Abstract
Tyrosine kinase inhibitors (TKIs) of epidermal growth factor receptor (EGFR) were previously the standard first-line treatments for lung cancers with activating EGFR mutations. The first-generation reversible EGFR TKIs, gefitinib and erlotinib, demonstrated substantial efficacy in the treatment of brain metastases from EGFR-mutated lung adenocarcinoma. However, the efficacy of afatinib, the second-generation irreversible EGFR TKI, as the first-line treatment in lung adenocarcinoma patients with brain metastasis has yet to be evaluated.
Here, we report cases of 3 patients who received afatinib alone as the first-line treatment in combination with whole-brain radiotherapy or following surgical resection of brain metastases. All 3 patients had EGFR L858R mutation. The first patient had lung adenocarcinoma with brain metastasis and no neurologic symptoms. After consultation, she received afatinib as a first-line treatment. Chest computed tomography and brain magnetic resonance imaging (MRI) showed partial response. The second patient had lung adenocarcinoma accompanied with a metastatic brain lesion associated with seizures. This patient received whole-brain radiotherapy and afatinib treatment following brain MRI and subsequently showed significant regression of the brain metastasis. The third patient had strabismus of the right eye, and brain MRI showed a single tumor at the cerebellar pontine angle. This patient underwent surgical resection of the tumor followed by afatinib treatment. He refused adjuvant radiotherapy after surgery for brain metastasis. The brain MRI showed no recurrent brain metastasis, and the patient had relatively less neurologic deficiency.
This series of 3 cases indicate that afatinib may be an appropriate first-line treatment alternative in patients having lung adenocarcinoma with EGFR mutations. Further retrospective analyses and prospective clinical trials are required to substantiate the efficacy of afatinib in the treatment of brain metastases of lung adenocarcinoma.
INTRODUCTION
Lung adenocarcinoma patients with epidermal growth factor receptor (EGFR) mutations generally respond well to EGFR tyrosine kinase inhibitors (TKIs).1 A proportion of these patients are found to have brain metastases at the time of lung adenocarcinoma diagnosis. Before the introduction of EGFR TKIs, only few cases of lung cancer were suitable for surgical resection and most patients needed brain radiotherapy before EGFR TKIs were used in lung cancer patients.2 Early relapse or dementia happened in the patients who received local intent or whole-brain radiotherapy. In the past 10 years, the first-generation EGFR TKIs have demonstrated impressive efficacy in the treatment of brain metastases originating from lung adenocarcinomas with EGFR mutations.3–5 EGFR TKIs can be used as first-line treatment without the need for immediate brain radiotherapy. Furthermore, brain radiotherapy can be performed later in patients resistant to EGFR TKIs.
Afatinib, the second-generation EGFR TKI, is an irreversible pan-human epidermal growth receptor TKI approved for the treatment of lung adenocarcinoma with EGFR mutations. LUX-LUNG 3 and LUX-LUNG 6 studies demonstrated increased progression free survival (PFS) with afatinib treatment. Hoffknecht et al,6 as part of the Afatinib Compassionate Use Consortium (ACUC), reported cerebral responses to afatinib treatment in 35% (11 of 31) of patients who were followed up with at least one cycle of chemotherapy and an EGFR TKI. To date, there have been no reports of clinical trials or case series demonstrating the efficacy of afatinib as a first-line treatment of lung adenocarcinoma with activating EGFR mutations and active brain metastases.
Substantial disease control has been observing in this case series concerning patients with varying clinical presentations indicating that afatinib may have efficacy as a first-line treatment for brain metastases resulting from lung adenocarcinoma with EGFR mutations.
CASE SERIES
Case A
A 61-year-old female with pleural effusion underwent computed tomography (CT) on March 29, 2015. CT revealed a number of lung nodules in addition to pleural effusion. Cellblock cytology confirmed the pulmonary lesions to be adenocarcinoma, and EGFR L858R (substitution at position 858 from a leucine to arginine) mutation was identified. PET-MRI (positron emission tomography-magnetic resonance imaging) revealed multiple lung, brain, bone, and liver metastases. The patient had no neurological symptoms despite multiple brain metastases observed on MRI (Figure 1A–D). After discussions with the patient and family, treatment with afatinib, instead of erlotinib or gefitinib, was initiated. Whole-brain radiotherapy was not performed because of the absence of neurological symptoms and its potential side effects. The patient received afatinib (40 mg/d) from April 23, 2015. Brain MRI (Figure 1E–H) and whole body CT showed marked regression of the brain metastatic lesions, metastatic liver nodules, and primary lung tumor on June 27, 2015, representing a partial response following afatinib treatment for 2 months. A good cerebral response to afatinib was observed in this case.
