Abstract
Quality of transitions of care is one of the first concerns in patient safety. Redesigning the discharge process to incorporate clinical pharmacy activities could reduce the incidence of postdischarge adverse events by improving medication adherence. The present study investigated the value of pharmacist counseling sessions on primary medication adherence after hospital discharge.
This study was conducted in a 1844-bed hospital in France. It was divided in an observational period and an interventional period of 3 months each. In both periods, ward-based clinical pharmacists performed medication reconciliation and inpatient follow-up. In interventional period, initial counseling and discharge counseling sessions were added to pharmaceutical care. The primary medication adherence was assessed by calling community pharmacists 7 days after patient discharge.
We compared the measure of adherence between the patients from the observational period (n = 201) and the interventional period (n = 193). The rate of patients who were adherent increased from 51.0% to 66.7% between both periods (P < 0.01). When discharge counseling was performed (n = 78), this rate rose to 79.7% (P < 0.001). The multivariate regression performed on data from both periods showed that age of at least 78 years old, and 3 or less new medications on discharge order were predictive factors of adherence. New medications ordered at discharge represented 42.0% (n = 1018/2426) of all medications on discharge order. The rate of unfilled new medications decreased from 50.2% in the observational period to 32.5% in the interventional period (P < 10−7). However, patients included in the observational period were not significantly more often readmitted or visited the emergency department than the patients who experienced discharge counseling during the interventional period (45.3% vs. 46.2%; P = 0.89).
This study highlights that discharge counseling sessions are essential to improve outpatients’ primary medication adherence. We identified predictive factors of primary nonadherence in order to target the most eligible patients for discharge counseling sessions. Moreover, implementation of discharge counseling could be facilitated by using Health Information Technology to adapt human resources and select patients at risk of nonadherence.
INTRODUCTION
Quality of transitions of care is one of the first concerns in patient safety. Lack of information at admission, discharge, or during hospitalization may cause adverse drug events (ADEs), which are often preventable. ADEs result from discrepancies between prescribed and current regimen, inappropriate medication prescribing, inadequate monitoring for adverse effects and poor adherence.1–5 Most of the time, medication adherence is low. Patients often take less than the half dose prescribed.6 Many reasons can explain nonadherence. For instance, patients often have a lack of knowledge or do not perceive benefits to take prescribed drugs.7–9 Indeed, studies have demonstrated that patients understand as little as 50% of what their physician tells them.6 Moreover, 11% to 30% of patients discharged from hospital to home experience postdischarge adverse events (AEs).10,11 Among all of the AEs, 91% are due to newly prescribed medications.10 Furthermore, healthcare professionals ensured comprehension of medication changes only 12% of the time.6 Patient's knowledge of predictable medication side effects can also reduce ADEs without compromising medication adherence.10,12 However, only 62% of patients recalled being warned about their side effects.10
In the past 20 years, patient safety strategies have been developed to reduce preventable ADEs. Clinical pharmacists play a leading role in the implementation of these patient safety strategies.13–15 Redesigning the discharge process to incorporate clinical pharmacy activities can reduce the incidence of postdischarge AEs.12 First, medication reconciliation is an accurate process to detect and resolve discrepancies.16,17 Our previous study showed that medication reconciliation decreased the rate of patients with at least one unintended discrepancies from 45.8% to 2.1% (P < 0.001).17 Second, medication review and prescription analysis improve the quality of prescribing18–20 Moreover, initial counseling session for inpatient and discharge counseling improve medication adherence.21,22 Regarding the promotion of adherence, most of studies explored adherence of all medications prescribed or of specific drug classes.21,23–25 To the best of our knowledge, no study has focused on pharmacist intervention on primary nonadherence or first fill adherence. The primary nonadherence occurs when a patient does not fill an initial prescription. It concerns 7% to 28% of e-prescriptions for newly prescribed medications.26–30 On the contrary, the secondary nonobservance occurs when a patient discontinues a medication after filling the initial prescription. Raebel et al29 estimated that it concerned about 32% of ongoing prescriptions for chronic diseases as hypertension, diabetes mellitus, and lipid disorders. The respect of the duration of new medications prescribed during hospitalization or at discharge is of the utmost importance as these medications treat diseases that may cause the hospitalization. Outpatient adherence to postdischarge medications reflects the good communication between hospital staff and patient.
The present study investigated the value of pharmacist counseling sessions on primary medication adherence after hospital discharge.
PATIENTS AND METHODS
Setting and Subjects
This study was conducted from November 2010 to June 2011 at Nimes University Hospital, an 1844-bed French hospital. We led a prospective study with an observational period and an interventional period. The study was carried out in a unit of infectious and tropical diseases (ITD) of 15 beds and a unit of general medicine (GM) of 30 beds. Around 2000 patients are treated every year in these units.
Inclusion Criteria
Patients in both periods were included at the same wards. All patients over the age of 18 years, admitted in ITD and GM units during the study period were eligible for inclusion in the study. Inclusions were carried out by consecutive admissions during the study period. There were no additional inclusion or exclusion criteria. Patients with dementia or under guardianship were not excluded.
