Abstract
Prevalence estimates of depression in hypertensive patients varied widely in existing studies. We conducted a systematic review and meta-analysis of observational studies to summarize the point prevalence of depressive symptoms in adults with hypertension.
Comprehensive electronic searches of PubMed, Web of Knowledge, China National Knowledge Internet (CNKI), Wangfang, and Weipu databases were conducted to identify any study in each database published from initial state to November 31, 2014, reporting the prevalence of depression in hypertensive patients. Random-effects model was used to estimate the prevalence of depressive symptoms. We also limited the analyses to studies using clinical interview and prespecified criteria for diagnosis. All statistical calculations were made by using the Stata Version 12.0 (College Station, TX) and Statsdirect Version 2.7.9.
We identified 41 studies with a total population of 30,796 in the present meta-analysis. The summarized prevalence of depression among hypertensive patients is 26.8% (95% confidence interval (CI): 21.7%–32.3%). Subgroup analysis shows the following results: for male 24.6%, 95% CI: 14.8%–35.9%, for female 24.4%, 95% CI: 14.6%–35.8%. For China: 28.5% (95% CI: 22.2%–35.3%); for other region (22.1%, 95% CI: 12.1%–34.1%); for community: 26.3% (95% CI: 17.7%–36.0%), for hospital: 27.2% (95% CI: 20.6%–34.5%). Estimated prevalence by interview was 21.3% (95% CI: 14.2%–30.0%); prevalence of depressive symptoms adjudicated by self-rating scales was 29.8% (95% CI: 23.3%–36.7%).
The observed heterogeneity in depression prevalence of hypertension may be attributed to differences in method of evaluation. Self-report scales should be cautious of estimating the presence of depression. Thus, interview-defined depression affects approximately one third of hypertensive patients. Effective interventions for depression on patient-centered are needed.
INTRODUCTION
Depression is a significant contributor to the global burden of disease. The World Mental Health Survey conducted in 17 countries found that on average about 1 in 20 people reported having an episode of depression in the previous experience. It is estimated that depression affects 350 million people around the world,1 with a lifetime risk of 7%.2 It will be likely to increase 5.7% of global burden of disease by 2020 and become the second one after ischemic heart disease. People with hypertension were at higher risk of all kinds of cardiovascular diseases.3–6 Approximately one fourth of the adults were diagnosed with hypertension, and the proportion will reach about 1/3 by 2025.7 Many people diagnosed with hypertension usually have tough experience such as somatic symptoms, lower quality of life, and role impairment.8 Above all of these factors may make them easier to get psychological distress, especially depression.9 Improving psychosocial aspects of living have been becoming an important part of building better health care, particularly for patients with hypertension. More and more psychologist have recognized addressing patients’ mental needs as their priority research fields.10 However, the prevalence situation of depression in hypertensive patients is still unclear. For a widely prevalent disease such as hypertension, even modest improvements in some targeted interventions of hypertensive patients may well have a significant impact at the whole population level.
Many studies had reported the prevalence of depression in hypertensive patients, but quantitative estimation for the overall prevalence of depression is scarce. Little is known about depression prevalence in hypertensive patients. Although it has become more convenient to assess depression situation through self-rating scales,11 such methods may focus on somatic symptoms, and these symptoms may be not a prominent symptom of depression and consequently. This may overestimate or underestimate depression prevalence in hypertensive patients.12 Thus, estimating the prevalence of depression in hypertensive patients is the first step toward understanding the burden of disease. We conducted a systematic review and meta-analysis of cross-sectional studies in patients with hypertension to estimate the prevalence of depression and the effects of diagnostic methods on estimation prevalence of depression.
METHODS
Literature Search Strategy
Retrieval online were conducted in the following databases: PubMed, Web of Knowledge, China National Knowledge Internet (CNKI), WanFang, and Weipu. The date of search was from initial state to April 31, 2015. The following search terms were used to identify the potential study: (“hypertension” or “high blood pressure”) and (“prevalence” or “epidemiologic studies”) and (“depression” or “depressive disorder” or “mood disorder” or “affective disorders” or “psychotic” or in all databases. We also retrieved the references of all publications to obtain all studies as possible as we can. Y.L. and P.C. conducted the literatures screening according to inclusion and excluding criteria. L.C. judged the disagreement.