FIGURE 1.
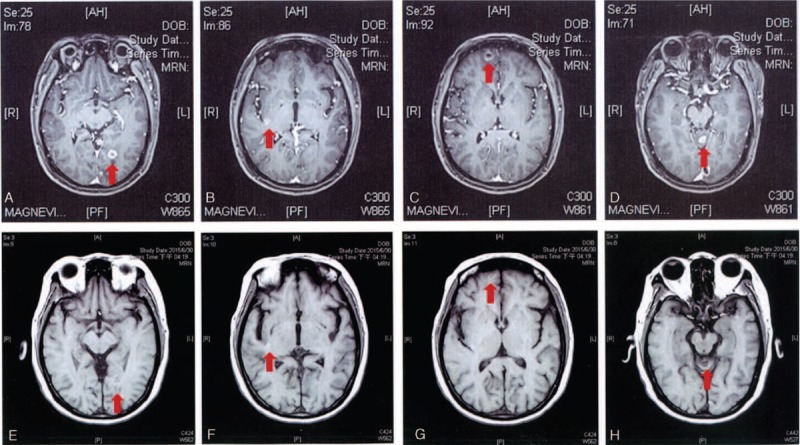
Brain MRI showing multiple metastatic brain lesions in case A (panels 1A to 1D). Regression of multiple brain metastases was observed after treatment with afatinib for >2 months (panels 1E to 1H). MRI, magnetic resonance imaging.
The findings of this case indicate the efficacy of afatinib as a first-line treatment in selected lung adenocarcinoma patients with brain metastases and no neurological symptoms.
Case B
A 52-year-old male was found to have a 2 cm nodule in the left upper lung and a brain lesion at the left periventricular region superior to left thalamus (Figure 2A and B). Histological examination of a CT-guided biopsy of the left lung nodule showed adenocarcinoma in February 2015. An L858R mutation was identified by EGFR genotype analysis. Bone scanning revealed no evidence of bone metastasis. The patient had a seizure attack for the first time during this admission. Whole-brain radiotherapy was performed with a total 30 Gray delivered in 10 fractions and afatinib 40 mg/d initiated following the diagnosis of lung adenocarcinoma with brain and mediastinal lymph node metastases. Following treatment with afatinib for 3 months, chest CT on May 16, 2015, showed regression of the lung tumor and metastatic mediastinal lymph nodes. Brain MRI on June 24, 2015, showed regression of brain metastases following afatinib treatment and whole-brain radiotherapy (Figure 2C and D). A significant cerebral response to combined systemic treatment with afatinib and whole-brain radiotherapy was observed in this case.
FIGURE 2.
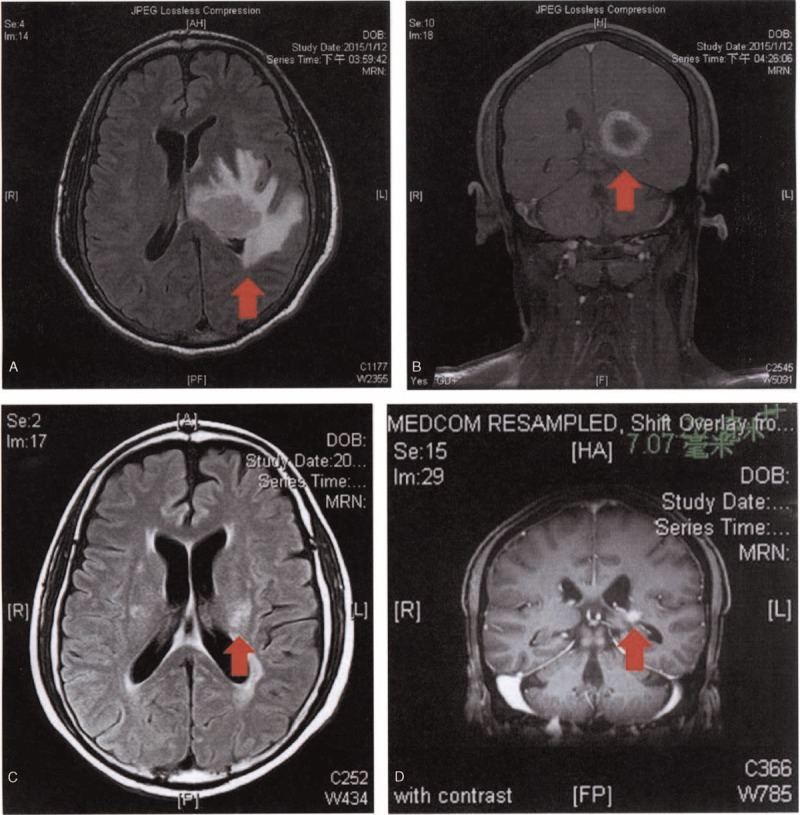
Brain MRI in case B showing brain metastases with mass effect (panels 2A and 2B). Marked regression of metastatic brain lesion on brain MRI following brain radiotherapy and afatinib treatment for 4 months (panels 2C and 2D). MRI, magnetic resonance imaging.
