Abstract
Bad Sobernheim Stress Questionnaire (BSSQ)-Deformity and BSSQ-Brace are the most widely used instruments for evaluating stress levels in adolescent idiopathic scoliosis (AIS) patients under brace treatment, and good reliability and validity have been demonstrated across different cultures. Great stress has been found among many adolescents, becoming a major concern for professionals. However, no previous research has addressed the cultural adaptations and psychometric testing of BSSQ-Deformity and BSSQ-Brace in China or the stress levels in AIS patients. The purposes of our study were to evaluate the cross-cultural adaptation and validation of the BSSQ-Deformity and BSSQ-Brace and to investigate stress levels in Chinese (AIS) patients under brace treatment.
The original (German) versions of BSSQ-Deformity and BSSQ-Brace were cross-culturally translated according to international guidelines. Psychometric properties such as reliability and construct validity were tested. Eighty-six AIS patients were included in our study, and 50 patients paid a second visit 3 to 7 days later to test reproducibility. Cronbach α and the intraclass coefficient were determined to assess internal consistency and reproducibility. Scoliosis Research Society patient questionnaire-22 (SRS-22) was applied to evaluate construct validity.
The mean BSSQ-Deformity and BSSQ-Brace scores were 15.3 and 13.4 points, respectively. Severe stress was observed in 12% of patients due to brace treatment. Item analysis demonstrated that each item was scored under a normal distribution with no redundancy. Psychometric analysis revealed excellent internal consistency (Cronbach α = 0.85 and 0.80, respectively) and reproducibility (intraclass correlation coefficient = 0.85 and 0.90, respectively) for BSSQ-Deformity and BSSQ-Brace. The correlation coefficients of BSSQ-Deformity, BSSQ-Brace and SRS-22 were 0.48 and 0.63, respectively.
In conclusion, BSSQ-Deformity and BSSQ-Brace have been successfully adapted to a Chinese background and psychometrically validated with excellent reliability and construct validity. Brace wearing is considered the main cause of stress in AIS patients under brace treatment.
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is one of the most prevalent diseases among teenagers, affecting their physical, mental, and social adaptation status.1 According to results from school screening, the incidence rate of AIS in teenagers is estimated from 0.87% to 2.5%, and 0.02% of patients require surgical treatment, in which case the Cobb angle is >45°, whereas 0.28% of patients require the use of a brace.2 Bracing is one of the most commonly adopted conservative therapies for the prevention of curve progression, often lasting for months or years and requiring the active participation of patients and their families.3 Therefore, increasing the quality of life of adolescents suffering from AIS has become increasingly important for health care professionals.4–6 Stress is a common factor deteriorating quality of life, such as the relationship between patients and their surrounding environment.7 In addition to the visible deformation of the body from scoliosis itself, the treatment may also make the patient uncomfortable and induce stress reactions.8–10 Wearing a corrective brace at school or outside the home is a major cause of mental discomfort. Freidel et al11 showed that female juvenile patients were less satisfied with their life, with less physical comfort, lower self-esteem, and higher depression levels compared with healthy controls. Psychological stress is becoming a major concern for professionals due to its correlation with reduced treatment compliance.11,12 Therefore, assessing stress levels has become a necessity in AIS patients undergoing brace treatment.
Weiss et al13 designed 2 questionnaires to assess the stress level induced by deformity (Bad Sobernheim Stress Questionnaire Deformity, BSSQ-Deformity) and brace treatment (Bad Sobernheim Stress Questionnaire Brace, BSSQ-Brace).10 BSSQ-Deformity and BSSQ-Brace have been proven reliable and valid to assess the stress levels in AIS patients with the original German version. It was discovered that almost 1 out of 3 of AIS patients undergoing bracing treatment were suffering from severe stress, and half of the patients were suffering from moderate stress, with the remaining 1 out of 6 showing no or only mild stress problems.10 BSSQ-Deformity and BSSQ-Brace were originally proposed in Germany, and they have thus far been cross-culturally adapted into Polish,14 Italian,15 Spanish,16 and Turkish17 versions, showing excellent reliability and construct validity. However, there are enormous cultural differences between China and Germany. It has been proven that cognitive processing is different in the developmental trajectories between Eastern and Western countries.18 Therefore, the cross-cultural adaptation of BSSQ-Deformity and BSSQ-Brace is indispensable if BSSQ is to be applied in China. The aim of this research was to validate the Chinese versions of the BSSQs, and then to evaluate stress levels in AIS patients under brace treatment.