Criteria for Inclusion
The following criteria were used for screening literature. First, study design included cross-sectional study, case-control, and baseline data of a cohort study. Second, sample size and point prevalence of depression were provided. Third, each paper should give a diagnose criteria for depression according to concrete depression scales. Fourth, investigation were conducted in hypertensive patients. The search language is limited in English and Chinese. We excluded studies in children and those reporting period prevalence rates.
Data Extraction and Quality Assessment
The following information was extracted for included study: first author, publication year, study design, sample selection method, sample source, diagnostic criteria, and method of measurement, sex ratio, sample, point prevalence of depression. We used the observational criteria to evaluate the study quality.13 These criteria included 11 items. One score was added when the study was conformed.
Statistical Analysis
We used Stata 11.0 (College Station, TX) and Statsdirect 2.7.9 to conduct all statistical analyses. The original point prevalence is transformed by back-transform of the weight mean (DerSimonian-Laird weights and inverse arcsine variance weights).14,15 The χ2 and the I2 statistic were used to evaluate the heterogeneity (low: I2 < 25% low, moderate: 25%–50%, high: I2 > 50%).16,17 In the present meta-analysis, the random effects model was used to pool estimation of point prevalence. Subgroup analysis was also conducted in order to know the prevalence of different category (region, sex, source of population, and types of depression assessment). Meta-regression was performed to explore effects of some potential variables on the pooled prevalence: cut-point score for diagnosis, mean age, sex, race, and region, sex, source of population and types of depression assessment. Begg Test and Egger Test were used to test the publication bias. P value of less than 0.05 was considered statistically significant. Ethical approval was not necessary as this study is a Systematic Review and Meta-Analysis.
RESULTS
Study Flow and Characteristics
Table 1 shows detailed information from the 41 studies selected. The first searches give 3890 records. In total, 3380 studies entered into the second screening stage after excluding some republication. In total, 475 studies were reviewed in full text. Finally, 41 studies were included in the meta-analysis. Figure 1 exhibits the screening process. In the surveys with samples, more than 80% of the studies are cross-sectional. In most of the studies, depression in patients with hypertension was reported using rating instruments either administered by clinicians and researchers or self-administered by participants. Diagnostic cut-point scores to define depression using self-administered questionnaires were widely heterogeneous (Table 1).
TABLE 1.
Characteristic of Studies on the Prevalence of Depression Among Patients With Hypertension
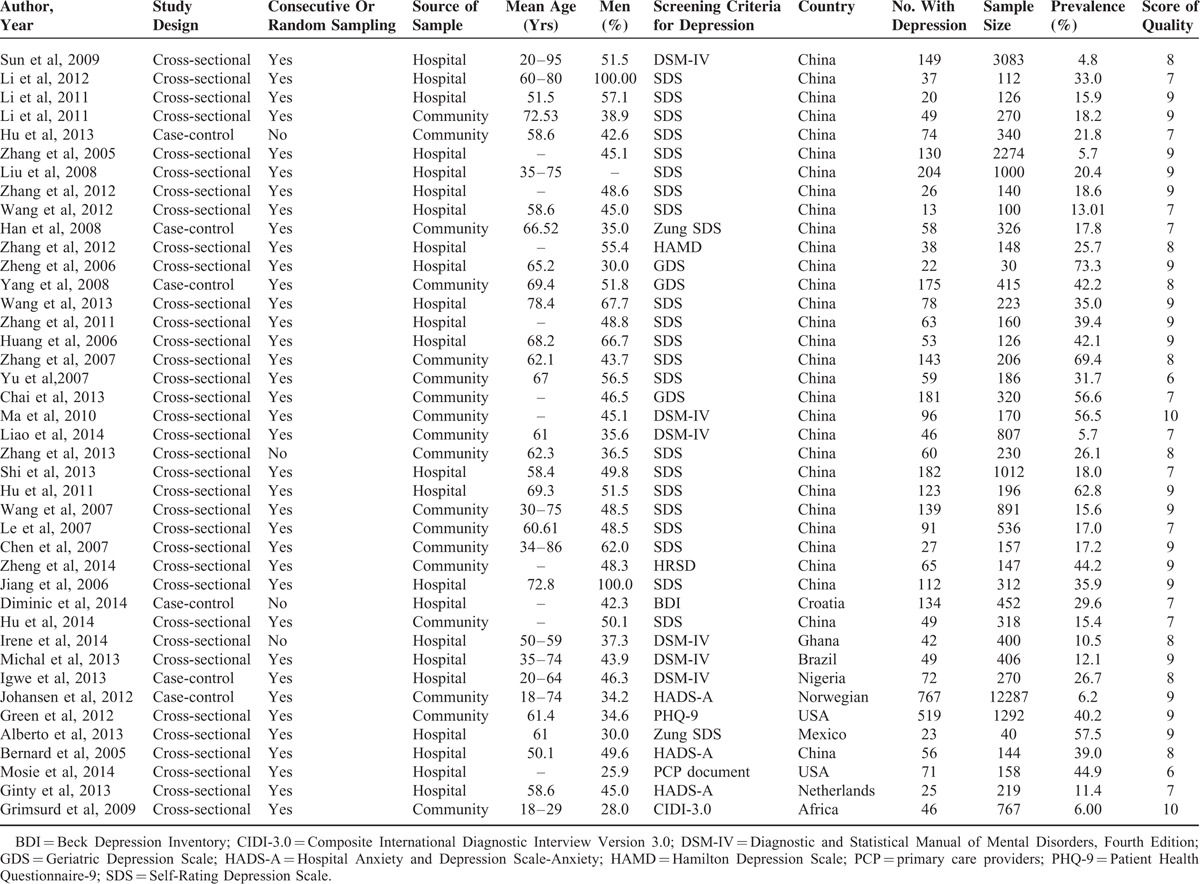
FIGURE 1.
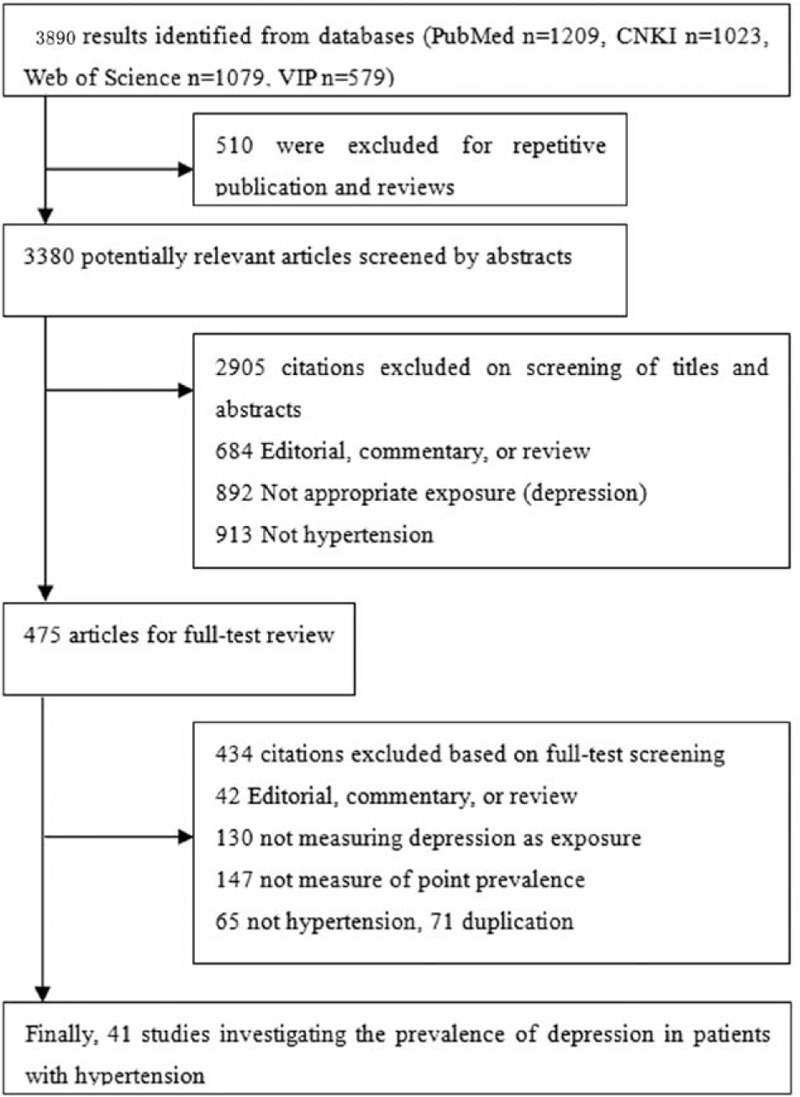
Flow diagram of included/excluded studies.