Ethics Statement and Trial Registration
Ethics approval was obtained from the Nimes hospital's ethics committee (no. 2011.03.01). The trial was authorized by the Information Technology and Freedoms Commission (CNIL, no. 1471663V0) which is the French data protection authority and by the French Agency for Medicine (ANSM). Written consent was obtained from all study participants or their legal representative for the patients under guardianship.
Study Design and Protocol
The study was divided in 2 periods of 3 months in order to avoid the contamination bias. The first 11 weeks control period was called “observational period.” During this period, a ward-based clinical pharmacist performed medication reconciliation and inpatient follow-up. The next 12 weeks period was called “interventional period.” The ward-based pharmacist performed medication reconciliation with initial counseling session, inpatient follow-up, and discharge counseling (Figure 1). The duration of the 2 periods has been chosen so as to obtain a sufficient and equal number of patients in both periods.
FIGURE 1.
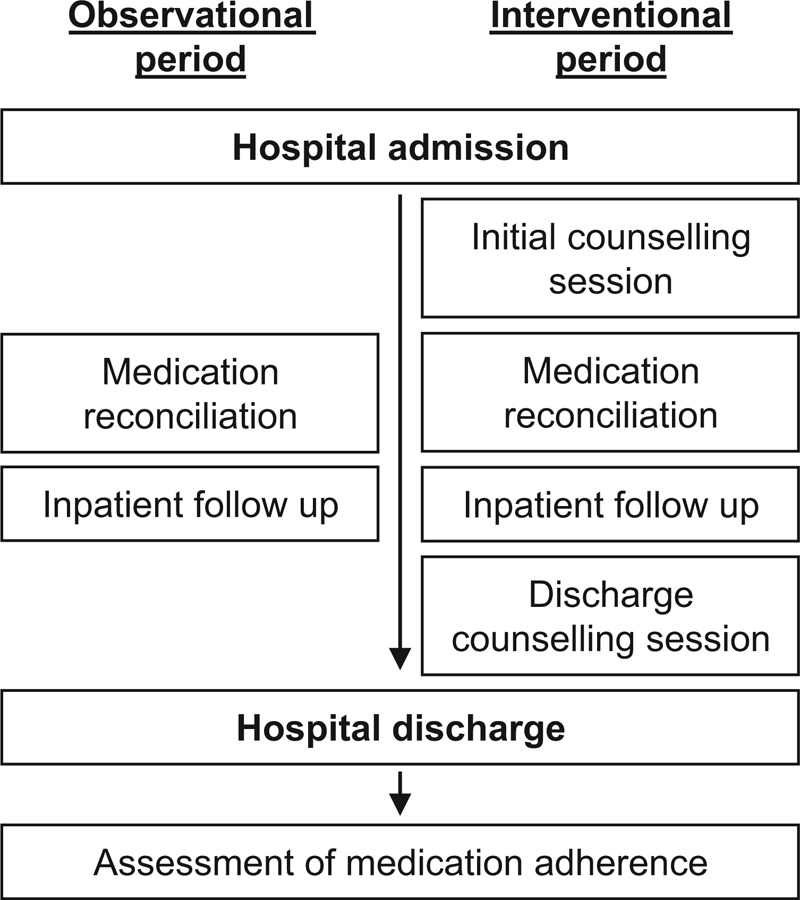
Study design.
Medication Reconciliation Process
Following a strict protocol, clinical ward-based pharmacists identified the most accurate list of the patient's medications called “best possible medication history” (BPMH) in collaboration with both nurses and physicians. First the pharmacist collected baseline demographics and medical history. Then, additional data such as laboratory tests could be collected. The BPMH gathers at least 3 sources of information that could be patient's interview, phone contact with the community pharmacist and/or the general practitioner, review of self-prepared medication list or personal medical records, review of medication containers, summaries of previous hospitalization or outpatient visits. The pharmacist collected information about prescribed and nonprescribed medications such as over-the counter medications, vitamins, herbals, drops, eyes drops, creams, inhaled medications, patches, and other products used to supplement patient's health. He compared the BPMH with patient's admission medication order, and detected discrepancies, that is, changes between medication history and admission orders. Then, he brought discrepancies to the attention of the prescriber which, if appropriate, made changes to the orders.
Inpatient Follow-Up
During patient hospitalization, pharmacists routinely performed prescription analysis that could be followed by pharmaceutical intervention when errors were detected. This analysis included checking incorrect doses, drug–drug interactions, the duration of the treatment, contraindications, restrictions of use, compliance with recommendations, and appropriate drug monitoring.
Initial Counseling Session
At admission, the initial counseling session was the first step for the pharmacist to promote better adherence. This session was performed during patient's interview of the medication reconciliation process. The pharmacists followed a standardized counseling session that allowed determining the patient understanding of his medications, his behavior toward the treatment, the barriers to adherence and social support. Pharmacist performed side effects review, drug allergies, and intolerances review. The aim was to know what the patient was really taking and how he had took his medication. A review of each medication indications was made in order to assess the patient's knowledge of medication use. Social support and patient's motivation for improving his health status were asked too. The pharmacy where the patient used to refill prescription was systematically investigated.
