Abstract
Evidence showing higher acute myocardial infarction (AMI) mortality rates among female compared with male inpatients has stimulated interest in whether this disparity is the result of biological factors or differences in the provision of healthcare services. We investigated the impact of sex on in-hospital mortality rates due to AMI, and evaluated the contribution of differences in the delivery of optimal medical services for AMI.
We retrospectively constructed a dataset of 85,329 new patients admitted to Korean hospitals with AMI between 2003 and 2007 from the Korea National Health Insurance Claims Database. We used the claims database to provide information about treatment after admission or death for each patient.
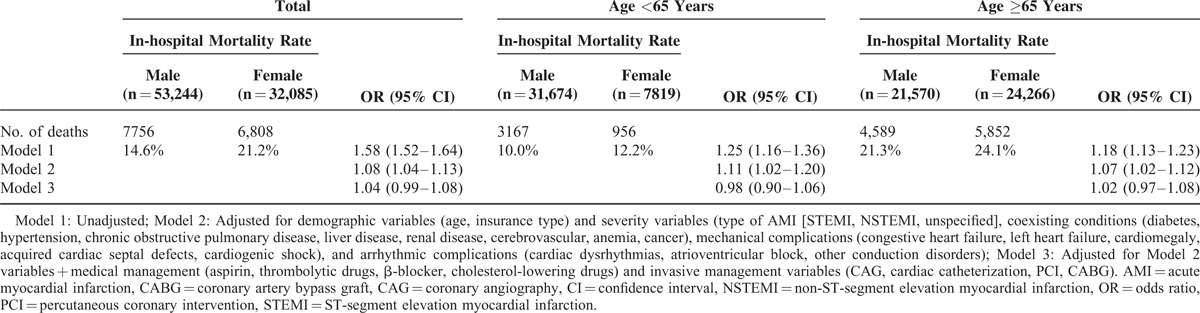
Proportionally more female than male patients aged 65 years or older had complications; however, proportionally fewer female patients underwent invasive procedures. Female patients had a higher in-hospital mortality rate than males (21.2% vs 14.6%, odds ratio [OR] 1.58, 95% confidence interval [CI] 1.52–1.64). The probability of death within 30 days after admission remained higher for females than males after adjusting for demographic characteristics and severity (OR 1.08, 95% CI 1.04–1.13). After additionally adjusting for invasive and medical management, the probability of death within 30 days did not differ between males and females (OR 1.04, 95% CI 0.99–1.08). A similar trend was revealed by an additional analysis of patients according to younger (<65 years) and older (≥65 years) age groups.
The higher in-hospital mortality rates after AMI in Korean female patients was associated with a lower procedure rate. Evidence indicating that AMI symptoms differ according to sex highlights the need for health policies and public education programs that raise awareness of sex-related differences in early AMI symptoms to increase the incidence of appropriate early treatment in females.
INTRODUCTION
Cardiovascular disease is a leading cause of death in Western countries, including Europe and the United States. The incidence of acute myocardial infarction (AMI) has increased rapidly in Korea as the result of a Westernized diet and an aging population.1,2 Although AMI has a relatively high mortality rate, the delivery of appropriate healthcare services may reduce death and disabilities caused by AMI.3
Several studies have shown that although the incidence of AMI is higher in males, in-hospital mortality is higher in females.1,4,5 The higher mortality rate in female patients has been attributed to a higher incidence of coexisting conditions such as hypertension and diabetes, and a greater number of severe myocardial conditions such as stenosis of the left anterior descending artery (LAD).5–9 Furthermore, female patients receive less thrombolytic or reperfusion therapy than male patients.10–13 Sex-related differences in cardiovascular disease severity may be related to biological differences; however, differences in the provision of optimal treatments suggest that social inequality may play a role in health inequality.14
We investigated the contribution of the disparity in the delivery of optimal medical services to sex-related differences in the rates of in-hospital mortality due to AMI.
METHODS
Data Source
Data were collected from the Korea National Health Insurance (KNHI) Claims Database of the Health Insurance Review and Assessment Service (HIRA) between 2003 and 2007. This database contains all of the claims provided by the National Health Insurance (NHI) and Medical Aid Programs. The NHI program covers 96% to 97% of the population as a compulsory social insurance scheme. The remaining 3% to 4% is protected under the Medical Aid Program as public healthcare assistance for the poor.15,16
The National Health Insurance Corporation (NHIC), the sole healthcare insurer in Korea, was established by statute, and is responsible for operating the NHI program. HIRA is charged with reviewing healthcare providers’ claims, and the Ministry of Health and Welfare (MOHW) supervises the program as a whole. The main sources of funding for the NHI are contributions from insured and government subsidies.15,17 Korea's healthcare delivery system and claims data have been described in detail.17,18
Study Population
Our retrospective cohort study of new AMI patients admitted to a hospital investigated whether sex-related differences in the rates of in-hospital mortality due to AMI were associated with disparities in access to optimal medical services. A total of 97,718 patients were diagnosed with AMI (Code ‘I21’ of the International Classification of Disease, 10th revision; ICD-10) as their primary condition between 2003 and 2007. Of those, 296 were referred to a clinic, 1806 were transferred to other hospitals, and 102 patients were younger than 20 years. These patients were excluded from the study population. An additional 10,185 patients were excluded because we could not identify the type of AMI (ST elevation myocardial infarction [STEMI], I21.0–3; non-STEMI [NSTEMI], I21.4; unspecified, I21.9 on the ICD–10). Thus, 85,329 patients were selected for analysis. We confirmed that AMI was the initial diagnosis by examining the database for non-AMI primary or secondary disease claims for each patient between December 1994, the year the computerized billing system was initiated, and December 2002.1,19 We used the claims database to provide information about treatment after admission or death for each patient.19 An ICD-10 diagnostic code consisting of at least 4 digits is necessary to identify AMI type (STEMI, NSTEMI, unspecified); however, 10.4% of the claims (n = 10,185) used the 3-digit code, “I21.” This may be because the AMI type had not been determined at the time of diagnosis or simply because the 3-digit code is sufficient for KNHI claims.15,19
Our study was approved by the Institutional Review Boards of the Health Insurance Review and Assessment Service.
