Abstract
STUDY DESIGN
Case report.
BACKGROUND
Proximal hamstring tendinopathy in runners is characterized by pain with passive hip flexion with the knee extended, active hip extension, and pain with sitting. Relatively little literature exists on the condition, and publications on nonsurgical treatment protocols are even more scarce. Surgical intervention, which comprises the majority of literature for treatment of this condition, is an option for cases that fail to respond to nonsurgical treatment.
CASE DESCRIPTION
The patient was a 34-year-old, otherwise healthy male triathlete with unilateral proximal hamstring tendinopathy diagnosed by ultrasound, who had pain only with running and prolonged sitting. After he failed to respond to 4 weeks of eccentric knee flexion and lumbopelvic musculature strengthening exercises, an eccentric hip extensor strengthening program using a treadmill was initiated. This treadmill exercise was performed on a daily basis, in addition to a lumbopelvic musculature strengthening program.
OUTCOMES
The patient noted a decrease in pain within 2 weeks of initiating the new exercise, and was able to return to gradual running after 4 weeks and to speed training after 12 weeks. He returned to competition shortly thereafter and had no recurrence for 12 months after the initiation of therapy. His score on the Victorian Institute of Sport Assessment-proximal hamstring tendons improved from 23 on initial presentation to 83 at 12 weeks after the initiation of therapy.
DISCUSSION
We described the management of a triathlete with subacute proximal hamstring tendinopathy, who responded well to nonsurgical treatment using eccentric hip extension strengthening using a treadmill.
LEVEL OF EVIDENCE
Therapy, level 4.
Keywords: running, tendon, triathlete
Clinically, proximal hamstring tendinopathy (PHT) is commonly seen in runners of all distances. Yet, to the authors’ knowledge, no incidence data have been published. Anatomically, the semitendinosus and the long head of the biceps femoris muscles combine to create a conjoined tendon that inserts medially on the ischial tuberosity and sacrotuberous ligament, abutted by the insertion of the semimembranosus more laterally on the tuberosity.18,26 The inferior border of the gluteus maximus and the sciatic nerve are within close proximity to the tendon.18 It is presumed that overuse, poor lumbopelvic stability, and relatively weak hamstring musculature contribute to the development of PHT.10
Runners with PHT often present with pain located near the ischial tuberosity of the affected limb that can extend down the posterior thigh.7,10,15,22 Sciatic nerve involvement and related symptoms, as evidenced by surgical exploratory findings, are often reported due to the sciatic nerve’s proximity to the site of injury.10,22,25 The sciatic nerve may be directly irritated by the proximal hamstring injury, creating true sciatic nerve involvement; however, most often PHT mimics sciatica by causing hamstring pain that refers down the posterior thigh. Common symptoms include pain with prolonged sitting, primarily on hard surfaces; pain with forward flexion of the trunk; and pain with running, often noted in the later part of the swing phase.10,22 Several diagnostic physical exam maneuvers have been described, including the Puranen-Orava test, the bent-knee stretch test, the modified bent-knee stretch test,5 and the supine 1-legged bridge.10 TABLE 1 lists common symptoms and physical exam findings seen in individuals with PHT.
TABLE 1.
