Abstract
To determine the efficacy of different methods of cardiopulmonary resuscitation (CPCR) training in 3 different groups of the society.
In a prospective and observational study of 2000 individuals in 3 different groups including G1, G2, and G3 4 different protocols of CPCR training were applied and their efficacy was compared between the groups. Also, 12 months after the study course, 460 participants from 3 groups were asked to take apart in a theoretical and practical examination to evaluate the long-term efficacy of the 4 protocols.
Among 2000 individuals took a parted in the study, 950 (47.5%) were G1, 600 (30%) were G2, and 450 (22.5%) were G3. G1 in 4 groups were 2.37 and 2.65 times more successful in pretest theoretical and 2.61 and 18.20 times more successful in practical examinations compared with G2 and G3 and gained highest improvement in CPCR skills. Other groups also showed significantly improved CPCR skills. Comparison of different methods of CPCR learning showed that the workshop using interactive lecture as well as human model, educational film, and reference CPCR book has the highest efficacy in all groups. This protocol of CPCR training showed more efficacy in long-term postdelayed evaluation. On the contrary, medical students had better long-term outcomes from the course.
Although G1 and G2 obtained better results in learning CPCR skills, in G3 also the theoretical and practical knowledge were improved significantly. This course increased confidence for doing CPCR in all groups of the study. Considering that the most of the bystanders at emergency states are general population, training this group of the society and increasing their confidence about performing CPCR can be so effective and lifesaving at emergency states. (Clinical trial. Gov registration: NCT02120573)
INTRODUCTION
The understanding of sudden cardiac death as a public health problem has paralleled the development of modern emergency medical services systems. In 1 study, it was found that sudden cardiac death is one of important clinical and public health problems, that lead to almost 400,000 to 450,000 death per year.1 A large amount of literature has discussed about the value of cardiopulmonary resuscitation (CPCR) training after out-of-hospital cardiac arrest.2–6 The role of traditional CPCR in sudden cardiac arrest survival has been recently disputed, given both the poor CPCR skill performance and retention by people who have not currently involved in cardiac resuscitation.2,7
Current European Resuscitation Guidelines 2010 recommend the use of prompt/feedback devices when training for CPCR.8 American Heart Association (AHA) also has guidelines for CPCR and CPCR education.9 In 1 study it was found that training of large numbers of volunteers is feasible, reliable, safe, and cost-effective.10
Substantial societal resources are focused on mass CPCR training11,12 and innovative methods to provide and improve CPCR training to the population in large population.2,7,13–15
Most of individuals in society do not enough attitudes about CPCR16 and in several studies, CPCR training courses have been led to significant attitude changes.17–19
The objective of this study was to evaluate the efficacy of different methods of CPCR training in 3 different groups of the society and evaluate the changes in participants’ attitude.
METHODS
Study Design
This was a prospective observational study of 2000 individuals in 3 different groups of the society, and it was approved through expedited review by all participating hospitals’ institutional review boards.
Study Setting and Population
At the first, programs, methods of training, components of the workshops as well as trainers, and medical education administrators were determined. Trainers were from emergency medical department with acceptable and high practical and scientific capabilities. Contents of the workshops were selected from the reference text book of CPCR20 and prepared as interactive lecturing format.
Study Protocol
Three different groups including medical students (G1), nonmedical students (G2), and general population (G3) of the society were admitted at the study via general recall in Shiraz University of Medical Sciences, in Shiraz city.
G1 were registered at School of Medicine, Shiraz University of Medical Sciences; G2 were training volunteers from Shiraz University, and G3 were gathered by a public enrollment in crowded zones of the city.
The persons who had participated at previous courses or workshops about CPCR, basic life support, and/or advanced life support were excluded from the study.
