Abstract
To compare the incidence and relative risk of falls between adults with and without diabetes, and to prospectively assess the role of history of severe hypoglycemia in the putative relationship between diabetes and falls in younger and older people, respectively.
The National Health Insurance Research Database in Taiwan was used in this cohort study. Diabetic cases (with and without history of severe hypoglycemia) and nondiabetic people were followed from 2000 to 2009. There were 31,049 people enrolled in each of the 3 groups. Subdistribution hazard ratio (sHR) of falls was estimated with considering death as a competing risk by using Fine and Gray method. Demographic characteristics, diabetes-related complications, and comorbidities associated with falls were adjusted in multivariable Cox regression model.
As compared to nondiabetic people, adjusted sHR was 1.13 for diabetes without history of severe hypoglycemia (DwoH) and 1.63 for diabetes with history of severe hypoglycemia (DwH), respectively. DwH group was associated with a higher risk than DwoH (adjusted sHR = 1.57). All of the excessive risks were more pronounced in people younger than 65 years old than in older people.
Patients with diabetes had increased risk of falls. Severe hypoglycemia was further associated with a higher risk in diabetes, the increased hazards were particularly pronounced in people younger than 65 years old. Because falls in younger people may result in a greater economic and social loss, our study call for proper attentions to prevention of falls in younger patients (<65 years old) with diabetes.
INTRODUCTION
Fall is the second leading cause of accidental deaths worldwide.1 It accounts for 11% of unintentional injury-related deaths and leads to losses of over 15 million disability-adjusted life-years annually.2 Nonfatal injuries due to falls such as fractures, lacerations, and head trauma usually result in physical activity restrictions, functional declines, and precipitate to impaired societal relationship in the elderly.3,4
An increased incidence of falls has been reported among older patients with diabetes.5–7 The excessive risk of falls in diabetes had been associated with poor glycemic control (glycosylated hemoglobin A1c [HbA1c] >7%) and higher prevalence of complications including visual impairment and peripheral neuropathy.8,9 Although intensive glycemic control may reduce or delay the onset of eye complications or neuropathy,10 a lower level of HbA1c is associated with a higher incidence of severe hypoglycemia.11,12 Some studies argued that hypoglycemic events were related to an increased risk of falls or fall-related fractures,13 but such relation has still been inconclusive.14–16 Whether a history of hypoglycemia precipitates patients with diabetes to fall is a crucial issue from the fall prevention point of view.
The risk of falls has been extensively studied in the elderly population, but little attention has been paid to the middle-aged and younger populations.17 As a rising incidence and prevalence of diabetes in younger age groups is emerging, information on the risk of diabetes-related falls in younger diabetes would help reduce the overall health burdens related to falls in diabetic populations.
We therefore conducted a large-scale cohort study to compare the incidence and relative risk of falls between adults with and without diabetes. To further assess the role of history of severe hypoglycemia in the putative relationship between diabetes and falls, we further categorized patients with diabetes into 2 groups according to their history of severe hypoglycemia. An age stratified analysis was conducted to elucidate whether the potential effects of diabetes and severe hypoglycemia vary with age.
MATERIALS AND METHODS
Data Source
Data of this study were retrieved from Taiwan's National Health Insurance Research Database (NHIRD), which stores beneficiary's records and medical claim data of the National Health Insurance (NHI). NHI is provided by the Taiwanese government, it universally covers medical insurance for almost all (>97%) citizens (the prisoners and military personnel exempted).18 The NHIRD is composed of several parts, including inpatient and outpatient medical claims, basic properties of hospitals, and demographic characteristics of the beneficiaries. To ensure the accuracy of the claims, the Bureau of NHI performs quarterly expert reviews on a random sample of ambulatory and inpatient claims.19 Individual person and institution cannot be identified under the protection of encrypted identification number. Full review by Institutional Review Board was exempted because the procedure of encrypting the identification number makes it impossible to identify individuals. Access to the NHIRD datasets is approved by the National Health Research Institutes Review Committee.
