Abstract
Primary pulmonary paraganglioma is a rare disease. We report a case of a 37-year old female patient with space-occupying lesions in the right lower pulmonary lobe during a routine examination without any symptoms. The patient underwent video-assisted thoracoscopic surgery (VATS) resection of the right middle lobe and dissection of hilar and mediastinal lymph nodes under general anesthesia. She recovered without recrudescence. Preoperative diagnosis is difficult. Accurate diagnosis requires pathological examination, and immunohistochemical test is particularly important. Complete resection is the first treatment option for solitary primary pulmonary paraganglioma; however, VATS is a better technique. Given the high local control rates and few complications of radiotherapy, it is considered as a standard treatment.
INTRODUCTION
Paraganglioma is a rare disease that affects 2 to 5 people per million per year.1 A limited number of cases and sample clinical studies have been reported about primary pulmonary paraganglioma. In this article, we report 1 case of this disease and introduce its diagnosis and treatment.
CASE PRESENTATION
Primary pulmonary paraganglioma is a rare disease and seldom reported. A 37-year-old Chinese stay-at-home woman was treated in our department. This patient had space-occupying lesions in the right lower pulmonary lobe during a routine examination without any symptoms. Her past medical history was unremarkable, and no similar cases were found in her family. Her physical examination did not reveal any abnormalities. Chest computed tomography (CT) showed a round-like soft tissue of approximately 3 cm × 2.8 cm in size. The CT values of the plain scan and enhancement scan were 44 and 245 Hu, respectively. No enlarged lymph nodes were observed at the bilateral hilus pulmonis or mediastina (Figure 1). Imaging examination showed a tumor with a rich blood supply beside the hilus pulmonis of the right lung combined with right middle lobe atelectasis. Tumor markers in lung cancer including carcino-embryonic antigen, neuron-specific enolase, cytokeratin fragment antigen 21-l, and squamous cell cancer were negative. Clinical examination eliminated other primary lesions. The patient underwent video-assisted thoracoscopic surgery (VATS) resection of the right middle lobe and dissection of hilar and mediastinal lymph nodes under general anesthesia on October 2013. During the operation, a lesion was found near the hilus pulmonis of the right middle lobe. The round-like and hard lesion was approximately 4 cm × 3 cm × 3 cm in size. The lesion also showed a relatively clear boundary, without evident membrane indentation, and was combined with the right middle pulmonary atelectasis and consolidation. No abnormality was observed in the other parts. Pathological diagnosis for intraoperative frozen section indicated benign tumor. Postoperative pathological diagnosis showed the following. First, the (right middle) lung tumor cells were fasciculate and aciniform, and between cell nests were thin vascular net. Moreover, the tumor cells had abundant granular, pink cytoplasm, and a few tumor giant cells and karyokinesis sign were observed. Interstitial fibrous tissue hyperplasia and hyaline degeneration were found in some areas. Immunohistochemistry showed that the tumor was paraganglioma. Second, no tumor was found at the incisal margin of bronchus. Third, the sending sample of lymph showed reactive hyperplasia. Immunohistochemical test results (Figure 2) revealed chromogranin A(+), synaptophysin(+), CD56(+), Ki-67 index of approximately 2%, creatine kinase (CK)(−), Vimentin(−), LCA(−), CK7(−), CK5/6(−), thyroid transcription factor (−), P63(−), human melanoma Black 45 (−), CD34 (vessel+), CD31 (vessel+), S100 (lesion+), Desmin (−), and MyoD1(−). The postoperative recovery of the patient was good, and the patient did not complain of obvious discomfort. After surgery, the case was followed until September 2014, and the tumor did not recrudesce.
FIGURE 1.

The chest computed tomography (CT) showed a round-like soft tissue of approximately 3 cm × 2.8 cm in size. The CT values of the plain scan and enhancement scan were 44 and 245 Hu, respectively. No enlarged lymph nodes were observed at the bilateral hilus pulmonis or mediastina.
FIGURE 2.
