Abstract
Anatomic data regarding femoral version, neck-shaft angle, and acetabular anteversion are still limited in Chinese Han adult population. The aim of this study was to investigate the effects of age, sex, and body laterality on the 3 important anatomic indicators in Chinese Han healthy adults.
Measurements were performed independently by 3 experienced observers using the picture archiving and communication system (PACS) in healthy adults who had received imaging tests of the femur and acetabulum between January 2009 and October 2014. Relevant data were measured and analyzed.
A total of 466 adults (353 males and 113 females) were included. The mean femoral version, neck-shaft angle, and acetabular anteversion for all were 10.62, 133.02, and18.79, respectively. Age-based analysis showed that adults younger than 60 years had a significantly higher neck-shaft angle (P < 0.001) but a significantly lower acetabular anteversion (P < 0.001) than those older than 60 years. Sex-based analysis revealed that females had significantly higher values of femoral version (P < 0.001) and acetabular anteversion (P < 0.001) than males. Laterality-based analysis found the left side had a significantly lower acetabular anteversion (P < 0.001) than the right side. Outcomes of multiple linear regression analysis indicated that femoral version may be associated with sex (P < 0.001) but not age (P = 0.076) or laterality (P = 0.430), neck-shaft angle may be associated with age (P < 0.001) but not sex (P = 0.378) or laterality (P = 0.233), and acetabular anteversion may be associated with age (P < 0.001) and sex (P < 0.001) but not laterality (P = 0.060).
In this representative Chinese cohort, neck-shaft angle may decrease, whereas acetabular anteversion may increase with age, females may have higher values of femoral version and acetabular anteversion than males, and the right body side may have a higher value of acetabular anteversion than the left side.
INTRODUCTION
Femoral version, neck-shaft angle, and acetabular anteversion are important anatomic indicators in clinical orthopedics. Femoral version and acetabular anteversion should be given full consideration during total hip arthroplasty (THA) to reduce the risk of postoperative dislocation.1,2 Additionally, it is reported that abnormal acetabular anteversion and/or femoral version participate in the etiogenesis of hip osteoarthritis,3,4 developmental dysplasia of the hip (DDH),5,6 and gluteal tendinopathy.7 Femoral neck-shaft angle, defined as an intersection angle by proximal femoral shaft axis and femoral neck axis, is another clinically significant parameter of proximal femoral geometry (PFG). Recent studies8,9 indicate that a greater neck-shaft angle may increase the risk of proximal femoral fracture. It is found that a lower neck-shaft angle may result in elevated risk of greater trochanteric pain syndrome (GTPS) in females.10 Therefore, on one hand, as possible pathogenic indicators of some hip disorders, the 3 parameters should be noted during hip surgeries; on the other hand, identifying normal ranges of the parameters and their influencing factors may help surgeons perform hip surgeries better and predict the risk of hip disorders or injury.
Data derived from plenty investigations of PFG were varied because they might have been affected by many factors, such as ethnicity, age, sex, body side, measurement methods, even climate, clothing, and lifestyle.11 In particular, ethnicity has been proved as one of the most important factors accounting for the variations. Currently, most PFG studies were performed in America,12–15 Europe,16,17 and other Asian countries like Japan,2,18 Korean,1,19 India,20 and Thailand.21 Although several similar studies11,22,23 were conducted in Chinese population, their sample sizes were limited. Additionally, analysis is insufficient regarding the effects of age, sex, and body laterality on the PFG parameters. Therefore, currently limited PFG information in Chinese population necessitated an updated report with a larger sample size and stratified analysis by age, sex, and body laterality.
The aim of the present study was to investigate characteristics of femoral version, neck-shaft angle, and acetabular anteversion in Chinese Han healthy adults. We sought to compare the 3 parameters between 2 age groups with cutoff age of 60 years, sexes and literalities; report the rates of femoral retroversion, coxa valgus, and coxavara for all as well as for both stratified analysis by age, sex, and laterality.
PATIENTS AND METHODS
Study Design, Setting, and Data Source
The present study, designed as a retrospective analysis of femoral version, neck-shaft angle and acetabular anteversion in Chinese Han healthy adults, was conducted in Nanfang Hospital, affiliated to Southern Medical University, a tertiary medical center in Guangzhou, South China. Images of the participants who underwent computer tomography (CT) and plain radiograph tests of the femur and acetabulum were initially screened in picture archiving and communication system (PACS). Further eligibility assessment was performed based on the following inclusion and exclusion criteria. Time limit was set from January 1, 2009 to October 31, 2014. Ethical approval and written consents from the participants were waived due to the retrospective design of the present study. However, their personal information were anonymized and de-identified before analysis.
Inclusion and Exclusion Criteria
Inclusion criteria of the study participants were Chinese Han adults, eligible and adequate imaging data for measurement, and absence of previous disorders that might affect measurements of the parameters. Exclusion criteria included: foreigners or non-Chinese Han population; incomplete imaging data; and previous fracture, arthritis, tumor, deformity, or surgery on the proximal part of the femur or acetabulum. If only one body side was available and eligible for measurement, this single side was also included for measurement.