Study Design and Subjects
This was a cohort study in which 2 groups of patients with diabetes and 1 reference group of nondiabetes were followed from 2000 to 2008.
The study sample was originated from a previous study, and details of the sample selection flow were addressed previously.20 In brief, the diabetic group included all prevalent cases who had at least 2 outpatient visits for diabetes in 2000, and the nondiabetic group were age- and sex-matched beneficiaries registered in 2000 and had never been diagnosed with diabetes from 1997 to 2000.
An individual was classified as a prevalent patient with diabetes if he or she had sought for medical care with a diagnosis of diabetes (International Classification of Diagnosis, 9th version, Clinical Modification [ICD9-CM]: 250 or A-code: A181) at any time in 2000 and then experienced 1 or more additional diagnoses for diabetes within the subsequent 12 months. The first and the last date of outpatient visits must be at least 30 days apart to avoid the accidental inclusion of miscoded patients. We excluded those who were admitted to the hospitals for any malignant cancer (ICD-9CM: 140-208) or any diagnoses of accidents during the period from 1997 to the date of first clinical visit for diabetes in 2000 (index date).
In this study, severe hypoglycemia was defined by ever presence of ICD9-CM codes of 250.3, 250.8, 251.0, 251.1, 251.2 in outpatient and inpatient visits before the index date. Diabetes with history of severe hypoglycemia group (DwH) and diabetes without history of severe hypoglycemia group (DwoH) were selected from the patients with diabetes. To avoid the potential of over-power, we selected a random sample of DwoH and reference group, respectively from the populations (ie, N = 456,275 for DwoH, N = 590,601 for reference group). The simple random sampling method was used to select study samples, of which, the distributions of basic characteristics (included variables listed in Table 1) were similar to those of the populations. The “DwH group” included a total of 31,049 patients with diabetes who had experienced at least 1 episode of severe hypoglycemia from January 1, 1997 to their index date. The “DwoH group” included a random sample of patients with diabetes who had no history of severe hypoglycemia (n = 31,049). The “reference group” in this study was also an equal-sized random sample selected from all nondiabetic individuals (n = 31,049).
TABLE 1.
Characteristics of the Study Subjects

Follow-Up
Index date for the patient with diabetes was the date of initial diagnosis of diabetes in 2000. For the reference group, it was January 1, 2000, or the first date of enrollment to NHI or if he/she enrolled after January 1, 2000. Follow-up period began from patient's index date to the occurrence of the following events whichever come first: the date of the first hospitalization due to falls, the date of attrition from the insurance, or December 31, 2008.
Outcome and Covariates
Only the falls needed admission to hospitals were identified as outcome events. The first occurrence of hospitalization due to falls was recognized as a fall-related diagnosis code noted in discharge diagnosis during the follow-up period. These codes were identified by listed external codes in ICD9-CM: E880.1, E880.9, E881.0, E883.9, E884.2, E884.6, E884.9, E885, E886.0, E887, E888, and E917.7. However, we cannot further distinguish between the falls occurring before or during hospitalizations.
Some other diabetes-related complications and comorbidities associated with falls which occurred between January 1, 1997 and the index date were identified by ICD-9CM codes, including obesity (278), mental disorders (290–319), neurological disorders (250.6, 337.1, 354, 355, 357.2, 358.1, 356.8, 430–432, 433, 434, 435, 436, 437, 438, 713.5, 729.2, 707, 730), cardiovascular disorders (250.7, 398.91, 401–405, 410–414, 425, 426–427, 428, 429.1, 429.2, 429.3, 440–448, 451, 452, 453, 454, 458, 459, 707, 785.4, 885–887, 895–897), endocrine disorders (259.4, 259.8, 261, 271.0, 271.1, 271.4, 272.0–272.4, 272.7, 273.3, 275.0, 276.7), renal disorders (250.4, 271.4, 580–588, 590, 593, 595, 596, 599, 791.0, 791.5, V420, V451, V56), epilepsy (345, 780.39), stroke (433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91, 435.9, 436, 437.1, 437.9), and substance abuse (303–305).