Four different used methods of CPCR training were:
I—T1 = interactive lecture in human model (Interactive lecturing workshop using lecture and human model [T1])
II—T2 = educational film (Workshop using educational film [T2])
III—T3 = T1+T2 (Workshop using lecture [T3])
IV—T4 = T1 + T2 + T3 + Reference book (Workshop using lecture, human model, educational film as well as reference book [T4])
Efficacy of these different mentioned methods was compared among the groups. In this study, the effects of training methods on knowledge, skill, and proficiency as well as their attitudes of trainees were evaluated and compared between 3 groups. All of the subjects were asked to perform a pretest evaluation of their knowledge about CPCR and emergency needed actions including 20 questions from Text book of CPCR.20
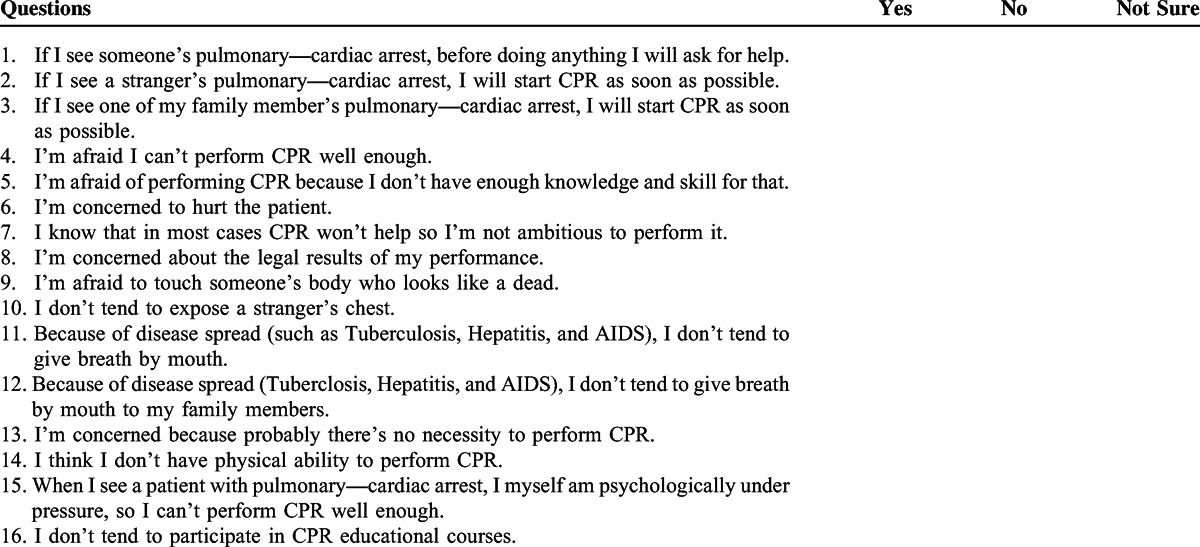
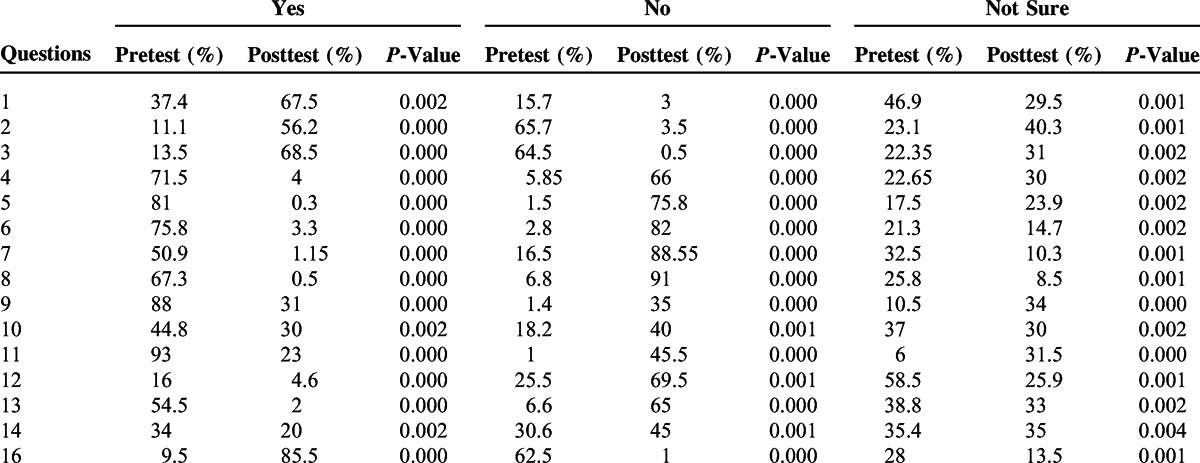
The participants at 4 different groups of the training methods were asked to fill questionnaire before and after the workshop (Table 1).