Study Variables
The primary outcome variable was 30-day in-hospital mortality rate defined as the proportion of patients with AMI who died within 30 days of follow-up after admission against the number of cases diagnosed with the disease.19 The primary independent variable was sex (male, female).
Covariates consisted of demographic characteristics, severity, and medical and invasive management. The demographic variables included age (20–44, 45–54, 55–64, 65–79, and >80 years) and type of insurance (health insurance, medical aid). Severity variables included type of AMI (STEMI, NSTEMI, unspecified), the presence or absence of coexisting conditions (diabetes, hypertension, chronic obstructive pulmonary disease [COPD], chronic liver disease, chronic renal disease, cerebrovascular disease, anemia, cancer), and the presence or absence of complications. Complications were subdivided into mechanical and arrhythmic complications. Mechanical complications referred primarily to left ventricular dysfunction and included congestive heart failure, left heart failure, cardiomegaly, acquired cardiac septal defects, and cardiogenic shock. Arrhythmic complications (ie, electrical instability) included cardiac dysrhythmias, atrioventricular blocks, and other conduction disorders.15,19,20
To determine whether sex-related differences in the rates of in-hospital mortality due to AMI were associated with disparities in the provision of medical or invasive management, we examined the procedures performed within 30 days of hospital admission.19 Medical management variables included aspirin, thrombolytic drugs (tissue plasminogen activator, urokinase, streptokinase, limaprost, tenecteplase), β-blockers, and cholesterol-lowering drugs (statins, fibrates). Invasive management variables included coronary angiography (CAG), cardiac catheterization, percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG).3,19,20 These medical and invasive management variables were the primary factors associated with in-hospital mortality among patients with AMI.3,19,20
Statistical Analysis
We performed chi-squared tests to evaluate sex-related differences in demographic characteristics and severity among patients with AMI. A multiple logistic regression model was used to evaluate sex-related differences in the rates of medical or invasive procedures and AMI in-hospital mortality. Rates were compared by adjusting for age, insurance type (National Health Insurance, Medical Aid), AMI type (STEMI, NSTEMI, unspecified), presence or absence of coexisting conditions, and presence or absence of complications. Medical or invasive management variables were added to the covariates to compare in-hospital mortality rates.
RESULTS
Patient Characteristics
Several characteristics were significantly different according to sex (Table 1). The proportion of female patients was higher than that of males among those 65 years of age or older (female 75.6% vs male 40.5%), Medical Aid recipients (female 14.8% vs male 6.8%, P < 0.001), and those with mechanical complications (female 8.6% vs male 4.8%, P < 0.001). In contrast, the proportion of male patients was higher than that of females among those diagnosed with STEMI (male 27.8% vs female 22.5%, P < 0.001) and with hypertension as a coexisting condition (male 26.4% vs female 24.1%, P < 0.001). Moreover, the age at onset of AMI differed according to sex (Figure 1). In males, the number of new AMI cases began to increase at the age of 30 years and reached a peak at 64 years of age (n = 1599). In contrast, new AMI cases did not significantly increase in females until the age of 50 years, with the greatest number of new patients occurring at age 76 (n = 1270). In-hospital mortality increased with age in male and female patients.
TABLE 1.