Statistical Methods
Characteristics of the 3 study groups were described with counts and percentages and were compared by using Chi-square test. Incidence rate of falls were calculated by dividing the number of people suffered from falls by the total person-years of follow-up. The confidence interval (CI) of incidence rate was estimated based on Poisson distribution. Proportional hazard regression models were used to estimate the hazard ratio (HR) of falls between groups. Since there was a large number of deaths that occurred during follow-up, the potential effect of competing mortality should be taken into account to estimate the relative hazard between groups.21 By taking death as a competing risk event and falls the interest risk, subdistribution hazard ratio (sHR) were estimated based on Fine and Gray method.22 Multivariate regression analyses were sequentially constructed. The first model was established by adjusting the sociodemographic characteristics; then, diabetic complications and other comorbidities associated with falls were additionally adjusted. Subgroup analyses were also performed for patients with diabetes who had developed major complications of diabetes. Forest plots were used to show the sHR in subgroups, the sHR had been adjusted for sociodemographic characteristics, diabetic complications, and other comorbidities associated with falls. Data management and analyses were performed by using SAS analytical software (version 9.3, SAS Institute, Inc., Cary, NC). A P-value of 0.05 was considered to indicate statistical significance.
RESULTS
Table 1 shows baseline characteristics of study subjects in the 3 study groups. Patients in DwoH group were similar to the subjects of reference group with respect to age, sex, geographic distribution, and urbanization level of residential areas. Relative to both DwoH and reference groups, DwH group was older and more likely to be females, live in Southern Taiwan and rural areas, and have more type 1 diabetes. The prevalence of diabetes-related complications and comorbidities associated with falls were also unequally distributed. Compared to the DwoH group, diabetes-related complications (ie, neurological, cardiovascular, endocrine, renal, and ophthalmic disorders) were more prevalent in the DwH group. Compared to the reference group, the patients with diabetes, regardless of hypoglycemia status, were more likely to be obese and more frequently to have epilepsy, stroke, and substance abuse that predispose to a higher risk of falls. In general, prevalence of aforementioned diabetes-related complications and comorbidities associated with falls was highest in the DwH group, followed by the DwoH group, and lowest in the reference group.
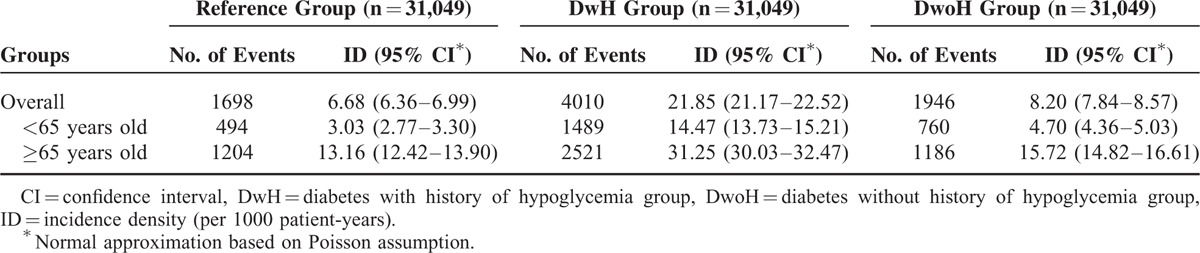
With a mean follow-up duration of 7.3 years (standard deviation: 2.9 years), 7654 (8.2%) had hospitalized for falls. The incidence rates of falls for the 3 groups were shown in Table 2. It was highest in the DwH group (21.85 per 1000 person-years). The incidence rate for the DwoH group was only slightly higher than that for reference group (8.20 vs. 6.68 per 1000 person-years). Such pattern was observed in both older (≥65 years old [y/o]) and younger (<65 y/o) subjects. Additionally, compared to the younger group, the older group was at greater risk of falls irrespective of their diabetes status or history of severe hypoglycemia.
TABLE 2.
