Abstract
The purpose of this study was to use finite element analysis to compare the biomechanical characteristics after lateral locking plate (LLP) or LLP with a medial anatomical locking plate (LLP-MLP) fixation of proximal humeral fractures with an unstable medial column.
First, a 3-dimensional, finite element analysis model was developed. Next, LLP and LLP-MLP implants were instrumented into the proximal humeral fracture models. Compressive and rotational loads were then applied to the humerus model to determine the biomechanical characteristics. Both normal and osteoporotic proximal humerus fractures were simulated using 2 internal fixation methods each under 7 loading conditions. To assess the biomechanical characteristics, the construct stiffness, fracture micromotion, and stress distribution on the implants were recorded and compared.
The LLP-MLP method provided both lateral and medial support that reduced the stress on the LLP and the amount of displacement in the fracture region. In contrast, the LLP method resulted in more instability in the medial column and larger magnitudes of stress. In osteoporotic bone, the LLP was more inclined to fail than LLP-MLP.
The LLP-MLP method provides a strong support for the medial column and increases the stability of the region surrounding the fracture.
INTRODUCTION
Comminuted fracture of the proximal humerus is a common injury, especially in patients with osteoporosis. Epidemiologic studies have shown that proximal humeral fractures account for 4% to 5%1,2 of all fractures and 45%3 of humerus fractures. Many different methods of internal fixation have been applied to proximal humeral fractures, such as intramedullary nailing,4,5 locking plates,6,7 and prosthetic replacement8,9 and so on. In recent years, locking plate has become popular and shown good clinic outcomes.10 Lateral locking plate (LLP) can provide rigid fixation and satisfactory biomechanical characteristics.11 However, some complications still haunts doctors, including varus malunion, screw cutout, nonunion, device failure, avascular necrosis, subacromial impingement, and infection.11–13 Among these complications, varus malunion is the most common.14
The varus malunion can often be attributed to the loss of a buttress on the medial column.14 To address this problem, some researchers have suggested placing oblique locking calcar screws. In their opinion, the placement of such calcar screws in the angular stable plate fixation of proximal humeral fractures was associated with less secondary loss of reduction by providing inferomedial support.15,16 However, Bai et al17 reported that calcar screws increased the axial and shear stiffness of the humerus, but did not improve the overall biomechanical stability, concluding that direct medial support may be a more effective strategy. Based on this work, we used a medial anatomical locking plate (MLP) to directly support the medial column. We believed that the combined application of MLP and LLP would provide a stable dual-column buttress for the treatment of proximal humerus fractures, especially in cases of severely comminuted or osteoporotic fractures. However, the biomechanical characteristics of LLP and LLP-MLP fixation have not been investigated.
Thus, the purpose of this study was to use finite element analysis to compare the biomechanical characteristics of LLP and LLP-MLP fixation. We simulated normal and osteoporotic proximal humerus fractures using the 2 different internal fixation methods each under 7 loading conditions. To assess the biomechanical characteristics of the repair, the construct stiffness, fracture micromotion, and implant stress distribution were determined and compared.
METHODS
Finite Element Models and Implants
This study was done at the Provincial Hospital Affiliated to Shandong University in Jinan, Shandong, China and permission was obtained from the hospital Ethics Committee. Authors had to obtain patient consent before enrolling participants in this study.
A 3-dimensional finite element method model was developed from a computed tomography (CT) scan of a 38-year-old healthy female subject. The proximal humeral fracture model with an unstable medial column was simulated as a 10 mm horizontal bone defect below the surgical neck (Fig. 1). The areas of cortical and cancellous bone were separated based on the CT values in Hounsfield units (HU). The CT values, as measured on our scanner (Lightspeed VCT, GE, Fairfield, CT), of cortical bone were 450 to 3000 HU and of cancellous bone were 150 to 450 HU. The strength of the humerus was simulated in 2 conditions: normal bone (Nor) and osteoporotic bone (Ost). The elastic modulus of the Ost model bone was decreased by 33% for cortical bone and 66% for cancellous bone.18
FIGURE 1.
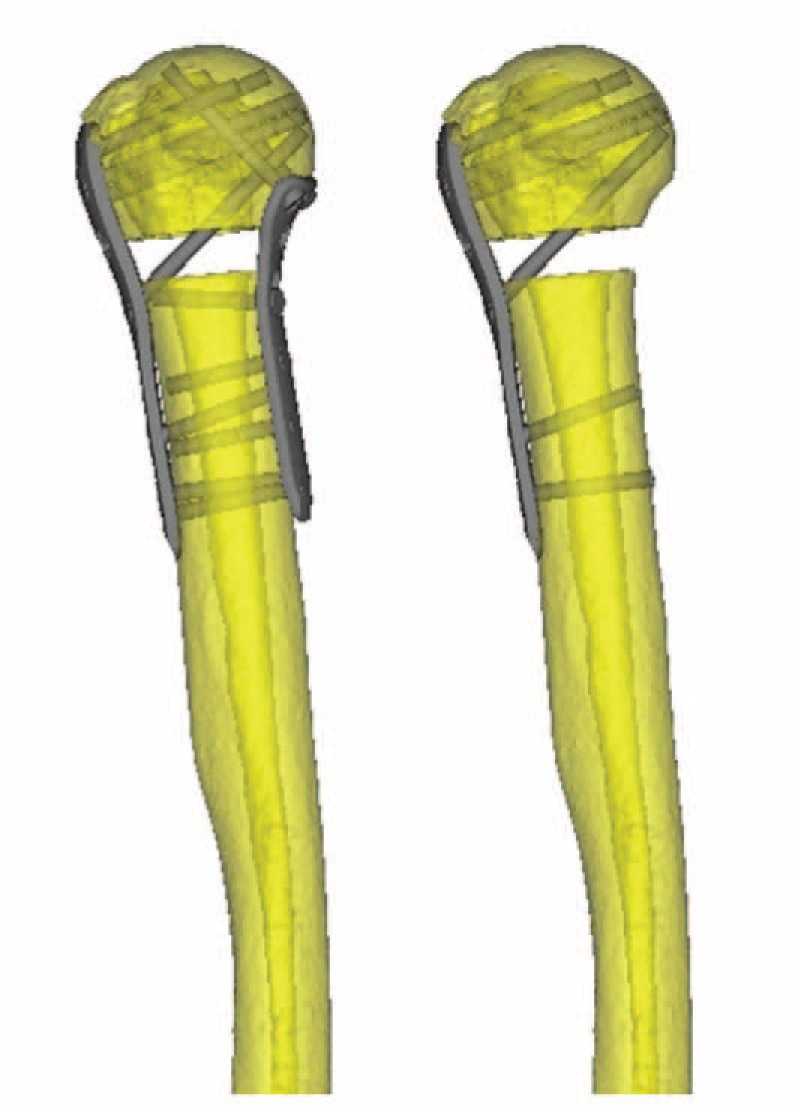
The proximal humeral fracture with an unstable medial column was simulated using a 10 mm horizontal bone defect below the surgical neck. The LLP and LLP-MLP fixations were instrumented into the proximal humeral fracture models by simulating a standard surgical technique. LLP = lateral locking plate, LLP-MLP = lateral locking plate and medial locking plate.
