Abstract
Polypharmacy is common in the elderly due to multimorbidity and interventions. However, the temporal association between polypharmacy and renal outcomes is rarely addressed and recognized. We investigated the association between cardiovascular (CV) polypharmacy and the risk of acute kidney injury (AKI) in elderly patients.
We used the Taiwan National Health Insurance PharmaCloud system to investigate the relationship between cumulative CV medications in the 3 months before admission and risk of AKI in the elderly at their admission to general medical wards in a single center. Community-dwelling elderly patients (>60 years) were prospectively enrolled and classified according to the number of preadmission CV medications. CV polypharmacy was defined as use of 2 or more CV medications.
We enrolled 152 patients, 48% with AKI (based upon Kidney Disease Improving Global Outcomes [KDIGO] classification) and 64% with CV polypharmacy. The incidence of AKI was higher in patients taking more CV medications (0 drugs: 33%; 1 drug: 50%; 2 drugs: 57%; 3 or more drugs: 60%; P = 0.05) before admission. Patients with higher KDIGO grades also took more preadmission CV medications (P = 0.04). Multiple regression analysis showed that patients who used 1 or more CV medications before admission had increased risk of AKI at admission (1 drug: odds ratio [OR] = 1.63, P = 0.2; 2 drugs: OR = 4.74, P = 0.03; 3 or more drugs: OR = 5.92, P = 0.02), and that CV polypharmacy is associated with higher risk of AKI (OR 2.58; P = 0.02). Each additional CV medication increased the risk for AKI by 30%.
We found that elderly patients taking more CV medications are associated with risk of adverse renal events. Further study to evaluate whether interventions that reduce polypharmacy could reduce the incidence of geriatric AKI is urgently needed.
INTRODUCTION
Clinical practitioners attempt to balance disease management with drug-related adverse events and economic costs or insurance coverage challenges when prescribing medications. Polypharmacy, the use of multiple medications, has become increasingly common in healthcare systems throughout the world because management of many chronic illnesses, such as hypertension, heart failure, coronary artery disease, musculoskeletal and neuropathic pain often requires multiple medications.1 However, drug-related adverse effects can occur when the number of medications increases, especially in elderly patients with multimorbidity. Moreover, as more medications are used adherence and compliance to treatments often decrease and drug interactions and adverse effects become more common.2,3 Prescription of complex regimens and the resultant nonadherence may potentially contribute to poor disease control, recurrent hospitalizations, and higher mortality.4,5 Thus, polypharmacy is an issue of critical importance for geriatric patients and their prescribers.
It is estimated that more than 50% of elderly people residing in the community receive cardiovascular (CV) medications, especially antihypertensive agents.6 CV medications are among the most commonly prescribed drugs in the elderly.7 A survey of nursing home residents (mean age: 85) found that 40% to 50% of the patients were taking antiplatelet agents and angiotensin II-converting enzyme inhibitors/angiotensin receptor blockers (ACEIs/ARBs).8 CV disorders, including heart failure and left ventricular hypertrophy, are often accompanied by systemic neurohormonal activation and renal maladaptation, increasing renal susceptibility to acute insults. The subsequent functional and even structural renal damages further complicate the management of the underlying CV disorders. On the other hand, patients with advanced chronic kidney disease (CKD) also tend to develop CV diseases, possibly owing to the accompanied chronic inflammation, hypertension, anemia, fluid overload, and divalent ion imbalances, as well as uremic toxin effects.9 Thus, acute kidney injury (AKI) is expectedly a frequent complication in patients with heart failure and related CV disorders, while CKD could serve both as a complication and a precipitant of incident CV diseases.10 CKD, by itself also a comorbidity, plays a role in influencing our pharmaceutical choices in managing CV diseases. In light of the above, elderly patients who have more CV comorbidities tend to use more medications and might have a higher risk of developing AKI from their complications arising during the treatment.
However, it is unclear whether the elevated risk of AKI in the elderly is associated with CV diseases themselves, the associated multimorbidity, or the pharmacologic regimen used to treat them (Figure 1). The effect of CV diseases and the accompanied comorbidity on the risk of AKI in the elderly has been widely recognized, such as the adverse influence posed by diabetes mellitus (DM), but the impact of concurrent CV medications use is rarely accounted for in the analyses. Previous research on the relationship between CV medications and risk of AKI mostly addressed the effect of individual CV medications, without considering the potential adverse effects exerted by polypharmacy. For example, researchers have reported that long-term preoperative ACEIs/ARBs use is associated with more AKI episodes in cardiac surgery recipients.11 Other research suggested that use of diuretics and antibiotics might correlate with subsequent development of renal dysfunction, especially in the elderly.12
FIGURE 1.

Study hypothesis.
We hypothesize that CV medications as well as polypharmacy, rather than the effect of CV disorders or their associated multimorbidity, is the principal factor associated with increased risk of subsequent AKI and adverse hospitalization outcomes in geriatric patients. Renal events, AKI in this study, were regarded as the complications (the main outcomes) during the clinical courses instead of comorbidities. We investigated this issue using a prospective geriatric cohort with a comprehensive review of admission diagnoses (the acute insult), concurrent comorbidities, and their medication usage within the past 3 months before admission.
MATERIALS AND METHODS
Study Design
The present study was performed at the National Taiwan University Hospital (NTUH), a tertiary referral center that treats patients from all parts of Taiwan. In-patients older than 60 years were prospectively enrolled from the general medical wards of the NTUH between January and December 2014. All enrollees provided informed consent. After enrollment, demographic profiles (age and gender), body mass index (BMI), and clinical data including comorbidities and main diagnosis at admission were collected. Hypertension was defined as past or current use of antihypertensive agents or blood pressure more than 140/90 mm Hg on admission. Coronary artery disease, heart failure, peripheral artery disease, and previous cerebrovascular events were recorded if documented by the presence of symptoms, laboratory results, and image findings. DM was recorded according to the most recent guidelines.13 Pulmonologists diagnosed chronic obstructive pulmonary disease (COPD) based on symptoms. Malignancy was verified by histopathologic data. CKD was defined as a baseline estimated glomerular filtration rate <60 mL/min/1.73 m2, calculated with the Modification of Diet in Renal Disease formula.
