Abstract
Esophageal perforation is a rare condition that is commonly missed. Male gender and alcohol use are predisposing risk factors. Most of the cases are iatrogenic or traumatic; nonetheless, spontaneous cases are not uncommon. It typically occurs after vomiting or straining as the increased intra-abdominal pressure transmits into the esophagus and results in the tear. One of the main complications is acute bacterial mediastinitis from contamination with esophageal flora. This condition can be life-threatening because it is very frequently misdiagnosed and appropriate management is often delayed.
A 49-year-old man presented with worsening sudden-onset interscapular back pain that then changed to chest pain with odynophagia and was found to have fever and leukocytosis.
Chest computed tomography revealed signs of mediastinitis with possible esophageal perforation. He reported symptoms started 2 days ago after lifting of heavy objects. Empiric antimicrobial was begun with conservative management and avoidance of oral intake. Barium esophagram and esophagogastroduodenoscopy revealed no signs of perforation or inflammation. His symptoms resolved and he gradually resumed oral intake. Blood cultures grew Methicillin-sensitive Staphylococcus aureus and he was discharged on appropriate antibiotics for 4 weeks. He did well on follow-up 3 months after hospitalization.
The case highlights the importance of considering esophageal etiologies of chest pain.
CASE REPORT
A 49-year-old man presented to our Emergency Department complaining of chest pain. It began 2 days prior to presentation while lifting heavy objects at home and was described as interscapular upper back stiffness then became midsternal and inspirational. The following day, he started to feel fatigued with fevers, anorexia, odynophagia, and nausea but denied vomiting. His medical history included hypertension and he had no surgical history. He had recent prolonged traveling. He used to drink socially but denied smoking. Vitals were stable with temperature of 38.4 °C, heart rate of 93 bpm, blood pressure 129/81 mmHg, and respiratory rate of 18 breaths/min. Physical examination was normal. Laboratory workup revealed leukocytosis of 14,640/μL with a predominance of neutrophils (82.4%). Electrocardiogram, chest radiograph, and serum Troponin T were normal. Given the history of traveling and pleuritic feature of chest pain, computed tomographic (CT) angiography was ordered. It ruled out pulmonary embolism; however, it showed mediastinal soft-tissue infiltration and stranding of the upper paraesophageal posterior mediastinal fat (Figure 1). These findings were concerning for mediastinitis due to possible esophageal perforation. Blood cultures were obtained then empiric broad-spectrum antimicrobial therapy with intravenous Vancomycin and Piperacillin/Tazobactam was initiated. Although barium esophagram did not show any signs of perforation (Figure 2), patient was instructed to avoid all oral intake during hospitalization. Because he was hemodynamically stable, conservative management was sought. Esophagogastroduodenoscopy was delayed for a few days in order to minimize risk of further esophageal perforation. Interestingly, it later did not show any signs of inflammation of the esophageal mucosa and only mild corporal gastritis, although biopsy did not show Helicobacter pylori. It was believed that the perforation had already healed spontaneously.
FIGURE 1.
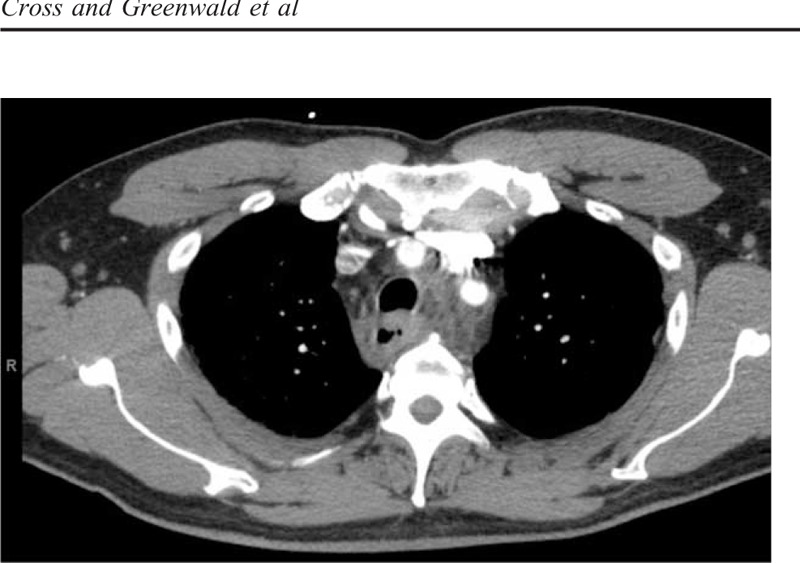
Computed tomographic angiography in the Emergency Department shows mediastinal soft-tissue infiltration and stranding of the upper paraesophageal posterior mediastinal fat. No mediastinal gas is detected.
