Abstract
Purpose of review
Heart failure prevention is an important public health goal. Increased physical activity and exercise may help to prevent heart failure, as they are associated with reduced heart failure incidence and potentially act through a variety of mechanisms to slow disease progression.
Recent findings
Increased physical activity, higher cardiorespiratory fitness, and lower sedentary time are associated with reduced heart failure incidence. These associations are consistent for occurrence of both heart failure with preserved versus reduced ejection fraction, the common subphenotypes of the condition. Physiologic cardiac and vascular remodeling occur across the normal range of physical activity in the community, and regular exercise (4–5 sessions per week) is necessary to mitigate age-associated reductions in ventricular compliance and cardiac mass.
Summary
Greater physical activity, lesser sedentary time and improved cardiorespiratory fitness are associated with reductions in heart failure risk. Various mechanisms may explain these findings including: reducing the prevalence of standard and novel cardiovascular risk factors, inhibiting pathologic cardiovascular remodeling, promoting physiologic remodeling, and improving cardiac, neurohormonal, skeletal muscle, pulmonary, renal, and vascular performance. Future research is needed to elucidate the optimal timing, duration, and modality of physical activity and exercise training necessary to prevent the development of heart failure.
Keywords: heart failure, physical activity, exercise, remodeling, prevention
Introduction
Heart failure (HF) is a growing public health problem, with a prevalence in the United States that is projected to increase from approximately 5.7 million people, to over 8 million by 2030 [1]. This rising prevalence has been attributed to improved survival of individuals with myocardial infarction and patients with HF, and to the high population burden of HF risk factors such as hypertension, obesity, diabetes and smoking [2, 3]. While physical activity and regular exercise are emphasized for promoting general cardiovascular health [4], contemporary HF guidelines have not adequately emphasized the importance of and recommendations for physical activity as a means of preventing the condition [5]. However, recent evidence suggests that physical inactivity may be an important risk factor for HF, and that physical activity and exercise training slow the progression of HF severity via several mechanisms.
Three features of the cardiovascular response to exercise make the associations with HF especially intriguing. First, in order to perform exercise, the cardiac output must increase significantly; in fact endurance athletes are known to increase their cardiac output by 6-fold during training [6]. Since HF results from an inability to augment cardiac output to meet the body’s metabolic demands, it is possible that exercise training might serve to preserve and maintain cardiac output in those individuals at greater risk for HF. Second, HF is primarily a disease of older people, in whom regular physical activity has been associated with reduced risks of cardiovascular events [7], cognitive decline [8], and all-cause mortality [9]. Since these disorders share common risk factors with HF, we might expect a similar beneficial impact of physical activity and exercise on HF too. Third, it has long been known that competitive athletes undergo physiologic cardiac remodeling [10], a response that might be employed to counteract the maladaptive (pathologic) cardiac remodeling that occurs upon exposure to risk factors, such as hypertension and obesity. In this review, we will present the evidence relating increased physical activity to a reduced risk of HF, explore these associations across the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) HF Stages (A–C), and then briefly evaluate biological mechanisms that might underlie the cardioprotective effects of physical activity and exercise.
Measuring Physical Activity
Before reviewing the associations of physical activity with HF, it is important to define physical activity in this context. A physical activity index, often used in community-based cohort studies, can be derived from questionnaires by combining participants’ self-reported average levels of activity during work, leisure-time, and exercise. Therefore exercise is a component of physical activity. Sedentary time can also be ascertained from physical activity questionnaires. Although many individuals with high levels of physical activity may also have lower sedentary times, these two variables are not always in congruence. For example, someone who has a sedentary job (sitting at a desk, for example) may also perform strenuous exercise daily, and thus may have relatively high levels of both sedentary time and physical activity.
Physical Activity and Heart Failure Incidence
A number of community-based studies have demonstrated an association of greater physical activity with a reduced incidence of HF. In both the Physicians Health Study [11] and the Women’s Health Initiative [12], a relatively high level of physical activity was one of several healthy lifestyle factors associated with a lower risk of HF. Conversely, physical inactivity, or sedentary time, was associated with an elevated risk for HF in the First National Health and Nutrition Examination Survey (NHANES I) [13]. Using data from the California Men’s Health Study, investigators confirmed that lower sedentary time and higher physical activity have independent and consistent associations with reductions in HF incidence [14*]. Similarly, in an elderly cohort from the Framingham Heart Study, there was an incremental reduction in HF incidence across tertiles of physical activity [15]. Furthermore, reductions in physical activity during the follow-up time were associated with additional elevations in the risk of HF. These investigators went a step further by evaluating the relations of physical activity to the risk of both HF subtypes, i.e., with preserved ejection fraction (HFPEF) versus reduced ejection fraction (HFREF). The association of lower physical activity with an increased risk of HF persisted for both HFPEF and HFREF (in minimally-adjusted models) and was attenuated after adjustment for body mass index (BMI), suggesting that excess weight might be along the causal pathway. Although maintenance of a healthy body weight with exercise may be an important factor in reducing the risk of HF, data from a Finnish cohort of 60,000 individuals demonstrated that physical activity was protective across levels of BMI, suggesting an effect that was independent of adiposity [16]. These aforementioned studies all relied on physical activity questionnaires to ascertain the level of physical activity, which might introduce misclassification.