Prevalence
All results of meta-analysis are shown in Table 2.
TABLE 2.
Summary of Prevalence and Heterogeneity Findings for Depressive Symptoms in Patients With Hypertension
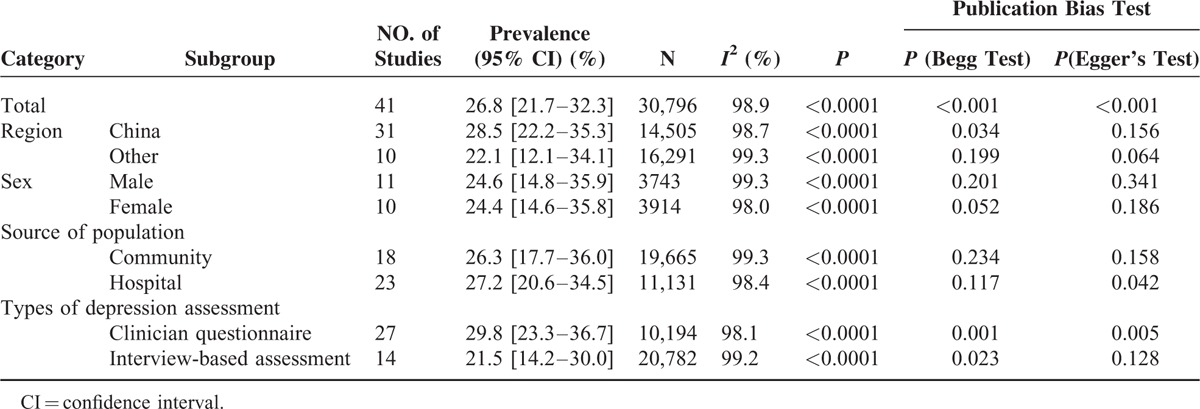
The point prevalence of depressive symptoms with 41 (see word document, Supplemental Content, which lists all studies included in the meta-analysis) individual study populations ranged between 0.5 and 73.0%, with an overall meta-analysis prevalence of 26.8% and evidence of high-level heterogeneity (I2 = 98.9%, P < 0.001).
In the region setting, the prevalence of depressive symptom in China's studies ranged between 0.5 and 73.0% in 31 populations comprising 14,505 participants. The summary prevalence of depression was 28.5% (95% CI: 22.2%–35.3%) with high-level heterogeneity (I2 = 98.7%). The estimated prevalence of depression from other regions (22.1%, 95% CI: 12.1%–34.1%) was statistically lower than was reported in China, P for subgroup difference <0.001.
In the sex setting, the pooled prevalence of depression for male (24.6%, 95% CI: 14.8%–35.9%) was almost equal to the prevalence for female (24.4%, 95% CI: 14.6%–35.8%). In the source of population setting, the pooled prevalence of depression from community was 26.3% (95% CI: 17.7%–36.0%), and was 27.2% (95% CI: 20.6%–34.5%) from hospital. The 2 subgroups have high-level heterogeneity (I2 = 99.3%, and I2 = 98.4%).
In the types of depression assessment setting, the summary meta-analytical prevalence of depressive symptoms adjudicated by self-rating scales in 27 studies (10,194 participants) was 29.8% (95% CI: 23.3%–36.7%), although tests for heterogeneity showed high-level inconsistency (I2 = 98.1%). Depression was assessed by interview in 14 studies on 20,782 hypertensive patients, and estimated prevalence was 21.3% (95% CI: 14.2%–30.0%) with high-level heterogeneity (I2 = 99.2%).
