Abstract
Unintentional injuries are the leading cause of death among children. Previous research has shown that most of the injuries occur in and around the home. Therefore, parents have a key role in the occurrence and prevention of injuries. In this study, we examined the relationship among home injuries to children and parental attention deficit hyperactivity disorder (ADHD) symptoms, parental attitudes, and children's behavioral problems.
Forty children who were admitted to the emergency department because of home injuries constitute the study group. The control group also consisted of 40 children, who were admitted for mild throat infections. The parents filled out questionnaires assessing parental ADHD, child behavioral problems, and parenting attitudes.
Scores were significantly higher for both internalizing disorders and externalizing disorders in study groups. We also found that ADHD symptoms were significantly higher among fathers of injured children compared with fathers of control groups. Democratic parenting was also found to correlate with higher numbers of injuries.
Parenting style, as well as the psychopathology of both the parents and children, is important factors in children's injuries. A child psychiatrist visit following an emergency procedure may help to prevent further unintentional injuries to the child.
INTRODUCTION
Unintentional injury in children is a growing global public health problem.1,2 It is estimated that tens of millions of children suffer from unintentional injuries and, unfortunately, around 1 million children die every year because of these injuries.2,3 Although death is the most dramatic result of injuries, it is not the most common one. Gallagher has shown that for each death, 45 children are hospitalized and 1300 children are admitted to emergency department (ED) because of injuries.4
Household environment has particular importance in unintentional injuries. The home is the leading location of injury for young children, accounting for nearly half of all childhood injuries.5,6 Preschoolers, who spend most of their time at home, are more prone to be exposed to home injuries compared with school age children.7,8
Caregivers have a key role in the occurrence and prevention of childhood injuries in the home. Research has shown that most injuries occur when children are in the care of a parent.9 It is also well known that parenting style which refers to the standard strategies parents use in raising their children has an impact on physical health of children.10 Although these studies suggest the possible role of quality and style of parenting, very little is known about the relationship between parenting style and unintentional injuries.11
Mental health status and psychiatric problems of both parents and children are also among the well-known risk factors for home injury.12,13 Attention deficit hyperactivity disorder (ADHD), characterized by overactivity, inattention, and impulsivity, is one of the most common childhood disorders.14 With respect to these characteristics, ADHD has the strongest relationship to injury risk among all childhood psychiatric disorders. Studies have shown that having ADHD nearly doubles the risk for injuries in childhood.13
ADHD is not only a childhood disorder, but over half of children with ADHD continue to have difficulties in adult life also.15 Childrearing is one of the areas in which individuals with ADHD have the most difficulty.16 They can be forgetful about important childrearing tasks, insensitive to the child's needs, and ineffective with respect to parental monitoring.16–18 Combining this data with genetic findings, which show that approximately 25% to 50% of children with ADHD have a parent with the disorder, it is highly expected that the presence of ADHD in the parents may also be a risk factor for home injuries in childhood.18 But the data on the role of parental ADHD in unintentional childhood injuries are lacking.
We hypothesized that parents of children who admit to ED for unintentional injuries may have significant ADHD symptoms or/and have a particular parenting style that might increase the risk of injuries. We also hypothesized that these children would have more psychiatric problems compared with their peers. Therefore, the aim of this study is to examine the relationship between unintentional home injuries and parental ADHD symptoms, parenting style, and children's behavioral problems.
MATERIALS AND METHODS
The study was conducted in the Erzurum Regional Training and Education Hospital in Turkey. Ethical clearance was obtained from the ethics committee of Ataturk University. All the parents were informed about the study, and the patients whose parents agreed to participate were also included in the study. The parents whose children were accepted into the study provided written informed consent. Patients, aged 1 to 5 years old, who were admitted to the ED because of unintentional home injury (March–June 2013) constitute the sample of the study group. We used the World Health Organization's (WHO) unintentional injury definition, and included children who were admitted with an injury which was accidentally occurred such as poisoning, burns and scalds, drowning, incision, falls, and transport-related injuries. Injuries that occurred because of interpersonal violence and self-harm were categorized as intentional injuries, and children who were referred for such injuries were excluded.19 Children who had a physical and sensory disability or a significant developmental delay that would make them more prone to injuries, which would therefore affect the interpretation of results, were not included in the study. Abbreviated Injury Scale (AIS) is coded on a scale of 1 to 6, where 1 being a minor injury and 6 being maximal. And we also excluded children whose AIS was ≥4 because asking parents to fill out questionnaires in such a situation would be ethically inappropriate and would decrease the reliability of the data.
