Abstract
Traditionally, major complications and unanticipated admission/readmission rates were used to assess outcome after day surgery. However, in view of the relative absence of major complications the quality of recovery (QOR) should be considered one of the principal endpoints after day surgery. In our study, the level of QOR is defined by a combination of the Global Surgical Recovery (GSR) Index and the Quality of Life (QOL).
The aim of this study was to analyze prevalence and predictors of QOR after day surgery on the fourth postoperative day.
Elective patients scheduled for day surgery from November 2008 to April 2010 were enrolled in a prospective cohort study. Outcome parameters were measured by using questionnaire packages at 2 time points: 1 week preoperatively and 4 days postoperatively. Primary outcome parameter is the QOR and is defined as good if the GSR index >80% as well as the postoperative QOL is unchanged or improved as compared with baseline. QOR is defined as poor if both the GSR index ≤80% and if the postoperative QOL is decreased as compared with baseline. QOR is defined as intermediate in all other cases. Three logistic regression analyses were performed to determine predictors for poor QOR after day surgery.
A total of 1118 patients were included. A good QOR was noted in 17.3% of patients, an intermediate QOR in 34.8%, and a poor QOR in 47.8% 4 days after day surgery. The best predictor for poor QOR after day surgery was type of surgery. Other predictors were younger age, work status, and longer duration of surgery. A history of previous surgery, expected pain (by the patient) and high long-term surgical fear were significant predictors of poor QOR in only 1 of 3 prediction models.
The QOR at home 4 days after day surgery was poor in the majority of patients and showed a significant procedure-specific variation. Patients at risk for poor QOR can be identified during the preoperative period based on type of surgery, age, work status, and the duration of the surgery.
INTRODUCTION
Nowadays, more than 50% of elective surgery is performed in an outpatient setting.1 Traditionally, major complications and unanticipated admission/readmission rates were used to assess outcome after day surgery.2–4 However, improvements in surgical and anesthetic techniques have resulted into low mortality and morbidity and low unanticipated admission/readmission rates.5–7
In view of the relative absence of major complications, the present evaluation of day surgery is based on the quality of recovery (QOR).8 The QOR is related to the patient́s ability to resume normal activities after discharge at home and should be considered 1 of the principal endpoints after day surgery.7 QOR is a complex phenomenon encompassing many dimensions in physical, psychological, and social health.9 In our study, the level of QOR is defined by a combination of the Global Surgical Recovery (GSR) Index10,11 and the quality of life (QOL).12
Most patients perceive surgery in an outpatient setting as less dangerous compared with the inpatient setting13 and they also expect a good quality and fast recovery including a rapid return to work status/daily activities without suffering from moderate to severe pain.14,15 The QOR is related to the type of surgery and the recovery process. A process which starts immediately after the surgery and may take from several days to weeks and even months.9,14 It should be taken into account that postoperative surveillance by professionals following discharge is less optimal after day surgery as compared with surgery in the inpatient setting.10,16 Finally, lack of adequate information and uncertainty appears to provoke anxiety and is the most common cause of dissatisfaction with day surgery care.17
As a result, there is a need of more in-depth understanding of the variability of QOR after different types of surgery performed in an outpatient setting. In this respect, the effect of demographic, psychological, social, and perioperative factors related to the QOR after various types of surgery in the outpatient setting needs to be analyzed. An optimal characterization of these patients can lead to improvement of QOR. These improvements will not only include a better preoperative empowerment of the patient as well as an improved prediction of the time-off from work but also a minimization of the occurrence of unplanned contacts with health professionals. The QOR after day surgery will furthermore be improved due to adjustment of patient expectations15 as well as the implementation of an improved home and follow-up care schedule.18–20 In view of ambulatory surgery, self-care needs to be feasible to secure the quality of care in general and pain management in particular. In this context, the first 3 to 5 days after the surgical procedures are considered to be essential.21
Hence, the aim of this study was to analyze the prevalence and predictors of QOR at the fourth postoperative day, in a large adult population undergoing day surgery. As a final outcome of this study we aim to provide an easily applicable predictive QOR-model after day surgery.
MATERIALS AND METHODS
Patients
This prospective longitudinal cohort study was approved by the Institutional Ethics Committee of the Maastricht University Medical Center+, and all patients gave informed consent to participate. All patients undergoing day surgery were eligible to participate, regardless of the type of surgery. Exclusion criteria were patients age <18 years, inability to express themselves, visual dysfunction, or insufficient understanding of the Dutch language.
Questionnaires
Patients were asked to complete 2 successive questionnaire packages.
First, a baseline questionnaire package was used to measure demographics (eg, age, gender, educational level, work) and baseline QOL. The EuroQol (EQ-5D) questionnaire was used to analyze QOL on 5 dimensions (ie, mobility, self-care, usual activity, pain/discomfort, and anxiety/depression).12 Furthermore, psychological variables were analyzed based on 3 validated questionnaires: the Pain Catastrophizing Scale (PCS), the Life Orientation Test Revised (LOT-R), and Surgical Fear Questionnaire (SFQ). For the PCS and LOT-R, shortened versions were used to keep the total number of questions within limits and thus avoiding patient refusal due to long questionnaires (ie, diminishing patient burden). In the PCS questionnaire, to measure catastrophic thinking, 6 of the 13 original items were used. These were 2 questions loading highest on each of the 3 subscales (ie, Items 5 and 12 for helplessness, Items 9 and 11 for rumination, and Items 6 and 13 for magnification).11,22 In the LOT-R, to measure personality trait optimism,23 4 of the originally 10 questions were used. Four filler questions were omitted and the 4 questions (2 positively phrased and 2 negatively phrased) loading highest on, respectively, the optimism and pessimism factor were selected.11 For analysis of fear of potential consequences of surgery, the 8-item SFQ was included. Within the SFQ, 4 items refer to fear of short-term consequences (eg, pain, side effects) and 4 items refer to fear of long-term consequences (eg, deterioration of health).24 Finally average and present pain intensity, the influence of pain on daily activities, analgesic use, and the number of visits to a medical doctor or other health care professionals were measured. All questions related to pain were analyzed based on an 11-point Numeric Rating Scale (NRS; where 0 = no pain, and 10 = worst pain imaginable).
Second, a follow-up questionnaire package was used to measure the 1-item GSR index and the EQ-5D. The GSR index represents a single question about the extent to which patients considered themselves to be recovered from the surgery (“if 100% recovery means your health is back to the same level as it was before the surgery, what percentage of recovery are you at now?”).10,11 In previous studies, the GSR index was measured at least 6 months after the surgery and good or near optimal GSR were defined as a GSR index of, respectively, >80% or 90%.11,25,26 In this study, good GSR is defined as a GSR index >80% and the cutoff value for poor GSR was set on a GSR index ≤ 80%. Furthermore, this questionnaire package included questions regarding average and present pain intensity related to the surgery, the influence of pain on daily activities, prescribed and over-the-counter analgesic use, the effect of analgesic use on pain severity, visits to healthcare professionals, postoperative side-effects, and complications like nausea, vomiting, wound infections.
