Abstract
This epidemiological survey in Spain estimates the burden of respiratory syncytial virus (RSV) infection in children up to 5 year of age during a 15-year period (1997–2011).
Observational retrospective survey was conducted by reviewing data of the National Surveillance System for Hospital Data, including >98% of Spanish hospitals. All hospitalizations related to RSV infection for children up to 5 years, reported during 1997–2011 period, were analyzed. Codes were selected by using the International Classification of Diseases 9th Clinical Modification 466.0–466.19, 480.1, and 079.6.
A total of 326,175 and 286,007 hospital discharges for children up to 5 and 2 years of age were reported during the study period. The annual incidence was 1072 and 2413 patients per 100,000, respectively. The average length of hospital stay was 5.7 (standard deviation 8.2) days. Four hundred forty-six deaths were reported; of those, 403 occurred in children <2 years and 355 (80%) occurred in children <12 months of age.
Hospitalization and mortality rates were significantly higher in boys and decrease significantly with age. The higher rate of hospitalization and mortality rates were found in the first year of life.
Annual average cost for National Health Care System was € 47 M with a mean hospitalization cost of €2162. The average length of hospitalization and costs were significantly higher in high-risk children.
RSV infections in children up to 5 year of age still pose a significant health threat in Spain, especially in the infants. The development of preventive, diagnostic, and therapeutic guidelines focused in children with comorbidities may help reduce the hospital and economic burden of the disease.
INTRODUCTION
Bronchiolitis is an acute pediatric disease of the lower respiratory tract. Bronchiolitis is the main cause of hospitalization due to respiratory infection in children <2 years of age. More than half of these hospitalizations are caused by the respiratory syncytial virus (RSV). A large proportion of RSV infections lead to hospitalizations, particularly when specific risk factors such as prematurity, heart, or lung disease and other chronic illnesses are present.1–4
RSV is one of the principal agents that cause severe lower respiratory tract disease both in children and adults.5,6 It is easily transmitted through respiratory secretions or through contaminated fomites. Because of this high infectivity the majority of the population suffers from RSV infection in early childhood. In regions with a temperate climate such as Spain, RSV infections occur in annual outbreaks starting toward the end of autumn and lasting till spring.1,5
The primary RSV infection does not result in complete immunity and secondary reinfections that present with different degrees of respiratory problems are common. It has been suggested that RSV infection is associated with chronic respiratory illness, particularly with bronchial hyperresponsiveness, in children <2 years of age.5,7 These chronic respiratory problems may last for >10 years after the primary infection.5
At present, no effective vaccine exists to prevent RSV infection. Instead, the most effective way to reduce the probability of virus transmission is a high level of hygiene (washing hands, etc). Apart from these health habits, a pharmacological intervention with monoclonal antibodies (palivizumab) in high-risk infants has proven to be effective preventing and reducing the burden of RSV associated hospitalizations among infants.8
Despite the high prevalence of bronchiolitis due to RSV and the increase in associated hospitalizations, only a few regional studies describe the incidence of hospitalizations related to RSV bronchiolitis in Spain.9,10 An assessment of the burden of hospitalizations related to RSV infections on a country level is missing. The objective of this study is to estimate the incidence of hospitalizations associated with bronchiolitis and the associated costs from 1997 to 2011 in Spain.
MATERIALS AND METHODS
A retrospective study using the national information system for hospital data (Conjunto Mínimo Básico de Datos; CMBD) from the Ministry of Health was performed. This system uses clinical codes from the Spanish version of the International Classification of Diseases 9th Clinical Modification (ICD-9-MC) and includes an estimated 98% of admissions in public hospitals and 99.5% of the Spanish population.11–13 CMBD database was established in 1997.
All hospital discharges for bronchiolitis in children under 5 years of age (ICD-9-CM: 466, acute bronchitis and bronchiolitis; 466.0, bronchitis, acute or subacute: fibrinous, membranous, pneumococcal, purulent, septic, viral with tracheitis, Croupous bronchitis, Tracheobronchitis acute—excludes: acute bronchitis with chronic obstructive pulmonary disease (491.22); 466.1, acute bronchiolitis: bronchiolitis (acute), capillary pneumonia; 466.11, acute bronchiolitis RSV; 466.19, acute bronchiolitis other; 480.1, pneumonia due to RSV; 079.6, RSV infection) any listed diagnosis position, among children <5 years of age reported during a 15-year period (January 1, 1997, through December 31, 2011, available data) were obtained.