Patient Characteristics According to Sex
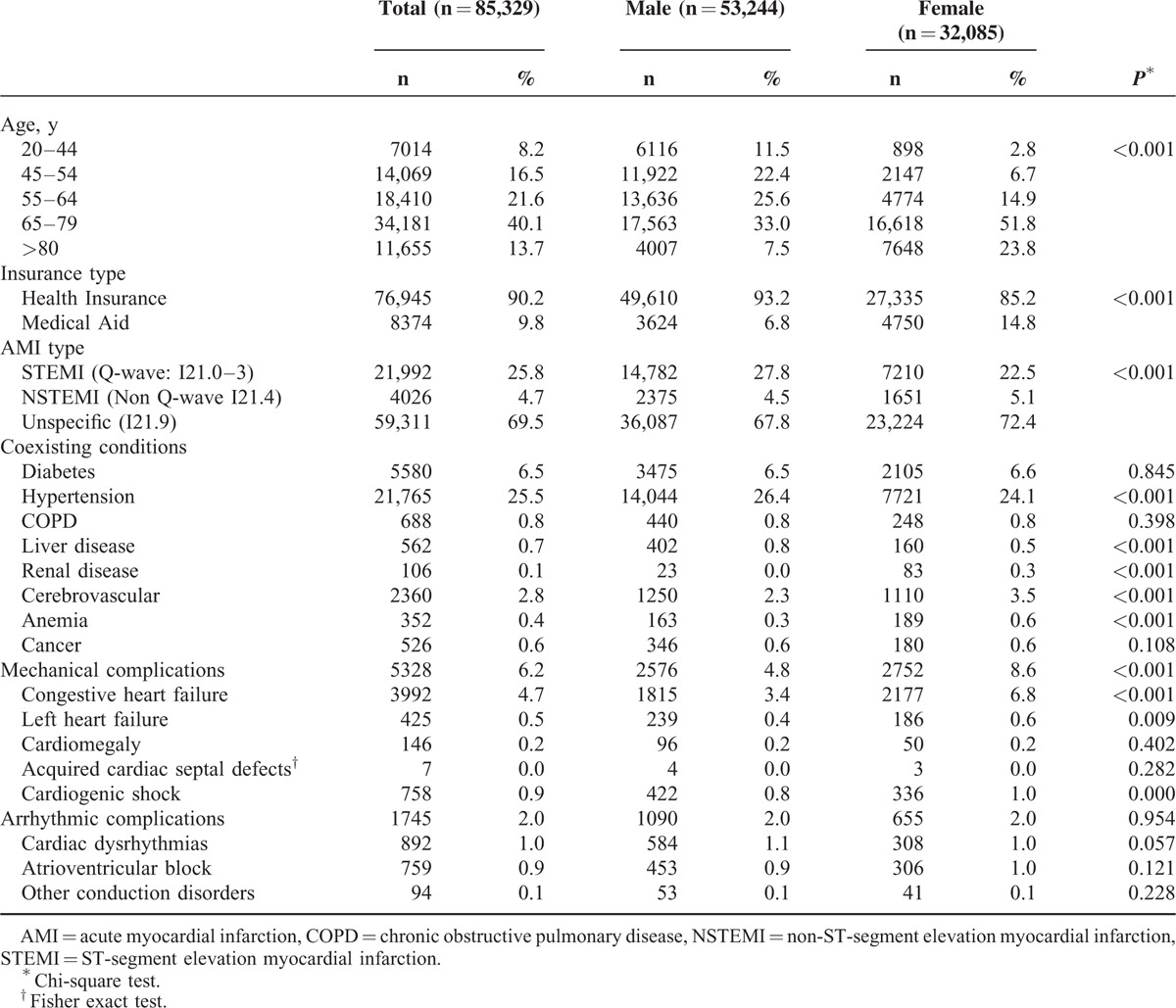
FIGURE 1.
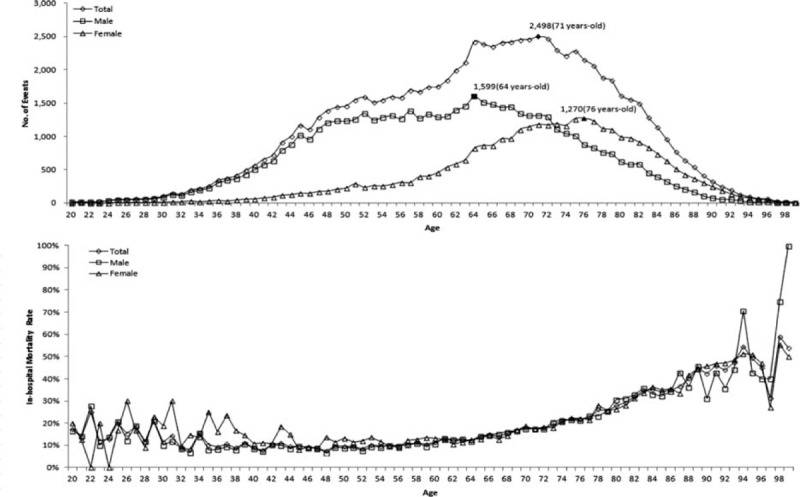
Incidence and in-hospital mortality rate according to age and sex.
Invasive and Medical Management
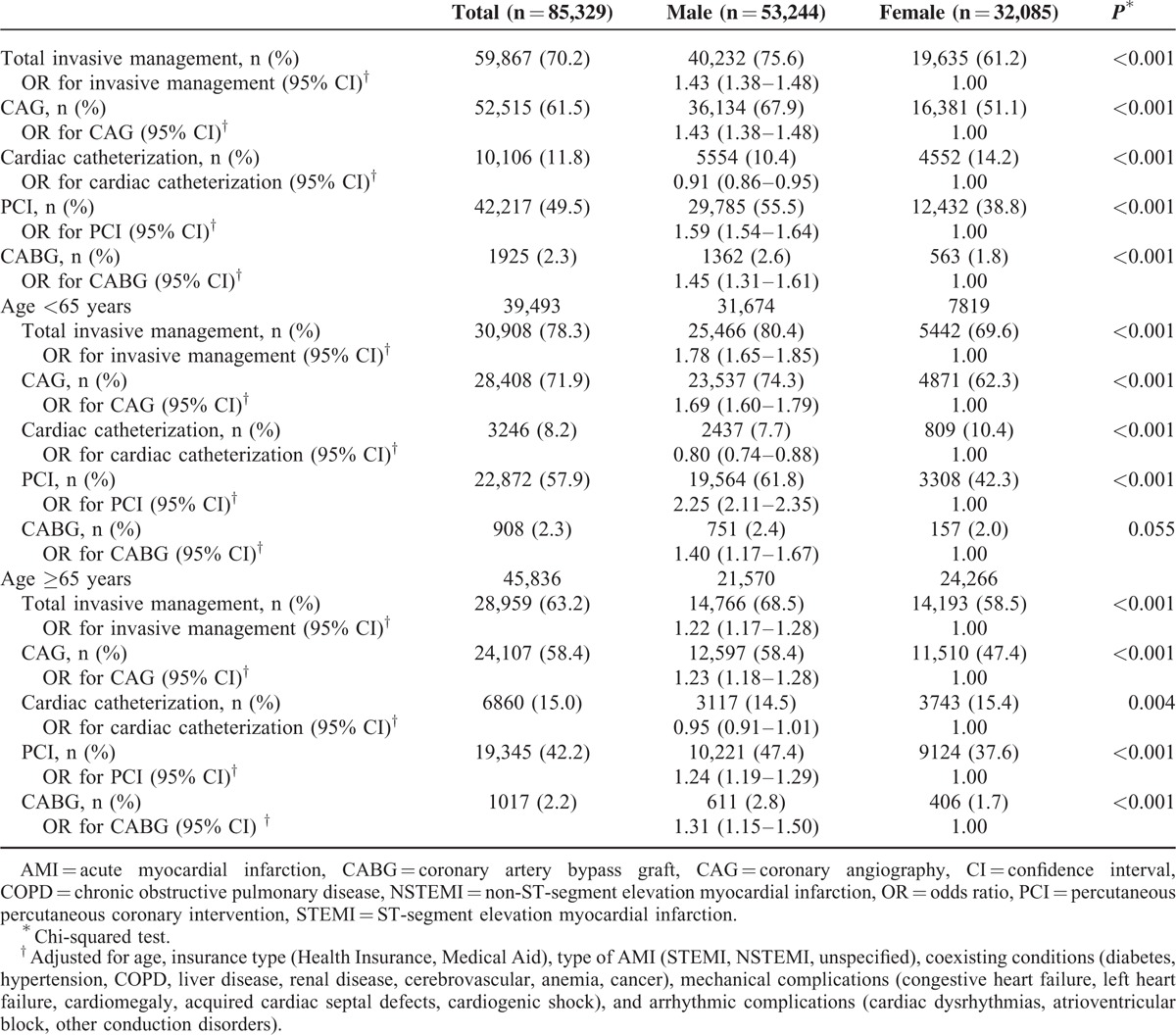
Males received a higher percentage than female patients of all invasive procedures with the exception of cardiac catheterization (CAG: male 67.9% vs female 51.1%, P < 0.001; PCI: male 55.5% vs female 38.8%, P < 0.001; CABG: male 2.6% vs female 1.8%, P < 0.001; Table 2). After adjusting for age, insurance type, AMI type, coexisting conditions, and complications, male patients were more likely than females to undergo invasive procedures (CAG: odds ratio [OR] 1.43, 95% confidence interval [CI] 1.38–1.48; PCI: OR 1.59, 95% CI 1.54–1.64; CABG: OR 1.45, 95% CI 1.31–1.61).
TABLE 2.
Odds Ratios of Patients With AMI Receiving Invasive Management Following Hospital Admission According to Sex
Conversely, the rate of medical management procedures performed after admission was higher in female than in male patients (male vs female: aspirin 42.4% vs 65.8%, P < 0.001; thrombolytic drugs 3.8% vs 4.6%, P < 0.001; β-blocker 30.8 vs 46.6%, P < 0.001; and cholesterol-lowering drugs 24.6 vs 38.4%, P < 0.001; Table 3). However, after adjusting for age, insurance type, AMI type, coexisting conditions, and complications, male patients had a higher probability of receiving medical management than female patients (aspirin: OR 1.06, 95% CI 1.02–1.11; thrombolytic drugs: OR 1.22, 95% CI 1.13–1.31; β-blocker: OR 1.05, 95% CI 1.01–1.08). In our sample, 59.5% (n = 31,674) of male patients were younger than 65 years, whereas 75.6% (n = 24,266) of female patients were 65 years of age or older. The sex-related differences in age distribution prompted us to conduct a further analysis of younger (<65 years) compared with older (≥65 years) patients.
TABLE 3.
