Abstract
Most of recurrent bladder carcinoma after partial cystectomy did not cause diagnostic difficulties for urologists, because of the appearance of typical papillary in ultrasonography or cystoscopy, and could be easily confirmed by tumor biopsy. Three patients, ages from 35 to 62 years, had undergone bladder sparing treatment for muscle invasive bladder cancer, all of them had biopsy revealed benign bladder lesion at surveillance cystoscopy. However, transurethral resection of bladder tumor showed high-grade muscle invasive urothelial bladder carcinoma for these patients. Two patients were thus delayed for timely cystectomy and consequently resulted in local or distal metastasis.
As a result, we recommended that timely pelvic enhanced computed tomography and transurethral resection of bladder tumor were necessary when bladder lesion occurred after partial cystectomy, avoiding the possibility of missing muscle invasive urothelial bladder carcinoma recurrence and delaying timely cystectomy.
INTRODUCTION
Although radical cystectomy with urinary diversion has been regarded as the standard treatment for muscle invasive bladder cancer (MIBC), it is associated with high postoperative complication and mortality as well as decreased quality of life.1 As a result, different kinds of bladder sparing approaches have been proposed for MIBC treatment. Partial cystectomy (PC) with pelvic lymph node dissection (PLND) combined with chemotherapy or radiotherapy, which offers complete tumor resection, accurate staging and good quality of life, is regarded as a good bladder sparing treatment modality.1,2 Even though, PC is still criticized for an unacceptable high recurrence rate.3 Recurrent bladder carcinoma after PC is usually correctly diagnosed by urologists, because of the appearance of typical papillary in ultrasonography or cystoscopy, and can be easily confirmed by tumor biopsy. However, in this case series, we presented 3 patients with rare deceptive benign appearance of recurrent MIBC after PC, which delayed timely diagnosis and treatment for 2 of them.
CASE SERIES
From January 2010 to December 2014, 93 consecutive patients underwent PC in our institution. Of these patients, 56 cases of PC with PLND were performed for MIBC. With a median follow-up of 21 months (range 4–52 months), 16 patients (28.6%) had bladder tumor recurrence and 11 salvage radical cystectomy were performed. Of the 16 patients who had bladder tumor recurrence, 2 men were diagnosed as deceptive MIBC recurrence after PC. During the same period of time, one another patient, who was referred to our hospital, presented the same characteristics of tumor recurrence in the course of disease. The clinical information of the 3 patients was presented in Table 1. All the patients declined cystectomy after transurethral resection of bladder tumors (TURBT) confirmed MIBC, and PC with PLND was thus performed instead. As lesions of the 3 patients were within 2 cm to ureteral orifice, ureteral reimplantation was performed at the same time. All patients recovered from PC surgery uneventfully and received 6 cycles of gemcitabine and cisplatinchemotherapy after surgery. Cystoscopy and bladder ultrasonography at 3 months’ interval were routinely examined. All interventions given were part of normal health care and ethicalapproval was thus not necessary needed.
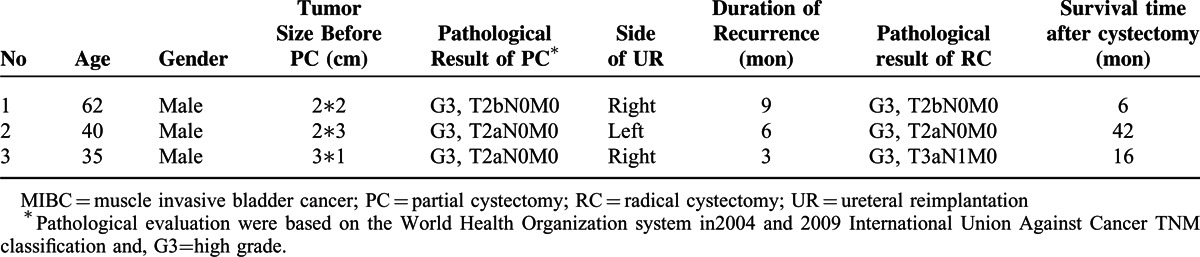
TABLE 1.