We used individual matching method; therefore, the control group was recruited after the study groups were completed. The control group consisted of children admitted to the ED because of mild throat infections. In Turkey, EDs accept all kinds of admissions, and throat infections are among the most common reasons for admissions. One control case that was age and sex matched with a study group and did not have a history of unintentional home injury that required a hospital admission was included in the study.
Parents were requested to fill out the questionnaires before the child's discharge from the ED, after all the medical procedures were finished and the child was stabilized. In the case of only one form filled out in home by his/her parent, the others fill out in hospital, and then returned to our unit.
INSTRUMENTS
Sociodemographic Data Form
We used a sociodemographic data form specifically prepared for this study. The form has 4 parts. The first part consists of questions asking for classical demographic data such as age, sex, and economic status. The second part has questions about the current injury and previous injury history in detail. The time, place, type of injury, and the presence of parents or other people where the injury took place were also requested in this section. The third part consists of questions about the psychiatric history and previous psychiatric help-seeking efforts of the family. The four part consists of questions about the type and severity of the trauma.
AIS
The AIS is an anatomically based coding system for classifying the severity of specific individual injuries. It represents the relative threat to life associated with the injury rather than a comprehensive assessment of the severity of the injury. The assessments are based on type, location, and severity of injury. The severity is coded on a scale of 1 to 6 (1 = minor, 2 = moderate, 3 = serious, 4 = severe, 5 = critical, and 6 = maximal).
Parent Attitude Research Instrument
The Parent Attitude Research Instrument (PARI) is a 115-item (5 subscales of 23 items each), 4-point Likert scale developed to measure parental attitudes about childrearing in the context of family life. This scale was adapted to Turkish in a shortened form consisting of 5 subscales of 60 items each. The overparenting subscale reflects overcontrolling, anxious, and overdemanding parental attitudes. The democratic attitudes section measures permissiveness, encouragement given to children, and allowing them to express themselves in a supportive and sharing relationship. Attitude of hostility and rejection reflects the mother's negative attitudes and feelings of incompetence. The marital discordance subscale measures the effect of marital discord on the childrearing activities of the parents. The authoritarian attitude subscale measures overpunishing and rigid parental attitudes. Higher scores imply that the person agreed with the particular attitude being measured.20 In this study, mothers were asked to fill the PARI.
Child Behavior Checklist
The Child Behavior Checklist (CBCL 1.5/5) measures behavioral, emotional, and social problems in children 1.5 to 5 years of age.21 The instrument consists of 100 items in 7 syndrome scales, which are emotionally reactive, anxious/depressed, somatic complaints, withdrawn, sleep problems, attention problems, and aggressive behavior. In addition to these 7 syndrome scores, a total roblems score; an internalizing problems score, which is a combination of emotionally reactive, anxious/depressed, somatic complaints, and withdrawn scores; and an externalizing problems score, formed by combining attention problems and aggressive behaviors score, can also be obtained. Higher scores indicate more of that particular behavior problem.4 The CBCL 1.5/5 has previously been translated and validated in Turkish.22
Adult ADHD Self-Report Scale
The Adult ADHD Self-Report Scale (ASRS) is the WHO's self-report rating scale for adult ADHD.23 In the ASRS, 18 items are measured on a 5-point scale (0–4: never/seldom to often). Higher scores indicate higher frequencies of symptoms and symptom load. The scale is designed in 2 sections, each with its own score. The first 9 items (Part A) reflect symptoms of inattention, and items 10 to 18 (Part B) reflect impulsivity or hyperactivity. We used raw scores and the total score approach. In this method, adult ADHD mean score was found 23, so we used this value as a statistical cutoff, and individuals with scores of higher than 23 were deemed to be at risk of adult ADHD. We chose this cutoff for covering only individuals who are only ”highly likely to have ADHD.24 Both parents were asked to fill out the ASRS.
