Abstract
Introduction
Physical inactivity and childhood obesity are prevalent in American children, with increased vulnerability in minority, low-resource populations. The aim of this study was to quantify the impact of physical education (PE) on in-school physical activity quantity and intensity in urban minority children attending public elementary schools.
Methods
This observational study included elementary children (N=212; mean age, 9.9 years; 81.7% black) in Grades 2–5 attending urban public schools with high eligibility for the National School Lunch Program. In-school physical activity was quantified during 4 school weeks across 4 months (January–April 2012) using Omron HJ-151 accelerometer–pedometers. Fitness was assessed with the 20-meter Progressive Aerobic Cardiovascular Endurance Run. Data were analyzed in 2013 using generalized estimating equations to determine the influence of PE and sex on total in-school steps and moderate to vigorous physical activity (MVPA) steps.
Results
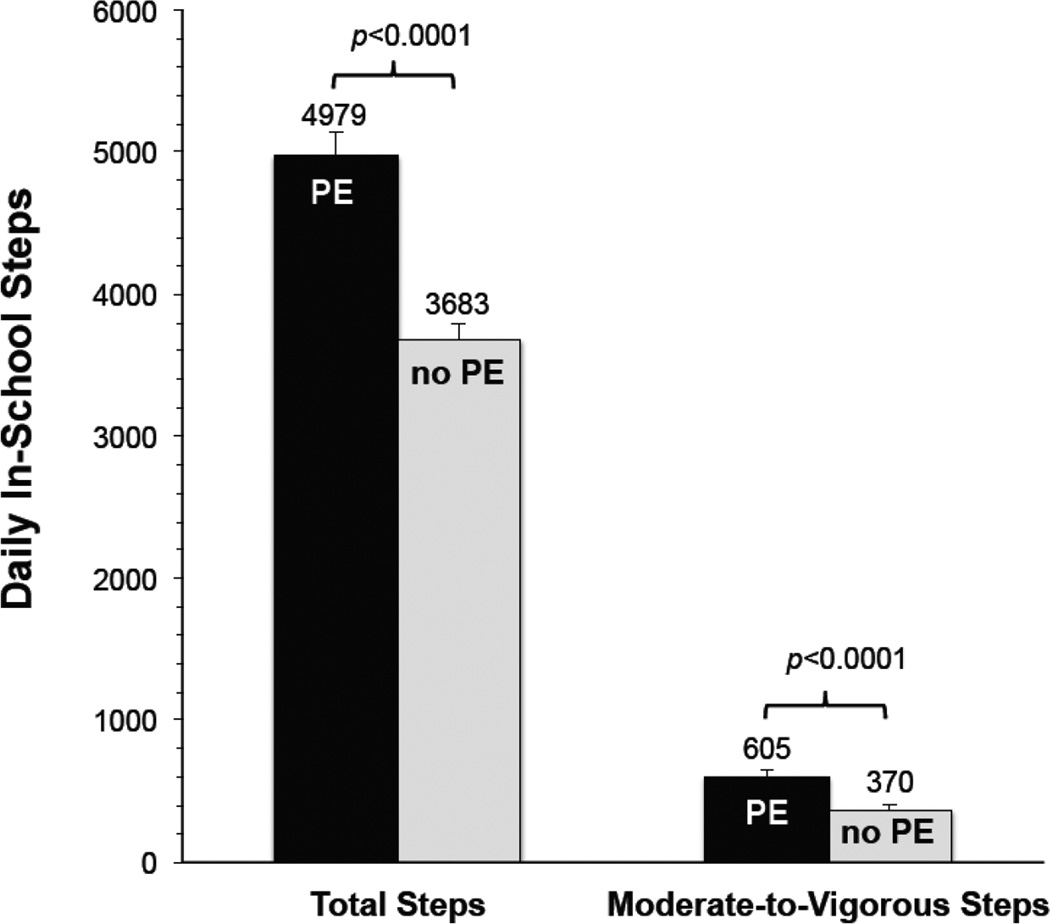
Based on 3,379 observation days (mean, 15.9 school days/student), students achieved higher in-school physical activity on days with PE (4,979 steps) than on days without PE (3,683 steps, p<0.0001). Likewise, MVPA steps were greater on days with PE than on days without PE (p<0.0001). Boys were more active than girls, but both accumulated more steps on days with PE. Low aerobic fitness was observed in 29.0% of students and overweight/obesity in 31.1%.