Two types of implants, the LLP and LLP-MLP, were instrumented into the proximal humeral fracture model (Fig. 1). The LLP was 90 mm in length and 2.5 mm in thickness (Waston Medical, Jiangsu, China), and the MLP was 70 mm in length and 2.5 mm in thickness (Waston Medical). The LLP and LLP-MLP were instrumented into the proximal humeral fracture models by simulating standard surgical techniques. The LLP was secured to the lateral proximal humerus with 6 proximal and 2 distal locking screws, and the MLP was fixed to the medial proximal humerus with 2 proximal locking screws, 3 distal locking screws, and 1 cortical screw. The threads of the locking screws and cortical screw were omitted to simplify the models. The humerus-LLP model contained a total of 139,150 elements and 72,986 nodes. The humerus-LLP-MLP model contained a total of 171,495 elements and 81,381 nodes.
Finite Element Analysis
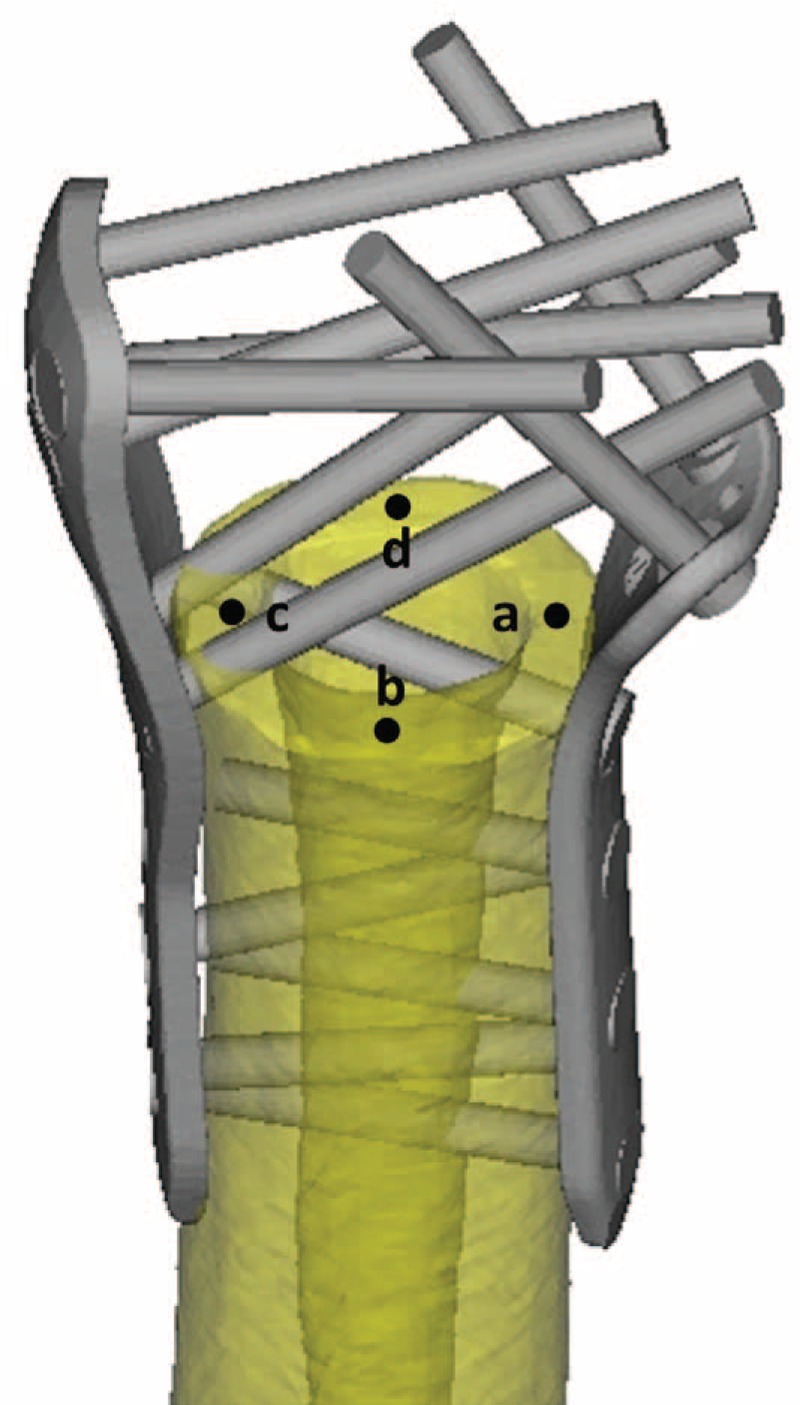
The finite element analysis was performed in Abaqus 6.13 (3DS, Waltham, MA). Linear elastic isotropic material properties were assigned to all models and implant materials. The properties of the bones and implants are shown in Table 1.18,20–23 The interface of the humeral head and the glenoid was fixed in the models of the proximal humeral fracture. The contact behavior of the plate/locking-screw and bone/locking-screw interfaces was defined as fully fixed. The contact behavior of the plate/bone and cortical-screw/bone interfaces was defined as surface-to-surface. The cortical screws were fixed into the plates and humeral cortices. All of the contact elements were defined as deformable elements. The analyses were performed assuming frictionless interactions to simplify the contact phenomena.
TABLE 1.