Procedure
Between November 2008 and April 2010, patients planned for day surgery and presenting at the outpatient clinic for preoperative assessment at the Maastricht University Medical Center+ were asked to participate. If consent was obtained, the patient received an envelope containing an informative letter about the study, the 2 questionnaire packages, and 2 return envelopes. Also, the patient received a standardized prescription for postoperative analgesics (ie, acetaminophen 1000 mg 4 times a day, and if necessary, acetaminophen/tramadol 650/75 mg 4 times a day). Patients were instructed to complete the baseline questionnaire package 1 week before the surgical procedure. Patients who did not return this questionnaire package were considered to be unwilling to participate, and no further attempts to contact them were made. The follow-up questionnaire package had to be completed at the fourth day after the surgery. Patients who returned the baseline questionnaire package, but did not return the follow-up questionnaire package, were reminded by regular mail or telephone. Only patients who returned both the baseline and the follow-up questionnaire packages were included into our analyses. All clinical information (eg, ASA physical status, surgical procedure, type of anesthesia, duration of the procedure, duration of hospital stay, unplanned admission, and readmission) were acquired by systematic chart review.
Outcome Measures
The main outcome variable in this study is QOR at 4 days after day surgery. The level of the QOR is defined by a combination of both the GSR and the QOL. QOR is defined as good if both the GSR index >80%11,25 and if the postoperative QOL is unchanged or improved as compared with baseline. QOR is defined as poor if both the GSR index ≤80% and if the postoperative QOL is reduced as compared with baseline. QOR is defined as intermediate in all other cases. Prevalence in view of QOR and predictors of poor QOR are studied.
Secondary outcome variables are prevalence of reduced GSR and QOL. Pre- and postoperative pain, visits to healthcare professionals, unplanned admissions and readmissions, postoperative side-effects, and complications like nausea, vomiting, wound infections during the first 4 days after day surgery are also studied.
To compare QOR, GSR, and QOL after various types of surgery, homogenous surgical groups were created, containing at least 20 procedures.27
Statistical Analysis
First, missing data were imputed using multiple data imputation according to the method described by Van Buuren et al.28 Each missing item was imputed 10 times, leading to 10 different data sets. Only demographic, clinical, and predictive values were imputed, missing outcome parameters were not.
For all 3 statistical analyses (poor vs both intermediate and good QOR, poor vs intermediate QOR, and poor vs good QOR), a univariate logistic regression analysis was performed for each predictive variable. Only variables with a P value <0.1 were included in the final multiple logistic regression model. A stepwise forward multiple logistic regression analysis was subsequently performed to determine predictors for poor QOR. Only variables that were significant in more than halve of the imputed datasets were considered as significant predictors in the pooled regression model.
The 3 logistic regression analysis models for prediction of poor QOR were based on 4 steps. The first step contained those variables which are most easy to obtain, even before the patient visits the outpatient clinic (ie, gender, age, and surgical procedure). In a second step, variables based on items which are relatively easy to obtain during the preoperative assessment (ie, ASA-level, work status, education level, previous surgery, preoperative pain, and preoperative analgesic use) were included. The third step contained mostly psychological variables (ie, expected postoperative pain by the patient, short- and long-term surgical fear, pain catastrophizing, optimism, and preoperative QOL). The fourth step included duration of surgery and type of anesthesia. A P value of <0.05 was considered to be statistically significant. The models’ ability to discriminate between patients with and without a poor QOR was estimated by the area under the curve (AUC) for the successive blocks. All analyses were performed using SPSS version 20.0 (SPSS, Inc., Chicago, IL).
RESULTS
General Characteristics
During the study period, 2500 patients were invited to participate: 1396 patients (56%) returned the baseline questionnaire. Ninety-two percent of these patients (N = 1282) returned the follow-up questionnaire, of which 164 patients were excluded: 5 patients were younger than 18 years, 1 patient was mentally impaired, and 27 patients underwent a planned inpatient procedure. One patient was excluded due to death from a nonrelated cause, and 5 patients were excluded because of missing data on primary outcome measures. Furthermore, 125 patients were excluded as they received a surgical procedure containing <20 patients. This resulted in data of 1118 patients for the final analysis (Figure 1).
FIGURE 1.
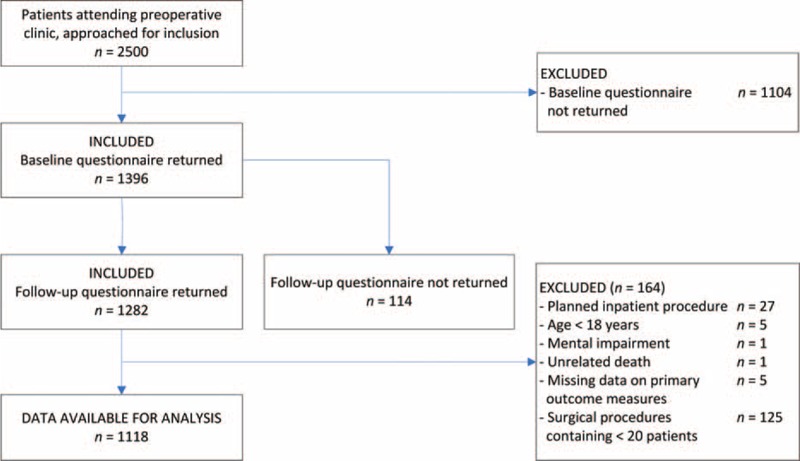
Flowchart depicting the inclusion and exclusion.
