Abstract
Deaf individuals have more cardiovascular risks than the general population that are believed to be related to their cardiovascular health knowledge disparities. This phenomenological study describes where 20 deaf sign language-using adolescents from Rochester, New York, many who possess many positive characteristics to support their health literacy, learn cardiovascular health information and their lived experiences accessing health information. The goal is to ultimately use this information to improve the delivery of cardiovascular health education to this population and other deaf adolescents at a higher risk for weak health literacy. Deaf bilingual researchers interviewed deaf adolescents, transcribed and coded the data, and described the findings. Five major sources of cardiovascular health information were identified including family, health education teachers, healthcare providers, printed materials, and informal sources. Despite possessing advantageous characteristics contributing to stronger health literacy, study participants described significant challenges with accessing health information from each source. They also demonstrated inconsistencies in their cardiovascular health knowledge, especially regarding heart attack, stroke, and cholesterol. These findings suggest a great need for additional public funding to research deaf adolescents’ informal health-related learning, develop accessible and culturally appropriate health surveys and health education programming, improve interpreter education, and disseminate information through social media.
Recent surveys of sign language-using deaf people’s health indicate that they experience more cardiovascular risks than hearing people (Barnett et al., 2011; Emond et al., 2015). Recent studies have also found that sign language-using deaf adults have inconsistent and weaker cardiovascular health knowledge (e.g., early heart attack and stroke symptoms) as compared to the general hearing population (Margellos-Anast, Estarziau, & Kaufman, 2006; McKee et al., 2011). Deaf people’s increased cardiovascular risks might be related to their cardiovascular health knowledge and literacy disparities (Margellos-Anast et al., 2006; McKee et al., 2011). This postulation is based on previously documented strong relationships between poor health literacy and poor health outcomes in the hearing populations (e.g., Baker, Parker, Williams, & Clark, 1998; Baker et al., 2007; Dewalt, Berkman, Sheridan, Lohr, & Pignone, 2004).
A study of elderly people in Iceland who had hearing problems found that these people experienced significantly worse cardiovascular disease mortality than those who did not have hearing problems (Fisher et al., 2014). To date, there is no documentation on the prevalence of cardiovascular disease outcomes (e.g., mortality, myocardial infarctions, strokes, congestive heart failure) in deaf people who use American Sign Language (ASL) in the United States. The lack of such “hard” cardiovascular disease outcomes in this population might be a result of larger and nationwide health surveys not accurately identifying subpopulations of, not being accessible to, or not recruiting a sufficient number of deaf people who use sign language (Barnett & Franks, 1999). Data about cardiovascular health literacy in hearing (non-deaf) people indicate that most hearing people have good knowledge of cardiovascular risk factors (e.g., hypertension, smoking, cholesterol, and physical activity) and health benefits of physical activity, but their knowledge does not always translate into healthier behaviors (Frost, 1992; Morrow, Krzewinski-Malone, Jackson, Bungum, & Fitzgerald, 2004). Several studies of large numbers of hearing people generally indicate that most of them are able to identify at least one heart attack and stroke symptom (Greenlund et al., 2004; Mata, Frank, & Gigerenzer, 2014) with most being able to identify four to six stroke warning symptoms (Lundelin et al., 2012). However, knowledge of stroke symptoms did not always translate into appropriate behaviors such as calling 911 when experiencing or witnessing stroke symptoms (Lecouturier et al., 2010). Hearing people also appear to have good knowledge about hypertension (Roccella, Bowler, Ames, & Horan, 1986) and cholesterol (Rasinger, Flores, Pakesch, & Sinzinger, 1989).
Similar findings have been found in hearing adolescents (Smalley, Wittler, & Oliverson, 2004) although one study did find that hearing adolescents had some gaps in their knowledge about nutrition (Bogdańska, Maniecka-Bryła, & Szpak, 2005). Furthermore, in another study of 873 high school students in Michigan, hearing adolescents lacked knowledge about cardiovascular disease as the greatest lifetime risk, placing it behind accidents and cancer, and they did not view themselves as being at risk for cardiovascular disease. They described cardiovascular disease as being more of a risk for men than for women and 40% of these respondents chose substance abuse, other than cigarettes, as the most important cardiovascular disease risk behavior (Vanhecke, Miller, Franklin, Weber, & McCullough, 2006).
Deaf people’s health literacy appear to share many of the same weaknesses (Pollard & Barnett, 2009) as those evident in subgroups of hearing people who might have difficulty accessing health information including those who have lower educational levels (Greenlund et al., 2004; Lundelin et al., 2012; Potvin, Richard, & Edwards, 2000), are immigrants (Chow, Chu, Tu, & Moe, 2008), have lower levels of social support (Steptoe & Wardle, 2001), and do not speak English at home (Gans, Assmann, Sallar, & Lasater, 1999; Nguyen et al., 2009). Deaf people also appear to share similar health literacy weaknesses with hearing people who have different racial/ethnicity (Dark & Ezenkwele, 2007; Winham & Jones, 2011) and cultural backgrounds (Chin et al., 2013; Nguyen et al., 2009; Sedibe et al., 2014; Sin, Fitzpatrick, & Lee, 2010). Factors contributing to deaf people’s health literacy weaknesses include inability to overhear health information, difficulty in understanding written health information (Jones, Renger, & Firestone, 2005), and communication barriers with their healthcare providers (Zazove et al., 1993).
In one study, deaf adults selected cardiovascular health education as their highest priority for health education topics (Jones et al., 2005). In response to this request made by deaf adults, we sought to learn how deaf adolescents access cardiovascular health information and develop health literacy skills. This information can then be used to fill the gap in developing effective health educational interventions to improve deaf people’s cardiovascular health knowledge and literacy skills. We chose to focus on deaf adolescents rather than deaf adults because adolescence is a critical developmental period when health education interventions have the potential to yield significant life-long benefits (e.g., Manganello, 2008).
The Nutbeam (2000) health literacy model was used to formulate a set of semistructured interview questions about deaf adolescents’ health literacy. This is one of the most widely accepted models of health literacy that is often used in studies of heath communication (see Nutbeam, 2008 for review). This model includes three sequential levels of health literacy: (a) functional health literacy, (b) interactive health literacy, and (c) critical health literacy. Manganello’s (2008) adolescent health literacy framework was also used to explore deaf adolescents’ sources of cardiovascular health information and their lived experiences with accessing these sources of information. This framework was constructed specifically for adolescents and is based on definitions, constructs, and concepts of health literacy as developed in the most recent report from the Institute of Medicine’s Committee on Health Literacy: Health Literacy: A Prescription to End Confusion (Nielsen-Bohlman, Pranzer, & Kindig, 2004). This robust, systematic model of health literacy encompasses family, educational, and health systems and enabled the researchers to set a priori codes related to adolescents’ health literacy. The use of both the Nutbeam model and Manganello framework allowed the researchers to explore widely for factors contributing to deaf adolescents’ health literacy development.