Meta-Regression Analysis, Publication Bias, and Sensitivity Analysis
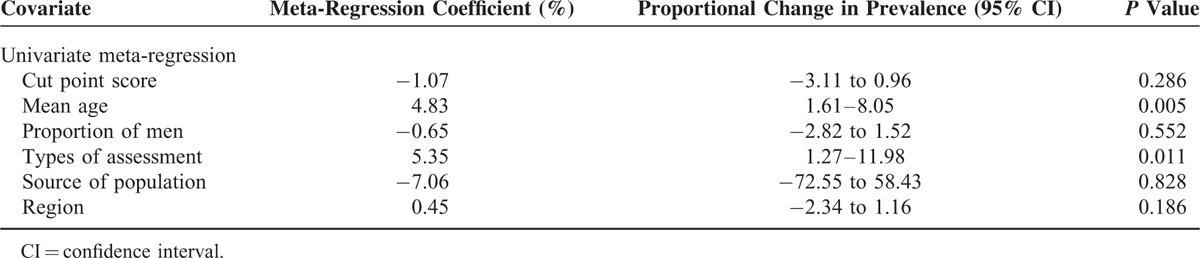
We conducted a meta-regression analysis to explore the potential heterogeneity among studies. Table 3 shows the results of meta-regression analysis. Cut-off value of depression, sex (male), source of study population, and different region had no influence on the pooled prevalence. However, mean age (P = 0.005) and methods of depression evaluation (P = 0.011) were positively associated with the pooled prevalence. The 1% growth of mean age went with 4.83% of depression in hypertensive. The methods of depression evaluation (clinician questionnaire) also affected the estimated prevalence. The funnel plot found an apparent publication bias. Both P for Begg and Egger test was less than 0.001. The sensitivity analysis was conducted by excluding 6 case-control studies, and the results kept stable.
TABLE 3.
Meta-Regression Analysis for the Prevalence of Depressive Symptoms in Patients With Hypertension
DISCUSSION
Thus far, there is a lack of pooled estimation regarding the prevalence of depression in hypertensive patients. This is the first systematical evaluation of published studies on the prevalence of depression in hypertensive patients. The present meta-analysis found that prevalence of depression is common in patients with hypertension and estimated prevalence was significantly associated with the diagnosis methods used to screen depression. The clinical interview showed approximately one-third (21.3%) of hypertensive patients have depressive symptoms, which was lower than screening scales-based tools (29.8%).
Our estimated prevalence of depression by clinical interview in hypertensive patients is 21.3%. This result is close to the prevalence of depression from patients with chronic kidney disease (20.3%),18 and also falls into the range of other clinical settings, such as heart failure (19.3%),19 primary care (17.3%),20 and cancer (16.3% 95% CI).21 But, obviously, this is higher than observed in settings of type 1 and type 2 diabetes (13.6% and 10.9%, respectively)22 and slightly lower than investigated in obstructive respiratory disease (27.6%). Above of all are apparently higher than result of a recent study supported by WHO revealed that around 5% of people in the community had depression during the last year,23 suggested that chronic disease is a crucial and common underlying determinant for depression, regardless of the biological mechanism.
The screening tools for evaluating depression mainly include 2 types: self-assessment and clinician-completed. Our study with 41 studies suggested that self-assessed screening tools of depression or depressive symptoms might overestimate the prevalence of depression in hypertensive patients to some extent, which is indicated by much higher point estimation of depression prevalence derived using self-administered diagnostic scales (30%) compared with pooled prevalence used by clinical-interviewed tools (21%). The reason could be that self-assessed report methods have some limitations. Specifically, the hypertensive patients may be confused about depression and hypertension symptoms such as poor appetite, sleep disorders, and fatigue symptoms. They probably considered these symptoms commonly suffered from hypertension as indication of depression or depressive symptoms and classified themselves as patients with depression. The method of clinical interview identified depression or depressive symptoms through clinical diagnostic criteria and can give a more precise estimation of depression prevalence.
