Abstract
Little was known about the effects of acupuncture on stroke recurrence. The aim of this study is to investigate whether ischemic stroke patients receiving acupuncture treatment have a decreased risk of stroke recurrence.
A retrospective cohort study of 30,058 newly diagnosed cases of ischemic stroke in 2000 to 2004 was conducted based on the claims of Taiwan National Health Insurance Research Database. The use of acupuncture treatment and stroke recurrence were identified during the follow-up period from 2000 to 2009. This study compared the risk of stroke recurrence between ischemic stroke cohorts with and without acupuncture treatment by calculating adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) of acupuncture associated with stroke recurrence in the Cox proportional hazard model.
The stroke recurrence rate per 1000 person-years decreased from 71.4 without to 69.9 with acupuncture treatment (P < 0.001). Acupuncture treatment was associated with reduced risk of stroke recurrence (HR 0.88; 95% CI 0.84–0.91). The acupuncture effect was noted in patients with or without medical treatment for stroke prevention but its impact decreased with aging of stroke patients. Compared with stroke patients without acupuncture treatment and medication therapy, the hazard ratios of stroke recurrence for those had medication therapy only, acupuncture only, and both were 0.42 (95% CI 0.38–0.46), 0.50 (95% CI 0.43–0.57), and 0.39 (95% CI 0.35–0.43), respectively.
This study raises the possibility that acupuncture might be effective in lowering stroke recurrence rate even in those on medications for stroke prevention. Results suggest the need of prospective sham-controlled and randomized trials to establish the efficacy of acupuncture in preventing stroke.
INTRODUCTION
Stroke remains a leading cause of death and the leading cause of disability worldwide.1 The costs of stroke to the family and the society underscore the importance of stroke prevention and management. Secondary stroke prevention remains a top priority in treating patients after the first stroke2–6 and is a key performance indicator in the American Heart Association/American Stroke Association Get With The Guidelines Stroke program,7 which have been followed in Taiwan.8 The mainstay in stroke prevention for patients with ischemic stroke in the Get With The Guidelines Stroke program is antithrombotic therapy.7
In addition to antithrombotics for stroke prevention, rehabilitation is an important therapy for facilitating functional recovery after stroke.9 Other than rehabilitation, stroke patients in Taiwan have the option of receiving complementary and alternative therapies including acupuncture that is approved for reimbursement by the National Health Insurance (NHI) in Taiwan.10
Acupuncture has been in practice among Chinese for more than 2000 years and has been increasingly integrated into the mainstream healthcare programs including those in the United States.11 In addition to various pain syndromes,9,12,13 acupuncture has increasingly attracted attention in treating stroke patients with mixed results.10,11,14–18 Meta-analyses suggest that the efficacy of acupuncture remains to be established.15,17 Despite the lack of solid evidence to support its clinical utility, acupuncture is a safe, low-cost, and viable alternative therapy, especially for patients with stroke-related disorders that do not respond to conventional medical or rehabilitative measures.
Favorable rehabilitation outcome aided by acupuncture in some stroke patients may increase physical activity to reduce stroke recurrence risk.19,20 Acupuncture may also have salutary actions on vascular function by increasing nitric oxide level, improving lipid profile, and lowering blood pressure.21–25 Pretreatment of electroacupuncture may reduce infarct size, improved neurological outcome in patients with cerebral infarction.26 Based on these ancillary effects of acupuncture that may all lead to lower stroke risk in stroke patients who receive acupuncture, we explore whether the incidence of stroke recurrence was lowered in stroke patients receiving acupuncture as compared with those without based on population-based claims in the National Health Insurance Research Database.
METHODS
Data Sources
Reimbursement claims in the NHI database were used in the present study. NHI has been implemented since March 1995, covering more than 99% of the 23 million population.27–30 The electronic database was encrypted with patient identifications scrambled to protect privacy of all subjects. This study was exempted from the review by the Internal Review Board. All beneficiaries’ inpatient and outpatient medical services such as simple demographics (gender, birth date, low-income status, and urbanization of living area), primary and secondary diagnoses with the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM), procedures, prescriptions, and medical expenditures are recorded in the National Health Insurance Research Database established by the National Health Research Institutes.28-30
Ethics Approval
Insurance reimbursement claims used in this study were from Taiwan's National Health Insurance Research Database. For protection of personal privacy, the electronic database was decoded with patient identifications scrambled for further public access for research. This study was evaluated and approved by Taiwan's National Health Research Institutes (NHIRD-100–122) and the Institutional Review Board of E-DA Hospital, Kaohsiung, Taiwan (2014012); this organization's regulations do not require informed consent because patient identification has been decoded and scrambled.28–30 This study was conducted in accordance with the Declaration of Helsinki.