Statistical Analyses
The data were analyzed using SPSS version 20.0 for Windows. A χ2 test and Mann–Whitney U test were used to compare the psychosocial variables of the study and control groups. The Mann–Whitney U test was used to compare PARI and CBCL (1–5 years) scores, and χ2 test was used to compare the ASRS scores of the 2 groups We used Pearson correlation analysis to identify the correlations between injury-related factors, and the PARI, ASRS, and CBCL scores of the study group. Those P values <0.05 were accepted as significant.
RESULTS
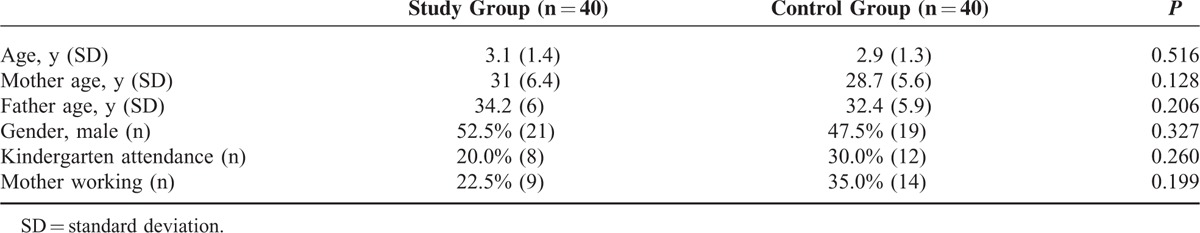
A total of 50 children met our inclusion criteria during our timeline, but 40 cases were included in the study. Forty-three (86%) of the parents agreed to participate in the study. In 3 ED admissions, only 1 parent was with the child. None of them returned the forms, and they were excluded from the study. The mean age was 3.1 (±1.4) years for the study group and 2.9 (±1.3) years for the control groups. In the study group, 52.5% (n = 21) were boys. The sociodemographic data of the participants are shown in Table 1.
TABLE 1.
The Sociodemographic Data of the Participants
45.2% of patients had fallen and 40% of patients had incision. In addition, 50% of patients were treated with simple medical treatment, and surgical treatment was 10%. The 4% of patients had life-threatening. In most injuries, only the mother (59%, n = 23) was at home. Only the father was at home for 2.6% (n = 1) of injuries, whereas both of the parents were at home for 23.1% (n = 9) of injuries. With regard to time of day, 33.3% of incidents occurred in the morning, 38.5% in the evening, and 28.2% occurred at night. Most of the injuries happened while the child was not alone in the room; either mother (66.7%, n = 14), father (4.8%, n = 1), both parents (23.8%, n = 5), or another adult (4.8%, n = 1) was in the room where the incident happened.