The study protocol was approved by the NTUH ethics committee (no. 201306089RINA) and was conducted in adherence with the Declaration of Helsinki.
Medication Identification and Categorization
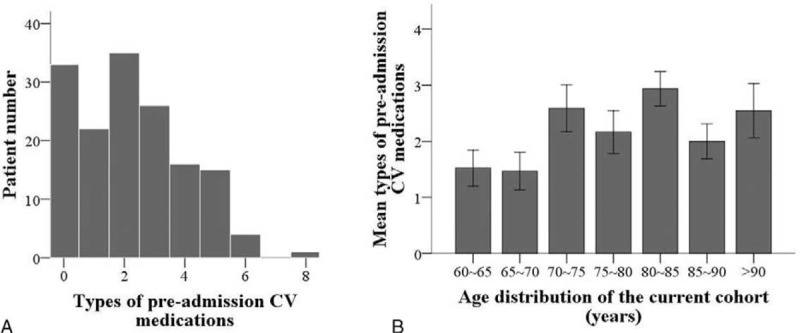
We recorded preadmission use of CV medications for all patients. CV polypharmacy was defined using the cumulative concept, that is the sum of all types of different medications prescribed for treating CV disorders within a 3-month period before admission.14 The CV medications included were antihypertensive agents (ACEIs/ARBs, β-blockers, calcium channel blockers, and α-blockers), antiarrhythmic agents, diuretics, lipid-lowering agents, nitrates, antiplatelet agents, and digoxin.15,16 Medications with nephrotoxic potentials, including aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), ACEIs/ARBs, diuretics, statin, calcineurin inhibitors, certain antibiotics, chemotherapeutic agents, and atypical antipsychotics (reportedly associated with AKI in the elderly),17 were recorded. The medication lists of all patients were retrospectively reviewed and recorded on the first day of admission using the Taiwan National Health Insurance PharmaCloud system (Figure 2).18 The PharmaCloud system is a web-based database established by Taiwan National Health Insurance that allows physicians to cross-check all out- and in-patient prescription records from the 3 month period before a medical encounter. A high percentage of the Taiwan population has insurance coverage (>99%), so the PharmaCloud system can accurately track essentially all medications used by each patient.
FIGURE 2.
Study design.
Outcome Variables
Elderly patients were prospectively followed after admission until death or discharge (Figure 2). The primary endpoint was the absence or presence of AKI at admission, and the secondary endpoint was duration of hospitalization and mortality during the index admission. AKI was diagnosed by serum creatinine (sCr) level, as described by the Kidney Disease Improving Global Outcomes (KDIGO) classification.19 These criteria classify AKI as grade 1 (sCr elevation 50% to 100% within 7 days or >0.3 mg/dL within 48 h), grade 2 (sCr elevation 100% to 200%), and grade 3 (sCr elevation >200% or >4 mg/dL, or initiation of dialysis). Baseline sCr was obtained within 3 months of admission.
Statistical Analysis
We used SPSS 18.0 software (SPSS Inc., Chicago, IL) for statistical analyses. Continuous variables are given as means ± standard deviations and compared with the independent t test. Categorical variables are given as number (percentage) and compared with the Chi-square test. We divided the entire cohort according to the number of CV drugs used before admission, and compared clinical variables of these groups. To investigate the relationship between preadmission CV polypharmacy and AKI on admission, we further stratified the cohort into those with or without initial AKI, and then analyzed group differences with the independent t-test. For calculation of odds ratios (ORs), we performed multiple regression analysis that incorporated demographic profiles, comorbidities, and admission diagnoses with stepwise variable selection to determine the effect of CV polypharmacy on subsequent AKI and hospitalization outcome. A 2-sided P value <0.05 was considered statistically significant.