TABLE 1.
The Questions for the Evaluation of Participant's Attitude About CPR
Also, after performing all training methods, posttest examination including theoretical and course plan practical examinations was performed for all individuals based on AHA criteria.21–23 In fact, 4 examinations were taken including theoretical pretest and posttest and practical pretest and posttest.
The results of the theoretical and practical examinations were calculated, and the changes of the individuals’ knowledge and practical performance, as well as their attitudes to perform CPCR at emergency states, between before and after education course were compared.
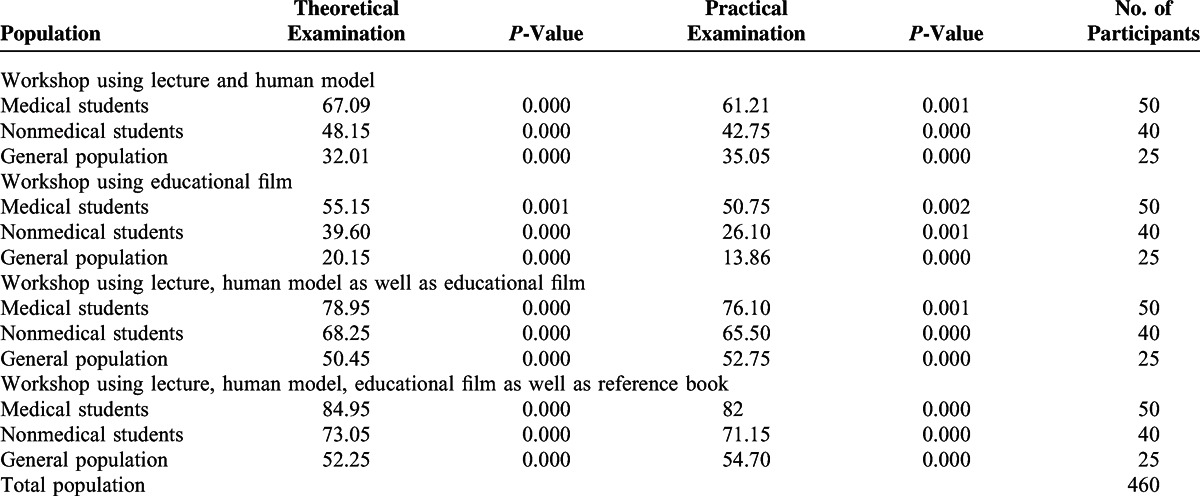
Twelve months after the end of the course, a postdelayed course evaluation of CPCR technique awareness was done on 460 participants from 3 different mentioned groups. They were randomly selected and called for asked to take apart in this study via phone calling and to enroll in theoretical and practical examination. In this postdelayed evaluation, long-term efficacy of 4 different methods of CPCR education were compared (Figure 1).
FIGURE 1.
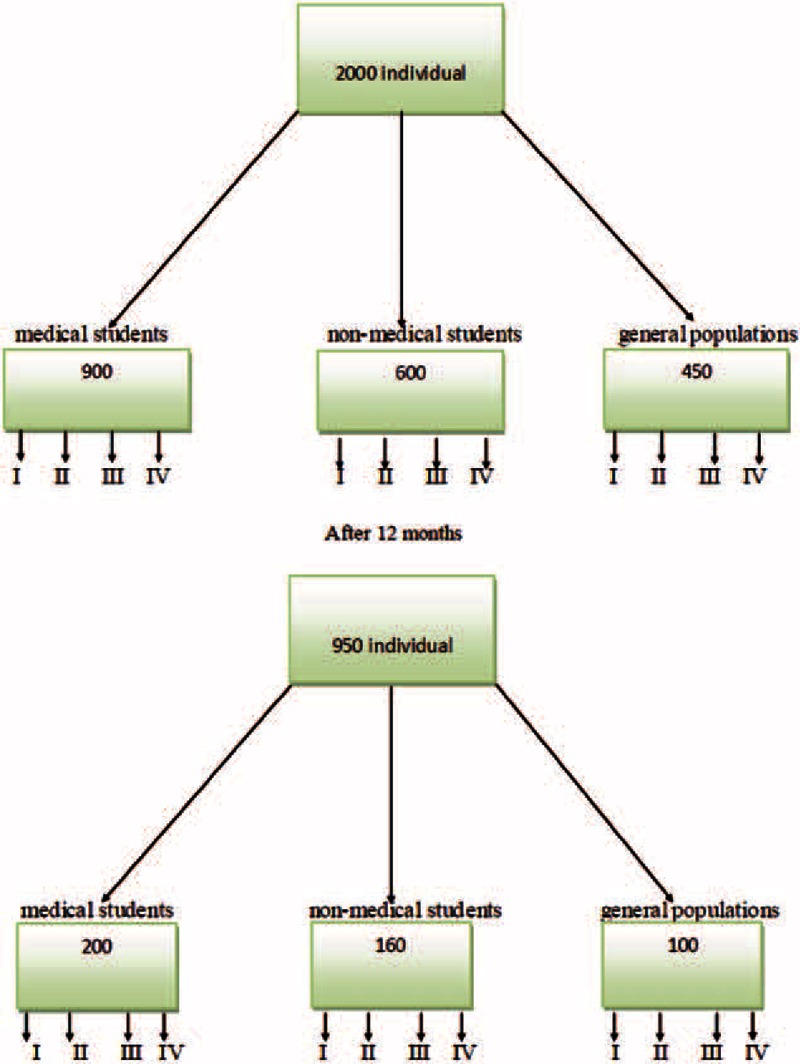
algorithm of attendees and their allocation. I: TI—Interactive lecturing workshop using lecture and human model. II: T2—Workshop using educational film. III: T3—Workshop using lecture, human model as well as educational film. IV: T4—Workshop using lecture, human model, educational film as well as reference book.