Discharge Counseling Session
The discharge counseling session helped patient understand their new medication regimen.30,31 It clarified the medications the patient should be taking after discharge. It occurred after the physician had written the discharge prescription. The ward-based pharmacist made a review of the purpose of discharge medication. This review included name, indication, dose, frequency, main side effects as well as special instructions for each medication; and it was sometimes facilitated with an illustrated medication schedule that clearly depicted this information and with patients’ drug containers. Discharge counseling allowed to promote adherence, and to anticipate barriers of adherence detected at the admission counseling session. Side effects were mentioned in order to improve patient's knowledge of predictable ADEs. The pharmacist asked patient to confirm in which pharmacy he used to refill prescription. Any significant findings during the counseling session were brought to the attention of the prescriber and, if appropriate, the discharge orders were modified.
Assessment of Medication Adherence
Seven days after discharge, the clinical pharmacist phoned to the community pharmacists to collect medication dispensing data. Significant findings were called to the patient's primary care physician.
DATA COLLECTION
Data of medication reconciliation, counseling sessions, and medication dispensing were collected by a structured and standardized data collection form. Data included age, ward, BPMH, medications at admission and discharge, unintentional discrepancies, name of community pharmacist. Medications data included medication type (new medications/medications to be continued), dose, route of administration, duration. Main diagnoses were extracted from our electronic health record system. There were no electronic generation of discharge instructions and no active electronic medication reconciliation process. Reliability of all data collection was ensured by the independent review of 2 investigators. The investigators who performed the pharmaceutical care activities and the data collection were 2 residents who benefited from an initial training in clinical pharmacy before the study. The data of hospital readmission within 30 days of initial discharge were extracted from our electronic health record system.
Outcome Variables
The primary outcome was outpatient primary medication adherence. Primary adherence was defined as filling all new medications at discharge. A patient who failed to fill 1 or more new medications at hospital discharge was considered as nonadherent. As secondary outcome, we analyzed the rates of hospital readmissions and emergency department visits within 30 days of initial discharge.
Statistical Analysis
Descriptive statistics are reported as counts and percentages for categorical variables and means and standard deviations for continuous variables with normal distribution and median and quartiles for others.
Comparisons of baseline characteristics and of putative risk factors between the 2 periods were performed with Student t test, Mann–Whitney test, Kruskal–Wallis test, the χ2 test or Fisher exact test as appropriate, to assess if the population of the 2 periods are comparable. The effects of putative predictors of the differences in medication adherence between patients from the observational and the interventional periods were evaluated. We first compared potentially relevant baseline characteristics and prescription records between patients fulfilling/not-fulfilling the outcome. All variables with a P-value lower than 0.20 were considered as potential covariates and adjusted logistic regression models were computed and adjusted odds radios and 95% confidence intervals were deduced. Variables were selected according a backward selection. Since, logistic regression requires log-linearity of continuous variables, when log-linearity assumptions were not true, continuous data were categorized according to deciles. In order to estimate the most parsimonious model, modalities with similar odds ratios were combined.
Analyses were performed by the Biostatistics Department of our university hospital. All analyses were performed using SAS software (SAS Institute, Cary, NC) version 9.3. P-values less than 0.05 were interpreted as statistically significant for 2-sided tests.
RESULTS
Patient Characteristics
During the study period, 394 patients were enrolled (Figure 2). As previously described,17 patient inclusions were balanced between the observational period (51.0%) and the interventional period (49.0%). The median length of stay was 8[Q25% = 4; Q75% = 12] days and the median age of included patients was 74 [Q25% = 59; Q75% = 82] years old. There was no significant difference between the observational period and the interventional period for length of stay (8[Q25% = 5; Q75% = 12.5] vs. 8[Q25% = 4; Q75% = 10], P = 0.16), age (76[Q25% = 63; Q75% = 83] vs. 72[Q25% = 56; Q75% = 82], P = 0.061), sex (53.5% vs. 53.9% men, P = 0.94) and care units (51.7% vs. 51.8% patients in GM, P = 0.99). The rate of new medications prescribed at discharge was not significantly different between the 2 periods (0.43[Q25% = 0.25; Q75% = 0.67] vs. 0.46[Q25% = 0.25; Q75% = 0.69], P = 0.22). Neither was the number of medications prescribed on discharge medication order (DMO) (8[Q25% = 6; Q75% = 10] vs. 7[Q25% = 4; Q75% = 9], P = 0.23).
FIGURE 2.
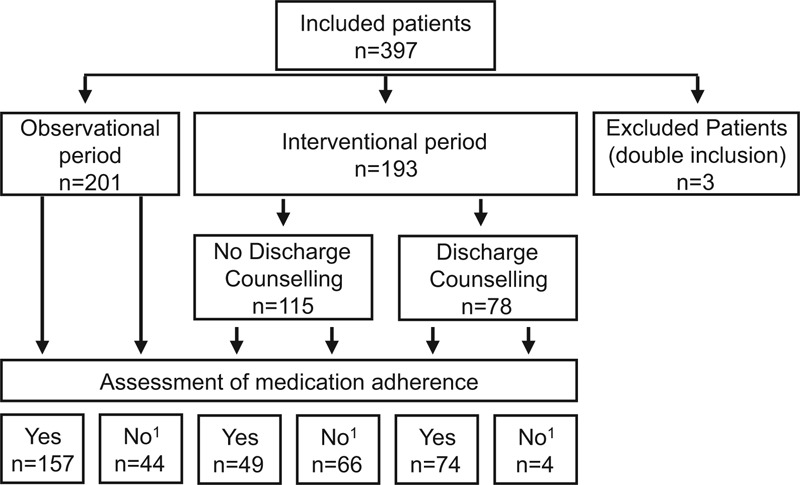
Flowchart. 1Transfer to another ward, no new medications at discharge, missing data.