METHODS
The BSSQs were cross-culturally translated into simplified Chinese according to internationally recognized guidelines.19 Then, psychometric properties such as reliability and validity were analyzed statistically.
Translation and Cross-Cultural Adaptation
The German versions of BSSQ-Deformity and BSSQ-Brace were translated into simplified Chinese using a translation and back-translation procedure.19 This process is feasible considering much experience in validation testing of other quality of life measurement tools.20,21 The committee was composed of AIS experts who are proficient in German, German teachers without AIS knowledge, 1 rehabilitation specialist, and 1 statistician. Then, a pilot test of the prefinal versions of BSSQ-Deformity and BSSQ-Brace was carried out in 20 patients with AIS. Linguistic ambiguity was reported by each participant and subsequently resolved by the committee. Eventually, the Chinese version BSSQ-Deformity and BSSQ-Brace were reached.
Participants
AIS patients who had undergone brace treatment using the same type of brace (Shanghai Delin Artificial Limb Recovering Equipment, China) were recruited from Changhai Hospital, China. Patients included in our study met the following criteria: wearing a brace >12 h/d for 3 months, Risser sign I-IV, Cobb angle 20° to 45°, age between 10 and 16 years, fully capable of reading and writing, and receiving no other treatment. Patients with congenital scoliosis, neuromuscular scoliosis, and other types of scoliosis who were unwilling to undertake the brace treatment, and patients with severe mental trauma, were excluded from this study. All participants completed the Scoliosis Research Society patient questionnaire-22 (SRS-22), BSSQ-Deformity, and BSSQ-Brace independently. Demographic data were collected. Medical history and radiological images were collected to confirm the diagnosis. To explore the adaptation of BSSQ-Deformity and BSSQ-Brace, test-retest reliability assessment was conducted. Fifty patients were randomly selected to complete the questionnaire again 3 to 7 days later. Written informed consent was obtained from their parents. This study was approved by the Ethics Committee in Changhai Hospital.
Instruments
BSSQ-Deformity and BSSQ-Brace
Both BSSQ-Deformity13 and BSSQ-Brace10 contain 8 items with a 5-point scale ranging from “0” (worst) to “4” (best). BSSQ-Deformity is designed to assess how the deformity affects the patient's mood, acceptance, and interactions with society. BSSQ-Brace is designed as an assessment of the brace treatment's effects on mood, social interactions, and subsequent stress levels. The stress criteria are defined as follows: 0 to 8 points indicate a high level of stress; 9 to 16 points indicate a moderate level of stress; and 17 to 24 points indicate a low level of stress.10
SRS-22
SRS-22, developed by Haher et al22, is a practical and disease-specific questionnaire to assess patients with idiopathic scoliosis. Asher et al23 further refined the SRS-24 into a 22-item version with excellent reliability and validity in assessing quality of life in idiopathic scoliosis. SRS-22 includes 5 dimensions: function activity level, pain, mental health, self-image, and management satisfaction. All items are scored with a 5-point scale ranging from “1” to “5.” The total quality of life score ranges from 22 to 110 points, the higher the score, the better the quality of life. SRS-22 has been shown to display good score distribution, internal consistency, reproducibility, and concurrent validity.24,25 It has been successfully adapted into Chinese with acceptable reliability and validity.26
Statistical Analysis
First, a standardized value of skewness (Z-skewness) was determined for each item to evaluate the item's response trend. Any item with a skewness value of <1.96 was considered to have a response trend of normal distribution.27 An item-total correlation coefficient was determined by Pearson correlation analysis. Items with an item-total correlation coefficient <0.20 were eliminated.28
Second, for reliability analysis, internal consistency was determined as Cronbach α, which was considered acceptable if the value was >0.70.29 To assess the temporal stability of BSSQ-Deformity and BSSQ-Brace, the intraclass correlation coefficient (ICC) was tested over a 3- to 7-day period. ICC values were interpreted as good (>0.60) or excellent (>0.80) reproducibility.30
Lastly, construct validity was analyzed by Pearson correlation coefficients for BSSQ and SRS-22. The results were interpreted as little or no relationship (r = |0–0.25|), fair (r = |0.25–0.50|), moderate to good (r = |0.50–0.75|), or excellent (r = |0.75–1.00|).31
It has been advised that a sample size of at least 50 is appropriate for analyses of reliability and construct validity.30 Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 18.0 (SPSS, Chicago, IL). Mean values were reported with standard deviation (SD), and ICC values were presented with 95% confidence intervals (CIs). A P value of <0.05 was considered statistically significant for all analyses.