The present study used a phenomenological approach where 20 deaf participants report common lived experiences of a phenomenon including what they experienced and how they experienced it (e.g., Creswell, 1998). This approach enabled the researchers to describe deaf adolescents’ self-reported experiences on learning and understanding cardiovascular health information. Also, within this approach, the researcher is not a detached or impartial observer—as it is claimed not possible to begin without presumptions or biases—instead the researcher is another interested subjective participant in the process. This requires the research team to make clear the experiences they bring into the study as well as the interpretations and meanings that have been placed on findings (e.g., Plummer, 1983; Stanley & Wise, 1993). In this study, all of the authors are deaf themselves: one is a developmental pediatrician, one is a developmental psychologist, and one is a neuropsychologist. We navigated the data with our in-group knowledge of the deaf experience and describe our observations of the findings in the Discussion section.
Method
Participants
Purposive sampling was used to ensure that the participating deaf adolescents were from different educational settings. The 20 participants were recruited from one school for the deaf and one public school serving mainstreamed deaf students in Rochester, New York. We did not assess participants’ hearing status, but all participants responded to recruitment materials specifically requesting sign language-using deaf high school students and all participants understood and used sign language fluently in interviews. Participants ranged from 14 to 19 years old and were in grades 9–12 (see Table 1 for demographic information). Almost half of the participants (n = 9) were female and one-fourth of the participants (n = 5) were of a non-White racial and/or ethnic background. Slightly more than half (n = 11) had deaf parents and the majority (n = 17) reported that their parents use sign language. Eighteen out of 20 participants described good communication with their parents. Three-fourths (n = 15) of the participants rated themselves as having good English reading skills.
Table 1.
Participants’ background characteristics
| ID | Gender | Race/ ethnicity | Age | Grade | School | Parents’ hearing status | Parents’ communication method | Quality of communication with parents | Self-reported English reading skills |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | White | 16 | 9th | Deaf school | Both hearing | Sign language | Good | Good |
| 2 | Female | Non-White | 17 | 11th | Deaf school | Both hearing | Spoken language | Poor | Poor |
| 3 | Female | White | 17 | 11th | Deaf school | Mother deaf, father hearing | Both sign and spoken language | Good | Good |
| 4 | Male | White | 16 | 11th | Deaf school | Both deaf | Sign language | Good | Good |
| 5 | Male | White | 16 | 10th | Deaf school | Both deaf | Sign language | Good | Good |
| 6 | Male | White | 16 | 11th | Deaf school | Both deaf | Sign language | Good | Good |
| 7 | Male | White | 18 | 12th | Deaf school | Both hearing | Sign language | Good | Poor |
| 8 | Male | Non-White | 18 | 11th | Deaf school | Both hearing | Spoken language | Good | Good |
| 9 | Male | White | 18 | 12th | Deaf school | Both deaf | Sign language | Good | Good |
| 10 | Female | White | 18 | 12th | Deaf school | Both hearing | Sign language | Good | Good |
| 11 | Male | Non-White | 18 | 12th | Deaf school | Both hearing | Spoken language | Poor | Poor |
| 12 | Male | Non-White | 18 | 12th | Deaf school | Both hearing | Both sign and spoken language | Good | Good |
| 13 | Male | White | 16 | 9th | Deaf school | Both deaf | Sign language | Good | Poor |
| 14 | Female | White | 18 | 12th | Deaf school | Both deaf | Sign language | Good | Good |
| 15 | Female | White | 16 | 11th | Deaf school | Both hearing | Sign language | Good | Good |
| 16 | Male | White | 15 | 10th | Deaf school | Both deaf | Sign language | Good | Poor |
| 17 | Female | White | 16 | 10th | Deaf school | Both deaf | Sign language | Good | Good |
| 18 | Female | White | 19 | 12th | Mainstream school | Both deaf | Sign language | Good | Good |
| 19 | Female | Non-White | 17 | 11th | Mainstream school | Mother deaf, father hearing | Sign language | Good | Good |
| 20 | Male | White | 14 | 9th | Mainstream school | Both hearing | Both sign and spoken language | Good | Good |
Procedures
The University of Rochester Institutional Review Board approved all research procedures. Semistructured interview questions were formulated using Nutbeam’s (2000) health literacy model as mentioned earlier and additional questions were developed to explore the participants’ knowledge about cardiovascular topics including heart attack, stroke, obesity, hypertension, diabetes, and cholesterol with a focus on the causes, mechanisms, prevention, and consequences of these health issues (see Figure 1 for interview questions). Participants who responded to the study’s recruitment advertisements, distributed through each school, were included in this study. The participants were informed of the purpose, data collection methods, privacy protection methods, and the right to withdraw from the interview at any time. All parents provided consent for students who were under 18 years old to participate in this study and all students provided assent. Two students who were 18 years old or older provided informed consent on their own.
Figure 1.
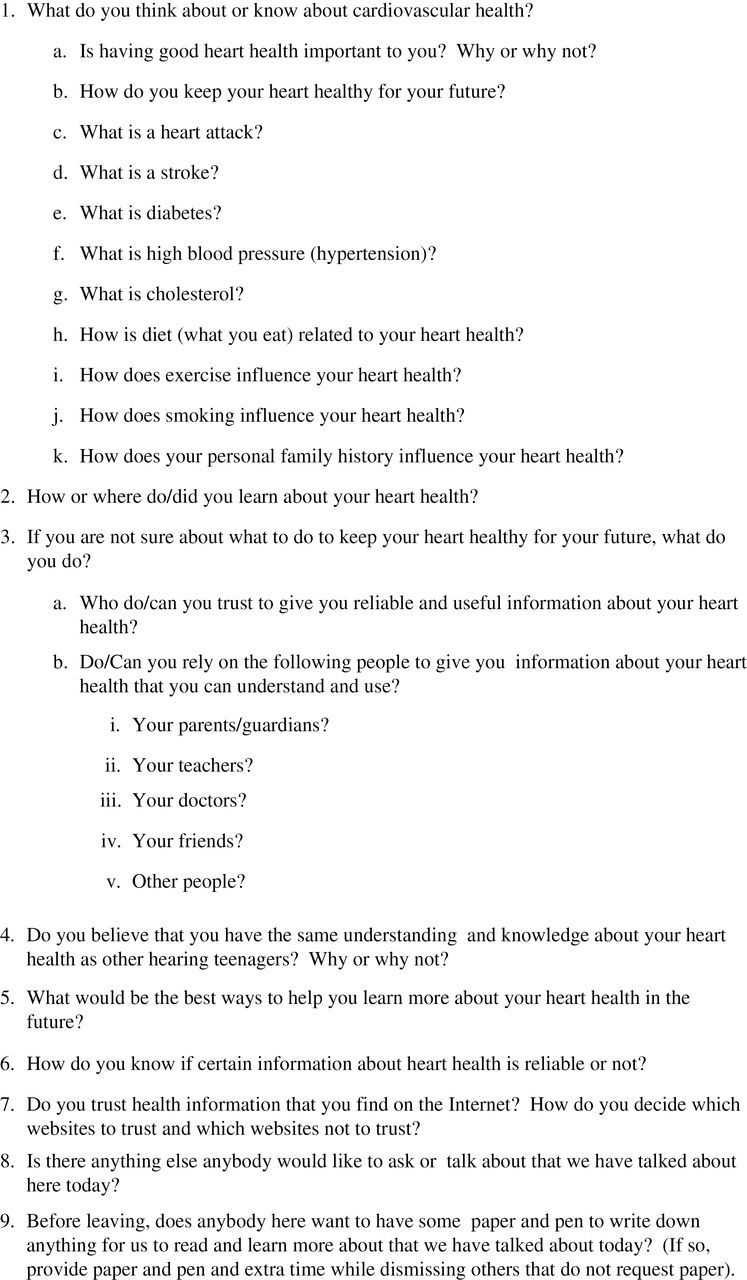
Semistructured interview questions based on the Nutbeam (2000) Health Literacy Model.
