Abstract
The aim of this study was to document the level of pain and functionality in the 12 months following orthopedic surgery and identify if high pain levels following discharge were associated with pain persisting at 12 months.
An observational prospective cohort study was undertaken, following 87 patients (mean age 62.4 years [18–92]; 47.1% male) who required orthopedic surgery at the Royal Hobart Hospital, Australia. Following an initial survey, patients were telephoned at 10 days, 6 weeks, 3 months, and 12 months after discharge.
Postdischarge pain levels were high with 97.4% of patients suffering pain at 10 days, 81.2% at 6 weeks and 79.5% at 3 months. Pain affected the ability to undertake activities of daily living (ADLs) for 32.7% and 20.0% of patients at 10 days and 6 weeks, respectively. Twelve months after discharge, 65.5% of patients reported pain persisting at the surgical site, with 29.9% of all patients suffering moderate–severe incidental pain; and nearly one quarter of patients reported pain affected their sleep or ADLs. Average pain levels rated as moderate–severe at 10 days (P = 0.01) and 6 weeks (P = 0.02) and pain of neuropathic origin at 3 months (30.2% vs 10.3% P = 0.03) and 12 months (30.4% vs 4.9% P = 0.01) were associated with persistent pain at 12 months.
Pain in the period following discharge from hospital is significant and undermanaged. Previous studies has shown that that acute pain, particularly in the first 48 hours following surgery is a predictor for long-term pain after surgery. This study adds to the current literature by showing that pain in the subacute period, following discharge from hospital is also associated with the pain persisting at 12 months. These findings have important implications for improving quality of life as well as potentially preventing persistent pain with increased follow-up and more intensive management of post-discharge pain.
INTRODUCTION
Up to 80% of patients undergoing surgery will experience acute postoperative pain.1 Under management of postoperative pain has been identified as a risk factor for the development of persistent pain,2,3 poor healing, venous thromboembolism, myocardial infarction, readmission to hospital, and extended length of hospital stay.4–6 One study found that following discharge from hospital for a surgical procedure, patients’ pain levels often got worse.7 Another study evaluating postdischarge pain after a total knee arthroplasty8 found that 1 month after discharge 52% of patients reported moderate pain and 16% severe pain while walking. However, there are few studies evaluating the period following discharge from hospital with current multimodal analgesic management plans.
Pain relief in the period following discharge from a surgical unit is potentially more complicated to manage than that during the inpatient phase. Patients are in charge of their own medication, there is sometimes a gap (perceived or actual) in terms of who is responsible for treating the patient (General Practitioner, who generally manages the care of a patient following a hospital discharge or surgeon), and there may be a reduction in the potency or dosing frequency of opioid analgesics when patients transition from an inpatient to home environment. The potential for an association between high pain levels following hospital discharge after surgery or trauma, and pain and functionality at 12 months has received minimal attention in the literature.3,9 To address this gap in the literature, we aimed to evaluate the level of pain, analgesic consumption, and functional status of patients over the 12 months following orthopedic surgery, and identify if higher pain levels during the subacute period (following discharge from hospital to 3 months after surgery) increase the risk of persistent pain at 12 months.
METHODS AND MATERIALS
A prospective, observational study was conducted following patients who underwent orthopedic surgery for a joint replacement (elective or emergency) or an open reduction and internal fixation procedure at the Royal Hobart Hospital, a 550-bed hospital in Tasmania, Australia between January and December 2013. At the time of recruitment, participants were required to be an inpatient and either have undergone surgery within the past 5 days or have been scheduled to undergo surgery during their admission. Exclusion criteria were patients aged less than 18 years, residents of aged care facilities, an inability to speak English, a history of dementia or suspected cognitive decline; and those who experienced a multitrauma event, allowing the focus to be on 1 surgical site.