RESULTS
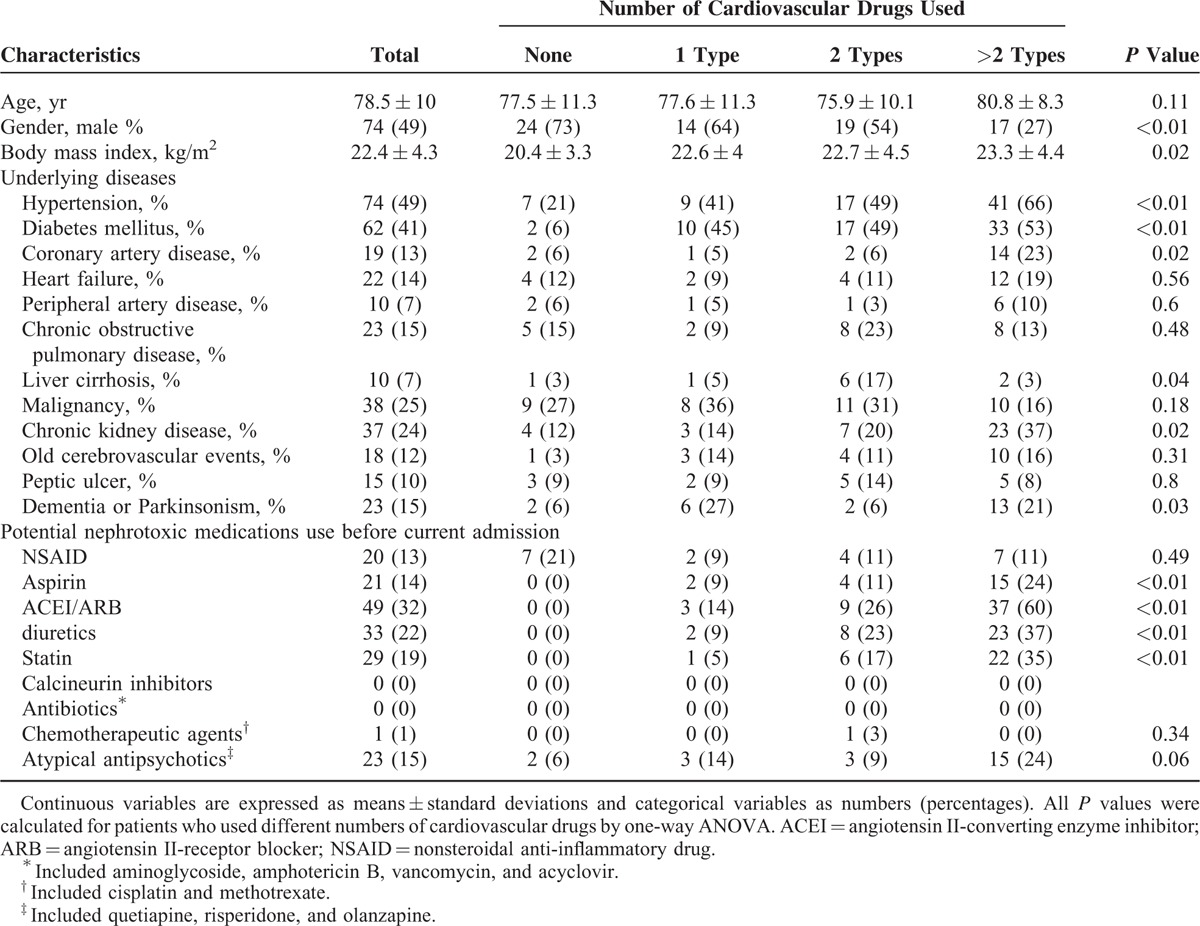
We enrolled 152 geriatric patients (age >60 years) during the 1-year study period. Figure 3A shows the number of CV drugs used by the entire cohort before admission (mean: 2.2 ± 1.8, range: 0–8). For subsequent analysis, we divided the cohort into quintiles of total number of CV drugs that were used (0 drugs: n = 33, 21.7%; 1 drug: n = 22, 14.5%; 2 drugs: n = 35, 23%; 3 or more drugs: n = 62, 40.8%). CV polypharmacy, defined as usage of 2 or more medications at the same time,20,21 was present in 64% (n = 97) of the study cohort. The prevalence of potentially inappropriate medications (PIMs) prescription in our cohort was 37.5% (n = 57), according to Screening Tool of Older Person's Prescriptions (STOPP) criteria for CV medications.22
FIGURE 3.
(A) Use of preadmission cardiovascular (CV) medications in the entire study cohort. (B) Use of preadmission CV medications of different age groups.
Table 1 shows the demographic and clinical characteristics of patients who used different numbers of CV drugs. Those taking more CV medications were more likely to be female (P < 0.01) and to have a higher BMI (P = 0.02). In addition, patients 70-year-old and older tend to take significantly more CV medications than those between 60 and 70 years old (Figure 3B). As expected, patients who took more CV medications were more likely to have hypertension (P < 0.01), DM (P < 0.01), coronary artery disease (P = 0.02), and CKD (P = 0.02). We discovered that the percentage of aspirin, ACEIs/ARBs, diuretics, and statin use increased stepwise with increasing CV medication counts (P < 0.01 for all types of drugs); however, other potential nephrotoxic drugs, including NSAIDs use, did not differ between groups with different CV medication counts (Table 1).
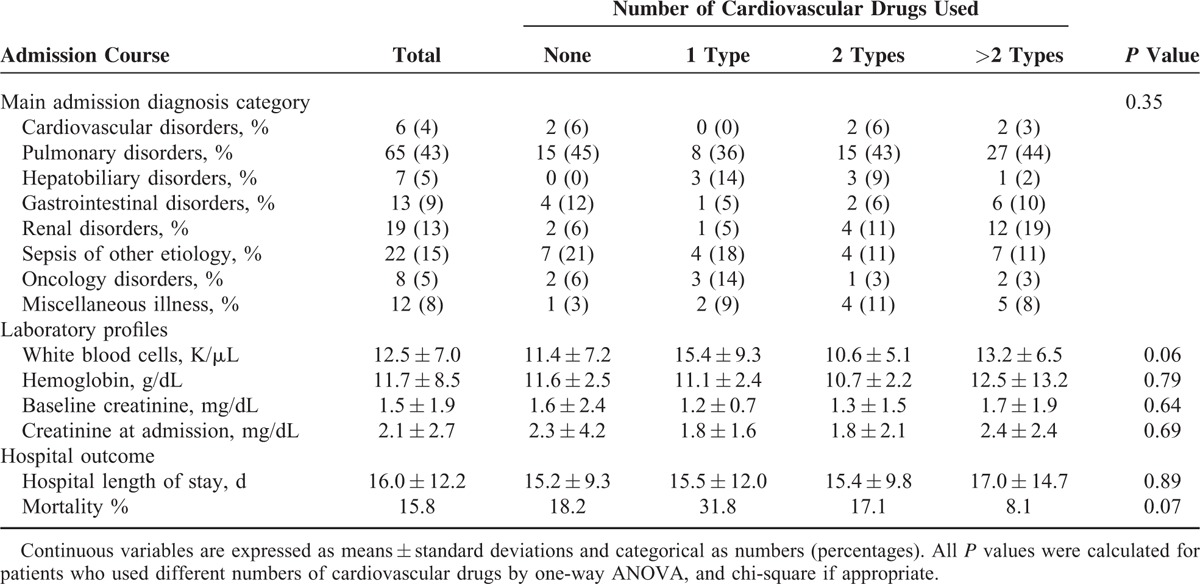
TABLE 1.
