Abstract
The relationship between atopic dermatitis (AD) and psychological distress has been well established for children and adolescents. However, it is unclear whether this relationship exists in young adults. This study aimed to assess the relationship between AD and psychological distress in young male adults in South Korea.
A cross-sectional study was conducted using regional conscription data from 2008 to 2012. A dermatologist diagnosed AD based on historical and clinical features, and determined severity using the eczema area and severity index. A psychiatrist used medical records, an interview, and a psychological test to examine psychological distress (depression, anxiety, and somatization). The relationship between psychological distress and AD was assessed by multivariate logistic regression analyses.
Among the 120,508 conscripts, 1517 (1.2%) presented with AD. The odds of having each type of psychological distress were significantly greater for individuals with AD compared with those without AD. The adjusted odds ratios for depression, anxiety, and somatization were 1.79 (95% CI 1.40–2.29), 1.38 (95% CI 1.08–1.76), and 1.75 (95% CI 1.40–2.20), respectively. Moderate-to-severe AD was significantly related to depression and somatization to a greater extent compared with mild AD.
Depression, anxiety, and somatization are strongly and independently associated with AD in young adult males. Early treatment of skin inflammation might modify the risk of psychiatric problems. Prospective cohort studies are needed to verify causal relationships.
INTRODUCTION
Atopic dermatitis (AD) is a chronic skin disease characterized by pruritus and eczematous skin lesions, and is often associated with other atopic disorders, such as allergic rhinitis and asthma.1 AD is a widely prevalent disease, as it affects 5% to 15% of children and accounts for 2% to 4% of adults.2,3 It is a global public health concern with increasing prevalence and substantial burden.4 Patients with AD have lower health-related quality of life compared with the general population, and increasing disease severity is related to greater impairment of life quality.5–7 The resultant psychological distress is one of the common comorbidities linked to AD, and could negatively affect quality of life.8
The association between AD and mental health comorbidities in children and adolescents has been well established.9,10 Recent large population-based studies have demonstrated that AD in children and adolescents is associated with mental health disorders including attention deficit hyperactivity disorder, depression, anxiety, conduct disorder, and autism.11,12 Additionally, there is a dose-dependent relationship between AD severity and mental health problems.11,13 In a prospective cohort study in Germany, children with infant-onset eczema were at increased risk for mental health problems in their childhood.14 Suicidal ideation is also more prevalent in adolescents with AD compared with healthy individuals, and both are significantly associated in a multivariate model.15
In a few studies that use adult samples, it has been reported that patients with AD have higher levels of depression and anxiety than controls.16–18 However, these studies have some inherent limitations such as small sample sizes, lack of controlling for potential confounders, or not considering AD severity. A study using a large general population found, after multivariate analyses, that somatization considerably contributes to the association between depression/anxiety and eczema.19 However, the authors in that study did not separate eczema into atopic and nonatopic, and were unable to show solely the effects of AD. Despite mental health problems in a young person potentially leading to many adverse outcomes, including significant impairments in work, education, and social interaction,20 there are no studies investigating the associations between AD and psychological distress in a large population of young adults. Therefore, the aim of the present study was to perform a comprehensive evaluation using a substantial amount of conscription data to examine psychological distress in young adults with AD.
METHODS
Data Source
In South Korea, it is mandatory for all men around 19 years of age to be examined for military conscription by the Military Manpower Administration. Each conscript is interviewed and examined to ascertain whether he has physical or mental problems that would impede military service. A conscript with such problems is required to submit medical records from physicians at clinics or hospitals. Presence and severity of a problem are determined by the conscription officers, medical specialists, through medical records, face-to-face interviews, and medical work-ups.
The present study was conducted using secondary data obtained from a regional Military Manpower Administration between February 1, 2008 and December 31, 2012, therefore institutional review board approval was not needed. The data included information on demographics and medical conditions of conscripts residing in Incheon, which is a metropolitan area with a population of approximately 3 million. The present study was conducted with approval from the Military Manpower Administration Committee in Incheon, South Korea.