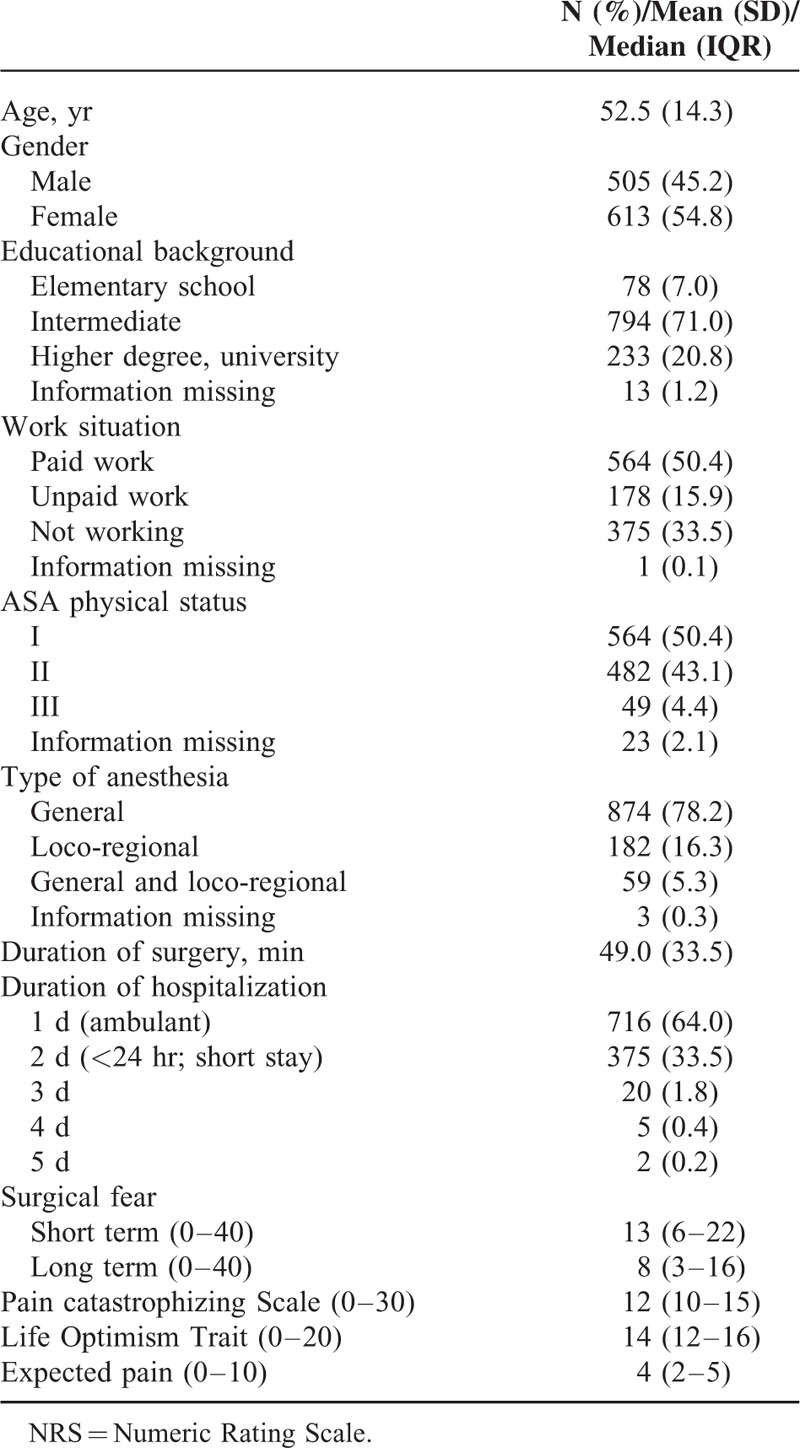
Baseline patient characteristics, including psychological parameters, are shown in Table 1. The mean age of all patients was 52.5 years (range 18–88 years). Most patients were classified as ASA I or II and 874 (78.2%) received general anesthesia, 182 (16.3%) received loco-regional anesthesia, and 59 patients (5.3%) received loco-regional anesthesia in addition to general anesthesia. The average duration of surgery was 49 min.
TABLE 1.
Baseline Patient Characteristics
Primary Outcome
Prevalence of QOR
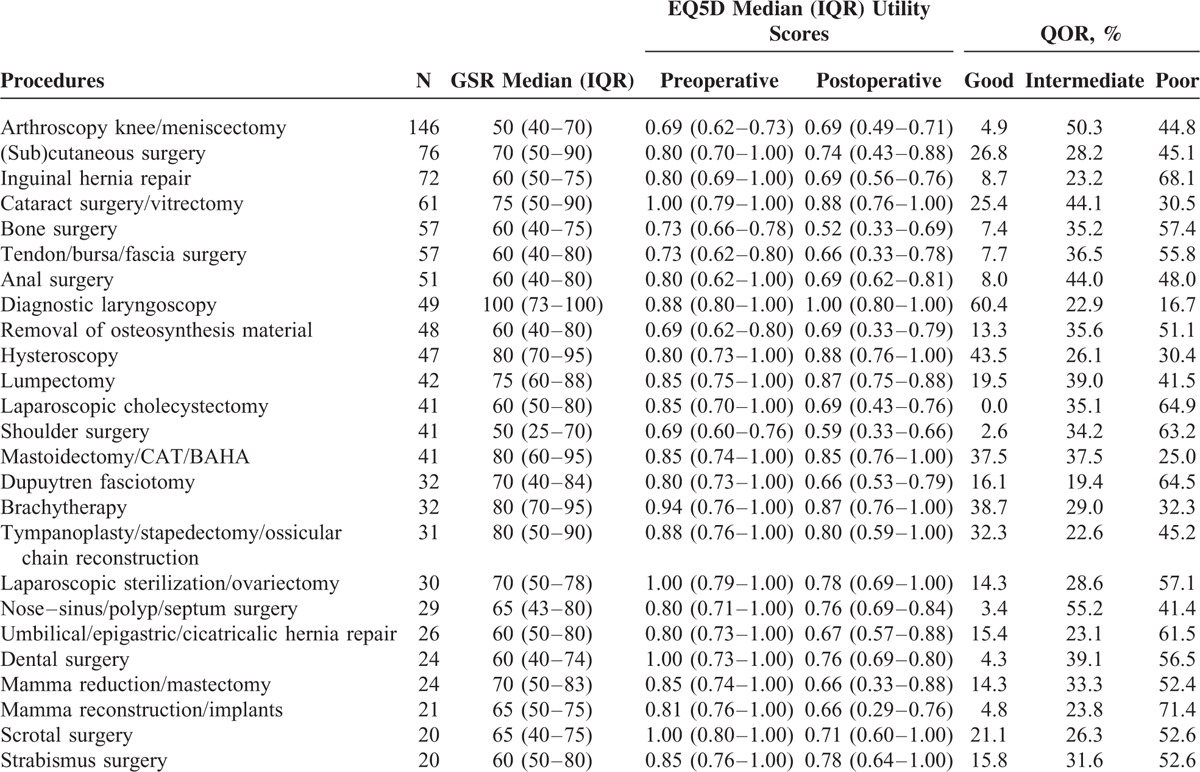
Overall, 17.3% of all patients showed a good QOR (ie, GSR >80% and equal/improved QOL), 34.8% an intermediate QOR (ie, GSR >80% or equal/improved QOL), and 47.8% of patients a poor QOR (ie, GSR ≤80% and reduced QOL) at 4 days after surgery. The percentages of patients with a good, intermediate, and poor QOR for the different surgical procedures are shown in Table 2. A great variability is seen in QOR between the different surgical procedures. For example, after laparoscopic cholecystectomy, none of the patients showed a good QOR at 4 days after surgery, whereas a good QOR was noted in 60% of the patients after diagnostic laryngoscopy.