In contrast, cardiorespiratory fitness can be directly measured and is closely related to physical activity and exercise. In the Cooper Center Longitudinal Study, mid-life cardiorespiratory fitness was measured by exercise testing and was observed to be strongly and inversely associated with HF mortality over the next 20 years [17]. Furthermore, fit individuals had significantly reduced risk of HF mortality compared with unfit individuals with the same risk factor profiles, demonstrating that the benefits of cardiorespiratory fitness were independent of traditional cardiovascular risk factors. The associations of physical activity with cardiorespiratory fitness were not explored.
The preceding reports demonstrate consistent findings linking higher physical activity, less sedentary time, and improved physical fitness with a reduced risk of HF. However, causal inferences are limited by the observational design of these prior investigations. Of greatest concern, perhaps, is the possibility of reverse causality whereby subclinical or undiagnosed cardiac dysfunction may be associated with lower levels of physical activity (for example), thereby apparently resulting in the association of the latter with HF risk. In order to further evaluate the impact of physical activity on HF risk, we will explore the associations of physical activity across the stages of HF disease progression.
Preventing the Development of Heart Failure Risk Factors (Stage A)
Stage A HF is characterized by the presence of established HF risk factors, including hypertension, obesity, diabetes, smoking, and coronary artery disease [5]. Each of these conditions leads to decrements in cardiac function by promoting myocardial ischemia and/or promoting adverse cardiac remodeling (stage B). Conversely, physical activity is associated with improvements in hypertension, obesity, blood glucose and reductions in the incidence of coronary artery disease [18]. An appraisal of the independent relations of physical activity with these individual risk factors is beyond the scope of this review. However, it is clear that one way in which physical activity may lead to a lower incidence of HF is by decreasing the burden and the severity of HF risk factors.
Preventing Adverse Changes in Cardiac Structure and Function (Stage B)
In athletes, the ability of the heart to adapt to the physiologic stress of exercise is well described, and has been termed “athlete’s heart” [10]. Increased left ventricle (LV) mass with proportional elevations in volume to preserve the LV mass-to-volume ratio (eccentric hypertrophy), improved LV diastolic function, right ventricle (RV) enlargement and increased left atrial volumes have been reported in endurance athletes (in whom higher stroke volumes are essential), but individual-level adaptations appear to be affected by the specific sport or the type of exercise performed [6, 10].
Observations from community-based studies indicate that favorable cardiac remodeling with physical activity is also detectable in non-athletes. In the Multi-Ethnic Study of Atherosclerosis (MESA), higher levels of physical activity were associated with greater LV mass and end-diastolic volumes in a non-athletic sample aged 45–84 years [19]. Physical activity, measured by accelerometry for one week, was associated with higher LV mass and reduced vascular stiffness in the Framingham Heart Study [20*]. Similarly, in the Cooper Center Longitudinal Study, higher cardiorespiratory fitness was associated with larger LV mass, increased end-diastolic diameters, and a lower prevalence of LV diastolic dysfunction [21*]. Although these epidemiologic data do support associations of physical activity with cardiac traits, much is unknown regarding the duration, modality and chronicity of physical activity necessary to achieve these results, and if these adaptations indeed affect individual outcomes.