Common Symptoms and Physical Examination Findings With Proximal Hamstring Tendinopathy
| Symptoms | Physical Exam Findings |
|---|---|
| Pain with trunk forward bending (passive hip flexion and knee extension) | Tenderness around the area of the ischial tuberosity |
| Localized pain in the area of the ischial tuberosity with prolonged sitting | Positive Puranen-Orava test |
| Referred pain down the posterior thigh, sometimes past the knee | Positive bent-knee stretch test |
| Pain with active hip extension and often knee flexion | Positive modified bent-knee stretch test |
| Pain worse with running | Positive supine 1-legged bridge (supine plank) test Excessive anterior pelvic tilt Possibly a positive seated slump test |
Magnetic resonance imaging and ultrasound have both been used to aid in diagnosis, with magnetic resonance imaging providing higher sensitivity.33 Common imaging features include increased tendon size, peritendinous T2 signal with a distal feathery appearance, and ischial tuberosity edema.9
The majority of the existing literature on the treatment of PHT revolves around surgical intervention, which has traditionally been reserved to address complete acute tears; however, recently, surgery has also been used to repair partial tears.3,4 Several nonsurgical options have been described for the treatment of PHT, including shockwave therapy,7 eccentric exercises with trunk/pelvis musculature strengthening,10,11 corticosteroid injection,33 massage/soft tissue mobilization,10,17 platelet-rich plasma injection,31 and a combined chiropractic approach.32 A recent description of 2 runners with PHT reported positive results with conservative treatment consisting of eccentric strengthening, lumbopelvic stabilization exercises, and trigger point dry needling of the hamstring and adductor magnus muscles.11
Eccentric strengthening is currently the most commonly accepted therapeutic exercise approach for the treatment of tendinopathy.13,14,19 The beneficial effects of eccentric exercises have been attributed to the greater tendon load generated when compared to concentric exercises,30 increased collagen synthesis,14 decreased neovascularization,20 and force fluctuations from tendon loading and unloading.24 Options for eccentric hamstring exercises include hamstring curl machines, reverse cable curls, weight-bearing hamstring curls on an exercise ball, reverse planks, kneeling “Norwegian” (or “Nordic”) leg curls, and standing single- or double-leg dead lifts. It is typically recommended that eccentric exercises for the treatment of tendinopathy be performed at a level sufficient for the individual to feel discomfort of the tendon.1,12,19,23 However, the majority of hamstring exercises focus on resisted knee flexion, whereas runners primarily rely on hip extension, moreso than knee flexion, to increase their speed.28,29 Our goal was to provide an eccentric hip extension exercise for PHT that would reproduce the patient’s typical tendon pain. In the present case, a patient who failed to initially respond to traditional eccentric exercises of the hamstring muscles was assigned an alternative exercise for the treatment of PHT that successfully improved his symptoms.
CASE DESCRIPTION
History
The patient was a 34-year-old, healthy man who had been participating in local triathlons for 14 years. He noted an insidious onset of deep buttock pain localized to the right ischial tuberosity, which started about 4 weeks prior to the clinical evaluation. His pain was exacerbated by forward bending of the trunk with locked knees (he did not have pain with hip flexion when his knees were flexed), prolonged sitting on hard surfaces, and running, primarily at high-intensity, when his pain could be as high as 7/10 (where 0 indicates no pain and 10 is the worst pain imaginable). He denied any referred pain other than mild radiation to the right lateral hamstring when the pain was more intense. He tried non-steroidal anti-inflammatories, without any significant relief. He denied numbness, tingling, weakness, bowel or bladder function changes, medication usage, recent or prior trauma, prior hamstring injuries, or prior history of stress fractures. He reported appropriate increase in his running and biking distances over the year, with no changes in footwear, bike setup, running surface, or intensity. He kept a training log indicating his daily mileage so that he was able to verify his recent training regimen. Weekly, his run mileage remained under 15 mi (24 km), his bike mileage was less than 100 mi (160 km), and he swam less than 5000 m; there were no sudden increases in training intensity or volume over the last several months. On presentation, he was able to run about 30 seconds before the onset of pain.
The Victorian Institute of Sport Assessment-proximal hamstring tendons (VISA-H) is a patient-reported outcome measure that was developed and validated for evaluating pain, function, and sporting activity in patients with PHT.6 Briefly, the VISA-H consists of 8 questions that ask about pain with activities and sport limitations related to PHT. Scores on the VISA-H range between 0 and 100, with a lower score indicating more pain and sport limitation. The minimal detectable change value for the VISA-H is approximately 4 points.6 The patient presented with a VISA-H score of 23. TABLE 2 summarizes the patient’s signs and symptoms throughout his treatment course.
TABLE 2.