The size of the focus groups was limited to six adolescents to allow for optimal interaction and participation. Three participants were interviewed individually because they preferred not to be in a focus group. A background questionnaire asking demographic information including their parents’ hearing status, whether their parents use sign language, and the quality of their communication with their parents was given to all participants. Participants were also asked to self-rate their English reading skills. All focus groups and individual interviews were then conducted in ASL by two ASL-fluent deaf interviewers and video-recorded. Each deaf adolescent was compensated for his/her time with a ten-dollar superstore gift card. A deaf researcher fluent in both ASL and English translated and transcribed the video recordings into written English and all of the transcriptions were checked for accuracy by a second deaf bilingual researcher. A team of three deaf researchers coded and organized themes related to deaf adolescents’ knowledge of and sources of cardiovascular health information. Manganello’s (2008) framework was used to set a priori codes related to family, educational, and health systems influences on health literacy. The team also coded cardiovascular health knowledge topics that the participants appeared to find difficult or unfamiliar.
Findings
The participants were asked about cardiovascular risks and their responses varied widely. Participants generally understood the benefits of a healthy diet and regular exercise, the wisdom of avoiding cigarette smoking, and some basic cardiovascular disease symptoms. However, most of these adolescents exhibited some inconsistencies in other areas of cardiovascular health knowledge including heart attack, stroke, and cholesterol (see Table 2 for sample quotes). Many were unable to explain the causes or what happens in a heart attack and a stroke, and only a very few were able to accurately describe cholesterol. For example, one participant (#19) described cholesterol as an artificial flavor that is added to food and another participant (#20) explained that cholesterol actually makes the heart healthier and pump better.
Table 2.
Sample quotes regarding cardiovascular health knowledge
| Knowledge about heart attack |
| Participant 1: “I have heard about it before, but I don’t know exactly what it means” |
| Participants 4: “I don’t know.” |
| Participant 6: “I don’t know.” |
| Participant 11: “A heart attack means if you use drugs, smoke cigarettes, or drink beer or wine. Don’t use drugs. You have to keep your heart safe.” |
| Participant 14: “Most of the time, it happens to older people. Sometimes it happens to younger people, I do not know.” |
| Participant 17: “There’s something inside the respiratory system that swells up and causes a heart attack. I do not know.” |
| Participant 18: “I really do not know (why the heart stops working in a heart attack?).” |
| Participant 19: “Sometimes if you eat too much candy…maybe, I am not sure, but I think you have blood clots in various places and if that happens, your heart does not work as good as it is supposed to and you have a heart attack.” |
| Participant 20: “It means something’s stuck and closes up the vessel and the heart cannot beat.” |
| Knowledge about stroke |
| Participant 3: “It means that something happens in the body that sends a message to the brain.” |
| Participant 14: “It is when you become paralyzed and cannot move. It can happen if you smoke a lot. My friend told me that is what happened to her husband. I feel bad about that. That’s what I know about a stroke.” |
| Participant 18: “I have no idea [about what causes stroke].” |
| Participant 20: “It [stroke] means that the body cannot feel the arm. It cannot function mechanically. It hits you almost like…You have a problem like diabetes.” |
| Knowledge about cholesterol |
| Participant 1: “I don’t remember.” |
| Participant 2: “I don’t know.” |
| Participant 3: “Every food has it. I’m not sure what it means.” |
| Participant 5: “I just learned about it in science. It’s related to the cells, but I have not learned enough.” |
| Participant 14: “No, that word sounds familiar.” |
| Participant 14: “It [cholesterol] is a little bad.” |
| Participant 15: “I forgot.” |
| Participant 18: “I am not sure. I have never heard of that word before.” |
| Participant 17: “It has something to do with too much salt. You see ‘cholesterol’ on food packages, but I forgot what it is.” |
| Participant 19: “Cholesterol is…I am not sure, but I am guessing…it is when you have extra flavor, like when you have fake flavor added…I am not sure.” |
| Participant 20: “It [cholesterol] makes the heart healthier and pump well. Hmm. Cholesterol is more like, it helps circulation in the heart, I guess.” |
Five common sources of cardiovascular health information were identified: (a) family, (b) health education teachers, (c) healthcare providers, (d) printed health information, and (e) informal learning (see Table 3 for sample quotes). Although the purpose of the study was to describe where they learn information, there were themes from all participants about difficulties accessing information (see Table 4 for sample quotes). The following subsections, beginning with the most frequently mentioned source, describe the participants’ perceptions of their learning of relevant health information and their challenges. The authors clarified emic (in-group) concepts unique to the deaf community in this section and the authors’ interpretations of these themes are then described in the Discussion section.
Table 3.