Study Population
In this cohort, 30058 adults (age ≥ 30 years) with ischemic stroke diagnosed for the first time in 2000–2004 were identified. Patients were then divided into 2 groups, without or with acupuncture therapy after stroke. We further randomly selected from those without acupuncture to constitute a control group that was matched by age, sex, and key variables with the acupuncture group, applying propensity score. Patients with ischemic stroke who were included in the acupuncture group received at least 6 sessions of acupuncture treatment. Only acupuncturists who are certified traditional Chinese medical doctor with acupuncture specialty fulfilling the yearly continuing acupuncture education requirements are qualified for filing NHI claims for acupuncture reimbursement.
Patients with and without acupuncture treatment were followed from the index event until the end of 2009 to identify the incidence of stroke recurrence. Comorbidities including hypertension, diabetes, and hyperlipidemia were identified as the key stroke risk factors that might contribute to stroke recurrence and compound the effectiveness of acupuncture treatment. Effects of medications for stroke prevention including antiplatelet agents, anticoagulants, and lipid-lowering agents on stroke recurrence were also assessed.
Criteria and Definition
ICD-9-CM was used to define ischemic stroke (ICD-9-CM 430–434). Hypertension (ICD-9-CM 401–405), diabetes (ICD-9-CM 250), hyperlipidemia (ICD-9-CM 272.0, 272.1, 272.2), liver cirrhosis (ICD-9-CM 571), mental disorder (ICD-9-CM 290–319), ischemic heart disease (ICD-9-CM 410–414), and renal dialysis (administration code D8, D9) were also identified.
Statistical Analysis
The chi-square tests were used to compare the distribution of age, sex, comorbidities, and medication in reference to stroke recurrence between groups with and without acupuncture treatment. The incidences (per 1000 person-years) of stroke recurrence and incidence rate ratio with 95% confidence intervals (CIs) were derived and compared between groups. Stroke severity was assessed based on length of stay and hospitalization expenditure reimbursed by the NHI. The Kaplan–Meier plot was applied to measure stroke recurrence over time and the Cox proportional hazards model to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). All statistical analyses were performed using SAS software version 9.1 (SAS Institute Inc., Carey, NC) with 2-sided P < 0.05 being taken to represent statistical significance.