Odds Ratios of Patients With AMI Receiving Medical Management Following Hospital Admission According to Sex
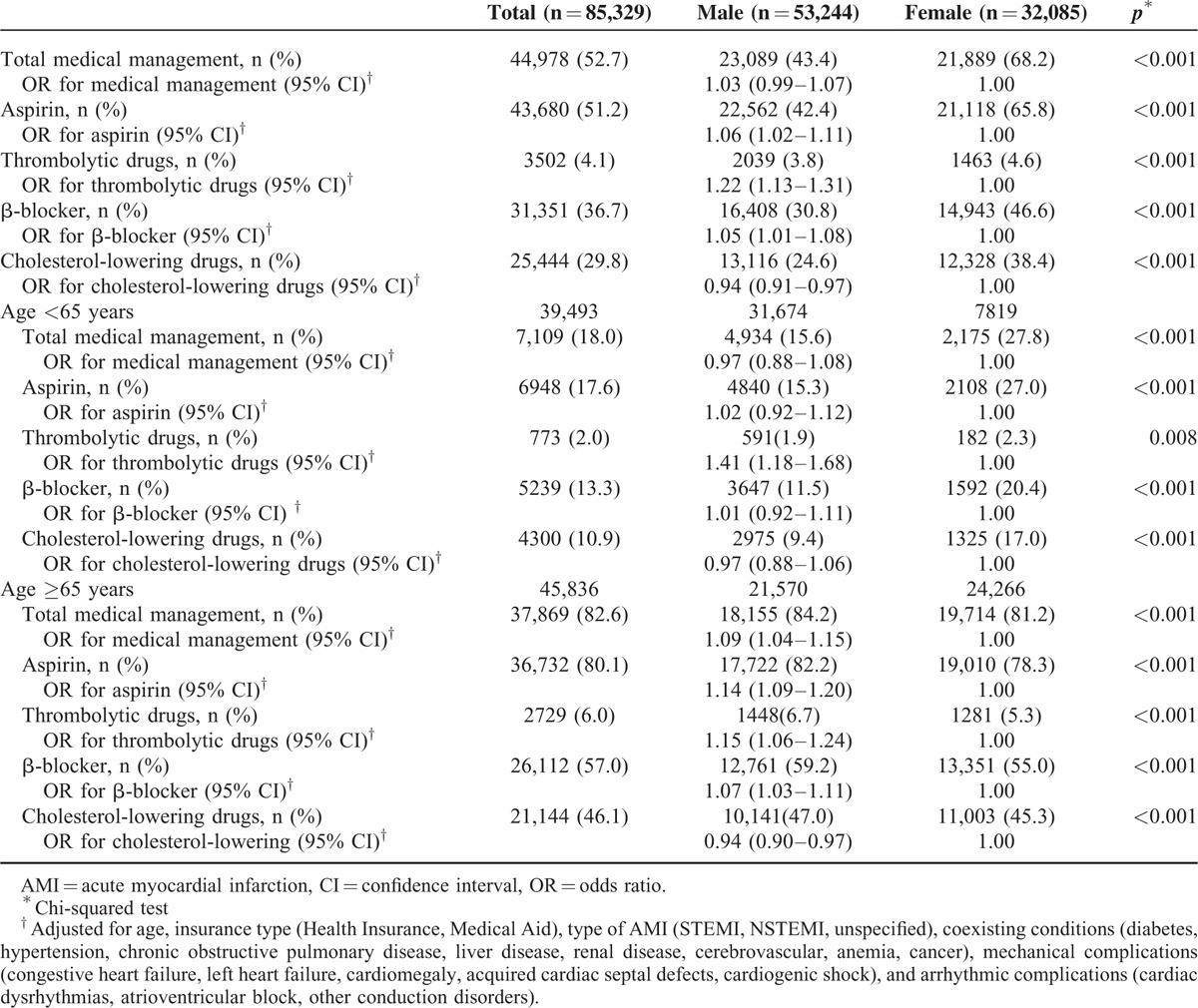
We found that males in both age groups (<65 and ≥65 years) had a higher probability of undergoing invasive procedures than female patients (<65 years: CAG, OR 1.69, 95% CI 1.60–1.79; PCI, OR 2.25, 95% CI 2.11–2.35; CABG, OR 1.40, 95% CI 1.17–1.67; 65 years of age or older: CAG, OR 1.23, 95% CI 1.18–1.28; PCI, OR 1.24, 95% CI 1.19–1.29; CABG, OR 1.31, 95% CI 1.15–1.50; Table 2). Furthermore, the odds of receiving medical treatment were higher for male than for female patients who were 65 years of age or older (aspirin, OR 1.14, 95% CI 1.09–1.20; thrombolytic drugs, OR 1.15, 95% CI 1.06–1.24; β-blocker, OR 1.07, 95% CI 1.03–1.11; Table 3). Male patients younger than 65 years of age were 1.41 times more likely to receive thrombolytic drugs than their female counterparts (95% CI 1.18–1.68).
In-Hospital Mortality
The in-hospital mortality rate was higher in female (21.2%) than in male patients (14.6%; crude OR 1.58, 95% CI 1.52–1.64; Table 4). After adjusting for demographic characteristics and severity, female patients had a higher probability of death within 30 days after admission than males (OR 1.08, 95% CI 1.04–1.13); however, following additional adjustment for performance of invasive and medical management procedures, the odds did not differ between male and female patients (OR 1.04, 95% CI 0.99–1.08). The analysis of patients according to younger (<65 years) and older (≥65 years) age groups revealed similar results.
TABLE 4.
Odds Ratios of Death Within 30 Days After Admission According to Sex
DISCUSSION
Age and sex-related differences in AMI mortality rates have been well documented. Previous studies have shown that in-hospital mortality rates due to AMI increase with age, and are higher in females than in males. In-hospital mortality in elderly patients is associated with higher incidences of congestive heart failure, arrhythmia, atrioventricular block, reinfarction, and multivessel disease, and lower frequencies of thrombolytic therapy, coronary angiography, and angioplasty.1,21,22 The high in-hospital mortality rate among females has been attributed to the large proportion of elderly female patients, higher incidences of hypertension, diabetes, heart failure, and left ventricular failure, and lower procedural rates for thrombolytic therapy, coronary angiography, and angioplasty during hospitalization.1,6,7
The results of previous studies suggested that the high mortality rate among females patients with AMI may be explained by the greater proportion of elderly female patients, and as a consequence, greater AMI severity,6–9 as well as the fact that females receive fewer treatments such as PCI and CABG than males.13,23 In our study population, a higher proportion of female than male patients aged 65 years or older were protected under Medical Aid and had mechanical complications, whereas a higher proportion of male patients were diagnosed with STEMI and had coexisting conditions including hypertension. Differences in age distribution and severity according to sex are likely to contribute to sex-related differences in the rates of in-hospital mortality. Indeed, we found that females with AMI had a higher 30-day mortality rate than male patients (male, 14.6% vs females, 21.2%). However, the 30-day mortality rate in females remained higher than that of males after adjusting for age and severity, suggesting that other factors contributed to the sex-related difference in mortality.