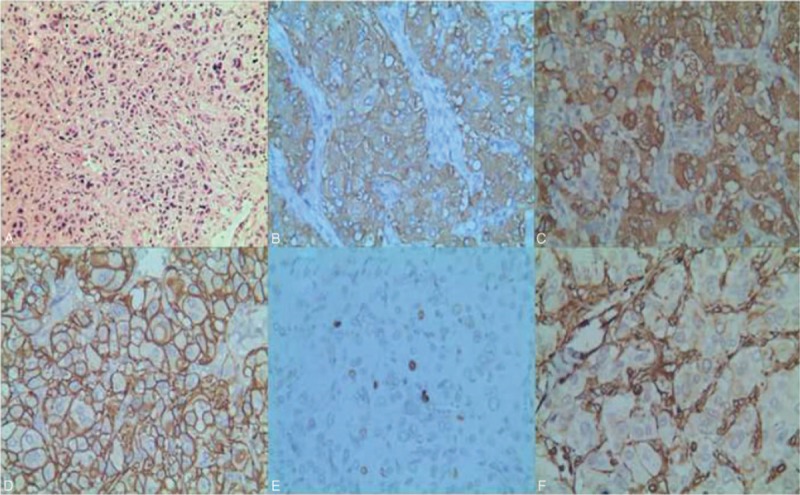
First, the (right middle) lung tumor cells were fasciculate and aciniform, and between cell nests were thin vascular net. Moreover, the tumor cells had abundant granular, pink cytoplasm, and a few tumor giant cells and karyokinesis sign were observed. Interstitial fibrous tissue hyperplasia and hyaline degeneration were found in some areas. Immunohistochemistry showed that the tumor was paragangliomea. Second, no tumor was found at the incisal margin of bronchus. Third, the sending sample of lymph showed reactive hyperplasia. Immunohistochemical test results (A-hematoxylin and original magnification 100×). Immunohistochemical test results: synaptophysin (syn)(+) (B-original magnification 400×), chromogranin A (CgA)(+) (C-original magnification 400×), CD56(+) (D-original magnification 400×), Ki-67 index about (2%) (E-original magnification 400×), and Vimentin(−) (F-original magnification 400×).
DISCUSSION
Paraganglioma originates from parasympathetic ganglion. This disease mainly occurs at body parts with rich paraganglions, such as head, neck, mediastinum, adrenal gland, and posterior peritoneum, even bladder, duodenum, and thyroid2 as reported. Paraganglioma is a rare disease that affects 2 to 5 people per million per year.1 Primary pulmonary paraganglioma is even rarer. Paragangliomas are slowly growing tumors, present as painless masses, and have a culture doubling time of approximately 42 years. The tumors are potentially low-grade malignant.3 However, invasive biological behaviors have been reported; these behaviors can cause adjacent lymph node metastasis,4 such as mediastinal lymph node.5 In general, most of the primary pulmonary paragangliomas do not show evident clinical symptoms. Few of these symptoms are cough and chest pain. The susceptible population is unknown. Other pulmonary benign tumors and special infections (eg, tuberculoma and inflammatory pseudotumor) are hard to distinguish through imaging examination. Therefore, preoperative diagnosis is difficult, and accurate diagnosis requires pathological examination. Pathologically, primary pulmonary paraganglioma should be identified from carcinoids and other diseases. Hence, immunohistochemical test is particularly important. Several authors summarized the genetic and clinical appearances of paragangliomas, attempting to identify the mutation of genes and determine the algorithm about genetic test6 and aiming an accurate treatment and better prognosis.
In this case, the patient refused the fibrobronchoscopic examination based on the following reasons. First, according to the imaging examination before surgery, the tumor had rich blood supply; therefore, the patient is at a high risk of bleeding in the process of fibrobronchoscopic forceps biopsy.7 Second, completely resection of the tumor should be conducted before operation.
Complete resection is the first treatment option for solitary primary pulmonary paraganglioma. However, the postoperative complication rate for such benign tumor is too high. Thoracoscopic surgery becomes the standard method of early lung cancer treatment.8 VATS allows excellent exposure of the operating field of vision and shows fine structure of lesions. Furthermore, VATS causes less surgical injury and postoperative pain than thoracotomy.9 Considering the reduced postoperative complications, conduciveness to postoperative recovery, and patient's aesthetic requirements, we preferred the VAST operation.8 Based on the condition during the operation, we have an option to continue VATS or perform open thoracotomy. In this case, the postoperative recovery was smooth without any complications.
During the surgery, the hilar and mediastinal lymph nodes were enlarged with a hard texture. To distinguish from malignant lymph node enlargement, we performed lymph node dissection.