Sample of quotes regarding sources of health information
| Parents and family |
| Participant 1: “My parents, especially. Because they are both doctors, so they tell me these things.” |
| Participant 5: “My parents and health class last year.” |
| Participant 19: “My mother and father and my family.” |
| Health education teachers |
| Participant 2: “Health class.” “Nothing [from anybody else].” |
| Participant 3: “My doctor. I learn information from here [school] and from my cardiologist.” |
| Participant 7: “The health class teacher, who also teaches gym class.” |
| Participant 11: “Teachers. The gym class teacher. “ |
| Participant 17: “A teacher. Teachers are older than me. Most older people tend to know about health.” |
| Participant 19: “Mostly health class…” |
| Healthcare providers |
| Participant 3: “My doctor. I learn information from here [school] and from my cardiologist.” |
| Participant 16: “I would ask a doctor. I would ask them [my parents], but if I do not understand, I would ask the doctor.” |
| Participant 20: “I would ask a doctor or a personal trainer.” |
| Printed health information |
| Participant 15: “I would check on the Internet. If I did not understand it, I would ask a friend who is good with reading.” |
| Participant 19: “...if there is some topic that I am interested in,…I can go on the Internet.” |
| Informal learning |
| Participant 9: “My immediate family [when asked about knowledge of family medical history], yes, maybe….yes, I know about my larger family medical history, but not in depth or too much about the past.” |
| Participant 10: “I do not have it [diabetes], but some people in my family do. I have seen some of them do a test to check their blood by pricking their finger...like if you have a high level of sugar, that can lead to a heart attack or death or something like that. So you have to check. I am very fuzzy on that.” |
| Participant 12: “I was eating with my family and I was 6 years old and someone had a heart attack and fell over.” |
| Participant 13: “Hearing people can hear things [reason why deaf people might know less health information than hearing people].” |
Table 4.
Sample quotes regarding accessing sources of health information
| Parents and family |
| General cardiovascular health information |
| Participant 1: “My parents, especially, because they are both doctors, so they tell me these things.” |
| Participant 8: “My parents tell me what is not good for me, like red meats because the fats and oils are not good for your heart...they [my parents in the Philippines] did not teach me, my host parents [in America] did...they [Filipino family] did not tell me [what causes a stroke].” |
| Participant 9: “Most of the time, my mother and father talk about it to me and inform me…Yes, of course [my parents use sign language], my entire family is deaf...we happened to have a discussion at dinner about the heart when my parents let me know that if I saw them experiencing pain in the left arm to call 911. They just let me know so I would be prepared.” |
| Participant 11: “They [my parents] do not us sign language so I do not understand and we do not have good communication…It is better here [at school] where I can understand.” |
| Participant 12: “Sometimes they [my parents] know. Sometimes they do not know.” |
| Family medical history |
| Participant 1: “I know a few things. I only know some information. I don’t know my older family medical history. I only know a few. My grandmother had cancer. I know that. My grandfather had a heart attack. I just know about those two…My father let me know. My mother does not tell me anything.” |
| Participant 2: “I don’t think so [could you report your family medical history to your doctor?]…it is kept quiet.” |
| Participant 5: “When I go to the doctor, the doctor tends to give my mother a paper that she fills out about our family medical history.” |
| Participant 7: “Yes [I have good communication with my family], they keep me aware of what’s happening in the family.” |
| Participant 9: “My immediate family, yes, maybe...yes, I know about my extended family medical history, but not in depth or too much about the past.” |
| Participant 14: “I do not know everything because they [my family] did not tell me. They tell me most things, but it is not much.” |
| Participant 15: “I just know about one person. I do not know [about the rest of my family medical history].” |
| Participant 17: “No. I only know a few things. I do not know much about it [my family medical history].” |
| Participant 18: “I would tell the doctor to ask my parents. I would say that I honestly do not know [about my family medical history].” |
| Health education teachers |
| Participant 15: “It was just basic information…I do not know if it will help me.” |
| Participant 17: “It [health class] has more to do with HIV/AIDS and that sort of thing. It’s not so much to do with health [they did not discuss heart attacks or stroke]. It did not make an impact on me. The school could have a class to teach us more detailed information.” |
| Participant 18: “It was basic. They did not really explain about the heart, what happens inside, or the different vocabulary. It was just the basics of how it works.” |
| Participant 19: “It’s mostly basic.” |
| Healthcare providers |
| Parents and family |
| Participant 1: “Somewhat. See my doctor is hearing and my mom usually interprets…Dad doesn’t interpret because he wants to give me privacy when it comes to talking about girl things. So we have been writing back and forth, but there are some words I cannot spell or some big words I do not understand. I prefer to have my mother interpret, but we have had some schedule conflicts.” |
| Participant 2: “I just stay quiet…It’s always my mother who talks with the doctor. I just sit there and watch them and stay quiet.” |
| Participant 5: “Sometimes, my mother will sit with the doctor so if I don’t understand him, she will interpret for me.” |
| Participant 7: “My doctor is good and smart, but his signing is so-so. I have my mother to interpret.” |
| Participant 8: “My doctor communicates to my grandmother or my aunt who communicates to me. Then I speak to my doctor. Nobody signs. |
| Participant 15: “My mother is hearing so she interprets for me. (Does she interpret everything?) No, not everything.” |
| Participant 17: “It depends. Sometimes I want to go by myself and will write back and forth. Sometimes I’ll tell my parents to call and get an interpreter. It depends on what is going on and what I think I need.” |
| Professional interpreters |
| Participant 1: “You have to ask in advance [to use professional interpreters with doctors].” |
| Participant 11: “I can talk, I am hard-of-hearing. Sometimes if we struggle, I may have an interpreter. There’s a balance…. Sometimes I do not feel like I get enough information from my doctor. I’m told that I seem to be healthy and doing fine. That’s not enough information” |
| Participant 18: “It depends. Some interpreters are really lousy and some are just okay. Some are really good.” |
| Printed communication |
| Participant 13: “Sometimes, I go by myself, sometimes with my parents, and sometimes with an interpreter. I went to the doctor recently, like two months ago, and now the doctor uses an iPad to communicate with my mother or with me.” |
| Participant 14: “A little bit, we write back and forth. Most of the time, my mother writes because I do not know the words the doctor uses. It is hard.” |
| Participant 18: “Well, if it’s on paper, some words are hard to explain. I will not know how to spell something or the doctor will misunderstand something.” |
| Participant 20: “Sometimes the doctor misses something [while writing back and forth], and I will point that out. The doctor will give me more answers then.” |
| Lack of sign language-fluent and deaf culture-competent providers |
| Participant 1: “I wouldn’t mind having a deaf doctor. Communication would be much more clear.” |
| Participant 3: “Doctors need to give respect to deaf people.” |
| Participant 13: “Getting information directly is better. It is ok if the hearing person is truly fluent in sign language and knows deaf culture…but not if it is just a hearing person [who does not know sign language].” |
| Participant 17: “I would prefer a deaf person signing over an interpreter.” |
| Printed health information |
| Participant 1: “I wish TV was in sign language instead of captioned because I don’t understand some words and that confuses me...It would be better to use an interpreter.” |
| Participant 5: “If there are some big words, I will not understand that, but I understand most of it.” |
| Participant 13: “No, I am not good at reading (can you understand health information you read?).” |
| Participant 14: “Sometimes I will understand it [printed health information] if it is easy, but most of the time I do not understand it.” |
| Participant 16: “Somewhat, I do not know (can you understand health information you read?).” |
| Informal learning |
| Participant 1: “I think it is not fair because hearing people are talking around us and some deaf people need to know what is going on. They may let it slide and say nothing...I wish the whole world knew sign language, but some people don’t want to bother with deaf people…” |
| Participant 3: “…deaf people miss out on a lot of information around them in the world…and sometimes they do not go on the computer a lot because they have not even learned that word yet so they don’t think about it.” |
| Participant 20: “Hearing people hear all this information about the heart. Deaf people get the information little by little. It takes a while to learn all of it. It is faster for hearing people.” |
Family
As with the general population (see Manganello, 2008), deaf adolescents’ families served as major sources of deaf adolescents’ general information about cardiovascular health. Family was the most common source identified by these participants although there was a great variation among participants as to how much information they had access to at home. Although the majority of the sample reported being able to understand their parents, participants who used sign language with their parents mentioned learning more about cardiovascular health from their families more than those who did not use sign language with their parents. Within the group of adolescents with parents fluent in ASL, exposure to cardiovascular health information was higher among those who have family members who took the initiative to share this information with them. Regardless of communication modality, many deaf adolescents described experiences where their parents would fill out a medical background form or answer verbal questions asking about their family medical history without sharing this information with them.