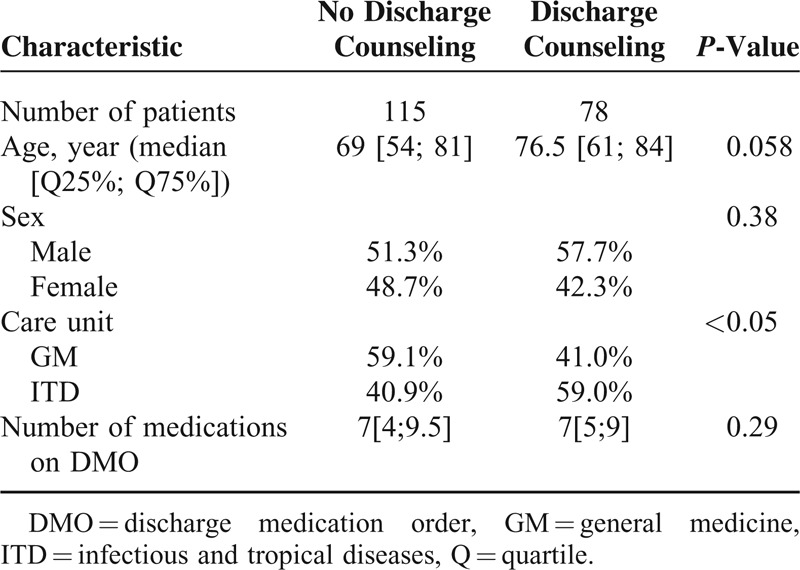
During the interventional period, discharge counseling was performed for 78 patients (40.4%) (Figure 2). Patients of ITD unit benefited significantly more often from discharge counseling than patients of GM unit (59.0% vs. 41.0%; P < 0.05) (Table 1) because they were less often transferred to another ward than patients of GM unit (12.1% vs. 38.2%; P < 0.0001). There were no other significant different characteristics between populations with and without discharge counseling in the interventional period (Table 1).
TABLE 1.
Patient Characteristics in the Interventional Period
Outpatient Medication Adherence
Assessment of Medication Adherence
Assessment of medication adherence was performed for 280 patients. It could not be performed for 114 patients, mainly during interventional phase (21.9% vs. 36.3%; P < 0.005) due to a higher transfer rate (20.4% vs. 31.1%; P < 0.05). Of these 114 patients, 86 (75.4%) were transferred to another ward and 17 (14.9%) had no prescriptions or no new medications at discharge. Two patients were transferred to another ward with no new prescribed medications. Overall, there were missing data which concerned 13 patients (11.4%) who were discharged at the week-ends or evenings and patients who were not discharged to their own home.
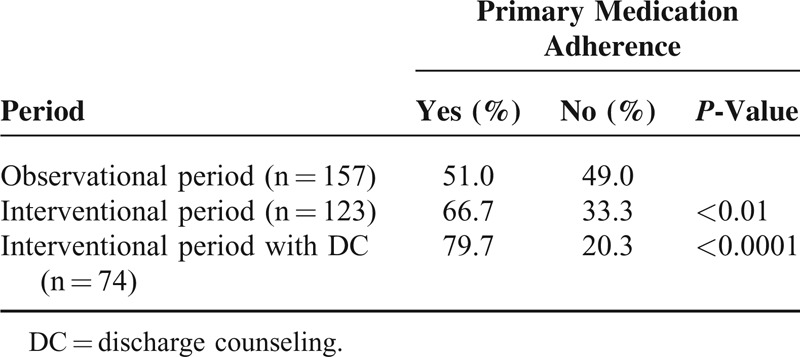
Finally, we compared the measure of adherence between 157 patients from the observational period and 123 patients included in the interventional period. The rate of patients who were adherent increased from 51.0% of the observational to 66.7% of the interventional period (P < 0.01). When discharge counseling was performed, this rate rose to 79.7% (P < 0.001) (Table 2).
TABLE 2.
Medication Adherence Assessment
The multivariate regression performed on data from both periods showed that age under 78 years old, and 3 or less new medications were predictive factors of adherence (Table 3). Patients with nervous system affections were about 2.5 times less adherent whereas patients with gastrointestinal tract affections were about 12 times more adherent (Table 3). There was no significant association between adherence and other major classes of diagnoses. For the 280 patients analyzed, the median number of medications prescribed on DMO was similar between adherent and nonadherent patients (7[Q25% = 5; Q75% = 10] vs. 8[Q25% = 5; Q75% = 10], P = 0.91). Therefore, this parameter was not included in the multivariate model.
TABLE 3.