Many authors proposed that paraganglioma is sensitive to radiation therapy, without serious side effects.10,11 Given the high local control rates and few complications, some authors consider radiotherapy as a first-choice treatment for paraganglioma.12 The effects of external beam radiation therapy have been evaluated. However, external beam radiation therapy can only be considered when local disease progresses.13 The use of the chemotherapy regimen is not unanimously approved. In some metastasis cases, sorafenib use has been reported.14,15
Pulmonary paragangliom needs to be differentiated from the following kinds of diseases, including lung cancer, lung tuberculoma, inflammatory pseudotumor, hamartoma, lung carcinoid tumor and lung metastasis tumor, etc.
CT and magnetic resonance imaging are the important imaging examination methods of positioning and qualitative diagnosis of paraganglioma. CT scan of pulmonary paraganglioma shows isodensity or slightly lower density. Enhanced scan shows significant enhancement.16 T1W1 of magnetic resonance imaging shows isodensity and low signal. T2W1 shows medium, high, or uneven mixed signal. DW1 shows high signal. Enhanced scan shows that the parenchyma of the tumor is partially obviously enhanced. The occupied effect of the tumor causes the corresponding clinical symptoms.17
Lung Cancer
Derived from bronchial epithelial cells and appears to invasive growth. Imaging examination shows that the tumor invades bronchi, blood vessels, adjacent tissues, and organs. The obstructive changes appear.18 Pulmonary paraganglioma is mainly located around blood vessels and nerve. Tumor is closely related to pulmonary blood vessels and nerves, rather than bronchia. This is the key point to differentiate pulmonary paraganglioma from lung cancer.16
Lung Metastasis Tumor
Multiple nodules in bilateral lungs with clear edge and uniform density, mainly in medium, lower, and peripheral lung field. The hilar nodes are enlarged. There is a history of primary malignant tumor, which can be differentiated by CT multidimensional reconstruction.
Pulmonary Tuberculoma
Pulmonary tuberculoma is mainly appeared in the dorsal pulmonary segment with uniform density and smooth boundary. The long rough burrs can be observed in some patients; enhanced scan shows the nonenhanced or circular enhanced focus. The caseous necrosis can be observed in the center of focus. The satellite foci are observed around the focus. The pleura is thickened. The hilar and mediastinal lymph nodes are not enlarged. The focus is not slowly absorbed or not absorbed after antituberculosis treatment.18,19
Pulmonary Inflammatory Pseudotumor
It is located around the lung field, mainly confined to a leaf. The shape is irregular. The focus often has the wide fundus and adheres on the pleura. The adjacent pleura is thickened. Enhanced scanning shows high density and homogeneous enhancement. The lesion can be shrank after antiinflammatory treatment.18,20
Hamartoma
The tumor components are complex. Most are carcinoid malformation caused by abnormal development of normal tissues. A few is mesenchymal tumors. Fat and calcification are the manifestation of most hamartomas. Popcorn-like calcification is common in pulmonary hamartoma.21
Lung Carcinoid
The histopathologic characteristics include typical neuroendocrine morphology with positive cytokeratin, the expressions of chromogranin A, synaptophysin, CD56, and other neuroendocrine factors. The expression of Ki-67 index is helpful for differential diagnosis. The feature of imaging examination is absent. The diagnosis needs to be clarified by the combination of clinical manifestations and pathological examination.22
Footnotes
Abbreviations: CK = creatine kinase, CT = computed tomography, VAST = video-assisted thoracoscopic surgery.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Santos P, Pimenta T, Taveira-Gomes A. Hereditary pheochromocytoma. Int J Surg Pathol 2014; 22:393–400. [DOI] [PubMed] [Google Scholar]
- 2.Treglia G, Giovanella L, Caldarella C, et al. A rare case of thyroid paraganglioma detected by (18)F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol 2014; 33:320–321. [DOI] [PubMed] [Google Scholar]