RESULTS
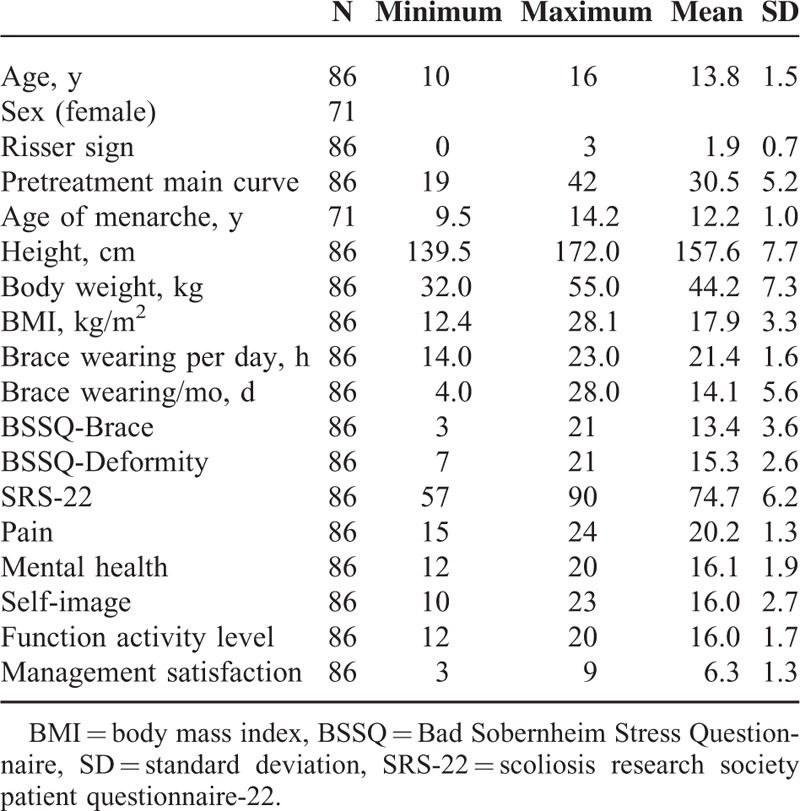
A total of 86 AIS patients were included in our study, 14 of whom were males and 72 were females. The average age was 13.8 years and the mean Cobb angle was 30.5°. All the participants filled out the questionnaires properly. The mean BSSQ-Deformity and BSSQ-Brace values were 15.3 and 13.4 points, respectively. The bracing time was 21.4 h/d, 14 d/mo. Demographic details are shown in Table 1. All the participants filled out the questionnaires with no comprehension problems. The mean time undertaken to complete the questionnaire was approximately 2 minutes.
TABLE 1.
Baseline Socio-Demographic and Clinical Characteristics
Stress levels were higher for patients with a brace than those with deformity (13.4 vs 15.3, P < 0.05). In addition, more patients reported stronger stress levels with brace treatment compared with those with deformity (12% vs 2%, P < 0.01). More patients reported lower stress levels due to deformity compared with braces (30% vs 15%, P < 0.01) (Figure 1).
FIGURE 1.
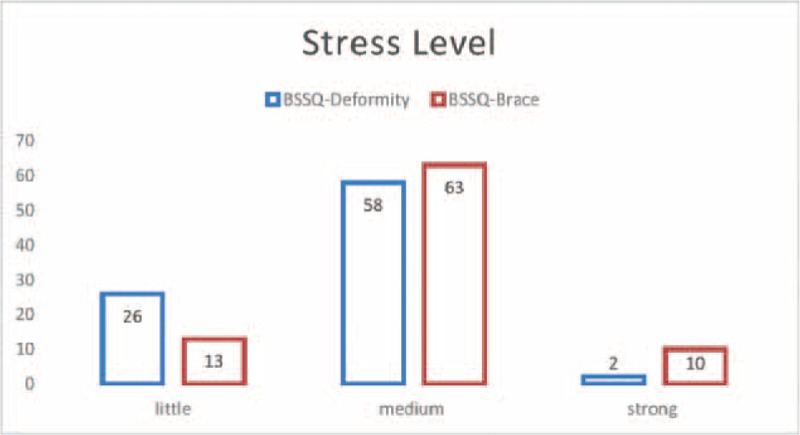
Stress levels related to deformity and brace wearing in AIS patients under brace treatment. AIS = adolescent idiopathic scoliosis.