Study Variables
A diagnosis of AD was made clinically and was based on historical and clinical features, such as personal or family history of atopy, morphology and distribution of eczematous skin lesions, and associated clinical signs. A conscription officer in dermatology confirmed AD presence through a medical certificate and physical examination; AD severity was measured using the eczema area and severity index. The eczema area and severity index involves an assessment of disease extent in 4 body regions (head/neck, upper limbs, trunk, and lower limbs) plus an evaluation of the intensity of a representative area of eczema (erythema, induration/papulation/edema, excoriation, and lichenification). The AD severity was divided into “mild” and “moderate-to-severe.”
The mental problems of conscripts were evaluated by a psychiatric officer using examinees’ medical records, an interview, and the Korean Military Multiphasic Personality Inventory (KMPI). The KMPI is a revised version of the conventional Minnesota Multiphasic Personality Inventory, adjusted for Korean conscription. The KMPI is similar to the Minnesota Multiphasic Personality Inventory in its overall features.21 Neurotic symptoms, psychotic symptoms, suicidal ideation, and other psychiatric symptoms are analyzed using the KMPI; each scale's scores are transformed into standardized T-scores. More details on the KMPI are described elsewhere.22 In the present study, psychological distress included depression, anxiety, and somatization in the neurosis set of the KMPI. Since the marked elevation of the T-score implies higher tendency to manifest psychological or psychiatric symptoms compared with the normal range of the score, we determined that an individual had psychological distress if they had a T-score >65.
Socio-demographic characteristics such as age, level of education, economic status, and family structure were investigated using a self-administered questionnaire. Level of education was categorized into 3 groups according to the duration of education: ≤6 years of education (elementary school or lower); 7 to 12 years (middle or high school); and ≥13 years (college or higher). Household economic status was categorized into 5 groups: very low, low, middle, high, and very high. Family structure was divided into 3 types by the number of parents residing with the conscripts: nonparent, single parent, and dual parent family.
Statistical Analysis
Univariate analyses for socio-demographic characteristics of conscripts were performed by independent t test and chi-square test. The differences in the proportion of depression, anxiety, and somatization by AD status and univariate associations were tested using a chi-square test. The linear trends of each psychological distress according to AD severity were analyzed by the Cochran-Armitage trend test. The multivariate associations between AD status and each type of psychological distress were investigated using logistic regression models. To adjust for potential confounders, covariates such as age, level of education, economic status, and family structure were included in the models. Considering that depression, anxiety, and somatization might be associated with each other, we also included the type of psychological distress other than the targeted one as covariates in the models to evaluate whether each type of psychological distress is associated with AD independently of the others. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). The results were reported as odds ratios (ORs), 95% confidence intervals (CIs), and P values. A P value of <0.05 was considered significant.
RESULTS
Among the 120,841 conscripts examined during the study period, 120,508 were included in the analyses. We excluded 333 conscripts from further analysis due to incomplete data in either the KMPI or socio-demographic characteristics. Prevalence of AD in the study population was 1.2% (1,517/120,508). Socio-demographic characteristics of the AD population and overall population are shown in Table 1. The AD population was younger than the non-AD population (19.8 ± 1.0 and 20.0 ± 1.2, P < 0.001). When compared with the non-AD population, the AD population showed a significantly higher proportion in the categories of low education level (≤12 years of education) and upper economic classes (“high” plus “very high”).
TABLE 1.