Conclusions
PE significantly increases total in-school and MVPA steps in urban minority elementary children. PE as a core subject can provide opportunities for urban, minority public school children in low-resource areas to achieve age-appropriate physical activity and fitness goals.
Introduction
Mounting evidence links childhood physical activity (PA) to musculoskeletal, cardiovascular, and mental health benefits, including lower adiposity and blood pressure (BP) and higher cardiorespiratory fitness, self-concept, and academic performance.1 The Physical Activity Guidelines for Americans2 and President’s Challenge Program3 recommend that children aged ≥6 years engage in ≥60 minutes of moderate to vigorous PA (MVPA) or 12,000 steps daily.2–4 Unfortunately, 58% of children and 92% of adolescents in America fail to meet these guidelines.5 PA barriers in urban settings include neighborhood safety concerns, financial constraints, or lack of access to safe playgrounds and organized activities.6 Problematically, 16.9% of American children and adolescents are obese, and racial/ethnic minorities are at greater risk than non-Hispanic whites.7,8
National initiatives,9 including Healthy People 2020,10 Surgeon General’s Vision for a Healthy and Fit Nation,11 and IOM’s Educating the Student Body,12 highlight school environments as ideal settings to provide multicomponent PA opportunities. Recommendations include enhancing physical education (PE) frequency and quality. Currently, daily PE is required in only 3.8% of public and private elementary schools.10
Pedometers are valid, reliable, objective monitors of ambulatory PA in children,13 yet the literature contains little data on in-school PA of urban minority children in low-resource neighborhoods. The aim of this study was to quantify the impact of PE on in-school PA quantity and intensity in urban minority children attending public elementary schools.
Methods
Study Population
Students in Grades 2–5 attending two public elementary schools in St. Louis, MO were invited to participate. Study inclusion required written consent of a parent/guardian and child verbal assent. This observational study was approved by the Washington University in St. Louis IRB and the Saint Louis Public Schools Research Review Committee.
Measures
In-school PA was quantified for 1 school week/month across 4 months (January–April 2012) using Omron HJ-151 uni-axial accelerometer-pedometers (Omron Healthcare, Lake Forest, IL) worn on the child’s waistband from the beginning to the end of each school day. These pedometers have been validated in children.14 Daily in-school steps and MVPA steps were saved in the instrument’s 7-day memory. At least 4 days of monitoring were required for inclusion in the analysis.15 PE classes were held twice per week in 50-minute sessions.
Cardiorespiratory fitness was assessed twice using the 20-meter Progressive Aerobic Cardiovascular Endurance Run (PACER; The Cooper Institute, Dallas, TX)16 in each school’s gymnasium. The highest number of completed laps was used to calculate maximal oxygen consumption (VO2max) with an age-, sex-, and BMI-specific formula.17 Low fitness was defined as lack of achievement of the Healthy Fitness Zone® based on sex- and age-specific VO2max standards for children aged ≥10 years.16 Additional health metrics included sex- and age-specific percentiles for BMI,7 waist circumference,8 and resting BP.18
Statistical Analysis
Analyses were conducted in 2013 using SAS, version 9.3. Generalized estimating equations with an exchangeable correlation matrix were used to compare total in-school steps and MVPA steps between PE and non-PE days and to explore sex differences. Pearson r correlation coefficients were used to explore associations between in-school steps and fitness. Significance was established using a two-tailed α=0.05.
Results
Of 222 enrolled children, 218 were assessed and 212 students (51% male) comprised the final sample. Mean age was 9.9 years (SD=1.2, range=7.7–12.3). Racial/ethnic distribution was 81.7% black, 14.9% white, 3.4% other, and 5.7% Hispanic. Eligibility for the National School Lunch Program (NSLP), an index of family poverty, was 87.6% and 97.5% at the two schools.
As shown in Table 1, the prevalence of combined overweight and obesity was 31.1%, similarly distributed in boys and girls. Equal proportions of students (18.4%) were classified as obese by BMI and abdominally obese by waist circumference. Elevated BP was observed in 4.2% of students. In an age-eligible subsample (n=100), low fitness was observed in 29.0%.
Table 1.