Medication Adherence-Influencing Factors From Observational Period vs. Interventional Period
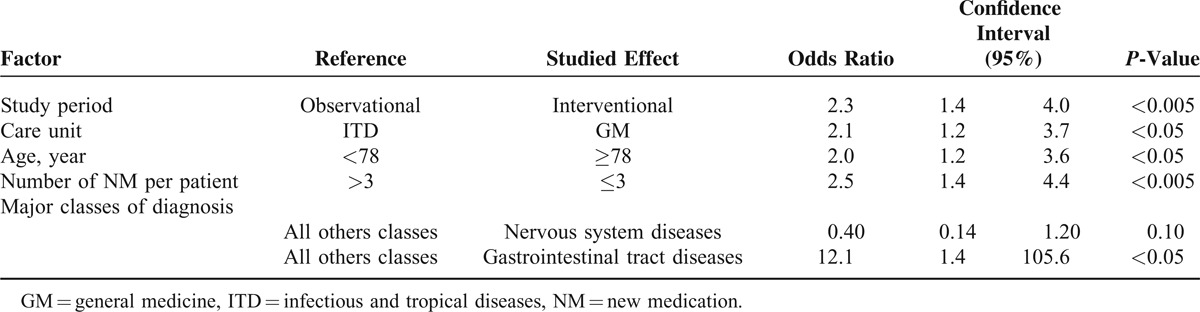
Multivariate regression performed on patients with discharge counseling (n = 74) versus patients from observational period (n = 157) confirmed these predictive factors. Moreover, this analysis showed that patients with kidney and urinary tract diseases were less adherent than other patients (OR: 0.26, 95% CI: 0.09–0.71).
Patients discharged from the ITD unit were less adherent than those discharged from the GM unit (Table 3). However, this result was not found on patients who benefited from discharge counseling (OR: 1.7, 95% CI: 0.90–3.30) and the odds ratio for the study period rose to 5.1 95% CI: 2.46–10.56.
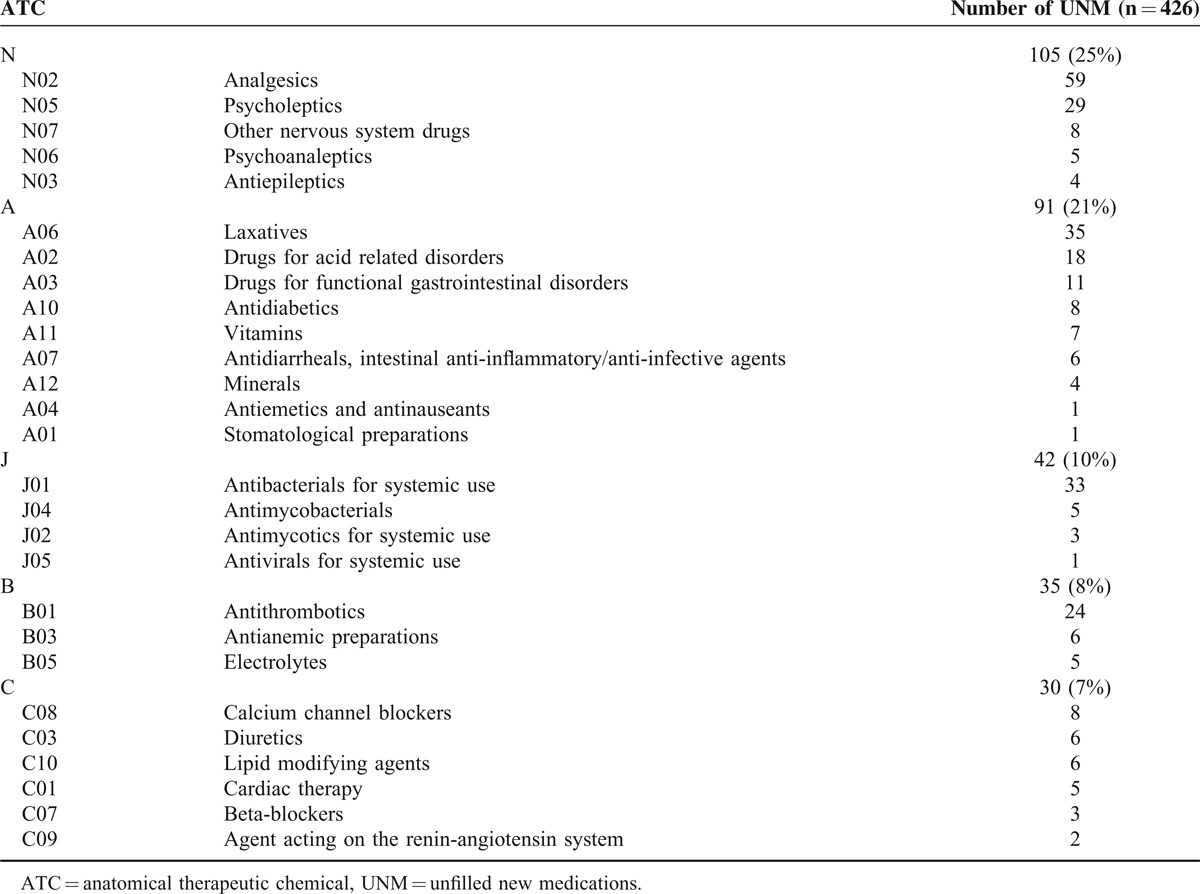
Characteristics of New Medications
New medications ordered at discharge represented 42.0% (n = 1018/2426) of all medications on DMO. The rate of unfilled new medications decreased from 50.2% (n = 270/538) in the observational period to 32.5% (n = 156/480) in the interventional period (P < 10–7). Patients from the ITD unit had significantly more new medications prescribed than patients from the GM unit (44.7% vs. 39.3%, P < 0.01). Most of the new medications which were not filled at 7 days are detailed in Table 4.