For each case, specific data were gathered on age, sex, average length of hospitalization, and comorbidity. Groups of age for study were 0, 1, 2, 3, 4, <2, and <5 years old. Comorbidities were defined as ICD-9-CM code—765.0–765.29 prematurity, from extreme immaturity to <37 weeks of gestation; ICD-9-CM code—770.0–770.9 bronchopulmonar dysplasia (BPD), including congenital pneumonia, infective pneumonia acquired prenatally—excluding: pneumonia from infection acquired after birth (480.0–486) and including fetal and newborn aspiration, interstitial emphysema and related conditions, pulmonary hemorrhage, pulmonary atelectasis, other and unspecified atelectasis, transitory tachypnea of newborn, chronic respiratory disease arising in the perinatal period, chronic respiratory disease arising in the perinatal period, other respiratory problems after birth, unspecified respiratory condition of fetus and newborn; ICD-9-CM code—758.0–758.9: congenital defects with cardiac affectation, including Down syndrome, Patau syndrome, Edwards syndrome, autosomal deletion syndrome, balanced autosomal translocation in normal individual, other conditions due to autosomal anomalies, Gonadal dysgenesis, Klinefelter syndrome, other conditions due to chromosome anomalies, conditions due to anomaly of unspecified chromosome; and ICD-9-CM code—745.0–747.9: congenital cardiopathies.
Statistical Methods
The annual incidence of hospitalizations admissions (per 100,000 population), average length of stay in the hospital (ALOS), mortality rate (per 100,000 population), and case-fatality rate (%) were calculated using as denominator data on the corrected population figures obtained. The distribution by age of the population covered in this study is considered to be equal to the general population.
Differences in proportions were assessed by the chi-square test and analysis of variance, and post-hoc Bonferroni correction was used for multiple comparisons. Poisson regression was used to assess differences in the hospitalization rate during the study period.
The cost to the health care system of these hospitalizations is estimated from the Ministry of Health. The cost was calculated by considering the diagnostic cost group, the total cost, and the number of discharges. The diagnostic cost group was based on the diagnosis-related group for hospitalized patient depending on discharge ICD classification, age, sex, and resources consumption. Each group has similar weight in hospital costs and can be apply to each related patient. The diagnosis-related group calculations are made by 3M™ Core Grouping Software. 3M Health Information Systems. 3M HIS Murray, UT 84123 USA.14 Estimated costs are reported since 2002 when Euro was introduced as currency in Spain.
In all test the significance level used was P < 0.05. Statistical analyses were performed using the Statistical Package for Social Sciences (IBM SPSS/PASW for windows, version 19.0; SPSS, Chicago, IL) and STATA 11 (StataCorp LP, College Station, TX).
This study does not need ethical approval by an ethics committee, given the characteristics of the study and the current legislation. Patient information is available for scientific purposes, being fully guaranteed the patient anonymity by preserving the personal identification data of the patient separate from clinical data.
RESULTS
A total of 326,175 hospital discharges due to bronchiolitis in children <5 year of age were reported during the 15-year study period (1072 hospitalizations/100,000 children <5 year of age). Of those, 286,007 occurred in children up to 2 years old (hospitalization rate of 2413/100,000). Mean age was 5.8 months (standard deviation [SD] 11) and 59.2% of the patients were male. The average length of hospital stay was 5.7 (SD 8.2) days and 5.9 (SD 8.7) in children up to 5 and 2 years of age, respectively. The 8.6% of the patients were readmitted in the following month due to a cause related to bronchiolitis. These figures did not change significantly during the study period.
Bronchiolitis was reported as the primary cause of hospitalization in 85% of the patients, being acute respiratory failure (2.5%), pneumonia (1.6%), bronchopneumonia (0.5%), rotavirus (0.5%), and acute urinary infection (0.3%) the main diagnoses in the remaining 15%. An important seasonality was observed, with 76% of the patients occurring between November and March.
Table 1 shows the number and hospitalization rate for bronchiolitis by year of age. The highest incidence of hospitalization is shown in the first year of life with a hospitalization rate per 100,000 children <12 months of 4136 (95% confidence interval [CI] 4120–4153). Then it decreases significantly with age (P < 0.001).
TABLE 1.
Hospitalization Rate (per 100,000) Due to RSV Bronchiolitis in Children <5 Years Old, 1997–2011
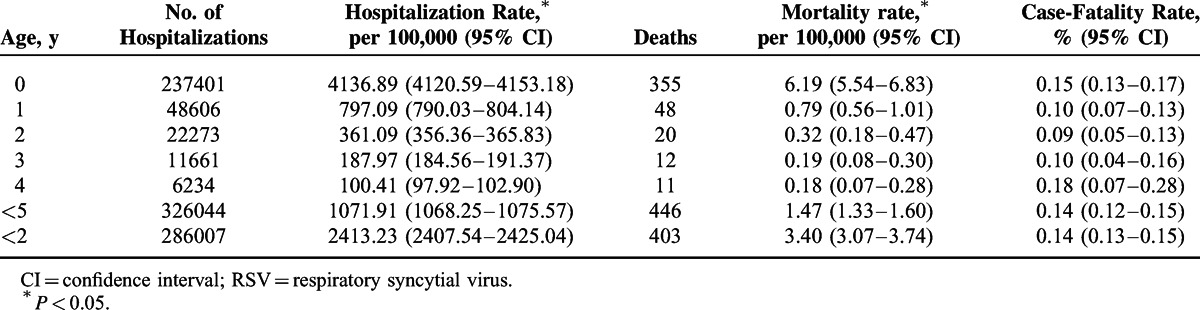
During the 15-year study period, a total of 446 deaths were reported. Of those, 355 (80%) were in patients of age <12 months, 48 (11%) were 1 years of age, 20 (4.5%) of age 2, 12 (2.7%) of age 3, and 11 (2.5%) were 4 years of age. The mortality rate was 1.47 deaths per 100,000 (95% CI 1.33–1.60) in children <5 years old and 3.40 deaths per 100,000 (95% CI 3.07–3.74) in children <2 years old (Table 1). The case-fatality rate was 0.14%, ranging from 0.11% to 0.18%.