Measurement Performance and Methods
Measurements of femoral version, neck-shaft angle, and acetabular anteversion were performed independently by 3 experienced observers. If there were any discrepancies of >5 degree between any of the 2 observers, measurements were performed by both of them again. The average values were used for statistical analysis.
Femoral version was measured using the Weiner method,24 by superimposing outcomes of the femoral neck axis and distal femoral condylar axis. Neck-shaft angle measurement, performed in standard anterior-posterior X-rays of the proximal femur or pelvis, was generated by the intersection angle between the femoral neck axis and proximal femoral shaft axis.25 Acetabular anteversion, defined as the angle formed by a line between the anterior and posterior acetabular ridge and a reference line perpendicular to a line between the posterior pelvic margins at the level of the sciatic notch,22 was measured on axial CT images through the acetabular center.
Statistical Analysis
Statistical analysis was conducted using the SPSS 17.0 software (SPSS Inc, Chicago, IL). Continuous data were presented as the mean and standard deviation. Dichotomous data were revealed as percentages. Two independent-samples t test was performed to evaluate the differences between 2 age groups and sexes. Paired-samples t test was taken to compare differences between the 2 body lateralities of the participants with available data of the both sides. Chi-square test was used to assess the differences in dichotomous variables. Multiple linear regression analysis was conducted to investigate the possible association of age, sex, and laterality with femoral version, neck-shaft angle, and acetabular anteversion separately. Statistically significant difference was defined as P value of <0.05.
RESULTS
Demographics
A total of 466 patients (353 males and 113 females) were included for measurement. The average age for all was 62.44 ± 18.72 years (range, 18–93 years). The mean age for males and females was 61.39 ± 18.18 years (range, 18–91 years) and 65.72 ± 20.04 years (range 18–93 years).
Primary Outcomes
Measurement Outcomes for All
The average values of femoral version, neck-shaft angle, and acetabular anteversion for all were 10.62 ± 9.02 (range, −15.66 to 39.12), 133.02 ± 4.49 (range, 118.74–143.15), and 18.79 ± 5.30 (range, 4.46–34.74), respectively.
Age-Based Analysis
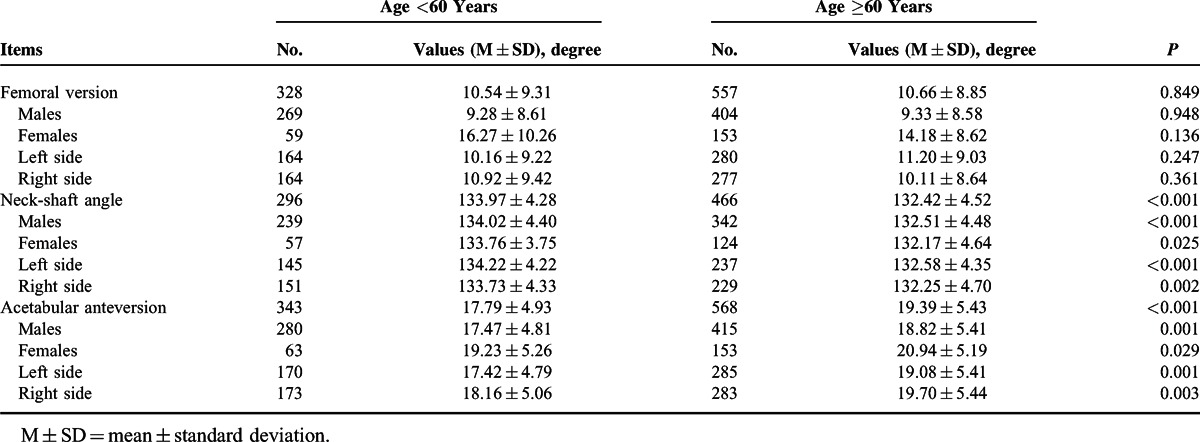
All measurement data were divided into 2 groups with cutoff age of 60 years. As shown in Table 1, participants younger than 60 years had a significantly higher neck-shaft angle (133.97 vs 132.42, P < 0.001), but a significantly lower acetabular anteversion (17.79 vs 19.39, P < 0.001) than those older than 60 years. Additionally, no significant difference was found regarding femoral version between the 2 age groups (P = 0.849). Moreover, subgroup analyses sorted by sex and body laterality were in accordance with the above outcomes (Table 1).
TABLE 1.