A striking theme, which emerged across the focus groups and interviews, was that many of these deaf adolescents did not appear to be aware of their family medical history. This appeared to be especially true for those from families not fluent in ASL. These adolescents were not able to overhear family conversations about relatives’ health or parents’ conversations with healthcare providers even when these adolescents were present (see Health Care Providers subsection).
Health Education Teachers
The second most frequent source of cardiovascular health information mentioned by the participants was learning from their health education teachers in health education classes at school. This trend was more apparent among those with parents not fluent in ASL as they appeared to seek health information from health education teachers, who are able to communicate with them, rather than their parents. However, several deaf adolescents reported that their classes provided health information that was too basic to have a meaningful impact on them. When the participants were asked about whether or not they learned their family medical history through school activities, none of the participants described any efforts by their health education teachers to improve their knowledge of their own family medical history.
Healthcare Providers
Since the city of Rochester in New York has healthcare providers who are deaf themselves and other healthcare providers who are fluent in ASL, some participants reported that they did not have difficulty communicating with their healthcare providers. These participants trusted their healthcare providers and learned health information from them. However, other participants reported significant barriers in their ability to communicate and interact with their healthcare providers. These participants explained that because they could not communicate with their healthcare provider, their parents and other family members would communicate with the provider for them. Of those who reported that their family members interpret for them, these participants described often being involved in only a part of the conversation or given a general summary of the parent’s dialogue with healthcare providers without much detail. According to these participants, their family members often answer questions from providers about their health and health history without interpreting the entire conversation. These participants reported not actively participating in conversations with their healthcare provider to learn about themselves and general health information.
Some participants used ASL interpreters when interacting with their healthcare providers. Some mentioned the challenge of having to schedule ASL interpreters ahead of time, which makes it difficult for them to obtain urgent care. As a result, their family members tended to communicate with healthcare providers for them. Nevertheless, some of the deaf adolescents did not always report having a positive experience when provided ASL interpreters. These participants explained that the quality of interpreters varied widely and some of their negative experiences caused them to choose not to have an interpreter present, preferring to interact with their healthcare providers through writing or typing back and forth. Yet, some of these participants experienced healthcare providers who were not willing to take the time to communicate in this method. Of those who have communicated with their providers in writing, some admitted that they do not always understand everything that is written down. Several deaf adolescents explained that they would be able to understand and learn more health information if they were able to directly interact with healthcare providers who are knowledgeable about Deaf culture and are able to use sign language with them.
Printed Health Information
The deaf adolescents with stronger self-reported reading skills relied on printed materials to supplement their cardiovascular health knowledge. They used the Internet and other written materials to read and learn about health information that interests them. Even with their stronger English literacy skills, many reported being overwhelmed by unfamiliar health terminology, which prevented them from understanding more complicated health issues. Many of these deaf adolescents reported that they would prefer to have the health information presented more visually, such as in ASL and with more pictures, models, and other visual descriptions. Overall, participants did not appear satisfied with the amount of accessible printed or digital media available to them about health information.
Informal Learning
Although many participants mentioned informal learning as another major source of health information, their ability to access this source depended on how well they were able to overhear and oversee conversations between other people. Informal learning was identified as being beneficial through both proximal and observational learning when deaf adolescents are exposed to health issues within their physical environments such as witnessing someone having a heart attack or watching a family member checking their finger-stick blood sugar level. Some of the participants with ASL-fluent parents mentioned learning about health information informally when they are able to oversee family conversations about health. However, even among those who reported good communication with their parents, some deaf adolescents described difficulties with accessing health information at home because they had trouble following family conversations that incorporate spoken language. Informal learning outside of the family was also reported to be limited. This included when family members (including siblings and relatives), educators, and other hearing people communicated with each other such as at the doctor’s office
Discussion
The deaf adolescents who participated in this study exhibited some inconsistent knowledge of cardiovascular health and risks as found in studies of deaf adults (Margellos-Anast et al., 2006; McKee et al., 2011). Our sample is unique, but representative of the Rochester deaf community with a majority of the participants having deaf parents, reporting that their parents use sign language, describing good communication with their parents, and self-rating themselves as having good English reading skills. As a result, this study might be considered as an investigation of a “privileged” or “cream-of-the crop” group of sign language-using deaf adolescents, and its findings, therefore, are limited in generalizing to a larger, more typical deaf population. However, it might also be true then that the results of significant health literacy weaknesses or challenges would likely to be worse and more alarming in other sign language-using deaf adolescents. The use of key informant interviews with three deaf adolescents yielded greater number of specific information and personal examples because each individual participant was asked to answer all questions directly in contrast to more general information that was shared in focus groups when the questions were posed to them as a group. However, the type of the interview did not produce any essential differences in the content of the information shared and emerging themes.
When generally compared to the cardiovascular health knowledge of “privileged” hearing adolescents, these “privileged” sign language-using deaf adolescents appear to have significantly weaker knowledge, especially about heart attack, stroke, and cholesterol. Unfortunately, this implies that many other sign language-using deaf adolescents are likely to have similar or even weaker cardiovascular health knowledge. Additional study is needed to assess cardiovascular health knowledge and literacy in deaf adolescents who primarily use spoken English.