Cardiac aging is characterized by concentric remodeling (preserved LV mass with reduced LV internal dimensions) and decrements in LV diastolic function, which are theorized to contribute to the increased risk of HF in older adults [22, 23]. Since physical activity has been related to higher LV internal dimensions and improved LV diastolic function, age-associated cardiac remodeling might be an appropriate target for exercise therapy. Levine and colleagues have explored this intriguing hypothesis in a number of experiments. Using invasive hemodynamic evaluation, these investigators measured LV compliance in twelve healthy sedentary seniors (mean age 70 years), twelve competitive Masters level athletes (mean age 68 years), and fourteen young but sedentary control subjects (mean age 29 years) [24]. The sedentary seniors displayed reduced LV compliance, while the Masters level athletes and sedentary young controls both had normal ventricular compliance curves, demonstrating that reductions in LV compliance with aging are not inevitable, and perhaps may be avoidable. Since the intensity of training required to compete as a Masters level athlete is not possible for most, these investigators next evaluated the “dose” of exercise required to prevent age-associated reductions in LV compliance [25**]. They studied 102 healthy seniors divided into 4 groups based on their exercise patterns over the preceding 25 years: sedentary (<2 exercise sessions/week), casual exercisers (2–3 sessions/week), committed exercisers (4–5 sessions/week) and competitive Masters level athletes (6–7 sessions/week). The sedentary seniors and casual exercisers had reduced LV compliance, while the committed exercisers achieved an average LV compliance approaching that of the Masters level athletes. In addition, using cardiac MRI, cardiac atrophy, characterized by decreased LV mass and end-diastolic volume with preserved mass-to-volume ratio, was observed in the casual exercisers and sedentary individuals.
Several of these investigators also carefully examined the effects of dedicated endurance training on cardiac structure and function. In one such study, 12 sedentary young adults were enrolled in a one-year exercise program designed to train them for a marathon [26**]. Training was relatively low intensity for the first 6 months and then became more rigorous. In the first 6–9 months, the participants developed increased LV mass without a change in volume (concentric hypertrophy), increased RV mass, increased RV end-diastolic volume, increased stroke volume and improved LV compliance. After the full year of the exercise training program, there was an increase in LV end-diastolic volume that restored the baseline mass-to-volume ratio (eccentric hypertrophy). However, the same changes were not observed in 12 sedentary seniors (mean age 70) undergoing one year of endurance training [27]. In these subjects, although eccentric hypertrophy was demonstrated, no significant improvement in LV compliance was observed. The authors hypothesized that some of the molecular or structural changes that result in reduced LV compliance with aging must, therefore, be irreversible.
To summarize, a number of cross-sectional studies have related higher levels of physical activity and cardiorespiratory fitness to increases in LV mass, higher LV internal dimensions, and reductions in vascular stiffness. Studies of seniors free of cardiovascular risk factors have demonstrated that age-related reductions in LV compliance are prevented by a regular exercise routine of at least 4–5 sessions per week. However, one year of endurance training in older adults with reduced LV compliance did not restore the LV compliance to that observed in younger individuals. Finally, although associations between physical fitness and LV systolic function were not observed, it is important to note that in these community-based studies, very few participants had asymptomatic LV dysfunction. The effects of exercise training and physical activity in this group remain unknown.
Prevention of Manifest Heart Failure or Disease Progression (Stage C)
Although it is largely outside the scope of this review, there is extensive literature supporting the benefits of exercise training for individuals with stable HF symptoms. To briefly summarize, in a large randomized controlled trial including over 2000 participants with HFREF, aerobic exercise training was associated with modest reductions in cardiovascular hospitalizations and mortality, and with improved quality of life [28, 29]. Additional studies have demonstrated reverse cardiac remodeling in response to exercise training in patients with HFREF [30, 31]. Although the data are less robust, there are also reports of improved functional capacity, enhanced quality of life, and suggestions of reverse remodeling with exercise training in individuals with HFPEF [32, 33*].
Biological Mechanisms Linking Exercise with Heart Failure Prevention
Favorable exercise-induced adaptations in a number of organ systems have been proposed to explain the associations of increased physical activity with reduced HF incidence and with improved clinical outcomes in those with overt HF. As previously discussed, physical activity, exercise training, sedentary time, and cardiorespiratory fitness have each been independently associated with HF incidence and cardiac remodeling. It is possible therefore, that each of these characteristics exerts independent and specific physiologic effects. However, due in part to the complexities of creating experimental models for sedentary time, non-exercise physical activity, and cardiorespiratory fitness, much more is known about the effects of exercise training.