Femoral Version, Neck-shaft Angle and Acetabular Anteversion for all, for Sexes, and Lateralities by Age
Sex-Based Analysis
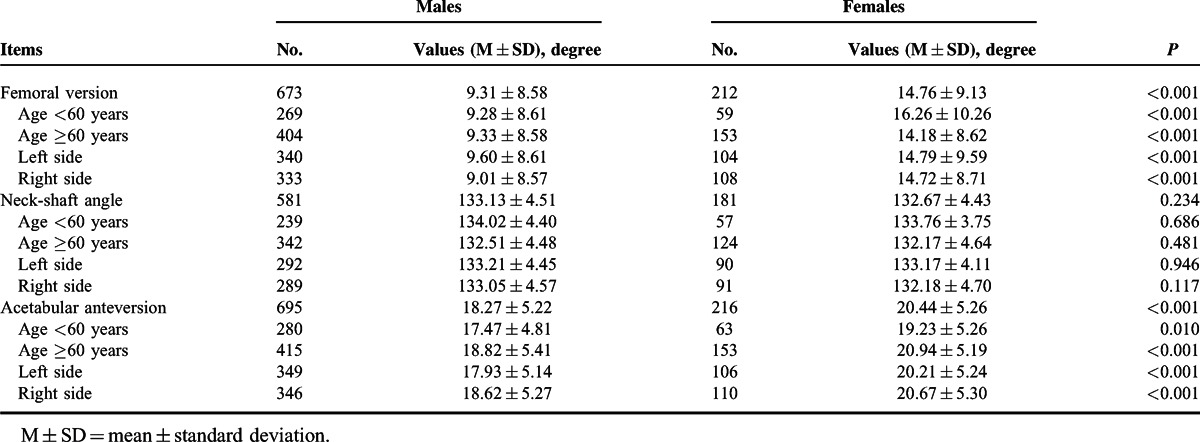
In the stratified analysis by sex (Table 2), females had significantly higher values of femoral version (14.76 vs 9.31, P < 0.001) and acetabular anteversion (20.44 vs 18.27, P < 0.001) than males. Additionally, no significant sex difference was found in neck-shaft angle (P = 0.234). Furthermore, subgroup analyses by age and body laterality also supported the above outcomes (Table 2).
TABLE 2.
Femoral Version, Neck-shaft Angle, and Acetabular Anteversion for Different Age Groups, for Lateralities by Sex
Laterality-Based Analysis
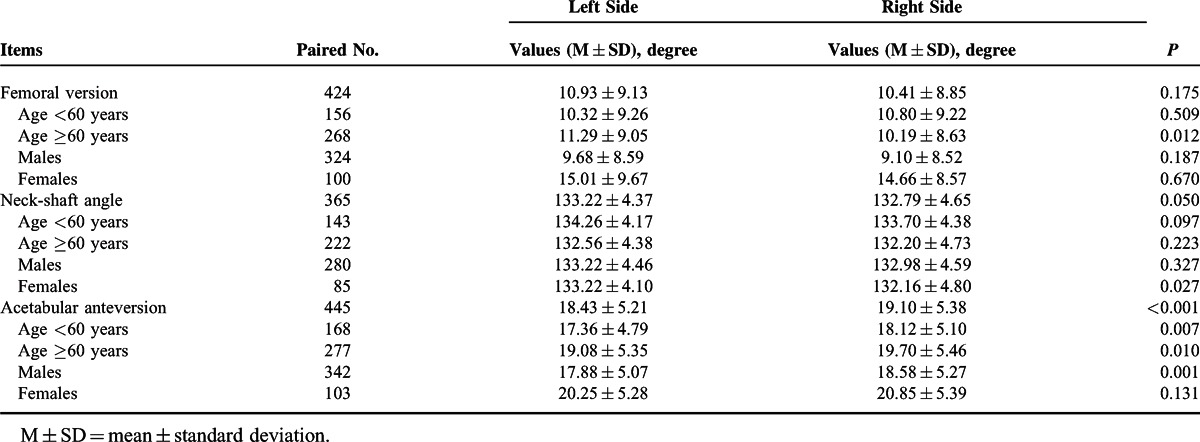
In the analysis by body laterality (Table 3), outcomes revealed no significant differences regarding femoral version (P = 0.175) and neck-shaft angle (P = 0.050) between the 2 lateralities in addition to a statistically higher acetabular anteversion in the right side of body (19.10 vs 18.43, P < 0.001). However, not all the outcomes of subgroup analysis sorted by age and sex were in agreement with the above results. First, adults older than 60 years had a significantly higher femoral version at the left side (11.29 vs 10.19, P = 0.012). Second, females had a significantly greater neck-shaft angle at the left side (133.22 vs 132.16, P = 0.027). Third, although the right laterality had a higher acetabular anteversion than the left laterality for all, no significant difference was found between the 2 sides in females (20.25 vs 20.85, P = 0.131). It requires more studies to certify whether these variances have clinical relevance or just in a statistical manner.
TABLE 3.
Femoral Version, Neck-shaft Angle and Acetabular Anteversion for Different Age Groups, for Sexes by Laterality
Multiple Linear Regression Analysis With Age, Sex, and Laterality as Covariates
Outcomes of multiple linear regression analysis showed that femoral version might be associated with sex (P < 0.001) but not age (P = 0.076) or laterality (P = 0.430), neck-shaft angle might be associated with age (P < 0.001) but not gender (P = 0.378) or laterality (P = 0.233), and acetabular anteversion might be associated with age (P < 0.001) and sex (P < 0.001) but not laterality (P = 0.060).
Secondary Outcomes
Rates of Femoral Retroversion, Coxa Valgus, and Coxavara
The rates of femoral retroversion (femoral version <0), coxa valgus (neck-shaft angle >140), and coxavara (neck-shaft angle <110) for all were 11.30% (100/885), 3.80% (29/762), and 0%, respectively.