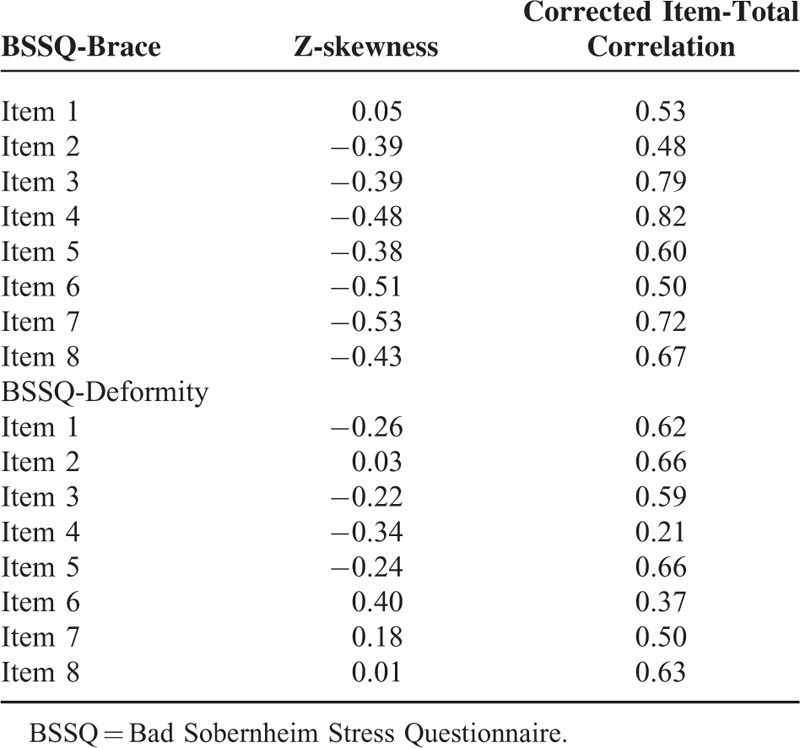
Response trend analysis revealed that all item scores were normally distributed, indicating that every item functioned properly. Item analysis proved the internal homogeneity of the construct because no item had an item-total correlation <0.20 in either construct (see Table 2).
TABLE 2.
Corrected Item-Total Correlation and Response Trend for Each Item on BSSQ
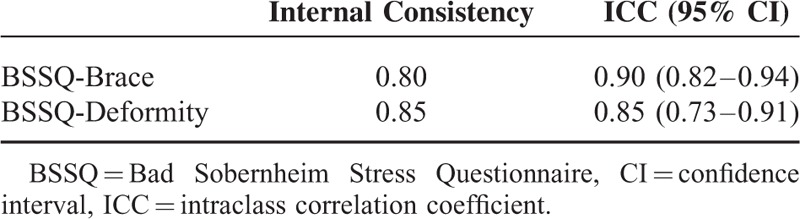
BSSQ-Deformity and BSSQ-Brace demonstrated excellent reliability. The Cronbach α values for BSSQ-Deformity and BSSQ-Brace were 0.85 and 0.80, respectively, indicating excellent internal consistency as both values were >0.70. In addition, BSSQ-Deformity and BSSQ-Brace exhibited extraordinary test-retest reliability with mean ICC values of 0.85 (0.73–0.91) and 0.90 (0.82–0.94, Table 3), respectively.
TABLE 3.
Internal Consistency and Test-Retest Reliability of BSSQ
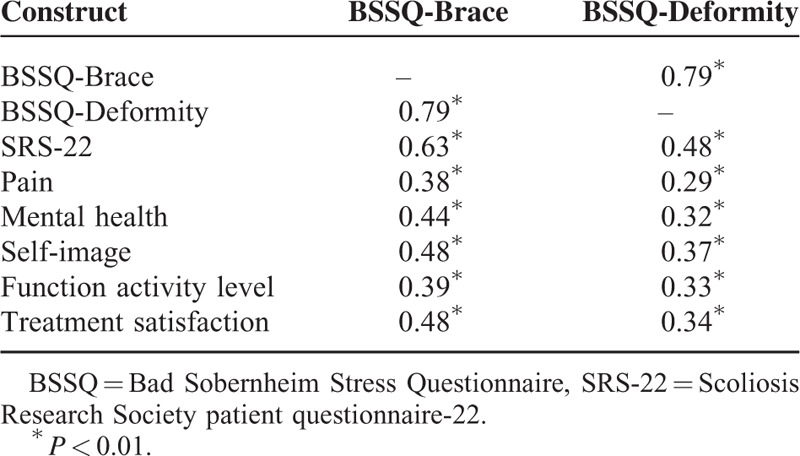
It was demonstrated that BSSQ-Deformity had a strong correlation with BSSQ-Brace. BSSQ-Brace had a higher correlation with SRS-22 compared with BSSQ-Deformity (0.63 vs 0.48, Table 4). Both BSSQ-Deformity and BSSQ-Brace had a marginally strong correlation with the self-image and treatment satisfaction domains, although the relationship with all 5 domains was deemed as fair.