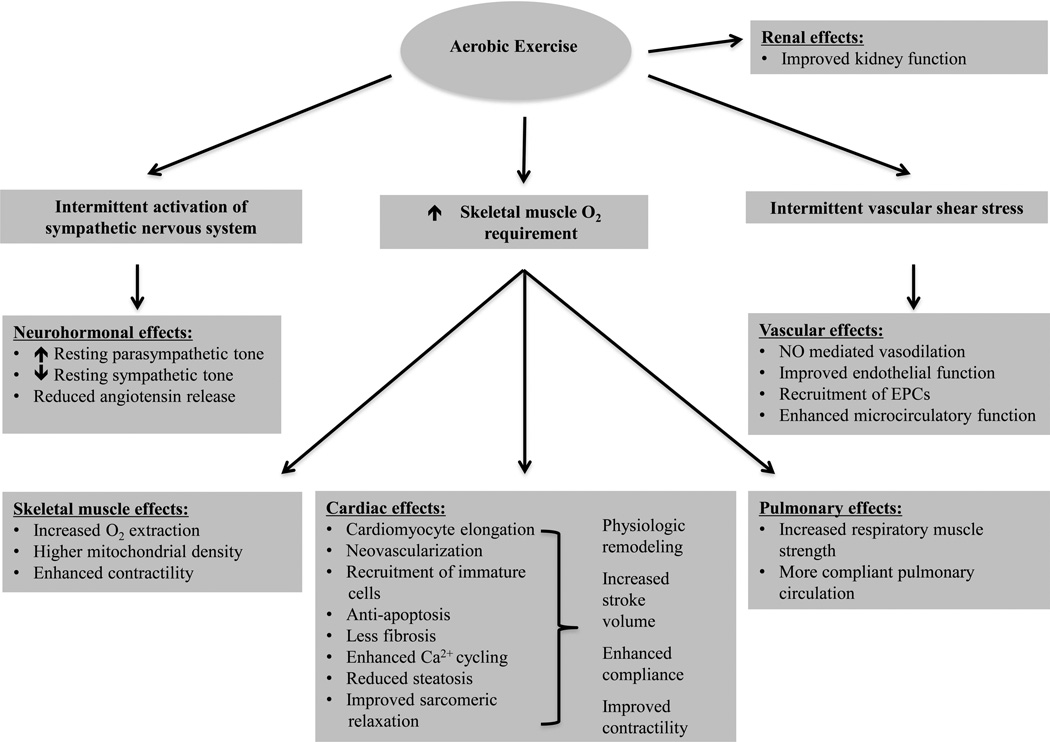
In the following section, we will briefly review the molecular pathways involved in the physiologic adaptations to exercise, organized by organ system (summarized in the Figure). It is important to consider that changes with exercise may more accurately be viewed as restoring end-organ adaptations to a true physiologic baseline (in an evolutionary sense for humans as hunter-gatherers), since contemporary societal levels of diminished physical activity and increased sedentary time are unprecedented in human evolution [34].
Figure.
Schematic representation of mechanisms potentially contributing to the benefits of exercise for prevention of heart failure.
O2 indicates oxygen; NO, nitric oxide; Ca2+, calcium.
Effects of Exercise on the Heart
Physiologic cardiac remodeling varies according to the specific hemodynamic load imposed, and manifests as eccentric remodeling with endurance training and concentric remodeling with resistance training [10]. However, these remodeling patterns demonstrate remarkable plasticity. This is best illustrated by studies of 2 weeks of forced bed rest, which resulted in reductions in LV mass consistent with cardiac atrophy, and were prevented by supine exercise training [35]. Controversy exists regarding the extent of overlap in signaling pathways responsible for physiologic cardiac hypertrophy in response to exercise, and pathologic cardiac hypertrophy resulting from risk factors such as hypertension and obesity. However, certain histologic characteristics are unique to the two types of cardiac hypertrophy patterns [36]. For example, pathologic hypertrophy is characterized by loss of cardiomyocytes with fibrotic replacement, while physiologic hypertrophy results from increases in cardiomyocytes size, neovascularization, and likely, myocyte proliferation [37*]. Indeed, animal models have demonstrated reductions in apoptotic signaling in cardiomyocytes with exercise. In a rat model, moderate exercise resulted in attenuation of age-associated increases in the Bax/Bcl-2 (Bax and Bcl-2 are cytosolic proteins, with a higher ratio promoting apoptosis) and increased expression of heat shock protein 70, which is known to reduce cardiomyocyte apoptosis [38]. Cardiomyocyte proliferation was also demonstrated in a mouse model of endurance training, which was attributed to transcriptional activation of CITED4 (a transcription factor promoting cardiomyocyte proliferation) expression and reductions in the expression of C/EBPβ (a transcription factor with roles in cell proliferation and differentiation) [39]. Furthermore, in a model of spontaneously hypertensive rats, exercise training attenuated the development of HF and was related to preservation of normal LV geometry and reductions in fibrosis through activation of the phosphoinositide 3-kinase (PI3K)- Akt pathway (the PI3K-Akt signaling pathway has been implicated in regulation of cell size, apoptosis and fibrosis) [40]. Furthermore, cardiomyocyte performance appears to be improved with exercise training as a result of a variety of mechanisms. For example, expression of sarcoplasmic reticulum Ca2+ ATPase (SERCA2a) mRNA and protein levels are increased by exercise, and result in improved calcium cycling and enhanced cardiac contractility [36].