Signs and Symptoms Over Time*
| Initial Presentation | After Initial Intervention (Week 4) | After 4 Weeks of Treadmill Exercise (Week 8) | After 8 Weeks of Treadmill Exercise (Week 12) | |
|---|---|---|---|---|
| Pain score with running (0–10) | 7 | 7 | 0 | 0 |
| Pain with sitting | Present | Present | Absent | Absent |
| Tendinopathy seen on ultrasound | Present | ... | Absent | ... |
| VISA-H score (0–100)† | 23 | 23 | ... | 83 |
| Running distance until onset of pain | 100 m | 100 m | 1 km, no pain | 5 km, no pain |
| Able to participate in interval training | No | No | No | Yes |
Abbreviation: VISA-H, Victorian Institute of Sport Assessment-proximal hamstring tendons.
The patient was treated using flexed-knee eccentric hamstring exercises from weeks 0 to 4, followed by an eccentric exercise performed with a treadmill starting at week 4.
A score of 100 represents no impairment.
Examination
The physical examination revealed that the patient was well developed, well nourished, thin, and in no acute distress. Pertinent positive examination findings included tenderness to palpation at the lateral aspect of the right ischial tuberosity that reproduced his pain, pain with a supine 1-legged bridge, a positive bent-knee test,5 and pain with end-range active hip extension with the knee fully extended. Negative exam findings included no pain with lumbar motion, no pain with hip range of motion performed with the knee flexed, no weakness, no asymmetry in deep tendon reflexes, negative seated slump test, negative straight leg raise test, negative sacroiliac and hip provocative maneuvers, negative single-leg hop test, no pelvic obliquity, and no leg-length discrepancy. He was able to perform 10 single-leg squats on each leg without contralateral hip drop.
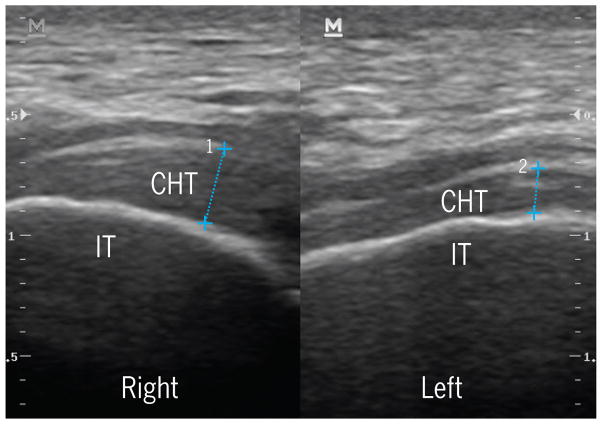
Musculoskeletal ultrasound (DC-8; Mindray Medical International Ltd, Shenzhen, China) was performed in the office, using a linear probe at a frequency of 12 MHz in long-axis orientation along the hamstring tendon at its insertion on the ischial tuberosity at a depth of 2 cm. The patient was in a prone position with the lower limbs relaxed. Previous literature33 has suggested using a 6- to 10-Hz probe, but the patient was quite thin, with a body mass index of 19 kg/m2, and good resolution was obtained when using the higher frequency. The probe was used to scan the length of the tendon. Notably, there was a thicker appearance with a more heterogeneous texture of the right (symptomatic) tendon compared to the left tendon at the site of pain over the conjoint hamstring tendon at its insertion at the ischial tuberosity. There was no insertional fluid or evidence of tearing noted at the ischial tuberosity, nor were there signs of bursal involvement. The patient noted concordance between the location of pain and the location of the ultrasound probe during imaging (FIGURE 1).
FIGURE 1.
Ultrasound images, performed at initial evaluation, of the proximal hamstring tendons near their insertion. The right side is the symptomatic side. Numbers 1 and 2 reflect the width of the tendon for the right (3.2 mm) and left (1.9 mm) limbs, respectively. Abbreviations: CHT, conjoined hamstring tendon; IT, ischial tuberosity.