RESULTS
Overall, there were 30,058 newly diagnosed cases of ischemic stroke. After matching with propensity score, there was no difference in age, sex, comorbidities relevant to stroke and medications for stroke prevention. In follow-up to the end of 2009, 4639 (30.9%) in the acupuncture group experienced stroke recurrence as compared with 5749 patients (38.3%) in the group without acupuncture (P < 0.001) (Table 1). The length of stay and hospitalization expenditure, 2 parameters that might reflect stroke severity, were not different between groups.
TABLE 1.
Characteristics of Stroke Patients With and Without Acupuncture Treatment∗
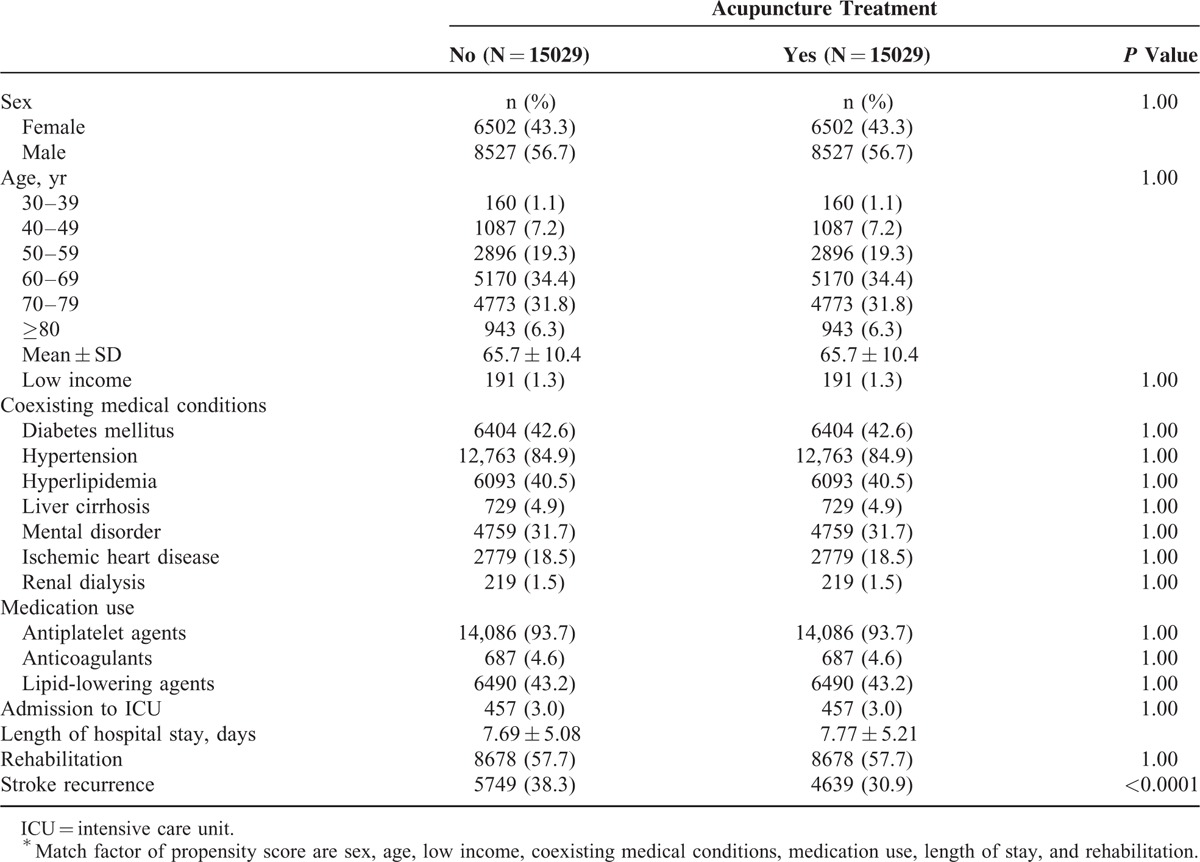
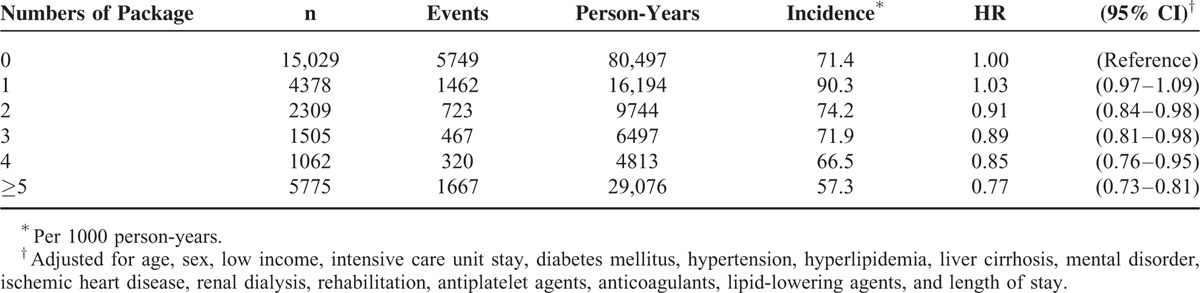
The stroke recurrence rate per 1000 person-years was 71.4 in the group without and 69.9 with acupuncture treatment, respectively (P < 0.001) (Table 2). The reduced risk of stroke recurrence was associated with acupuncture treatment (HR 0.88, 95% CI 0.84–0.91). Acupuncture treatment appeared to reduce stroke recurrence rate in both sexes and across the age groups. Its effect was noted in patients with or without comorbidities relevant to ischemic stroke including hypertension, diabetes, or hyperlipidemia. Acupuncture effect in stroke prevention appeared to be more apparent among those not on medications for stroke prevention. Table 3 presents interaction of medication for stroke prevention and acupuncture treatment. The HR was also significantly lower in those with only acupuncture treatment. Compared with stroke patients without acupuncture treatment and medication therapy, the hazard ratios of stroke recurrence for those had medication therapy only, acupuncture only, and both were 0.42 (95% CI 0.38–0.46), 0.50 (95% CI 0.43–0.57), and 0.39 (95% CI 0.35–0.43), respectively. Compared with stroke patients with medication therapy but without acupuncture treatment, the HR of stroke recurrence for those with both acupuncture treatment and medication therapy was 0.93 (95% CI 0.89–0.97). In Table 4, the risk of stroke recurrence was associated with numbers of package of acupuncture treatment (P < 0.0001).
