Abstract
The transgender community represents an understudied population in the literature. The objective of this study was to compare risk behavior, and HIV and sexually transmitted infection (STI) rates between transgender women and transgender men undergoing community-based HIV testing.
With this retrospective analysis of a cohort study, we characterize HIV infection rates as well as reported risk behaviors and reported STI in 151 individual transgender women and 30 individual transgender men undergoing community based, voluntary screening for acute and early HIV infection (AEH) in San Diego, California between April 2008 and July 2014.
HIV positivity rate was low for both, transgender women and transgender men undergoing AEH screening (2% and 3%, respectively), and the self-reported STI rate for the prior 12 months was 13% for both. Although transgender women appeared to engage in higher rates of risk behavior overall, with 69% engaged in condomless receptive anal intercourse (CRAI) and 11% engaged in sex work, it is important to note that 91% of transgender women reported recent sexual intercourse, 73% had more than 1 sexual partner, 63% reported intercourse with males, 37% intercourse with males and females, and 30% had CRAI.
Our results indicate that in some settings rates of HIV infection, as well as rates of reported STIs and sexual risk behavior in transgender men may resemble those found in transgender women. Our findings support the need for comprehensive HIV prevention in both, transgender women and men.
INTRODUCTION
Transgender women are considered to be one of the highest risk groups for HIV infection.1–4 In a recent meta-analysis, the pooled HIV prevalence was 19.1% in transgender women worldwide (n = 11,066), and 21.7% for transgender women in the United States (n = 2705, from 9 studies).1,5–12 In another meta-analysis, large percentages of transgender women (range 27%–48%) reported engaging in risky behaviors, such as condomless receptive anal intercourse (CRAI), multiple casual partners, or sex work.13 Notably, however, risk behavior and HIV prevalence data varied widely between studies.1,8–11,14,15 Also HIV prevalence has been 11.8%, and therefore markedly lower in 18 other studies focusing on self-reported HIV seropositivity among transgender women.13
To date, very few studies evaluated HIV prevalence and risk behaviors among transgender men. Most of these studies reported that both, HIV prevalence rates (range 0–3%) and risk behaviors were low among transgender men.1,6,13 In contrast, similar HIV prevalence rates (about 10%), risk behavior, and sexually transmitted infection (STI) rates in transgender men when compared to transgender women were reported in a more recent study.11 The objective of this study was to compare risk behavior, HIV, and STI rates between transgender women and transgender men undergoing community-based HIV testing with detection of acute and early HIV infection (AEH).
METHODS
This retrospective analysis of a cohort study comprises transgender persons who underwent voluntary HIV screening (single and repeat testers) in San Diego, California with the “Early Test” between April 2008 and July 2014. During this time, 181 transgender persons self-identified as transgender men or women and were included in the analysis.
The “Early Test” (https://theearlytest.ucsd.edu) is a community-based, voluntary, confidential AEH screening program that provides point-of-care rapid HIV antibody testing followed by reflex HIV nucleic acid amplification testing in all antibody negative persons.16–18 With the “Early Test” program approximately 4000 individuals per month are screened free of charge at 5 regular plus additional mobile-testing sites (including sites at the Lesbian, Gay, Bisexual, Transgender Center; the Gay Men's Health Clinic; the San Diego County Health Department; the Antiviral Research Center; substance abuse treatment centers; and special community event venues) in San Diego, United States. Similar to other settings in the United States men who have sex with men (MSM) bear the greatest burden of HIV infection in San Diego, which is resembled in the “Early Test” where 72% of tests overall, 85% of repeat testing encounters, and 88% of HIV diagnoses are among MSM.16 Risk behavior was collected by using a risk assessment form with 19 detailed survey questions (focusing primarily on sexual risk behavior, substance use, STI diagnoses – all reported for the prior 12 months – and demographics). Survey questions were assessed and the form filled out by the testing staff before each HIV-testing encounter, and data were later entered into the data system (always in duplicate to minimize data entry errors). After testing clients were recommended to come back 6 months later for the next testing encounter.
For statistical analysis SPSS 21 (SPSS Inc., Chicago, IL) was used. Outcome measures included risk behavior and STIs reported for the previous 12 months at every testing encounter, as well as HIV diagnoses. Outcome measures were compared between transgender women and transgender men using Chi-squared (for proportions) or Mann–Whitney U test (for continuous variables, such as numbers of partners). A P-value > 0.5 was considered statistically significant.
The University of California, San Diego Human Research Protections Program approved the study protocol and consent. All study participants provided voluntary, written informed consent before any study procedures.