In the stratified analyses by age, sex, and laterality, no statistical differences were found regarding femoral retroversion rate (under 60 years vs over 60 years: 12.20% vs 10.77%, P = 0.518) or coxa valgus rate (under 60 years vs over 60 years: 5.07% vs 3.00%, P = 0.147) between 2 age groups. Additionally, males had a significantly higher femoral retroversion rate than females (13.52% vs 4.24%, P < 0.001). However, there was no significant sex difference regarding coxa valgus rate (4.48% vs 1.66%, P = 0.084). Furthermore, no significant differences were identified between the left and right sides of body regarding femoral retroversion rate (11.04% vs 11.56%, P = 0.804) or coxa valgus rate (4.45% vs 3.16%, P = 0.351).
DISCUSSION
Femoral version, neck-shaft angle, and acetabular anteversion are important PFG indicators during hip surgeries. Moreover, abnormal values of the above 3 parameters may be associated with hip disorders like femoroacetabular impingement (FAI), hip osteoarthritis, and fractures. Therefore, identification of their normal ranges and possible influencing factors in healthy population can benefit clinical orthopedics. To provide more detailed and convincing PFG data in Chinese population, the present study in a larger cohort of Chinese Han healthy adults investigated the effects of age, sex, and body laterality on the 3 PFG parameters. Our measurements revealed that neck-shaft angle decreased, whereas acetabular anteversion increased with age, females had higher values of femoral version and acetabular anteversion than males, and the right side of body had a higher acetabular anteversion than the left side.
We found that femoral version in Chinese healthy adults was associated with sex but not age or laterality. In other words, females had a significantly higher femoral version than males. According to Nguyen and Shultz,26 heredity and behavioral factors (eg, sitting in the “reverse tailor's” position, frequent in-toe belly sleeping) may contribute to greater femoral version in females. As a parameter of PFG and lower extremity alignment (LEA), femoral version plays an important role in lower extremity function. Understanding the sex difference in femoral version may help better clarify its role as a potential risk factor of injury, though definite relationship has not been established between the 2 aspects.26
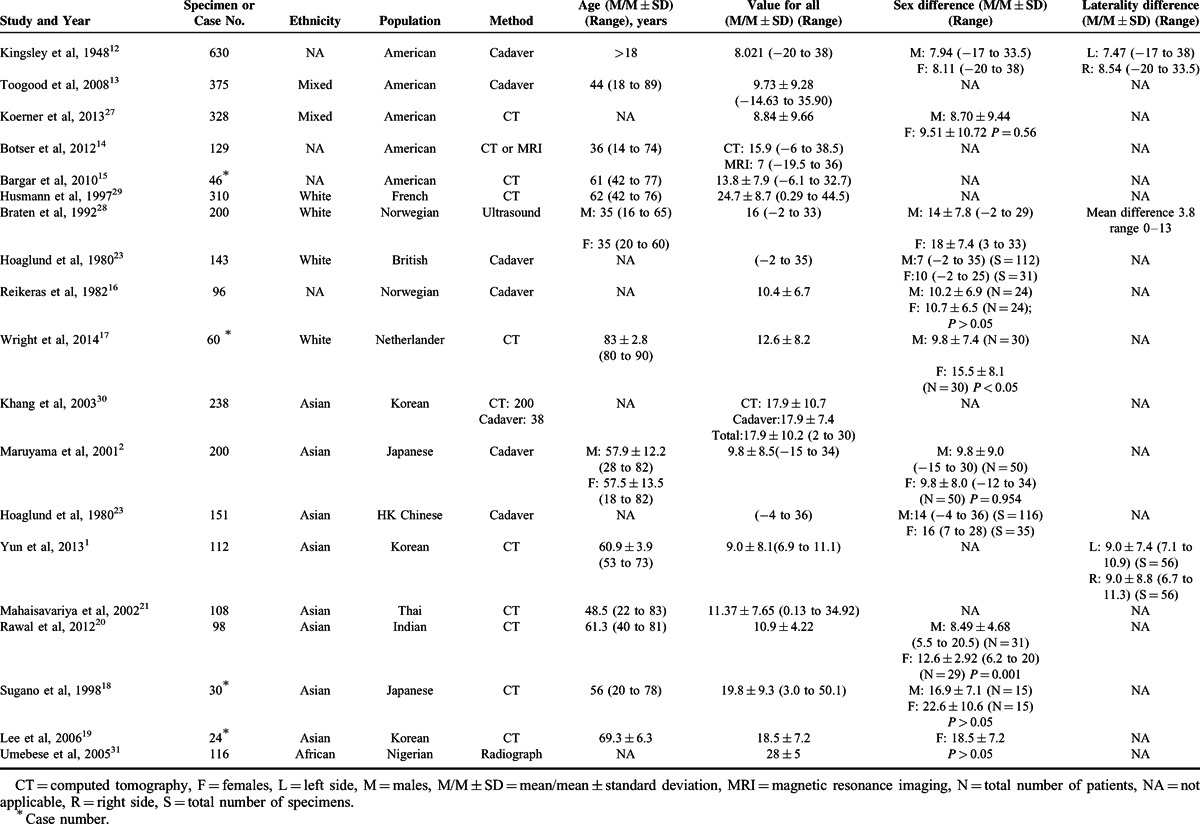