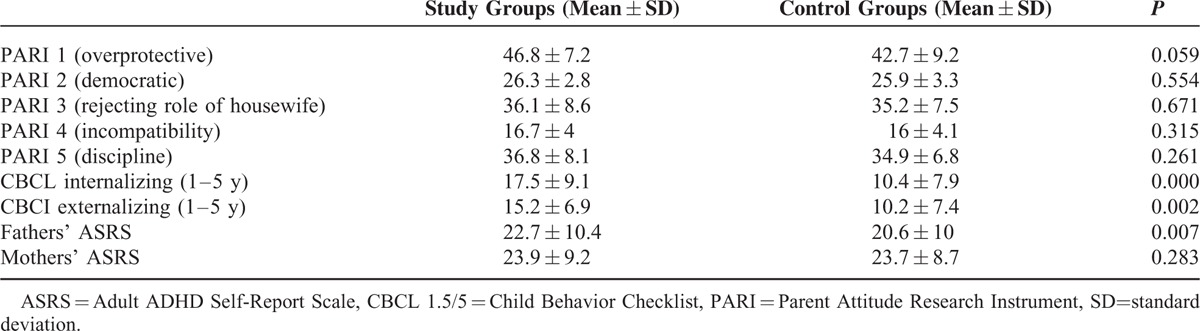
Twenty-three fathers and 23 mothers have ASRS higher scores in our study group. We found that ADHD risk of fathers was significantly higher in children admitted because of home injury compared with the control groups (P = 0.007). Having a father with high ADHD risk caused approximately a 2-fold increase in the relative risk of children to be exposed to home injuries (odds ratio = 2.88). In addition, having a father with high ADHD risk (P = 0.005) was associated with an increase in the internalizing disorder scores in children. Fathers’ ADHD scores also had a relationship with which body regions were injured. Head injuries were significantly correlated with higher ADHD scores (P = 0.036) in fathers. There was no relationship between the child's injury risk and the presence of the father with ADHD risk in the home at the time of the accident. We could not find a significant difference between maternal ADHD risk in the study and control groups (P = 0.283).
The results revealed that both the internalizing (P:0.000) and externalizing (P:0.002) disorder scores of children were higher among study groups than in the control groups and these were statistically significant.
Democratic parenting scores of mothers, which reflect more permissiveness and relatively less control over children, were positively correlated with the number of total injuries experienced by children (P = 0.007, r = 0.461). Table 2 shows the analysis of comparison of PARI, CBCL, and ASRS scores for the study and control groups.
TABLE 2.
Analysis of Comparison of PARI, CBCL, and ASRS Scores of Study and Control Groups
DISCUSSION
The basic characteristics of home injuries in our study were consistent with the literature. Most of the injuries occurred in the morning or in the evening; most of the victims were boys and there was an adult—usually a parent—in the room, in parallel with the injuries described in previous studies.1,11
One of the main findings of this study was the link between home injury in children and the ADHD symptomatology of their fathers. Parental mental distress is well known to affect the injury risk for children, and this finding was consistent with the previous research showing this relationship.12 Maternal depression and anxiety have been shown to predict increased injury risk among young children.25,26 However, most of the previous research that focused on the role of the mothers’ psychopathology and the role of the fathers’ psychopathology in the occurrence and prevention of childhood injuries is unclear.27 In fact, there is evidence that the father's psychopathology has a relationship with children's adjustment problems in general.28 In addition, it was shown that fathers have a protective role in toddlers’ safety similar to that of mothers.27 But, to the best of our knowledge, there is a lack of data showing the link between a father's ADHD and his children's injury risk, and this is the first study reporting a relationship between fathers’ ADHD symptoms and risk of injury to their children.