It should be noted that training the basics of CPCR, theoretical, and practical examinations were done based on AHA guidelines for CPCR.22,23 All participants were informed about the research and filled an informed consent, and the protocol was approved by Ethics Committee of Research Faculty of University with code of 91-1234.
Statistical Analysis
The date were analyzed using Minitab 16.0 and SPSS 20.0, and the results from theoretical and practical pretest/posttest were compared and analyzed with Paired t test, one-way ANOVA, and Fischer exact test. All variables exhibited the evidence of a possible relation (P < 0.10) to the outcome variable. One way ANOVA and κ2 statistical tests were used to compare the efficacy of CPCR training methods.
RESULTS
During the study period, 2000 subjects who were involved, including 950 (47.5%) G1, 600 (30%) G2, and 450 (22.5%) participants from G3.
Four different methods of education were compared in these 3 different groups of the society including workshop using T1, T2, and workshop using T1 as well as T2, and workshop using T1, T2 as well as reference book. (Table 2)
TABLE 2.
Demographic Data of Attendees
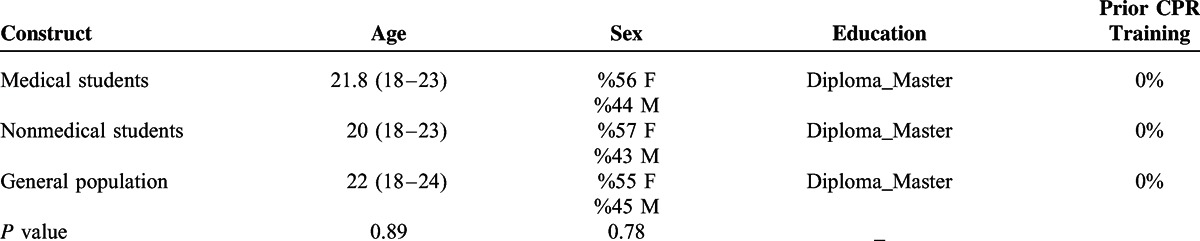
Two groups of training included 237 G1, 150 G2, and 112 people from G3 in another 2 groups, 238 G1, 150 G2, and 113 people from G3 were included.
G1 in 4 groups were significantly more oriented to CPCR compared with other individuals, and better scores achieved at pretest theoretical and practical examinations. Also, mean scores of the G2 were better than G3 in all groups of the education. But there was no significant difference between them.