Material Properties of Finite Element Models
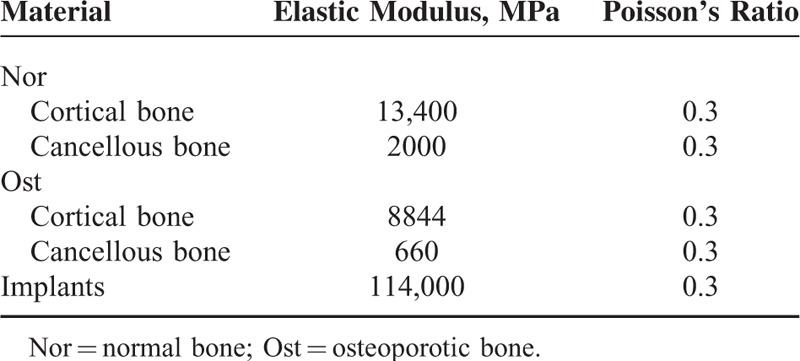
Compressive and rotational loads were applied to the humerus model to simulate the functions of the shoulder joint, including abduction, adduction, flexion, extension, axial compression, and internal and external rotation (Fig. 2). For compression, 100 N loads were distributed onto the shaft of the humerus in 4 directions to simulate the effects of muscle abduction, adduction, flexion, and extension. In addition, 200 N loads were applied to the ends of the humerus to simulate axial compression. To simulate internal and external rotations, 7.5 and −7.5 Nm torques were applied to the end of the humerus around the humeral mechanical axis.
FIGURE 2.
Compressive and rotational loads were applied to the humerus model to simulate the functions of the shoulder joint, including abduction, adduction, flexion, extension, axial compression, and internal and external rotation.
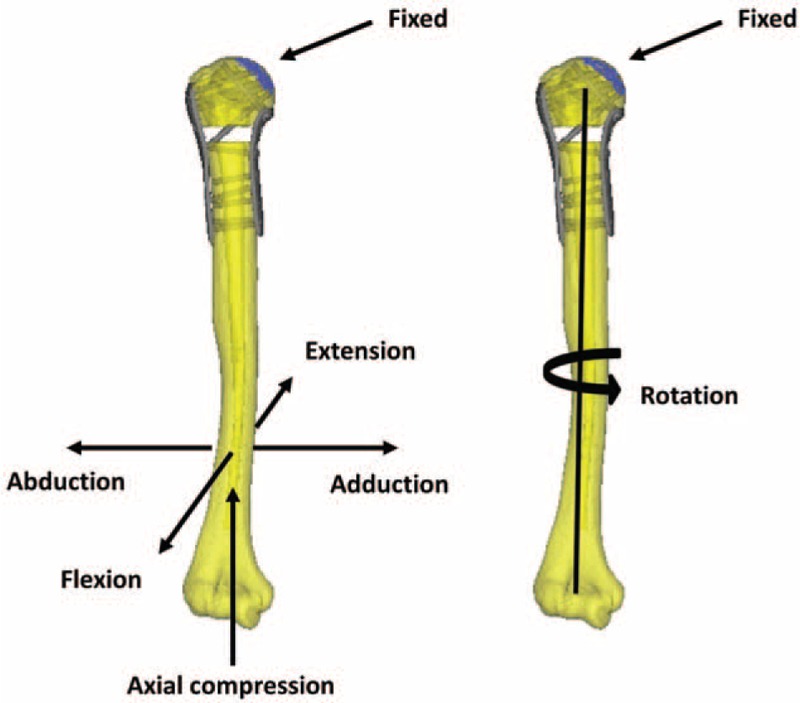
The stiffness of the simulations was determined to compare the stabilities of the different constructs. The stability of the fracture zone was assessed as the displacement of the fracture gap. Four points were defined on the distal fracture gap to measure the displacements (Fig. 3): the medial (a), anterior (b), lateral (c), and posterior (d). To assess the force conditions, the von Mises stress distribution and maximum stresses on the implants were determined.
FIGURE 3.
The medial (a), anterior (b), lateral (c), and posterior (d) points on the distal fracture gap.
RESULTS
Construct Stiffness
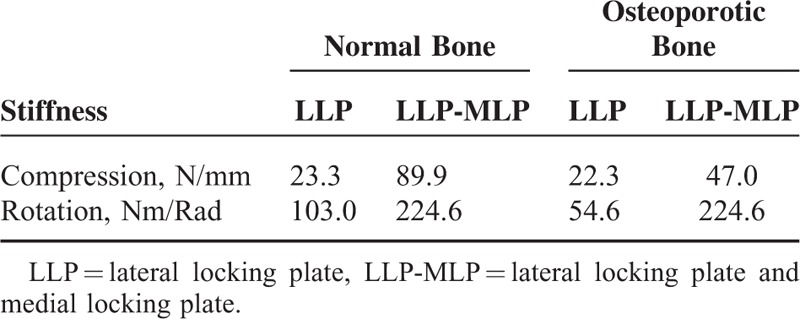
The compressive and rotational stiffness of the LLP and LLP-MLP fixation techniques are shown in Table 2. When assuming Nor properties, LLP-MLP fixation provided a higher construct stiffness than LLP fixation. Similar results were also found when assuming an Ost bone condition, especially for rotational stiffness. In fact, the LLP-MLP rotational stiffness in Ost bone was 224.6 N/Rad, approximately 4 times larger than the LLP rotational stiffness.
TABLE 2.
The Construct Stiffness of Humerus
Implant Stress
The maximum von Mises stress and stress distribution after LLP fixation under different loading conditions are shown in Figure 4 and Table 3. During shoulder joint abduction or adduction, the stress was concentrated on the deformation site where was area from the broad to the narrow on the LLP. During shoulder joint flexion or extension, the maximum stress occurred on the proximal and distal locking screws after LLP fixation. The maximum stress under axial compression occurred on the deformation site and on the proximal and distal locking screws. During internal and external rotation of the shoulder joint, the stress was minimal.
FIGURE 4.
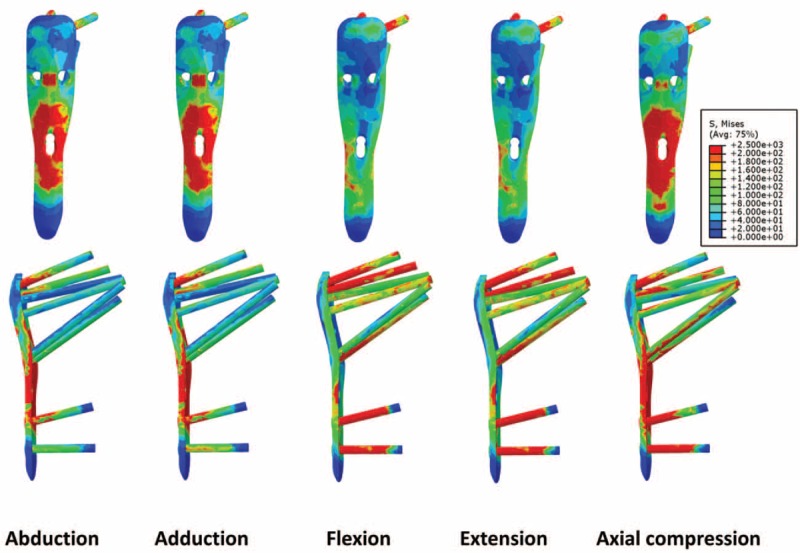
The maximum von Mises stress and the stress distribution on the lateral locking plate (LLP) under different motion conditions.