The Manganello (2008) health literacy framework utilized in this phenomenological study made it possible to identify five common sources where deaf adolescents learn cardiovascular health information: family, health education teachers, healthcare providers, printed health information, and informal learning. Each of these sources provided cardiovascular health information, but participants in our study reported challenges accessing information from all of these sources. In studies of hearing people, most named healthcare providers as their desired source of further health information (Frost, 1992) and mass media was cited as their main source of cardiovascular disease information (Piwoński, Rywik, & Wp4f1wska, 1986).
Families were identified as the most common source of cardiovascular health information. Deaf adolescents’ reliance on their parents and other family members as a robust source of cardiovascular health information depends on their ability to effectively communicate with each other. In this study, deaf adolescents who learn such information from their families typically come from homes of parents who are fluent in ASL and those who took initiative to share health information with their children. The benefits of positive parental modeling and involvement in their children’s health are life-long and parents can be effective teachers of health habits at home when prompted by health educators (Norton, Froelicher, Waters, & Carrieri-Kohlman, 2003).
One major issue, perhaps the greatest issue, is these deaf adolescents’ access to their family medical history—most participants were unsure of their family cardiovascular health history. Family medical history is one of the strongest influences on the risk of developing heart disease and stroke and knowing one’s family medical history can help to reduce the risk of developing health problems. Such knowledge is important to help one gain from lifestyle changes and screening tests. During appointments with healthcare providers, the first step in the process is often learning the patient’s family medical history to determine the type of tests that might need to be ordered. Healthcare providers rely on this information to make an appropriate diagnosis and determine the best treatment. Without this, healthcare providers then have to explore more broadly (more time-consuming and expensive) risking possible misdiagnosis and maltreatment.
Many family members of deaf adolescents, regardless of ASL fluency, might not realize that they need to explicitly communicate information about their family medical history to their deaf children. At the same time, the lack of prior cardiovascular health knowledge can also make it difficult for these adolescents to comprehend family health information that is presented to them. Increasing deaf adolescents’ access to and understanding of their own family medical history must be a priority in order to promote long-standing preventive health practices that could significantly reduce health-related cost burden on our society.
Clearly, the health education programs through schools are making efforts toward supporting deaf adolescents’ cardiovascular health knowledge, which can be quite effective if the students are able to directly communicate with and understand their health education teachers. Some deaf adolescents could also benefit from supplemental health education to provide them with more impactful and meaningful health information. If not already done, we recommend that health education curriculum for deaf students include assignments or activities that encourage these students to explore their family medical history with their families.
Deaf adolescents’ communication with their healthcare providers also can be a problem. Family members often accompany deaf adolescents to medical appointments and might serve as the family medical historian without signing or looking at their deaf child. If they are able to interpret and choose to interpret, they might only interpret or summarize a part of the dialogue with providers. The loss of access to such dialogue reflects a missed informal learning opportunity that is typically available to hearing children. Not only do they lose an opportunity to learn more about their own health and their family medical history, but deaf adolescents also lose an opportunity to participate in a dialogue with their healthcare provider. Such dialogue is needed to learn cardiovascular health information and other health information as well as how the health system operates. Increasing the number of qualified professional medical interpreters and educating more families and professionals about the appropriate roles of family members and professional interpreters could help provide deaf adolescents with greater access to health information while interacting with their healthcare providers.
Deaf adolescents also might experience some challenges understanding printed cardiovascular health information from the Internet or other written materials. Many might struggle with complicated medical and scientific terminologies and insufficient visual descriptions of such complex concepts. In a review of health literacy issues in deaf population, Smith, Massey-Stokes, and Lieberth (2012) call for an implementation and evaluation of a web-based repository of health information delivered in ASL. Despite this recommendation, much of the health information on the Internet is not always accessible to ASL users (Smith et al., 2012). Even when health websites contain videos in ASL, navigating and finding such information can be difficult for some (Kushalnagar, Naturale et al., 2014).
McKee et al. (2011) and Margellos-Anast et al. (2006) assert that more cardiovascular health materials be available in ASL and more programs deliver in-person presentations in ASL such as the Deaf Heart Health Intervention educational program in Arizona (Jones et al., 2005) to maximize deaf signers’ understanding and minimize their misconceptions. The Child and Adolescent Trial for Cardiovascular Health (CATCH) and the Standard Adolescent Health Heart Program are two prominent examples that adolescents do benefit from in-person health education interventions that increase their cardiovascular knowledge and lead to healthier behaviors (Killen et al., 1989; McGraw et al., 1996). Such programs should be adapted for and trialed in deaf adolescents who are likely to benefit from such increased exposure to essential cardiovascular health information.
Some deaf adolescents might also be unable to glean additional cardiovascular health information through informal learning from their physical environments. For example, a deaf adolescent sitting at the dinner table at home with hearing family members might miss out on information from spoken conversations about various health issues affecting the family, such as a grandmother who recently had a heart attack and now has to take some new medicines and change her diet and lifestyle (Hauser, O’Hearn, McKee, Steider, & Thew, 2010). When this pattern is applied to all the other potential sources of informal learning through auditory means, such as mass media and randomly overheard conversations in public places or school hallways, deaf adolescents are likely to be at a significant risk for limited exposure to health information (Barnett, 1999; Tamaskar et al., 2000; Zazove et al., 1993). When deaf people perceive their communication and information access to be poor, this negatively impacts their quality of life (Kushalnagar et al., 2011; Kushalnagar, McKee, et al., 2014; Kushalnagar, Bruce, Sutton, & Leigh, 2015). The combination of limited health knowledge and low perceived quality of life risks earlier onset or more significant cardiovascular health problems. Future research is needed to identify specific health knowledge that deaf adolescents are missing, especially informal health information, so that this information can be included in health education interventions targeted for this at-risk population.
Furthermore, in order to provide more accurate data about deaf people’s cardiovascular health outcomes, future health surveys should be made fully accessible to deaf people who use various communication modalities, accurately identify subpopulations of deaf people who might be at increased risk such as deaf people who use sign language, and more actively recruit these people (Barnett & Franks, 1999).
Conclusion
Deaf adolescents who use sign language in Rochester, New York, many who possess positive characteristics to support cardiovascular health literacy, continue to describe significant challenges with accessing their sources of health information. These challenges are likely contributing to their inconsistent cardiovascular health knowledge. Such findings in this “privileged” group of sign language-using deaf adolescents raise serious concerns about the probability of even weaker cardiovascular health literacy in other deaf adolescents who reside in areas that are less deaf-populated and do not provide health-related lectures and programs in ASL. Additional public funding is needed to support research on deaf adolescents’ informal health-related learning, develop accessible and culturally appropriate health surveys and health education programming (Sadler et al., 2001), improve interpreter education, and disseminate information through social media.