TABLE 2.
Median (IQR) Global Surgical Recovery (GSR) Score, EQ5D Utility Scores, and Quality of Recovery (QOR) per Surgical Procedure (N ≥ 20)
Predictors and Prediction Model of QOR
Poor vs Both Intermediate and Good QOR
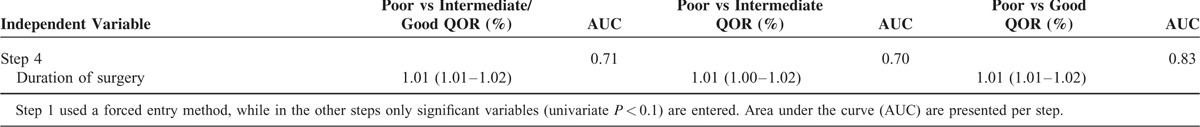
After univariate logistic regression analysis, preoperative pain, preoperative medication use, pain catastrophizing, optimism, and type of anesthesia were not statistically significant, and were therefore not included in the multivariate logistic regression model. Multivariate analysis showed younger age, type of surgery, work status (ie, having a paid job), higher expected pain, and longer duration of surgery to be the most important predictors for poor QOR (Table 3 ).
TABLE 3.
Results of the Logistic Regression Analysis for Global Surgical Recovery
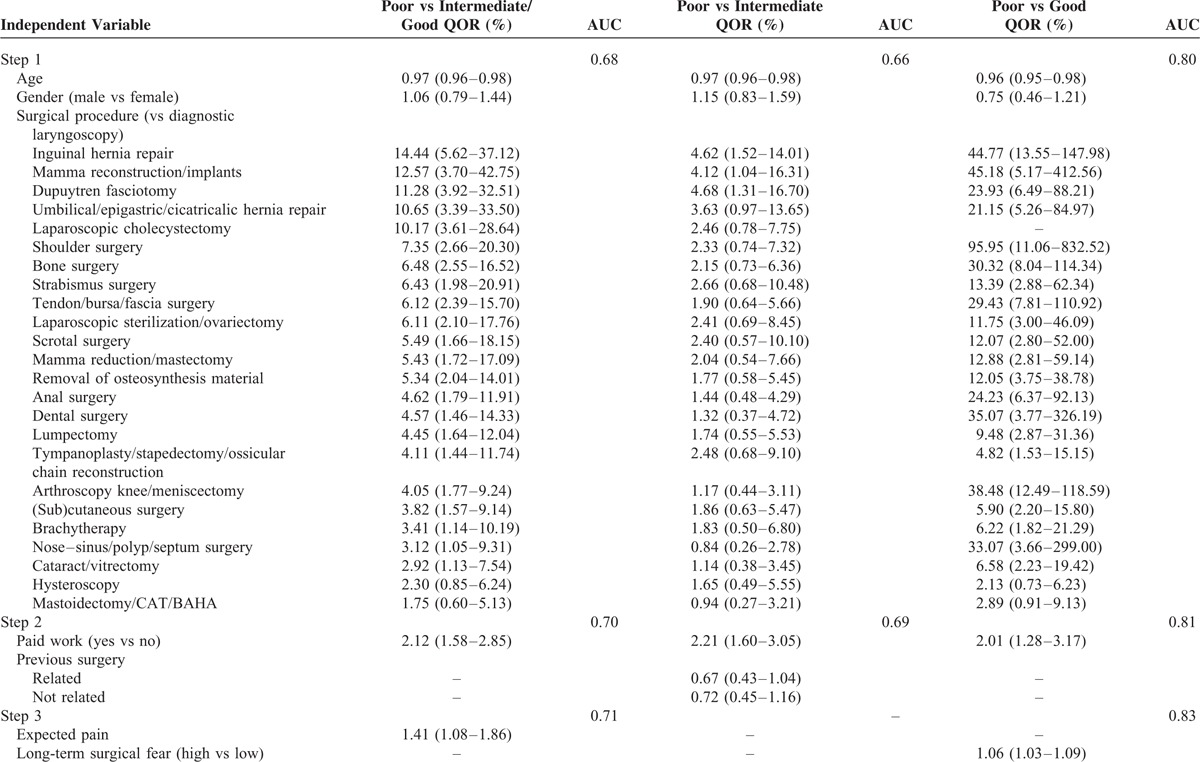
A predictive model was developed: the first step in the logistic regression model resulted in a prediction with an AUC of 0.68, which mostly depended on the surgical procedure. Contrary to gender, younger age was also found to be a significant predictor of poor recovery in our model. The second step improved our predictive model to an AUC of 0.70 as work status showed an association with poor QOR. The third step slightly improved our predictive model, as a higher expected postoperative pain was found to have a relation with poor QOR. The only statistically significant predictor of the final and fourth step in our prediction model turned out to be longer duration of surgery and slightly improved our model to a fairly adequate prediction with an AUC of 0.71.
Poor vs Intermediate QOR
After univariate logistic regression analysis, preoperative pain, preoperative medication use, short- and long-term surgical fear, pain catastrophizing, optimism, and type of anesthesia were not statistically significant, and were therefore not included in the multivariate logistic regression model. Multivariate analysis showed younger age, type of surgery, work status (ie, having a paid job), having had previous surgery, and longer duration of surgery to be the most important predictors for poor QOR (Table 3 ).
The first step in the prediction model resulted in an AUC of 0.66. After the second step of the model, an improvement is seen to an AUC of 0.69, due to the predictive value of work status and previous surgery. The final step (step 4) in the model showed a slight improvement to an AUC of 0.70, due to duration of surgery.
Poor vs Good QOR
After univariate logistic regression analysis, previous surgery, optimism, and type of anesthesia were not statistically significant, and were therefore not included in the multivariate logistic regression model. Multivariate analysis showed younger age, type of surgery, work status (ie, having a paid job), long-term surgical fear, and longer duration of surgery to be the most important predictors for poor QOR (Table 3 ).
The first step in the prediction model resulted already in a good prediction with an AUC of 0.80. After the second step of the model, an improvement is seen to an AUC of 0.81, due to the predictive value of work status and previous surgery. After the third step, an improvement is seen to an AUC of 0.83, due to long-term surgical fear, and the final step showed no improvement in AUC, although a longer duration of surgery was found to be a significant predictor of poor QOR.
Secondary Outcome Variables
Prevalence of GSR
Four days after surgery, median (IQR) GSR index for the total population is 70% (50% to 80%). A total of 229 patients (21%) scored a GSR of >80% 4 days after surgery. Patients receiving knee arthroscopy or shoulder surgery recovered worst (median GSR index of 50%), whereas patients receiving a diagnostic laryngoscopy recovered best (median GSR index of 100%) at 4 days after surgery (Table 2).