Highest improvement in CPCR skills was also achieved in G1 in both theoretical and practical evaluations. However, other groups of the participants also showed significantly improvements in CPCR skills. It is expected that G3 had less knowledge in CPCR skills compared with G1 and G2; so, mean scores in pretest theoretical for G1 in 4 groups were 2.37 and 2.65 times more and in practical examinations 2.61 and 18.20 times more compared with G2 and G3 and gained highest improvement in CPCR skills.
The comparison of different methods of CPCR learning showed that the workshop using interactive lecture as well as human model, educational film, and reference CPCR book has the highest efficacy to train theoretical and practical CPCR skills in 3 different groups of participants. The results of pretest and posttest evaluation of CPCR learning methods in different groups of participants are mentioned in (Table 3).
TABLE 3.
Mean Score Resulted from Evaluation of Different Methods of CPR Education in 3 Different Groups of the Society (Score From 100)
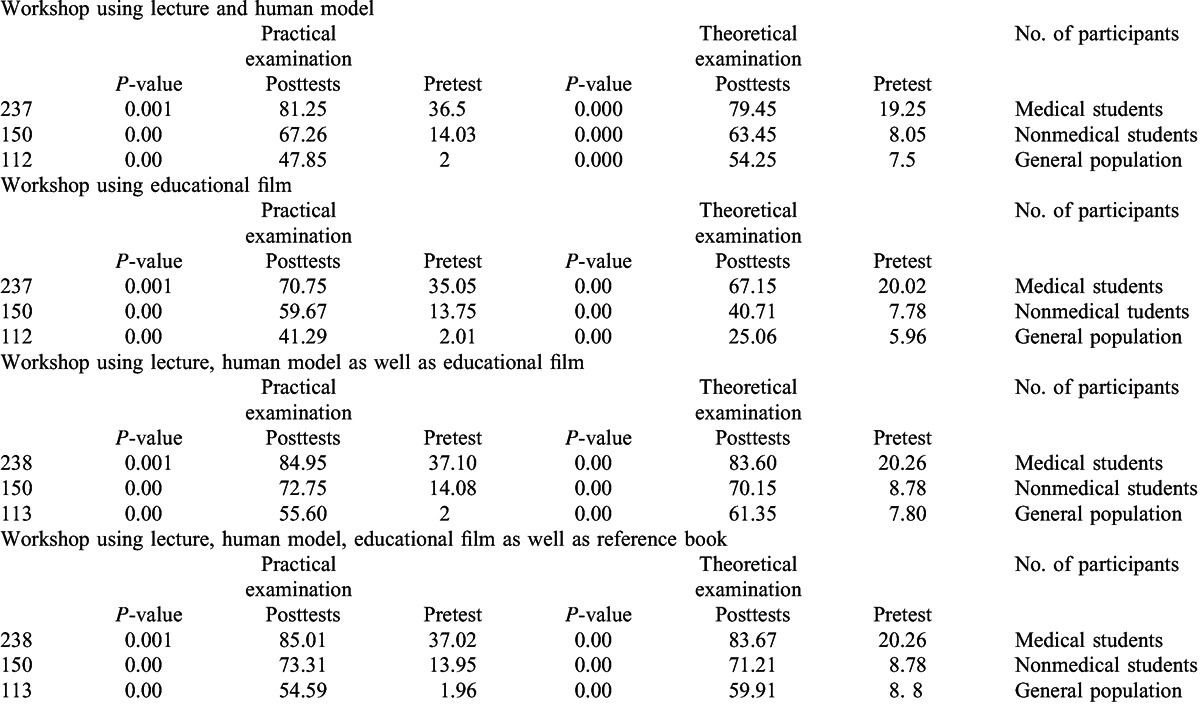
In 3 groups of the study, the 1st method of CPCR training was significantly better than the 2nd method (P value < 0.05). Although the 4th method had better results in CPCR training, there was no significant difference between the efficacy of 3rd and 4th training methods in practical and theoretical examinations (P value > 0.05). On the contrary, the 3rd and 4th method significantly were better than 1st and 2nd methods of training (P value < 0.05).
One year after the core study, postdelayed theoretical and practical examinations were taken to evaluate CPCR trained skills in 460 participants from previous groups. In each group of training, 50 G1, 40 G2, and 25 participants from G3 were included. The results showed that G1 in 4 different groups of CPCR training had better scores compared with other individuals and the method using more and effective facilities such as educational film and reference CPCR book showed better performances at theoretical and practical examinations (Table 4).