Baseline Characteristics of the Study Cohort (n = 152)
On admission, the main diagnoses were pulmonary disorders, and admission diagnosis did not differ significantly among those taking different numbers of CV medications (Table 2). Laboratory data, including hemogram, baseline sCr, and admission sCr, was also similar in those taking different numbers of medications.
TABLE 2.
Admission Course (Diagnosis, Laboratory Profile, and Outcome) of Patients Who Used Different Numbers of Cardiovascular Drugs
On admission, 73 patients (48%) presented with AKI, and patients taking more CV medications had a significantly higher incidence of AKI (0 drugs: 33%; 1 drug: 50%; 2 drugs: 57%; 3 or more drugs: 60%; P = 0.05). An alternative analysis indicated that those with initial AKI took significantly more preadmission medications than those without AKI (2.5 vs 1.9, P = 0.03). Next, we stratified the 73 patients with AKI according to KDIGO criteria (Figure 4). The results indicate that patients with increasingly severe AKI (higher KDIGO grade) took more preadmission medications (P = 0.04).
FIGURE 4.
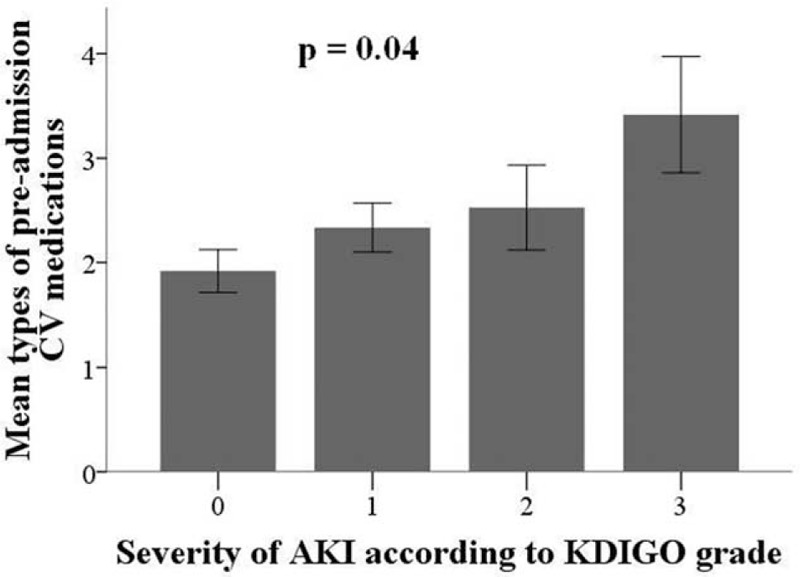
Use of preadmission cardiovascular medications in patients with different severities of acute kidney injury, based on Kidney Disease Improving Global Outcomes criteria.
A total of 24 patients (15.8%) died during hospitalization, and the mean length of hospitalization was 16 days. There were no significant differences in duration of hospitalization (P = 0.89) and mortality (P = 0.07) in patients using different numbers of medications.
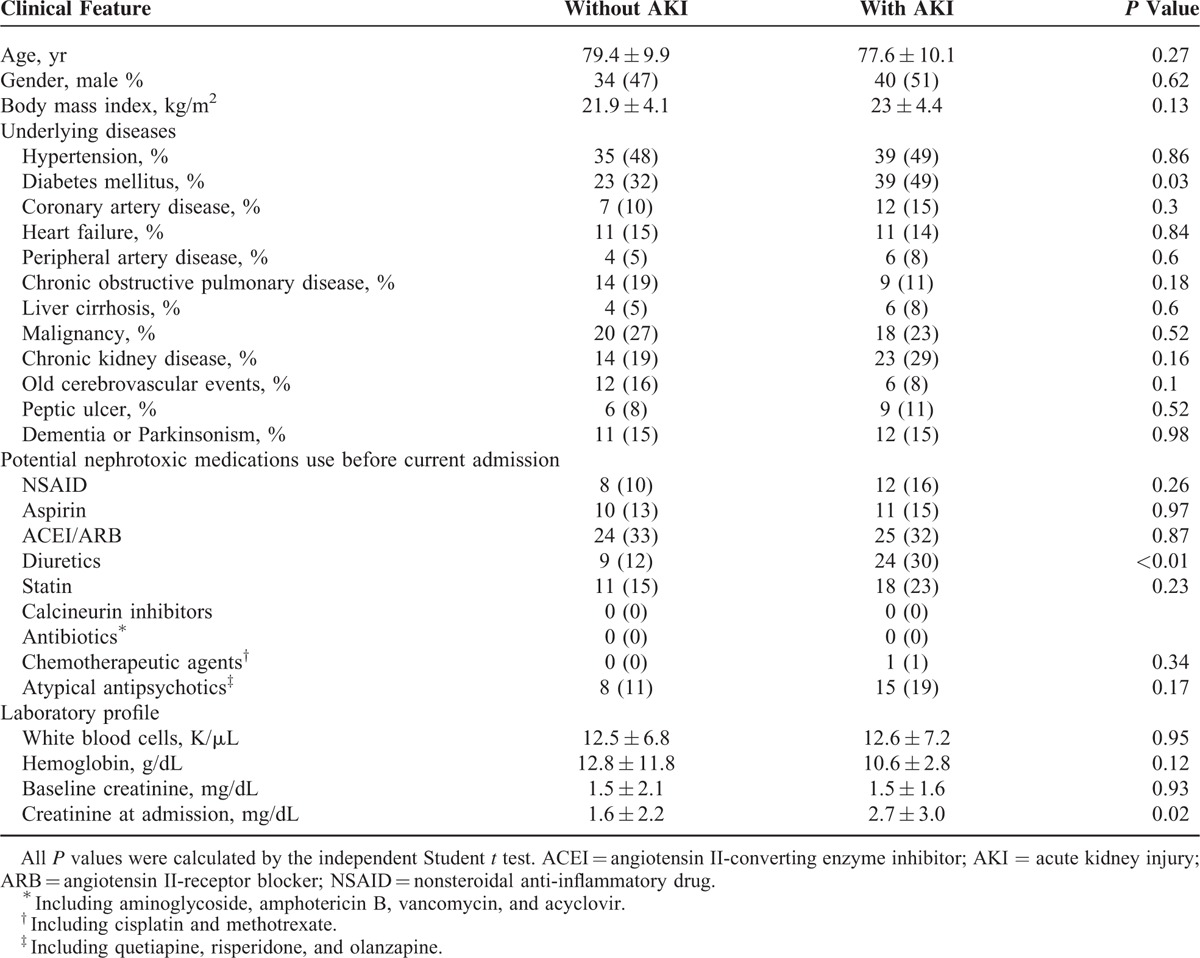
We also compared the clinical and laboratory data of patients with and without initial AKI (Table 3). Patients with AKI were more likely to have DM (P = 0.03) and higher sCr at admission (P = 0.02), but there were no differences in the other measured variables, including other potential nephrotoxic medications used in the preceding 3 months before admission. Similarly, the percentage of PIMs prescription among elderly with and without AKI did not differ (the former vs the latter, 44.3% vs 30.1%; P = 0.07). However, diuretics use was significantly more common in those with AKI compared to those without (P < 0.01).