TABLE 4.
Pearson Correlation Coefficient of BSSQ With Other Measures of Scoliosis
DISCUSSION
AIS is one of the most prevalent diseases affecting teenagers.32 A number of massive school screening studies have reported that the prevalence rate is approximately 2% to 3%.33,34 AIS is regarded as a chronic disease due to the extended period of treatment. Accumulated evidence has proven the effectiveness of bracing in halting the progress of scoliosis,4 especially the randomized controlled clinical trial by Weinstein et al.35 Although bracing is considered to be an effective and noninvasive therapy, it was reported that bracing may deteriorate quality of life and mental health in adolescent patients, restricting function and daily activities and damaging self-image.8–11 Other studies have revealed that stress caused by bracing is the most important issue in conservative treatment.8,9 Because bracing requires an extended period of treatment, it is of vital importance to increase the compliance of patients and decrease its side effects on quality of life.12 Therefore, creating effective ways to assess the quality of life is the first step in tackling this widespread problem. Currently, SRS-22, the short form (36) health survey, and spine appearance questionnaire are the available instruments.22,36,37 However, these measures take a long time to complete, and stress is seldom mentioned. BSSQ-Deformity and BSSQ-Brace were developed by German investigators to focus on the stress level induced by scoliosis and bracing.10,13 They have been cross-culturally adapted into Polish,14 Italian,15 Spanish,16 and Turkish17 versions, showing excellent reliability and construct validity. The present study demonstrated that BSSQ-Deformity and BSSQ-Brace are reliable and valid for assessing stress level in patients with AIS in Mainland China.
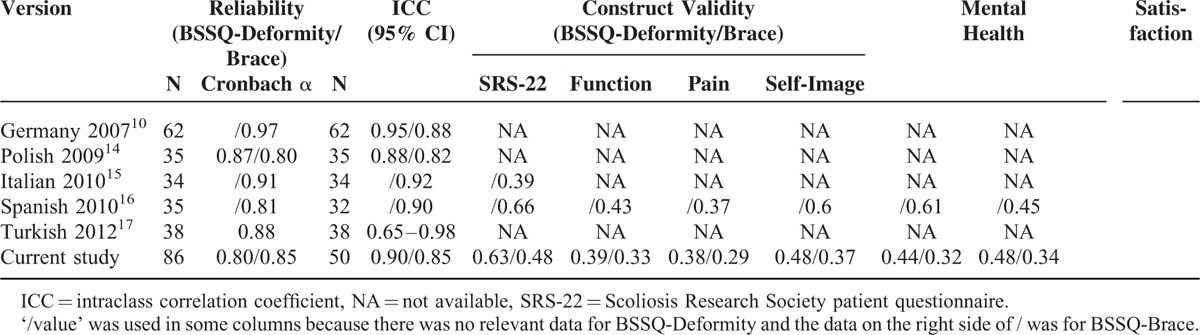
The translation process was not troublesome due to aggregated experience in the validation of other quality of life measures by our group. Eighty-six patients were recruited in the present study, constituting the largest study population among validation studies (see Table 5). It has been noted that a minimum of 50 patients is required for effective statistical analysis.19 However, only the German study10 and our study met this criterion, partly because few patients are referred for bracing treatment and because scoliosis is only discovered by parents when it has already progressed. All participants answered the Chinese version within 2 minutes without any difficulties, indicating its excellent clinical utility and great suitability for administration.
TABLE 5.
Comparison on Reliability and Construct Validity Between Different Cultural Versions of BSSQ
Item analysis revealed that no item was redundant in that all the items had an item-total score correlation >0.20. The scores of each item were distributed in a normal distribution, indicating that each item measured the range of possible states of the relevant question. Statistically speaking, skewness analysis has a similar meaning with floor or ceiling effect analysis. In the original German version, floor or ceiling results were >15%, which indicated that the items could not measure the extent of the problem properly.10 However, in subsequent Polish, Spanish, and Italian studies and our Chinese study, ceiling and floor effects were <5%,14–16 probably because the original German study had diverse participants and severe scoliosis, whereas the others recruited only AIS patients with a medium degree of scoliosis.