Clinical Information of Patients with Deceptive MIBC Recurrence
Case 1. Lesions, measuring 2.5 × 1 cm, with cystitis glandularis appearance were found at the right lateral wall of bladder when the patient underwent cystoscopy 9 months after cystectomy. The pathology result of random biopsy at 3 different sites of the lesion showed cystitis glandularis with von Brunn's nests proliferation. Two months later, the patient presented gross hematuria, and contrast-enhanced pelvic computed tomography (CT) revealed irregular thickening and significantly enhanced bladder wall. The size of the lesion was found slightly increased in cystoscopy; however, the pathology of random biopsy still showed cystitis glandularis. TURBT was then performed, and high-grade muscle invasive urothelial carcinoma with urothelialcystitis glandularis was diagnosed by pathological examination. The patient then underwent cystectomy with ileal conduit diversion. However, the patient died 6 months after cystectomy with multiple distal metastasis.
Case 2. Cystoscopic evaluation revealed polypoidlesion, measuring 2 × 1 cm, on the left bladder wall 6 months after PC. Pathologic evaluation of random biopsy revealed chronic bladder inflammation without evidence of malignancy. However, ultrasonography and CT showed enhanced, thickening of left bladder wall. TURBT was carried out and the pathology showed high-grade muscle invasive urothelial bladder cancer. Cystectomy with orthotopicneo bladder diversion was thus performed, and the patient was now still alive without bladder tumor recurrence for 48 months.
Case 3. Polypoid lesions, measuring 1 × 1 cm, on the right bladder wall near the internal urethral orifice were found at cystoscopy 3 months after PC in another hospital. Pathologic examination of biopsy showed chronic bladder inflammation with proliferation of von Brunn's nests. The patient thus did not receive any treatment or further examination. He was referred into our hospital 2 months later because of right renal area dull pain. Cystoscopy examination confirmed the lesion aforementioned (Figure 1A). Pathologic evaluation of repeated multiple random biopsy still showed no evidence of malignant tumor. However, computed tomography urography (CTU) revealed right-sided hydroureteronephrosis and thicken bladder wall with unclear boundary to the surrounding tissue (Figure 1B, Figure 1C). Comparison between the CT scan after tumor recurrence and before PC were made in Figure 1. TURBT was performed and the pathological evaluation revealed high-grade muscle invasive bladder urothelial carcinoma. The patient underwent cystectomy with ileal conduit diversion, and the gross pathologic examination showed that the bladder cancer had infiltrated the surrounding tissue with one lymph node metastasis. The patient was now alive with no evidence of recurrence for 15 months.
FIGURE 1.
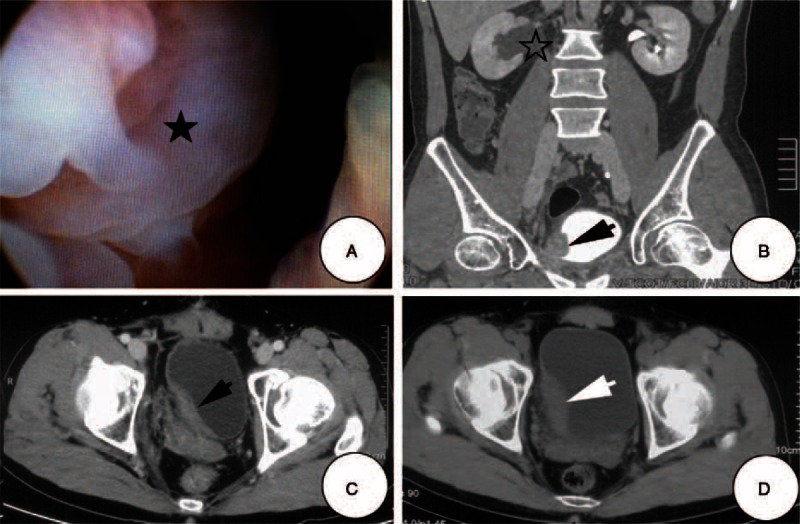
Cystoscopy and CT image. A. Cystoscopy displayed cystitis glandularis appearance lesion (solid asterisk) on the right bladder wall near the internal urethral orifice; B. CTU confirmed hydroureteronephrosis (hollow asterisk) caused by mass on the right lateral bladder wall (black arrow); C. transverse CT image showed an irregular right lateral bladder wall thickened with unclear boundary to the surrounding tissue (black arrow); D. CT confirmed bladder mass on the right lateral bladder wall before bladder sparing treatment (white arrow).
