 < P < 0.010.
To evaluate the correlation between cell proliferation activity and metastatic ability, we studied expression of PCNA and CD44v6 in the primary site. Among these 56 patients, twenty-one expressed both PCNA and CD44v6 and 5 expressed neither PCNA nor CD44v6 in the primary site, twenty expressed CD44v6 but did not express PCNA, whereas ten did not express CD44v6 but expressed PCNA in the primary site (Table 4). No difference was observed between expression of CD44v6 and PCNA in the primary site(0.250 < P < 0.500).
Table 4.
Expression of PCNA and CD44v6 in colorectal carcinoma at primary sites
| PCNA |
CD44v6 |
|
| - | + | |
| - | 5 | 20 |
| + | 10 | 21 |
Note: χ2 = 1.06, 0.250 < P < 0.500
Cell morphology
Immunohistochemical staining with PCNA showed a selective nuclear pattern (Figure 1, Figure 2). Intensely positive staining with CD44v6 mainly occurred on the cell membrane surface of tumor cells (Figure 3). Expression of CD44v6 in corresponding metastatic lymph node showed that tumor cells were invading lymph node from periphery (Figure 4).
DISCUSSION
One of the first steps in multistage colonic carcinogenesis is increased cell proliferation. PCNA, which is a nonhistone nuclear protein of 36 kilodaltons, also is known as cyclin and an auxiliary factor in DNA polymerase, plays a very important role in DNA replication[22]. Because of this direct relation with cell proliferation, PCNA is considered to be an important factor in prognosis. In fact, it has been described as a significant factor in the prognosis of colorectal carcinoma in several studies[10-12]. CD44, a glycoprotein of the membrane penetration type, functions as an extracellular matrix glycan receptor and a hyaluronate receptor[23]. As a consequence of studies in rats showed that CD44v6 could confer metastatic potential to rat pancreatic carcinoma cell lines[24], studies addressing the prognostic and biological significance of CD44 variant expression in human cancer have largely been focused on CD44v6. Overexpression of CD44v6 has been demonstrated in colorectal neoplasia by immunohistochemistry, RT-PCR and in situ hybridization. Their expression was found to correlate with tumor stage[13-17]. As for prognosis, it was shown that expression of CD44v6 correlate with poor survival rate and was an independent prognosticator in patients who underwent radical surgery. Hence, it identifies individuals with a high propensity to develop metastases. These patients might benefit from adjuvant therapy[16].
Despite intensive research in recent years, very little is known about the characteristic changes of malignant colorectal tumor cells during the process of metastases. We examined expression of these two factors in both primary site and metastatic lymph node. Among these 56 patients, twenty-four expressed PCNA in both the primary site and metastatic lymph node and thirteen expressed PCNA in neither the primary site nor metastatic lymph node. The concordence rate of PCNA expression in the primary site and in the metastatic lymph node was 66.1% (0.010 < P < 0.025). That is to say, compared with primary site, PCNA expression in metastatic lymph node had no significant change. This suggests that cell proliferation activity revealed by PCNA still exists in the tumor cells of metastatic lymph nodes. Similarly, the concordence rate of CD44v6 expression in the primary site and in the metastatic lymph node was 75.0% (0.005 < P < 0.010). This also means that metaststic ability revealed by CD44v6 still exists in the tumor cells of metastatic lymph nodes.
Although cell proliferation and metastasis are a very complicated problem involving many molecular mechanisms and biologic factors, our study partially showed that tumor cells in metastatic lymph node of colorectal carcinoma still possessed cell proliferation activity and metastatic ability of tumor cells in primary site. However, Kimball et al[25] isolated a cellular subpopulation from a human colonic carcinoma cell line and Brattain et al[26] reported that malignant cells from a human colonic carcinoma possessed heterogeneity. A question rises: do tumor cells of colorectal carcinoma not possess heterogeneity between the primary site and the metastatic lymph node It is well known that cancer cell population, either as a solid tumor mass in vivo or as a continuous cell line in vitro, is an ever-changing entity due to their genetic instability and selective environmental pressure. A tumor mass consists of different cell clones, a phenomenon known as tumor heterogeneity[27,28]. Based on this phenomenon, tumor cell clones with different biological properties have been isolated from a number of human and animal tumor cell lines. The differences included a variety of biological characteristics such as tumor cell morphology, karyotypes, in vitro and in vivo growth patterns[29,30], DNA ploidy[31] tumorigenicity, metastatic patterns and metastatic potentials[32]. Cancer metastasis is the ultimate display of complex interactions between the malignant cells and the host defense mechanism. The process of metastasis consists of selection and sequential steps that include angiogenesis, detachment, motility, invasion of the extracellular matrix, intravasation, circulation, adhesion, extravasation into the organ parenchyma and growth[28]. The ability of cancer cells to form metastasis depends on a set of unique biological properties that enable the malignant cells to complete all those steps of metastatic cascade. But this basically biological theory is not in contradiction with our present study, because our results are a clinicopathologic outcome depending upon experiment.