TABLE 3.
Clinical Features of Patients With and Without AKI at Admission
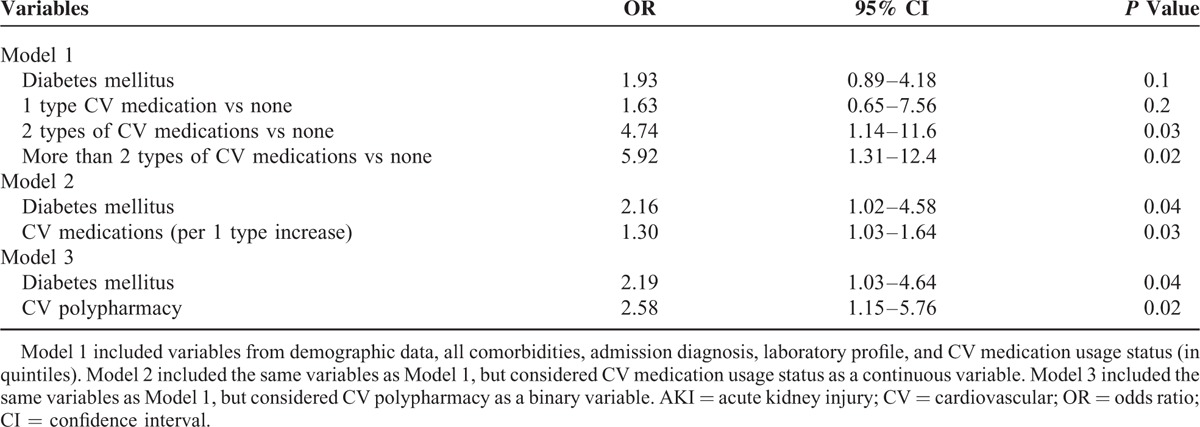
Finally, we determined whether preadmission CV polypharmacy was associated with AKI at admission by use of multiple regression analysis, with presence of AKI at admission as the dependent variable (Table 4). The results show that patients who used more CV medications exhibited greater risk of AKI than those who used no medications (1 drug: OR = 1.63, P = 0.2; 2 drugs: OR = 4.74, P = 0.03; 3 or more drugs: OR = 5.9, P = 0.02), independent of any comorbidity. Sensitivity analysis, with CV medication count as a linear variable, indicated that addition of a single new CV medication increased the risk for AKI by 30%. An alternative analysis indicated that patients with CV polypharmacy also had a greater risk of AKI (OR = 2.58; P = 0.02). Inclusion of nephrotoxicants including aspirin, NSAID, ACEIs/ARBs, and statin use in the regression models essentially did not change our results. However, inclusion of PIMs in our regression model significantly attenuated the significant association of CV polypharmacy with the risk of AKI (in model 1, P = 0.44; in model 2, P = 0.35), while the association remained significant in model 3 (P = 0.02). Similarly, inclusion of diuretics use also significantly attenuated the association in models 1 (P = 0.35) and 2 (P = 0.1) but not in model 3 (P = 0.05).
TABLE 4.
Multiple Regression Analyses of Factors Independently Associated With Development of AKI
DISCUSSION
The results of this study indicate that preadmission CV polypharmacy is associated with subsequent AKI in elderly patients even after adjusting for the acute insults (CV diseases per se), the associated comorbidities, and the individual CV medication components, and that the risk of AKI increased with CV polypharmacy aggravation. However, CV polypharmacy had no effect on the duration of hospitalization and mortality in our cohort. These findings suggest that CV polypharmacy of geriatric patients is an important albeit under-appreciated issue that deserves more attention.