TABLE 4.
Mean Score Resulted From Postdelayed Evaluation of CPR Education in Called Participants From 3 Different Groups After 12 Months
Participants’ attitude about performing CPCR at emergency states significantly improved and participants were more willing to do CPCR at needed states. The results of attitude changes of the participants about CPCR are summarized in Table 5.
TABLE 5.
Changes of Participants’ Attitudes About CPR Before and After the CPR Course
DISCUSSION
CPCR is series of lifesaving actions that improve the chance of survival following cardiac arrest24 and willingness to perform CPCR is a topic that has received much attention in the literature.25–29
Some communities provide their first responders with Basic Life Support training and an automated external defibrillator, whereas others rely on paramedics trained to provide advanced life support.30 It is not clear whether different approaches to provider training affect survival rates from out of hospital cardiac arrest (OHCA).31,32
So, many literatures have evaluated the efficacy of different methods of CPCR training.33–36
This study includes the evaluation of different methods of CPCR training in different groups of the society. Some studies reported that video self-instruction to be more effective in teaching CPCR performance than the traditional AHA's classroom training method.2,5,37
Díez et al revealed that in comparison to the traditional training method involving an instructor, training G1 in CPCR with voice assist manikin (VAM) improves the quality of some practical CPCR skills.8
This study has 2 dimensions: in 1 aspect, the efficacy of 4 different standard protocols of CPCR training is evaluated, and on the other hand, 3 different groups of the society are compared for learning the CPCR. The attitudes of the participants about CPCR were also compared before and after the course.
Because of different levels of previous knowledge and orientation state about CPCR in these groups, significant differences were observed in pretest theoretical practical scores.
Obviously, the knowledge of medical students about CPCR is more than of other participants, and they achieved better scores at theoretical and practical examinations. G2 even had more knowledge about CPCR compared with general population.
Comparing 4 methods of CPCR training in these 3 groups of the society, it seems that the training workshop using lecture, human model, educational film as well as reference book has more quantitative and qualitative efficacy in CPCR and BLS training in all groups of the study. On the other hand, the lowest efficacy was in workshop using T2 alone.
It seems that practical training using human model beside the educational CPCR film and reference CPCR book has a critical role in course efficacy. In other words, using more and practical facilities such as T1 and T2 besides interactive lecturing increase the efficacy of the course.
Performing a postdelayed theoretical and practical CPCR examination 12 months after the course allowed us to evaluate the long-term efficacy of mentioned 4 methods of CPCR training.
The best persistent method of CPCR training in this study was the 4th one, because in this method, effective facilities such as (T4) human model and practical training were used and the CPCR reference book and educational films were also available for users.
In this study, it was found that the method that was more effective at the course had more long-lasting effects. In fact, presence of educational film and reference book allows the participants to refresh their skills and knowledge and remember more easily the course components.
CPCR training programs need to be developed in different groups of the society. There are substantial challenges to deliver training programs for G3, in contrast to college-based programs. Other methods for CPCR refresher training, such as Internet-based training, also have been advocated but not critically evaluated. Our data also document that a higher educational level is associated with CPCR performance. CPCR training and retraining programs need to vary at different educational levels of the population.
This CPCR course had high and positive effects on participants’ attitude and after the course it was found that the participants were more willing to do CPCR in emergency states. It seems that suitable training of CPCR as well as explaining the key points and its importance and feasibility can improve the individual's attitude about CPCR and decrease the individuals’ fear of performing not suitable CPCR. Such courses that train all society groups lead to more lifesaving attempts in emergency states. On the other hand, suitable training of CPCR points can decline the wrong beliefs about CPCR such as disease transmission and also increase the dare for performing CPCR.
CONCLUSION
Such effective CPCR courses can lead to improve theoretical and practical skills in G1 and G2 and also in G3. On the other hand, the confidence about performing CPCR increased significantly in all groups of the study especially in G3. Considering that the most of the bystanders at emergency states are G3, training this group of the society can be so effective and lifesaving at emergency states.
Study Limitation
This study is observational, and randomization could not be done and further randomized studies may determine the best way to teach CPCR.