Incidence Density of Falls in Reference Group and Diabetic Patients With or Without History of Hypoglycemia
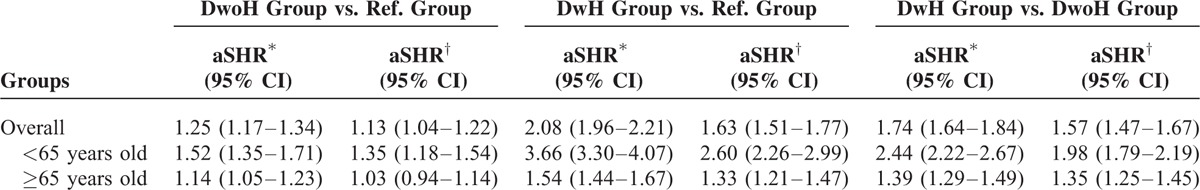
The head-to-head comparisons of the hazard of falls between the 3 groups are shown in Table 3. Multivariable analyses showed that, compared to the reference group, patients in the DwH and DwoH group were both at greater risk of falls even after adjustment for basic geo-demographic factors including age, sex, geographic areas, and urbanization level of residential areas. As the history of comorbidities and diabetes-related complications were further adjusted, despite the effect size attenuated, both DwH group and DwoH groups were still showed significantly increased adjusted sHR of 1.63 (95% CI: 1.51–1.77) and 1.13 (95% CI: 1.04–1.22), respectively. As we look into the effect of history of severe hypoglycemia on falls in patients with diabetes, the hazard of falls was significantly higher in the DwH group than in the DwoH group (adjusted sHR, 1.57; 95% CI: 1.47–1.67). The age-stratified analyses consistently showed that the sHR of falls in relation to diabetes or history of severe hypoglycemia were particularly higher in the younger group (<65 y/o) than in older people (≥65 y/o) (P-value for interaction was <0.001 in all 3 comparisons).
TABLE 3.
Subdistribution Hazard Ratios of Falls in Comparisons of All Three Groups
A forest plot shown in Figure 1 presents the results of subgroup analyses. The adjusted sHR of falls for the DwH group relative to the DwoH group were further examined according to major complications. All of the adjusted sHR of falls were consistently higher in the DwH group, regardless of complications.
FIGURE 1.
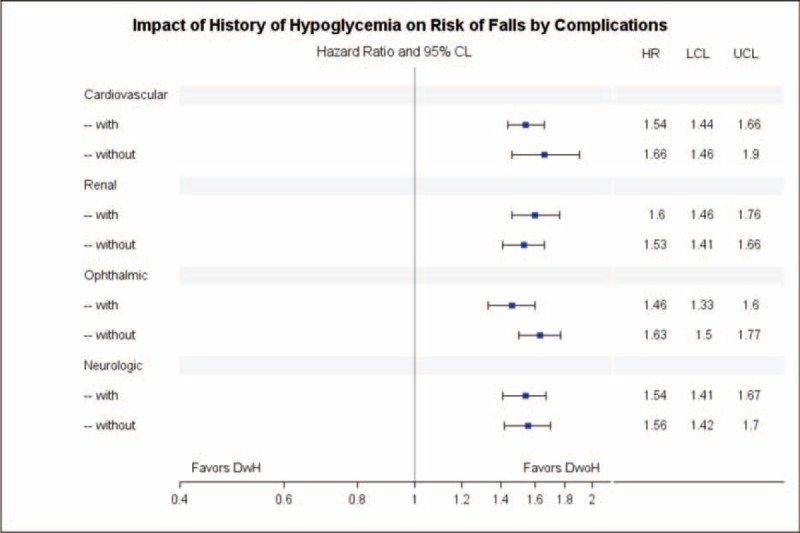
Forest plot for adjusted subdistribution hazard ratios of falls in subgroups with or without complications of diabetes.