At the point of recruitment an initial face-to-face survey was conducted. Participants were then contacted by telephone 10 days, 6 weeks, 3 months, and 12 months after discharge from the orthopedic ward. If the initial attempt at contact for the 10 day, 6 week, or 3 month surveys was unsuccessful, the participant was telephoned daily for between 5 and 10 days. If the participant could not be reached after this time no data were collected for that time point, and the participant was contacted at the next scheduled data collection point. At 12 months, all participants were telephoned and where the initial attempt was unsuccessful, repeated calls were made for 1 month, before the participant was considered lost to follow-up. Pain on discharge, discharge medications, compliance with discharge advice or medication usage, and outcomes from follow-up appointments with the hospital were not recorded as part of this study.
During the initial survey, basic demographic and clinical characteristics of the patient were collected including age, social history, and previous pain conditions. In addition, the Hospital Anxiety and Depression Scale (HADS) was administered at baseline. An HADS score of 8 or more for anxiety or depression is considered to be clinically significant.10 The Pain Catastrophizing Scale (PCS) was also administered at baseline, with a Pain Catastrophizing Scale score of 30 or more considered to be clinically significant.11,12 Participants were also asked to rate their level of optimisim (1 very pessimistic, 10 very optimistic), health (1 very unhealthy, 10 very health), pain tolerance (1 copes very well with pain, 10 unable to cope with pain), fear of pain (1 not scared of pain, 10 very scared of pain), and whether they had support when discharged home during this initial interview. The participant's medical notes were reviewed to collect information about intraoperative and acute postoperative pain and its management, as well as medications and medical conditions on admission.
The information collected during the follow-up interviews included the average and the worst levels of pain over the previous week as well as a number of aspects regarding functionality including sleep and activities of daily living (ADLs). Analgesic use in the 24 hours prior to the interview was also recorded (irrespective of the indication for use) and opioid doses were converted to oral morphine equivalents (MEQ).13 At 3 and 12 months the 7-item Douleur Neuropathique 4 (DN4) questionnaire was also administered; a score of 3 or more on the 7 point scale was classified as being consistent with pain of neuropathic origins.14 Recruitment and follow-up interviews were all conducted by the same researcher.
In addition to the directions provided with discharge analgesics, orthopedic patients are provided written information regarding the management of pain following discharge. This information states mild pain should be managed with acetaminophen 4 g daily initially until pain settles where it should then be reduced to, as required. If pain is moderate a non-steroidal anti-inflammatory drugs should be added, followed by tramadol or acetaminophen and codeine if required. If pain is severe immediate release oxycodone should be taken as required, in addition to regular non-steroidal anti-inflammatory drugs and acetaminophen.
Approximately 40% of patients who undergo a joint replacement will experience persistent pain associated with the surgery.15 It was estimated that approximately 100 to 150 eligible patients would be operated on during the year of recruitment; thus, between 79 and 109 patients would need to be recruited for a statistically significant sample size.
Analysis was performed using SPSS Statistics 20 for Windows (SPSS Inc., Chicago, IL). Chi-square and Mann–Whitney U tests were undertaken to evaluate for group differences. Associations between baseline demographics, clinical characteristics, intraoperative, and postoperative factors as well as pain scores at different time points were tested against those who experienced pain at 12 months and those who did not. A P-value of <0.05 was considered to be statistically significant. Missing data were addressed by excluding patients from univariate analysis who did not have the data point of interest recorded.
The University of Tasmania's Health and Medical Research ethics committee granted approval (H12833) for this project and all patients gave informed consent to participate in this study.
RESULTS
One hundred and twenty patients were approached for inclusion in the study, with 101 patients agreeing to participate. Fourteen patients were subsequently excluded for the following reasons: death (1), withdrawal from the study due to ill health/personal reasons (7), lost to follow-up (5), and required further surgery (1).