Interventions
The patient was asked to stop running and was initially treated with a combination of weight-bearing and non–weight-bearing exercises. His initial program consisted of the following 2 exercises, performed 1 to 2 times daily, using controlled motions and a slow eccentric phase over approximately 5 seconds: seated hamstring curls on a weight machine (using 2 legs for the concentric and 1 leg for the eccentric portion of the exercise) and supine hamstring curls with feet on an exercise ball (starting with double-leg curls, with the goal of progressing to single-leg curls). The patient was instructed to perform the eccentric strengthening to the point of reproducing his typical tendon pain, as long as the pain was not progressively getting worse or disabling. Three sets of 15 repetitions were to be performed for each exercise.
The patient also performed 3 to 5 sets, once daily, of plank and side plank exercises, each held for 1 minute initially and progressing to 2 minutes, focusing on maintaining a neutral pelvis alignment. Finally, he was instructed in performing light hamstring stretching, short of the point of pain, for 3 minutes daily. He was also permitted to swim and cycle, as long as it was pain free; he performed these a few times a week without pain and upper-body resistance training once weekly. During this initial approach to treatment, which lasted 4 weeks, the patient was seen twice by a therapist to correct minor errors in technique.
After 4 weeks, the patient had only slight improvement in symptoms, despite good adherence to the program. His pain would return with any attempt at running that would occur during normal daily activities, such as catching a bus or playing with his children, and the pain intensity was unchanged at 7/10. He noted that the hamstring exercises never caused him pain, even when performed at maximal effort. Given the lack of changes in symptoms and the findings of the clinical exam, a repeat diagnostic ultrasound was not performed at this time. However, the options of performing magnetic resonance imaging, needle tenotomy, and/or a corticosteroid injection were discussed, but the patient preferred continuing with a nonsurgical approach to treatment.
Given the lack of progress, we devised a method of eccentric hamstring strengthening that the patient could perform with a standard treadmill. The patient faced backward on a treadmill set at a speed of approximately 0.5 mi (0.8 km) per hour. He was instructed to hold onto the rails with both hands, with his uninvolved stationary limb placed off of the belt, while maintaining a neutral pelvic position. The hip of the involved limb was then extended while maintaining the knee extended, and the foot was placed on the belt behind the patient (FIGURE 2A). The patient then resisted the belt as it pulled his foot and limb forward, while maintaining a neutral pelvic posture (FIGURES 2B and 2C). When providing active resistance to the movement of the belt, the patient’s familiar buttock pain was reproduced as his hip moved toward flexion. The patient was therefore instructed to provide enough resistance to reproduce his typical pain to a moderate level (a numeric pain rating of between 4 and 6 on a 11-point scale) during exercise. He was also instructed to make sure that the pain did not get progressively worse or become disabling.
FIGURE 2.
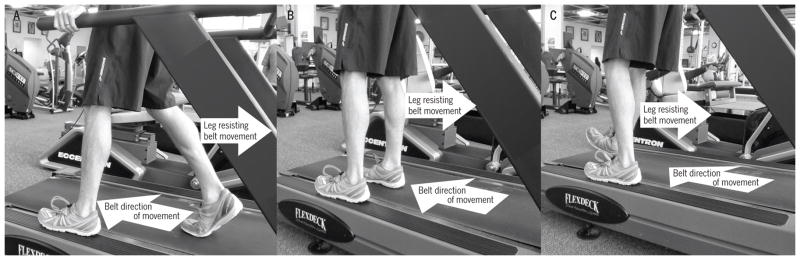
Eccentric hamstring-strengthening exercise using the treadmill. The treadmill is turned on to a slow speed, with the individual facing backward on the treadmill while holding on to the hand rails. The support side (the left leg, in this case) is placed off of the treadmill belt. (A) The involved leg (the right leg, in this case) is extended at the hip while keeping the knee mostly extended, and the individual is instructed to resist the forward motion of the belt with the leg. (B) The involved leg continues to actively resist the motion of the belt. (C) The involved leg continues to resist the belt before being repositioned to the starting point in (A).
