Abstract
Double-lumen catheters have been used widely to obtain temporary access in patients who are in need of acute hemodialysis (HD) because of acute renal failure. Several complications are associated with the insertion of these catheters, including bleeding, infection, injuries to arteries, and deep venous thrombosis. An arteriovenous fistula (AVF) is a rare but significant complication following catheterization for temporary HD. Herein, we present a case of AVF associated with leg swelling 6 months after the removal of
a double-lumen HD catheter.
We describe a special case of a 42-year-old man who experienced acute renal failure secondary to diabetic ketoacidosis (DKA). A 12-Fr dialysis catheter was inserted in the right femoral vein. Six months after catheter removal, the patient was admitted
for pain and swelling in the right leg. Color Doppler ultrasound and three-dimensional computed tomography (CT) revealed an AVF between the right femoral vein and the right femoral superficial artery. The fistula was repaired successfully by vascular surgeons.
This case highlights that an AVF is a rare but significant complication after catheterization for temporary HD. The nephrologist should be wary of the potential of this complication and perform clinical and medical examinations at the insertion and removal of temporary HD catheters.
INTRODUCTION
Adequate vascular access is of critical importance for patients who require extracorporeal renal replacement therapy. Although an arteriovenous fistula (AVF) is the golden standard access for hemodialysis, temporary dialysis catheters are frequently required. The National Kidney Foundation Kidney Disease Outcomes Quality Initiative (K/DOQI) suggests that catheter access is usually achieved through cannulation of 1 of the 3 easily accessible central veins, namely the femoral, internal jugular, or subclavian veins.1 The internal jugular veins are preferable locations for insertion. However, the femoral vein is often selected as well, depending on the patient's condition.2 Several complications are associated with the insertion of these catheters, including infection, bleeding, deep venous thrombosis, and injuries to arteries. Thrombosis and infections are the common complications during catheter insertion as well as in the already inserted catheters.3 An AVF is a rare but severe complication following catheterization for patients who require hemodialysis. We describe a case of an iatrogenic AVF after cannulation of the femoral vein for temporary HD leading to leg swelling 6 months after removal of a hemodialysis catheter.
CASE PRESENTATION
A 42-year-old Asian man with a history of diabetic ketoacidosis and acute renal failure (ARF) was first admitted to a satellite hospital 6 months ago. The nephrologist examined the patient and thought he was in need of emergent hemodialysis. Emergency hemodialysis was scheduled. A temporary double-lumen HD catheter was smoothly inserted into the right femoral vein. Ultrasound had not yet been used for catheter insertion. Blood samples were collected through the catheter to confirm its venous origin, and HD was performed through the catheter. The same catheter was subsequently used for 3 sessions of HD. Bleeding from the catheter insertion site was observed 5 days after admission, when he walked to the restroom. At that time, the platelet count was normal and international normalized ratio (INR) was 2.45. No angiography was performed because bleeding was presumably caused by catheter movement. Six days later, the serum creatinine level become normal and urine volume was much more than 1500 ml/day after the comprehensive treatment. The catheter was removed to stop the continuous bleeding; as a result, the patient was able to walk without bleeding and subsequently discharged. The patients received insulin therapy and stayed in good condition in the follow-up.
Six months after the catheter removal, he was admitted to our institution because of right lower limb swelling and calf pain. On physical examination, the temperature was 36.9°C and blood pressure was 140/80 mmHg, the jugular venous pressure was normal, and the pulse was regular at 75 beats/min. Body mass index (BMI, weight/height2) was 21.5. Pulmonary abnormalities were not observed and abnormal heart sound was not heard. A bruit was heard on auscultation and a thrill was felt at the inguinal area. Serum levels of creatinine, blood urea nitrogen (BUN), and hemoglobin were 98 μmol/L, 5.6 mmol/L, and 10.8 g/dL, respectively. His serum potassium and sodium were 4.9 and 138 mEq/L, respectively. Serum PO4 level was 3.8 mg/dL. Serum calcium level was 9.4 mg/dL. The ECG revealed normal sinus rhythm. Chest radiograph revealed no cardiomegaly along with a cardiothoracic ratio of 48.0%. An AVF was detected by color Doppler ultrasound between the right superficial femoral artery (SFA) and the right femoral vein and subsequently it was confirmed by 3-dimensional reconstruction with CT and angiography (Figures 1 and 2).