DISCUSSION
Bladder sparing treatment is considered as an important alternative treatment approach for MIBC. Nowadays, various modalities of bladder-sparing methods have been reported and investigated, among which PC with PLND after completeness of TURBT plus chemotherapy or radiotherapy is regarded as a rational one.4 It was reported that the 5-year cancer specific survival rate after PC bladder sparing treatment ranges from 67% to 69%.2–4 Although the 5-year survival rate of PC is comparable to radical cystectomy, and the quality of life for MIBC patients have been greatly improved, this therapeutic approach has not yet been regarded as a standard treatment option for MIBC because of lack of randomizedtrials.1 Critics of PC also argued that the tumor recurrence rate after PC was relatively high, which ranged from 19% to 58%, and two-thirds of tumor recurrence appeared during the first 2 years.5 As a result, one important component of bladder sparing treatment modality was vigilant surveillance after surgery, because early detection of tumor recurrence resulted in excellent outcome of salvage radical cystectomy.6 However, the window to salvage cystectomy was short, and the disease carried a poor prognosis once patients developed extravesical disease caused by delayed diagnosis.6
Regular cystoscopy and random biopsy of suspected lesion played a pivotal role in detecting early recurrence. However, in the present study, 3 patients showed deceptive early MIBC recurrence with a cystitis glandularis crust covered on the surface after bladder sparing treatment, escaping random multiple biopsies. As a consequence, 2 patients missed the optimal opportunity for early diagnosis and delayed timely cystectomy. Enhanced CT and CTU were also the preferred method for bladder surveillance, which showed high accuracy for detecting and staging urinary tract cancer.7,8 Although biopsy revealed negative results in the present cases, CT or CTU showed enhanced and thickened bladder wall, which suggested highly suspicious of bladder cancer recurrence. Therefore, patients showed suspicious lesions in cystoscopy with negative biopsy, enhanced CT or CTU should be recommended for further evaluation rather than watchful waiting.
It was well known that urothelial carcinoma could present variable morphologic and microscopic features. Someinvasive variants, such as nested variant and microcystic carcinoma, might even mimic benign lesions, which may cause difficulties for pathologists in the differential diagnosis.9,10 However, in the present study, the pathological sections of the biopsy tissue obtained at cystoscopy of the 3 patients were blindly sent to 2 different pathologists for further evaluation after TURBT confirmed MIBC, the results were also suggestive of benign tissue, excluding the possibility of nested variant or microcysticurothelial carcinoma. The relationship between the formation of cystitis glandularis and MIBC recurrence was unknown, but several factors might contribute to the deceptive appearance formation. First, such situation potentially reflected a response to bladder injury or chronic bladder inflammation caused by bladder surgery.11 In addition, ureteral reimplantation was reported to be associated with high recurrence and poor prognosis after PC.2,12 It was interesting that all patients with deceptive MIBC recurrence had undergone ureteral reimplantation, which suggested that ureteral reimplantation might be a risk factor for such kind of recurrence.