The patient immediately noted pain when performing this exercise, as compared to the lack of pain when performing the exercises assigned in the initial 4 weeks. He was instructed to perform this exercise 1 to 2 times daily for 3 sets of 12 to 15 repetitions. He was also asked to perform his plank exercises, progressing to contralateral single-leg/single-arm planks (eg, left arm on the floor and left leg raised off the floor) to be held for 30 seconds at a time and increasing to 60 seconds on each side. He also performed the double-leg, exercise-ball hamstring curls with the same number of sets and repetitions, progressing to unweighted, single-leg curls as an additional hamstring-strengthening exercise. He was permitted to do any of the other hamstring exercises and stretching, as an optional part of his regimen, but they were not mandatory.
OUTCOMES
THE PATIENT NOTED THAT THE PAIN began to decrease within 2 weeks of initiating the treadmill exercises, allowing greater patient-perceived force to be generated for an equivalent amount of pain (4/10). The speed of the treadmill remained unchanged. He reported performing the exercises once daily on most days for the prescribed amount of sets and repetitions; he did not do any of the prior exercises that had been prescribed as optional.
He was able to resume a gradual return to running starting 4 weeks after initiating the treadmill exercise, as his pain by that time was absent when performing maximal effort on the exercise. His return-to-run protocol consisted of increasing his running mileage by 0.5 mi (0.8 km) per day each week, starting at a distance of 0.5 mi at a speed 2 minutes per mile (1:15 per km) slower than his usual running pace (eg, he ran 0.5 mi per day in week 1, 1 mi [1.6 km] per day in week 2, 1.5 mi [2.4 km] per day in week 3, etc), with no running on consecutive days. He was also progressed in his strengthening regimen to single-leg hamstring curls on an exercise ball, while continuing his treadmill exercise and lumbopelvic musculature strengthening program.
Ultrasound imaging was repeated 8 weeks after the initial evaluation and showed a decrease in the tendon diameter, without tenderness from contact with the probe (diameter, 2.0 mm for the right tendon and 2.3 mm for the left tendon at the former site of pain). The ultrasound image (FIGURE 3) was obtained with a 12-MHz linear probe in the long axis of the hamstring tendon at a screen depth of 3.5 cm, with the patient prone and the lower limbs relaxed. Images of the conjoint tendon of the hamstring at the ischial tuberosity insertion were screen captured at approximately the same location on both sides of the patient. The measurement for the conjoint tendon thickness was taken over the ischial tuberosity at its thickest point on both sides.
FIGURE 3.
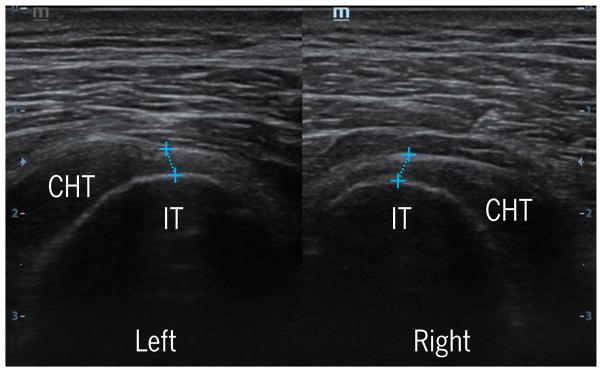
Ultrasound images, performed at 8 weeks after initial examination, of the proximal hamstring tendons near their insertion. The right side is the symptomatic side; the widths of the 2 tendons are similar. Abbreviations: CHT, conjoined hamstring tendon; IT, ischial tuberosity.
On physical examination, the patient had significantly decreased tenderness to palpation of the proximal hamstring tendon, decreased pain with the aforementioned provocative maneuvers, and decreased report of pain with sitting (maximum, 2/10 intensity). He was able to begin speed training approximately 12 weeks after the initial examination, at which point his VISA-H score was 83 and he had complete resolution of the previously reported pain complaints with forward bending at the trunk or sitting. He continued to do the same eccentric hamstring exercise on the treadmill without change of form. One year after initial evaluation, the patient had not had a recurrence of pain, had a VISA-H score of 100, and had returned to competition 6 months earlier.