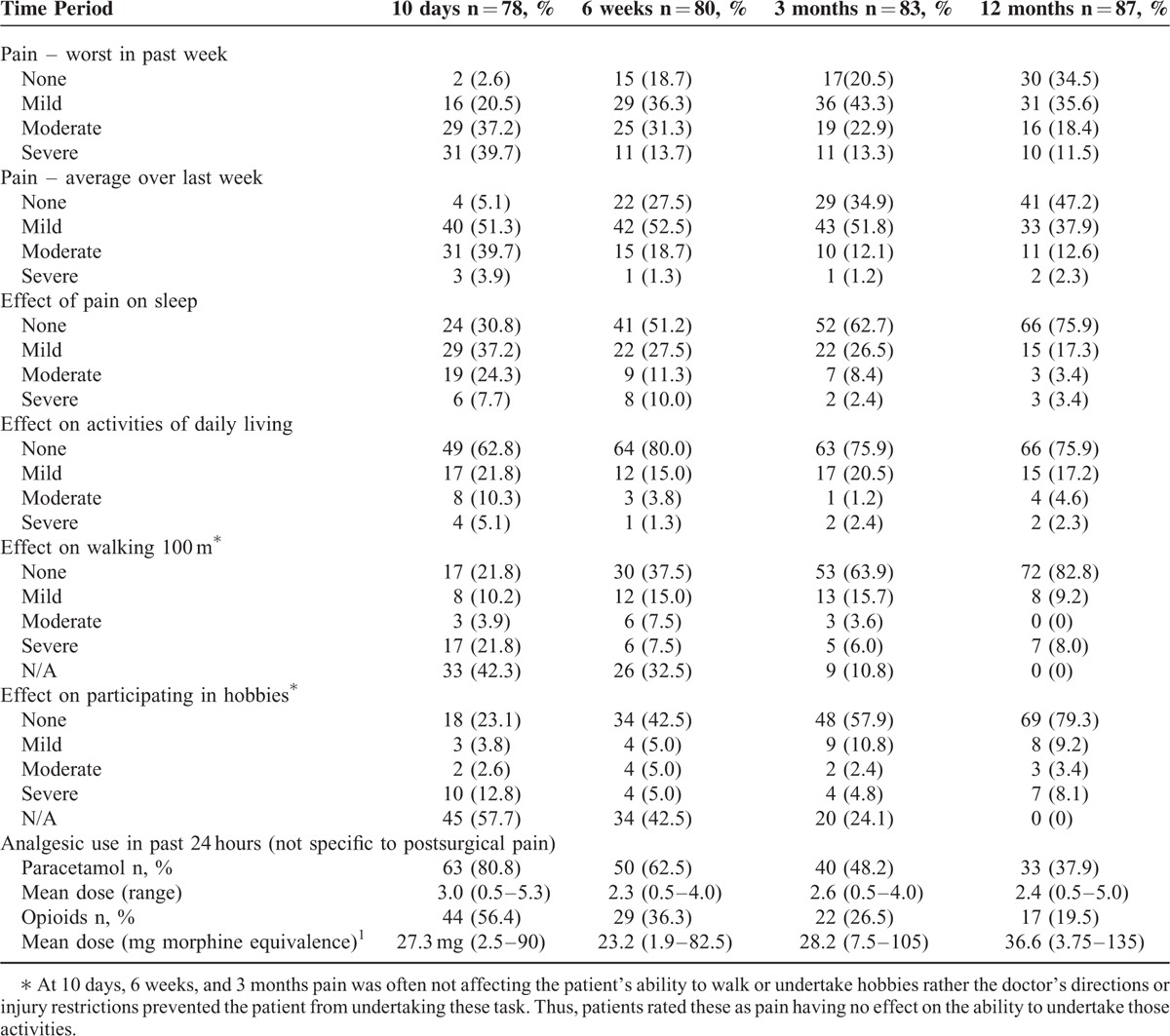
Table 1 shows the demographics and clinical characteristics of the participants. There were no statistically significant differences in relation to baseline characteristics between those who experienced on average, at least mild pain at 12 months and those who did not experience pain. The use of intraoperative ketamine was significantly different between the groups, with patients prescribed intraoperative ketamine being more likely to have pain persisting at 12 months (34.8% vs 14.6% P = 0.03). Patients who were administered regular acetaminophen postoperatively appeared less likely to experience pain at 12 months, although this was not statistically significant (P = 0.07). Persistent pain at 12 months was associated with moderate–severe levels of pain (on average) at 10 days (P = 0.01) and 6 weeks (P = 0.02), and also with a DN4 score of 3 or more, at 3 months (P = 0.03) and 12 months (P = 0.01).