FIGURE 2.
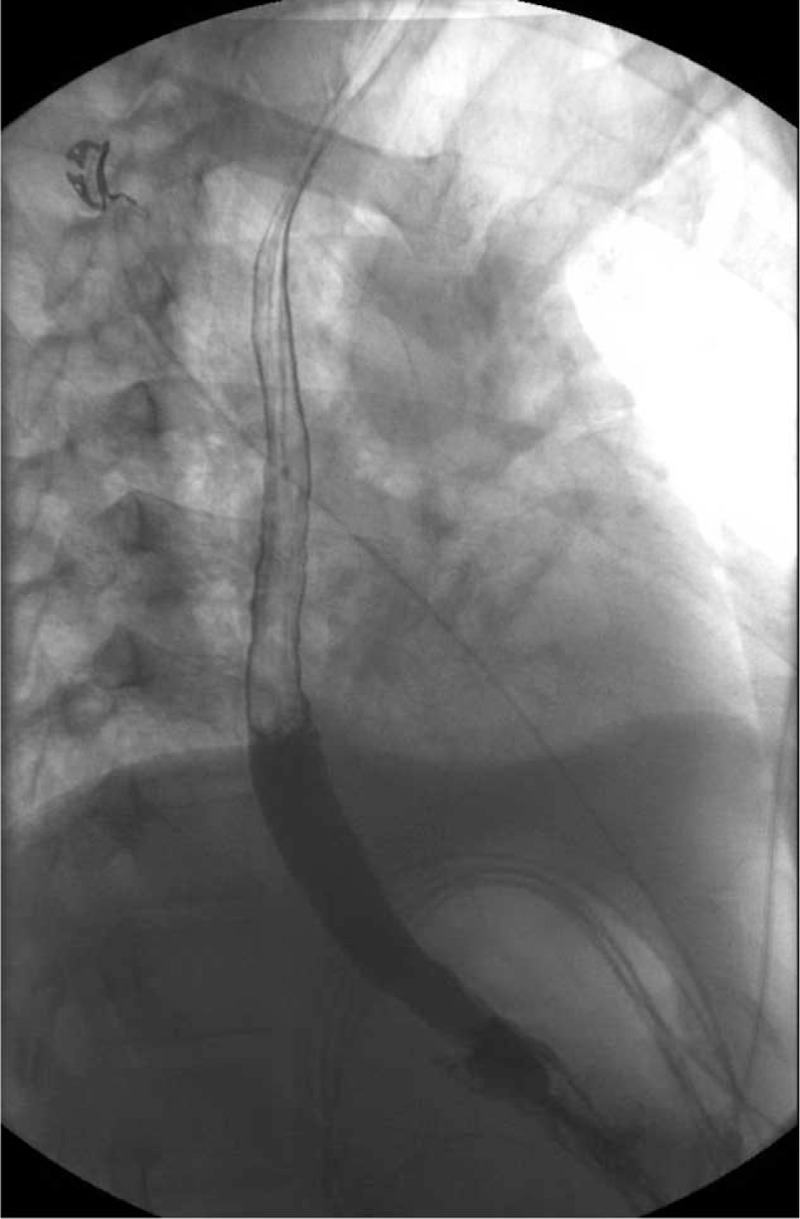
Esophagram obtained on 2nd day of hospitalization showed no signs of esophageal perforation.
The blood cultures grew Methicillin-sensitive Staphylococcus aureus, therefore Vancomycin was discontinued and Piperacillin/Tazobactam was switched to intravenous Naficillin. Oral Metronidazole was started as well to provide coverage for anaerobes. Over the 6-day course of hospitalization, the fevers and leukocytosis resolved, the chest pain improved significantly, and repeat blood cultures were negative. Oral feeding was introduced and advanced gradually without complications. He was discharged on the same antibiotics for 4 weeks. He continued to do well on follow-up 3 months after hospitalization.