Figure 1 shows hospitalization rate for bronchiolitis by gender during the 15 years of study. Hospitalization rates significantly increased until 2000 and since then slightly decreased. Hospitalization rates were significantly higher in boys both in children <5 years old (1232 vs 898/100,000, respectively; P < 0.038) and in children <2 years old (2731 vs 2019/100,000, respectively; P < 0.029). Mortality rates were also significantly higher in boys (1.53 vs 1.38/100,000; P < 0.022 in children <5 and 3.65 vs 3.13/100,000, P < 0.028 in children <2 years old, respectively). Case-fatality rate did not differ by gender.
FIGURE 1.
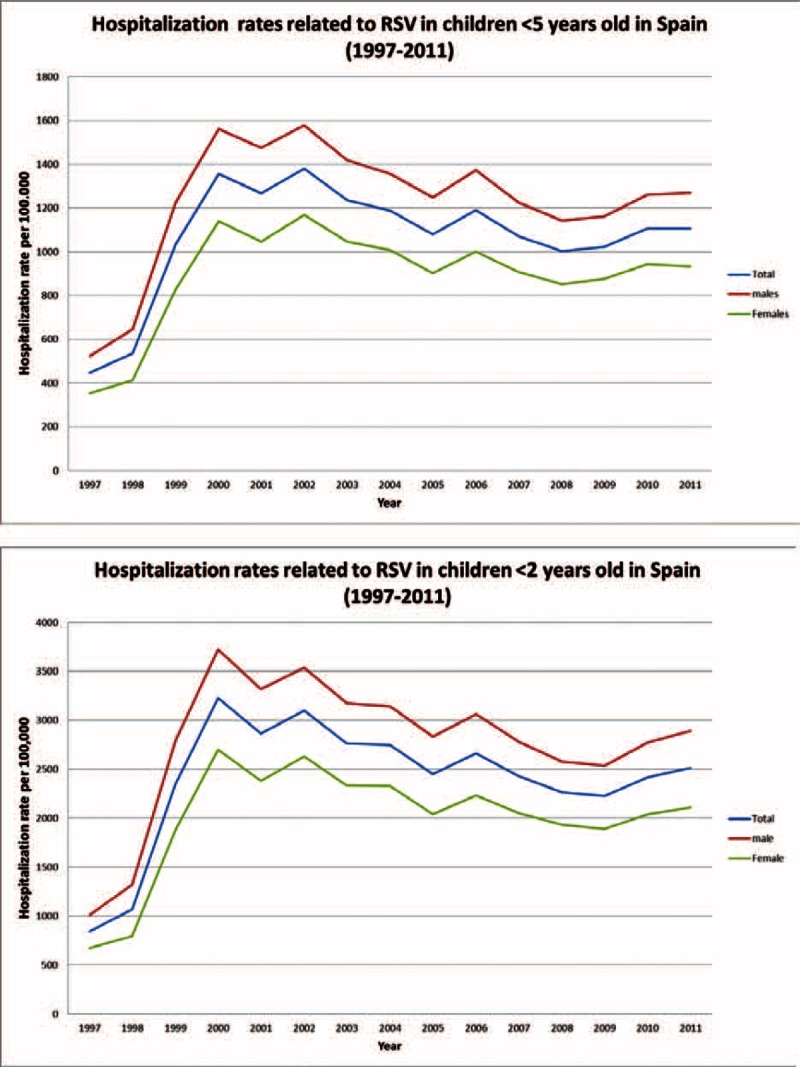
Hospitalization rates related to respiratory syncytial virus (RSV) bronchiolitis in children <5 years old and <2 years old in Spain (1997–2011).
Figure 2 shows the hospitalization rate per Autonomous Region in Spain. The highest rates in children <5 years old were found in Aragon (1520/100,000), Catalonia (1419/100,000), and Extremadura (1455/100,000), whereas the lowest rates were found in Cantabria (768/100,000), Basque Country (680/100,000), and Murcia (795/100,000). The highest rates in children <2 years old were found in Extremadura (3474/100,000), Asturias (3274/100,000), and Aragon (3095/100,000), whereas the lowest rates were found in Basque Country (1548/100,000), La Rioja (1794/100,000), and Murcia (1839/100,000).
FIGURE 2.