The findings of this case indicate the efficacy of afatinib treatment and brain radiotherapy in lung adenocarcinoma patients with brain metastases and neurological symptoms.
Case C
A 55-year-old male smoker with no previous history of systemic disease was diagnosed with lung cancer. The patient reported back pain for several weeks before the development of strabismus in November 2014. Brain MRI identified a right petroclival tumor (Figure 3A). Angiography revealed the presence of a suspected meningioma in the right petroclival region. The strabismus was found to be due to abducens nerve palsy. The patient underwent surgical resection with pathological examination showing a TFF-1-positive metastatic adenocarcinoma. Chest CT (Figure 3B and C) and bone scanning showed the presence of a tumor in the left lower lung with multiple bone and lung-to-lung metastases. Genotyping identified L858R EGFR mutation of the metastatic brain tumor. Brain radiotherapy and afatinib therapy were arranged following discussions with the patient and his family. The patient received afatinib treatment at our outpatient clinic. Brain radiotherapy was refused. Brain CT found no evidence of brain metastasis recurrence on January 23, 2015. Chest CT showed a partial response of the lung cancer to treatment on May 15, 2015 (Figure 3E and F). Brain MRI found no evidence of brain metastasis recurrence on May 23, 2015 (Figure 3D). Strabismus persisted, but the patient reported improvement of his visual field. The patient initially required bed rest, but was able to walk unaided following afatinib treatment for 3 months.
FIGURE 3.
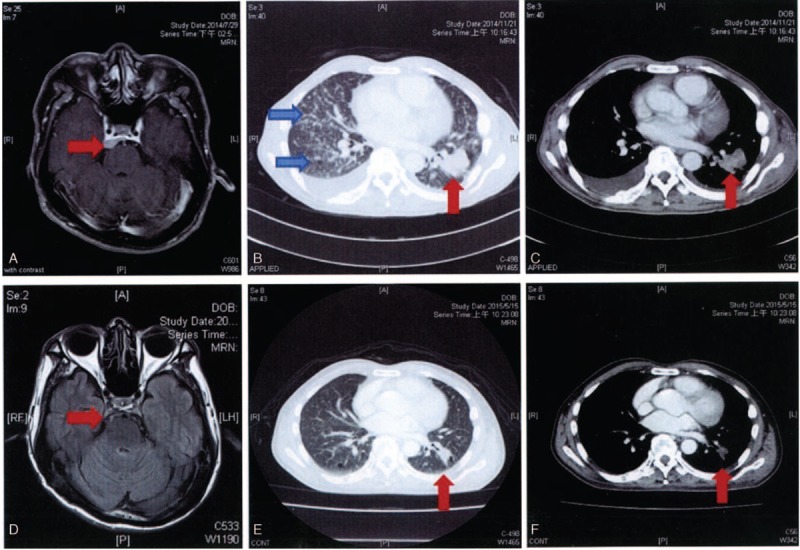
Meningeal metastases in the cerebropontin area in case C (panel 3A). Chest CT revealed a tumor located in the left lower lung and multiple interstitial infiltrations (panels 3B and 3C). Chest CT showed a partial response after afatinib treatment for 7 months. Brain MRI found no evidence of recurrence following afatinib treatment for 9 months. CT, computed tomography; MRI, magnetic resonance imaging.
The findings of this case indicate the efficacy of 6 months afatinib treatment in a lung adenocarcinoma patient with a single meningeal metastasis without the development of recurrence.
Ethics Statement
This was a retrospective study of reviewed medical charts. Additional informed consent was not required for a retrospective review of medical charts. Patient information, including names and chart numbers, were deleted for de-identification before data analyses. Patient confidentiality was ensured at all times. The design of this study was approved by the institutional Review Board of the Chang Gung Medical Foundation (IRB No. 103-2502B).