TABLE 1.
Baseline Demographics and Clinical Characteristics According to Pain at Surgical Site at 12 months Following Surgery (n = 87)
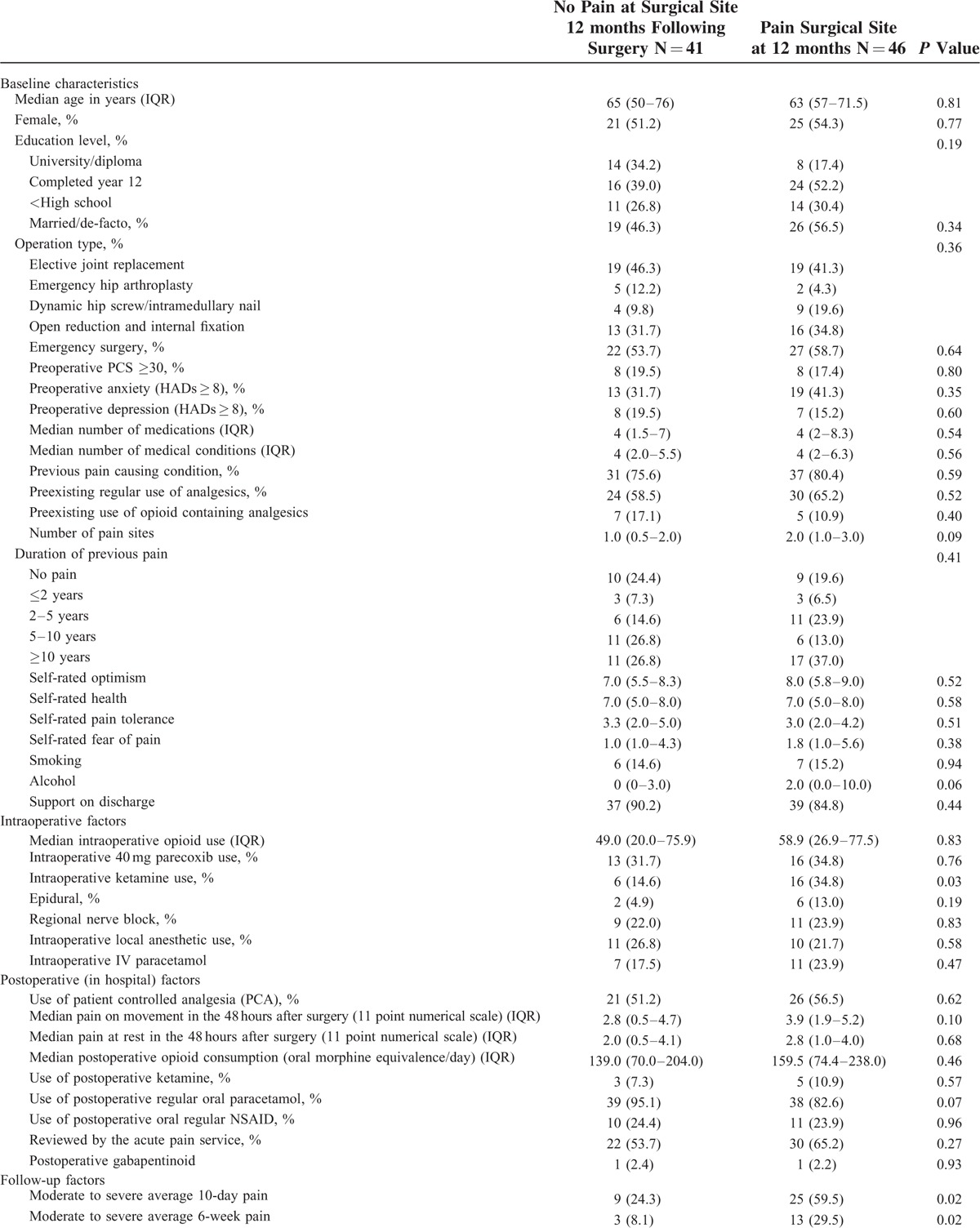
Table 2 shows the level of pain, functionality and analgesic use across the 12-month follow-up period. At 10 days, 97.4% of participants reported pain, with 43.6% experiencing moderate–severe pain on average. Pain affected 69.3% of patients’ ability to sleep and 38.5% of patients’ ability to undertake ADLs. Analgesic use was high with 80.8% taking acetaminophen and 56.4% taking opioids, 97.1% of participants with moderate–severe average pain used analgesics at 10 days.