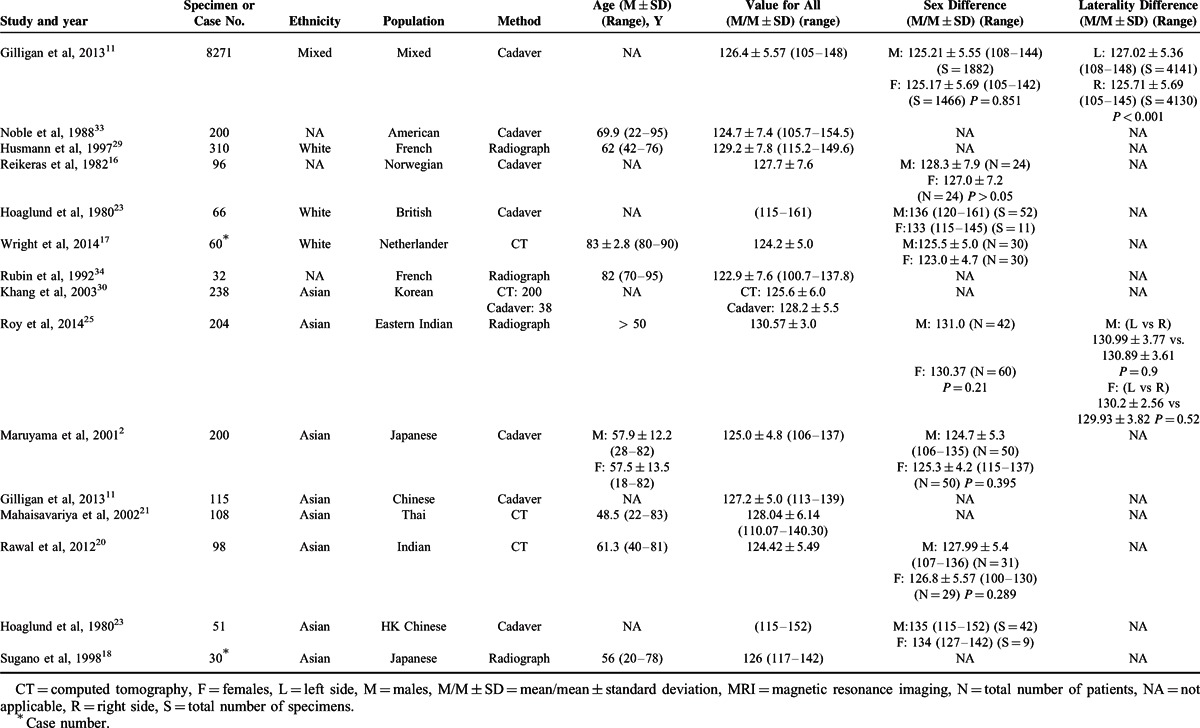
Previous reports of femoral version were mainly from Americans,12–15,27 Europeans,16,17,23,28,29 Asians,1,2,18–21,23,30 and Africans31 (Table 4). The average values of femoral version reported for the 4 populations ranged from 8.0212 to 15.9,14 10.416 to 24.7,29 9.01 to 19.818 and 28 (single report),31 respectively. In a current measurement of the largest number of American cadavers, Kingsley et al12 found similar values between sexes and body lateralities. Similarly, Koerner et al27 also reported no sex difference (P = 0.56) in Americans. However, inconsistency existed regarding the femoral version between sexes in European and Asian populations. Reikeras et al16 identified no sex difference (P > 0.05) in 48 Norwegians. But Wright et al17 indicated that females had a statistically greater value than males (P < 0.05) in 60 Netherlanders. Similarly in Asian, Maruyama et al2 showed no significant sex difference in 100 Japanese (P = 0.954), consistent with what reported by Sugano et al.18 However, in a cohort of 60 Indians, Rawal et al20 found a significantly higher value of femoral version in females than in males (P = 0.001). A single study31 based on 116 Nigerians revealed no significant difference between the two sexes. Therefore, ethnicity and geography may be another factors accounting for the variations of femoral version in addition to sex.
TABLE 4.
Previous Reports Regarding Outcomes of Femoral Version for All, for Sexes, and Body Lateralities
As another important parameter of PFG, the value of neck-shaft angle is probably associated with age but not sex or laterality in Chinese Han population. As revealed clearly in Table 1, adults younger than 60 years had a significantly greater neck-shaft angle than those older than 60 years. In other words, femoral neck-shaft angle may decrease with age, which is in accordance with a recent study,32 investigating the effects of growth and aging on proximal femoral bone in Chinese females. We think this is probably because area bone mineral density (aBMD) gradually decreases with age, resulting in gradually decreased support strength from the proximal femur. Therefore, just as Wang et al32 indicated, both deterioration of aBMD and inadequate compensatory change in bone geometry account for the increased risk of fractures in elderly, especially for females.