DISCUSSION
SUBSEQUENT TO A LACK OF POSITIVE response to 4 weeks of using flexed-knee, eccentric hamstring-strengthening exercises, we devised a simple method to exercise the hamstring muscles eccentrically while maintaining knee extension. The patient started improving within 2 weeks of initiating the eccentric exercise performed on a treadmill, and had complete resolution of symptoms and returned to full activities within 12 weeks. Our primary assumption to explain the difference in response to exercises is that the treadmill exercise enabled the patient to create sufficient force in the affected tendon to provoke pain during exercises,8,16 which has been suggested to be an important part of eccentric training for tendinopathy in other areas of the body.1,19
While the recovery of this patient was on the faster side of previously reported recovery times for injuries involving the proximal hamstring,2 it should be noted that the patient had already been performing 4 weeks of alternative strengthening exercises, which might have allowed a more rapid recovery than would otherwise be expected. The proposed treadmill exercise has the benefit of allowing the patient to titrate the force based on perceived pain during the exercise.1,19 Furthermore, the hamstring muscles were loaded in a body position that was functional for the patient, who commented that the strain felt on the tendon when doing the exercise correlated with the point of pain during the running stride. Additionally, we believe that runners will strongly relate to this type of eccentric exercise, as it incorporates typical equipment associated with running: a treadmill.
One limitation of this case is the absence of magnetic resonance images, which the patient declined due to cost. Magnetic resonance imaging has been found to be more sensitive than ultrasound for diagnosing PHT.33 Though the measurement of distance with ultrasound has been demonstrated to be accurate,21,27 identification of tendon thickening requires a comparison (either the contralateral side or a re-evaluation at a later time). Though the unilateral nature of the patient’s symptoms allowed for a subjective contralateral comparison and the location of pain could be used as a landmark, the identical location on the asymptomatic side was difficult to identify. Similarly, once the patient became symptom free, a later comparison at the identical location was difficult to identify with ultrasound and was based on the best approximation of the ultrasonographer. In standard practice of musculoskeletal ultrasonography, bilateral comparisons are performed by creating a screenshot image that best represents the mirror image of the contralateral side by using bony landmarks. There are limitations to this method, because individuals may have bony abnormalities (ie, bone spurs) that create variations in side-to-side bony landmarks. However, this method reflects the best standards of practice in ultrasound imaging.
We stress the importance of appropriate lumbopelvic posture in this method and recommend the concomitant use of lumbopelvic-strengthening exercises, with additional potential benefit from soft tissue mobilization or massage. Our patient did not demonstrate sciatic nerve symptoms, which might have changed our treatment plan and should be monitored throughout the course of treatment. Additionally, our patient demonstrated no hip abductor strength deficits, which should also be considered in the initial biomechanical evaluation of the patient. The patient in this case was highly motivated, which is a requirement for such a time-intensive therapy.
CONCLUSION
THIS CASE REPORT DEMONSTRATES the use of an alternative method for treatment of PHT using eccentric strengthening of the hamstring muscles, using a treadmill. Though our patient demonstrated significant improvement with our method, further study of this exercise in a larger population of patients with PHT is warranted before this approach can be recommended for implementation.
Acknowledgments
Dr Rho's time is paid for in part by a grant from the National Institutes of Health (K12HD001097-16).