Characteristics of the Study Population
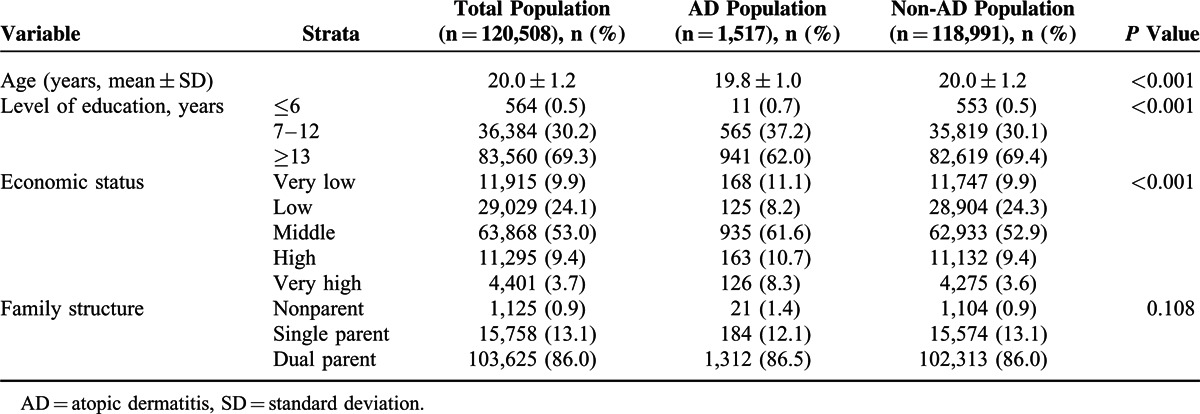
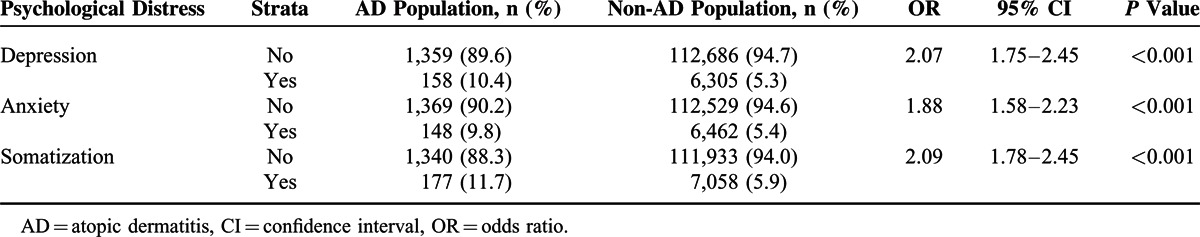
Table 2 shows the differences in the prevalence of psychological distress according to AD presence. The proportion of individuals with at least 1 type of psychological distress was higher in the AD population than in the non-AD population (18.7% and 8.9%, respectively, P < 0.001). The prevalence of each type of psychological distress such as depression, anxiety, and somatization was significantly higher in the AD population. We also found significant relationships between AD and depression (OR 2.07, 95% CI 1.75–2.45), anxiety (OR 1.88, 95% CI 1.58–2.23), and somatization (OR 2.09, 95% CI 1.78–2.45) in the univariate analyses.
TABLE 2.
Prevalence of Psychological Distress According to the Presence of Atopic Dermatitis
We then examined the prevalence of depression, anxiety, and somatization according to AD severity category. The prevalence of each type of psychological distress showed significant differences for each AD severity category (Table 3). Depression (12.0%), anxiety (10.0%), and somatization (12.6%) were most prevalent in individuals with moderate-to-severe AD. There were also linear trends showing that the prevalence of psychological distresses increased with AD severity.
TABLE 3.