Several additional mechanisms have been hypothesized to explain improved ventricular diastolic function with exercise. Myocardial steatosis, which is related to low levels of physical fitness and elevated BMI, results in reductions in ventricular distensibility [41]. Another intriguing explanation for improved ventricular diastolic function with exercise training is posttranslational modification of the cardiomyocyte protein titin. There is evidence from a mouse model that phosphorylation of titin, an important sarcomeric protein, is affected by exercise resulting in reduced sarcomere stiffness that in turn translates into improvements in ventricular compliance and distensibility [42].
Neurohormonal Balance
Increased neuroadrenergic drive contributes to HF disease progression. Several lines of research support a role for exercise in restoring a healthy neurohormonal balance. In one study of individuals with chronic HF, a 16% reduction in plasma norepinephrine concentration was observed after 8 weeks of exercise training [43]. Furthermore, in a rat model of ischemic HF, exercise training was associated with significant reduction in angiotensin converting enzyme mRNA expression in cardiomyocytes [44]. Although restoration of a healthy neurohormonal balance in patients with chronic HF is certainly beneficial, the extent to which these changes are helpful in preventing HF is unclear. However, given that an elevated resting heart rate (resulting from increased sympathetic and reduced parasympathetic tone) has been associated with incident HF, this hypothesis warrants further investigation [45].
Improved Function of Endothelium and Peripheral Vasculature
Intermittent increases in the laminar shear stress associated with exercise are responsible for favorable effects on the vascular endothelium [34]. Laminar shear stress activates PI3K and nitric oxide (NO), which promote vascular dilation. Further contributing to improved endothelial function with exercise, endothelial progenitor cells (EPCs) and mesenchymal stem cells are mobilized from the bone marrow, and serve to maintain vascular integrity [34]. In addition to the endothelium-mediated vasodilation of the larger and medium-sized resistance vessels, the smaller arterioles are controlled via metabolic and myogenic signals, which are both favorably affected by exercise and improve microcirculatory function.
Skeletal Muscle Performance
Exercise intolerance is a cardinal clinical feature of HF and reduced efficiency of peripheral oxygen extraction in the skeletal muscles is an important contributor [46]. Exercise training improves skeletal muscle performance by promoting increased mitochondrial density, improved contractility and enhanced peripheral oxygen extraction [47], thereby enhancing skeletal muscle performance during exercise.
Pulmonary Function
Pulmonary function is improved by exercise training in several ways. For instance, ventilatory efficiency increases during exercise training as a result of increased respiratory muscle strength. In addition, it has been suggested that exercise training may lead to improved distensibillity of the pulmonary circulation [48*]. At this time, the cardiopulmonary interactions with exercise and their relations to myocardial performance and future HF risk remain largely unexplored.
Renal Function
Less sedentary time and higher cardiorespiratory fitness are associated with better kidney function [49, 50]. Improved endothelial and microvascular function, and control of risk factors for kidney disease, such as obesity and hypertension, are hypothesized to contribute to the observed associations, but precise mechanisms have not been determined.
In addition to the above mechanisms and organ systems, many others are likely to contribute to the beneficial effects of exercise in those at elevated risk for HF. Additional research is warranted to uncover the optimal exercise training techniques for each biological pathway and target organ, and to discover ways in which this knowledge may be harnessed to develop individualized exercise regimens.
Conclusion
In observational studies, increased physical activity, lesser sedentary behavior, and greater cardiorespiratory fitness all correlate with a reduced risk of HF. Physical activity might affect the progression of HF by reducing the prevalence of HF risk factors, encouraging physiologic cardiac remodeling, and by resulting in improvements in mortality and HF symptoms in those with clinical HF. Modifications in several biological pathways affecting cardiac performance, neurohormonal balance, endothelial function, peripheral muscle composition and lung function may all contribute to the relations of physical activity and exercise with HF prevention. Therefore, we believe that the current evidence supports recommendations for regular exercise and maintaining physical activity in the elderly in order to prevent HF in the general population.
However, several unanswered questions need to be addressed before these observations can be leveraged to determine optimal activity recommendations for individuals at elevated risk for HF. First, what is the optimal exercise program for HF prevention? Studies are needed to compare the cardiovascular responses to different exercise modalities, frequencies, intensities and durations both in older individuals at high risk of HF and in patients with established HF. Second, are the effects of exercise on risk of and clinical outcomes in those with HFPEF versus HFREF the same? Although there is evidence that higher levels of physical activity in the elderly are protective for both HFPEF and HFREF [15], it is not clear how specific exercise programs might modify these risks. Third, can exercise regimens be tailored to different forms of pathologic cardiac remodeling, i.e. those with stage B HF? For example, we might consider that an elderly woman with concentric remodeling may potentially benefit from aerobic exercise, while a young man with a dilated cardiomyopathy might benefit from strength training to restore their pre-morbid mass-to-volume ratios. Fourth, are the effects of physical activity or exercise influenced by age, sex, race or by the presence of comorbidities? Different cardiac remodeling patterns have been described according to these factors, but the effects of physical activity in different groups is not well understood. Fifth, are there intermediate measures of HF risk that we might be able to measure in response to exercise (i.e., valid surrogate outcomes of exercise efficacy)? This area of research is not well developed at this time. However, biochemical or imaging biomarkers of the heart’s response to exercise might be harnessed to refine HF risk and determine the optimal training program.