Prevalence of QOL
In the majority of patients and surgical procedures, a reduced total EQ5D-utility score is noted at the fourth postoperative day as compared with baseline (Table 2). Nevertheless wide variability in total EQ5D scores between surgical procedures is noted where for instance improvement is found in patients having had a diagnostic laryngoscopy, hysteroscopy, or lumpectomy. After knee arthroscopy, removal of osteosynthesis material or mastoidectomy/CAT/BAHA, median EQ5D-utility scores were unchanged. In our population of ambulatory patients more problems on 4 out of 5 domains of the EQ-5D (ie, mobility, self-care, usual activities, and pain/discomfort) were noted at the fourth day after surgery as compared with baseline. In only 1 of 5 domains (anxiety/depression), less problems were reported. Median total EQ5D-utility score, as well as health state were significantly lower at 4 days after the surgery (P < 0.001 and P = 0.031, respectively) (Table 4).
TABLE 3 (Continued).
Results of the Logistic Regression Analysis for Global Surgical Recovery
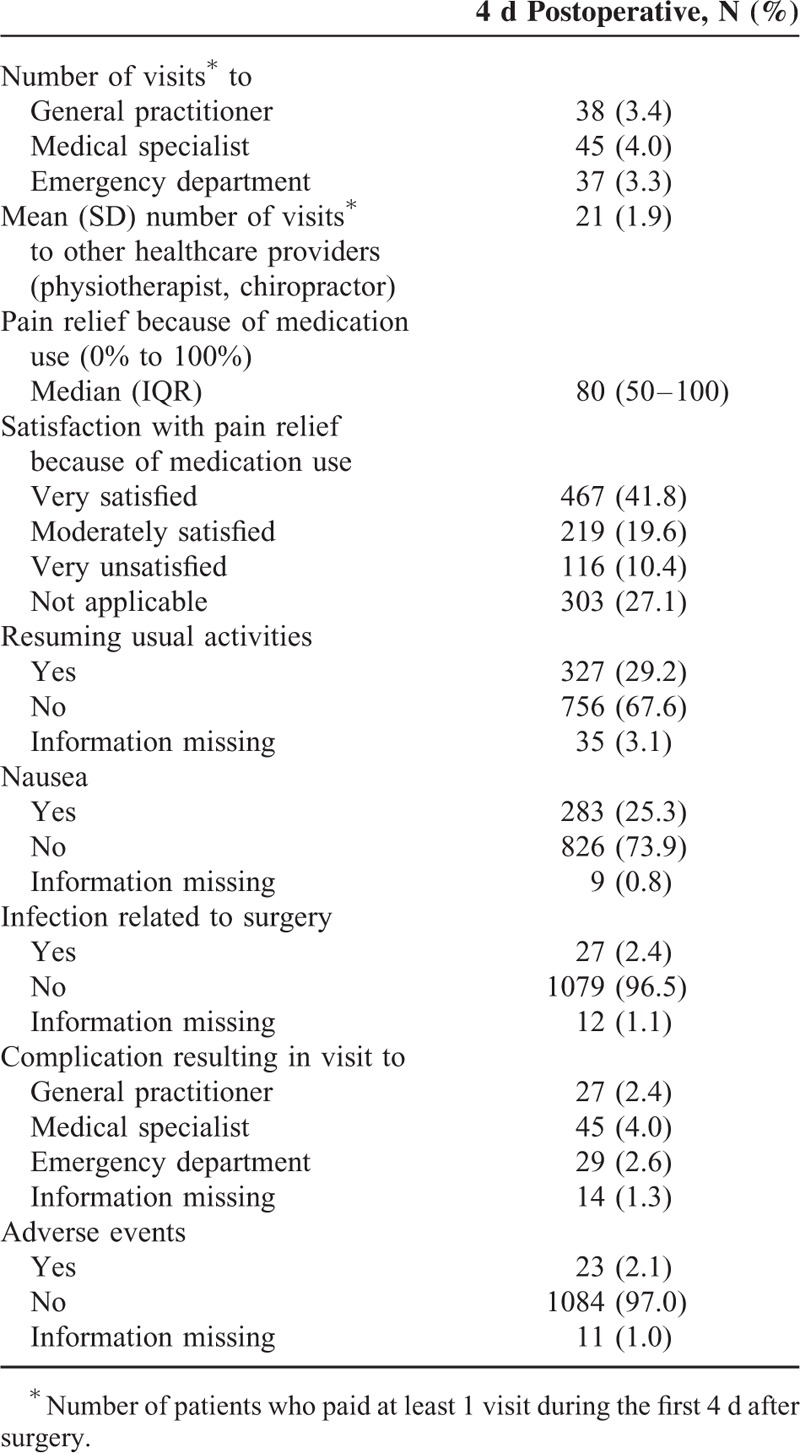
Other Secondary Outcome Variables
For pre- and postoperative pain scores, see Table 5. Seven-hundred sixteen (64%) of all patients were treated on an ambulatory basis (Table 1), and 375 (33.5%) on terms of a short-stay admission (<24 hr). Twenty-seven patients (2.4%) had an unplanned admission and stayed in hospital for over 24 hr (20 patients stayed for 3 days, 5 patients for 4 days, and 2 patients for 5 days) because of unforeseen complications. Furthermore, 83 visits were made to a general practitioner (n = 38) or medical specialist (n = 45) in the first 4 days after surgery. Also, 37 patients (3.3%) paid a visit to the emergency department (Table 6). Other complications like nausea and wound infections occurred in 25.3% and 2.4% of the patients, respectively (Table 6).
TABLE 4.