Prevalence of Psychological Distress According to the Severity of Atopic Dermatitis
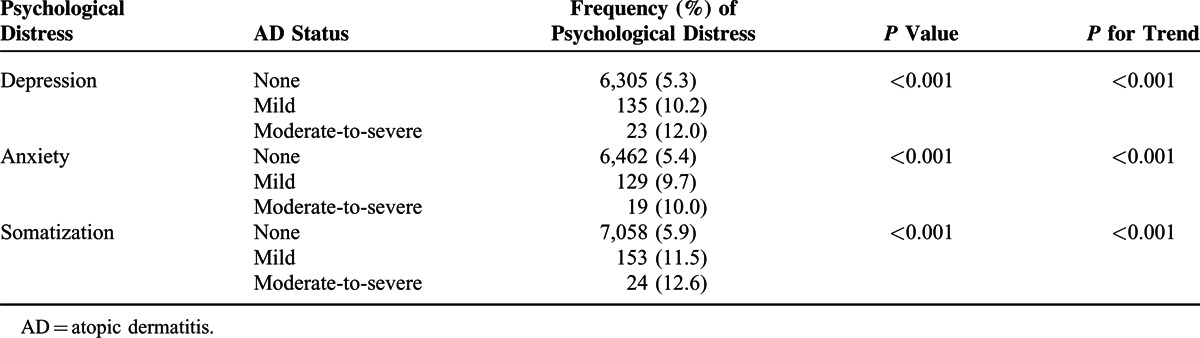
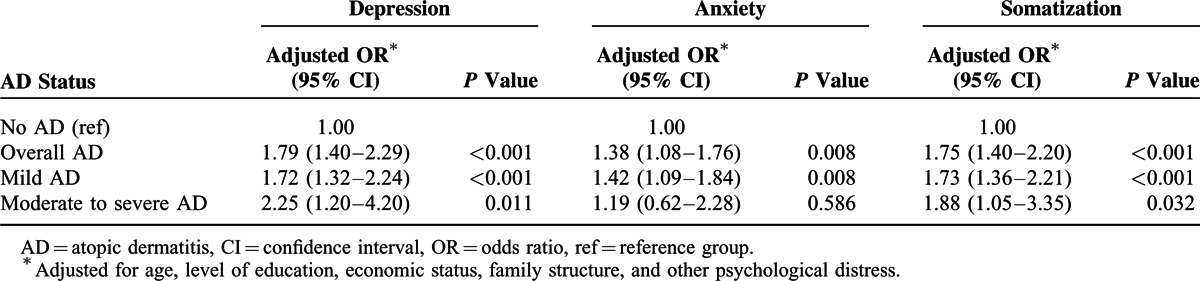
Table 4 reports the associations between AD and psychological distress according to AD status in the logistic regression models adjusting for potential confounders. Depression, anxiety, and somatization showed significant associations with overall AD independently of one another, irrespective of severity (OR 1.79, 95% CI 1.40–2.29, 1.38, 1.08–1.76, and 1.75, 1.40–2.20, respectively). After stratifying AD by severity, depression and somatization were still significantly associated with both mild and moderate-to-severe AD. We found that moderate-to-severe AD was related to depression and somatization to a greater extent than mild AD. In the case of anxiety, there was a significant association with mild AD (OR 1.42, 95% CI 1.09–1.84) but not with moderate-to-severe AD (OR 1.19, 95% CI 0.62–2.28).
TABLE 4.
Odds of Psychological Distress in Young Adult Males by Atopic Dermatitis Status
DISCUSSION
The present study was designed to investigate comprehensively whether psychological distress was related to AD in a large population of young adult males. We found that individuals with AD had an increased prevalence of depression, anxiety, and somatization compared with those without AD. A patient with more severe AD showed a tendency of the higher probability to have such psychological distresses. Depression, anxiety, and somatization were significantly and independently associated with AD presence even after controlling for potential confounders. Moreover, the associations between AD and depression/somatization correlated with AD severity.