Owing to the lack of evidence from previous research on this topic, it is unclear how fathers’ ADHD is linked to children's risk of injury, but the other results of this study may help us understand the extent of the relationship. We found that in most cases the fathers were not at home when the injury occurred, and there was not a relationship between injury risk and the presence of the father with high ADHD symptoms at home. On the contrary, consistent with previous research that shows that parental ADHD is related with childhood psychopathology, internalization disorder scores were found to be higher in injured children with a father with high ADHD risk compared with children with fathers whose ADHD symptoms were in the normal range.29 Although the relationship between internalization disorders and injury risk is unclear, some symptoms seen in internalization disorders, such as nervousness, impaired communication, which may decrease help-seeking behaviors, and inattention, might make children more prone to injuries.30 These findings suggest that the effect of fathers’ ADHD on children's injury risk is not necessarily related to the fathers’ direct role in the incident; indirect effects, such as an impaired mental state in the child, may also lead to injuries. Another explanation may be found in the fathers’ role modeling in the family. Fathers are important role models for preschoolers, in particular for boys.31 Studies have shown that fathers and mothers communicate with preschoolers in different ways during their time together.32,33 These differences may have implications for children's risk for injury.12 Fathers play with their toddlers more physically and may interact in more dangerous ways, which allows children to experience some risks at home under supervision.12 But fathers with ADHD, who were shown to have problems recognizing injury risk, who cannot enforce safety rules, and who are more permissive toward their children, may not be able to provide the necessary supervision for preventing possible injuries. Moreover, they may be behaving as models for risk-taking behaviors.17,34 The finding that children whose fathers have ADHD symptoms were more prone to head injuries, which generally occur because of more dangerous actions, compared with extremity injuries also supports this hypothesis and is consistent with previous research.35
Our finding showing the relationship between psychiatric problems and home injuries corroborate the findings of a great deal of the previous work in this field.36–38 Jokela et al38 have shown that 1 standard deviation increase in externalizing score was associated with 10% to 19% increase in the rate of injuries in childhood, adolescence, and adulthood.39 A number of factors may be contributing this link such as working memory, behavioral inhibition, impulsivity, and attention problems which are more common in children with externalizing disorders.40 However, it was somewhat surprising that the number of home injuries increase in the context of democratic parenting attitudes of mothers. Democratic parenting generally refers to positive parenting attitudes, and has been shown to have many benefits in children's mental development.41 But injury risk seems to be an exception. Morrongiello et al11 found that both moderately and highly permissive parents use teaching techniques that elevate young children's risk of medically attended injury. Our results match this observation, and support the idea that permissive parenting may be a risk factor for injuries to children.
CONCLUSION
Notwithstanding some limitations, the current findings from this study add substantially to our understanding of unintentional home injuries to children. To the best of our knowledge, this study was the first to show the role of father's ADHD symptoms in unintentional injuries to children. It is suggested that the association of parental ADHD and unintentional home injuries to children is investigated in future studies. These studies may be particularly important for injury prevention programs. The present study confirms previous findings, and contributes additional evidence to suggest that child psychopathology may play a role in childhood injuries. A child psychiatry consultation should be considered for children with repeated injuries or head injuries. The study also has implications for parenting style. Although being permissive and allowing room for curiosity and exploration are essential for toddlers’ mental development, it is important to establish rules that provide for the child's safety.
LIMITATIONS
The results of this study are subject to certain limitations. For instance, the sample size was relatively small, and caution must be applied while interpreting the results. Another limitation was that we used only 1 informant for parenting attitudes. Although mothers are the only resource of information in most of the studies in child injury literature, gathering information from fathers could give additional information. Although we used the highest cutoff to enhance specificity, we could not use further diagnostic assessments and structured interviews for diagnosing psychiatric disorders among children and parents. There were 2 main reasons for this choice. It was impossible for us to apply further diagnostic instruments in emergency services. Our second alternative was to call the families following the incident and ask for a detailed interview that would last nearly 2 hours. This would be after they had already been subjected to a police interview in ED. We considered that this would be anxiety-provoking, and could be seen as blaming the parents, which would affect the reliability of the reports. Because of the same time limit issues and the Turkish parents’ common childrearing practices which gives the major role for preschooler children to mothers, we obtained the parenting data only from mothers.