FIGURE 1.

Three-dimensional CT revealing an arteriovenous fistula between the right superficial femoral artery and the right femoral vein (arrow).
FIGURE 2.
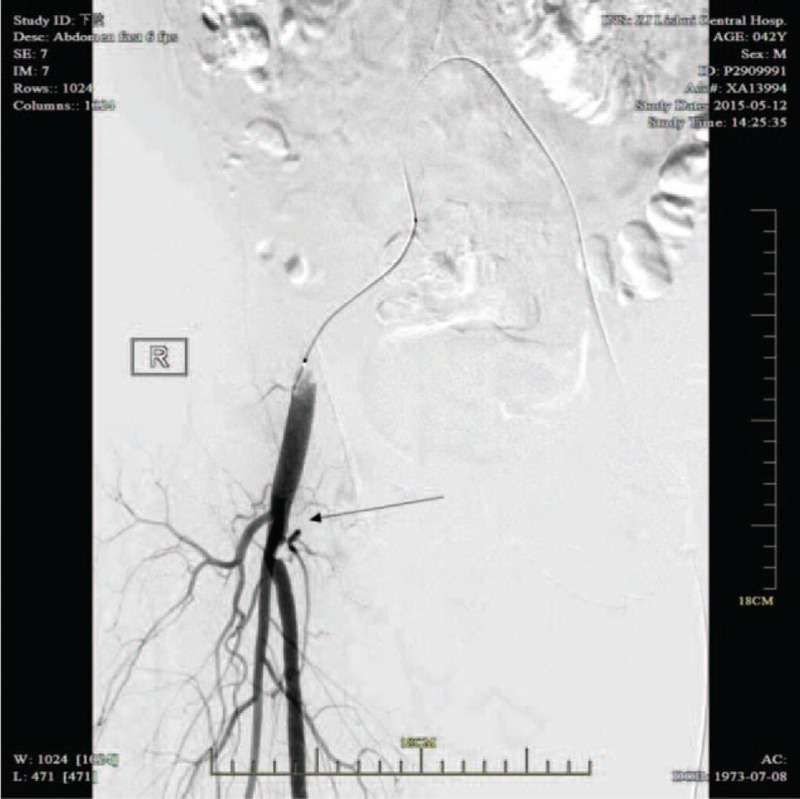
Angiography revealing the arteriovenous communication (between the superficial femoral artery and superficial femoral vein).
Then, the patient was transferred to the vascular surgery department. Initial treatment involved dilation of the stenotic lesion immediately beneath the bifurcation of the right common iliac artery using a balloon and stent insertion. During operation, the surgeon found a 3-mm diameter fistula between the right femoral vein and the right SFA. The right femoral vein and SFA were separated carefully. Then, vascular repairing was carried out with running nonabsorbable sutures. Repeat lower extremity angiography showed that fistula was repaired. The patient was discharged 8 days after surgery.