There are a few epidemiological studies on relationships between AD and psychological distress in adults. Some studies reported that patients with AD have more marked depression than healthy adults did, and that patients with more severe AD are more depressive.16,18,23 Yang et al24,25 investigated the association between AD and depression, and the modifying effects of smoking and serum total immunoglobulin E level on the association. They found that the association between AD and depression remained significant after adjusting for the possible modifiers, suggesting that the association is strongly independent of those factors. In terms of anxiety, it has been demonstrated that patients with AD are more likely to be anxious than healthy individuals.16,26,27 However, a previous study reported a nonsignificant difference in the anxiety scale between the AD group and normal controls,23 and other studies showed no significant correlation between AD severity and anxiety.27,28 These discrepancies in the findings on anxiety may result from the cross-sectional study design and complex relationship as determined by a variety of factors, not only AD severity. For these reasons, the results of our study could have a nonsignificant association between anxiety and moderate-to-severe AD. In a population-based study, the association between somatization and nonspecific eczema, which included atopic and nonatopic eczema, was strong and followed a dose-response pattern.29 The study also found that nonspecific eczema-somatization association is robust for adjustments for depression and anxiety while the associations of nonspecific eczema with depression and anxiety are not significant after adjusting for somatization. These findings are inconsistent with the results of the present study that both depression and anxiety were significantly associated with AD in the models controlling for somatization. This may come from the difference of the characteristics of study subjects such as age group, gender, and the type of dermatitis included in the analyses.
The mechanisms underlying AD and psychological distresses have been unclear thus far. The altered immunological responses in AD might be 1 mechanism through which patients with AD often accompany psychological distress. Peripherally produced proinflammatory cytokines penetrate the blood–brain barrier directly via active transport or indirectly via vagal nerve stimulation, which facilitates bidirectional communication between the central nervous system and peripheral immune system.30 Therefore, the shared inflammatory mediators might result in the comorbidity of psychological distress in AD patients. Pruritus, a major symptom of AD, might be a factor mediating the vicious cycle of AD in individuals with psychological distress. Depressed patients often have an elevated level of central corticotrophin-releasing factor, which might decrease the threshold for itching.31 A recent experimental study showed that depressed patients with AD report higher induced itch than AD patients without depression.32 Moreover, elevated anxiety in AD patients could increase the conditioning of a scratch response to an itching stimulus.31 Thus, we speculate that psychological distresses could contribute to AD severity.
The present study, to our knowledge, is the first attempt to comprehensively investigate the relationships between AD and types of psychological distress in young adults using a large dataset. Using data from a large population, we could avoid selection biases common in hospital samples, and compare the strengths of potentially weak associations. In the present study, medical specialists evaluated AD and psychological distress based on information such as a conscript's medical record, interview, physical examination, and validated psychological test, whereas several previous studies have obtained data via self-report. This ensured that the misdiagnoses for AD and psychological distress were minimized. We evaluated the independent effects of depression, anxiety, and somatization by adjusting for the potential confounding effects between each type of psychological distress.
Our study had several limitations. Most important are the study's cross-sectional design and chosen study population. Using cross-sectional data, a temporal relationship between AD and the development of psychological distress was unable to be established, thereby limiting the interpretation of our findings regarding causality. Data used were also confined to young adult males; this leads to a lack of generalizability of our findings. In a study of the general population, anxiety and depression were associated with AD in both middle-aged men and women.19 Moreover, a previous study of adolescents aged 17 to 19 years reported that girls with AD do have an increased risk of psychological distress, but with a weaker association than that noted in boys.33 We cannot rule out the underreporting of AD. Since a conscription officer performed additional examinations for only conscripts who submitted their past medical records, AD patients could be misclassified in the healthy population if they did not report their disease. Despite potential bias weakening the associations, our results were still significant and strong. Moreover, the AD prevalence in our study was similar to the prevalence reported in a study of Danish conscripts.34 The conscription itself may be a cause of psychological distress. However, since both the AD and control groups were under the same potential distress during conscription, it is unlikely that this factor is responsible for our observed associations. Finally, we included potential confounders such as age, level of education, and economic status in the models. Nevertheless, residual confounding cannot be excluded completely. However, this limitation has probably not produced the main findings of the present study. Prospective cohort studies using a general population should be performed in the future to provide additional evidence regarding the causal relationship between AD and psychological distress.
In conclusion, the results of our study reveal that depression, anxiety, and somatization are strikingly and independently associated with AD in young adult males. The strengths of the associations are altered by AD severity. Our findings suggest that early treatment of skin inflammation might modify the risk of psychiatric problems, and psychological consultations are needed to prevent the aggravation of AD symptoms.