RESULTS
A total of 14,612 unique clients underwent HIV screening using the “Early Test” between April 2008 and July 2014, including 181 (1.23%) persons who self-identified as transgender persons (who had 278 voluntary HIV tests). Median age was 28 years (inter-quartile range [IQR] 23–35 years); 52% reported Hispanic ethnicity, 24% White race, and 24% other races (mainly Black and Asian).
The sample comprised 151 (83%) unique transgender women and 30 (17%) unique transgender men. Median age was significantly lower among transgender men when compared to transgender women (P = 0.001), while no difference was found for race or ethnicity. Twenty-eight (19%) of transgender women and 1 (3%) transgender man underwent repeat testing during the period of study (median of 3 tests/year). Demographic characteristics for transgender women and transgender men are depicted in Table 1.
TABLE 1.
Demographic Characteristics and Prevalence of Self-Reported STIs/Risk Behaviors in the Prior 12 Months of Transgender Individuals Undergoing Community-Based Screening for Acute/Early HIV
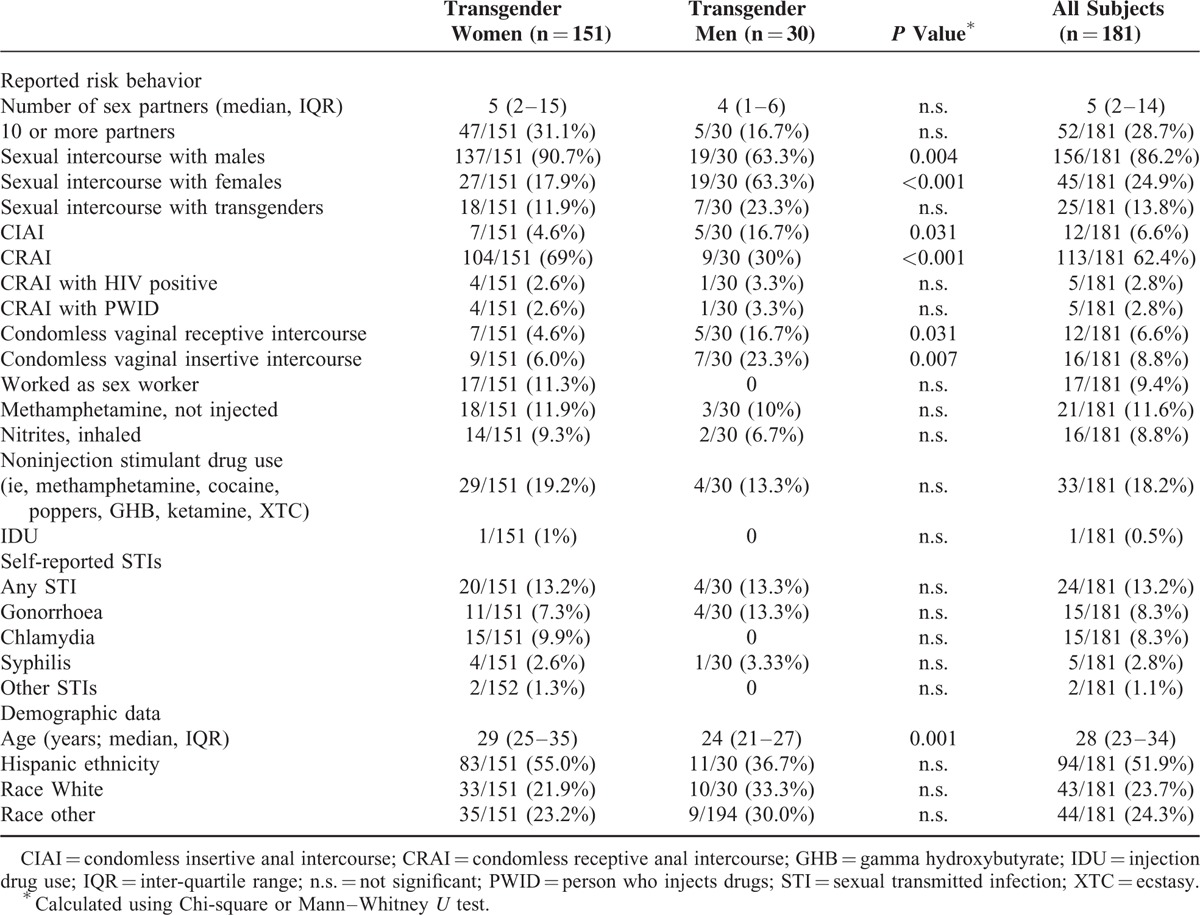
Overall, 3 of 151 transgender women (1.99%, 1 AEH, 2 chronic) and 1 of 30 transgender men (3.33%, chronic) were newly diagnosed with HIV infection resulting in an HIV cumulative positivity rate of 2% for transgender women and 3% for transgender men. Self-reported STIs for both transgender women and men during the previous 12 months are depicted in Table 1, and included mostly gonorrhea, chlamydia (exclusively reported by transgender women), and syphilis. Proportions of clients reporting any recent STI diagnosis were the same among transgender women and men (13% for both).