Pre- and Postoperative EuroQol 5D Scores
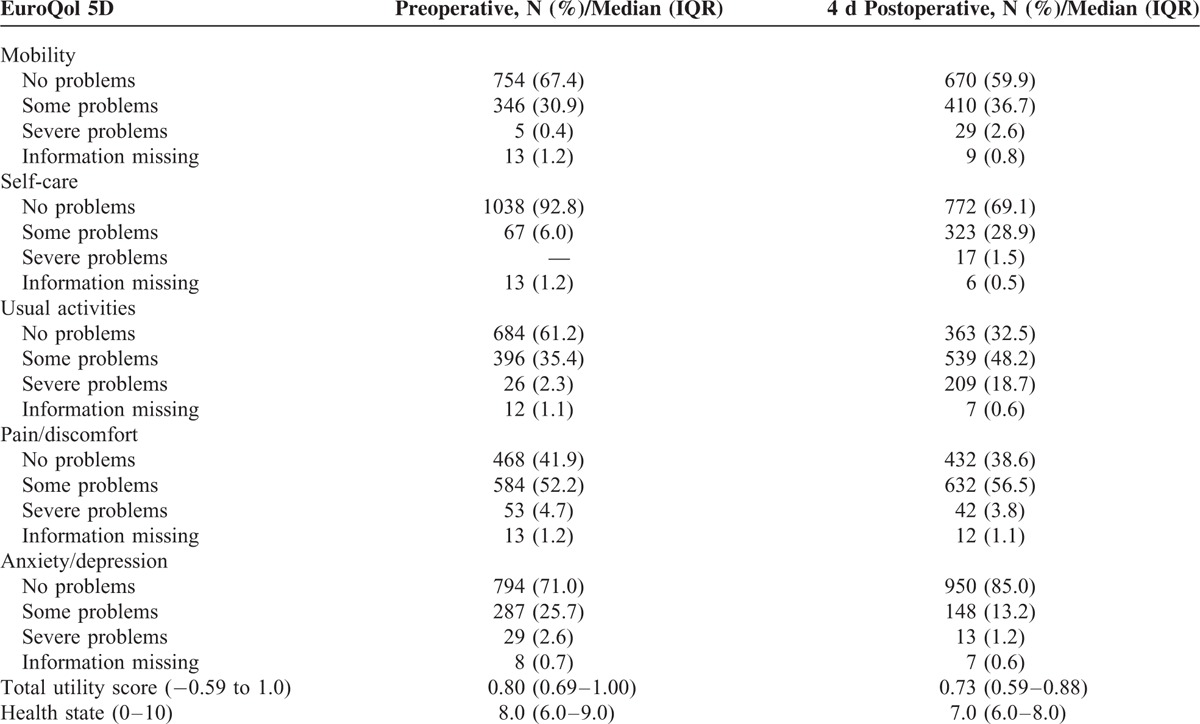
TABLE 5.
Preoperative and 4 d Postoperative Recovery, Pain intensity, and Pain Interference With Usual Activities
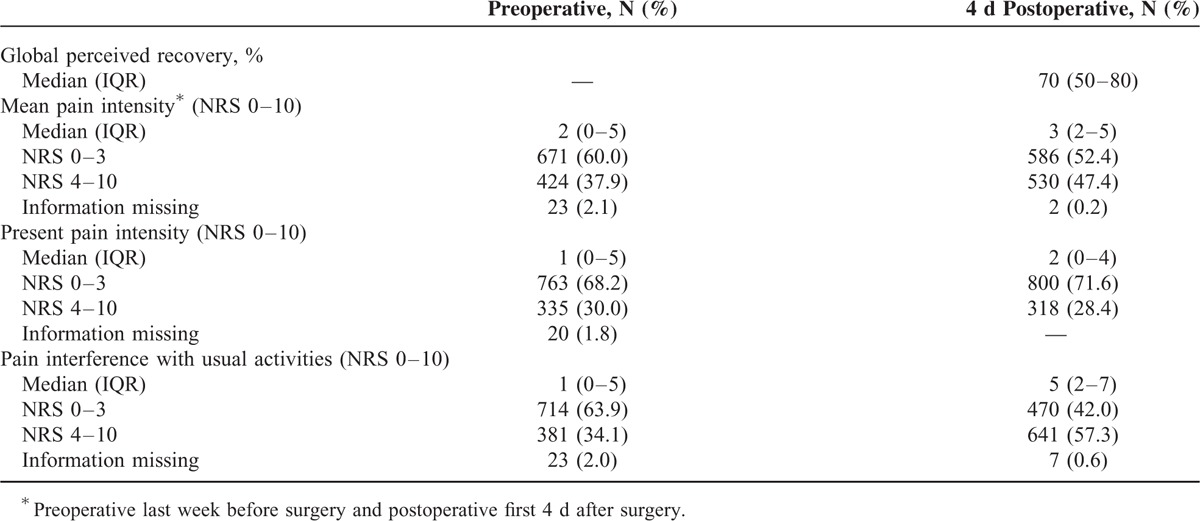
TABLE 6.
Healthcare Utilization, PONV, Complications
DISCUSSION
To our knowledge, this is the largest prospective cohort study to date, assessing prevalence and predictors of QOR after a wide range of surgical procedures (or groups of close related procedures) performed in an ambulatory setting.
The results of the present study suggest that QOR 4 days after day surgery was good (ie, GSR >80% and equal/improved QOL) in only 17.3% of patients and showed a clear procedure-related variation (Table 2). Furthermore, almost 40% of patients had problems with mobility, more than 30% of patients experienced problems with self-care, more than 60% with usual activities, and pain/discomfort was observed in 60% of the patients. A minority of patients expressed concerns related to anxiety/depression when compared with baseline. In selected groups such as shoulder surgery, bone surgery, and hernia repair, the incidence of poor outcome was even higher.
Our data are in line with recent literature, as poor recovery has been reported in the majority of patients undergoing inguinal hernia repair, arthroscopic procedures, or cosmetic breast augmentation in an ambulatory setting after 1 week.14 Moreover, Bratwall and Stromberg14 reported that more than 80% of patients were in need of support from a relative or friend during the first period at home. Furthermore, patients undergoing an orthopedic procedure were found to be at highest risk for inappropriate postoperative recovery 1 week after day surgery.18 In a heterogenic group of 701 patients undergoing elective inpatient and outpatient surgery, a complete recovery (defined as recovered on all domains of the postoperative quality recovery scale [PQRS]) was only noted in 11% of cases at the third postoperative day.29 On the other hand, comparing patient-reported recovery profiles using the EQ-5D did not result in overall changes between preoperative and postoperative EQ-5D scores at 2 weeks postoperatively.30 However, a procedure-specific approach has not been used in this study. In contrast, another study also using the EQ-5D reported a significant difference in time to reach full recovery between several procedures.31
Another primary goal of this study was to identify predictors of poor QOR on the fourth day after day surgery. Our data showed that type of surgery is the best predictor of poor QOR (Table 3 ). Other predictors for poor QOR were younger age, paid work, and longer duration of surgery.
The correlation of younger age and poor QOR is in line with literature findings, as several studies observed that acute postoperative pain is associated with younger age, and pain represents an important dimension of postsurgical recovery.7,8,32 On the other hand, younger age was shown to be associated with a better physical recovery (measured by physical activity) compared with baseline at 3 weeks postoperatively.9 These different findings are most likely related to differences in study design (different time points and end points, different patient populations). Patients with a paid job seem to experience a lower QOR compared with patients without. A possible explanation for this finding might be that these patients desire longer sick leave and therefore describe their recovery as less optimal.