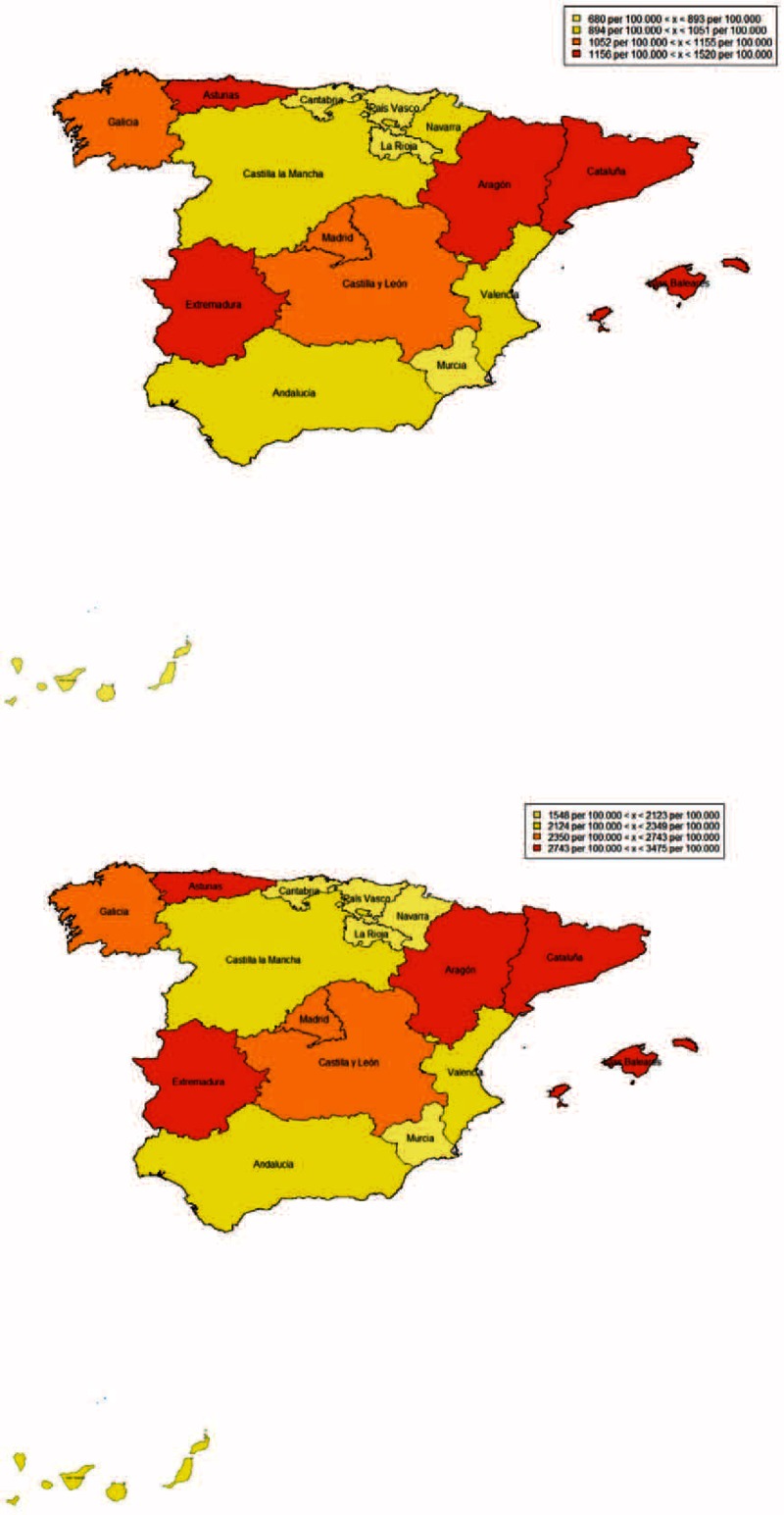
Regional hospitalization rates due to respiratory syncytial virus (RSV) bronchiolitis in children <5 years old and <2 years old in Spain (1997–2011).
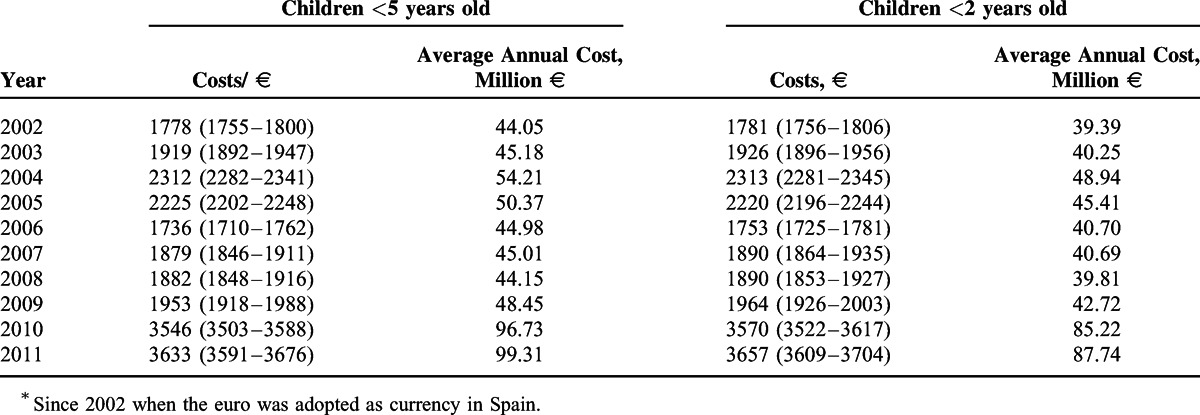
Annual average cost for National Health Care System for bronchiolitis requiring hospitalization was € 47 M with a mean hospitalization costs of €2162 in children up to 5 years old. This figures reached an annual average cost of € 41 M and a mean hospitalization costs of €2166 in children up to 2 years old. Table 2 shows the average unit and global cost for hospitalization since 2002, when the euro was introduced in Spain.