Both BSSQ-Deformity and BSSQ-Brace exhibited acceptable reliability. In fact, all versions of BSSQ-Deformity and BSSQ-Brace had a Cronbach α coefficient of >0.70, except for the original German version of BSSQ-Deformity.13 The reason may be that there was great variance in the study population, whereas the other study had a small population and homogeneous patients. Therefore, BSSQ-Deformity and BSSQ-Brace were found to be internally homogeneous constructs for measuring stress levels in AIS patients. In addition, the scores remained stable in test-retest analysis (ICC = 0.82–0.98), indicating their clinical utility in follow-up evaluations of treatment.14–17
To test the construct validity of BSSQ-Deformity and BSSQ-Brace, SRS-22 is the most commonly applied instrument due to its international acceptance. Similarly, the Italian and Spanish studies used SRS-22 to explore construct validity.15,16 For BSSQ-Brace, the gross correlation coefficient with SRS-22 ranged from 0.39 to 0.66. In this study, the coefficient was 0.48, indicating a good relationship between BSSQ-Brace and SRS-22. All 5 domains of SRS-22 had similar degrees of correlation with BSSQ-Brace, but a marginally higher coefficient was found for self-image. In the Spanish study, the self-image and mental health domains had higher correlation with BSSQ-Brace than the others (0.60, 0.61 vs 0.43, 0.37, and 0.45), indicating that BSSQ-Brace is specifically targeted at the assessment of mental health and stress-related self-esteem. In accordance with other research, BSSQ-Deformity and BSSQ-Brace could also measure function and pain to some extent. To our knowledge, the current study is the first research to report the construct validity of BSSQ-Deformity.13,14 In our research, BSSQ-Deformity had a higher correlation with SRS-22 than did BSSQ-Brace (0.63 vs 0.48), and BSSQ-Deformity had a higher correlation with the self-image and satisfaction domain in SRS-22, although the difference was not significant. These results showed that BSSQ-Deformity and BSSQ-Brace were designed specifically to measure stress-related self-image and other mental problems caused by scoliosis and subsequent brace treatment.
Most of the participants reported a moderate stress level during brace treatment. The mean scores of BSSQ-Deformity and BSSQ-Brace were 15.3 and 13.4, respectively. To evaluate scoliosis-related stress levels, BSSQ-Deformity was applied, and the results showed that 2% of the participants reported a severe stress level. To assess brace-induced stress levels, BSSQ-Brace was used, and the results showed that 12% of participants reported severe stress levels, which was almost 6 times the amount of scoliosis-related stress. Therefore, bracing can aggravate stress levels in AIS patients. Other studies have reported similar results. In the original German version, the mean BSSQ-Brace value was 12.5, and 27% reported a severe stress level.10 The Italian and Spanish studies reported mean values of 12.6 and 11.7 for AIS patients under brace treatment.15,16 In 3 Polish studies, the mean BSSQ-Deformity values were 18, 18.3, and 17.9, and the mean BSSQ-Brace values were 9, 12.3, and 11.3.9,14,38 One study reported that 22.9% of patients had a severe stress level due to brace treatment.14 It should be noted these studies included only female patients. Considering the above results, it is fair to conclude that bracing can be considered a significant cause of stress independent of scoliosis itself. For those who are wearing a brace, approximately 10% to 30% suffer from a severe level of stress, which should be an important finding.
With the progress of personal health care, health-related quality of life has become a major concern for health care providers. Chinese orthopedic surgeons are paying more attention to patient compliance with treatment, especially in the environment of intense doctor-patient relationships.39 In addition, parents in China pay more attention to their children because he or she is more likely to be the only child in the family. Therefore, it is necessary to introduce instruments to evaluate the quality of life in adolescent patients and take measures to increase their compliance and satisfaction with their treatment. Thus, BSSQ-Deformity and BSSQ-Brace are desperately needed by orthopedic doctors in Mainland China.
Although the findings from this study provide strong support for the validity and reliability of the Chinese versions of BSSQ-Deformity and BSSQ-Brace, it should be acknowledged that several salient limitations apply. First, the study population may not ideally represent the entire population of AIS patients in Mainland China even though they were from different regions of China. There are diverse ethnic groups, dialects, and local cultures in China such as in Tibet and Xinjiang province. Second, only AIS patients were included in this study. Whether BSSQ-Deformity and BSSQ-Brace could be applied in patients with other types of scoliosis requires further exploration. Third, the participants included had medium scoliosis with a mean Cobb angle of approximately 30°. The item scale may be adopted if it is used to assess the stress level in severe scoliosis patients. Some studies noted that the stress level is correlated with Cobb angle.