Footnotes
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
References
- 1.Alfredson H, Pietilä T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360–366. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- 2.Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med. 2007;35:1716–1724. doi: 10.1177/0363546507303563. http://dx.doi.org/10.1177/0363546507303563. [DOI] [PubMed] [Google Scholar]
- 3.Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-013-2817-0. In press. http://dx.doi.org/10.1007/s00167-013-2817-0. [DOI] [PubMed]
- 4.Bowman KF, Jr, Cohen SB, Bradley JP. Operative management of partial-thickness tears of the proximal hamstring muscles in athletes. Am J Sports Med. 2013;41:1363–1371. doi: 10.1177/0363546513482717. http://dx.doi.org/10.1177/0363546513482717. [DOI] [PubMed] [Google Scholar]
- 5.Cacchio A, Borra F, Severini G, et al. Reliability and validity of three pain provocation tests used for the diagnosis of chronic proximal hamstring tendinopathy. Br J Sports Med. 2012;46:883–887. doi: 10.1136/bjsports-2011-090325. http://dx.doi.org/10.1136/bjsports-2011-090325. [DOI] [PubMed] [Google Scholar]
- 6.Cacchio A, De Paulis F, Maffulli N. Development and validation of a new VISA questionnaire (VISA-H) for patients with proximal hamstring ten-dinopathy. Br J Sports Med. 2014;48:448–452. doi: 10.1136/bjsports-2012-091552. http://dx.doi.org/10.1136/bjsports-2012-091552. [DOI] [PubMed] [Google Scholar]
- 7.Cacchio A, Rompe JD, Furia JP, Susi P, San-tilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med. 2011;39:146–153. doi: 10.1177/0363546510379324. http://dx.doi.org/10.1177/0363546510379324. [DOI] [PubMed] [Google Scholar]
- 8.Cahalan TD, Johnson ME, Liu S, Chao EY. Quantitative measurements of hip strength in different age groups. Clin Orthop Relat Res. 1989:136–145. [PubMed] [Google Scholar]
- 9.De Smet AA, Blankenbaker DG, Alsheik NH, Lindstrom MJ. MRI appearance of the proximal hamstring tendons in patients with and without symptomatic proximal hamstring tendinopathy. AJR Am J Roentgenol. 2012;198:418–422. doi: 10.2214/AJR.11.6590. http://dx.doi.org/10.2214/AJR.11.6590. [DOI] [PubMed] [Google Scholar]
- 10.Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. Phys Sportsmed. 2005;33:32–43. doi: 10.3810/psm.2005.05.89. http://dx.doi.org/10.3810/psm.2005.05.89. [DOI] [PubMed] [Google Scholar]
- 11.Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. J Orthop Sports Phys Ther. 2014;44:198–205. doi: 10.2519/jospt.2014.4905. http://dx.doi.org/10.2519/jospt.2014.4905. [DOI] [PubMed] [Google Scholar]
- 12.Jonsson P, Wahlström P, Öhberg L, Alfredson H. Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14:76–81. doi: 10.1007/s00167-004-0611-8. http://dx.doi.org/10.1007/s00167-004-0611-8. [DOI] [PubMed] [Google Scholar]
- 13.Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. Br J Sports Med. 2007;41:e3. doi: 10.1136/bjsm.2006.030916. http://dx.doi.org/10.1136/bjsm.2006.030916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Langberg H, Kongsgaard M. Eccentric training in tendinopathy – more questions than answers. Scand J Med Sci Sports. 2008;18:541–542. doi: 10.1111/j.1600-0838.2008.00864.x. http://dx.doi.org/10.1111/j.1600-0838.2008.00864.x. [DOI] [PubMed] [Google Scholar]
- 15.Lempainen L, Banke IJ, Johansson K, et al. Clinical principles in the management of hamstring injuries. Knee Surg Sports Traumatol Arthrosc. doi: 10.1007/s00167-014-2912-x. In press. http://dx.doi.org/10.1007/s00167-014-2912-x. [DOI] [PubMed]
- 16.Malliaropoulos N, Papalexandris S, Papalada A, Papacostas E. The role of stretching in rehabilitation of hamstring injuries: 80 athletes follow-up. Med Sci Sports Exerc. 2004;36:756–759. doi: 10.1249/01.mss.0000126393.20025.5e. [DOI] [PubMed] [Google Scholar]