TABLE 4.
Main Classes of Unfilled New Medications According to ATC Classification System
Postdischarge Healthcare Utilization
Postdischarge healthcare utilization data showed no significant difference between the observational period and the interventional period (45.3% vs. 41.5%; P = 0.44). Patients included in the observational period were not significantly more readmitted or visited the emergency department than patients with discharge counseling during the interventional period (45.3% vs. 46.2%; P = 0.89).
DISCUSSION
We previously showed that medication reconciliation performed by clinical pharmacists reduces the rate of drug-related problems at hospital admission.17 But secure medication care is not enough; we must understand the obstacles to medication adherence and bypass them. For this reason, we performed a study to determine the rate of nonadherent patients and understand the limits to adherence to antiinfective drugs.25 Because hospital discharge remains a critical point in transition of care, we propose in this study to describe the impact of discharge counseling implementation in real-life conditions. Thus, for reasons of feasibility, discharge counseling could not be performed for all the patients included in interventional period. Moreover, more than half of patients were transferred to other wards during the study and all DMO could not be recovered. Because there were more transferred patients from the GM unit, discharge counseling was performed more often on patients from the ITD unit. However, patient's characteristics were comparable between both units. Outcome analysis was performed for all patients included because the noncompletion of discharge counseling reflects real life. We also checked that patient's characteristics were comparable with or without discharge counseling in interventional period.
To date, no study has assessed the impact of pharmaceutical counseling on primary adherence. Our results showed that counseling sessions performed by a ward-based clinical pharmacist improve primary adherence. We observed a greater impact when initial counseling session was associated to a discharge counseling session. Previous studies demonstrated the beneficial effects of clinical pharmacist on medication adherence without discriminating primary and secondary adherence. Several studies found significantly better levels of medication adherence when pharmaceutical counseling sessions were performed.21,22,32,33 However some studies showed no significant differences.34,35
Primary nonadherence is an important phenomenon since timely initiation of medications is critical for treating both acute and chronic conditions. First-fill prescription also reflects the good communication between patient and healthcare professionals and the comprehension of medication prescriptions. The rate of primary adherence in the observational period (51%) was lower than those reported by other authors (72–92 %).27–29,36,38 However, these studies investigated first-fill prescription within 30 days29,37,38 or more27 rather than 7 days as in our study. The increase in the collection period includes a larger proportion of nonadherent patients. Yet, it seems appropriate to assess the primary adherence on a short-time delay. The later the patient fills its order, the more it is likely to have a bad secondary adherence. The delay of first-fill prescription may be explained by the fact that, in the best case, the patient already had at home a part of prescribed medications, or on the contrary, he did not realize the importance to cure himself. Therefore, over 7 days, we estimated that there was a lack of primary adherence.
Most of studies investigated databases from health insurances to obtain more exhaustive data.27,29,37,38 Some studies focused on specific drug classes such as diabetic37 or antihypertensive medications.38 We showed that 25% of new medications unfilled are used to treat nervous system diseases and 21% to treat gastrointestinal tract diseases. The most common new medications unfilled 7 days after discharge were analgesics (13.8%) and laxatives (8.2%). Fischer et al27 showed similar results about pain medications which were the most unfilled new medications. We also observed that antibiotics for systemic use (7.7%) and antithrombotics (5.6%) were common newly prescribed medications which were unfilled at 7 days. A possible reason is that, at postdischarge, patients felt healed and did not understand the importance of their treatment, most of the time because of lack of communication from health professionals. These results were less significant for chronic disease management perspective because we cannot exclude that some patients had yet these medications at home. However nonadherence to these drug classes can carry potential harm for the patient.
Few authors studied discriminative ability of logistic models for primary adherence.27,29,37 We identified predictive factors for primary adherence in order to identify patients at risk. Adverse criteria were an age over 78 years old, a number of newly prescribed medications over 3 and hospitalization for nervous system disease. As also showed by Fischer et al,27 our results confirmed that age was a predictive factor of nonadherence. However, unlike them, we found an upper limit to 65 years old. We established for the first time that major classes of diagnosis were the strongest predictor of primary adherence and that the probability of nonadherence increase with the number of newly prescribed medications. Some studies focused on the number of drugs ordered and refills37,38 but the number of newly prescribed medications seems more appropriate to assess primary adherence. As health literacy assessment was not included in our study, we could not link this parameter with misunderstanding prescription drug labels as Davis and colleagues did.39
We did not report differences in readmission rates between both periods (45.3% vs. 41.5%). However, most of studies have not be able to highlight any differences in postdischarge healthcare utilization32,33,40 even if the study sample size was bigger than ours.12,41 Schnipper et al34 showed that pharmacist counseling was associated with a significant lower rate of both preventable ADEs 30 days after discharge, and hospital readmission, but with no differences in medication adherence. Still et al42 suggested that after stratification based on readmission risk, the moderate-risk pharmacy-counseled group had a significantly lower 30-day readmission rate than the moderate-risk control group (3.8% vs. 18.9%; P = 0.033). We did not assess the causes of visits in the emergency department or readmissions. Hence, we could not know the proportion of patients that were readmitted for preventable reasons. Furthermore postdischarge healthcare utilization is a complex process and it is difficult to isolate the cause-to-effect relationship between medication adherence and emergency department visit or hospital readmission. Our study did not aim, neither was not powered, to detect this effect.