Key Points.
Physical activity and regular physical exercise are associated with a reduced incidence of heart failure.
In cross-sectional studies, physical activity is associated with specific morphologic changes in cardiac structure.
Reduced cardiac compliance occurs with aging and can be prevented by regular exercise.
Molecular mechanisms involving the performance of the cardiac, vascular, pulmonary, skeletal muscle, renal and autonomic nervous systems may contribute to the benefits of exercise for prevention of heart failure.
Future research is essential to determine how best to use physical activity recommendations and exercise therapy to mitigate heart failure risk.
Acknowledgments
None
Financial support and sponsorship
This work was supported by National Institute of Health T32-HL007604 (MN) and by the National Heart, Lung, and Blood Institute’s Framingham Heart Study contract N01-HC-25195 (RSV).
Footnotes
Conflicts of interest
The authors have no conflicts of interest.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Dunlay SM, Roger VL. Understanding the epidemic of heart failure: past, present, and future. Current heart failure reports. 2014;11:404–415. doi: 10.1007/s11897-014-0220-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luscher TF. Heart failure: the cardiovascular epidemic of the 21st century. Eur Heart J. 2015;36:395–397. doi: 10.1093/eurheartj/ehv004. [DOI] [PubMed] [Google Scholar]
- 4.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960–2984. doi: 10.1016/j.jacc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart FailureA Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2013;62:e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 6.Baggish AL, Wood MJ. Athlete's heart and cardiovascular care of the athlete: scientific and clinical update. Circulation. 2011;123:2723–2735. doi: 10.1161/CIRCULATIONAHA.110.981571. [DOI] [PubMed] [Google Scholar]
- 7.Kannel WB, Sorlie P. Some health benefits of physical activity. The Framingham Study. Arch Intern Med. 1979;139:857–861. [PubMed] [Google Scholar]
- 8.Larson EB, Wang L, Bowen JD, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med. 2006;144:73–81. doi: 10.7326/0003-4819-144-2-200601170-00004. [DOI] [PubMed] [Google Scholar]
- 9.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. Jama. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 10.Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE. The athlete's heart. A meta-analysis of cardiac structure and function. Circulation. 2000;101:336–344. doi: 10.1161/01.cir.101.3.336. [DOI] [PubMed] [Google Scholar]
- 11.Djoussé L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agha G, Loucks EB, Tinker LF, et al. Healthy Lifestyle and Decreasing Risk of Heart Failure in Women. Journal of the American College of Cardiology. 2014;64:1777–1785. doi: 10.1016/j.jacc.2014.07.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.He J, Ogden LG, Bazzano LA, et al. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Archives of Internal Medicine. 2001;161:996–002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 14. Young DR, Reynolds K, Sidell M, et al. Effects of physical activity and sedentary time on the risk of heart failure. Circulation. Heart failure. 2014;7:21–27. doi: 10.1161/CIRCHEARTFAILURE.113.000529. A large cohort study evaluating the associations of both physical activity and sedentary time with incident HF. This study showed that both lesser physical activity and more sedentary time contributed to increased risk of HF.
- 15.Kraigher-Krainer E, Lyass A, Massaro JM, et al. Association of physical activity and heart failure with preserved vs. reduced ejection fraction in the elderly: the Framingham Heart Study. European journal of heart failure. 2013;15:742–746. doi: 10.1093/eurjhf/hft025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu G, Jousilahti P, Antikainen R, et al. Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation. 2010;121:237–244. doi: 10.1161/CIRCULATIONAHA.109.887893. [DOI] [PubMed] [Google Scholar]
- 17.Farrell SW, Finley CE, Radford NB, Haskell WL. Cardiorespiratory fitness, body mass index, and heart failure mortality in men: Cooper Center Longitudinal Study. Circulation. Heart failure. 2013;6:898–905. doi: 10.1161/CIRCHEARTFAILURE.112.000088. [DOI] [PubMed] [Google Scholar]
- 18.Physical activity and cardiovascular health. NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. Jama. 1996;276:241–246. [PubMed] [Google Scholar]
- 19.Turkbey EB, Jorgensen NW, Johnson WC, et al. Physical activity and physiological cardiac remodelling in a community setting: the Multi-Ethnic Study of Atherosclerosis (MESA) Heart. 2010;96:42–48. doi: 10.1136/hrt.2009.178426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Andersson C, Lyass A, Larson MG, et al. Physical activity measured by accelerometry and its associations with cardiac structure and vascular function in young and middle-aged adults. Journal of the American Heart Association. 2015;4 doi: 10.1161/JAHA.114.001528. These investigators used an objective measure of physical activity (accelerometry) over the course of one week, and demonstrated direct associations of greater physical activity with LV mass, left atrial size and an inverse association with vascular stiffness.