Footnotes
Abbreviations: ADHD = attention deficit hyperactivity disorder, AIS = Abbreviated Injury Scale, ASRS = Adult ADHD Self-Report Scale, CBCL 1.5/5 = Child Behavior Checklist, ED = emergency department, PARI = Parent Attitude Research Instrument.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Hyder AA, Sugerman DE, Puvanachandra P, et al. Global childhood unintentional injury surveillance in four cities in developing countries: a pilot study. Bull World Health Organ 2009; 87:345–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peden M. World Report on Child Injury Prevention. Geneva: World Health Organization & United Nations Children's Fund; 2008. [PubMed] [Google Scholar]
- 3.Mathers C, Fat DM, Boerma J. The Global Burden of Disease: World Health Organization. The World Health Report 2004. Geneva: WHO; 2004. [Google Scholar]
- 4.Gallagher SS, Finison K, Guyer B, et al. The incidence of injuries among 87,000 Massachusetts children and adolescents: results of the 1980-81 Statewide Childhood Injury Prevention Program Surveillance System. Am J Public Health 1984; 74:1340–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phelan KJ, Khoury J, Xu Y, et al. A randomized controlled trial of home injury hazard reduction: the HOME injury study. Arch Pediatr Adolesc Med 2011; 65:339–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dershewitz RA, Williamson JW. Prevention of childhood household injuries: a controlled clinical trial. Am J Public Health 1977; 67:1148–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gulliver P, Dow N, Simpson J. The epidemiology of home injuries to children under five years in New Zealand. Aust N Z J Public Health 2005; 29:29–34. [DOI] [PubMed] [Google Scholar]
- 8.Linnan M. Child mortality and injury in Asia: survey results and evidence. Florence, UNICEF Innocenti Researsh Centre, 2007. (http://www.unicef-irc.org/publications/pdf/iwp_2007_06.pdf. accessed 21 January 2008). Innocenti Working Paper 2007-06, Special Series on Child Injury No.3). [Google Scholar]
- 9.Saluja G, Brenner R, Morrongiello BA, Cheng TL. The role of supervision in child injury risk: definition, conceptual and measurement issues. Inj Control Saf Promot 2004; 11:17–22. [DOI] [PubMed] [Google Scholar]
- 10.Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull 2002; 128:330–366. [PubMed] [Google Scholar]
- 11.Morrongiello BA, Corbett M, McCourt M, et al. Understanding unintentional injury risk in young children II. The contribution of caregiver supervision, child attributes, and parent attributes. J Pediatr Psychol 2006; 31:540–551. [DOI] [PubMed] [Google Scholar]
- 12.Schwebel DC, Roth DL, Elliott MN, et al. The association of activity level, parent mental distress, and parental involvement and monitoring with unintentional injury risk in fifth graders. Accid Anal Prev 2011; 43:848–852. [DOI] [PubMed] [Google Scholar]
- 13.Lange H, Buse J, Bender S, et al. Accident proneness in children and adolescents affected by ADHD and the impact of medication. J Atten Disord 2014; 27:1–9.doi: 10.1177/1087054713518237. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Cautionary statement for forensicuse of DSM-5. Diagnostic and Statistical Manual of Mental Disorders 5th ed.2013; doi:10.1176/appi.books.9780890425596.744053. [Google Scholar]
- 15.Weiss M, Hechtman LT, Weiss G. ADHD in Adulthood: A Guide to Current Theory, Diagnosis, and Treatment. Baltimore: Johns Hopkins University Press; 1999. [Google Scholar]
- 16.Eakin L, Minde K, Hechtman L, et al. The marital and family functioning of adults with ADHD and their spouses. J Atten Disord 2004; 8:1–10. [DOI] [PubMed] [Google Scholar]
- 17.Johnston C, Mash EJ, Miller N, et al. Parenting in adults with attention-deficit/hyperactivity disorder (ADHD). Clin Psychol Rev 2012; 32:215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans SW, Vallano G, Pelham W. Treatment of parenting behavior with a psychostimulant: a case study of an adult with attention-deficit hyperactivity disorder. J Child Adolesc Psychopharmacol 1994; 4:63–69. [Google Scholar]