TABLE 1 (Continued).
Baseline Demographics and Clinical Characteristics According to Pain at Surgical Site at 12 months Following Surgery (n = 87)
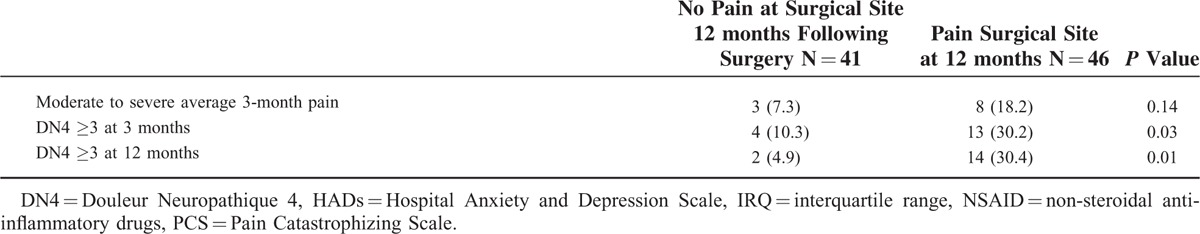
TABLE 2.
Pain Scores and Functionality Across the Follow-Up Period
At 6 weeks, 20.1% of participants experienced on average moderate–severe pain. Pain affected 48.8% of patients’ ability to sleep and 20.3% of patients’ ability to undertake ADLs. Amongst those with moderate–severe pain, 94.1% reported taking analgesia.
By 3 months pain levels continued to improve, although 65.1% of participants were still experiencing some pain, with 13.3% experiencing moderate–severe average pain. At 3 months, 37.3% of patients found pain at the surgical site affected their sleep and 24.1% found pain affected their ability to undertake ADLs. Analgesics were taken by 90.1% of participants with moderate–severe average pain.
At 12 months, 65.5% of participants reported at least mild pain during the week prior to the follow-up, with 14.9% of participants experience moderate–severe average pain. Nearly one quarter of participants reported that pain was adversely affecting their sleep, and/or their ability to perform ADLs. Analgesics were taken by 84.6% of participants with moderate to severe average pain, with 61.5% of this group taking an opioid. Four people with a DN4 of 3 or more at 12 months were taking opioids dosages ranging from 30 to 135 mg MEQ/day.
DISCUSSION
This study followed 87 people for a 12-month period after they underwent orthopedic surgery. The level of pain as well as functional impairment following orthopedic surgery was considerable. At 12 months, over 50% of patients reported experiencing some persistence of pain at the surgical site in the previous week. The use of analgesics, although generally high throughout the follow-up period, was still suboptimal in some cases, with a number of participants experiencing moderate–severe pain but not taking analgesia. This study also found that moderate–severe average pain scores during the subacute period following hospital discharge was associated with pain 12 months following surgery. This finding is supported by other studies that found pain at discharge,16 high pain levels in the first month after a hip fracture surgery17 and pain at 3 months following a major trauma18 all predicted persistent pain beyond 6 to 12 months.