TABLE 2.
Stroke Recurrence Rates Based on Demographic, Comorbidity, and Therapy Profiles With and Without Acupuncture
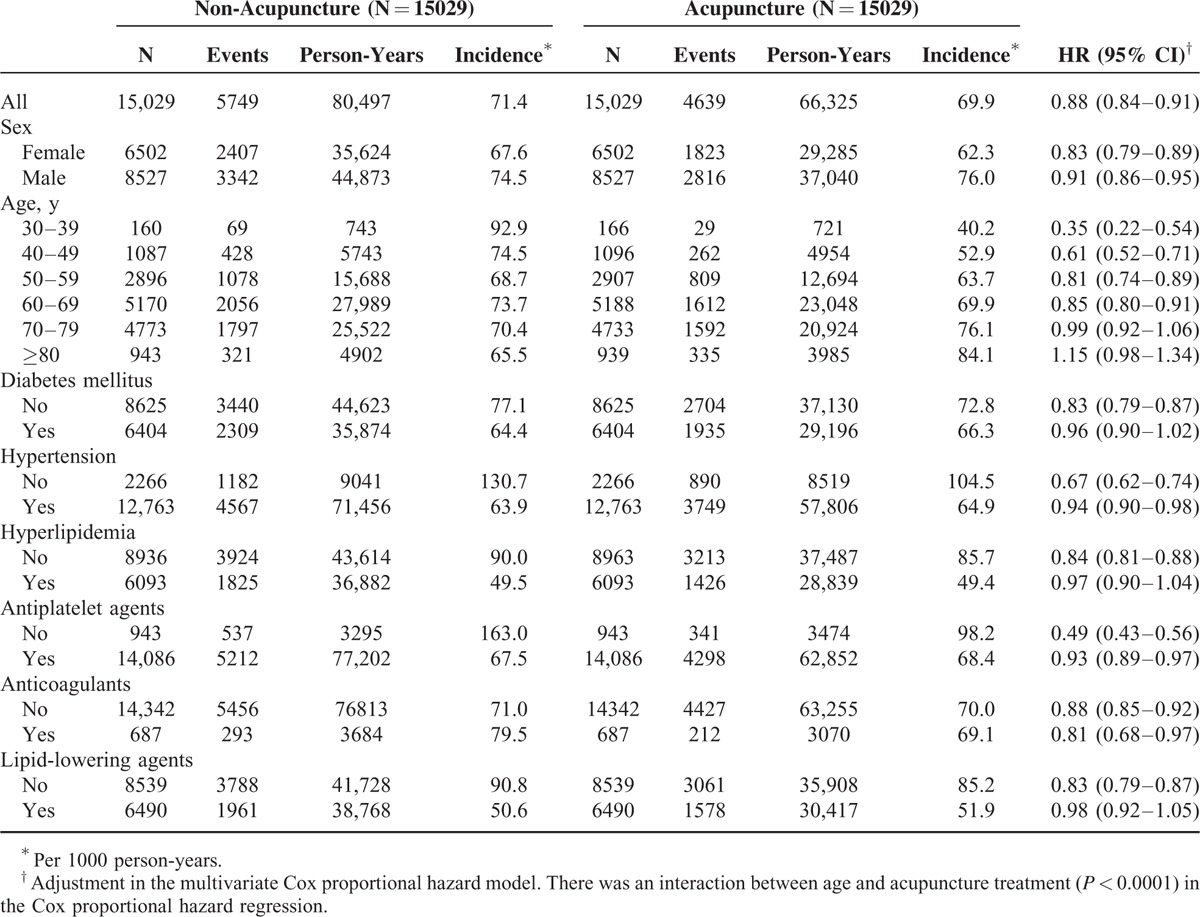
TABLE 3.