DISCUSSION
Our case series provides information regarding the efficacy of afatinib as a first-line treatment for lung adenocarcinoma with brain metastases and EGFR mutations. The 3 cases presented herein had different clinical presentations that were largely representative of the majority of lung adenocarcinoma patients with brain metastases. The first case of a patient having a lung adenocarcinoma with multiple brain metastases, but no neurological symptoms demonstrated an excellent response to first-line afatinib treatment. The second case demonstrated a good response of primary and metastatic lesions to combined systemic afatinib treatment and brain radiotherapy in a patient with neurological symptoms. The third case demonstrated the use of first-line afatinib treatment following surgical resection of meningeal metastasis. To date, there have been no reported retrospective studies or prospective clinical trials of first-line afatinib treatment in cases of lung adenocarcinoma with brain metastases. Our case series provides information regarding the efficacy of first-line afatinib in selected cases of lung adenocarcinoma with brain metastases.
Herein, as we report only 3 cases, further studies are required to fully demonstrate the efficacy of first-line afatinib in achieving cerebral responses. Hoffknecht et al6 from the ACUC reported a 31% cerebral response rate in patients who had received at least one cycle of chemotherapy and at least one EGFR TKI, providing further evidence of the efficiency of afatinib treatment in patients with brain metastases.6 Patients received afatinib as the third-line treatment or greater. The cerebral response rate reported by Hoffknecht et al may have been higher if afatinib had been used as the first-line treatment before the development of resistance to chemotherapy and prior EGFR TKI therapy.3,7,8 The ACUC study reported good cerebral responses to afatinib, although the included patients had been treated with EGFR TKI and chemotherapybefore afatinib treatment.6 Our case series provides evidence of the efficacy of first-line afatinib in lung adenocarcinoma patients with brain metastases. Further studies including greater numbers of patients are required to confirm our findings and provide a rationale for future prospective studies.
The low cerebrospinal fluid (CSF) concentration of reversible first-generation EGFR TKIs may be responsible for the high rates or recurrence and progression observed with these pharmacological agents.4,9,10 The higher CSF concentration obtained with erlotinib led to its consideration as a treatment for brain metastases in patients with EGFR-mutated lung cancer.3,4,9,10 Pulsed high doses of EGFR TKIs are recommended in lung adenocarcinoma patients with resistance to previous EGFR TKI therapy, although there is a lack of clinical trials providing evidence to support this recommendation.4,10,11 Afatinib has been shown to have a lower IC50 than the reversible first-generation EGFR TKI in in vitro studies.6 Hoffknecht et al reported 2 cases from the ACUC study. The first patient had a CSF afatinib concentration of approximately 1 nM. A concentration of 1 nM is higher than the IC50 for lung cancer cell lines with EGFR L858R mutation or deletion of EGFR exon 19. The second patient received afatinib 50 mg/d as a third-line treatment. The dose was increased to 60 mg/d at 9 months and then 70 mg/d at 12 months. The patient had rapid progression following 6 months of afatinib 70 mg/d and received afatinib treatment for a total of 16 months. The subgroup analyses of patients with brain metastases in the ACUC study provided evidence of the efficacy of afatinib in the treatment of brain metastases from lung adenocarcinoma.
The LUX-LUNG 3 and LUX-LUNG 6 studies reported increased PFS compared with previous clinical trials of first-generation reversible EGFR TKIs. A lack of studies of afatinib, a newly approved EGFR TKI for lung cancer, in lung cancer patient with brain metastases has limited the clinical application of afatinib in these patients. The ACUC study and a small number of case reports have demonstrated the efficacy of afatinib in lung cancer patients with resistance to reversible EGFR TKIs. Afatinib may have similar or greater efficacy in the treatment of metastatic brain lesions in patients with lung adenocarcinoma. The findings of the 3 clinical cases presented herein indicate afatinib may represent an efficacious first-line treatment for patients with brain metastases from lung adenocarcinoma.
The combination of afatinib with radiotherapy or surgery may provide better control of brain metastases from lung adenocarcinoma.8,12–14 Metastasectomy of solitary brain metastases resulted in better or the same survival in a number of studies of erlotinib. The third case in this series had no recurrence of meningeal metastasis following surgery and afatinib treatment. Combination of surgery and afatinib may represent a valid option in select patients with solitary brain metastasis. The addition of erlotinib to whole-brain radiotherapy has been shown to result in similar response rates but reduced recurrence of brain metastases. A proportion of patients with brain metastases and no neurological symptoms receive EGFR TKI alone due to the side effects of whole-brain radiotherapy. The first case in this series had no neurological symptoms from multiple brain metastases and had a good cerebral response to afatinib alone. The second case in the present series had developed seizures and received whole-brain radiotherapy and afatinib treatment accordingly. Brain MRI in these cases showed a good response to combination of afatinib and radiotherapy. Depending on the results of clinical trials or case reports of the use of erlotinib and afatinib, afatinib plus brain radiotherapy or surgery may represent a reasonable choice in the treatment of EGFR-mutated lung cancer with brain metastases.