This study has some limitations. Indeed, to reflect real-life conditions and to avoid contamination bias, we performed a prospective study with an alternate month design instead of a randomized controlled study. Medication dispensing data were only collected with phone calls (patients could go to another community pharmacy even if they were asked twice) and not compared with exhaustive data base from health insurance. In some cases, electronic prescriptions to recover prescriptions after patient's discharge were not available. The ward-based pharmacist was able to collect only 70.5% of medication dispensing data and performed discharge counseling for only 40.4% of inpatients because of logistic problems (eg, week-end, time constraints, patients who did not return at their own home). However, our work reflects the real-life context in which we need to improve quality of healthcare system.
CONCLUSION
This study highlights that discharge counseling sessions are essential to improve outpatient primary adherence. Ward-based pharmacist plays an indispensable role before patient discharge by transmitting medication information and assessing its understanding. He liaises between hospital and community. We identified predictive factors of primary nonadherence in order to target the most eligible patients for discharge counseling sessions. However, additional studies must be conducted to identify further criteria of primary nonadherence. Moreover, the implementation of discharge counseling could be facilitated by using Health Information Technology to adapt human resources and select patients at risk of nonadherence.
Uncited Reference
32.
Acknowledgment
We would like to thank Dr. Mariella Lomma for proofreading the manuscript.
Footnotes
Abbreviations: ADE = adverse drug event, AE = adverse event, ANSM = French Agency for Medicine, BPMH = best possible medication history, CNIL = Information Technology and Freedoms Commission, DMO = discharge medication order, GM = general medicine, ITD = infectious and tropical diseases.
Author contributions: GLB, CRM, CC, VR, JMK, and AS conceived and designed the experiments; FD and FA performed the experiments; GLB, SB, CRM, and CC analyzed the data; GLB, FD, SB, CRM, CC, VR, JMK, and AS contributed reagents/materials/analysis tools; GLB and CRM wrote the paper; FD, SB, CC, JMK, and AS contributed to the various drafts of the report.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.LaPointe NM, Jollis JG. Medication errors in hospitalized cardiovascular patients. Arch Intern Med 2003; 163:1461–1466. [DOI] [PubMed] [Google Scholar]
- 2.Abbasinazari M, Hajhossein Talasaz A, Eshraghi A, et al. Detection and management of medication errors in internal wards of a teaching hospital by clinical pharmacists. Acta Med Iran 2013; 51:482–486. [PubMed] [Google Scholar]
- 3.Geurts MM, van der Flier M, de Vries-Bots AM, et al. Medication reconciliation to solve discrepancies in discharge documents after discharge from the hospital. Int J Clin Pharm 2013; 35:600–607. [DOI] [PubMed] [Google Scholar]
- 4.Kuo GM, Touchette DR, Marinac JS. Drug errors and related interventions reported by United States clinical pharmacists: the American College of Clinical Pharmacy practice-based research network medication error detection, amelioration and prevention study. Pharmacotherapy 2013; 33:253–265. [DOI] [PubMed] [Google Scholar]
- 5.Paulino EI, Bouvy ML, Gastelurrutia MA, et al. Drug related problems identified by European community pharmacists in patients discharged from hospital. Pharm World Sci 2004; 26:353–360. [PubMed] [Google Scholar]
- 6.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003; 163:83–90. [DOI] [PubMed] [Google Scholar]
- 7.Burke LE, Dunbar-Jacob J. Adherence to medication, diet, and activity recommendations: from assessment to maintenance. J Cardiovasc Nurs 1995; 9:62–79. [DOI] [PubMed] [Google Scholar]
- 8.Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008; CD000011. doi: 10.1002/14651858.CD000011.ub3. [DOI] [PubMed] [Google Scholar]
- 9.Chan FW, Wong FY, So WY, et al. How much do elders with chronic conditions know about their medications? BMC Geriatr 2013; 13:59.doi: 10.1186/1471-2318-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ 2004; 170:345–349. [PMC free article] [PubMed] [Google Scholar]
- 11.Kripalani S, Roumie CL, Dalal AK, et al. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med 2012; 157:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker PC, Bernstein SJ, Jones JN, et al. Impact of a pharmacist-facilitated hospital discharge program: a quasi-experimental study. Arch Intern Med 2009; 169:2003–2010. [DOI] [PubMed] [Google Scholar]
- 13.Crotty M, Rowett D, Spurling L, et al. Does the addition of a pharmacist transition coordinator improve evidence-based medication management and health outcomes in older adults moving from the hospital to a long-term care facility? Results of a randomized, controlled trial. Am J Geriatr Pharmacother 2004; 2:257–264. [DOI] [PubMed] [Google Scholar]
- 14.Kaboli PJ, Hoth AB, McClimon BJ, et al. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med 2006; 166:955–964. [DOI] [PubMed] [Google Scholar]