DISCUSSION
There are multiple causes of “chest pain” and it is always crucial to carefully evaluate the history of present illness, review of systems, and comorbidities then perform a thorough physical examination. Subsequently, clinicians can make their lists of possible diagnoses and start the appropriate workup and management. Undoubtedly, cardiac and pulmonary etiologies should always be considered and evaluated, especially in the presence of risk factors. These include acute coronary syndromes, aortic dissection, pulmonary embolism, pneumothorax, etc.
The pain in our case started initially in the interscapular upper back area, thus aortic dissection should be among the differential diagnosis. One should note that normal chest radiographs and absence of difference in blood pressure between the upper extremities do not necessarily rule it out, thus high suspicion is required. However, the development of anorexia and fevers in our patient made this diagnosis less likely. Alternatively, pneumonia could have been a possible diagnosis and can sometimes result in pleuretic chest pain. Other general causes of pleuretic or inspirational chest pain include pulmonary embolism, acute pericarditis, and costochondritis. However, the presentation, history, and workup were not consistent with many of those diagnoses.
Clinicians should remember the other structures in the chest – if it is a part of the chest, it can be the cause of “chest pain.” Other important causes of chest pain that are commonly missed are those of an esophageal origin, such as esophageal spasm and esophageal perforation.
Esophageal perforation is a rare condition where a full-thickness tear of the esophageal wall occurs. Male gender and alcohol use are predisposing risk factors. Most of the cases are iatrogenic or traumatic; nonetheless, spontaneous cases are not uncommon. It typically occurs after vomiting or straining as the increased intra-abdominal pressure transmits into the esophagus and results in the tear. One of the main complications is acute bacterial mediastinitis from contamination with esophageal flora. This condition can result in life-threatening sepsis if diagnosis is missed and antimicrobial therapy is delayed.
ESOPHAGEAL PERFORATION
Esophageal perforation is a rare condition (3.1 per 1,000,000 per year) that is commonly misdiagnosed and can be fatal if not promptly treated.1 Iatrogenic causes, usually due to paraesophageal surgery or esophagoscopy, make up to 59% of cases.2 The next leading cause is spontaneous rupture (15%) followed by foreign body ingestion (12%).2 Other less common etiologies include trauma and malignancy (approximately 10%).2
Boerhaave syndrome or effort rupture is the most common type of spontaneous esophageal perforation. It is usually the result of a sudden increase the intraesophageal pressure while the intrathoracic pressure is negative. These conditions occur during vomiting, straining, coughing, seizing, and weightlifting. The sudden increase in intra-abdominal pressure transmits into the esophagus and results in full-thickness tear of the esophageal wall. This perforation usually involves the left posterolateral aspect of the distal intrathoracic esophagus; however, it can occur in the cervical or intra-abdominal esophagus as well.
This syndrome is most frequently seen in patients aged 50 to 70 years (almost 80% of patients) and is 5 times more common in men than women.3 Alcoholism or heavy drinking is present in 40% of cases which may explain the age and male predominance.4 Risk factors include malignancy, drug- and alcohol-induced esophagitis, and Barrett ulcers which commonly compromise the integrity of the mucosal wall. Nonetheless, perforation can occur in a normal esophagus as well.
COMPLICATIONS
Perforation of the esophagus causes gastric contents and normal flora of the esophagus to leak into the mediastinal space, which can result in inflammation and even infection. Complications of such infection can lead to sepsis and organ failure with a mortality rate approaching 100% if diagnosis is missed and left untreated.5
MEDIASTINITIS
Mediastinitis is typically caused by infection of the organs and tissues in the mediastinal space. Infection can occur through direct contamination, hematogenous, or lymphatic spread or extension of infection from the head, neck, lung, pleura, chest wall, or peritoneum.6 The most common cause of acute mediastinitis is iatrogenic etiologies as a consequence of esophageal and cardiac surgery, tracheal intubation, and endoscopic procedures.7,8 Occasionally, acute mediastinitis is caused by esophageal perforation or rupture of the tracheobronchial tree.9 With the esophageal perforation, its bacterial flora can directly contaminate the mediastinum and result in infection. Acute mediastinitis has been reported to occur in 1% of patients with esophageal perforation.8 The severity is variable and can range from mild pleuritis or pericarditis to fulminant infection.