There is clear evidence that the management of pain (by both patients and doctors) following discharge is an area that requires increased attention, not only with regard to the impact this has on persistence of pain 12 months following surgery, but also to improve the quality of life and functional status of patients. A range of actions would be required to achieve this objective including greater patient education regarding management of postoperative pain and when to seek further assistance with pain management as well as additional follow-up with the health care practitioners following discharge.
There were no statistically significant differences between the groups in relation to baseline demographics; however, this may be due to the small sample size. The apparently counterintuitive finding that participants prescribed ketamine in the intraoperative period were more likely to have pain at 12 months is potentially due to anesthetists identifying these patients as being at a higher risk of acute or persistent pain. Amongst those patients who did not receive regular postoperative acetaminophen, 80.0% had persisting pain at 12 months, although this association was not statistically significant due to the small sample size. Considering the good safety profile of acetaminophen and evidence suggesting it reduces opioid consumption following surgery,19 it is concerning to see 10 patients were not prescribed regular acetaminophen postoperatively.
A DN4 of 3 or more at 3 months was associated with pain at 12 months, and for those with pain at 12 months, a DN4 of 3 or more was common. This was not surprizing as a number of studies have identified persistent postoperative pain often has a neuropathic component.2,20,21 Despite this, the use of gabapentinoids postoperatively was minimal, even though studies have indicated that it can reduce acute postoperative pain22 and persistent postoperative pain.23 Postoperative use of gabapentinoids and early identification and management of those with neuropathic symptoms may potentially aid in reducing the incidence and severity of persistent pain following surgery.
There are a number of strengths to this study, including the prospective nature and high participant retention rate throughout follow-up. Treatment protocols and follow-up procedures may vary between hospitals and different countries, and thus potentially these results may not be generalizable to other health care settings. Although the small sample size is a limitation that needs to be acknowledged, this study nonetheless demonstrates that pain and disability in the postdischarge period following orthopedic surgery is considerable with over 40% of patients suffering on average moderate–severe pain 10 days following discharge. In addition, we found that moderate–severe average pain scores at 10 days and 6 weeks postoperatively, were associated with pain persisting at 12 months. These findings have important implications for improving quality of life during this period as well as potentially preventing persistent postoperative pain. This study highlights the need for additional research to evaluate whether increased intervention regarding pain management following hospital discharge can improve pain outcomes and functionality 12 months after orthopedic surgery.
Footnotes
Abbreviations: ADLs = activities of daily living, DN4 = Douleur Neuropathique 4, HADS = Hospital Anxiety and Depression Scale.
This research was supported by a grant from the Royal Hobart Hospital Research Fund (no 13–012).