At first test, the vast majority of transgender women (95%) and transgender men (91%) reported sexual intercourse during the previous 12 months. Sexual intercourse with males was reported by 91% of transgender women and 63% of transgender men (P = 0.004, median 4 male partners, IQR 2–14), while sexual intercourse with females was reported by 63% of transgender men and 19% of transgender women (P > 0.001, median 1 female partner, IQR 1–3). Intercourse with both males and females was reported significantly more frequently among transgender men (37% vs 13% among transgender women; P = 0.001). In addition 25/181 transgender clients overall (14%, no significant difference between transgender women and men) reported sexual intercourse with transgender partners (median 1, IQR 1–3 partners); of whom 56% (14/25) also had intercourse with both males and females. Total number of sexual partners in the prior 12 months was slightly higher among transgender women, although this difference was not significant. CRAI was reported significantly more frequently among transgender women (69% vs 13%, P > 0.001), while condomless insertive anal intercourse was more frequently reported among transgender men (17% vs 5%, P = 0.031). The exchange of sex for money or goods was reported by 17 transgender women (11%) only. Rates of injected and noninjected substance use did not differ between transgender women and men. Table 1 provides prevalence of risk behaviors at first test reported for the prior 12 months in transgender women and men. With regard to STI rates or risk behavior no difference was observed between different ethnicities and races.
DISCUSSION
This represents one of the largest samplings of transgender persons undergoing AEH screening. The HIV positivity rate, at 2.2%, found for transgender clients in the setting of a community-based AEH screening program, is much lower than previous studied and self-reported prevalence rates among transgender women,5,7–10,12,19,20 but similar to self-reported prevalence reported for transgender men.1,6,13,14,21 The overall HIV positivity rate (2.2%) was also similar to the rate (2.1%) reported by Center of Disease Control and Prevention (CDC) HIV-testing sites across the United States for transgender clients.3 The transgender population reflected in the CDC report was at the highest risk of HIV when testers were broken down by gender, with cisgender females constituting 0.2% of new HIV diagnoses and cisgender males constituting 0.9%. Interestingly, the transgender group in our study has lower rates of new HIV diagnoses than the 4.69% found in our MSM population.16,17
When our cohort is broken down by gender, transgender women had a slightly lower (not significant) HIV rate (1.99%) than transgender men (3.33%) although this was based on only 1 case among transgender men. Nevertheless, this is an interesting finding in the context of the predominance of literature suggesting that transgender women represent a higher HIV risk group. Most studies describe much higher HIV rates in transgender women than transgender men, sometimes as high as 68%.1,5,7–10,12–14,19–21 The CDC data, to which our numbers are most similar, simply use the blanket of “transgender” for its results and do not break down results further.3 Because our data is the result of only a single individual in a small cohort of transgender men, the overall prevalence of HIV in transgender men may differ.
We also found that 13.3% of transgender men self-reported STIs (mostly gonorrhea), which is higher than the STI rates reported previously for transgender men (6% and 7%).13 In contrast, cumulative self-reported STI rates of 13.2% in transgender women found in this study fall within the (lower) range of what have been previously reported.12 In a 2008 meta-analysis of transgender risk behavior, self-reported prior STI diagnosis in MTF was between 12% to 79% in 10 studies, with a weighted mean of 21.1%.13
Also notable were the high rates of risk behaviors seen in both groups. Although transgender women appeared to engage in higher rates of risk behavior overall, with 69% engaged in CRAI and 11% engaged in sex work, it is important to note that 91% of transgender women reported recent sexual intercourse, 73% had more than 1 sexual partner, 63% reported intercourse with males, 37% intercourse with males and females, and 30% had CRAI. This finding stands in contrast to a previous study, where 66% of transgender men reported either no sex at all or only intercourse with 1 sex partner.6
The most important limitation of the study is the small sample size, in particular of transgender men. Also, the age of the transgender women was significantly higher than the age of transgender men which might have influenced risk behavior and infection outcomes.
In conclusion, our results indicate that in some setting rates of HIV infection, as well as rates of reported STIs and sexual risk behavior in transgender men may resemble those found in transgender women. Our finding has also been supported by another recent study.11 Our results therefore highlight the need for comprehensive HIV prevention, including preexposure prophylaxis, in both transgender women and men in similar settings.