TABLE 2.
Costs of RSV Bronchiolitis Hospitalizations in Children <5 Years Old and <2 Years Old in Spain Since 2002∗
Of the 315,872 patients under the age of 5 hospitalized due to bronchiolitis during the study period, 3.2% (n = 10,303) presented at least 1 of the studied comorbidities; congenital cardiopathies 2.3% (n = 7652), congenital defects with cardiac affectation 0.7% (n = 2325), prematurity 0.3% (n = 1011), and BPD 1% (n = 3114). Of the 286,007 patients under the age of 2 hospitalized due to bronchiolitis during the study period, 3.3% (n = 9451) presented at least 1 of the studied comorbidities; congenital cardiopathies 2.5% (n = 7106), congenital defects with cardiac affectation 0.7% (n = 1900), prematurity 0.4% (n = 1010), and BPD 1.1% (n = 3048).
Table 3 compares ALOS and costs of hospitalizations during the study period in presence or not of the predefined comorbidities. The ALOS for congenital cardiopathies, congenital defects with cardiac affectation, prematurity, and BPD were significantly higher than non–high-risk groups. Costs were also significantly higher in the comorbidity groups.
TABLE 3.
ALOS and Cost of Hospitalizations Due to RSV Bronchiolitis in Risk Groups
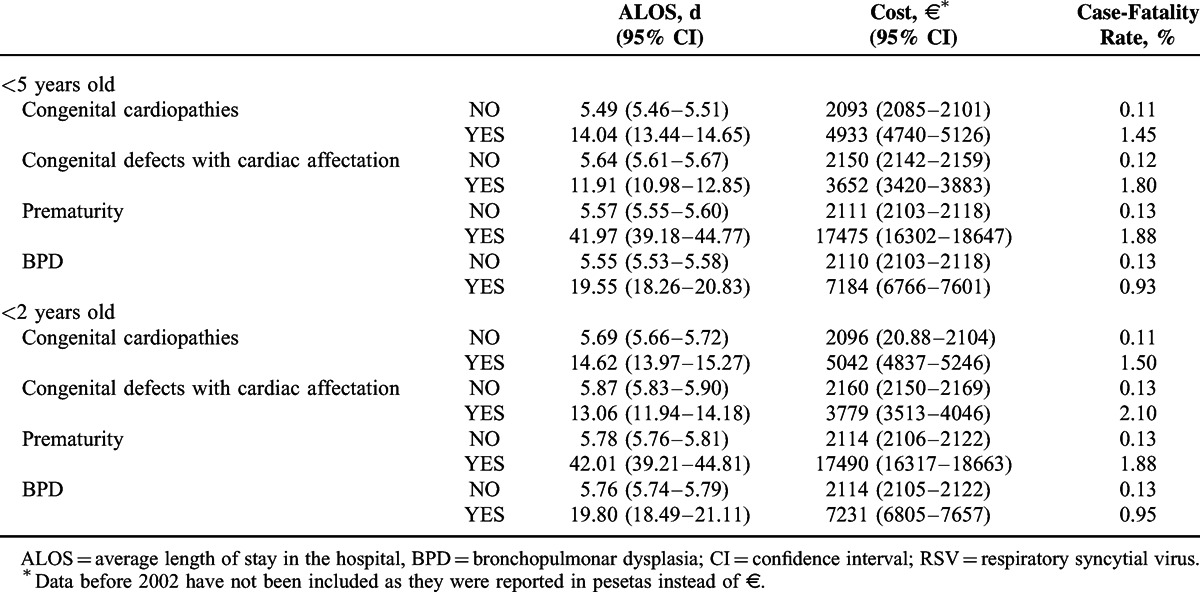
Of the 446 deaths reported in hospitalized children up to 5 years old, 111 (25%) presented at least 1 of the predefined comorbidities. This percentage reaches 26.6% (107/403) when only considering children <2 years old. For all categories and comorbidities, the ALOS and costs were significantly higher when compared with non–high-risk children.