Depression in hypertensive patients is associated with poorer health status, including lower quality of life,24–26 increased medical sources,27 lower rate of treatment compliance,28 and even increased mortality.29 People with depression could suffer from the lack of occupational and social role function.30 It is easier for hypertensive patients with depression to further develop depressive symptoms. Although depression combined with hypertension could have additional adverse impact on physical function and quality of life of patients, there are still no sufficient data to prove that screening of depression in hypertensive patients can have positive effects in the improvement of clinical symptoms and physical health. As far as we know, systematic evaluation of depression in hypertensive patients has not been done, implementation of available screening methods for depression has not been done, and existing randomized trials of interventions still have some limitations such as smaller sample size, shorter duration, and lack of reliance on related clinical outcomes.31–33 Besides, it is probably inappropriate to carry out effective interventions for depression from other chronic diseases into the hypertensive patients. The eluting period of different drug and the cardiovascular events frequency could have some impact on effectiveness and risk of the treatment in hypertensive patients.
Limitations
Although this meta-analysis includes more studies and a larger number of sample sizes than individual studies, some limitations needed to be illustrated clearly. The main limitations were the limited amount of information, as well as the marked and largely unexplained heterogeneity in estimation between contributing studies. First, most of the studies included in the meta-analysis were from China. This prevalence of depression among hypertension may be more typical in Chinese population. Second, the prespecified subgroup analysis suggested significant differences in the prevalence estimation based on region in individual studies; they should be interpreted with caution. Third, the studies included in the meta-analysis had some methodological differences. These limitations may make patients in single study different from those excluded patients in some significant ways. Finally, we also did not estimate the prevalence of other common psychological symptoms.
CONCLUSIONS
The observed heterogeneity in depression prevalence of hypertension may be attributed to differences in method of evaluation. Self-report scales should be cautious of estimating the presence of depression. Thus, interview-defined depression affects approximately one third of hypertensive patients. Effective interventions for depression on patient-centered are needed.
Acknowledgment
We thank all our colleagues working in the Department of Epidemiology and Health Statistics, School of Public Health of Central South University.
Footnotes
Abbreviations: BDI = Beck Depression Inventory, CI = confidence interval, CIDI-3.0 = Composite International Diagnostic Interview Version 3.0, CNKI = China National Knowledge Internet, DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, GDS = Geriatric Depression Scale, HADS-A = Hospital Anxiety and Depression Scale-Anxiety, HAMD = Hamilton Depression Scale, PCP = primary care providers, PHQ-9 = Patient Health Questionnaire-9, SDS = Self-Rating Depression Scale.
This work was supported by Hunan Province Science and Technology Project (2014SK2013), fundamental research funds for the central universities of Central South University (2014zzts069), and Graduate Innovation Project of Hunan Province (CX2014B097).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.World Health Organization, Sixty-fifth world health assembly 2012. http://www.who.int/mediacentre/events/2012/wha65/journal/en/index4.html Accessed December 11, 2014. [Google Scholar]
- 2.Waraich P, Goldner EM, Somers JM, et al. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry 2004; 49:124–138. [DOI] [PubMed] [Google Scholar]
- 3.Faraco G, Iadecola C. Hypertension: a harbinger of stroke and dementia. Hypertension 2013; 62:810–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van den Hoogen PC, Feskens EJ, Nagelkerke NJ, et al. The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven Countries Study Research Group. N Engl J Med 2000; 342:1–8. [DOI] [PubMed] [Google Scholar]
- 5.Mahmoodi BK, Matsushita K, Woodward M, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: a meta-analysis. Lancet 2012; 380:1649–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schillaci G, Pucci G, Perlini S. From hypertension to hypertrophy to heart failure: the role of cardiotrophin-1. J Hypertens 2013; 31:474–476. [DOI] [PubMed] [Google Scholar]