TABLE 3.
The Maximum von Misses Stress in the LLP

The maximum von Mises stress and stress distribution after LLP-MLP fixation are shown in Figure 5 and Table 3. The maximum von Mises stress was clearly decreased by at least 50% in the LLP-MLP condition compared with the LLP fixation. The maximum von Mises stress in the Nor and Ost bone conditions are shown in Table 3. The maximum von Mises stress was increased after LLP fixation in the Ost bone, especially compared with the use of LLP-MLP.
FIGURE 5.
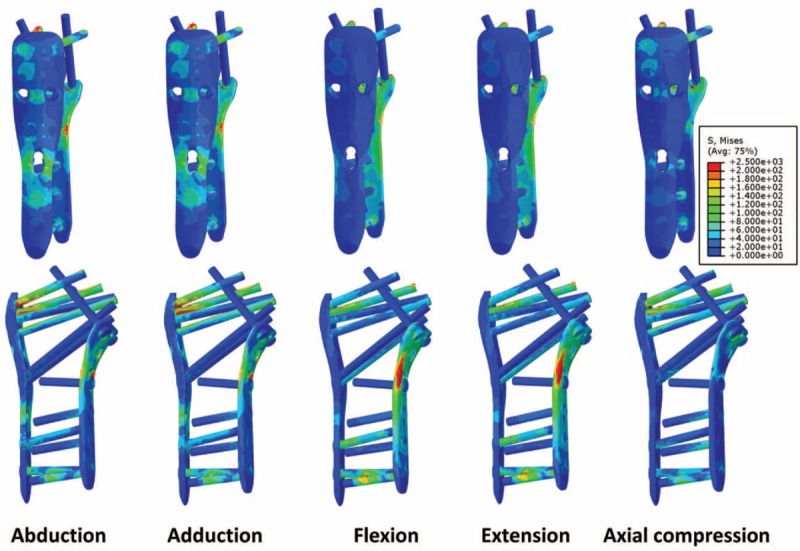
The maximum von Mises stress and the stress distribution on the lateral locking plate and medial locking plate (LLP-MLP).
Fracture Displacements
The fracture displacements measured during different simulated activities are shown in Figure 6 . The distributions of the compressive and rotational displacements are shown in Figure 7. In general, the displacements measured were significantly reduced by using the MLP in addition to the LLP. In the Ost bone condition, however, the displacements of points b, c, and d were increased during abduction and adduction after LLP-MLP fixation. For both LLP and LLP-MLP, the stability of the fractures was decreased in the Ost bone condition.
FIGURE 6.
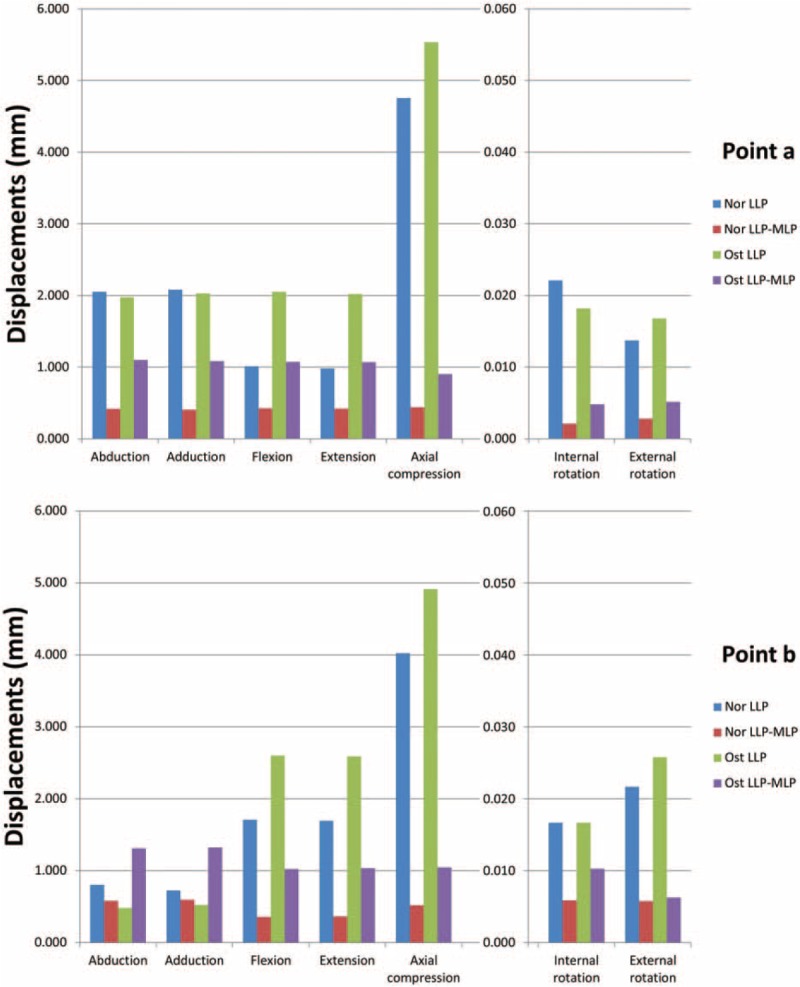
The displacements of the fracture region under different loading conditions in both the Nor and Ost bone after LLP and LLP-MLP fixation. LLP = lateral locking plate, LLP-MLP = lateral locking plate and medial locking plate, Nor = normal bone; Ost = osteoporotic bone.
FIGURE 6 (Continued).