Our study showed that there was no significant association between expression of CD44v6 and PCNA in the primary site (0.250 < P < 0.500). This result partially indicated that there existed no absolute association between cell proliferation activity and metastatic ability in colorectal carcinoma. At present, whether tumor cell growth rate is directly related to metastasis is not clear yet. Yasoshima et at[33] using metastatic gastric cancer cell line, and Samiei et al[34] using metastatic mammary clones found that metastasis was independent of tumor cell growth, while other works[35-37] showed a close association between tumor cell growth rate and metastasis. Further study of the correlation between cell proliferation activity and metastatic ability in colorectal carcinoma is therefore needed.
In conclusion, we have partially demonstrated in the present study that tumor cells in metastatic lymph node of colorectal carcinoma still possess cell proliferation activity and metastatic ability in primary site. There may be no association between cell proliferation activity and metastatic ability in colorectal carcinoma.
Footnotes
Edited by Zhao M and Wang XL
References
- 1.Mayer RJ, O'Connell MJ, Tepper JE, Wolmark N. Status of adjuvant therapy for colorectal cancer. J Natl Cancer Inst. 1989;81:1359–1364. doi: 10.1093/jnci/81.18.1359. [DOI] [PubMed] [Google Scholar]
- 2.Moertel CG. Chemotherapy for colorectal cancer. N Engl J Med. 1994;330:1136–1142. doi: 10.1056/NEJM199404213301608. [DOI] [PubMed] [Google Scholar]
- 3.Steele G. Advances in the treatment of early- to late-stage colorectal cancer: 20 years of progress. Ann Surg Oncol. 1995;2:77–88. doi: 10.1007/BF02303706. [DOI] [PubMed] [Google Scholar]
- 4.Greene FL, Stewart AK, Norton HJ. A new TNM staging strategy for node-positive (stage III) colon cancer: an analysis of 50, 042 patients. Ann Surg. 2002;236:416–21; discussion 421. doi: 10.1097/00000658-200210000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fisher ER, Sass R, Palekar A, Fisher B, Wolmark N. Dukes' classification revisited. Findings from the National Surgical Adjuvant Breast and Bowel Projects (Protocol R-01) Cancer. 1989;64:2354–2360. doi: 10.1002/1097-0142(19891201)64:11<2354::aid-cncr2820641127>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 6.Douglass HO, Moertel CG, Mayer RJ, Thomas PR, Lindblad AS, Mittleman A, Stablein DM, Bruckner HW. Survival after postoperative combination treatment of rectal cancer. N Engl J Med. 1986;315:1294–1295. doi: 10.1056/NEJM198611133152014. [DOI] [PubMed] [Google Scholar]
- 7.Laurie JA, Moertel CG, Fleming TR, Wieand HS, Leigh JE, Rubin J, McCormack GW, Gerstner JB, Krook JE, Malliard J. Surgical adjuvant therapy of large-bowel carcinoma: an evaluation of levamisole and the combination of levamisole and fluorouracil. The North Central Cancer Treatment Group and the Mayo Clinic. J Clin Oncol. 1989;7:1447–1456. doi: 10.1200/JCO.1989.7.10.1447. [DOI] [PubMed] [Google Scholar]
- 8.Krook JE, Moertel CG, Gunderson LL, Wieand HS, Collins RT, Beart RW, Kubista TP, Poon MA, Meyers WC, Mailliard JA. Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med. 1991;324:709–715. doi: 10.1056/NEJM199103143241101. [DOI] [PubMed] [Google Scholar]
- 9.Harris GJ, Church JM, Senagore AJ, Lavery IC, Hull TL, Strong SA, Fazio VW. Factors affecting local recurrence of colonic adenocarcinoma. Dis Colon Rectum. 2002;45:1029–1034. doi: 10.1007/s10350-004-6355-1. [DOI] [PubMed] [Google Scholar]