Footnotes
Abbreviations: AHA = American Heart Association, CPCR = cardiopulmonary resuscitation, G1 = medical students, G2 = nonmedical students, G3 = general population, T1 = Interactive lecturing workshop using lecture and human model, T2 = Workshop using educational film, T3 = Workshop using lecture, human model as well as educational film, T4 = Workshop using lecture, human model, educational film as well as reference book.
This study was funded by HSR of Medical Education of Shiraz University of Medical Sciences Faculty of Education, Education Development Center.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Zheng Z-J, Croft JB, Giles WH, et al. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001; 104:2158–2163. [DOI] [PubMed] [Google Scholar]
- 2.Braslow A, Brennan RT, Newman MM, et al. CPCR training without an instructor: development and evaluation of a video self-instructional system for effective performance of cardiopulmonary resuscitation. Resuscitation 1997; 34:207–220. [DOI] [PubMed] [Google Scholar]
- 3.McKenna SP, Glendon A. Occupational first aid training: decay in cardiopulmonary resuscitation (CPCR) skills. J Occup Psychol 1985; 58:109–117. [Google Scholar]
- 4.Dracup K, Guzy PM, Taylor SE, et al. Cardiopulmonary resuscitation (CPCR) training: consequences for family members of high-risk cardiac patients. Arch Inter Med 1986; 146:1757. [DOI] [PubMed] [Google Scholar]
- 5.Batcheller AM, Brennan RT, Braslow A, et al. Cardiopulmonary resuscitation performance of subjects over forty is better following half-hour video self-instruction compared to traditional four-hour classroom training. Resuscitation 2000; 43:101–110. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton R. Nurses’ knowledge and skill retention following cardiopulmonary resuscitation training: a review of the literature. J Adv Nurs 2005; 51:288–297. [DOI] [PubMed] [Google Scholar]
- 7.Korttila K, Vertio H, Savolainen K. Importance of using proper techniques to teach cardiopulmonary resuscitation to laymen. Acta Anaesth Scand 1979; 23:235–241. [DOI] [PubMed] [Google Scholar]
- 8.Díez N, Rodríguez-Díez MC, Nagore D, et al. A randomized trial of cardiopulmonary resuscitation training for medical students: voice advisory mannequin compared to guidance provided by an instructor. Simul Healthc 2013; 8:234–241. [DOI] [PubMed] [Google Scholar]
- 9.Bhanji F, Mancini ME, Sinz E, et al. Part 16: Education, Implementation, and Teams 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122:S920–S933. [DOI] [PubMed] [Google Scholar]
- 10.Capucci A, Aschieri D, Piepoli MF, et al. Tripling survival from sudden cardiac arrest via early defibrillation without traditional education in cardiopulmonary resuscitation. Circulation 2002; 106:1065–1070. [DOI] [PubMed] [Google Scholar]
- 11.Pane GA, Salness KA. A survey of participants in a mass CPCR training course. Ann Emerg Med 1987; 16:1112–1116. [DOI] [PubMed] [Google Scholar]
- 12.del Águila JG, López-Rebollo E, Fernández-Valle P, et al. Mass CPCR training. Resuscitation 2013; 84,:S42. [Google Scholar]
- 13.Messmer P, Jones S. Saving lives. An innovative approach for teaching CPCR. Nurs Health Care Perspect 1997; 19:108–110. [PubMed] [Google Scholar]
- 14.Swor R, Compton S, Vining F, et al. A randomized controlled trial of chest compression only CPCR for older adults—a pilot study. Resuscitation 2003; 58:177–185. [DOI] [PubMed] [Google Scholar]
- 15.Todd KH, Braslow A, Brennan RT, et al. Randomized, controlled trial of video self-instruction versus traditional CPCR training. Anna Emerg Med 1998; 31:364–369. [DOI] [PubMed] [Google Scholar]
- 16.Suh JW, Choi JY, Lee TR, et al. A study on attitudes toward and knowledge of cardiopulmonary resuscitation in Korean high school students. J Korean Soc Emerg Med 2012; 23:901–906. [Google Scholar]
- 17.Lynch B, Einspruch EL. With or without an instructor, brief exposure to CPCR training produces significant attitude change. Resuscitation 2010; 81:568–575. [DOI] [PubMed] [Google Scholar]