Similar to femoral version, femoral neck-shaft angle is also affected by many factors. In a recent study based on a global neck-shaft angle database of 8271 femora, Gilligan et al11 indicated that sex, age, body laterality, climate, clothing, and lifestyle were potential sources of variation for neck-shaft angle. They also found that the average value of neck-shaft angle for all was about 127 degree, with 130 degree, 126 degree, and 125 degree for populations in Pacific, Europe, and America. As shown in Table 5,2,11,16–18,20,21,23,25,29,30,33,34 the mean neck-shaft angle for Americans, Europeans, and Asians ranged from 124.7 degree (single study),33 122.934 to 129.2,29 124.4220 to 130.57,25 respectively. Although most of the published studies reported no significant difference between sexes,2,11,20,25 their stratified analysis for sex difference revealed that males tended to have a higher value of neck-shaft angle than females, which is supported by the present study. Additionally, we are also in agreement with the report by Hoaglund et al23 in HK Chinese. They found the average neck-shaft angles for males and females were 135 and 134, quite similar to our measurements of 133.13 and 132.67, respectively. However, Gilligan et al11 in a cadaveric study of 115 Chinese showed that the mean neck-shaft angle was 127, quite lower than our 133 degree. We think that this might have been caused by different climates (Beijing vs Guangzhou) involved in the 2 studies. Just as Gilligan et al11 indicated, the climatic trends for neck-shaft angle are negative for latitude, whereas positive for temperature. Although the result of laterality-based analysis in our study is in accordance with Roy et al25 reporting no significant laterality difference for neck-shaft angle, we found a greater value at the left side (especially in subgroup analysis for females), which was supported by Gilligan et al.11 It requires more future investigations whether body laterality difference existed.
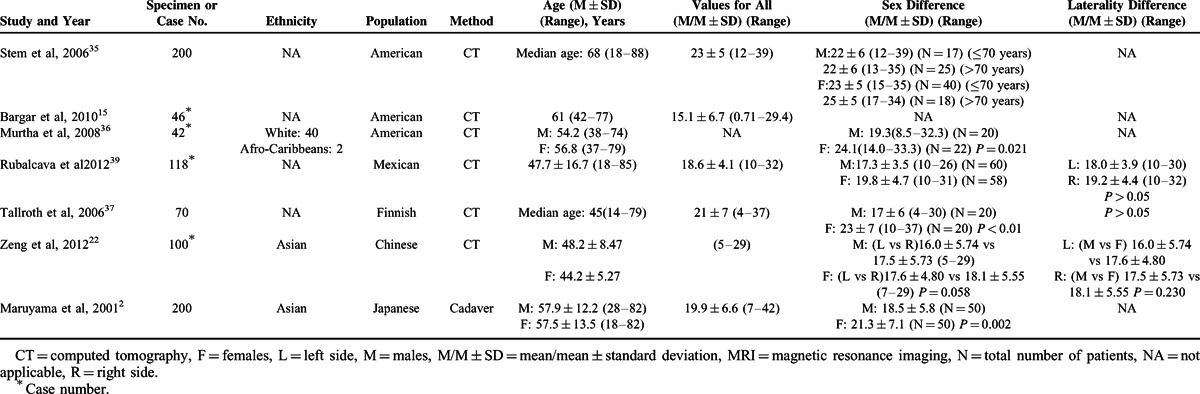
TABLE 5.
Previous Reports Regarding Outcomes of Neck-shaft Angle for all, for Genders and Body Lateralities
The present study found that acetabular anteversion was associated with age and sex but not laterality. Specifically speaking, initially, adults younger than 60 years had a significantly lower acetabular anteversion than those older than 60 years. That is to say, acetabular anteversion may increase with age. Similar to our outcomes, Stem et al35 found a significantly higher acetabular anteversion in people older than 70 years than those younger than 70 years in females. Although the causes for such age-related change in acetabular anteversion are still not clear, just as Stem et al35 stated, the altered acetabular orientation may be associated with an increased risk of osteoarthritis. Second, our finding that females had a significantly higher acetabular anteversion than males is in accordance with most of the previous outcomes (Table 6).2,15,22,35–37,39 Pincer-type FAI, associated with acetabular retroversion, is more frequently observed in females, but we found females had a greater value of acetabular anteversion than males, which supports the viewpoints38 that pincer-type FAI in females cannot be explained by differences of acetabular anteversion alone. Third, although our multiple linear regression analysis showed that acetabular anteversion may be unrelated to laterality, laterality-based analysis showed that the right side may have a higher value of acetabular anteversion than the left side, which is in consistent with Rubalcava et al.39 We consider that this side difference may be caused by habitually dominant use of the right lower extremity in Chinese population. As the sample size of present study is still not large enough, more studies are warranted.
TABLE 6.
Previous Reports Regarding Outcomes of Acetabular Anteversion for all, for Sexes, and Body Lateralities
In our study, the femoral retroversion rate for all was 11.30% and statistically higher in males than in females (13.52% vs 4.24%, P < 0.001). However, Koerner et al27 reported that the femoral retroversion rates for white Americans, African Americans, and Hispanics in males were 21.4%, 15.1%, and 7.1%, respectively, whereas18.8%, 23.5%, and 14.3% in females. Although males had a higher rate of coxa valgus than females (4.48% vs1.66%) in the present study, no statistical difference was identified. In addition, no significant differences were found regarding femoral retroversion rate and coxa valgus rate, neither between 2 age groups nor between body literalities.