The correlation between the somatic variable longer duration of surgery and poor QOR is in line with a previous study, as Peters et al11 observed an association between longer duration of surgery and long-term poor recovery 6 months after surgery. These results may point to the role of central sensitization since longer operations are associated with more enduring nociceptive input which may increase the chance of central sensitization, and subsequently persistent pain and poor QOR.11
The predictive power of the psychological variables was less strong. Expected pain (by the patient) is a predictor of poor QOR, compared with the combined group intermediate and good QOR and high long-term surgical fear is a predictor of poor QOR compared with good QOR. However, these psychological variables did not improve the AUC of their predictive model and all psychological variables even fell out of the third model (poor vs intermediate recovery). Nonetheless, in 1958 already, Janis33 proposed that a curvilinear relationship exists between preoperative psychological distress and postoperative recovery. And in a review, Munafo and Stevenson34 already have described an association between preoperative anxiety and early in-hospital recovery. As a consequence, further research is needed to shed more light on the exact relationship between psychological variables and postoperative QOR.
QOR after day surgery is an important measure and needs to be determined at various time-points. Most studies have either evaluated the early in-hospital course and/or the first 24 to 48 hr after day surgery,20,35–38 or have focused at a time frame between 1 week and 1 year after the surgery.9,14,18,25,30,39–41 The present study is the first to assess QOR at an intermediate time point of 4 days after day surgery. This time point was chosen based on a previous study from our group, showing an important number of patients still experiencing significant pain even at the fourth day after day surgery.42
Postoperative recovery is a complex phenomenon encompassing many dimensions in physical, psychological, and social health.9 There are several instruments for assessing the intermediate (3–7 days) and late (1 month) QOR after day surgery,8,43 including QOL questionnaires which may fulfill the requirements for assessing QOR.9 However, so far there is no general agreement on the optimal instrument for evaluating QOR and outcome following day surgery.39 We applied the convenient and validated 1-item GSR index together with the EuroQol 5D. We combined these 2 tools in an attempt to comprise all dimensions of QOR.
This is the first study to date to analyze a wide spectrum of possible predictors of poor QOR after day surgery, including patient characteristics, type and duration of surgery and anesthesia, social and psychological factors. The postoperative course can be affected by all those aspects.44 Another strength of this study is that we were able to assign the types of surgery to a wide range of homogenous surgical groups and that surgical groups were only selected for comparison when they contained at least 20 procedures.27 In contrast, all previous studies assigned the types of surgery to broad surgical disciplines such as general, urological, or orthopedic surgery11,18,25,38,40,41 or assessed only a few surgical procedures (making comparison between a wide range of procedures impossible).9,14,39
This study also has several limitations. Firstly, we did not include the Functional Recovery Index or the postoperative quality of recovery scale (PQRS), 2 tools specifically developed to assess different domains of recovery after surgery since these tools were not available at the time our study started.7,8,29
Secondly, outcome measures were only assessed at the fourth postoperative day, with a baseline measurement for predictor variables. Hence, we were not able to infer a postoperative health trajectory since this requires a minimum of 3 data points.45 Thirdly, this is a questionnaire-based survey and the response rate was 51% for both baseline and follow-up questionnaire. Hence, there is a possible danger of selection bias. Still, the response rate is similar to other questionnaire-based surveys.
Finally, there is a wide variation in the proportion of day surgery cases performed in different countries and even between hospitals in the same country because of differences in patient selection and differences in surgical procedures performed in an ambulatory setting.46
Furthermore, the landscape of ambulatory care is rapidly changing since innovations in surgical techniques and improvements in perioperative pain management and antiemetic therapy have allowed to perform more complex surgical procedures and to operate on older and higher risk patients in an outpatient setting.47 As a result, the generalizability of our results can be questioned. However, we tried to enhance the representativeness of our study by assigning the types of surgery included in our cohort to a wide range of homogenous surgical groups.
In conclusion, the present study involving a large cohort of day surgery patients shows a clear procedure-specific variation in QOR, after a 4-day period. The best predictor for poor QOR after day surgery was type of surgery. Other predictors were younger age, work status, and longer duration of surgery. A history of previous surgery and the psychological variables expected pain (by the patient) and high long-term surgical fear were significant predictors of poor QOR in only 1 of 3 logistic regression models.
Footnotes
Abbreviations: AUCa = rea under the curve, GSR = Global Surgical Recovery, LOT-R = Life Orientation Test Revised, PCS = Pain Catastrophizing Scale, QOLq = uality of life, QORq = uality of recovery, SFQ = Surgical Fear Questionnaire.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep 2009; 11:1–25. [PubMed] [Google Scholar]
- 2.Chung F, Un V, Su J. Postoperative symptoms 24 hours after ambulatory anaesthesia. Can J Anaesth 1996; 43:1121–1127. [DOI] [PubMed] [Google Scholar]
- 3.Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery: a prospective study. Can J Anaesth 1998; 45:612–619. [DOI] [PubMed] [Google Scholar]
- 4.Warner MA, Shields SE, Chute CG. Major morbidity and mortality within 1 month of ambulatory surgery and anesthesia. JAMA 1993; 270:1437–1441. [DOI] [PubMed] [Google Scholar]
- 5.Mattila K, Hynynen M. Intensium Consortium Study G. Day surgery in Finland: a prospective cohort study of 14 day-surgery units. Acta Anaesthesiol Scand 2009; 53:455–463. [DOI] [PubMed] [Google Scholar]
- 6.Aldwinckle RJ, Montgomery JE. Unplanned admission rates and postdischarge complications in patients over the age of 70 following day case surgery. Anaesthesia 2004; 59:57–59. [DOI] [PubMed] [Google Scholar]
- 7.Wong J, Tong D, De Silva Y, et al. Development of the Functional Recovery Index for ambulatory surgery and anesthesia. Anesthesiology 2009; 110:596–602. [DOI] [PubMed] [Google Scholar]
- 8.Jakobsson J. Ambulatory anaesthesia to improve the recovery process. Curr Opin Anaesthesiol 2011; 24:599–600. [DOI] [PubMed] [Google Scholar]