Risk Factor Prevalence Among Urban Public Elementary School Children
| All | Boys | Girls | Grade | ||||
|---|---|---|---|---|---|---|---|
| 2 | 3 | 4 | 5 | ||||
| N | 212 | 108 | 104 | 44 | 57 | 50 | 61 |
| % Overweight: BMI ≥85th and <95th percentile | 12.7 | 13.0 | 12.5 | 11.4 | 14.0 | 16.0 | 9.8 |
| % Obese: BMI ≥95th percentile | 18.4 | 18.5 | 18.3 | 18.2 | 15.8 | 20.0 | 19.7 |
| % Abdominally obese: WC ≥90th percentile | 18.4 | 16.7 | 20.2 | 20.5 | 14.0 | 24.0 | 16.4 |
| % Elevated BP: SBP or DBP ≥90th percentile or BP ≥120/80 mm Hg | 4.2 | 3.7 | 4.8 | 6.8 | 3.5 | 2.0 | 4.9 |
| % Low fitness: VO2max <Healthy Fitness Zone® | 29.0 | 28.3 | 28.8 | ||||
Note: Data are reported as percentages per stratum. Low fitness was determined using the 20-meter Progressive Aerobic Cardiovascular Endurance Run (PACER) in a subsample of 100 students (46 boys, 54 girls) aged ≥ 10 years. Use of the Healthy Fitness Zone® standards was permitted by The Cooper Institute, Dallas, TX.
WC, waist circumference; BP, Blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure.
A total of 3,379 PA assessments were acquired (mean days/student, 15.9; SD=3.4; range=4–20; mean steps/day, 4,216 steps/day; SD=2,067). Figure 1 highlights that total in-school steps were greater by 1,296 steps/day on PE days than non-PE days. On PE days, students achieved 41.5% of the recommended 12,000 steps in school, compared with 30.7% on non-PE days. MVPA was 235 steps/day greater on PE days than non-PE days.
Figure 1.
Daily in-school total steps and moderate-to-vigorous intensity steps on days with physical education (PE) and days without PE among 212 urban public elementary school children in 2012.
Note: Bars reflect mean and SE steps for 3,379 PA monitoring days across 4 months. Generalized estimating equations with an exchangeable correlation matrix were used to determine the influence of PE on total steps and moderate-to-vigorous steps.
Boys were more active than girls, achieving more total in-school steps (4,386 [SD=2,182] vs 4,053 [SD=1,937] steps/day, p=0.02) and more MVPA steps (529 [SD=772] vs 407 [513] MVPA steps/day, p=0.004). On days with PE, boys and girls similarly increased total steps (+1,413 and +1,184, respectively, p=0.15), but boys increased MVPA steps to a greater extent than girls (+308 vs +178 MVPA steps, p=0.003). No significant correlations were observed between fitness and daily in-school steps or MVPA steps (both p>0.10)
Discussion
Our key finding was that PE enabled urban minority elementary school children to achieve 35.2% more in-school steps and 63.5% more MVPA steps relative to days without PE. This is substantive, considering that in-school PA was low in these children compared with expected in-school steps defined by Tudor-Locke et al.19 (6,700–7,600 steps/day for boys; 4,900–6,100 for girls). To our knowledge, this is the first study quantifying the influence of PE on in-school PA in urban, predominantly black, elementary-age children from low-resource neighborhoods. Many children exhibited low fitness and the proportion classified as overweight or obese in our sample (31.1%) was similar to the National Health and Nutrition Examination Survey sample of youth assessed in 2011–2012 (31.8%).7
Our observation that PA was 1,296 steps greater on days with a 50-minute PE class supports previous studies of Hispanic children in the Bronx, NY with 89–99% NSLP eligibility (+724 steps/day on PE days)20 and Hispanic and African American children in the south with approximately 75% NSLP eligibility (1,296 steps/60-min PE class).21 Similarly, PE was shown to be the single greatest contributor (23%–25%) to in-school steps in American Indian children22 and Hispanic and non-Hispanic girls in the Southwest.23 Importantly, both boys and girls experienced benefits of PE, which supports previous research.24 When economic and environmental barriers to PA exist, the “whole-of-school approach” that includes PE as a core subject12 is critical for providing PA opportunities for all children.