In conclusion, BSSQ-Deformity and BSSQ-Brace have been successfully adapted and psychometrically validated in Chinese versions with good clinical utility, reliability, and construct validity for AIS patients. Bracing is considered the main cause of stress in AIS patients under brace treatment. At least 10% of patients suffer from severe stress problems due to wearing a brace. This work may help to promote the application of BSSQ and the evaluation of stress levels of patients in Mainland China.
Footnotes
Abbreviations: AIS = adolescent idiopathic scoliosis, BSSQ = bad sobernheim stress questionnaire, ICC = intraclass correlation coefficient, SRS-22 = scoliosis research society patient questionnaire-22.
Neither the authors, their immediate families, nor any research foundation with which they are affiliated received any financial payments or other benefits from any commercial entity related to the subject of this article.
XX, FW, MY, and QH contributed to this manuscript equally.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Danielsson AJ, Wiklund I, Pehrsson K, et al. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J 2001; 10:278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luk KD, Lee CF, Cheung KM, et al. Clinical effectiveness of school screening for adolescent idiopathic scoliosis: a large population-based retrospective cohort study. Spine (Phila Pa 1976) 2010; 35:1607–1614. [DOI] [PubMed] [Google Scholar]
- 3.Zaina F, De Mauroy JC, Grivas T, et al. Bracing for scoliosis in 2014: state of the art. Eur J Phys Rehabil Med 2014; 50:93–110. [PubMed] [Google Scholar]
- 4.Maruyama T, Grivas TB, Kaspiris A. Effectiveness and outcomes of brace treatment: a systematic review. Physiother Theory Pract 2011; 27:26–42. [DOI] [PubMed] [Google Scholar]
- 5.Schlösser TP, Stadhouder A, Schimmel JJ, et al. Reliability and validity of the adapted Dutch version of the revised Scoliosis Research Society 22-item questionnaire. Spine J 2014; 14:1663–1672. [DOI] [PubMed] [Google Scholar]
- 6.Leszczewska J, Czaprowski D, Pawłowska P, et al. Evaluation of the stress level of children with idiopathic scoliosis in relation to the method of treatment and parameters of the deformity. Sci World J 2012; 2012:538409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breznitz S, Goldberger L. Stress research at a crossroads. Handbook of stress: Theoretical and Clinical Aspects 2nd ed.New York: Free Press; 1993.. 3–6. [Google Scholar]
- 8.MacLean WE, Jr, Green NE, Pierre CB, et al. Stress and coping with scoliosis: psychological effects on adolescents and their families. J Pediatr Orthop 1989; 9:257–261. [PubMed] [Google Scholar]
- 9.Kotwicki T, Kinel E, Stryła W, et al. Estimation of the stress related to conservative scoliosis therapy: an analysis based on BSSQ questionnaires. Scoliosis 2007; 2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss HR, Werkmann M, Stephan C. Brace related stress in scoliosis patients—comparison of different concepts of bracing. Scoliosis 2007; 2:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freidel K, Petermann F, Reichel D, et al. Quality of life in women with idiopathic scoliosis. Spine (Phila Pa 1976) 2002; 27:E87–91. [DOI] [PubMed] [Google Scholar]
- 12.Rivett L, Rothberg A, Stewart A, et al. The relationship between quality of life and compliance to a brace protocol in adolescents with idiopathic scoliosis: a comparative study. BMC Musculoskelet Disord 2009; 10:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Botens-Helmus C, Weiss HR, Reichel D, et al. Reproducibility and criterion validity of the BSSQ stress questionnaire for patients with scoliosis. Proceedings of the 3rd International Conference on Conservative Management of Spinal Deformities & Scientific meeting of the SOSORT, April 7–8, Poznan, 2006. [Google Scholar]
- 14.Misterska E, Głowacki M, Harasymczuk J. Polish adaptation of Bad Sobernheim Stress Questionnaire-Brace and Bad Sobernheim Stress Questionnaire-Deformity. Eur Spine J 2009; 18:1911–1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlösser TP, Stadhouder A, Schimmel JJ, et al. Determination of quality of life in adolescents with idiopathic scoliosis subjected to conservative treatment. Scoliosis 2010; 5:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D’Agata E, Testor CP, Rigo M. Spanish validation of Bad Sobernheim Stress Questionnaire (BSSQ (brace).es) for adolescents with braces. Scoliosis 2010; 5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yilmaz HG, Kuru T, Yavuzer G. Turkish adaptation and reliability of Bad Sobemheim Stress Questionnaire in adolescents with idiopathic scoliosis using spinal brace. Turk Fiz Tip Rehab Derg 2012; 58:225–228. [Google Scholar]