- 18.Källestedt M-LS, Berglund A, Herlitz J, et al. The impact of CPCR and AED training on healthcare professionals’ self-perceived attitudes to performing resuscitation. Scand J Trauma Resusc Emerg Med 2012; 20:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iwami T, Kitamura T, Nishiyama C, et al. editors. Systematic CPCR Training in Elementary Schools and Students’ Attitudes Toward CPCR and AED Use. Circulation 530 Walnut St, Philadelphia, PA: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 20.Hasani H, Kamali M, Kojuri J, Bordbar S, Reisi H. Comprehensive textbook of CPCR, Jameeneghar publication 84 Nazari St. Enghelab St. Tehran, Iran; 2001. [Google Scholar]
- 21.Stapleton ER. Basic life support cardiopulmonary resuscitation. Cardiol Clin 2002; 20:1–12. [DOI] [PubMed] [Google Scholar]
- 22.Berg RA, Hemphill R, Abella BS, et al. Part 5: adult basic life support 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122:S685–S705. [DOI] [PubMed] [Google Scholar]
- 23.Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPCR overview 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122:S676–S684. [DOI] [PubMed] [Google Scholar]
- 24.Sasson C, Rogers MA, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010; 3:63–81. [DOI] [PubMed] [Google Scholar]
- 25.Axelsson Å, Herlitz J, Ekström L, et al. Bystander-initiated cardiopulmonary resuscitation out-of-hospital. A first description of the bystanders and their experiences. Resuscitation 1996; 33:3–11. [DOI] [PubMed] [Google Scholar]
- 26.McCormack AP, Damon SK, Eisenberg MS. Disagreeable physical characteristics affecting bystander CPCR. Ann Emerg Med 1989; 18:283–285. [DOI] [PubMed] [Google Scholar]
- 27.Brenner B, Kauffman J, Sachter JJ. Comparison of the reluctance of house staff of metropolitan and suburban hospitals to perform mouth-to-mouth resuscitation. Resuscitation 1996; 32:5–12. [DOI] [PubMed] [Google Scholar]
- 28.Ryoo H, Park J, Lee M, et al. Factors affecting public recognition and willingness to perform bystander CPCR in Daegu metropolitan city. J Emerg Med 2012; 43:925. [Google Scholar]
- 29.Na YH, Song KJ, Cho GC, et al. Effect of public re-education in willingness to perform bystander cardiopulmonary resuscitation (CPCR). J Korean Soc Emerg Med 2011; 22:656–661. [Google Scholar]
- 30.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation 2004; 63:233–249. [DOI] [PubMed] [Google Scholar]
- 31.Stiell IG, Nesbitt LP, Pickett W, et al. The OPALS Major Trauma Study: impact of advanced life-support on survival and morbidity. Can Med Assoc J 2008; 178:1141–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nichol G, Stiell IG, Laupacis A, et al. A cumulative meta-analysis of the effectiveness of defibrillator-capable emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med 1999; 34:517–525. [PubMed] [Google Scholar]
- 33.Brennan RT, Braslow A, Batcheller AM, et al. A reliable and valid method for evaluating cardiopulmonary resuscitation training outcomes. Resuscitation 1996; 32:85–93. [DOI] [PubMed] [Google Scholar]
- 34.Cave DM, Aufderheide TP, Beeson J, et al. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools a science advisory from the American Heart Association. Circulation 2011; 123:691–706. [DOI] [PubMed] [Google Scholar]
- 35.Dine CJ, Gersh RE, Leary M, et al. Improving cardiopulmonary resuscitation quality and resuscitation training by combining audiovisual feedback and debriefing∗. Crit Care Med 2008; 36:2817–2822. [DOI] [PubMed] [Google Scholar]
- 36.Reder S, Cummings P, Quan L. Comparison of three instructional methods for teaching cardiopulmonary resuscitation and use of an automatic external defibrillator to high school students. Resuscitation 2006; 69:443–453. [DOI] [PubMed] [Google Scholar]
- 37.Todd KH, Heron SL, Thompson M, et al. Simple CPCR: a randomized, controlled trial of video self-instructional cardiopulmonary resuscitation training in an African American church congregation. Ann Emerg Med 1999; 34:730–737. [DOI] [PubMed] [Google Scholar]