DISCUSSION
An AVF is an abnormal connection or passageway between an artery and a vein. AVF may result from stab injury, severe penetrating wounds, endovascular therapy. AVFs can be spontaneous, which can develop spontaneously or be caused by trauma.4 It is reported that traumatic AVF, a complication of femoral vein catheter insertion for HD, is an exceptional disease. However, when it occurs, it is often caused by damage to an artery while inserting a catheter into a vein. Chronic limb edema, false aneurysms degeneration, and high output cardiac failure due to fistula are common complications.5,6 To prevent this, ultrasound guidance is recommended. Several studies7–11 have demonstrated that real-time ultrasound guidance is superior to traditional landmark insertion techniques for the insertion of dialysis catheters because real-time ultrasound guidance is of particular value in increasing “first-pass” rates and reducing the risk of hematoma formation and other complications related to catheter insertion. So, ultrasound-guided catheter insertion is recommended by K/DOQI.1 Moreover, the use of a fine-gauge needle to locate the vein before introduction of the guide wire using the Seldinger needle is suggested as well.12
AVF as a complication of dual-lumen HD catheter insertion has been described in the medical literature. Kuramochi et al12 described a case of right superficial femoral AVF with a symptom of arterial bleeding. Chiba et al13 reported a case of an AVF associated with calf pain 2 months after the removal of the catheter. According to the literature,12–16 the most common initial symptoms were swelling, hemorrhage, limb pain, hematoma, thromboembolism, and cardiac failure. Limb swelling along with calf pain as the initial symptom was rare in any of the cases. But in this case, the patient was initial with a symptom of limb swelling and calf pain. Aggravation of calf pain and swelling started after walking.
Chiba et al13 reported a case of femoral AVF observed 2 months after catheter removal. In the present case, femoral AVF was observed 6 months after catheter removal. It seems that femoral AVF might be observed later than cervical AVF, probably because of inaccessibility to the groin area. Several explanations were possible for the formation of femoral AVF:13
(1) The femoral head provides posterior bony support, and it might be difficult to achieve hemostasis for the lack of bony support during compression following catheter removal.
(2) AVF once closed by a hematoma might be reopened by movement or anticoagulation with heparin during HD.
(3) Presumably, femoral AVF formation is caused by relatively larger caliber of the catheter and occult arterial puncture. In the present case, the anticoagulation with heparin during HD might be a reason for femoral AVF formation.
The risks factors that increase the likelihood of developing AVFs included distal groin punctures, arterial hypertension, antiplatelet therapy, and peri-procedural anti-coagulation17 In this case, the low puncture might increase the likelihood of developing AVFs. Moreover, there was no real-time ultrasound-guided that had been used for catheter insertion. The traditional landmark insertion techniques are commonly performed using anatomic landmarks to guide vessel cannulation. These traditional techniques cannot direct visualization of the target vein during catheter placement and are associated with an increased complication rate.
It may contribute to difficulty in venous cannulation. So, it is recommended that real-time ultrasound is performed to direct guidance of the needle insertion to avoid repeated blind punctures.18
CONCLUSION
Femoral venous catheterization is frequently selected to achieve temporary access to circulation in patients requiring acute hemodialysis. There have been wide reports on complications associated with central venous catheter insertion. However, few reports can be seen about femoral AVF formation. But AVF is a rare complication and occasionally fatal. Thus, it is important for nephrologists and nursing staff to be aware of this potential complication and to perform thorough clinical and medical examinations at the insertion and removal of temporary HD catheters. It is recommended that real-time ultrasound guidance should be used for catheters insertion to avoid inadvertent arterial puncture.
Footnotes
Abbreviations: ARF = Acute renal failure, AVF = Arteriovenous Fistula, CT = Computed Tomography, DKA = Diabetic ketoacidosis, ECG = Electrocardiograph, HD = Hemodialysis, IJV = Internal jugular vein, INR = International Normalized Ratio, SFA = Superficial femoral artery.
Wenhui Lei and Xueping Yu Chuxiao shao planned the article and contributed to data collection, discussing content, writing, and reviewing the article. Lie Jin, Jian Wang, and Chuifen Wu conceived the study and participated in its design, study supervision, and helping to write the article.
All authors have no conflicts of interest.