Experts recommend that 33%–50% of PE time be spent in MVPA,25 with around 60–63 steps/minute during a 30-minute PE class.26 The estimated step rate in our students during 50-minute PE classes was approximately 25.9 steps/minute. The Omron pedometer’s 4-second filter excludes steps taken in activity bouts lasting <4 seconds, which may have contributed to lower step counts than school studies that used the Yamax Digi-Walker pedometer. PE quality may be enhanced by providing age- and sex-appropriate activities led by specialist instructors (particularly for minority girls who often accrue less MVPA than boys), increasing PE frequency, and limiting class sizes.
Limitations
Limitations include exclusively measuring in-school PA without segmenting the school day. Therefore, we were unable to assess achievement of national PA guidelines in our sample.
Conclusions
Our findings support frequent PE for elementary-age children, particularly in urban public school districts serving minority children in low-resource environments. Consistent with national priorities to combat childhood obesity, creating healthy school environments includes requiring quality PE daily. Modifications to state policies and resource allocation to public schools are critical. Future research should evaluate the health, behavioral, and academic benefits of PE policy changes in urban public schools.
Acknowledgments
Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 and subaward TL1 TR000449 from the National Center for Advancing Translational Sciences of the NIH and the St. Louis Community/University Health Research Partnerships grant sponsored by Washington University, Saint Louis University, and BJC HealthCare. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. The study sponsors did not have any role in the study design; collection, analysis, or interpretation of data; writing the manuscript; or submitting this report for publication. We thank members of the Nutrition and Exercise Science Laboratory at Washington University School of Medicine, Program in Physical Therapy. We are tremendously grateful for the support of administration, staff, and students at participating St. Louis Public Schools vested in our project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Strong WB, Malina RM, Blimkie CJR, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146(6):732–737. doi: 10.1016/j.jpeds.2005.01.055. http://dx.doi.org/10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 2.U.S. DHHS. 2008 Physical Activity Guidelines for Americans. Washington, DC: US DHHS; 2008. [Google Scholar]
- 3.President's Council on Fitness, Sports & Nutrition. President's Challenge Program. Presidential Active Lifestyle Award (PALA+) The President's Challenge; www.presidentschallenge.org/tools-resources/docs/getfit_old.pdf. [Google Scholar]
- 4.Colley RC, Janssen I, Tremblay MS. Daily step target to measure adherence to physical activity guidelines in children. Med Sci Sports Exerc. 2012;44(5):977–982. doi: 10.1249/MSS.0b013e31823f23b1. http://dx.doi.org/10.1249/MSS.0b013e31823f23b1. [DOI] [PubMed] [Google Scholar]
- 5.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. http://dx.doi.org/10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 6.Kottyan G, Kottyan L, Edwards NM, Unaka NI. Assessment of active play, inactivity and perceived barriers in an inner city neighborhood. J Community Health. 2014;39(3):538–544. doi: 10.1007/s10900-013-9794-6. http://dx.doi.org/10.1007/s10900-013-9794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. http://dx.doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernández JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004;145(4):439–444. doi: 10.1016/j.jpeds.2004.06.044. http://dx.doi.org/10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 9.Pate RR, Davis MG, Robinson TN, Stone EJ, McKenzie TL, Young JC. Promoting physical activity in children and youth: A leadership role for schools: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Physical Activity Committee) in collaboration with the Councils on Cardiovascular Disease in the Young and Cardiovascular Nursing. Circulation. 2006;114(11):1214–1224. doi: 10.1161/CIRCULATIONAHA.106.177052. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.177052. [DOI] [PubMed] [Google Scholar]
- 10.U.S. DHHS. Healthy People 2020: Physical Activity. HealthyPeople.gov. www.healthypeople.gov/2020/topics-objectives/topic/physical-activity/objectives.
- 11.U.S. DHHS. Surgeon General’s Vision for a Healthy and Fit Nation Fact Sheet. SurgeonGeneral.gov. http://www.surgeongeneral.gov/initiatives/healthy-fit-nation/obesityvision_factsheet.html#PAGE_4.