MICROBIOLOGY
In general, acute mediastinitis is usually caused by anaerobic (41%) or mixed aerobic–anaerobic bacterial flora (41%); however, aerobic or facultative bacteria are not uncommon (18%).10 The most common anaerobes are Prevotella, Porphyromonas, and Peptostreptococcus species then Bacteroides fragilis group. On the other hand, the most common aerobes are α-hemolytic Streptococcus, S. aureus, and Klebsiella pneumoniae.10
In the cases of acute mediastinitis secondary to esophageal perforation, anaerobes are more frequently cultured.10 They are mostly viridans Streptococcus and fusiform rods which are parts of the esophageal flora.11 The normal flora of the esophagus varies considerably between individuals. It has a close relationship to the oral flora with a slightly higher prevalence of lactobacilli and enteric rods in distal esophagus which may be due to the influence of gastric acidity.11 Therefore, the location of esophageal perforation can determine the microbiology resulting in the mediastinitis. In our case, the proximal location of the esophageal perforation explains the contamination with S. aureus which is present in the esophageal flora in 13% of subjects.
CLINICAL PRESENTATION
The most common presenting symptom is chest pain (85% of cases).12 The pain can in the interscapular upper back area given the proximity of the esophagus to the spine. Regardless, pain can vary depending on the location of perforation and is classically preceded by vomiting or eating. It is usually pleuritic in nature and may be differentiated from angina by inquiring about alleviating and exacerbating factors. Patients may also present with odynophagia, dyspnea, tachypnea, cyanosis, tachycardia, fever, and hypotension which may develop within hours of the perforation. On physical examination, crepitus due to subcutaneous emphysema may be felt with palpation of the chest wall. Additionally, mediastinal crackling may be heard with the heart beat in a subset of patients.12
DIAGNOSIS
Diagnosis of esophageal perforation or mediastinitis can be difficult because of the nonspecific symptoms. Fevers with tachycardia and elevation of inflammatory markers usually indicate an infectious etiology that should be worked up.
Contrast esophagography can reveal the location and size of the perforation but sensitivity is highly variable with a false-negative rate of 10%.5 Barium contrast is most successful at confirming small perforations with a sensitivity of 90%. Unfortunately, it can cause an inflammatory response in the mediastinum, pleura, or pericardium; therefore, it should be avoided if perforation is suspected. Alternatively, a water-soluble contrast agent, such as Gastrografin, is safe and preferred for initial studies though it has lower sensitivity (50%–75%).13 Flexible esophagoscopy is more sensitive but it is invasive and carries the risk of further perforation, thus it should be avoided in the setting of acute perforation.
Conventional chest radiography may show widening of the upper mediastinum and loss of the normal contours.9,14 However, it is usually not diagnostic in most cases because of the nonspecific signs.14 CT scans have become very useful in the diagnosis of esophageal perforation missed on esophagography.8 Furthermore, their sensitivity and specificity in detecting mediastinitis secondary to esophageal perforation can reach 100%, even in early clinical presentation.15 They can detect esophageal thickening or extraluminal gas or contrast medium which indicates esophageal perforation.8 Additionally, increased attenuation of mediastinal fat, localized mediastinal fluid collections, pericardial or pleural effusions, and mediastial lymphadenopathy are other signs that support the diagnosis of mediastinitis.15 Due to their high sensitivity and specificity, CT scans are important imaging modalities that can facilitate early diagnosis of esophageal rupture and its complications and even help guide management.
MANAGEMENT
Initial management of esophageal perforation should include avoidance of oral intake accompanied by nutritional support. Intravenous proton pump inhibitor should be administered to decrease the chemical inflammation secondary to gastric content. After obtaining blood cultures, intravenous antimicrobial therapy should be promptly initiated. It should be broad-spectrum to provide empiric coverage for the possible-mixed aerobic–anaerobic bacterial infection caused by the esophageal flora.2 Drainage of fluid collections should be considered if present and surgical intervention may be needed depending on the size and location of the perforation and the condition of the patient. Therefore, consultation with cardiothoracic surgeons is recommended.6,7 Monitoring for resolution of fevers, leukocytosis, bacteremia, and presenting symptoms can help guide management and determine duration of antimicrobial therapy. If specific pathogens are isolated from blood cultures or drainage from mediastinal fluid collection, the antimicrobial therapy can be later modified and narrowed to target them.