- 3.Kiziltan HS, Ozucer B, Eris AH, et al. Bilateral carotid paraganglioma: surgery and radiotherapy. Clin Med Insights Case Rep 2014; 7:53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi H, Han J, Liu N, et al. A gangliocytic patially glandular paraganglioma with lymph node metastasis. Diagn Pathol 2014; 9:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang JJ, Liu T, Peng F. Primary paraganglioma of the lung: a case report and literature review. J Int Med Res 2012; 40:1617–1626. [DOI] [PubMed] [Google Scholar]
- 6.Martins R, Bugalho MJ. Paragangliomas/pheochromocytomas: clinically oriented genetic testing. Int J Endocrinol 2014; 2014:794187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu LH, Liu CC, Ko JS, et al. Safety of interventional bronchoscopy through complication review at a cancer center. Clin Respir J 2014; doi: 10.1111/crj.12225. (in press). [DOI] [PubMed] [Google Scholar]
- 8.Chung JH, Choi YS, Cho JH, et al. Uniportal ideo-assisted thoracoscopic lobectomy: an alternat ive to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015; 20:813–819. [DOI] [PubMed] [Google Scholar]
- 9.Goto T, Kadota Y, Mori T, et al. Video-assisted thoracic surgery for pneumothorax: republication of a systematic review and a proposal by the guideline committee of the Japanese Association for Chest Surgery. Gen Thorac Cardiovasc Surg 2015; 63:8–13. [DOI] [PubMed] [Google Scholar]
- 10.Elshaikh MA, Mahmoud Ahmed AS, Kinney SE, et al. Recurrent head and neck chemodectomas as comparison of surgical and radiotherapeutic results. Int J Radiat Oncol Biol Phys 2002; 52:953–956. [DOI] [PubMed] [Google Scholar]
- 11.Gilbo P, Morris CG, Amdur RJ, et al. Radiotherapy for benign head and neck paragangliomas: a 45-year experience. Cancer 2014; 120:3738–3743. [DOI] [PubMed] [Google Scholar]
- 12.Smee RI, Jayasekara J, Williams JR, et al. Paragangliomas: presentation and management by radiotherapy at the Prince of Wales Hospital. J Med Imaging Radiat Oncol 2015; 59:229–235. [DOI] [PubMed] [Google Scholar]
- 13.Vogel J, Atanacio AS, Prodanov T, et al. External beam radiation therapy in treatment of malignant pheochromocytoma and paraganglioma. Front Oncol 2014; 4:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin Y, Li Q, Huang W, et al. Successful treatment of paraganglioma with sorafenib: a case report and brief review of the literature. Onco Targets Ther 2013; 6:1559–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gunaldi M, Kara IO, Duman BB, et al. A new approach to the treatment of metastatic paraganglioma: sorafenib. Cancer Res Treat 2014; 46:411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang JJ, Liu T, Peng F. Primary paraganglioma of the lung: a case report and literature review. J Int Med Res 2012; 40:1617–1626. [DOI] [PubMed] [Google Scholar]
- 17.Elsayes KM, Leyendecker JR, Narra VR, et al. Pheochromocytoma of the organ of Zuckerkandl. Unusually small lesion detected with magnetic resonance imaging. Saudi Med J 2005; 26:107–110. [PubMed] [Google Scholar]
- 18.Feng ST, Chen JD, Meng QF, et al. Imaging features of lung carcinoma, pulmonary tuberculoma, and inflammatory pseudotumor on helical incremental dynamic CT scan – a report of 44 cases. Ai Zheng 2006; 25:348–351.[Article in Chinese]. [PubMed] [Google Scholar]
- 19.Im JG, Itoh H, Han MC. CT of pulmonary tuberculosis. Semin Ultrasound CT MR 1995; 16:420–434. [DOI] [PubMed] [Google Scholar]
- 20.Kim TS, Han J, Kim GY, et al. Pulmonary inflammatory pseudotumor (inflammatory myofibroblastic tumor): CT features with pathologic correlation. J Comput Assist Tomogr 2005; 29:633–639. [DOI] [PubMed] [Google Scholar]
- 21.Zehani-Kassar A, Ayadi-Kaddour A, Marghli A, et al. Clinical characteristics of resected bronchial hamartoma. Study of seven cases. Rev Mal Respir 2011; 28:647–653.[Article in French]. [DOI] [PubMed] [Google Scholar]
- 22.Hörsch D, Schmid KW, Anlauf M, et al. Neuroendocrine tumors of the bronchopulmonary system (typical and atypical carcinoid tumors): current strategies in diagnosis and treatment. Conclusions of an expert meeting February 2011 in Weimar, Germany. Oncol Res Treat 2014; 37:266–276. [DOI] [PubMed] [Google Scholar]