Footnotes
Abbreviations: AD = atopic dermatitis, CI = confidence interval, KMPI = Korean Military Multiphasic Personality Inventory, OR = odds ratio.
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Bieber T. Atopic dermatitis. N Engl J Med 2008; 358:1483–1494. [DOI] [PubMed] [Google Scholar]
- 2.Deckert S, Kopkow C, Schmitt J. Nonallergic comorbidities of atopic eczema: an overview of systematic reviews. Allergy 2014; 69:37–45. [DOI] [PubMed] [Google Scholar]
- 3.Kelsay K, Klinnert M, Bender B. Addressing psychosocial aspects of atopic dermatitis. Immunol Allergy Clin North Am 2010; 30:385–396. [DOI] [PubMed] [Google Scholar]
- 4.Carroll CL, Balkrishnan R, Feldman SR, et al. The burden of atopic dermatitis: impact on the patient, family, and society. Pediatr Dermatol 2005; 22:192–199. [DOI] [PubMed] [Google Scholar]
- 5.Kiebert G, Sorensen SV, Revicki D, et al. Atopic dermatitis is associated with a decrement in health-related quality of life. Int J Dermatol 2002; 41:151–158. [DOI] [PubMed] [Google Scholar]
- 6.Maksimovic N, Jankovic S, Marinkovic J, et al. Health-related quality of life in patients with atopic dermatitis. J Dermatol 2012; 39:42–47. [DOI] [PubMed] [Google Scholar]
- 7.Holm EA, Wulf HC, Stegmann H, et al. Life quality assessment among patients with atopic eczema. Br J Dermatol 2006; 154:719–725. [DOI] [PubMed] [Google Scholar]
- 8.Wittkowski A, Richards HL, Griffiths CE, et al. The impact of psychological and clinical factors on quality of life in individuals with atopic dermatitis. J Psychosom Res 2004; 57:195–200. [DOI] [PubMed] [Google Scholar]
- 9.Simpson EL. Comorbidity in Atopic Dermatitis. Curr Dermatol Rep 2012; 1:29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fennessy M, Coupland S, Popay J, et al. The epidemiology and experience of atopic eczema during childhood: a discussion paper on the implications of current knowledge for health care, public health policy and research. J Epidemiol Community Health 2000; 54:581–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity in patients with atopic dermatitis. J Allergy Clin Immunol 2013; 131:428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmitt J, Romanos M, Schmitt NM, et al. Atopic eczema and attention-deficit/hyperactivity disorder in a population-based sample of children and adolescents. JAMA 2009; 301:724–726. [DOI] [PubMed] [Google Scholar]
- 13.Slattery MJ, Essex MJ, Paletz EM, et al. Depression, anxiety, and dermatologic quality of life in adolescents with atopic dermatitis. J Allergy Clin Immunol 2011; 128:668–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmitt J, Apfelbacher C, Chen CM, et al. Infant-onset eczema in relation to mental health problems at age 10 years: results from a prospective birth cohort study (German Infant Nutrition Intervention plus). J Allergy Clin Immunol 2010; 125:404–410. [DOI] [PubMed] [Google Scholar]
- 15.Halvorsen JA, Lien L, Dalgard F, et al. Suicidal ideation, mental health problems, and social function in adolescents with eczema: a population-based study. J Invest Dermatol 2014; 134:1847–1854. [DOI] [PubMed] [Google Scholar]
- 16.Arima M, Shimizu Y, Sowa J, et al. Psychosomatic analysis of atopic dermatitis using a psychological test. J Dermatol 2005; 32:160–168. [DOI] [PubMed] [Google Scholar]
- 17.Takahashi H, Tsuji H, Honma M, et al. Japanese patients with psoriasis and atopic dermatitis show distinct personality profiles. J Dermatol 2013; 40:370–373. [DOI] [PubMed] [Google Scholar]