DISCUSSION AND CONCLUSIONS
This population-based prospective study revealed that diabetic cases with or without a history of severe hypoglycemia were more likely to fall than those without diabetes. It also reported that history of severe hypoglycemia was associated with an increased risk of falls in patients with diabetes. Such excessive hazard was not only found in the older people, it was even more pronounced in people younger than 65 y/o. Unlike most studies discussed the risk of accidents basing on insulin-treated diabetes or type 2 diabetes in older people,16 this study included general diabetic adults, and most of them were presumably type 2 diabetes patients23 and treated by oral antidiabetic agents.4,24
The present study confirmed the findings of previous studies that found an increased risk of falls associated with diabetes.6,8,13,25 However, for patients with diabetes, the relation between glycemic control and the risk of falls has still been inconclusive. Previous studies reported that achieving a lower target of HbA1c by intensive therapy or noninsulin treatment did not increase the risk of falls in patients with type 2 diabetes,14,25 a higher risk of fall was only found in insulin-treated diabetes.25 Nevertheless, these studies did not investigate the relationship between hypoglycemia and the risk of falls.
To the best of our knowledge, there were only 2 population-based studies that investigated the relationship of history of hypoglycemia and the risk of fall in diabetes,15,16 both had reported an elevated risk associated with the concurrent or history of hypoglycemia (adjusted odds ratio = 1.70 [95% CI: 1.58–1.83]15; adjusted HR = 1.36 [95% CI: 1.13–1.65]).16 The present study revisited this issue in a population-based settings in Asia, and provided better estimation of association for putative link by considering competing mortality. Our finding (adjusted sHR = 1.57 [95% CI: 1.47–1.67]) was consistent with the 2 aforementioned studies.15,16 Moreover, our subgroup analyses further showed that the association consistently exists in subgroups with or without various complications of diabetes. It may have implied that the threat of prior severe hypoglycemia on the risk of falls was a common challenge to all diabetic patients regardless of their vascular complications.
Previous studies rarely reported the risk of falls among the young and middle-aged patients.17 Fall-related injuries usually resulted in physical activity restrictions, functional declines, and impaired societal relationship in the elderly,27 they may also resulted in work days loss and interference of family in young- and middle-age populations.17 Given the increasingly burden and the downward onset-age of diabetes,27,28 the potential disease and economic impacts of falls in younger diabetic populations deserves more attentions. Our study confirmed an increased risk of falls in older patients with diabetes with or without history of severe hypoglycemia, it also reported an even higher hazard ratio of falls in younger patients with diabetes. Nevertheless, our finding was discrepant from a previous study which found that history of severe hypoglycemia in diabetes was associated with a significant increased hazard of falls in the older people, but not in the younger people.16 It is not clear what causes such inconsistent results. A much higher incidence (particularly in the older people) was noticed in our study sample. In addition, duration of diabetes in these 2 studies might also partly account for the difference. Regretfully, information on duration of diabetes was not available in both studies. The discrepant findings may also be explained by the different attributes and reimbursement policy of insurances in different studies. The present study was based on a compulsory, high-coverage National Health Insurance that provides a high accessibility for medical services and might present more events of falls or falling episodes with less severity that were more likely to occur in the people younger than 65 y/o.
Our study advanced the findings of previous studies in the following aspects. First, the present study considered death without prior fall-related hospitalizations as a competing risk and provided estimations of sHRs. Since substantial percentage of patients died during the period of follow-up, introducing competing risk analysis can improve the validation of the risk estimation.21 Second, most of previous studies discussed the risk of accidents basing on insulin-treated diabetes16 or diabetes in older people,15 this study included general diabetic adults and reported a higher risk of falls in people younger than 65 y/o. In Taiwan, at least 99% of the general diabetic adults were type 2 diabetes patients23 and nearly 90% of them were treated by oral antidiabetic agents only.24
There were several limitations in the present study and it should be cautious in interpreting the findings. The present study did not completely include all episodes of hypoglycemia and falls. We did not investigate the influence of mild hypoglycemia which had been self-managed by patients or their families and did not need medical services. The incidence of hospitalizations due to falls may also have been underestimated since it was possible that physicians did not mention the fall as an external cause of injuries at discharge in medical claims. However, such misclassifications of severe hypoglycemia or falls were likely to be nondifferential, which could only lead to the observed association toward the null.