Subacute pain as a predictor of long-term pain following orthopedic surgery: an Australian prospective 12 month observational cohort study.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Vadivelu N, Mitra S, Narayan D. Recent advances in postoperative pain management. Yale J Biol Med 2010; 83:11–25. [PMC free article] [PubMed] [Google Scholar]
- 2.Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth 2008; 101:77–86. [DOI] [PubMed] [Google Scholar]
- 3.Niraj G, Rowbotham DJ. Persistent postoperative pain: where are we now? Br J Anaesth 2011; 107:25–29. [DOI] [PubMed] [Google Scholar]
- 4.Carr DB, Gousas LC. Acute pain. Lancet 1999; 353:2051–2058. [DOI] [PubMed] [Google Scholar]
- 5.Twersky R, Fishman D, Homel P. What happens after discharge? Return hospital visits after ambulatory surgery. Anesth Analg 1997; 84:319–324. [DOI] [PubMed] [Google Scholar]
- 6.Morrison RS, Magaziner J, McLauglin MA, et al. The impact of post-operative pain on outcomes following hip fractures. Pain 2003; 103:303–311. [DOI] [PubMed] [Google Scholar]
- 7.Apfelbaum JL, Chen C, Mehta SS, et al. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 2003; 97:534–540. [DOI] [PubMed] [Google Scholar]
- 8.Andersen LØ, Gaarn-Larsen L, Kristensen BB, et al. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia 2009; 64:508–513. [DOI] [PubMed] [Google Scholar]
- 9.Wildgaard K, Ravn J, Kehlet H. Chronic post-thorocotomy pain: a critical review of pathogenic mechanisms and strategies for prevention. Eur J Cardiothorac Surg 2009; 36:170–180. [DOI] [PubMed] [Google Scholar]
- 10.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67:361–370. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan MLJ, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess 1995; 7:524–532. [Google Scholar]
- 12.Sullivan MJL. The Pain Catastrophizing Scale User Manual [Web Page]. Available at http://sullivan-painresearch.mcgill.ca/pdf/pcs/PCSManual_English.pdf [Accessed March 18, 2015]. [Google Scholar]
- 13.Gippsland Region Palliative Care Consortium Clinical Practice Group Opioid Conversion Guidelines. Available at http://www.grpcc.com.au/wp-content/uploads/2014/01/GRPCC-CPG002_1.0_2011-Opioid-Conversion-Guidelines.pdf [Accessed June 2, 2015]. [Google Scholar]
- 14.Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes associated with nervouse or somatic lesions and development of a new neuropathic pain disgnostic questionnaire (DN4). Pain 2005; 114:29–36. [DOI] [PubMed] [Google Scholar]
- 15.Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain 2011; 152:566–572. [DOI] [PubMed] [Google Scholar]
- 16.Williamson OD, Epi GD, Gabbe BJ, et al. Predictors of moderate or severe pain 6 months after orthopedic injury: a prospective cohort study. J Orthop Trauma 2009; 23:139–144. [DOI] [PubMed] [Google Scholar]
- 17.Shyu YL, Chen M, Wu C, et al. Postoperative pain and its impact on quality of life for hip-fractured older people over 12 months after hospital discharge. J Clin Nurs 2009; 18:755–764. [DOI] [PubMed] [Google Scholar]
- 18.Rivara FP, MacKenzie EJ, Jurkovich GJ, et al. Prevalence of pain in patients 1 year after major trauma. Arch Surg 2008; 143:282–287. [DOI] [PubMed] [Google Scholar]
- 19.Maund E, McDavid C, Rice S, et al. Paracetamol and selective and non-selective non-steroidal anti-inflammtory drugs for reduction in morphine related side effects after major surgery. Br J Anaesth 2011; 106:292–297. [DOI] [PubMed] [Google Scholar]
- 20.Phillips JRA, Hopwood B, Arthur C, et al. The natural history of pain and neuropathic pain after knee replacement a prospective cohort study of the point prevalence of pain and neuropathic pain to a minimum three-year follow-up. Bone Joint J 2014; 96-B:1227–1233. [DOI] [PubMed] [Google Scholar]
- 21.Dualé C, Ouchchane L, Schoeffler P. the EDONIS Investigating group and Dubray C. Neuropathic aspects of persistent postsurgical pain: a French multicenter survey with a 6-month prospective follow-up. J Pain 2014; 15:24.e1–24.e20. [DOI] [PubMed] [Google Scholar]
- 22.Tiippana EM, Hamunen K, Kontinen VK, et al. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg 2007; 104:1545–1556. [DOI] [PubMed] [Google Scholar]
- 23.Clarke H, Bonin RP, Orser BA, et al. The Prevention of chronic postsurgical pain using gabapentin and pregabalin: A combined systematic review and meta-analysis. Anesth Analg 2012; 115:428–442. [DOI] [PubMed] [Google Scholar]