In our final model, which was further adjusted for invasive and medical management procedures, the sex-related difference in in-hospital mortality rates disappeared, suggesting that this disparity was related to differences in procedure rates rather than age and severity. In this model, the comparison of invasive and medical management performance rates between males and females revealed that rates were higher for males than females, suggesting that female patients did not receive optimal treatment for AMI as often as male patients.
Previous studies have shown an association between lower procedure rates and higher mortality in female patients with AMI.23,24 Hanratty et al23 attributed their finding of higher in-hospital mortality rates among females compared with males (30% vs 19%, crude OR 1.78, 95% CI 1.46–2.18) to the delivery of inappropriate procedures following hospital admission. Furthermore, Vaccarino et al24 reported that female patients younger than 65 years of age had a higher in-hospital mortality rate than males of the same age, and concluded that less frequent delivery of thrombolytic therapy was a contributing factor. One explanation for lower procedure rates in females is the high proportion of elderly patients. Ischemic heart disease is rarely detected in females before the age of 70 years because of the antiatherogenic effect of the female sex hormone, estrogen.4,24,25 For this reason, more elderly patients with AMI are female. We found that AMI occurred at a later age in females than in males. The frequency of AMI cases was highest at 64 years of age in males and 76 years in females. Thus, it is likely that invasive procedures such as CABG and PCI were performed less frequently in elderly female patients. However, our analysis of patients grouped according to younger (<65 years) and older (≥65 years) ages revealed that invasive procedures were performed less often in females compared with males in both age groups, indicating that advanced age did not explain the lower rates of invasive procedures in females.
Taken together, these findings show the possibility that the health inequality in female patients with AMI arises from social inequality rather than biological differences such as age and severity. Health inequality implies that an individual's level of health is not determined by biological factors, but rather, by inequality in conventional social factors such as social class, sex, race, and place of residence differentiating opportunities or quality of life among individuals, for which an individual's risk of disease or level of health is differently structured.14 According to The Global Gender Gap Report26 published by The World Economic Forum in October 2014, South Korea ranked 117 of 142 countries, indicating that females severely trail males in economic participation and opportunity, educational attainment, health and survival, and political empowerment. Moon et al27 documented several cases in which female patients in Korea received less aggressive management than males. Furthermore, the cause of myocardial infarction in females is less well understood than in males, complicating the delivery of appropriate care for females who experience AMI symptoms.28
Moreover, although AMI symptoms differ in males and females due to anatomical differences, most of the information and educational materials available to the public focus on AMI symptoms in males. Thus, public awareness of sex-related differences in AMI symptoms is not sufficient, and may hinder females from seeking or receiving appropriate treatment in a timely fashion. Chest pain, which is considered to be the classic symptom of acute coronary syndrome (ACS), is experienced more often by males than females. Females generally experience atypical symptoms, particularly nausea, vomiting, dyspnea, and abdominal symptoms, rather than chest pain.4,29–31 Because chest pain is the classic ACS symptom, patients tend to visit the hospital only if they have chest pain that they perceive as serious enough to require treatment. However, females who do not experience chest pain are less likely to seek or receive immediate emergency care, leading to a delay in treatment.32,33 Korea is a traditional patriarchal society in which the economic participation of females is low compared with that of males,26 and the family economy is dependent on males. Thus, the decision for a female to undergo expensive procedures may be delayed accordingly. These socioculture characteristics could have contributed to the disparity in treatment and subsequent higher in-hospital AMI mortality rates among the females observed in our study.
We were unable to specify the AMI type for all of the patients in our study. ICD-10 diagnosis codes with at least 4 digits are necessary to distinguish between STEMI and NSTEMI AMI types. We found that 10.4% of the claims (n = 10,185) used the 3-digit code, “I21,” perhaps because the type of AMI may not have been determined at the time of diagnosis or simply because the 3-digit code is sufficient for provider reimbursement claims to the KNHI.34 Nevertheless, we believe that STEMI patients were rare among those subjects whose AMI type was not identifiable. Healthcare providers would likely have stated on the claim that the patient was diagnosed with STEMI because the NHI payment model is fee-for-service, and the fee for STEMI is particularly high. Moreover, the results of a separate analysis that included patients whose AMI type could not be identified did not differ from those of the main analysis. Thus, the exclusion of subjects whose AMI type could not be identified was unlikely to have had a major impact on our results.
An additional limitation was the validation of the diagnosis of AMI. This study used the KNHI Claims Database, which was designed for cost claim issues, not research. Thus, the validation of diagnoses may be problematic. It might have caused an underestimation of prescriptions. However, when the Korea Centers for Disease Control and Prevention and the Health Insurance Review and Assessment Service jointly investigated medical records for some claim samples in which AMI (ICD-10: I21) was diagnosed as a primary disease, AMI was confirmed in 93.9% of the samples.19,35
Despite these limitations, our study had several strengths. We examined a large sample of new AMI patients admitted to Korean hospitals over a 5-year period to assess sex-related differences in AMI in-hospital mortality and to identify the underlying causes. Furthermore, it divided the study population according to age (<65, ≥65) and found sex difference in mortality in older age (≥65) as well as younger age (<65). Previous studies have found higher in-hospital mortality rates among females compared with males in the younger age bracket; however, no sex-related differences in in-hospital mortality rates have been reported among older patients.24,36 Those studies have suggested that the distinct pathophysiology of coronary heart disease in premenopausal or middle-aged women may be a major contributor of making sex difference in AMI mortality. It is based on the hypothesis that the pathophysiology of coronary heart disease in premenopausal or middle-aged women may differ from the more common disease of older women and of men. Looking at the detail, sex differences in AMI mortality showed only in the younger age group (<65); plaque erosions were the predominant abnormality in premenopausal women who died suddenly, whereas rupture of plaques was more common in older women and in men; younger women who died suddenly of coronary causes had less narrowing of the coronary arteries than older women or men.4,24 As a result, those studies have highlighted that female sex itself is not an independent risk factor for in-hospital mortality.