Moreover, this study only identified the episode of severe hypoglycemia at baseline; the cumulative effect of repeated severe hypoglycemia cannot be directly measured. Despite that, previous studies found that the history of hypoglycemia per se was an independent risk factor of current hypoglycemia,29 autonomic failure including defective glucose counterregulation and hypoglycemia unawareness may result in recurrent hypoglycemia in type 1 diabetes or advanced type 2 diabetes.30 Therefore, falls noted concurrently in prevalent cases of diabetes may also represent a prior history of sever hypoglycemia.
Finally, we were unable to collect the information of certain environmental risk factors for falls in one's daily life (eg, unsatisfactory living arrangement and inadequate physical activities), thus, residual confounding resulting from incomplete adjustment for such environmental risk factors may not be completely avoided.
In conclusions, this population-based prospective study confirmed a higher risk of falls in diabetes than in nondiabetes, irrespective the patients with or without a history of severe hypoglycemia. The history of severe hypoglycemia further increased hazard of falls in diabetes; and, the increased hazard was particularly pronounced in younger patients (<65 y/o) with diabetes. Because severe hypoglycemia-related falls in younger people with diabetes may result in work day losses and interference of family function, our study calls for proper attentions in prevention of falls in younger patients (<65 y/o) with diabetes who had history of severe hypoglycemia. Further studies investigating the influence of medication use on the risk of falls and the incidence and frequency of hypoglycemia episode are warranted.
UNCITED REFERENCE
Footnotes
Abbreviations: HbA1c = glycosylated hemoglobin A1c, NHIRD = National Health Insurance Research Database, NHI = National Health Insurance, ICD9-CM = International Classification of Diagnosis, 9th version, Clinical Modification, DwH = diabetes with history of severe hypoglycemia, DwoH = diabetes without history of severe hypoglycemia, CI = confidence interval, HR = hazard ratio, sHR = subdistribution hazard ratio, y/o = years old.
This study is also based in part on data from the NHIRD provided by the Bureau of National Health Insurance and the Department of Health and managed by National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health, or National Health Research Institutes.
The authors have no conflicts of interest to disclose.
This study was supported by grant from the Ministry of Science and Technology, (NSC101–2314-B-006-076-MY3). Chung-Yi Li is principal investigator of the project supported by Ministry of Health and Welfare (MOHW104-HPA-H-114-114705). The funders have no role in conducting and submitting this work.
REFERENCES
- 1.WHO MCo. WHO Factsheets_Falls. 2012. http://www.who.int/mediacentre/factsheets/fs344/en/ Accessed 2014/10/6, 2014 [Google Scholar]
- 2.Chandran A, Hyder AA, Peek-Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev 2010; 32:110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berlie HD, Garwood CL. Diabetes medications related to an increased risk of falls and fall-related morbidity in the elderly. Ann Pharmacother 2010; 44:712–717. [DOI] [PubMed] [Google Scholar]
- 4.Chiang CW, Chiu HF, Chen CY, et al. Trends in the use of oral antidiabetic drugs by outpatients in Taiwan: 1997–2003. J Clin Pharm Ther 2006; 31:73–82. [DOI] [PubMed] [Google Scholar]
- 5.Yau RK, Strotmeyer ES, Resnick HE, et al. Diabetes and risk of hospitalized fall injury among older adults. Diabetes Care 2013; 36:3985–3991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz AV, Hillier TA, Sellmeyer DE, et al. Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care 2002; 25:1749–1754. [DOI] [PubMed] [Google Scholar]
- 7.Wallace C, Reiber GE, LeMaster J, et al. Incidence of falls, risk factors for falls, and fall-related fractures in individuals with diabetes and a prior foot ulcer. Diabetes Care 2002; 25:1983–1986. [DOI] [PubMed] [Google Scholar]