DISCUSSION
The objective of this retrospective epidemiology study was to show the hospitalization burden of severe bronchiolitis in Spain and to highlight the impact in public health and high costs to the National Health Care System of bronchiolitis in young children, especially in children up to 5 years of age. The hospitalization rate of bronchiolitis-related hospitalizations in children up to 5 years old is 100 times the hospitalization rate of meningococcal meningitis,15 400 times pneumococcal meningitis,16 40 times meningococcal infection,17 or 20 times rotavirus infection,18 in the same group of age in similar periods in Spain. Four children up to 12 months of age in every 100 were hospitalized due to bronchiolitis during the study period. In addition, RSV contributes to worsen other pathologies. A 6-year prospective study conducted in children <14 years old with community-acquired pneumonia in Madrid show that RSV has an important role in community-acquired pneumonia of children requiring hospitalization.19
Our hospitalization rates were similar to those reported in England for children up to 1 year of age (24.2/1000)20 and lower to those reported in preterm infants in Italy (4.70/100 person-years)21 or Canada, with an overall hospitalization rate for RSV of 3.6% for infants of 33 to 35 weeks of gestational age.22 Contrary to hospitalization data in the United States, with no significant difference between 1997 and 2006,23 hospitalization rates varied in Spain. They significantly increased from 1997 to 2000, slightly decreased since 2000 and increased again since 2010. Low rates in 1997–1999 period may be influenced by the recent implementation of the national information system for hospital data in 1997 and variations in coding practices for bronchiolitis diagnosis. Consistently with previously published data in Germany, France, and Canada, our date show that the hospitalization and mortality rate were significantly higher in male.22,24–25 Several studies showed that males develop respiratory tract infections more frequently than females, except for sinusitis, otitis externa, and probably tonsillitis. Anatomic, lifestyle, behavioral, and socioeconomic differences between males and females may explain these differences.26,27 Taking into account that our study is restricted to patients up to 5 years old, the most plausible explanation seems to be the gender differences in the anatomy and physiology of the pediatric airway. There is evidence that the peripheral airways are disproportionately narrower during the early years of life in males, which may predispose for lower respiratory tract infections.28
Although the case-fatality rate of bronchiolitis hospitalizations is low—0.14%—because of the high incidence there are 30 deaths per year. This case-fatality rate increases significantly in our study among the high-risk groups. This is consistent with different studies showing that in children with RSV infection and underlying diseases, the illness severity is higher than in healthy children.29,30 Chronic disease per se is a risk factor for bronchiolitis related hospitalizations.31
Palivizumab is a humanized monoclonal antibody directed against the F protein of RSV. It is the only licensed product to prevent severe RSV disease in high-risk children. Palivizumab may have a role in the prevention of severe lower respiratory infection by RSV in patients with comorbidity.32,33 The introduction of palivizumab in prematures diminished hospitalization for RSV bronchiolitis, oxygen need, length of hospital stay, and mechanical ventilation.34 The strict fulfillment of prophylactic recommendations against RSV is the only protective factor that can be modulated to decrease the acute respiratory infection hospital admission rate.35 In otherwise healthy preterm infants, palivizumab treatment resulted in a significant reduction in wheezing days during the first year of life, even after the end of treatment.36
Some studies have shown the cost-effectiveness of palivizumab against severe RSV disease requiring hospitalization among preterm infants and other high-risk infants in Spain.37–39
Hospitalization due to bronchiolitis in children up to 5 years old impose to the National Health Care System 47 M € each year, much higher for example than the 5 M € per year for meningococcal infection in general population.15 The cost for the emergency department expenses of bronchiolitis in Spain is estimated to add up to about €20 million per year.40
There is a significant increase in costs in 2010 and 2011 comparing with the previous years. In this point authors are just reporting estimations from the Ministry of Health and have no explanation for this 2-fold increase.
The cost per hospitalization significantly increased in the high-risk groups: congenital cardiopathies, congenital defects with cardiac affectation, prematurity, and BPD. Our results were consistent with those published in RSV hospitalization in moderately prematurely born infants, that was associated with increased health-related cost of care.41
This study has some limitations derived from the use of CMBD. The reliability of the CMBD depends on the quality of the discharge report and the clinical history, as well as the codification process variables. Quality controls have been done to assess the validity of CMBD and the codification process has improved since 2001.42 Nevertheless, CMBD can be considered as a useful tool for this approach.
Studies focused in the epidemiology and the incidence of bronchiolitis are needed to evaluate current and future preventive measures implementation. Despite current preventive and therapeutic measures available to control acute bronchiolitis, the burden of hospitalizations in our country is very important. The development of more effective preventive strategies, especially for high-risk children (ie, specific indications of palivizumab) is needed. Efforts to enhance surveillance should be continued.
Acknowledgments
The authors acknowledge the support received from Subdirección General del Instituto de Información Sanitaria in providing the information.
Footnotes
Abbreviations: RSV = respiratory syncytial virus, ICD-9-CM = International Classification of Diseases 9th Clinical Modification, SD = standard deviation, BPD = bronchopulmonar dysplasia, ALOS = average length of stay in the hospital.