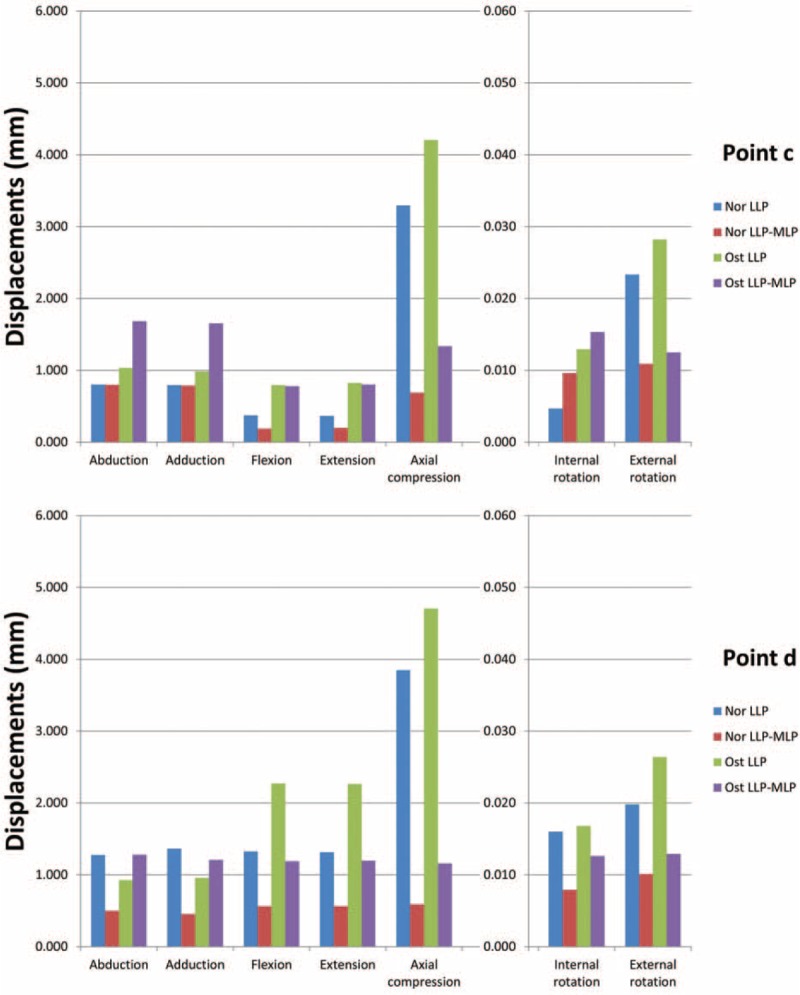
The displacements of the fracture region under different loading conditions in both the Nor and Ost bone after LLP and LLP-MLP fixation. LLP = lateral locking plate, LLP-MLP = lateral locking plate and medial locking plate, Nor = normal bone; Ost = osteoporotic bone.
Illustrative Case Study
A 62-year-old female patient sustained a fracture of her proximal humerus with an unstable medial column after a fall. Preoperative anteroposterior radiographs and CT scans were performed (Fig. 8). The patient strongly preferred surgery to return to normal life as soon as possible.
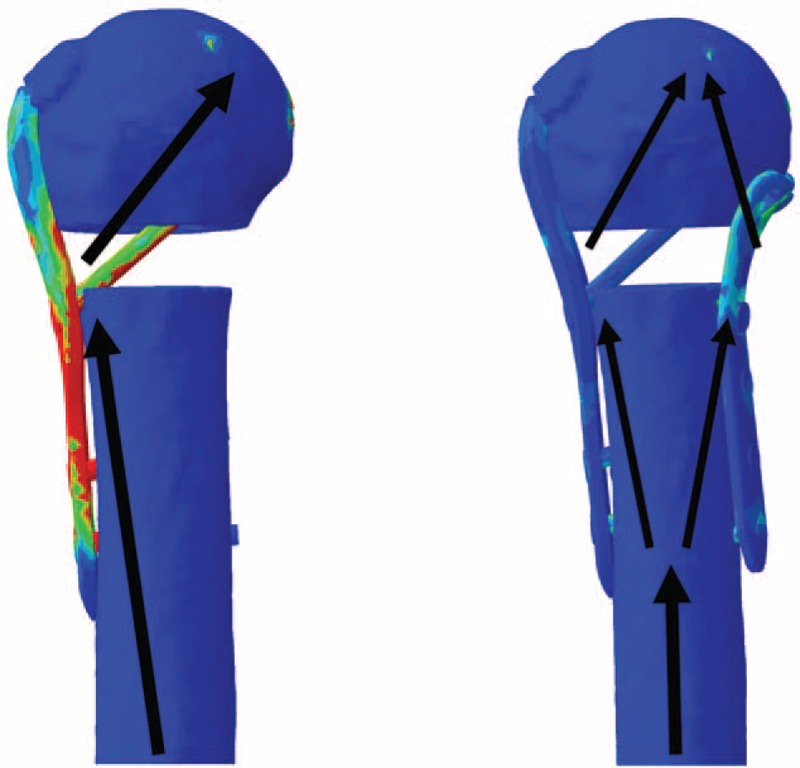
FIGURE 7.
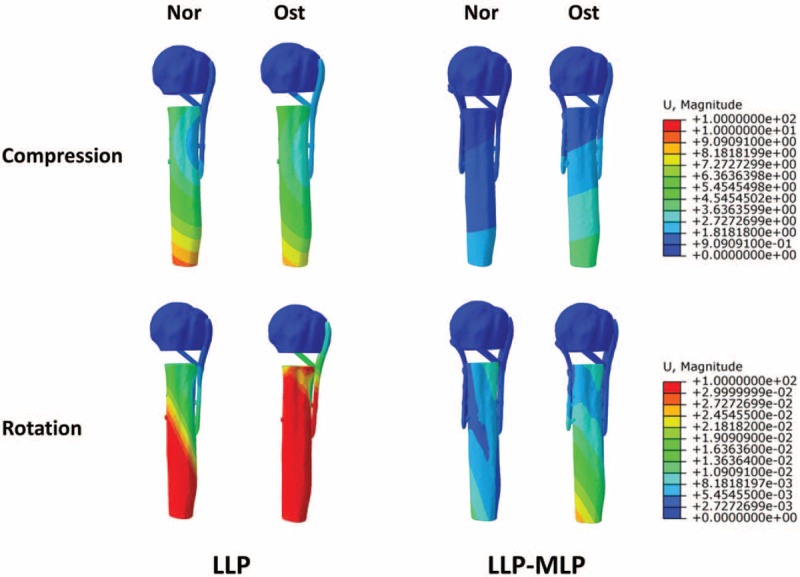
The distribution of displacements of the humerus under different conditions.
In illustrative case, the quantity and placement of locking screws were not same as finite element analysis because of different fractures. The LLP was fixed to the lateral proximal humerus with 2 parallel proximal, 2 crossed proximal, 2 distal locking screws, and 1 cortical screw. The MLP was fixed to the medial proximal humerus with 3 proximal and 2 distal locking screws.