REFERENCES
- 1.III NKF-K/DOQI Clinical Practice Guidelines for Vascular Access: update 2000. Am J Kidney Dis 2001; 37 (1 Suppl 1):S137–S181. [DOI] [PubMed] [Google Scholar]
- 2.Santoro D, Benedetto F, Mondello P, et al. Vascular access for hemodialysis: current perspectives. Int J Nephrol Renovasc Dis 2014; 7:281–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Premuzic V, Tomasevic B, Erzen G, et al. [Temporary and permanent central venous catheters for hemodialysis]. Acta Med Croatica 2014; 68:167–174. [PubMed] [Google Scholar]
- 4.Puca AE, Pignatelli F. An adult case of idiopathic internal carotid-internal jugular vein arteriovenous fistula. Ann Vasc Surg 2015; 29:e845–847. [DOI] [PubMed] [Google Scholar]
- 5.Huseyin S, Yuksel V, Guclu O, et al. A rare etiology of heart failure: traumatic arteriovenous fistula due to stab injury 17 years ago. Balkan Med J 2015; 32:309–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thavarajan D, Bakran A. Iatrogenic arteriovenous fistula in the groin presenting as cardiac failure. NDT Plus 2009; 2:46–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin BS, Huang TP, Tang GJ, et al. Ultrasound-guided cannulation of the internal jugular vein for dialysis vascular access in uremic patients. Nephron 1998; 78:423–428. [DOI] [PubMed] [Google Scholar]
- 8.Cavatorta F, Zollo A, Galli S, et al. Ultrasound-guided cannulation and endocavitary electrocardiography placement of internal jugular vein catheters in uremic patients: the importance of routine chest X-ray evaluation. J Vasc Access 2001; 2:37–39. [DOI] [PubMed] [Google Scholar]
- 9.Gallieni M. Central vein catheterization of dialysis patients with real time ultrasound guidance. J Vasc Access 2000; 1:10–14. [DOI] [PubMed] [Google Scholar]
- 10.Shime N, Hosokawa K, MacLaren G. Ultrasound Imaging Reduces Failure Rates of Percutaneous Central Venous Catheterization in Children. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 2015. [DOI] [PubMed] [Google Scholar]
- 11.Stone MB, Nagdev A, Murphy MC, et al. Ultrasound detection of guidewire position during central venous catheterization. Am J Emerg Med 2010; 28:82–84. [DOI] [PubMed] [Google Scholar]
- 12.Kuramochi G, Ohara N, Hasegawa S, et al. Femoral arteriovenous fistula: a complication of temporary hemodialysis catheter placement. J Artif Organs 2006; 9:114–117. [DOI] [PubMed] [Google Scholar]
- 13.Chiba K, Hara M, Takeshita Y, et al. Femoral arteriovenous fistula associated with calf pain 2 months after removal of a haemodialysis catheter. BMJ Case Rep 2013; 2013: pii: bcr2013010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan CC, Lee V, Chu W, et al. Carotid jugular arteriovenous fistula: an unusual complication of internal jugular vein catheterization in children. Pediatr Blood Cancer 2012; 59:1302–1304. [DOI] [PubMed] [Google Scholar]
- 15.Bahcebasi S, Kocyigit I, Akyol L, et al. Carotid-jugular arteriovenous fistula and cerebrovascular infarct: a case report of an iatrogenic complication following internal jugular vein catheterization. Hemodial Int 2011; 15:284–287. [DOI] [PubMed] [Google Scholar]
- 16.Patel HV, Sainaresh VV, Jain SH, et al. Carotid-jugular arteriovenous fistula: a case report of an iatrogenic complication following internal jugular vein catheterization for hemodialysis access. Hemodial Int 2011; 15:404–406. [DOI] [PubMed] [Google Scholar]
- 17.Kelm M, Perings SM, Jax T, et al. Incidence and clinical outcome of iatrogenic femoral arteriovenous fistulas: implications for risk stratification and treatment. J Am Coll Cardiol 2002; 40:291–297. [DOI] [PubMed] [Google Scholar]
- 18.Aslam N, Palevsky PM. Insertion of temporary dialysis catheters with the aid of real-time ultrasound. Saudi J Kidney Dis Transpl 2001; 12:375–381. [PubMed] [Google Scholar]