- 21. Brinker SK, Pandey A, Ayers CR, et al. Association of cardiorespiratory fitness with left ventricular remodeling and diastolic function: the Cooper Center Longitudinal Study. JACC. Heart failure. 2014;2:238–246. doi: 10.1016/j.jchf.2014.01.004. Cross-sectional report of the association of higher cardiorespiratory fitness with greater physiologic cardiac remodeling in non-athletes.
- 22.Cheng S, Xanthakis V, Sullivan LM, et al. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: longitudinal observations from the Framingham Heart Study. Circulation. 2010;122:570–578. doi: 10.1161/CIRCULATIONAHA.110.937821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Redfield MM, Jacobsen SJ, Borlaug BA, et al. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation. 2005;112:2254–2262. doi: 10.1161/CIRCULATIONAHA.105.541078. [DOI] [PubMed] [Google Scholar]
- 24.Arbab-Zadeh A, Dijk E, Prasad A, et al. Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110:1799–1805. doi: 10.1161/01.CIR.0000142863.71285.74. [DOI] [PubMed] [Google Scholar]
- 25. Bhella PS, Hastings JL, Fujimoto N, et al. Impact of lifelong exercise "dose" on left ventricular compliance and distensibility. J Am Coll Cardiol. 2014;64:1257–1266. doi: 10.1016/j.jacc.2014.03.062. Cross-sectional associations of the “dose” of physical activity achieved and cardiac structure and function in 102 healthy seniors. Committed exercisers and Masters athletes had healthy left ventricular compliance as opposed to the increased ventricular stiffness observed in more sedentary groups.
- 26. Arbab-Zadeh A, Perhonen M, Howden E, et al. Cardiac remodeling in response to 1 year of intensive endurance training. Circulation. 2014;130:2152–2161. doi: 10.1161/CIRCULATIONAHA.114.010775. Comprehensive evaluation of the cardiac adaptations observed in 12 sedentary young adults during training for a marathon. Physiologic remodeling and improved LV diastolic compliance were described after training.
- 27.Fujimoto N, Prasad A, Hastings JL, et al. Cardiovascular effects of 1 year of progressive and vigorous exercise training in previously sedentary individuals older than 65 years of age. Circulation. 2010;122:1797–1805. doi: 10.1161/CIRCULATIONAHA.110.973784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. Jama. 2009;301:1439–1450. doi: 10.1001/jama.2009.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flynn KE, Pina IL, Whellan DJ, et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. Jama. 2009;301:1451–1459. doi: 10.1001/jama.2009.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hambrecht R, Gielen S, Linke A, et al. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure: A randomized trial. Jama. 2000;283:3095–3101. doi: 10.1001/jama.283.23.3095. [DOI] [PubMed] [Google Scholar]
- 31.Haykowsky MJ, Timmons MP, Kruger C, et al. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am J Cardiol. 2013;111:1466–1469. doi: 10.1016/j.amjcard.2013.01.303. [DOI] [PubMed] [Google Scholar]
- 32.Edelmann F, Gelbrich G, Dungen HD, et al. Exercise training improves exercise capacity and diastolic function in patients with heart failure with preserved ejection fraction: results of the Ex-DHF (Exercise training in Diastolic Heart Failure) pilot study. J Am Coll Cardiol. 2011;58:1780–1791. doi: 10.1016/j.jacc.2011.06.054. [DOI] [PubMed] [Google Scholar]
- 33. Pandey A, Parashar A, Kumbhani DJ, et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circulation. Heart failure. 2015;8:33–40. doi: 10.1161/CIRCHEARTFAILURE.114.001615. Meta-analysis of the effects of exercise in 276 patients with HFPEF. Cardiorespiratory fitness and quality of life were improved without statistically significant changes in LV diastolic function or remodeling.