- 18.Kuwabara M, Smith LB. Cross-cultural differences in cognitive development: attention to relations and objects. J Exp Child Psychol 2012; 113:20–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 1993; 46:1417–1432. [DOI] [PubMed] [Google Scholar]
- 20.Wei X, Wang Z, Yang C, et al. Development of a simplified Chinese version of the Hip Disability and Osteoarthritis Outcome Score (HOOS): cross-cultural adaptation and psychometric evaluation. Osteoarthritis Cartilage 2012; 20:1563–1567. [DOI] [PubMed] [Google Scholar]
- 21.Wei X, Yi H, Wu B, et al. A valid cross-culturally adapted simplified Chinese version of the Quebec Back Pain Disability Scale. J Clin Epidemiol 2012; 65:1321–1328. [DOI] [PubMed] [Google Scholar]
- 22.Haher TR, Gorup JM, Shin TM, et al. Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine (Phila Pa 1976) 1999; 24:1435–1440. [DOI] [PubMed] [Google Scholar]
- 23.Asher M, Min Lai S, Burton D, et al. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) 2003; 28:63–69. [DOI] [PubMed] [Google Scholar]
- 24.Lonjon G, Ilharreborde B, Odent T, et al. Reliability and validity of the French-Canadian version of the scoliosis research society 22 questionnaire in France. Spine (Phila Pa 1976) 2014; 39:E26–34. [DOI] [PubMed] [Google Scholar]
- 25.Sathira-Angkura V, Pithankuakul K, Sakulpipatana S, et al. Validity and reliability of an adapted Thai version of Scoliosis Research Society-22 questionnaire for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012; 37:783–787. [DOI] [PubMed] [Google Scholar]
- 26.Zhao L, Zhang Y, Sun X, et al. The Scoliosis Research Society-22 questionnaire adapted for adolescent idiopathic scoliosis patients in China: reliability and validity analysis. J Child Orthop 2007; 1:351–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Field A. Exploratory factor analysis. Discovering Statistics Using SPSS 3rd ed.Los Angeles: SAGE Publications; 2009. 627–681. [Google Scholar]
- 28.Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use. New York: Oxford University Press; 1995. [Google Scholar]
- 29.Nunnally J, Bernstein I. Psychometric Theory. San Francisco, CA: McGraw-Hill; 1994. [Google Scholar]
- 30.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86:420–428. [DOI] [PubMed] [Google Scholar]
- 31.Colton T. Statistics in Medicine. Boston, MA: Little, Brown and Company; 1974. [Google Scholar]
- 32.Altaf F, Gibson A, Dannawi Z, et al. Adolescent idiopathic scoliosis. BMJ 2013; 346:f2508. [DOI] [PubMed] [Google Scholar]
- 33.Plaszewski M, Nowobilski R, Kowalski P, et al. Screening for scoliosis: different countries’ perspectives and evidence-based health care. Int J Rehabil Res 2012; 35:13–19. [DOI] [PubMed] [Google Scholar]
- 34.Ueno M, Takaso M, Nakazawa T, et al. Prevalence rate of idiopathic scoliosis in Tokyo: school screening of more than 250,000 children. J Orthop Sci 2011; 16:1–6. [DOI] [PubMed] [Google Scholar]
- 35.Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013; 369:1512–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Danielsson AJ, Hasserius R, Ohlin A, et al. Body appearance and quality of life in adult patients with adolescent idiopathic scoliosis treated with a brace or under observation alone during adolescence. Spine (Phila Pa 1976) 2012; 37:755–762. [DOI] [PubMed] [Google Scholar]
- 37.Sanders JO, Harrast JJ, Kuklo TR, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 2007; 32:2719–2722. [DOI] [PubMed] [Google Scholar]
- 38.Misterska E, Glowacki M, Harasymczuk J. Brace and deformity-related stress level in females with adolescent idiopathic scoliosis based on the Bad Sobernheim Stress Questionnaires. Med Sci Monit 2011; 17:CR83–CR90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jingang A. Which future for doctors in China? Lancet 2013; 382:936–937. [DOI] [PubMed] [Google Scholar]