- 18.Takaki H, Ishii Y. Sense of coherence, depression, and anger among adults with atopic dermatitis. Psychol Health Med 2013; 18:725–734. [DOI] [PubMed] [Google Scholar]
- 19.Klokk M, Gotestam KG, Mykletun A. Factors accounting for the association between anxiety and depression, and eczema: the Hordaland health study (HUSK). BMC Dermatol 2010; 10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med 1998; 28:109–126. [DOI] [PubMed] [Google Scholar]
- 21.Oh CH, Lim HK, Chung J, et al. The psychopathological influence of congenital heart disease in Korean male adolescents: an analysis of multiphasic personal inventory test results. Yonsei Med J 2012; 53:1107–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paik HK, Oh CH, Choi K, et al. Influence of history of brain disease or brain trauma on psychopathological abnormality in young male in Korea: analysis of multiphasic personal inventory test. J Korean Neurosurg Soc 2011; 50:114–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hashiro M, Okumura M. Anxiety, depression and psychosomatic symptoms in patients with atopic dermatitis: comparison with normal controls and among groups of different degrees of severity. J Dermatol Sci 1997; 14:63–67. [DOI] [PubMed] [Google Scholar]
- 24.Yang YW, Tseng KC, Chen YH, et al. Associations among eczema, asthma, serum immunoglobulin E and depression in adults: a population-based study. Allergy 2010; 65:801–802. [DOI] [PubMed] [Google Scholar]
- 25.Yang YW, Chen YH, Huang YH. Cigarette smoking may modify the risk of depression in eczema among adults: a preliminary study using NHANES 2005-2006. J Eur Acad Dermatol Venereol 2011; 25:1048–1053. [DOI] [PubMed] [Google Scholar]
- 26.Oh SH, Bae BG, Park CO, et al. Association of stress with symptoms of atopic dermatitis. Acta Derm Venereol 2010; 90:582–588. [DOI] [PubMed] [Google Scholar]
- 27.Linnet J, Jemec GB. An assessment of anxiety and dermatology life quality in patients with atopic dermatitis. Br J Dermatol 1999; 140:268–272. [DOI] [PubMed] [Google Scholar]
- 28.Ginsburg IH, Prystowsky JH, Kornfeld DS, et al. Role of emotional factors in adults with atopic dermatitis. Int J Dermatol 1993; 32:656–660. [DOI] [PubMed] [Google Scholar]
- 29.Klokk M, Stansfeld S, Overland S, et al. Somatization: the under-recognized factor in nonspecific eczema. The Hordaland Health Study (HUSK). Br J Dermatol 2011; 164:593–601. [DOI] [PubMed] [Google Scholar]
- 30.Wilson CJ, Finch CE, Cohen HJ. Cytokines and cognition – the case for a head-to-toe inflammatory paradigm. J Am Geriatr Soc 2002; 50:2041–2056. [DOI] [PubMed] [Google Scholar]
- 31.Buske-Kirschbaum A, Geiben A, Hellhammer D. Psychobiological aspects of atopic dermatitis: an overview. Psychother Psychosom 2001; 70:6–16. [DOI] [PubMed] [Google Scholar]
- 32.Schut C, Bosbach S, Gieler U, et al. Personality traits, depression and itch in patients with atopic dermatitis in an experimental setting: a regression analysis. Acta Derm Venereol 2014; 94:20–25. [DOI] [PubMed] [Google Scholar]
- 33.Saunes M, Smidesang I, Holmen TL, et al. Atopic dermatitis in adolescent boys is associated with greater psychological morbidity compared with girls of the same age: the Young-HUNT study. Br J Dermatol 2007; 156:283–288. [DOI] [PubMed] [Google Scholar]
- 34.Steffensen FH, Sorensen HT, Gillman MW, et al. Low birth weight and preterm delivery as risk factors for asthma and atopic dermatitis in young adult males. Epidemiology 2000; 11:185–188. [DOI] [PubMed] [Google Scholar]