Most reports agree that there is a progressive age-dependent increase in the incidence of AKI, with a 3- to 8-fold higher risk in the elderly, depending on how “elderly” is defined.23,24 Moreover, the average age of AKI patients has gradually increased over time (mean age: 70–80 years).25 These trends support the finding that 48% of our elderly patients (mean age: 78.5 years) presented with AKI on admission (Table 1). The in-hospital mortality of our elderly patients (15.8%) was also within the range reported in other studies of community-acquired AKI (11% to 20%).26,27
AKI is more common in patients with DM, possibly related to the milieu of hyperglycemia. Experimental studies have shown that elevated glucose levels could increase oxidative stress in kidneys, reduce local nitric oxide levels with impairment of vasodilation responses, compromise endothelial functions, and enhance ischemic reperfusion injury.28 Epidemiological surveys also revealed that presence of DM is associated with 2- to 3-fold higher risk for AKI in patients undergoing surgery.29 In the present study, although the percentage of DM among elderly patients with and without AKI differed significantly (49% vs 32%; P = 0.03), multiple regression analysis did not identify DM as a significant risk factor for AKI development (Table 4). We presume that the following factors might be responsible; first, past reports did not include polypharmacy and few of them included nephrotoxic medications in their analysis. Alternatively, the study population also differed. We focused on elderly patients (≥65 years), while others mostly addressed different clinical settings instead of specific age group. Finally, our modest case number might also be 1 contributory factor.
Currently, there is no standard definition for polypharmacy in the literature, even though the risk of compound medication use is considered significant. Polypharmacy was conventionally defined as use of at least 1 PIM, or use of 2 to 6 or more concurrent medications.30 We considered polypharmacy as use of 2 or more medications because of the higher sensitivity and the ease to determine by chart review, but the true impact of polypharmacy on patients might still be confounded by multiple comorbidities that require treatment by multiple drugs and by the potential for poor adherence in the elderly. Indeed, previous research found that 1/3 to 1/2 of patients had poor adherence to antihypertensive and lipid-lowering drugs.31 Consequently, we also adopted the concept of “cumulative polypharmacy” to better characterize the usage of CV drugs in our cohort. Our analyses suggested that the use of more CV drugs was associated with subsequent development of AKI, and supports the view that polypharmacy might have a significant clinical impact, especially renal outcomes. Thus, it is likely that, apart from the effect of CV diseases and the associated comorbidities, CV polypharmacy might negatively influence clinical outcomes.
Past studies suggested that polypharmacy increased the risk of geriatric syndromes (sphincter incontinence, cognitive and balance impairment), the rate of hospitalization, and the number of in-hospital complications.32,33 However, few reports examined the relationship between polypharmacy and AKI. One such report based on an insurance database found that prolonged polypharmacy increased the risk of hospitalization for AKI.34 However, the low sensitivity of billing codes (∼17%), variable exclusion criteria, and lack of descriptions of AKI severity and laboratory details are limitations of this study.35 Another study indicated that use of each additional drug before surgery was associated with a 2.7-fold higher risk of postoperative complications, including acute renal failure36; moreover, this risk was mostly from CV medications, because exclusion of these medications significantly attenuated the observed negative effect.36 Taken together with our results, this supports the view that, in addition to the conventional belief that a single-drug-class can induce AKI, polypharmacy— especially CV polypharmacy—was also associated with the risk of renal dysfunction. Moreover, we demonstrated a dose-dependent relationship between CV polypharmacy and AKI risk (more severe CV polypharmacy accompanying more severe AKI), which strengthens our proposition that such biologic association existed in the elderly (Figure 4). However, the lack of influence of polypharmacy on hospital mortality might be explained by other in-hospital events that altered medication regimens and counter-acted the negative impact of CV polypharmacy (Figure 5).
FIGURE 5.
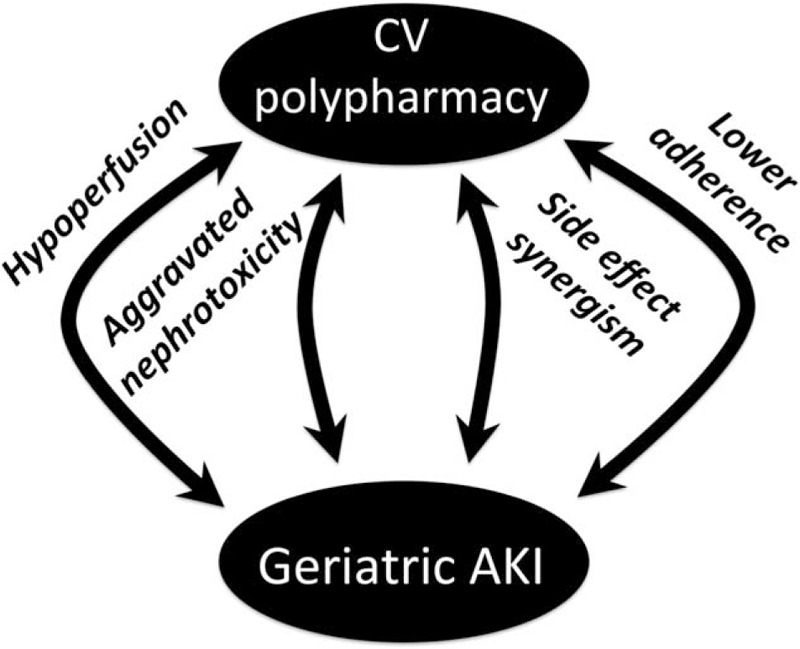
Possible influence of cardiovascular polypharmacy on renal events and hospital outcomes.