- 7.Mittal BV, Singh AK. Hypertension in the developing world: challenges and opportunities. Am J Kidney Dis 2010; 55:590–598. [DOI] [PubMed] [Google Scholar]
- 8.Almas A, Patel J, Ghori U, et al. Depression is linked to uncontrolled hypertension: a case-control study from Karachi, Pakistan. J Ment Health 2014; 23:292–296. [DOI] [PubMed] [Google Scholar]
- 9.Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety depression and stress on anti-hypertensive medication adherence. Int J Ment Health Syst 2014; 8:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Junius-Walker U, Voigt I, Wrede J, et al. Health and treatment priorities in patients with multimorbidity: report on a workshop from the European General Practice Network meeting ’Research on multimorbidity in general practice’. Eur J Gen Pract 2010; 16:51–54. [DOI] [PubMed] [Google Scholar]
- 11.Ried LD, Tueth MJ, Handberg E, et al. Validating a self-report measure of global subjective well-being to predict adverse clinical outcomes. Qual Life Res 2006; 15:675–686. [DOI] [PubMed] [Google Scholar]
- 12.Hedayati SS, Bosworth HB, Kuchibhatla M, et al. The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int 2006; 69:1662–1668. [DOI] [PubMed] [Google Scholar]
- 13.Rostom A, Dubé C, Cranney A, Saloojee N, Richmond Sy. (2004) Celiac Disease. Rockville (MD): Agency for Healthcare Research and Quality (US); (Evidence Reports/Technology Assessments, No. 104.) Appendix D. Quality Assessment Forms. http://www.ncbi.nlm.nih.Gov/books/NBK35156/ Accessed August 31, 2014. [Google Scholar]
- 14.Stuart A, Ord JK. Kendall's Advanced Theory of Statistics. 6th ed.London, UK: Edward Arnold; 1996. [Google Scholar]
- 15.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177–188. [DOI] [PubMed] [Google Scholar]
- 16.Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 17.Higgins J, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmer S, Vecchio M, Craig JC, et al. Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int 2013; 84:179–191. [DOI] [PubMed] [Google Scholar]
- 19.Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006; 48:1527–1537. [DOI] [PubMed] [Google Scholar]
- 20.O’Connor EA, Whitlock EP, Beil TL, et al. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med 2009; 151:793–803. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011; 12:160–174. [DOI] [PubMed] [Google Scholar]
- 22.Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2011; 24:1069–1078. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization, WHO marks 20th Anniversary of World Mental Health Day. http://www.who.int/mediacentre/news/notes/2012/mental_health_day_20121009/en/ Accessed December 11, 2014. [Google Scholar]
- 24.Rueda B, Perez-Garcia AM. Coping strategies, depressive symptoms and quality of life in hypertensive patients: mediational and prospective relations. Psychol Health 2013; 28:1152–1170. [DOI] [PubMed] [Google Scholar]
- 25.Saboya PM, Zimmermann PR, Bodanese LC. Association between anxiety or depressive symptoms and arterial hypertension, and their impact on the quality of life. Int J Psychiatry Med 2010; 40:307–320. [DOI] [PubMed] [Google Scholar]
- 26.Batal O, Khatib OF, Bair N, et al. Sleep quality, depression, and quality of life in patients with pulmonary hypertension. Lung 2011; 189:141–149. [DOI] [PubMed] [Google Scholar]
- 27.Maguire LK, Hughes CM, McElnay JC. Exploring the impact of depressive symptoms and medication beliefs on medication adherence in hypertension: a primary care study. Patient Educ Couns 2008; 73:371–376. [DOI] [PubMed] [Google Scholar]
- 28.Moise N, Davidson KW, Chaplin W, et al. Depression and clinical inertia in patients with uncontrolled hypertension. JAMA Intern Med 2014; 174:818–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oganov RG, Pogosova GV, Koltunov IE, et al. Depressive symptoms worsen cardiovascular prognosis and shorten length of life in patients with arterial hypertension and ischemic heart disease. Kardiologiia 2011; 51:59–66. [PubMed] [Google Scholar]
- 30.Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA 1989; 262:914–919. [PubMed] [Google Scholar]
- 31.Wang L, Li J. Role of educational intervention in the management of comorbid depression and hypertension. Blood Press 2003; 12:198–202. [DOI] [PubMed] [Google Scholar]
- 32.Coventry P. Multicondition collaborative care intervention for people with coronary heart disease and/or diabetes, depression and poor control of hypertension, blood sugar or hypercholesterolemia improves disability and quality of life compared with usual care. Evid Based Med 2012; 17:e13. [DOI] [PubMed] [Google Scholar]
- 33.Bogner HR, de Vries HF, Kaye EM, et al. Pilot trial of a licensed practical nurse intervention for hypertension and depression. Fam Med 2013; 45:323–329. [PMC free article] [PubMed] [Google Scholar]