- 10.Kanazawa Y, Onda M, Tanaka N, Seya T. Proliferating cell nuclear antigen and p53 protein expression in submucosal invasive colorectal carcinoma. J Nippon Med Sch. 2000;67:242–249. doi: 10.1272/jnms.67.242. [DOI] [PubMed] [Google Scholar]
- 11.Onodera H, Maetani S, Kawamoto K, Kan S, Kondo S, Imamura M. Pathologic significance of tumor progression in locally recurrent rectal cancer: different nature from primary cancer. Dis Colon Rectum. 2000;43:775–781. doi: 10.1007/BF02238013. [DOI] [PubMed] [Google Scholar]
- 12.Seong J, Chung EJ, Kim H, Kim GE, Kim NK, Sohn SK, Min JS, Suh CO. Assessment of biomarkers in paired primary and recurrent colorectal adenocarcinomas. Int J Radiat Oncol Biol Phys. 1999;45:1167–1173. doi: 10.1016/s0360-3016(99)00302-8. [DOI] [PubMed] [Google Scholar]
- 13.Wielenga VJ, Heider KH, Offerhaus GJ, Adolf GR, van den Berg FM, Ponta H, Herrlich P, Pals ST. Expression of CD44 variant proteins in human colorectal cancer is related to tumor progression. Cancer Res. 1993;53:4754–4756. [PubMed] [Google Scholar]
- 14.Finn L, Dougherty G, Finley G, Meisler A, Becich M, Cooper DL. Alternative splicing of CD44 pre-mRNA in human colorectal tumors. Biochem Biophys Res Commun. 1994;200:1015–1022. doi: 10.1006/bbrc.1994.1551. [DOI] [PubMed] [Google Scholar]
- 15.Fox SB, Fawcett J, Jackson DG, Collins I, Gatter KC, Harris AL, Gearing A, Simmons DL. Normal human tissues, in addition to some tumors, express multiple different CD44 isoforms. Cancer Res. 1994;54:4539–4546. [PubMed] [Google Scholar]
- 16.Mulder JW, Kruyt PM, Sewnath M, Oosting J, Seldenrijk CA, Weidema WF, Offerhaus GJ, Pals ST. Colorectal cancer prognosis and expression of exon-v6-containing CD44 proteins. Lancet. 1994;344:1470–1472. doi: 10.1016/s0140-6736(94)90290-9. [DOI] [PubMed] [Google Scholar]
- 17.Gotley DC, Fawcett J, Walsh MD, Reeder JA, Simmons DL, Antalis TM. Alternatively spliced variants of the cell adhesion molecule CD44 and tumour progression in colorectal cancer. Br J Cancer. 1996;74:342–351. doi: 10.1038/bjc.1996.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fukuse T, Hirata T, Tanaka F, Yanagihara K, Hitomi S, Wada H. Prognosis of ipsilateral intrapulmonary metastases in resected nonsmall cell lung cancer. Eur J Cardiothorac Surg. 1997;12:218–223. doi: 10.1016/s1010-7940(97)00122-x. [DOI] [PubMed] [Google Scholar]
- 19.Ichinose Y, Hara N, Ohta M. Synchronous lung cancers defined by deoxyribonucleic acid flow cytometry. J Thorac Cardiovasc Surg. 1991;102:418–424. [PubMed] [Google Scholar]
- 20.Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975;70:606–612. [PubMed] [Google Scholar]
- 21.Nanashima A, Yamaguchi H, Sawai T, Yasutake T, Tsuji T, Jibiki M, Yamaguchi E, Nakagoe T, Ayabe H. Expression of adhesion molecules in hepatic metastases of colorectal carcinoma: relationship to primary tumours and prognosis after hepatic resection. J Gastroenterol Hepatol. 1999;14:1004–1009. doi: 10.1046/j.1440-1746.1999.01991.x. [DOI] [PubMed] [Google Scholar]
- 22.Bravo R, Frank R, Blundell PA, Macdonald-Bravo H. Cyclin/PCNA is the auxiliary protein of DNA polymerase-delta. Nature. 1987;326:515–517. doi: 10.1038/326515a0. [DOI] [PubMed] [Google Scholar]
- 23.Aruffo A, Stamenkovic I, Melnick M, Underhill CB, Seed B. CD44 is the principal cell surface receptor for hyaluronate. Cell. 1990;61:1303–1313. doi: 10.1016/0092-8674(90)90694-a. [DOI] [PubMed] [Google Scholar]