- 12.IOM. Educating the student body: Taking physical activity and physical education to school. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 13.Tudor-Locke C, Williams JE, Reis JP, Pluto D. Utility of pedometers for assessing physical activity: convergent validity. Sports Med. 2002;32(12):795–808. doi: 10.2165/00007256-200232120-00004. http://dx.doi.org/10.2165/00007256-200232120-00004. [DOI] [PubMed] [Google Scholar]
- 14.Hart TL, Brusseau T, Kulinna PH, McClain JJ, Tudor-Locke C. Evaluation of low-cost, objective instruments for assessing physical activity in 10–11-year-old children. Res Q Exerc Sport. 2011;82(4):600–609. doi: 10.1080/02701367.2011.10599796. http://dx.doi.org/10.1080/02701367.2011.10599796. [DOI] [PubMed] [Google Scholar]
- 15.Trost SG, Pate RR, Freedson PS, Sallis JF, Taylor WC. Using objective physical activity measures with youth: How many days of monitoring are needed? Med Sci Sports Exerc. 2000;32(2):426–431. doi: 10.1097/00005768-200002000-00025. http://dx.doi.org/10.1097/00005768-200002000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Meredith MD, Welk GJ, editors. FitnessGram & ActivityGram Test Administration Manual. 4th ed. Dallas, TX: The Cooper Institute; 2010. [Google Scholar]
- 17.Zhu W, Plowman SA, Park Y. A primer-test centered equating method for setting cut-off scores. Res Q Exerc Sport. 2010;81(4):400–409. doi: 10.1080/02701367.2010.10599700. http://dx.doi.org/10.1080/02701367.2010.10599700. [DOI] [PubMed] [Google Scholar]
- 18.National High Blood Pressure Education Program Working Group on Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2):555–576. http://dx.doi.org/10.1542/peds.114.2.S2.555. [PubMed] [Google Scholar]
- 19.Tudor-Locke C, McClain JJ, Hart TL, Sisson SB, Washington TL. Expected values for pedometer-determined PA in youth. Res Q Exerc Sport. 2009;80(2):164–174. doi: 10.1080/02701367.2009.10599550. http://dx.doi.org/10.1080/02701367.2009.10599550. [DOI] [PubMed] [Google Scholar]
- 20.Reznik M, Wylie-Rosett J, Kim M, Ozuah PO. Physical activity during school in urban minority kindergarten and first-grade students. Pediatrics. 2013;131(1):e81–e87. doi: 10.1542/peds.2012-1685. http://dx.doi.org/10.1542/peds.2012-1685. [DOI] [PubMed] [Google Scholar]
- 21.Dauenhauer BD, Keating XD. The influence of physical education on physical activity levels of urban elementary students. Res Q Exerc Sport. 2011;82(3):512–520. doi: 10.1080/02701367.2011.10599784. http://dx.doi.org/10.1080/02701367.2011.10599784. [DOI] [PubMed] [Google Scholar]
- 22.Brusseau TA, Kulinna PH, Tudor-Locke C, Ferry M. Daily physical activity patterns of children living in an American Indian community. J Phys Act Health. 2013;10(1):48–53. doi: 10.1123/jpah.10.1.48. [DOI] [PubMed] [Google Scholar]
- 23.Brusseau TA, Kulinna PH, Tudor-Locke C, Ferry M, van der Mars H, Darst PW. Pedometer-determined segmented physical activity patterns of fourth- and fifth-grade children. J Phys Act Health. 2011;8:279–286. doi: 10.1123/jpah.8.2.279. [DOI] [PubMed] [Google Scholar]
- 24.Tudor-Locke C, Lee SM, Morgan CF, Beighle A, Pangrazi RP. Children's pedometer-determined physical activity during the segmented school day. Med Sci Sports Exerc. 2006;38(10):1732–1738. doi: 10.1249/01.mss.0000230212.55119.98. http://dx.doi.org/10.1249/01.mss.0000230212.55119.98. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, McKenzie TL, Alcaraz JE, et al. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Am J Public Health. 1997;87:1328–1334. doi: 10.2105/ajph.87.8.1328. http://dx.doi.org/10.2105/AJPH.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scruggs PW, Beveridge SK, Eisenman PA, et al. Quantifying physical activity via pedometry in elementary physical education. Med Sci Sports Exerc. 2003;35(6):1065–1010. doi: 10.1249/01.MSS.0000069748.02525.B2. http://dx.doi.org/10.1249/01.MSS.0000069748.02525.B2. [DOI] [PubMed] [Google Scholar]