- 8.Tilling LM, Darawil K, Britton M. Falls as a complication of diabetes mellitus in older people. J Diabetes Complications 2006; 20:158–162. [DOI] [PubMed] [Google Scholar]
- 9.de Boer MR, Pluijm SMF, Lips P, et al. Different aspects of visual impairment as risk factors for falls and fractures in older men and women. J Bone Miner Res 2004; 19:1539–1547. [DOI] [PubMed] [Google Scholar]
- 10.Ismail-Beigi F, Craven T, Banerji MA, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet 2010; 376:419–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329:977–986. [DOI] [PubMed] [Google Scholar]
- 12.Skyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA Diabetes Trials: a position statement of the American Diabetes Association and a Scientific Statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol 2009; 53:298–304. [DOI] [PubMed] [Google Scholar]
- 13.Liao C-C, Lin C-S, Shih C-C, et al. Increased risk of fracture and postfracture adverse events in patients with diabetes: two nationwide population-based retrospective cohort studies. Diabetes Care 2014; 37:2246–2252. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz AV, Margolis KL, Sellmeyer DE, et al. Intensive glycemic control is not associated with fractures or falls in the ACCORD randomized trial. Diabetes Care 2012; 35:1525–1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston SS, Conner C, Aagren M, et al. Association between hypoglycaemic events and fall-related fractures in Medicare-covered patients with type 2 diabetes. Diabetes Obes Metab 2012; 14:634–643. [DOI] [PubMed] [Google Scholar]
- 16.Signorovitch JE, Macaulay D, Diener M, et al. Hypoglycaemia and accident risk in people with type 2 diabetes mellitus treated with non-insulin antidiabetes drugs. Diabetes Obes Metab 2013; 15:335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Talbot LA, Musiol RJ, Witham EK, et al. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 2005; 5:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lu JF, Hsiao WC. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Affairs 2003; 22:77–88. [DOI] [PubMed] [Google Scholar]
- 19.Cheng TM. Taiwan's new national health insurance program: genesis and experience so far. Health Affairs 2003; 22:61–76. [DOI] [PubMed] [Google Scholar]
- 20.Chen HF, Chen P, Li CY. Risk of malignant neoplasms of liver and biliary tract in diabetic patients with different age and sex stratifications. Hepatology (Baltimore, Md) 2010; 52:155–163. [DOI] [PubMed] [Google Scholar]
- 21.Berry SD, Ngo L, Samelson EJ, et al. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc 2010; 58:783–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94:496–509. [Google Scholar]
- 23.Jiang Y-D, Chang C-H, Tai T-Y, et al. Incidence and prevalence rates of diabetes mellitus in Taiwan: analysis of the 2000–2009 Nationwide Health Insurance database. J Formos Med Assoc 2012; 111:599–604. [DOI] [PubMed] [Google Scholar]
- 24.Chang C-H, Jiang Y-D, Chung C-H, et al. National trends in anti-diabetic treatment in Taiwan, 2000–2009. J Formos Med Assoc 2012; 111:617–624. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz AV, Vittinghoff E, Sellmeyer DE, et al. Diabetes-related complications, glycemic control, and falls in older adults. Diabetes Care 2008; 31:391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schiller JS, Kramarow EA, Dey AN. Fall injury episodes among noninstitutionalized older adults: United States, 2001–2003. Adv Data 2007; 392:1–16. [PubMed] [Google Scholar]
- 27.Narayan KM, Boyle JP, Geiss LS, et al. Impact of recent increase in incidence on future diabetes burden: U.S., 2005–2050. Diabetes Care 2006; 29:2114–2116. [DOI] [PubMed] [Google Scholar]
- 28.Forouhi NG, Wareham NJ. Epidemiology of diabetes. Medicine 2010; 38:602–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller CD, Phillips LS, Ziemer DC, et al. Hypoglycemia in patients with type 2 diabetes mellitus. Arch Intern Med 2001; 161:1653–1659. [DOI] [PubMed] [Google Scholar]
- 30.Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med 2013; 369:362–372. [DOI] [PubMed] [Google Scholar]