- 34.Gielen S, Schuler G, Adams V. Cardiovascular effects of exercise training: molecular mechanisms. Circulation. 2010;122:1221–1238. doi: 10.1161/CIRCULATIONAHA.110.939959. [DOI] [PubMed] [Google Scholar]
- 35.Levine BD, Zuckerman JH, Pawelczyk JA. Cardiac atrophy after bed-rest deconditioning: a nonneural mechanism for orthostatic intolerance. Circulation. 1997;96:517–525. doi: 10.1161/01.cir.96.2.517. [DOI] [PubMed] [Google Scholar]
- 36.Ellison GM, Waring CD, Vicinanza C, Torella D. Physiological cardiac remodelling in response to endurance exercise training: cellular and molecular mechanisms. Heart. 2012;98:5–10. doi: 10.1136/heartjnl-2011-300639. [DOI] [PubMed] [Google Scholar]
- 37. Wei X, Liu X, Rosenzweig A. What do we know about the cardiac benefits of exercise? Trends in cardiovascular medicine. 2014 doi: 10.1016/j.tcm.2014.12.014. An excellent review of molecular mechanisms underlying improved cardiac function with exercise, with a particular focus on cardiomyocyte proliferation.
- 38.Siu PM, Bryner RW, Martyn JK, Alway SE. Apoptotic adaptations from exercise training in skeletal and cardiac muscles. FASEB J. 2004;18:1150–1152. doi: 10.1096/fj.03-1291fje. [DOI] [PubMed] [Google Scholar]
- 39.Bostrom P, Mann N, Wu J, et al. C/EBPbeta controls exercise-induced cardiac growth and protects against pathological cardiac remodeling. Cell. 2010;143:1072–1083. doi: 10.1016/j.cell.2010.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miyachi M, Yazawa H, Furukawa M, et al. Exercise training alters left ventricular geometry and attenuates heart failure in dahl salt-sensitive hypertensive rats. Hypertension. 2009;53:701–707. doi: 10.1161/HYPERTENSIONAHA.108.127290. [DOI] [PubMed] [Google Scholar]
- 41.Sarma S, Carrick-Ranson G, Fujimoto N, et al. Effects of age and aerobic fitness on myocardial lipid content. Circulation. Cardiovascular imaging. 2013;6:1048–1055. doi: 10.1161/CIRCIMAGING.113.000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hidalgo C, Saripalli C, Granzier HL. Effect of exercise training on post-translational and post-transcriptional regulation of titin stiffness in striated muscle of wild type and IG KO mice. Archives of biochemistry and biophysics. 2014;552–553:100–107. doi: 10.1016/j.abb.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 43.Coats AJ, Adamopoulos S, Radaelli A, et al. Controlled trial of physical training in chronic heart failure. Exercise performance, hemodynamics, ventilation, and autonomic function. Circulation. 1992;85:2119–2131. doi: 10.1161/01.cir.85.6.2119. [DOI] [PubMed] [Google Scholar]
- 44.Xu X, Wan W, Powers AS, et al. Effects of exercise training on cardiac function and myocardial remodeling in post myocardial infarction rats. Journal of molecular and cellular cardiology. 2008;44:114–122. doi: 10.1016/j.yjmcc.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ho JE, Larson MG, Ghorbani A, et al. Long-term cardiovascular risks associated with an elevated heart rate: the Framingham Heart Study. Journal of the American Heart Association. 2014;3:e000668. doi: 10.1161/JAHA.113.000668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dhakal BP, Malhotra R, Murphy RM, et al. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: the role of abnormal peripheral oxygen extraction. Circulation. Heart failure. 2015;8:286–294. doi: 10.1161/CIRCHEARTFAILURE.114.001825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ventura-Clapier R. Exercise training, energy metabolism, and heart failure. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2009;34:336–339. doi: 10.1139/h09-013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Al Dandachi G, Londner C, Caumont-Prim A, et al. Ageing and endurance training effects on quantity and quality of pulmonary vascular bed in healthy men. Respiratory research. 2014;15:8. doi: 10.1186/1465-9921-15-8. Demonstration of cross-sectional associations between endurance sport participation and higher pulmonary vascular compliance.
- 49.Hawkins MS, Sevick MA, Richardson CR, et al. Association between physical activity and kidney function: National Health and Nutrition Examination Survey. Medicine and science in sports and exercise. 2011;43:1457–1464. doi: 10.1249/MSS.0b013e31820c0130. [DOI] [PubMed] [Google Scholar]
- 50.Kokkinos P, Faselis C, Myers J, et al. Exercise Capacity and Risk of Chronic Kidney Disease in US Veterans: A Cohort Study. Mayo Clinic proceedings. 2015 doi: 10.1016/j.mayocp.2015.01.013. [DOI] [PubMed] [Google Scholar]