The cathedra “Evaluación de Resultados en Salud, Rey Juan Carlos University” is sponsored by Abbvie.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Ochoa Sangrador C. González de Dios J y Grupo de Revisión del Proyecto aBREVIADo (BRonquiolitis-Estudio de Variabilidad, Idoneidad y Adecuación) Conferencia de Consenso sobre bronquiolitis aguda (II): epidemiología de la bronquiolitis aguda. Revisión de la evidencia científica. An Pediatr (Barc) 2010; 72:222e1–222e26. [DOI] [PubMed] [Google Scholar]
- 2.Zhou H, Thompson WW, Viboud CG, et al. Hospitalizations associated with influenza and respiratory syncytial virus in the United States, 1993–2008. Clin Infect Dis 2012; 54:1427–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kristensen K, Hjuler T, Ravn H, et al. 1 chronic diseases, chromosomal abnormalities, and congenital malformations as risk factors for respiratory syncytial virus hospitalization: a population-based Cohort Study. Clin Infect Dis 2012; 54:810–817. [DOI] [PubMed] [Google Scholar]
- 4.Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet 2010; 375:1545–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Welliver RC. Respiratory syncytial virus and other respiratory viruses. Pediatr Infect Dis J 2003; 22:S6–12. [DOI] [PubMed] [Google Scholar]
- 6.Blanken MO, Rovers MM, Molenaar JM, et al. Neonatal Network Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N Engl J Med 2013; 368:1791–1799. [DOI] [PubMed] [Google Scholar]
- 7.Falsey AR, Hennessey PA, Formica MA, et al. Walsh EEPh Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med 2005; 352:1749–1759. [DOI] [PubMed] [Google Scholar]
- 8.Figueras Aloya J, López Sastre J, Medrano López C, et al. Consenso multidisciplinar español sobre la profilaxis de la infección respiratoria pediátrica por virus respiratorio sincitial. An Pediatr (Barc) 2008; 69:63–71. [DOI] [PubMed] [Google Scholar]
- 9.Díez Domingo J, Ridao López M, Úbeda Sansano I, et al. Incidencia y costes de la hospitalización por bronquiolitis y de las infecciones por virus respiratorio sincitial en la Comunidad Valenciana. Años 2001 y 2002. An Pediatr (Barc) 2006; 65:325–330. [DOI] [PubMed] [Google Scholar]
- 10.Vicente D, Montes M, Cilla G, et al. Hospitalization for respiratory syncytial virus in the paediatric population in Spain. Epidemiol Infect 2003; 131:867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ministerio de Sanidad y Consumo. Clasificación internacional de enfermedades 9 revisión, modificación clínica. 1994. [Google Scholar]
- 12.Instituto Nacional de la Salud. Subdirección General de Coordinación Administrativa. Conjunto Mínimo Básico de Datos. Hospitales del INSALUD2001. Madrid: 2002. http://www.ingesa.msc.es/. [Google Scholar]
- 13.Rivero Cuadrado A. El conjunto mínimo básico de datos en el SNS: inicios y desarrollo actual. Rev Fuentes Estadísticas 2000; 49:18-19. http://www.ingesa.msc.es/estadEstudios/documPublica/pdf/CMBD-2001.pdf Accessed January 18. 2014. [Google Scholar]
- 14.Schreyögg J, Stargardt T, Tiemann O, et al. Methods to determine reimbursement rates for diagnosis related groups (DRG): a comparison of nine European countries. Health Care Manag Sci 2006; 9:215–223. [DOI] [PubMed] [Google Scholar]
- 15.Gil-Prieto R, García-García L, Alvaro-Meca A, et al. The burden of hospitalizations for meningococcal infection in Spain (1997–2008). Vaccine 2011; 29:5765–5770. [DOI] [PubMed] [Google Scholar]
- 16.Gil Prieto R, San Román Montero J, Gómez Alejandre C, et al. Epidemiology of pneumococcal meningitis hospitalizations in pediatric population in Spain (1998–2006). Vaccine 2009; 27:2669–2673. [DOI] [PubMed] [Google Scholar]
- 17.Montero JM, Prieto RG, Alejandre CG, et al. Hospital admissions for meningococcal infection in Spain (1997–2005). J Infect 2009; 58:15–20. [DOI] [PubMed] [Google Scholar]
- 18.Gil-Prieto R, San Martín M, de Andrés AL, et al. Hospital-acquired rotavirus infections in Spain over a ten-year period (1998–2007). Hum Vaccin 2009; 5:748–753. [DOI] [PubMed] [Google Scholar]
- 19.LG.García-García ML, Calvo C, Pozo F, et al. Spectrum of respiratory viruses in children with community-acquired pneumonia. Pediatr Infect Dis J 2012; 31:808–813. [DOI] [PubMed] [Google Scholar]
- 20.Murray J1, Bottle A1, Sharland M2, et al. Medicines for Neonates Investigator Group Risk factors for hospital admission with RSV bronchiolitis in England: a population-based birth cohort study. PLoS One 2014; 9:e89186.doi: 10.1371/journal.pone.0089186. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pezzotti P, Mantovani J, Benincori N, et al. Incidence and risk factors of hospitalization for bronchiolitis in preterm children: a retrospective longitudinal study in Italy. BMC Pediatr 2009; 9:56.doi: 10.1186/1471-2431-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carbonell-Estrany X, Figueras-Aloy J, Law BJ. Infección Respiratoria Infantil por Virus Respiratorio Sincitial Study Group; Pediatric Investigators Collaborative Network on Infections in Canada Study Group Identifying risk factors for severe respiratory syncytial virus among infants born after 33 through 35 completed weeks of gestation: different methodologies yield consistent findings. Pediatr Infect Dis J 2004; 23 (11 Suppl):S193–S201. [DOI] [PubMed] [Google Scholar]