Incidence and Hazard Ratio of Stroke Recurrence Among Different Therapy Groups
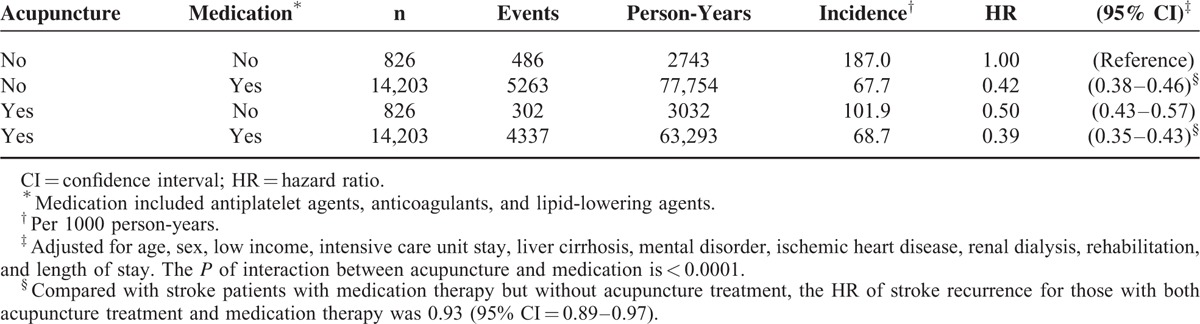
TABLE 4.
Risk of Stroke Recurrence in Association With Numbers of Package of Acupuncture Treatment
The Kaplan–Meier model showed that, during the follow-up period to the end of 2009, ischemic stroke patients with acupuncture treatment had lower cumulative rate of recurrent stroke than those without acupuncture treatment (log-rank P < 0.0001) (Figure 1).
FIGURE 1.
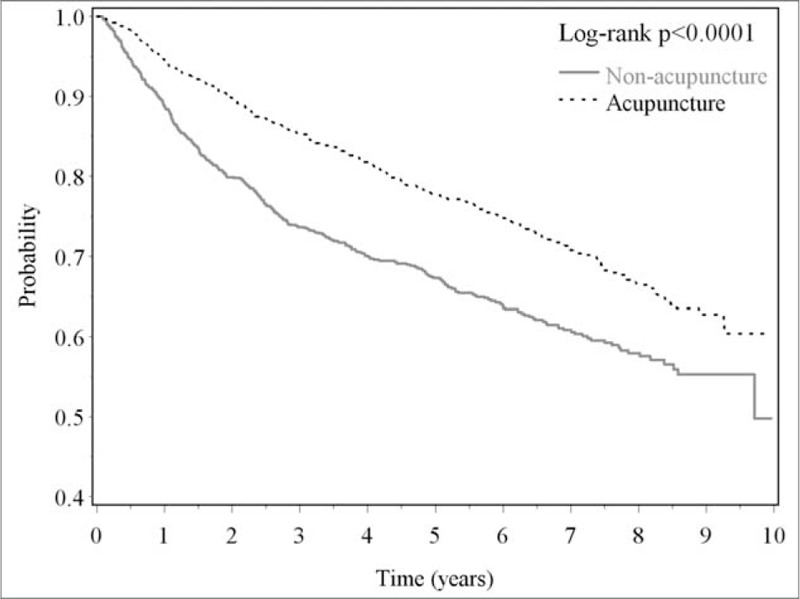
Kaplan–Meier analysis for stroke recurrence in ischemic stroke patients newly diagnosed in 2000 to 2004 with and without acupuncture treatment for follow-up to the end of 2009.
DISCUSSION
Using claims data from the National Health Insurance Research Database, we conducted a nationwide, population-based, propensity score-matched, retrospective cohort study that investigated the lower risk of recurrent stroke in ischemic stroke patients with acupuncture treatment than those without acupuncture treatment. The present study also showed that the biological gradient relationship between the numbers of package acupuncture treatment and reduced recurrent stroke. This is the first large-scale investigation reporting the effectiveness of acupuncture treatment on reducing the stroke recurrence in ischemic stroke patients.
Antithrombotic therapies, including antiplatelet agents and oral anticoagulants, are the mainstay in the primary and secondary stroke prevention.5,6,31–34 Acupuncture is a widely used procedure in Chinese medicine for patients with various diseases.12–18,21–25 Acupuncture has also been applied to stroke patients for reducing spasticity and pain and for improving motor function.10,14–18 Although systematic reviews on the effect of acupuncture, as a supplement therapy for rehabilitation in stroke patients, show mixed results,14–18 the infarct size and neurological outcome was improved after the treatment with electroacupuncture in patients with cerebral infarction.26 Overall, acupuncture has not been shown in well-designed sham-controlled and randomized trials to be effective in improving functional outcomes after stroke.14,17 Acupuncture is accepted by NHI in Taiwan for caring several diseases including stroke. More than 18% of patients with ischemic stroke in Taiwan received acupuncture for at least 6 sessions to qualify for NHI reimbursement. We noted that among those receiving acupuncture, the stroke recurrence rate was lower than those without.