Postoperative anteroposterior radiographs (Fig. 9) showed the successful application of LLP-MLP fixation to treat the proximal humeral fracture. After 6 months, the anteroposterior radiographs and range of motion were shown in Figures 10 and 11. The patient had not experienced any complications, such as varus malunion, screw cutout, nonunion, device failure, or avascular necrosis.
FIGURE 8.
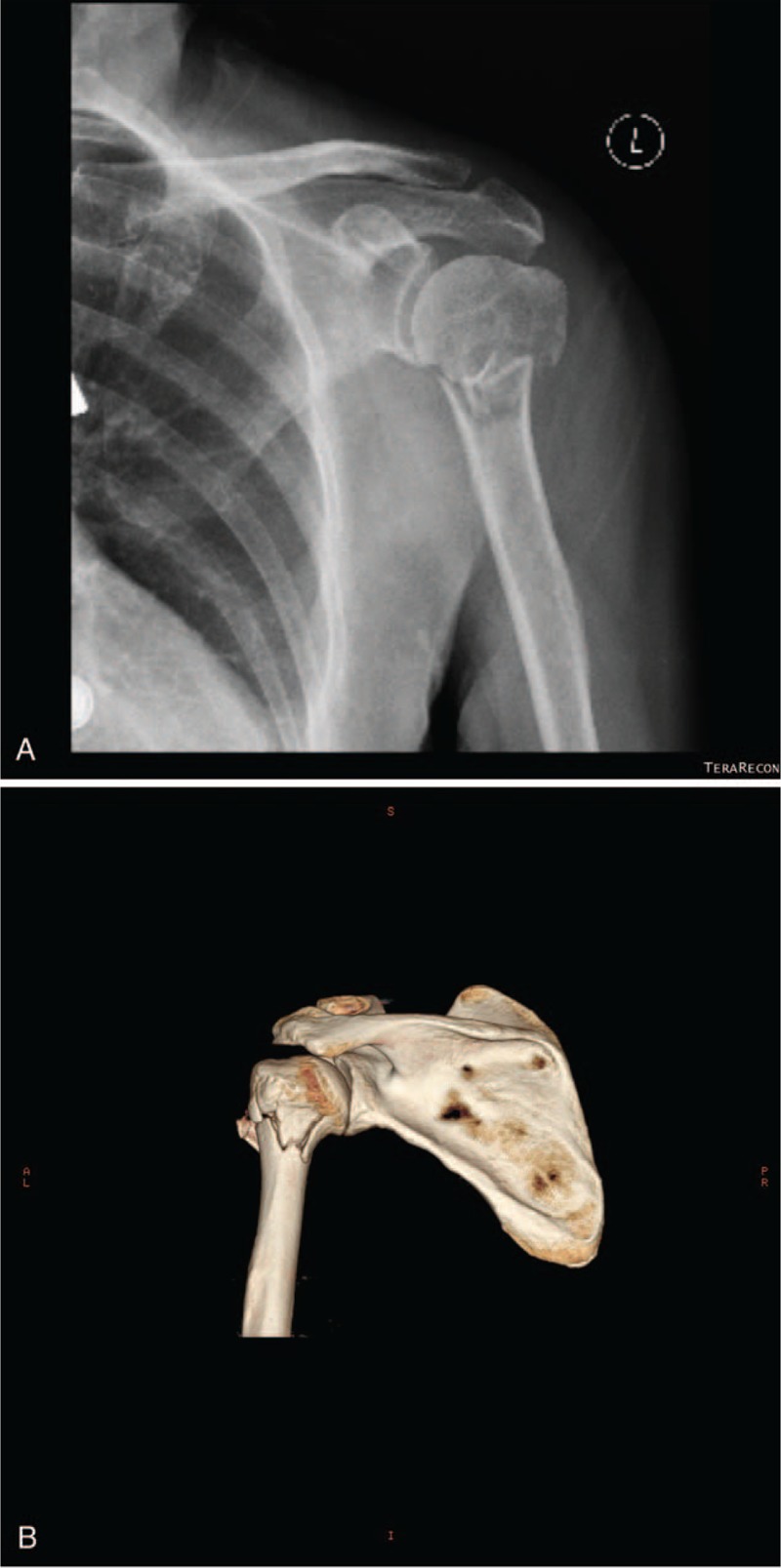
A 62-year-old female patient sustained a proximal humerus fracture with an unstable medial column after falling. (A, B) Preoperative anteroposterior radiographs and computed tomography (CT) scanning were performed.
FIGURE 9.

The postoperative anteroposterior radiograph shows the application of the LLP and MLP. LLP = lateral locking plate, MLP = medial locking plate.
FIGURE 10.

The radiographic data at 6 months after the operation.
DISCUSSION
Although the lateral locking plate technique was developed to treat proximal humeral fractures, the procedure has a surprizingly high rate of complications. A systematic review by Sproul et al14 reported that the rate of complications was 49%, with varus malunion being the most common complication. Especially for patients with osteoporosis, the complications occurred more frequently.19,20 From the biomechanical perspective, the LLP provides rigid lateral fixation, direct partial rotational stability, and indirect medial buttressing. Combining LLP with MLP should theoretically improve the stability of the medial column and rotation. However, no previous studies have determined the medial column stability of the proximal humerus after treatment with LLP-MLP. Therefore, the aim of the present study was to determine the fracture stability and implant stress after treatment with LLP and LLP-MLP.
Implant Stress
The maximum axial compression von Mises stress on the LLP implant was 2251.0 MPa. The proximal and distal locking screws, which are the most likely sites for failure after internal fixation, withstood the highest stresses. The maximum von Mises stress was decreased to 546.5 MPa after in the LLP-MLP method. This result shows that the MLP distributes the stress on the LLP, which may reduce the risk of implant failure, possibly by transferring the loads through both the lateral and medial pathways (Fig. 12). Similar results were also found in the other loading conditions.
FIGURE 11.