- 23.Stockman LJ, Curns AT, Anderson LJ, et al. Respiratory syncytial virus-associated hospitalizations among infants and young children in the United States, 1997–2006. Pediatr Infect Dis J 2012; 31:5–9. [DOI] [PubMed] [Google Scholar]
- 24.Liese JG, Grill E, Fischer B, et al. Munich RSV Study Group Incidence and risk factors of respiratory syncytial virus-related hospitalizations in premature infants in Germany. Eur J Pediatr 2003; 162:230–236. [DOI] [PubMed] [Google Scholar]
- 25.Gouyon JB, Rozé JC, Guillermet-Fromentin C, et al. Hospitalizations for respiratory syncytial virus bronchiolitis in preterm infants at <33 weeks gestation without bronchopulmonary dysplasia: the CASTOR study. Epidemiol Infect 2013; 141:816–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Falagas ME1, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Respir Med 2007; 101:1845–1863. [DOI] [PubMed] [Google Scholar]
- 27.Simoes EA. Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. J Pediatr 2003; 143:S118–S126. [DOI] [PubMed] [Google Scholar]
- 28.Gupta R, Helms PJ, Jolliffe IT, et al. Seasonal variation in sudden infant death syndrome and bronchiolitis—a common mechanism? Am J Respir Crit Care Med 1996; 154 (2 Pt 1):431–435. [DOI] [PubMed] [Google Scholar]
- 29.Moreno-Perez D, Calvo C. Five Study Group Epidemiological and clinical data of hospitalizations associated with respiratory syncytial virus infection in children under 5 years of age in Spain: FIVE multicenter study. Influenza Other Respir Viruses 2014; 8:209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Figueras-Aloy J, Carbonell-Estrany X, Quero-Jiménez J, et al. FLIP-2 Study: risk factors linked to respiratory syncytial virus infection requiring hospitalization in premature infants born in Spain at a gestational age of 32 to 35 weeks. Pediatr Infect Dis J 2008; 27:788–793. [DOI] [PubMed] [Google Scholar]
- 31.Kristensen K, Hjuler T, Ravn H, et al. Chronic diseases, chromosomal abnormalities, and congenital malformations as risk factors for respiratory syncytial virus hospitalization: a population-based cohort study. Clin Infect Dis 2012; 54:810–817. [DOI] [PubMed] [Google Scholar]
- 32.Sánchez-Solis M, Gartner S, Bosch-Gimenez V, et al. Is palivizumab effective as a prophylaxis of respiratory syncytial virus infections in cystic fibrosis patients? A meta-analysis. Allergol Immunopathol (Madr) 2013; 43:298–303. [DOI] [PubMed] [Google Scholar]
- 33.Rodriguez R, Ramilo O. Respiratory syncytial virus: how, why and what to do. J Infect 2014; 68 suppl 1:S115–S118. [DOI] [PubMed] [Google Scholar]
- 34.Hervás D, Reina J, Yañez A, et al. Epidemiology of hospitalization for acute bronchiolitis in children: differences between RSV and non-RSV bronchiolitis. Eur J Clin Microbiol Infect Dis 2012; 31:1975–1981. [DOI] [PubMed] [Google Scholar]
- 35.Medrano López C, García-Guereta L. CIVIC Study Group Community-acquired respiratory infections in young children with congenital heart diseases in the palivizumab era: the Spanish 4-season civic epidemiologic study. Pediatr Infect Dis J 2010; 29:1077–1082. [DOI] [PubMed] [Google Scholar]
- 36.Blanken MO, Rovers MM, Molenaar JM, et al. Dutch RSV Neonatal Network Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N Engl J Med 2013; 368:1791–1799. [DOI] [PubMed] [Google Scholar]
- 37.Nuijten MJ, Wittenberg W. Cost effectiveness of palivizumab in Spain: an analysis using observational data. Eur J Health Econ 2010; 11:105–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Resch B, Sommer C, Nuijten MJ, et al. Cost-effectiveness of palivizumab for respiratory syncytial virus infection in high-risk children, based on long-term epidemiologic data from Austria. Pediatr Infect Dis J 2012; 31:e1–e8. [DOI] [PubMed] [Google Scholar]
- 39.Nuijten M, Lebmeier M, Wittenberg W. Cost effectiveness of palivizumab for RSV prevention in high-risk children in the Netherlands. Med Econ 2009; 12:291–300. [DOI] [PubMed] [Google Scholar]
- 40.Garcia-Marcos L, Valverde-Molina J, Pavlovic-Nesic S, et al. the BCOST group Pediatricians’ attitudes and costs of bronchiolitis in the emergency department: a prospective multicentre study. Pediatr Pulmonol 2014; 49:1011–1019. [DOI] [PubMed] [Google Scholar]
- 41.Shefali-Patel D, Paris MA, Watson F, et al. RSV hospitalization and healthcare utilisation in moderately prematurely born infants. Eur J Pediatr 2012; 171:1055–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peiro S, Librero J. Evaluación de la calidad a partir del conjunto mínimo de datos básicos al alta hospitalaria. Rev Neurol 1999; 29:651–661. [PubMed] [Google Scholar]