CONCLUSION
Afatinib has efficacy in the treatment of EGFR-mutated lung adenocarcinoma with brain metastases. The ACUC study proved a role for afatinib in the treatment of brain metastases from lung adenocarcinoma in patients with resistance to prior EGFR TKI therapy and chemotherapy. The findings of this case series indicate the use of afatinib alone or in combination with radiotherapy or surgery has efficacy in a range of clinical presentations of EGFR-mutated lung adenocarcinoma with brain metastases.
Acknowledgments
The authors thank the research grant from Chang Gung Memorial Hospital, Taiwan (CMRPG 3D1911) for funding.
Footnotes
Abbreviations: CSF = cerebrospinal fluid, CT = computed tomography, EGFR = epidermal growth factor receptor, L858R = substitution at position 858 from a leucine to arginine, MRI = magnetic resonance imaging, PFS = progression free survival, TKI = tyrosine kinase inhibitor.
S-HL and M-HH contributed equally to this work as first authors.
This project was supported by the research grant from Chang Gung Memorial Hospital, Taiwan (CMRPG 3D1911).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Hsieh MH, Fang YF, Chang WC, et al. Complex mutation patterns of epidermal growth factor receptor gene associated with variable responses to gefitinib treatment in patients with non-small cell lung cancer. Lung Cancer 2006; 53:311–322. [DOI] [PubMed] [Google Scholar]
- 2.Lin NU. Targeted therapies in brain metastases. Curr Treat Options Neurol 2014; 16:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee E, Keam B, Kim DW, et al. Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non-small-cell lung cancer. J Thorac Oncol 2013; 8:1069–1074. [DOI] [PubMed] [Google Scholar]
- 4.Clarke JL, Pao W, Wu N, et al. High dose weekly erlotinib achieves therapeutic concentrations in CSF and is effective in leptomeningeal metastases from epidermal growth factor receptor mutant lung cancer. J Neurooncol 2010; 99:283–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yi HG, Kim HJ, Kim YJ, et al. Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are effective for leptomeningeal metastasis from non-small cell lung cancer patients with sensitive EGFR mutation or other predictive factors of good response for EGFR TKI. Lung Cancer 2009; 65:80–84. [DOI] [PubMed] [Google Scholar]
- 6.Hoffknecht P, Tufman A, Wehler T, et al. Efficacy of the irreversible ErbB family blocker afatinib in epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI)-pretreated non-small-cell lung cancer patients with brain metastases or leptomeningeal disease. J Thorac Oncol 2015; 10:156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang J, Yu J, Sun X, et al. Epidermal growth factor receptor tyrosine kinase inhibitors in the treatment of central nerve system metastases from non-small cell lung cancer. Cancer Lett 2014; 351:6–12. [DOI] [PubMed] [Google Scholar]
- 8.D’Antonio C, Passaro A, Gori B, et al. Bone and brain metastasis in lung cancer: recent advances in therapeutic strategies. Ther Adv Med Oncol 2014; 6:101–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng Y, Feng W, Wu J, et al. The concentration of erlotinib in the cerebrospinal fluid of patients with brain metastasis from non-small-cell lung cancer. Mol Clin Oncol 2014; 2:116–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hata A, Kaji R, Fujita S, et al. High-dose erlotinib for refractory brain metastases in a patient with relapsed non-small cell lung cancer. J Thorac Oncol 2011; 6:653–654. [DOI] [PubMed] [Google Scholar]
- 11.Kuiper JL, Smit EF. High-dose, pulsatile erlotinib in two NSCLC patients with leptomeningeal metastases—one with a remarkable thoracic response as well. Lung Cancer 2013; 80:102–105. [DOI] [PubMed] [Google Scholar]
- 12.Li L, Liu LY, Chen M, et al. A pilot study of conformal radiotherapy combined with erlotinib-based multimodality therapy in newly diagnosed metastatic non-small-cell lung cancer. Eur Rev Med Pharmacol Sci 2015; 19:1812–1820. [PubMed] [Google Scholar]
- 13.Lee SM, Lewanski CR, Counsell N, et al. Randomized trial of erlotinib plus whole-brain radiotherapy for NSCLC patients with multiple brain metastases. J Natl Cancer Inst 2014; 19:dju151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerber NK, Yamada Y, Rimner A, et al. Erlotinib versus radiation therapy for brain metastases in patients with EGFR-mutant lung adenocarcinoma. Int J Radiat Oncol, Biol, Phys 2014; 89:322–329. [DOI] [PMC free article] [PubMed] [Google Scholar]