The mechanisms underlying the association between CV polypharmacy and AKI could be complex, but can be classified as hemodynamic factors (systemic or glomerular), aggravation of nephrotoxicity, synergism of side effects, and impairment of adherence (Figure 5). First, use of multiple CV medications may affect blood pressure significantly, leading to bradycardia and ultimately to impaired renal perfusion. Use of ACEIs/ARBs might further reduce the glomerular filtration rate (GFR) and thereby increase the risk for AKI in elderly patients.11 Second, CV medications may lead to aggravation of nephrotoxicity; in other words, drugs compromising renal perfusion might indirectly reduce the excretion of other medications from the kidneys, causing adverse drug reactions and AKI, an outcome that would not have occurred without polypharmacy. Third, side effects of different CV medications could act together synergistically and precipitate AKI. For instance, concurrent use of dronedarone and diuretics can increase the risk of dehydration-related prerenal azotemia from both diarrhea (dronedarone) and excessive urine loss (diuretic).37 Fourth, from the patients’ perspective, polypharmacy might reduce adherence to vital CV medications, leading to poor disease control, including hypertensive crisis, dyslipidemia, and atherosclerosis, all of which might alter the risk of subsequent AKI.2,3,38 Finally, it is possible that CV polypharmacy is also accompanied by concurrent use of other nephrotoxic medications, including NSAIDs. Elderly patients frequently had chronic musculoskeletal pain, the prevalence of which increases as population ages in addition to higher CV comorbidities.39 As NSAIDs are frequently co-prescribed for pain relieving purpose, NSAIDs might play an important role in precipitating these adverse events, while topical NSAIDs might be safer.40 Since the inclusion of PIMs and diuretics use significantly attenuated the significance of CV polypharmacy in some but not all our models, the association between CV polypharmacy might be mediated partially by PIMs prescription or specific component of the pharmaceutical regimen. Consequently, CV polypharmacy might be associated with the development of AKI through the effects of medications per se or by altering patient behaviors (adherence).
Our study has strengths and limitations. Through the cross-comparison of a comprehensive administrative pharmaceutical database and laboratory records, we successfully established the relationship between CV polypharmacy and the development of AKI in a cohort of elderly patients. We also demonstrated that the severity of AKI increased as patients used more CV drugs. These findings support the view that polypharmacy and AKI are frequently associated. However, the present study is also limited by the relatively modest case numbers and the sole inclusion of elderly subjects who had acute episodes that required hospitalization. It is possible that many patients with subtler or more gradual alterations of renal function, such as the sub-AKI,41 were not included. If so, this would result in an under-estimation of risk. In addition, it is possible that the elevated risk of AKI in the elderly might also result from other individual components of their CV medications besides their cumulative effect. We have tried to address this issue through the adjustment for multiple potential nephrotoxicants in our regression models, and the effect of most identified agents seemed modest. Nonetheless, we could not rule out the possibility that the higher risk of AKI in these patients came from their comorbidities. Despite all these limitations, our findings can still serve as a useful foundation for larger and more thorough studies of the impact of polypharmacy on AKI risk in geriatric patients.
CONCLUSION
In the present study, CV polypharmacy, defined as use of 2 or more CV medications, was associated with significantly higher frequency of AKI in geriatric patients. Moreover, patients who used more CV medications had more severe AKI. Although our findings lend support to the potential adverse influence of CV polypharmacy in geriatric patients, the risk–benefit ratio of CV polypharmacy is still unclear. Further studies that use different criteria to define polypharmacy and that harness interventions to ameliorate CV polypharmacy would be needed to draw a more definitive conclusion.
ACKNOWLEDGMENTS
We are grateful to the medical and nursing staffs of the multidisciplinary wards of NTUH for their support in data collection.
Footnotes
Abbreviations: ACEI = angiotensin II-converting enzyme inhibitor, AKI = acute kidney injury, ARB = angiotensin-II receptor blocker, BMI = body mass index, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CV = cardiovascular, DM = diabetes mellitus, KDIGO = Kidney Disease Improving Global Outcomes, MDRD = Modification of Diet in Renal Disease, NSAID = nonsteroidal anti-inflammatory drug, NTUH = National Taiwan University Hospital, OR = odds ratio, PIM = potentially inappropriate medication, sCr = serum creatinine, STOPP = Screening Tool of Older Person's Prescriptions.
Author contributions: Study design (C-TC, H-BT); data analysis (C-TC, H-BT, C-YW, Y-FL, N-CH, K-YH); drafting article (all authors); and approval of article (all authors).
This study is financially supported by NTUH (project nos. 102-N2249 and 103-N2525).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62:e147–e239. [DOI] [PubMed] [Google Scholar]
- 2.Knafl GJ, Riegel B. What puts heart failure patients at risk for poor medication adherence. Patient Prefer Adherence 2014; 8:1007–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pasina L, Brucato AL, Falcone C, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging 2014; 31:283–289. [DOI] [PubMed] [Google Scholar]
- 4.Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006; 333:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu P-H, Yang C-Y, Yao Z-L, et al. Relationship of blood pressure control and hospitalization risk to medication adherence among patients with hypertension in Taiwan. Am J Hypertens 2010; 23:155–160. [DOI] [PubMed] [Google Scholar]