Our study has several limitations. First, the measurements of femoral version, neck-shaft angle, and acetabular anteversion we reported cannot lead to a comprehensive understanding of PFG in Chinese Han adult population because there are still many other parameters of PFG, such as femoral head off set, femoral head diameter, and acetabular abduction. Second, although we tried to reduce possible bias, through independent measurement by 3 experienced observers, bias cannot have been eliminated entirely. In addition to the measurement disparity between different observers, other factors like image quality and specific measurement method also might have caused bias. Third, although findings of the present study were based on 466 adults, sex distribution in the sample size was imbalanced so that cautious attitude should be taken toward females-related findings. Moreover, it should be noted that, in addition to age, sex, and body laterality reported in present study, PFG may be affected by other factors, such as aBMD, body height, and weight. Therefore, future PFG studies should take full consideration of all the above aspects.
In summary, our study based on a larger sample size of Chinese Han population finds the following: neck-shaft angle may decrease whereas acetabular anteversion may increase with age; females may have higher values of femoral version and acetabular anteversion than males; and the right side of body may have a higher acetabular anteversion than the left side. Additionally, based on the current data, no significant differences have been identified regarding femoral retroversion rate as well as coxa valgus rate between 2 age groups or body literalities except for a significantly higher femoral retroversion rate in males.
Acknowledgements
The authors thank Prof Allen P. Liang for revising this manuscript. The authors are also grateful for the support of Natural Science Foundation of China (Grant No. 31440043), Natural Science Foundation for the Youth of China (Grant No. 81401777), and Guangdong Provincial Natural Science Fund Doctor Startup Project (Grant No. S2012040006946).
Footnotes
Abbreviations: aBMD = area bone mineral density, CT = computer tomography, DDH = developmental dysplasia of the hip, FAI = femoroacetabular impingement, GTPS = greater trochanteric pain syndrome, LEA = lower extremity alignment, MRI = magnetic resonance imaging, PACS = picture archiving and communication system, PFG = proximal femoral geometry, THA = total hip arthroplasty.
JN and PL contributed equally to this study.
Funding support: This study was supported by Natural Science Foundation of China (Grant No. 31440043), Natural Science Foundation for the Youth of China (Grant No. 81401777) and Guangdong Provincial Natural Science Fund Doctor Startup Project (Grant No. S2012040006946).
The authors certify that they, or any members of their immediate families, have no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
REFERENCES
- 1.Yun HH, Yoon JR, Yang JH, et al. A validation study for estimation of femoral anteversion using the posterior lesser trochanter line: an analysis of computed tomography measurement. J Arthroplasty 2013; 28:1776–1780. [DOI] [PubMed] [Google Scholar]
- 2.Maruyama M, Feinberg JR, Capello WN, et al. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res 2001; 52–65.(393). [PubMed] [Google Scholar]
- 3.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res 2003; 263–269.(417). [DOI] [PubMed] [Google Scholar]
- 4.Li H, Wang Y, Oni JK, et al. The role of femoral neck anteversion in the development of osteoarthritis in dysplastic hips. Bone Joint J 2014; 96-B:1586–1593. [DOI] [PubMed] [Google Scholar]
- 5.Sankar WN, Neubuerger CO, Moseley CF. Femoral anteversion in developmental dysplasia of the hip. J Pediatr Orthop 2009; 29:885–888. [DOI] [PubMed] [Google Scholar]
- 6.Sarban S, Ozturk A, Tabur H, et al. Anteversion of the acetabulum and femoral neck in early walking age patients with developmental dysplasia of the hip. J Pediatr Orthop B 2005; 14:410–414. [DOI] [PubMed] [Google Scholar]
- 7.Moulton KM, Aly AR, Rajasekaran S, et al. Acetabular anteversion is associated with gluteal tendinopathy at MRI. Skeletal Radiol 2015; 44:47–54. [DOI] [PubMed] [Google Scholar]
- 8.Gnudi S, Sitta E, Pignotti E. Prediction of incident hip fracture by femoral neck bone mineral density and neck-shaft angle: a 5-year longitudinal study in post-menopausal females. Br J Radiol 2012; 85:e467–e473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Im GI, Lim MJ. Proximal hip geometry and hip fracture risk assessment in a Korean population. Osteoporos Int 2011; 22:803–807. [DOI] [PubMed] [Google Scholar]
- 10.Fearon A, Stephens S, Cook J, et al. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. Br J Sports Med 2012; 46:888–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilligan I, Chandraphak S, Mahakkanukrauh P. Femoral neck-shaft angle in humans: variation relating to climate, clothing, lifestyle, sex, age and side. J Anat 2013; 223:133–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kingsley PC, Olmsted KL. A study to determine the angle of anteversion of the neck of the femur. J Bone Joint Surg Am 1948; 30A:745–751. [PubMed] [Google Scholar]