- 17.McCormack JR. The management of bilateral high hamstring tendinopathy with ASTYM® treatment and eccentric exercise: a case report. J Man Manip Ther. 2012;20:142–146. doi: 10.1179/2042618612Y.0000000003. http://dx.doi.org/10.1179/2042618612Y.0000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller SL, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):108–116. doi: 10.2106/JBJS.G.01281. http://dx.doi.org/10.2106/JBJS.G.01281. [DOI] [PubMed] [Google Scholar]
- 19.Murtaugh B, Ihm JM. Eccentric training for the treatment of tendinopathies. Curr Sports Med Rep. 2013;12:175–182. doi: 10.1249/JSR.0b013e3182933761. http://dx.doi.org/10.1249/JSR.0b013e3182933761. [DOI] [PubMed] [Google Scholar]
- 20.Öhberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic mid-portion Achilles tendinosis? Knee Surg Sports Traumatol Arthrosc. 2004;12:465–470. doi: 10.1007/s00167-004-0494-8. http://dx.doi.org/10.1007/s00167-004-0494-8. [DOI] [PubMed] [Google Scholar]
- 21.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–1406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 22.Puranen J, Orava S. The hamstring syndrome. A new diagnosis of gluteal sciatic pain. Am J Sports Med. 1988;16:517–521. doi: 10.1177/036354658801600515. [DOI] [PubMed] [Google Scholar]
- 23.Purdam CR, Jonsson P, Alfredson H, Lorentzon R, Cook JL, Khan KM. A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. Br J Sports Med. 2004;38:395–397. doi: 10.1136/bjsm.2003.000053. http://dx.doi.org/10.1136/bjsm.2003.000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rees JD, Lichtwark GA, Wolman RL, Wilson AM. The mechanism for efficacy of eccentric loading in Achilles tendon injury; an in vivo study in humans. Rheumatology (Oxford) 2008;47:1493–1497. doi: 10.1093/rheumatology/ken262. http://dx.doi.org/10.1093/rheumatology/ken262. [DOI] [PubMed] [Google Scholar]
- 25.Saikku K, Vasenius J, Saar P. Entrapment of the proximal sciatic nerve by the hamstring tendons. Acta Orthop Belg. 2010;76:321–324. [PubMed] [Google Scholar]
- 26.Sato K, Nimura A, Yamaguchi K, Akita K. Anatomical study of the proximal origin of hamstring muscles. J Orthop Sci. 2012;17:614–618. doi: 10.1007/s00776-012-0243-7. http://dx.doi.org/10.1007/s00776-012-0243-7. [DOI] [PubMed] [Google Scholar]
- 27.Saxton DW, Farquhar CM, Rae T, Beard RW, Anderson MC, Wadsworth J. Accuracy of ultrasound measurements of female pelvic organs. Br J Obstet Gynaecol. 1990;97:695–699. doi: 10.1111/j.1471-0528.1990.tb16241.x. [DOI] [PubMed] [Google Scholar]
- 28.Schache AG, Blanch PD, Dorn TW, Brown NA, Rosemond D, Pandy MG. Effect of running speed on lower limb joint kinetics. Med Sci Sports Exerc. 2011;43:1260–1271. doi: 10.1249/MSS.0b013e3182084929. http://dx.doi.org/10.1249/MSS.0b013e3182084929. [DOI] [PubMed] [Google Scholar]
- 29.Schache AG, Dorn TW, Williams GP, Brown NA, Pandy MG. Lower-limb muscular strategies for increasing running speed. J Orthop Sports Phys Ther. 2014;44:813–824. doi: 10.2519/jospt.2014.5433. http://dx.doi.org/10.2519/jospt.2014.5433. [DOI] [PubMed] [Google Scholar]
- 30.Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986:65–68. [PubMed] [Google Scholar]
- 31.Wetzel RJ, Patel RM, Terry MA. Platelet-rich plasma as an effective treatment for proximal hamstring injuries. Orthopedics. 2013;36:e64–e70. doi: 10.3928/01477447-20121217-20. http://dx.doi.org/10.3928/01477447-20121217-20. [DOI] [PubMed] [Google Scholar]
- 32.White KE. High hamstring tendinopathy in 3 female long distance runners. J Chiropr Med. 2011;10:93–99. doi: 10.1016/j.jcm.2010.10.005. http://dx.doi.org/10.1016/j.jcm.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010;195:993–998. doi: 10.2214/AJR.09.3674. http://dx.doi.org/10.2214/AJR.09.3674. [DOI] [PubMed] [Google Scholar]