- 6.Callisaya ML, Sharman JE, Close J, et al. Greater daily defined dose of antihypertensive medication increases the risk of falls in older people—a population-based study. J Am Geriatr Soc 2014; 62:1527–1533. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Zhao Z, Lin E, et al. Unintended effects of cardiovascular drugs on the pathogenesis of Alzheimer's disease. PLoS ONE 2013; 8:e65232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beloosesky Y, Nenaydenko O, Gross Nevo RF, et al. Rates, variability, and associated factors of polypharmacy in nursing home patients. Clin Interv Aging 2013; 8:1585–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clementi A, Virzi GM, Goh CY, et al. Cardiorenal syndrome type 4: a review. Cardiorenal Med 2013; 3:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Virzì GM, Clementi A, Brocca A, et al. The hemodynamic and nonhemodynamic crosstalk in cardiorenal syndrome type 1. Cardiorenal Med 2014; 4:103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coca SG, Garg AX, Swaminathan M, et al. Preoperative angiotensin-converting enzyme inhibitors and angiotensin receptor blocker use and acute kidney injury in patients undergoing cardiac surgery. Nephrol Dial Transplant 2013; 28:2787–2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Handler SM, Cheung PW, Culley CM, et al. Determining the incidence of drug-associated acute kidney injury in nursing home residents. J Am Med Dir Assoc 2014; 15:719–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014; 37:S81–S90. [DOI] [PubMed] [Google Scholar]
- 14.Fincke BG, Snyder K, Cantillon C, et al. Three complementary definitions of polypharmacy: methods, application and comparison of findings in a large prescription database. Pharmacoepidemiol Drug Saf 2005; 14:121–128. [DOI] [PubMed] [Google Scholar]
- 15.Tjia J, Fischer SH, Raebel MA, et al. Baseline and follow-up laboratory monitoring of cardiovascular medications. Ann Pharmacother 2011; 45:1077–1084. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg PB, Mielke MM, Tschanz J, et al. Effects of cardiovascular medications on rate of functional decline in Alzheimer disease. Am J Geriatr Psychiatry 2008; 16:883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hwang YJ, Dixon SN, Reiss JP, et al. Atypical antipsychotic drugs and the risk for acute kidney injury and other adverse outcomes in older adults: a population-based cohort study. Ann Intern Med 2014; 161:242–248. [DOI] [PubMed] [Google Scholar]
- 18.Pharmacloud System. (accessed January 24, 2015) [Google Scholar]
- 19.Section 2: AKI definition. Kidney Int Suppl 2012;2:19–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu J, Yang M, Luo L, et al. Polypharmacy among nonagenarians/centenarians in rural China. Intern Med J 2014; 44:1193–1199. [DOI] [PubMed] [Google Scholar]
- 21.Veehof L, Stewart R, Haaijer-Ruskamp F, et al. The development of polypharmacy: a longitudinal study. Fam Pract 2000; 17:261–267. [DOI] [PubMed] [Google Scholar]
- 22.Gallagher P, Ryan C, Byrne S, et al. STOPP (Screening Tool of Older Person's Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther 2008; 46:72–83. [DOI] [PubMed] [Google Scholar]
- 23.Chao C-T, Wu V-C, Lai C-F, et al. Advanced age affects the outcome-predictive power of RIFLE classification in geriatric patients with acute kidney injury. Kidney Int 2012; 82:920–927. [DOI] [PubMed] [Google Scholar]
- 24.Abdel-Rahman EM, Okusa MD. Effects of aging on renal function and regenerative capacity. Nephron Clin Pract 2014; 127:15–20. [DOI] [PubMed] [Google Scholar]
- 25.Ali T, Khan I, Simpson W, et al. Incidence and outcomes in acute kidney injury: a comprehensive population-based study. J Am Soc Nephrol 2007; 18:1292–1298. [DOI] [PubMed] [Google Scholar]
- 26.Chertow GM, Burdick E, Honour M, et al. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 2005; 16:3365–3370. [DOI] [PubMed] [Google Scholar]
- 27.Wonnacott A, Meran S, Amphlett B, et al. Epidemiology and outcomes in community-acquired versus hospital-acquired AKI. Clin J Am Soc Nephrol 2014; 9:1007–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Melin J, Hellberg O, Fellstrom B. Hyperglycemia and renal ischaemia-reperfusion injury. Nephrol Dial Transplant 2003; 18:460–462. [DOI] [PubMed] [Google Scholar]
- 29.Thakar CV, Arrigain S, Worley S, et al. A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol 2005; 16:162–168. [DOI] [PubMed] [Google Scholar]
- 30.Bushardt RL, Massey EB, Simpson TW, et al. Polypharmacy: misleading, but manageable. Clin Interv Aging 2008; 3:383–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med 2012; 125:882–887.e1. [DOI] [PubMed] [Google Scholar]
- 32.Alexopoulou A, Dourakis SP, Mantzoukis D, et al. Adverse drug reactions as a cause of hospital admissions: a 6-month experience in a single center in Greece. Eur J Intern Med 2008; 19:505–510. [DOI] [PubMed] [Google Scholar]
- 33.Patterson SM, Cadogan CA, Kerse N, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 2014; 10:CD008165. [DOI] [PubMed] [Google Scholar]
- 34.Chang Y-P, Huang S-K, Tao P, et al. A population-based study on the association between acute renal failure (ARF) and the duration of polypharmacy. BMC Nephrol 2012; 13:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grams ME, Waikar SS, MacMahon B, et al. Performance and limitations of administrative data in the identification of AKI. Clin J Am Soc Nephrol 2014; 9:682–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kennedy JM, Van Rij AM, Spears GF, et al. Polypharmacy in a general surgical unit and consequences of drug withdrawal. Br J Clin Pharmacol 2000; 49:353–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Young C, Wayne MM, Leaver RPL. Reversible acute kidney injury requiring haemodialysis five days after starting dronedarone in a stable 71-year-old man at risk of cardiovascular polypharmacy. J R Coll Physicians Edinb 2013; 43:122–125. [DOI] [PubMed] [Google Scholar]
- 38.Liu YH, Liu Y, Chen JY, et al. LDL cholesterol as a novel risk factor for contrast-induced acute kidney injury in patients undergoing percutaneous coronary intervention. Atherosclerosis 2014; 237:453–459. [DOI] [PubMed] [Google Scholar]
- 39.Barkin RL, Beckerman M, Blum SL, et al. Should nonsteroidal anti-inflammatory drugs (NSAIDs) be prescribed to the older adults? Drugs Aging 2010; 27:775–789. [DOI] [PubMed] [Google Scholar]
- 40.Barkin RL. Reducing cardiovascular risks of nonsteroidal anti-inflammatory drugs by using topical formulations. Am J Cardiol 2009; 104:1315. [DOI] [PubMed] [Google Scholar]
- 41.Fujii T, Uchino S, Takinami M, et al. Subacute kidney injury in hospitalized patients. Clin J Am Soc Nephrol 2014; 9:457–461. [DOI] [PMC free article] [PubMed] [Google Scholar]