- 15.Milner J, Wiemer D. Hospital pharmacists take the lead in discharge counseling. Drug Topics 2012; 156:13. [Google Scholar]
- 16.Kwan JL, Lo L, Sampson M, et al. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158 (5 Pt 2):397–403. [DOI] [PubMed] [Google Scholar]
- 17.Leguelinel-Blache G, Arnaud F, Bouvet S, et al. Impact of admission medication reconciliation performed by clinical pharmacists on medication safety. Eur J Intern Med 2014; 25:808–814. [DOI] [PubMed] [Google Scholar]
- 18.De Smet PA, Denneboom W, Kramers C, et al. A composite screening tool for medication reviews of outpatients: general issues with specific examples. Drugs Aging 2007; 24:733–760. [DOI] [PubMed] [Google Scholar]
- 19.Ulfvarson J, Rahmer PB, Fastbom J, et al. Medication reviews with computerized expert support: evaluation of a method to improve the quality of drug utilization in the elderly. Int J Health Care Qual Assur 2010; 23:571–582. [DOI] [PubMed] [Google Scholar]
- 20.Lehnbom EC, Stewart MJ, Manias E, et al. The impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother 2014; 48:1298–1312.Epub 2014 Jul 21. [DOI] [PubMed] [Google Scholar]
- 21.Smith L, McGowan L, Moss-Barclay C, et al. An investigation of hospital generated pharmaceutical care when patients are discharged home from hospital. Br J Clin Pharmacol 1997; 44:163–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Rashed SA, Wright DJ, Roebuck N, et al. The value of inpatient pharmaceutical counseling to elderly patients prior to discharge. Br J Clin Pharmacol 2002; 54:657–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA 2006; 296:2563–2571. [DOI] [PubMed] [Google Scholar]
- 24.Rubio-Valera M, Serrano-Blanco A, Magdalena-Belío J, et al. Effectiveness of pharmacist care in the improvement of adherence to antidepressants: a systematic review and meta-analysis. Ann Pharmacother 2011; 45:39–48. [DOI] [PubMed] [Google Scholar]
- 25.Faure H, Leguelinel-Blache G, Salomon L, et al. Assessment of patient adherence to anti-infective treatment after returning home. Med Mal Infect 2014; 44:417–422. [DOI] [PubMed] [Google Scholar]
- 26.Karter AJ, Parker MM, Moffet HH, et al. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res 2009; 44 (5 Pt 1):1640–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med 2010; 25:284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fischer MA, Choudhry NK, Brill G, et al. Trouble getting started: predictors of primary medication nonadherence. Am J Med 2011; 124:1081.e9–1081.e22. [DOI] [PubMed] [Google Scholar]
- 29.Raebel MA, Ellis JL, Carroll NM, et al. Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med 2012; 27:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oliveira-Filho AD, Morisky DE, Costa FA, et al. Improving post-discharge medication adherence in patients with CVD: a pilot randomized trial. Arq Bras Cardiol 2014; 103:503–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandra A, Malcolm N, Fetters M. Practicing health promotion through pharmacy counseling activities. Health Promot Pract 2003; 4:64–71. [DOI] [PubMed] [Google Scholar]
- 32.Bolas H, Brookes K, Scott M, et al. Evaluation of a hospital-based community liaison pharmacy service in Northern Ireland. Pharm World Sci 2004; 26:114–120. [DOI] [PubMed] [Google Scholar]
- 33.Sarangarm P, London MS, Snowden SS, et al. Impact of pharmacist discharge medication therapy counseling and disease state education: Pharmacist Assisting at Routine Medical Discharge (Project PhARMD). Am J Med Qual 2013; 28:292–300. [DOI] [PubMed] [Google Scholar]
- 34.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med 2006; 166:565–571. [DOI] [PubMed] [Google Scholar]
- 35.Calvert SB, Kramer JM, Anstrom KJ, et al. Patient-focused intervention to improve long-term adherence to evidence-based medications: a randomized trial. Am Heart J 2012; 163:657. e1–665.e1. [DOI] [PubMed] [Google Scholar]
- 36.Fallis BA, Dhalla IA, Klemensberg J, et al. Primary medication non-adherence after discharge from a general internal medicine service. PLoS One 2013; 8: e61735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shah NR, Hirsch AG, Zacker C, et al. Factors associated with first-fill adherence rates for diabetic medications: a cohort study. J Gen Intern Med 2009; 24:233–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens 2009; 22:392–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis TC, Wolf MS, Bass PF, III, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med 2006; 145:887–894. [DOI] [PubMed] [Google Scholar]
- 40.Nazareth I, Burton A, Shulman S, et al. A pharmacy discharge plan for hospitalized elderly patients—a randomized controlled trial. Age Ageing 2001; 30:33–40. [DOI] [PubMed] [Google Scholar]
- 41.Lipton HL, Bird JA. The impact of clinical pharmacists’ consultations on geriatric patients’ compliance and medical care use: a randomized controlled trial. Gerontologist 1994; 34:307–315. [DOI] [PubMed] [Google Scholar]
- 42.Still KL, Davis AK, Chilipko AA, et al. Evaluation of a pharmacy-driven inpatient discharge counseling service: impact on 30-day readmission rates. Consult Pharm 2013; 28:775–785. [DOI] [PubMed] [Google Scholar]