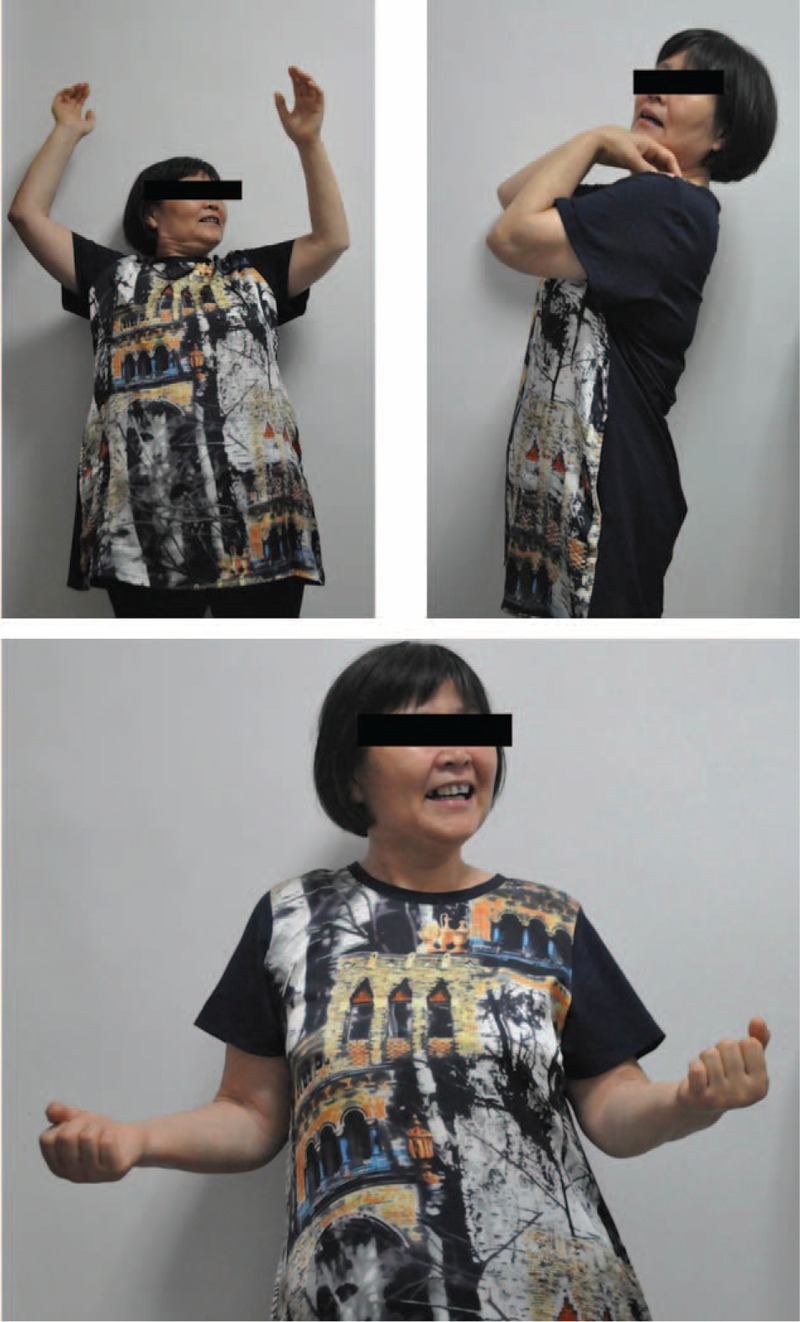
The range of motion at 6 months after the operation.
FIGURE 12.
Lateral locking plate and medial locking plate (LLP-MLP) fixation provides both lateral and medial support, and loads are transferred through both the lateral and medial pathways.
Although the calcar screws were heavily loaded after LLP treatment, the stress on the calcar screws was decreased when using the LLP-MLP method. Calcar screws mainly provide medial support,21 suggesting that the medial support function of the calcar screws was largely replaced by the MLP during treatment with LLP-MLP. Thus, the data suggest that MLP provides strong medial support and the use of calcar screws may not be necessary for LLP-MLP.
Fracture Displacements and Construct Stiffness
Fracture displacement is one measure of the stability of the fracture region. The results reported here showed that the use of the MLP significantly decreased the amount of displacement in abduction, adduction, flexion, extension, axial compression, and internal and external rotation. The amount of displacement during axial compression was decreased by 85.4% on average with LLP-MLP compared with LLP alone. The displacements of point a, which represents the stability of the medial column, was particularly affected. When simulating activities, the displacements of point a were decreased by 60.0%, indicating that the stability of the medial column was improved and suggesting that the incidence of varus malunion may be decreased with LLP-MLP fixation. Similar results were found for points b, c, and d. This result was supported by the construct stiffness results. Together, they indicate that LLP-MLP provides more construct stability than LLP alone, and increased stability is beneficial for fracture healing. Another advantage of strong fixation using LLP-MLP is that patients can perform exercise earlier after surgery to recover as much shoulder joint function as possible.
An interesting phenomenon became apparent based on the distribution of the displacements measured during compression and rotation. After LLP fixation, the distal locking screws acted as a pivot point under loading, creating instability in the medial column (Fig. 7). This interesting phenomenon was not present after LLP-MLP fixation, which stabilized the medial column.
Normal and Osteoporotic Bone
In the Ost condition, the displacements of the fracture zone and the stress on the LLP and MLP implants were increased compared with those measured in the Nor condition, illustrating that osteoporosis changes the biomechanical properties of the fixation. As was found for Nor, the displacements and the maximum von Mises stress were decreased when using LLP-MLP compared with LLP. However, other results were unexpected. During shoulder abduction and adduction, the displacements of point b, c, and d were larger in LLP-MLP than LLP fixation. A weak antipullout strength between the screws and Ost may explain this unexpected result. Because the force direction is parallel to the long axis of the screws during shoulder joint abduction and adduction, the screws have a tendency to be pulled out, making the fracture region unstable. In addition, the shape and thickness of the Ost were very different than those of Nor. In the present study, we only changed the elastic modulus of the tissue to simulate Ost, but did not adjust the shape or thickness of the model. This is certainly 1 limitation of the study; however, we created the osteoporotic model according to other relevant finite element researches.18,22–26 Therefore, the conclusions should be further studied using biomechanical testing to determine the feasibility for the osteoporosis. As a precaution, this new technology should not be performed in the severe osteoporotic patients.
Illustrative Case
The radiologic data from this case showed that the line of force of the fracture was not bad and that conservative treatment would be acceptable. However, the patient strongly desired to have surgery to return to her normal life, leading us to decide to perform an internal fixation. The LLP-MLP fixation provides more support for the medial column of the proximal humerus than LLP fixation. The medial approach provides the operator a clear view of the medial column to perform reduction and bone grafting in severe cases. Because the finite element method results indicated that the calcar screws were unnecessary with LLP-MLP, we did not instrument the calcar screws in this illustrative case. Moreover, placing the calcar screws increases the surgical trauma because the deltoid muscle must be cut. For the MLP, using 5 screws in 2 planes is enough because the main effect is medial support.