CONCLUSIONS
Early MIBC recurrence after bladder sparing therapy could simultaneously occurred with cystitis glandularis caused by bladder surgery; this rare situation might lead to diagnosis of cystitis glandularis without realizing bladder cancer recurrence and missed the best treatment opportunity. The present cases served to remind and alert the urologists to be aware of the possibility of bladder cancer recurrence even when the biopsy of the bladder lesion was benign. As a result, timely pelvic enhanced CT and TURBT were necessary when bladder lesion occurred after PC, avoiding the possibility of missing MIBC recurrence and delaying timely cystectomy.
Footnotes
Abbreviations: CT = computed tomography, CTU = computed tomography urography, MIBC = muscle invasive bladder cancer, PC = Partial cystectomy, PLND = pelvic lymph node dissection, TURBT = transurethral resectionof bladder tumors.
CX, SZ, ZZ contributed equally to the paper and are co-first authors.
This study did not receive any funding support, and all people making contributions to the paper had been included in the authorship.
The authors declared that they have no relevant financial interests. No benefits had or will be received from a commercial party related directly or indirectly to the subject of this article.
REFERENCES
- 1.Koga F, Kihara K. Selective bladder preservation with curative intent for muscle-invasive bladder cancer: a contemporary review. Int J Urol 2012; 19:388–401. [DOI] [PubMed] [Google Scholar]
- 2.Ma B, Li H, Zhang C, et al. Lymphovascular invasion, ureteral reimplantation and prior history of urothelial carcinoma are associated with poor prognosis after partial cystectomy for muscle-invasive bladder cancer with negative pelvic lymph nodes. Eur J Surg Oncol 2013; 39:1150–1156. [DOI] [PubMed] [Google Scholar]
- 3.Holzbeierlein JM, Lopez-Corona E, Bochner BH, et al. Partial cystectomy: a contemporary review of the Memorial Sloan-Kettering Cancer Center experience and recommendations for patient selection. J Urol 2004; 172:878–881. [DOI] [PubMed] [Google Scholar]
- 4.Kassouf W, Swanson D, Kamat AM, et al. Partial cystectomy for muscle invasive urothelial carcinoma of the bladder: a contemporary review of the M. D. Anderson Cancer Center experience. J Urol 2006; 175:2058–2062. [DOI] [PubMed] [Google Scholar]
- 5.Kuczyk M, Machtens S, Bokemeyer C, et al. Surgical bladder preserving strategies in the treatment of muscle-invasive bladder cancer. World J Urol 2002; 20:183–189. [DOI] [PubMed] [Google Scholar]
- 6.Knoedler J, Frank I. Organ-sparing surgery in urology: partial cystectomy. Curr Opin Urol 2015; 25:111–115. [DOI] [PubMed] [Google Scholar]
- 7.Jinzaki M, Matsumoto K, Kikuchi E, et al. Comparison of CT urography and excretory urography in the detection and localization of urothelial carcinoma of the upper urinary tract. AJR Am J Roentgenol 2011; 196:1102–1109. [DOI] [PubMed] [Google Scholar]
- 8.Jinzaki M, Tanimoto A, Shinmoto H, et al. Detection of bladder tumors with dynamic contrast-enhanced MDCT. AJR Am J Roentgenol 2007; 188:913–918. [DOI] [PubMed] [Google Scholar]
- 9.Lopez-Beltran A, Cheng L. Histologic variants of urothelial carcinoma: differential diagnosis and clinical implications. Hum Pathol 2006; 37:1371–1388. [DOI] [PubMed] [Google Scholar]
- 10.Williamson SR, Lopez-Beltran A, Montironi R, et al. Glandular lesions of the urinary bladder: clinical significance and differential diagnosis. Histopathology 2011; 58:811–834. [DOI] [PubMed] [Google Scholar]
- 11.Capozza N, Collura G, Nappo S, et al. Cystitis glandularis in children. BJU Int 2005; 95:411–413. [DOI] [PubMed] [Google Scholar]
- 12.Fahmy N, Aprikian A, Tanguay S, et al. Practice patterns and recurrence after partial cystectomy for bladder cancer. World J Urol 2010; 28:419–423. [DOI] [PubMed] [Google Scholar]