- 13.Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 2009; 467:876–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Botser IB, Ozoude GC, Martin DE, et al. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy 2012; 28:619–627. [DOI] [PubMed] [Google Scholar]
- 15.Bargar WL, Jamali AA, Nejad AH. Femoral anteversion in THA and its lack of correlation with native acetabular anteversion. Clin Orthop Relat Res 2010; 468:527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reikeras O, Hoiseth A, Reigstad A, et al. Femoral neck angles: a specimen study with special regard to bilateral differences. Acta Orthop Scand 1982; 53:775–779. [DOI] [PubMed] [Google Scholar]
- 17.Wright SJ, Boymans TA, Grimm B, et al. Strong correlation between the morphology of the proximal femur and the geometry of the distal femoral trochlea. Knee Surg Sports Traumatol Arthrosc 2014; 22:2900–2910. [DOI] [PubMed] [Google Scholar]
- 18.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 1998; 22:610–614. [DOI] [PubMed] [Google Scholar]
- 19.Lee YS, Oh SH, Seon JK, et al. 3D femoral neck anteversion measurements based on the posterior femoral plane in ORTHODOC system. Med Biol Eng Comput 2006; 44:895–906. [DOI] [PubMed] [Google Scholar]
- 20.Rawal B, Ribeiro R, Malhotra R, et al. Anthropometric measurements to design best-fit femoral stem for the Indian population. Indian J Orthop 2012; 46:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahaisavariya B, Sitthiseripratip K, Tongdee T, et al. Morphological study of the proximal femur: a new method of geometrical assessment using 3-dimensional reverse engineering. Med Eng Phys 2002; 24:617–622. [DOI] [PubMed] [Google Scholar]
- 22.Zeng Y, Wang Y, Zhu Z, et al. Differences in acetabular morphology related to side and sex in a Chinese population. J Anat 2012; 220:256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoaglund FT, Low WD. Anatomy of the femoral neck and head, with comparative data from Caucasians and Hong Kong Chinese. Clin Orthop Relat Res 1980; 10–16.(152). [PubMed] [Google Scholar]
- 24.Weiner DS, Cook AJ, Hoyt WJ, et al. Computed tomography in the measurement of femoral anteversion. Orthopedics 1978; 1:299–306. [PubMed] [Google Scholar]
- 25.Roy S, Kundu R, Medda S, et al. Evaluation of proximal femoral geometry in plain anterior-posterior radiograph in eastern-Indian population. J Clin Diagn Res 2014; 8:C1–C3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther 2007; 37:389–398. [DOI] [PubMed] [Google Scholar]
- 27.Koerner JD, Patel NM, Yoon RS, et al. Femoral version of the general population: does “normal” vary by gender or ethnicity? J Orthop Trauma 2013; 27:308–311. [DOI] [PubMed] [Google Scholar]
- 28.Braten M, Terjesen T, Rossvoll I. Femoral anteversion in normal adults. Ultrasound measurements in 50 men and 50 women. Acta Orthop Scand 1992; 63:29–32. [DOI] [PubMed] [Google Scholar]
- 29.Husmann O, Rubin PJ, Leyvraz PF, et al. Three-dimensional morphology of the proximal femur. J Arthroplasty 1997; 12:444–450. [DOI] [PubMed] [Google Scholar]
- 30.Khang G, Choi K, Kim C, et al. A study of Korean femoral geometry. Clin Orthop Relat Res 2003; 406:116–122. [DOI] [PubMed] [Google Scholar]
- 31.Umebese PF, Adeyekun A, Moin M. Radiological assessment of femoral neck-shaft and anteversion angles in adult Nigerian HIPS. Niger Postgrad Med J 2005; 12:106–109. [PubMed] [Google Scholar]
- 32.Wang Q, Chen D, Cheng SM, et al. Growth and aging of proximal femoral bone: a study with women spanning three generations. J Bone Miner Res 2015; 30:424–430. [DOI] [PubMed] [Google Scholar]
- 33.Noble PC, Alexander JW, Lindahl LJ, et al. The anatomic basis of femoral component design. Clin Orthop Relat Res 1988; 148–165.(235). [PubMed] [Google Scholar]
- 34.Rubin PJ, Leyvraz PF, Aubaniac JM, et al. The morphology of the proximal femur. A three-dimensional radiographic analysis. J Bone Joint Surg Br 1992; 74:28–32. [DOI] [PubMed] [Google Scholar]
- 35.Stem ES, O’Connor MI, Kransdorf MJ, et al. Computed tomography analysis of acetabular anteversion and abduction. Skeletal Radiol 2006; 35:385–389. [DOI] [PubMed] [Google Scholar]
- 36.Murtha PE, Hafez MA, Jaramaz B, et al. Variations in acetabular anatomy with reference to total hip replacement. J Bone Joint Surg Br 2008; 90:308–313. [DOI] [PubMed] [Google Scholar]
- 37.Tallroth K, Lepisto J. Computed tomography measurement of acetabular dimensions: normal values for correction of dysplasia. Acta Orthop 2006; 77:598–602. [DOI] [PubMed] [Google Scholar]
- 38.Tannenbaum E, Kopydlowski N, Smith M, et al. Gender and racial differences in focal and global acetabular version. J Arthroplasty 2014; 29:373–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rubalcava J, Gomez-Garcia F, Rios-Reina JL. Acetabular anteversion angle of the hip in the Mexican adult population measured with computed tomography. Acta Ortop Mex 2012; 26:155–161. [PubMed] [Google Scholar]