LESSONS LEARNED
Detailed and thorough history, review of systems, and physical examination are always important in order to establish diagnosis.
Without ignoring possible cardiac or pulmonary etiologies, it is important to remember that any structure in the chest can result in “chest pain.”
Esophageal etiologies of chest pain are commonly ignored. Those include esophageal perforation which can result in acute bacterial mediastinitis and thus be life-threatening if missed. High suspicion is required.
CT imaging is very useful in diagnosis and guiding management.
Management includes abstaining from oral intake, intravenous antimicrobial and proton pump inhibitor therapies, and, if indicated, surgical management.
DISCLOSURE
No patient consent was needed because no information that can identify patients is shared.
Footnotes
MRC and MFG are equal contributors to this work.
REFERENCES
- 1.Vidarsdottir H, Blondal S, Alfredsson H, et al. Oesophageal perforations in Iceland: a whole population study on incidence, aetiology and surgical outcome. Thorac Cardiovasc Surg 2010; 58:476–480. [DOI] [PubMed] [Google Scholar]
- 2.Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004; 77:1475–1483. [DOI] [PubMed] [Google Scholar]
- 3.Clément R1, Bresson C, Rodat O. Spontaneous oesophageal perforation. J Clin Forensic Med 2006; 13:353–355. [DOI] [PubMed] [Google Scholar]
- 4.Brauer RB, Liebermann-Meffert D, Stein HJ, et al. Boerhaave's syndrome: analysis of the literature and report of 18 new cases. Dis Esophagus 1997; 10:64–68. [DOI] [PubMed] [Google Scholar]
- 5.Bladergroen MR, Lowe JE, Postlethwait RW. Diagnosis and recommended management of esophageal perforation and rupture. Ann Thorac Surg 1986; 42:235. [DOI] [PubMed] [Google Scholar]
- 6.Athanassiadi KA. Infections of the mediastinum. Thorac Surg Clin 2009; 19:37–45. [DOI] [PubMed] [Google Scholar]
- 7.Jabłoński S, Brocki M, Kordiak J, et al. Acute mediastinitis: evaluation of clinical risk factors for death in surgically treated patients. ANZ J Surg 2013; 83:657–663. [DOI] [PubMed] [Google Scholar]
- 8.White CS, Templeton PA, Attar S. Esophageal perforation: CT findings. AJR Am J Roentgenol 1993; 160:767–770. [DOI] [PubMed] [Google Scholar]
- 9.Giménez A, Franquet T, Erasmus JJ, et al. Thoracic complications of esophageal disorders. Radiographics 2002; 22:S247–S258. [DOI] [PubMed] [Google Scholar]
- 10.Brook I, Frazier EH. Microbiology of mediastinitis. Arch Intern Med 1996; 156:333–336. [PubMed] [Google Scholar]
- 11.NorderGrusell E1, Dahlén G, Ruth M, et al. Bacterial flora of the human oral cavity, and the upper and lower esophagus. Dis Esophagus 2013; 26:84–90. [DOI] [PubMed] [Google Scholar]
- 12.Callaghan J. The Boerhaave syndrome (spontaneous rupture of the oesophagus). Br J Surg 1972; 59:41–44. [DOI] [PubMed] [Google Scholar]
- 13.Buecker A, Wein BB, Neuerburg JM, et al. Esophageal perforation: comparison of use of aqueous and barium-containing contrast media. Radiology 1997; 202:683–686. [DOI] [PubMed] [Google Scholar]
- 14.Blencowe NS, Strong S, Hollowood AD. Spontaneous oesophageal rupture. BMJ 2013; 346:f3095. [DOI] [PubMed] [Google Scholar]
- 15.Exarhos DN, Malagari K, Tsatalou EG, et al. Acute mediastinitis: spectrum of computed tomography findings. Eur Radiol 2005; 15:1569–1574. [DOI] [PubMed] [Google Scholar]