Footnotes
Abbreviations: AEH = acute and early HIV infection, CDC = Center of Disease Control and Prevention, CRAI = condomless receptive anal intercourse, IQR = inter-quartile range, MSM = men who have sex with men, STI = sexually transmitted infections.
MH and NG contributed equally to this work.
This work was supported by funds from the Max Kade Foundation, New York (Max Kade Postdoctoral Research grant), the International Research Fellowship in NeuroAIDS (R25-MH081482), and grants from the National Institutes of Health: AI093163, AI100665, DA034978, AI036214, AI43638, AI074621, AI106039, and AI007385-24.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
MH served on the speakers’ bureau of Merck, SJL and SM both reported grant funding from Gilead Sciences, Inc. The remaining author has no conflicts of interest to disclose.
REFERENCES
- 1.Kenagy GP. HIV among transgendered people. AIDS Care 2002; 14:127–134. [DOI] [PubMed] [Google Scholar]
- 2.CDC. HIV Among Transgender People in the United States. [serial online]. 2013. [Google Scholar]
- 3.CDC. HIV Testing at CDC-Funded Sites, United States, Puerto Rico, and the U.S. Virgin Islands, 2010. 2011. [Google Scholar]
- 4.Nuttbrock L, Hwahng S, Bockting W, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquir Immune Defic Syndr 2009; 52:417–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baral SD, Poteat T, Stromdahl S, et al. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis 2013; 13:214–222. [DOI] [PubMed] [Google Scholar]
- 6.Clements-Nolle K, Marx R, Guzman R, et al. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health 2001; 91:915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murrill CS, Liu KL, Guilin V, et al. HIV prevalence and associated risk behaviors in New York City's house ball community. Am J Public Health 2008; 98:1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schulden JD, Song B, Barros A, et al. Rapid HIV testing in transgender communities by community-based organizations in three cities. Public Health Rep 2008; 123 Suppl 3:101–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shrestha RK, Sansom SL, Schulden JD, et al. Costs and effectiveness of finding new HIV diagnoses by using rapid testing in transgender communities. AIDS Educ Prev 2011; 23:49–57. [DOI] [PubMed] [Google Scholar]
- 10.Simon PA, Reback CJ, Bemis CC. HIV prevalence and incidence among male-to-female transsexuals receiving HIV prevention services in Los Angeles County. AIDS 2000; 14:2953–2955. [DOI] [PubMed] [Google Scholar]
- 11.Stephens SC, Bernstein KT, Philip SS. Male to female and female to male transgender persons have different sexual risk behaviors yet similar rates of STDs and HIV. AIDS Behav 2011; 15:683–686. [DOI] [PubMed] [Google Scholar]
- 12.Kellogg TA, Clements-Nolle K, Dilley J, et al. Incidence of human immunodeficiency virus among male-to-female transgendered persons in San Francisco. J Acquir Immune Defic Syndr 2001; 28:380–384. [DOI] [PubMed] [Google Scholar]
- 13.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav 2008; 12:1–17. [DOI] [PubMed] [Google Scholar]
- 14.Reisner SL, Vetters R, White JM, et al. Laboratory-confirmed HIV and sexually transmitted infection seropositivity and risk behavior among sexually active transgender patients at an adolescent and young adult urban community health center. AIDS Care 2015; 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reisner SL, Mimiaga MJ, Bland S, et al. HIV risk and social networks among male-to-female transgender sex workers in Boston, Massachusetts. J Assoc Nurses AIDS Care 2009; 20:373–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoenigl M, Green N, Mehta SR, et al. Risk factors for acute and early HIV infection among men who have sex with men (MSM) in San Diego, 2008 to 2014: a cohort study. Medicine (Baltimore) 2015; 94:e1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoenigl M, Weibel N, Mehta SR, et al. Development and validation of the San Diego Early Test (SDET) score to predict acute and early HIV infection risk in men who have sex with men. Clin Infect Dis 2015; 61:468–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morris SR, Little SJ, Cunningham T, et al. Evaluation of an HIV nucleic acid testing program with automated Internet and voicemail systems to deliver results. Ann Intern Med 2010; 152:778–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDS 2013; 27:621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poteat T, Reisner SL, Radix A, et al. epidemics among transgender women. Curr Opin HIV AIDS 2014; 9:168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reisner SL, Perkovich B, Mimiaga MJ. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS 2010; 24:501–513. [DOI] [PMC free article] [PubMed] [Google Scholar]