- 9.Tran TT, Kaneva P, Mayo NE, et al. Short-stay surgery: what really happens after discharge? Surgery 2014; 156:20–27. [DOI] [PubMed] [Google Scholar]
- 10.Kleinbeck SV. Self-reported at-home postoperative recovery. Res Nurs Health 2000; 23:461–472. [DOI] [PubMed] [Google Scholar]
- 11.Peters ML, Sommer M, de Rijke JM, et al. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg 2007; 245:487–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Agt HM, Essink-Bot ML, Krabbe PF, et al. Test-retest reliability of health state valuations collected with the EuroQol questionnaire. Soc Sci Med 1994; 39:1537–1544. [DOI] [PubMed] [Google Scholar]
- 13.Mottram A. Day surgery patients’ perceptions of risk: a qualitative research study. Ambul Surg 2012; 17:69–73. [Google Scholar]
- 14.Brattwall M, Warren Stomberg M, Rawal N, et al. Patients’ assessment of 4-week recovery after ambulatory surgery. Acta Anaesthesiol Scand 2011; 55:92–98. [DOI] [PubMed] [Google Scholar]
- 15.Mottram A. “Like a trip to McDonalds”: a grounded theory study of patient experiences of day surgery. Int J Nurs Stud 2011; 48:165–174. [DOI] [PubMed] [Google Scholar]
- 16.Berg K, Arestedt K, Kjellgren K. Postoperative recovery from the perspective of day surgery patients: a phenomenographic study. Int J Nurs Stud 2013; 50:1630–1638. [DOI] [PubMed] [Google Scholar]
- 17.Bellani ML. Psychological aspects in day-case surgery. Int J Surg 2008; 6 Suppl 1:S44–S46. [DOI] [PubMed] [Google Scholar]
- 18.Berg K, Kjellgren K, Unosson M, et al. Postoperative recovery and its association with health-related quality of life among day surgery patients. BMC Nurs 2012; 11:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ip HY, Chung F. Escort accompanying discharge after ambulatory surgery: a necessity or a luxury? Curr Opin Anaesthesiol 2009; 22:748–754. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell M. Home recovery following day surgery: a patient perspective. J Clin Nurs 2015; 24:415–427. [DOI] [PubMed] [Google Scholar]
- 21.Jakobsson JG. Pain management in ambulatory surgery: a review. Pharmaceuticals 2014; 7:850–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess 1995; 7:524–532. [Google Scholar]
- 23.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994; 67:1063–1078. [DOI] [PubMed] [Google Scholar]
- 24.Theunissen M, Peters ML, Schouten EG, et al. Validation of the Surgical Fear Questionnaire in adult patients waiting for elective surgery. PLoS ONE 2014; 9:e100225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoofwijk DM, Fiddelers AA, Peters ML, et al. Prevalence and predictive factors of chronic postsurgical pain and poor global recovery one year after outpatient surgery. Clin J Pain 2015 Jan 6. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26.Peters ML, Sommer M, van Kleef M, et al. Predictors of physical and emotional recovery 6 and 12 months after surgery. Br J Surg 2010; 97:1518–1527. [DOI] [PubMed] [Google Scholar]
- 27.Gerbershagen HJ, Aduckathil S, van Wijck AJ, et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 2013; 118:934–944. [DOI] [PubMed] [Google Scholar]
- 28.Van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1999; 18:681–694. [DOI] [PubMed] [Google Scholar]
- 29.Royse CF, Newman S, Chung F, et al. Development and feasibility of a scale to assess postoperative recovery: the post-operative quality recovery scale. Anesthesiology 2010; 113:892–905. [DOI] [PubMed] [Google Scholar]
- 30.Suhonen R, Virtanen H, Heikkinen K, et al. Health-related quality of life of day-case surgery patients: a pre/posttest survey using the EuroQol-5D. Qual Life Res 2008; 17:169–177. [DOI] [PubMed] [Google Scholar]
- 31.Brattwall M, Stomberg MW, Rawal N, et al. Patient assessed health profile: a six-month quality of life questionnaire survey after day surgery. Scand J Public Health 2010; 38:574–579. [DOI] [PubMed] [Google Scholar]
- 32.Gramke HF, de Rijke JM, van Kleef M, et al. Predictive factors of postoperative pain after day-case surgery. Clin J Pain 2009; 25:455–460. [DOI] [PubMed] [Google Scholar]
- 33.Janis IL. Psychological stress; psychoanalytic and behavioral studies of surgical patients. 1st ed.New York: Wiley; 1958. [Google Scholar]
- 34.Munafo MR, Stevenson J. Anxiety and surgical recovery. Reinterpreting the literature. J Psychosom Res 2001; 51:589–596. [DOI] [PubMed] [Google Scholar]
- 35.De Oliveira GS, Jr, Fitzgerald P, Streicher LF, et al. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg 2012; 115:262–267. [DOI] [PubMed] [Google Scholar]
- 36.Lindqvist M, Royse C, Brattwall M, et al. Post-operative Quality of Recovery Scale: the impact of assessment method on cognitive recovery. Acta Anaesthesiol Scand 2013; 57:1308–1312. [DOI] [PubMed] [Google Scholar]
- 37.McIntosh S, Adams J. Anxiety and quality of recovery in day surgery: a questionnaire study using Hospital Anxiety and Depression Scale and Quality of Recovery Score. Int J Nurs Pract 2011; 17:85–92. [DOI] [PubMed] [Google Scholar]
- 38.Vinoles J, Ibanez MV, Ayala G. Predicting recovery at home after ambulatory surgery. BMC Health Serv Res 2011; 11:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mattila K, Lahtela M, Hynynen M. Health-related quality of life following ambulatory surgery procedures: assessment by RAND-36. BMC Anesthesiol 2012; 12:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Idvall E, Berg K, Unosson M, et al. Assessment of recovery after day surgery using a modified version of quality of recovery-40. Acta Anaesthesiol Scand 2009; 53:673–677. [DOI] [PubMed] [Google Scholar]
- 41.Mijderwijk H, van Beek S, Klimek M, et al. Lorazepam does not improve the quality of recovery in day-case surgery patients: a randomised placebo-controlled clinical trial. Eur J Anaesthesiol 2013; 30:743–751. [DOI] [PubMed] [Google Scholar]
- 42.Gramke HF, de Rijke JM, van Kleef M, et al. The prevalence of postoperative pain in a cross-sectional group of patients after day-case surgery in a university hospital. Clin J Pain 2007; 23:543–548. [DOI] [PubMed] [Google Scholar]
- 43.Herrera FJ, Wong J, Chung F. A systematic review of postoperative recovery outcomes measurements after ambulatory surgery. Anesth Analg 2007; 105:63–69. [DOI] [PubMed] [Google Scholar]
- 44.Bettelli G. High risk patients in day surgery. Minerva Anestesiol 2009; 75:259–268. [PubMed] [Google Scholar]
- 45.Singh-Manoux A, Ferrie JE, Chandola T, et al. Socioeconomic trajectories across the life course and health outcomes in midlife: evidence for the accumulation hypothesis? Int J Epidemiol 2004; 33:1072–1079. [DOI] [PubMed] [Google Scholar]
- 46.Toftgaard C, Parmentier G. Lemos P, Jarrett PEM, Philip B. International terminology in ambulatory surgery and its worldwide practice. Day Surgery: Development and Practice. London: International Association for Ambulatory Surgery; 2006. 35–60. [Google Scholar]
- 47.White PF, White LM, Monk T, et al. Perioperative care for the older outpatient undergoing ambulatory surgery. Anesth Analg 2012; 114:1190–1215. [DOI] [PubMed] [Google Scholar]