- 24.Günthert U, Hofmann M, Rudy W, Reber S, Zöller M, Haussmann I, Matzku S, Wenzel A, Ponta H, Herrlich P. A new variant of glycoprotein CD44 confers metastatic potential to rat carcinoma cells. Cell. 1991;65:13–24. doi: 10.1016/0092-8674(91)90403-l. [DOI] [PubMed] [Google Scholar]
- 25.Kimball PM, Brattain MG. Isolation of a cellular subpopulation from a human colonic carcinoma cell line. Cancer Res. 1980;40:1574–1579. [PubMed] [Google Scholar]
- 26.Brattain MG, Fine WD, Khaled FM, Thompson J, Brattain DE. Heterogeneity of malignant cells from a human colonic carcinoma. Cancer Res. 1981;41:1751–1756. [PubMed] [Google Scholar]
- 27.Fidler IJ. Tumor heterogeneity and the biology of cancer invasion and metastasis. Cancer Res. 1978;38:2651–2660. [PubMed] [Google Scholar]
- 28.Fidler IJ. Critical factors in the biology of human cancer metastasis: twenty-eighth G.H.A. Clowes memorial award lecture. Cancer Res. 1990;50:6130–6138. [PubMed] [Google Scholar]
- 29.Dexter DL, Spremulli EN, Fligiel Z, Barbosa JA, Vogel R, VanVoorhees A, Calabresi P. Heterogeneity of cancer cells from a single human colon carcinoma. Am J Med. 1981;71:949–956. doi: 10.1016/0002-9343(81)90312-0. [DOI] [PubMed] [Google Scholar]
- 30.Dexter DL, Kowalski HM, Blazar BA, Fligiel Z, Vogel R, Heppner GH. Heterogeneity of tumor cells from a single mouse mammary tumor. Cancer Res. 1978;38:3174–3181. [PubMed] [Google Scholar]
- 31.Bonsing BA, Corver WE, Fleuren GJ, Cleton-Jansen AM, Devilee P, Cornelisse CJ. Allelotype analysis of flow-sorted breast cancer cells demonstrates genetically related diploid and aneuploid subpopulations in primary tumors and lymph node metastases. Genes Chromosomes Cancer. 2000;28:173–183. doi: 10.1002/(sici)1098-2264(200006)28:2<173::aid-gcc6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 32.Solimene AC, Carneiro CR, Melati I, Lopes JD. Functional differences between two morphologically distinct cell subpopulations within a human colorectal carcinoma cell line. Braz J Med Biol Res. 2001;34:653–661. doi: 10.1590/s0100-879x2001000500014. [DOI] [PubMed] [Google Scholar]
- 33.Yasoshima T, Denno R, Kawaguchi S, Sato N, Okada Y, Ura H, Kikuchi K, Hirata K. Establishment and characterization of human gastric carcinoma lines with high metastatic potential in the liver: changes in integrin expression associated with the ability to metastasize in the liver of nude mice. Jpn J Cancer Res. 1996;87:153–160. doi: 10.1111/j.1349-7006.1996.tb03153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Samiei M, Waghorne CG. Clonal selection within metastatic SP1 mouse mammary tumors is independent of metastatic potential. Int J Cancer. 1991;47:771–775. doi: 10.1002/ijc.2910470525. [DOI] [PubMed] [Google Scholar]
- 35.Li Y, Tang ZY, Ye SL, Liu YK, Chen J, Xue Q, Chen J, Gao DM, Bao WH. Establishment of cell clones with different metastatic potential from the metastatic hepatocellular carcinoma cell line MHCC97. World J Gastroenterol. 2001;7:630–636. doi: 10.3748/wjg.v7.i5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Price JE, Bell C, Frost P. The use of a genotypic marker to demonstrate clonal dominance during the growth and metastasis of a human breast carcinoma in nude mice. Int J Cancer. 1990;45:968–971. doi: 10.1002/ijc.2910450532. [DOI] [PubMed] [Google Scholar]
- 37.Suzuki N, Frapart M, Grdina DJ, Meistrich ML, Withers HR. Cell cycle dependency of metastatic lung colony formation. Cancer Res. 1977;37:3690–3693. [PubMed] [Google Scholar]