However, this study showed that AMI in-hospital mortality was higher in women compared with men regardless of age. This result brought into question the possibility of other factors besides biological factors. Our analysis showed that less aggressive treatment in women was significant factor to explain sex differences in AMI in-patient mortality. It was the same in all the age groups. Also, in a regard that a major limitation which previous studies couldn’t confirm gender differences in AMI mortality of the older age group was the small size of sample,24 it would be meaningful that this study analyzed sex differences in AMI in-hospital mortality of all age groups using a nationwide NHI claims data.
Moreover, we compared the performance rates of invasive procedures, which are significantly associated with AMI in-hospital mortality, and medical management strategies according to sex to determine whether procedure rates in males and females were related to in-hospital mortality. Few previous studies have found sex-related differences in medical treatment for myocardial infarction, with the exception of reperfusion therapy.4,27
In conclusion, we found that the 30-day mortality rate of inpatients with AMI in Korean hospitals was higher in females than in males, possibly because female patients received fewer invasive and medical procedures than males. Same results were shown in an additional analysis conducted with the study population divided into younger age (<65) and older age (≥65). Our findings showed the possibility that differences in the health care services provided to males and females in the hospital were likely to be influenced more by social inequality than biological differences. Further study is being needed to determine the reasons for these sex differences. Of the many relevant social inequalities that should be addressed, information about the signs and symptoms of AMI, with a particular focus on sex-related differences, is the most urgently needed. Government health policies, public education materials, and health-promotion campaigns that explain sex-related differences in early AMI symptoms must be developed to facilitate the recognition and early treatment of AMI in females.
Footnotes
Abbreviations: ACS = acute coronary syndrome, AMI = acute myocardial infarction, CABG = coronary artery bypass graft, CAG = coronary angiography, CFR = Case-fatality Rate, CI = confidence interval, COPD = chronic obstructive pulmonary disease, ICD-10 = the International Classification of Disease, 10th revision, LAD = left anterior descending artery, NSTEMI = non-ST elevation myocardial infarction, OECD = Organization for Economic Cooperation and Development, OR = odds ratio, PCI = percutaneous coronary intervention, STEMI = ST-segment Elevation Myocardial Infarction, t-PA = tissue plasminogen activator.
The authors report no conflicts of interest.
REFERENCES
- 1.Hong JS, Kang HC, Lee SH, et al. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997–2007. Korean Circ J 2009; 39:467–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abildstrom SZ, Rasmussen S, Rosén M, et al. Trends in incidence and case fatality rates of acute myocardial infarction in Denmark and Sweden. Heart 2003; 89:507–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stukel TA, Lucas FL, Wennberg DE. Long-term outcomes of regional variations in intensity of invasive vs medical management of Medicare Patients with acute myocardial infarction. JAMA 2005; 293:1329–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park JS, Kim YJ, Shin DG, et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: from the Korean Acute Myocardial Infarction Registry (KAMIR) study. Clin Cardiol 2010; 33:E1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borzak S, Weaver WD. Sex and outcome after myocardial infarction: a case of sexual politics? Circulation 2000; 102:2458–2459. [DOI] [PubMed] [Google Scholar]
- 6.Karlson BW, Herlitz J, Hartford M. Prognosis in myocardial infarction in relation to gender. Am Heart J 1994; 128:477–483. [DOI] [PubMed] [Google Scholar]
- 7.Fiebach NH, Viscoli CM, Horwitz RI. Differences between women and men in survival after myocardial infarction: biology and methodology. JAMA 1990; 263:1092–1096. [PubMed] [Google Scholar]
- 8.Gottlieb S, Harpaz D, Shotan A, et al. Sex differences in the management and outcome after acute myocardial infarction in the 1990 s: a prospective observational community-based study. Circulation 2000; 102:2484–2490. [DOI] [PubMed] [Google Scholar]
- 9.Marrugat J, Sala J, Masiá R, et al. Mortality differences between men and women following first myocardial infarction. RESCATE Investigators. Recursos Empleados en el Síndrome Coronario Agudo y Tiempo de Espera. JAMA 1998; 280:1405–1409. [DOI] [PubMed] [Google Scholar]
- 10.Gan SC, Beaver SK, Houck PM, et al. Treatment of acute myocardial infarction and 30-day mortality among women and men. N Engl J Med 2000; 343:8–15. [DOI] [PubMed] [Google Scholar]
- 11.Yarzebski J, Col N, Pagley P, et al. Gender differences and factors associated with the receipt of thrombolytic therapy in patients with acute myocardial infarction: a community-wide perspective. Am Heart J 1996; 131:43–50. [DOI] [PubMed] [Google Scholar]