- 19.Unıntentıonal Chıldhood Injurıes. Children's Health and the Environment. WHO Training Package for the Health Sector. World Health Organization. 2015. http://slideplayer.com/slide/4907196/ (accessed: 30 July, 2015). [Google Scholar]
- 20.Le Compte WA, Oner N. Development of the Turkish edition of the State-trait anxiety inventory. Cross-Cultural Anxiety 1976; 1:51–67. [Google Scholar]
- 21.Achenbach TM, Rescorla L. ASEBA Preschool Forms & Profiles: An Integrated System of Multi-informant Assessment: Aseba (2000). [Google Scholar]
- 22.Erol N, Şimsek Z. Mental health profile of Turkey: distribution of competence and behavioral problems. Mental health profile of Turkey: preliminary report Aydoğdu Ofset, Ankara: 1997: 12-33. [Google Scholar]
- 23.Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med 2005; 35:245–256. [DOI] [PubMed] [Google Scholar]
- 24.Schwebel DC, Brezausek CM. Chronic maternal depression and children's injury risk. J Pediatr Psychol 2008; 33:1108–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradbury K, Janicke DM, Riley AW, et al. Predictors of unintentional injuries to school-age children seen in pediatric primary care. J Pediatr Psychol 1999; 24:423–433. [DOI] [PubMed] [Google Scholar]
- 26.Morrongiello BA, Walpole B, McArthur BA. Brief report: young children's risk of unintentional injury: a comparison of mothers’ and fathers’ supervision beliefs and reported practices. J Pediatr Psychol 2009; 34:1063–1068. [DOI] [PubMed] [Google Scholar]
- 27.Kane P, Garber J. Parental depression and child externalizing and internalizing symptoms: unique effects of fathers’ symptoms and perceived conflict as a mediator. J Child Fam Stud 2009; 18:465–472. [Google Scholar]
- 28.Humphreys KL, Mehta N, Lee SS. Association of parental ADHD and depression with externalizing and internalizing dimensions of child psychopathology. J Atten Disord 2012; 16:267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crijnen AA, Achenbach TM, Verhulst FC. Comparisons of problems reported by parents of children in 12 cultures: total problems, externalizing, and internalizing. J Am Acad Child Adolesc Psychiatry 1997; 36:1269–1277. [DOI] [PubMed] [Google Scholar]
- 30.Jia R, Schoppe-Sullivan SJ. Relations between coparenting and father involvement in families with preschool-age children. Dev Psychol 2011; 47:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McBride BA, Mills G. A comparison of mother and father involvement with their preschool age children. Early Child Res Q 1993; 8:457–477. [Google Scholar]
- 32.Lamb ME. The role of the father in child development: John Wiley & Sons. (2004) [Google Scholar]
- 33.Garzon DL. Contributing factors to preschool unintentional injury. J Pediatr Nurs 2005; 20:441–447. [DOI] [PubMed] [Google Scholar]
- 34.DiScala C, Lescohier I, Barthel M, et al. Injuries to children with attention deficit hyperactivity disorder. Pediatrics 1998; 102:1415–1421. [DOI] [PubMed] [Google Scholar]
- 35.Rowe R, Maughan B, Goodman R. Childhood psychiatric disorder and unintentional injury: findings from a national cohort study. J Pediatr Psychol 2004; 29:119–130. [DOI] [PubMed] [Google Scholar]
- 36.Glania T, Lialiaris T, Tripsianis G, et al. Is psychopathology related to children's unintentional injury? Int J Adolesc Med Health 2010; 22:567–574. [DOI] [PubMed] [Google Scholar]
- 37.Schwebel DC, Roth DL, Elliott MN, et al. Association of externalizing behavior disorder symptoms and injury among fifth graders. Acad Pediatr 2011; 11:427–431. [DOI] [PubMed] [Google Scholar]
- 38.Jokela M, Power C, Kivimaki M. Childhood problem behaviors and injury risk over the life course. J Child Psychol Psychiatry 2009; 50:1541–1549. [DOI] [PubMed] [Google Scholar]
- 39.Stevens J, Quittner AL, Zuckerman JB, et al. Behavioral inhibition, self-regulation of motivation, and working memory in children with attention deficit hyperactivity disorder. Dev Neuropsychol 2002; 21:117–139. [DOI] [PubMed] [Google Scholar]
- 40.Darling N, Steinberg L. Parenting style as context: an integrative model. Psychol Bull 1993; 113:487. [Google Scholar]
- 41.Oryan S, Gastil J. Democratic parenting: paradoxical messages in democratic parent education theories. Int Rev Educ 2013; 59:113–129. [Google Scholar]