Funding
This study was supported by grant number K01 HL103173-01 from the National Heart Lung and Blood Institute (NHLBI) of the National Institutes of Health. This work was also partially supported by Cooperative Agreement Number U48DP001910 from the U.S. Centers for Disease Control and Prevention (CDC). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NHLBI or CDC.
Conflicts of Interest
No conflicts of interest were reported.
Acknowledgments
We gratefully acknowledge the assistance of Nikki Cherry, Dr. Nancy Chin, Kailea Colayori, Jessica Contreras, Tiffany Panko, Dr. Denise Thew, and Dr. Deirdre Schlehofer.
References
- Baker D. W., Parker R. M., Williams M. V., Clark W. S. (1998). Health literacy and the risk of hospital admission. Journal of General Internal Medicine, 13, 791–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D. W., Wolf M. S., Feinglass J., Thompson J. A., Gazmararian J. A., Huang J. (2007). Health literacy and mortality among elderly persons. Archives of Internal Medicine, 167, 1503–1509. [DOI] [PubMed] [Google Scholar]
- Barnett S. (1999). Clinical and cultural issues in caring for deaf people. Family Medicine, 31, 17–22. [PubMed] [Google Scholar]
- Barnett S., Franks P. (1999). Deafness and mortality: Analyses of linked data from the National Health Interview Survey and National Death Index. Public Health Reports (Washington, D.C.: 1974), 114, 330–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett S., Klein J. D., Pollard R. Q., Jr., Samar V., Schlehofer D., Starr M., Pearson T. A. (2011). Community participatory research with deaf sign language users to identify health inequities. American Journal of Public Health, 101, 2235–2238. 10.2105/AJPH.2011.300247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdańska A., Maniecka-Bryła I., Szpak A. (2005). The evaluation of secondary school students’ knowledge about risk factors of cardiovascular disease. Roczniki Akademii Medycznej w Białymstoku (1995), 50(Suppl. 1), 213–215. [PubMed] [Google Scholar]
- Chin N. P., Cuculick J., Starr M., Panko T., Widanka H., Dozier A. (2013). Deaf mothers and breastfeeding: Do unique features of deaf culture and language support breastfeeding success? Journal of Human Lactation, 29, 564–571. 10.1177/0890334413476921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow C. M., Chu J. Y., Tu J. V., Moe G. W. (2008). Lack of awareness of heart disease and stroke among Chinese Canadians: Results of a pilot study of the Chinese Canadian Cardiovascular Health Project. The Canadian Journal of Cardiology, 24, 623–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell J. W. (1998). Qualitative inquiry and research design. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Dark C. K., Ezenkwele U. A. (2007). Access to care as a predictor of patients’ knowledge of cardiovascular diseases. Journal of the National Medical Association, 99, 1338–1346. [PMC free article] [PubMed] [Google Scholar]
- Dewalt D. A., Berkman N. D., Sheridan S., Lohr K. N., Pignone M. P. (2004). Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine, 19, 1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emond A., Ridd M., Sutherland H., Allsop L., Alexander A., Kyle J. (2015). The current health of the signing Deaf community in the UK compared with the general population: A cross-sectional study. BMJ Open, 5, e006668. 10.1136/bmjopen-2014-006668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher D., Li C. M., Chiu M. S., Themann C. L., Petersen H., Jónasson F., Cotch M. F. (2014). Impairments in hearing and vision impact on mortality in older people: The AGES-Reykjavik Study. Age and Ageing, 43, 69–76. 10.1093/ageing/aft122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost R. (1992). Cardiovascular risk modification in the college student: Knowledge, attitudes, and behaviors. Journal of General Internal Medicine, 7, 317–320. [DOI] [PubMed] [Google Scholar]
- Gans K. M., Assmann S. F., Sallar A., Lasater T. M. (1999). Knowledge of cardiovascular disease prevention: An analysis from two New England communities. Preventive Medicine, 29, 229–237. [DOI] [PubMed] [Google Scholar]
- Greenlund K. J., Keenan N. L., Giles W. H., Zheng Z. J., Neff L. J., Croft J. B., Mensah G. A. (2004). Public recognition of major signs and symptoms of heart attack: Seventeen states and the US Virgin Islands, 2001. American Heart Journal, 147, 1010–1016. [DOI] [PubMed] [Google Scholar]
- Hauser P. C., O’Hearn A., McKee M., Steider A., Thew D. (2010). Deaf epistemology: Deafhood and deafness. American Annals of the Deaf, 154, 486–492. [DOI] [PubMed] [Google Scholar]
- Jones E. G., Renger R., Firestone R. (2005). Deaf community analysis for health education priorities. Public Health Nursing (Boston, Mass.), 22, 27–35. [DOI] [PubMed] [Google Scholar]
- Killen J. D., Robinson T. N., Telch M. J., Saylor K. E., Maron D. J., Rich T., Bryson S. (1989). The Stanford Adolescent Heart Health Program. Health Education Quarterly, 16, 263–283. [DOI] [PubMed] [Google Scholar]
- Kushalnagar P., Bruce S., Sutton T., Leigh I. W. (2015). Early life communicative stress is gender-specific and related to adulthood depression. Poster Session at the Meeting of the American Psychological Association, Toronto, Canada. [Google Scholar]
- Kushalnagar P., McKee M., Smith S. R., Hopper M., Kavin D., Atcherson S. R. (2014). Conceptual model for quality of life among adults with congenital or early deafness. Disability and Health Journal, 7, 350–355. 10.1016/j.dhjo.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushalnagar P., Naturale J., Paludneviciene R., Smith S. R., Werfel E., Doolittle R., DeCaro J. (2014). Health websites: Accessibility and usability for American Sign Language users. Health Communication, 5, 1–8. 10.1080/1-410236.2013.853226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushalnagar P., Topolski T. D., Schick B., Edwards T. C., Skalicky A. M., Patrick D. L. (2011). Mode of communication, perceived level of understanding, and perceived quality of life in youth who are deaf or hard of hearing. Journal of Deaf Studies and Deaf Education, 16, 512–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecouturier J., Murtagh M. J., Thomson R. G., Ford G. A., White M., Eccles M., Rodgers H. (2010). Response to symptoms of stroke in the UK: A systematic review. BMC Health Services Research, 8, 157. 10.1186/1472-6963-10-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundelin K., Graciani A., García-Puig J., Guallar-Castillón P., Taboada J. M., Rodríguez-Artalejo F., Banegas J. R. (2012). Knowledge of stroke warning symptoms and intended action in response to stroke in Spain: A nationwide population-based study. Cerebrovascular Diseases (Basel, Switzerland), 34, 161–168. 10.1159/000341408 [DOI] [PubMed] [Google Scholar]