- 12.Hollenbeak CS, Weisman CS, Rossi M, et al. Gender disparities in percutaneous coronary interventions for acute myocardial infarction in Pennsylvania. Med Care 2006; 44:24–30. [DOI] [PubMed] [Google Scholar]
- 13.Kanamasa K, Ishikawa K, Hayashi T, et al. Increased cardiac mortality in women compared with men in patients with acute myocardial infarction. Intern Med 2004; 43:911–918. [DOI] [PubMed] [Google Scholar]
- 14.House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Soc Behav 2002; 43:125–142. [PubMed] [Google Scholar]
- 15.Hong JS, Kang HC. Seasonal variation in case fatality rate in Korean patients with acute myocardial infarction using the 1997-2006 Korean National Health Insurance Claims Database. Acta Cardiol 2014; 69:513–521. [DOI] [PubMed] [Google Scholar]
- 16.National Health Insurance Corporation. National Health Insurance Program of Korea. Seoul: Health Care Delivery System; 2007. [Google Scholar]
- 17.Kang HC, Hong JS. Do differences in profiling criteria bias performance measurements? Economic profiling of medical clinics under the Korea National Health Insurance program: an observational study using claims data. BMC Health Serv Res 2011; 11:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang HC, Hong JS, Park HJ. Development of peer-group-classification criteria for the comparison of cost efficiency among general hospitals under the Korean NHI program. Health Serv Res 2012; 47:1719–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong JS, Kang HC, Lee SH. Comparison of case-fatality rates for acute myocardial infarction in weekday vs. weekend admissions in South Korea. Circ J 2010; 74:496–502. [DOI] [PubMed] [Google Scholar]
- 20.Kostis WJ, Demissie K, Marcella SW, et al. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 2007; 356:1099–1109. [DOI] [PubMed] [Google Scholar]
- 21.Manolio TA, Furberg CD. Age as a predictor of outcome: what role does it play? Am J Med 1992; 92:1–6. [DOI] [PubMed] [Google Scholar]
- 22.Paul SD, O’Gara PT, Mahjoub ZA, et al. Geriatric patients with acute myocardial infarction: cardiac risk factors profiles, presentation, thrombolysis, coronary interventions, and prognosis. Am Heart J 1996; 131:710–715. [DOI] [PubMed] [Google Scholar]
- 23.Hanratty B, Lawlor DA, Robinson MB, et al. Sex differences in risk factors, treatment and mortality after acute myocardial infarction: an observational study. J Epidemiol Community Health 2000; 54:912–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaccarino V, Parsons L, Every NR, et al. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med 1999; 341:217–225. [DOI] [PubMed] [Google Scholar]
- 25.Gorodeski GI. Impact of the menopause on the epidemiology and risk factors of coronary artery heart disease in women. Exp Gerontol 1994; 29:357–375.Review. [DOI] [PubMed] [Google Scholar]
- 26.World Economic Forum. The Global Gender Gap Report 2014. Geneva: 2014. http://www3.weforum.org/docs/GGGR14/GGGR_CompleteReport_2014.pdf (accessed December 2, 2014) [Google Scholar]
- 27.Moon KW, Lee MY, Chung WS, et al. Sex differences in early management of patients with acute myocardial infarction (AMI) in the 1990s. Korean Circ J 2003; 32:85–91.[Korean]. [Google Scholar]
- 28.Kim CJ, Hur HK, Lee JK. A study on knowledge about myocardial infarction in Korean population. J Korean Acad Adult Nurs 1999; 11:288–297.[Korean]. [Google Scholar]
- 29.Chen W, Woods SL, Wilkie DJ, et al. Gender differences in symptom experiences of patients with acute coronary syndromes. J Pain Symptom Manage 2005; 30:553–562. [DOI] [PubMed] [Google Scholar]
- 30.Goldberg R, Goff D, Cooper L, et al. Age and sex differences in presentation of symptoms among patients with acute coronary disease: the REACT Trial. Rapid Early Action for Coronary Treatment. Coron Artery Dis 2000; 11:399–407. [DOI] [PubMed] [Google Scholar]
- 31.Milner KA, Funk M, Richards S, et al. Gender differences in symptom presentation associated with coronary heart disease. Am J Cardiol 1999; 84:396–399. [DOI] [PubMed] [Google Scholar]
- 32.DeVon HA, Ryan CJ. Chest pain and associated symptoms of acute coronary syndromes. J Cardiovasc Nurs 2005; 20:232–238.Review. [DOI] [PubMed] [Google Scholar]
- 33.Lee EK. Gender differences in coronary artery disease knowledge and symptom perceptions in patients with acute coronary syndromes. Graduate School of Soonchunhyang University. Asan: 2009 [Korean]. [Google Scholar]
- 34.Hong JS, Kang HC. Regional differences in treatment frequency and case-fatality rates in Korean patients with acute myocardial infarction using the Korea National Health Insurance Claims Database: Findings of a large retrospective cohort study. Medicine 2014; 93:e287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim J. Construction of National Surveillance System for Cardiovascular & Cerebrovascular Disease. Korea Centers for Disease Control and Prevention, Health Insurance Review & Assessment Service. Seoul: 2006 [Korean]. [Google Scholar]
- 36.Bueno H, Vidán MT, Almazán A, et al. Influence of sex on the short-term outcome of elderly patients with a first acute myocardial infarction. Circulation 1995; 92:1133–1140. [DOI] [PubMed] [Google Scholar]