With respect to the shoulder contracture, this new technique was applied on a small number of patients which is a limitation of our study. According to the existing results, it remains unknown whether this new technology would lead to shoulder stiffness. This question may be resolved by retrospective analysis of a large number patient in further research.
However, the medial approach is not easy to learn because of the complex anatomy of the neurovascular structures. Obviously, the surgeon must be very familiar with the regional anatomy and operate carefully to avoid iatrogenic injury to the nerves and blood vessels. Moreover, LLP-MLP combination was applied in a few patients, and larger studies must be investigated before this new method can be recommended.
CONCLUSIONS
Treatment of proximal humeral fractures with an unstable medial column using LLP and MLP is feasible. Compared with LLP alone, the LLP-MLP fixation provides strong support for the medial column and enhances the stability of the fracture region, which may reduce the incidence of varus malunion. Another benefit of the rigid fixation is that patients can engage in functional exercises earlier after surgery to reduce the incidence of shoulder ankylosis.
Footnotes
Abbreviations: CT = computed tomography, HU = Hounsfield units, LLP = lateral locking plate, LLP-MLP = lateral locking plate and medial locking plate, MLP = medial locking plate, Nor = normal bone, Ost = osteoporotic bone.
YH and JH contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res 2006; 442:100–108. [DOI] [PubMed] [Google Scholar]
- 2.Kristiansen B, Barfod G, Bredesen J, et al. Epidemiology of proximal humeral fractures. Acta Orthop 1987; 58:75–77. [DOI] [PubMed] [Google Scholar]
- 3.Huttunen TT, Launonen AP, Pihlajamäki H, et al. Trends in the surgical treatment of proximal humeral fractures–a nationwide 23-year study in Finland. BMC Musculoskelet Disord 2012; 13:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mihara K, Tsutsui H, Suzuki K, et al. New intramedullary nail for the surgical neck fracture of the proximal humerus in elderly patients. J Orthop Sci 2008; 13:56–61. [DOI] [PubMed] [Google Scholar]
- 5.Zhu Y, Lu Y, Wang M, et al. Treatment of proximal humeral fracture with a proximal humeral nail. J Shoulder Elbow Surg 2010; 19:297–302. [DOI] [PubMed] [Google Scholar]
- 6.Ricchetti ET, DeMola PM, Roman D, et al. The use of precontoured humeral locking plates in the management of displaced proximal humerus fracture. J Am Acad Orthop Surg 2009; 17:582–590. [DOI] [PubMed] [Google Scholar]
- 7.Plecko M, Kraus A. Internal fixation of proximal humerus fractures using the locking proximal humerus plate. Oper Orthop Traumatol 2005; 17:25–50. [DOI] [PubMed] [Google Scholar]
- 8.Kontakis G, Koutras C, Tosounidis T, et al. Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br 2008; 90:1407–1413. [DOI] [PubMed] [Google Scholar]
- 9.Vallier HA. Treatment of proximal humerus fractures. J Orthop Trauma 2007; 21:469–476. [DOI] [PubMed] [Google Scholar]
- 10.Ring D. Current concepts in plate and screw fixation of osteoporotic proximal humerus fractures. Injury 2007; 38:59–68. [DOI] [PubMed] [Google Scholar]
- 11.Südkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. J Bone Joint Surg 2009; 91:1320–1328. [DOI] [PubMed] [Google Scholar]
- 12.Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma 2009; 23:163–172. [DOI] [PubMed] [Google Scholar]
- 13.Lee CW, Shin SJ. Prognostic factors for unstable proximal humeral fractures treated with locking-plate fixation. J Shoulder Elbow Surg 2009; 18:83–88. [DOI] [PubMed] [Google Scholar]
- 14.Sproul RC, Iyengar JJ, Devcic Z, et al. A systematic review of locking plate fixation of proximal humerus fractures. Injury 2011; 42:408–413. [DOI] [PubMed] [Google Scholar]
- 15.Gardner MJ, Weil Y, Barker JU, et al. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma 2007; 21:185–191. [DOI] [PubMed] [Google Scholar]
- 16.Osterhoff G, Ossendorf C, Wanner GA, et al. The calcar screw in angular stable plate fixation of proximal humeral fractures–a case study. J Orthop Surg Res 2011; 6:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bai L, Fu Z, An S, et al. Effect of calcar screw use in surgical neck fractures of the proximal humerus with unstable medial support: a biomechanical study. J Orthop Trauma 2014; 28:452–457. [DOI] [PubMed] [Google Scholar]
- 18.Turner AWL, Gillies RM, Sekel R, et al. Computational bone remodelling simulations and comparisons with DEXA results. J Orthop Res 2005; 23:705–712. [DOI] [PubMed] [Google Scholar]
- 19.Hsiao PC, Chen TJ, Li CY, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: a population-based cohort study. Medicine 2015; 94:e532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wähnert D, Hofmann-Fliri L, Richards RG, et al. Implant augmentation: adding bone cement to improve the treatment of osteoporotic distal femur fractures: a biomechanical study using human cadaver bones. Medicine 2014; 93:e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner MJ, Boraiah S, Helfet DL, et al. Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma 2008; 22:195–200. [DOI] [PubMed] [Google Scholar]
- 22.Liang D, Ye LQ, Jiang XB, et al. Biomechanical effects of cement distribution in the fractured area on osteoporotic vertebral compression fractures: a three-dimensional finite element analysis. J Surg Res 2015; 195:246–256. [DOI] [PubMed] [Google Scholar]
- 23.Chen SH, Chiang MC, Hung CH, et al. Finite element comparison of retrograde intramedullary nailing and locking plate fixation with/without an intramedullary allograft for distal femur fracture following total knee arthroplasty. Knee 2014; 21:224–231. [DOI] [PubMed] [Google Scholar]
- 24.Li Y, Liu ZS, Bai XM, et al. Investigation of the effects of graded models on the biomechanical behavior of a bone-dental implant system under osteoporotic conditions. Pak J Med Sci 2013; 29:619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amirouche F, Solitro G, Broviak S, et al. Primary cup stability in THA with augmentation of acetabular defect. A comparison of healthy and osteoporotic bone. Orthop Traumatol Surg Res 2015; (in press). [DOI] [PubMed] [Google Scholar]
- 26.Polikeit A, Nolte LP, Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine 2003; 28:991–996. [DOI] [PubMed] [Google Scholar]