- Manganello J. A. (2008). Health literacy and adolescents: A framework and agenda for future research. Health Education Research, 23, 840–847. [DOI] [PubMed] [Google Scholar]
- Margellos-Anast H., Estarziau M., Kaufman G. (2006). Cardiovascular disease knowledge among culturally Deaf patients in Chicago. Preventive Medicine, 42, 235–239. [DOI] [PubMed] [Google Scholar]
- Mata J., Frank R., Gigerenzer G. (2014). Symptom recognition of heart attack and stroke in nine European countries: A representative survey. Health Expectations, 17, 376–387. 10.1111/j.1369-7625.2011.00764.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGraw S. A., Sellers D. E., Stone E. J., Bebchuk J., Edmundson E. W., Johnson C. C., Luepker R. V. (1996). Using process data to explain outcomes. An illustration from the Child and Adolescent Trial for Cardiovascular Health (CATCH). Evaluation Review, 20, 291–312. [DOI] [PubMed] [Google Scholar]
- McKee M., Schlehofer D., Cuculick J., Starr M., Smith S., Chin N. P. (2011). Perceptions of cardiovascular health in an underserved community of deaf adults using American Sign Language. Disability and Health Journal, 4, 192–197. 10.1016/j.dhjo.2011.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow J. R., Jr., Krzewinski-Malone J. A., Jackson A. W., Bungum T. J., FitzGerald S. J. (2004). American adults’ knowledge of exercise recommendations. Research Quarterly for Exercise and Sport, 75, 231–237. [DOI] [PubMed] [Google Scholar]
- Nguyen T. T., Liao Y., Gildengorin G., Tsoh J., Bui-Tong N., McPhee S. J. (2009). Cardiovascular risk factors and knowledge of symptoms among Vietnamese Americans. Journal of General Internal Medicine, 24, 238–243. 10.1007/s11606-008-0889-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen-Bohlman L., Pranzer A. M., Kindig D. A. (Eds.). (2004). Health literacy: A prescription to end confusion. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Norton D. E., Froelicher E. S., Waters C. M., Carrieri-Kohlman V. (2003). Parental influence on models of primary prevention of cardiovascular disease in children. European Journal of Cardiovascular Nursing, 2, 311–322. [DOI] [PubMed] [Google Scholar]
- Nutbeam D. (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15, 259–267. [Google Scholar]
- Nutbeam D. (2008). The evolving concept of health literacy. Social Science & Medicine (1982), 67, 2072–2078. [DOI] [PubMed] [Google Scholar]
- Piwoński J., Rywik S., Wp4f1wska H. (1989). Basic principles of the prevention of cardiovascular diseases in light of knowledge and opinions of the Polish community. I. Knowledge of the causes of the spreading epidemic of cardiovascular diseases. Kardiologia Polska, 32(Suppl. 2), 41–46. [PubMed] [Google Scholar]
- Plummer K. (1983). Documents of life: An introduction to the problems and literature of a humanistic method. London: Unwin Hyman. [Google Scholar]
- Pollard R. Q., Barnett S. (2009). Health-related vocabulary knowledge among deaf adults. Rehabilitation Psychology, 54, 182–185. 10.1037/a0015771. [DOI] [PubMed] [Google Scholar]
- Potvin L., Richard L., Edwards A. C. (2000). Knowledge of cardiovascular disease risk factors among the Canadian population: Relationships with indicators of socioeconomic status. CMAJ: Canadian Medical Association Journal, 162, S5–S11. [PMC free article] [PubMed] [Google Scholar]
- Rasinger E., Flores J., Pakesch G., Sinzinger H. (1989). Cholesterol 87–status of knowledge of the Vienna public. Wiener klinische Wochenschrift, 101, 408–412. [PubMed] [Google Scholar]
- Roccella E. J., Bowler A. E., Ames M. V., Horan M. J. (1986). Hypertension knowledge, attitudes, and behavior: 1985 NHIS findings. Public Health Reports (Washington, D.C.: 1974), 101, 599–606. [PMC free article] [PubMed] [Google Scholar]
- Sadler G. R., Huang J. T., Padden C. A., Elion L., Galey T. A., Gunsauls D. C., Brauer B. (2001). Bringing health care information to the deaf community. Journal of Cancer Education, 16, 105–108. [DOI] [PubMed] [Google Scholar]
- Sedibe H. M., Kahn K., Edin K., Gitau T., Ivarsson A., Norris S. A. (2014). Qualitative study exploring healthy eating practices and physical activity among adolescent girls in rural South Africa. BMC Pediatrics, 14, 211. 10.1186/1471-2431-14-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin M. K., Fitzpatrick A. L., Lee K. (2010). Cardiovascular health perceptions in multigenerational Korean immigrants. Family & Community Health, 33, 254–261. 10.1097/FCH.0b013e3181f3b2d3 [DOI] [PubMed] [Google Scholar]
- Smalley S. E., Wittler R. R., Oliverson R. H. (2004). Adolescent assessment of cardiovascular heart disease risk factor attitudes and habits. The Journal of Adolescent Health, 35, 374–379. [DOI] [PubMed] [Google Scholar]
- Smith C. E., Massey-Stokes M., Lieberth A. (2012). Health information needs of d/Deaf adolescent females: A call to action. American Annals of the Deaf, 157, 41–47. [DOI] [PubMed] [Google Scholar]
- Stanley L., Wise S. (1993). Breaking out again: Feminist ontology and epistemology. London: Routledge. [Google Scholar]
- Steptoe A., Wardle J. (2001). Health behaviour, risk awareness and emotional well-being in students from Eastern Europe and Western Europe. Social Science & Medicine (1982), 53, 1621–1630. [DOI] [PubMed] [Google Scholar]
- Tamaskar P., Malia T., Stern C., Gorenflo D., Meador H., Zazove P. (2000). Preventive attitudes and beliefs of deaf and hard-of-hearing individuals. Archives of Family Medicine, 9, 518–525. [DOI] [PubMed] [Google Scholar]
- Vanhecke T. E., Miller W. M., Franklin B. A., Weber J. E., McCullough P. A. (2006). Awareness, knowledge, and perception of heart disease among adolescents. European Journal of Cardiovascular Prevention and Rehabilitation, 13, 718–723. [DOI] [PubMed] [Google Scholar]
- Winham D. M., Jones K. M. (2011). Knowledge of young African American adults about heart disease: A cross-sectional survey. BMC Public Health, 11, 248. 10.1186/1471-2458-11-248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zazove P., Niemann L. C., Gorenflo D. W., Carmack C., Mehr D., Coyne J. C., Antonucci T. (1993). The health status and health care utilization of deaf and hard-of-hearing persons. Archives of Family Medicine, 2, 745–752. [DOI] [PubMed] [Google Scholar]