After the matching procedure by propensity score, there was no significant difference in age, sex, coexisting medical conditions, medications, and length of stay or hospitalization expenditure for the first stroke admission between stroke patients with and without acupuncture treatment. Age is the most important stroke risk factor.35,36 If there is any impact of age, the acupuncture group has a slighter higher mean age than the control group. These observations make it unlikely that difference in age can be accounted for lower stroke recurrence rate in the acupuncture group. It is worth noting that there appears to have an age-dependent effect on incidence rate ratio that is significantly lower in younger stroke patients (Table 3).
However, among those receiving medical treatment, acupuncture treatment appears to lower the stroke recurrence rate as well (Table 4). The finding that the effect of acupuncture in reducing stroke recurrence rate was still noted up to 10 years in follow-up is interesting. This long-lasting acupuncture effect is worth exploring to establish evidence-based acupuncture reduction of stroke recurrence.
A question can also be raised concerning potential difference in stroke severity between groups. Table 2 shows that there was no significant difference in length of stay or hospitalization expenditure for the first stroke, 2 indirect indicators of stroke severity. Figure 1 shows that the probability for being free of a second stroke was significantly higher among those with acupuncture treatment than those without. The validity of the data presented in this retrospective study is also supported by the finding that those receiving medical treatment fared better than those without as presented in Table 4.
Based on the findings of this study, we proposed some possible explanations for clarifying the effectiveness of acupuncture treatment on stroke recurrence. While systematic reviews failed to establish that acupuncture is a valid rehabilitative measure in improving functional outcome in stroke patients, there are a number of publications showing acupuncture was indeed effective in improving neurological function or physical capability among stroke patients.15,16 Increased physical activities have been shown to reduce stroke risk.37 We have also shown that physical activity is effective in reducing stroke mortality.19 These findings together raise the possibility that acupuncture may have impact through improved physical activity to reduce the risk of recurrent stroke. The salutary effect of acupuncture may not be restricted to improvement in physical activity. It has been shown that acupuncture is useful in lowering blood pressure,21,22 reducing the expression of inflammatory mediators,38 and improving lipid profile.24,25 It is believed that lower blood pressure, lipid profile, and less inflammation mediators may lead ischemic stroke patients with acupuncture treatment to have decreased risk of recurrent stroke.
This study has some limitations. First, as we used retrospective medical claims data from health insurance that lacked detailed patient's information in detail on lifestyle as well as physical, psychiatric, and laboratory examinations, we were unable to differentiate whether these factors influenced the effects of acupuncture treatment on stroke patients. Second, we used ICD-9-CM codes claimed by physicians for the stroke without clarifying the severity of disease, our study would have been improved if we had information of National Institute of Health Stroke Scale. Third, our study could not show the acupuncture points used in patient care due to the limited information from National Health Insurance Research Database. While acupuncture treatment for NHI reimbursement has been closely monitored with strict regulatory accreditation guidelines, the acupuncture protocols were not controlled as in clinical trial settings. Finally, another limitation is that stroke patients who chose acupuncture might have been more motivated to improve post-stroke complications than those did not. Our additional analysis (not shown in the tables) also showed that receiving Chinese herbal medicine (1 of subtypes of traditional Chinese medicine that was also covered in the Taiwan's National Health Insurance) was associated with reduced risk of recurrent stroke in both stroke patients with (HR 0.73, 95% CI 0.68–0.78) and without (HR 0.63, 95% CI 0.59–0.67) receiving acupuncture treatment
CONCLUSIONS
In this nationwide retrospective cohort study of ischemic stroke patients, the reduced risk of recurrent stroke was found in the cohorts with acupuncture treatment. Patients with ischemic stroke underwent medication and acupuncture treatment had the lowest risk of stroke recurrence. However, the potential beneficial effects of acupuncture as a supplement measure to reduce stroke recurrence deserve further exploration in well designed clinical trials with stringent acupuncture protocols and sham control in a blinded fashion.
Footnotes
Abbreviations: CI = confidence interval, HR = hazard ratio, ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification, NHI = National Health Insurance.
This study is based in part on data obtained from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health, or National Health Research Institutes.
Dr C-CL has equal contribution with the first author.
This study was supported in part by Committee on Chinese Medicine and Pharmacy, Department of Health, Taiwan (CCMP99-RD-035), Taiwan Ministry of Science and Technology (MOST103-2320-B-214-010-MY2), Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW104-TDU-B-212-113002), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM104010092), NRPB Stroke Clinical Trial Consortium (MOST 103-2325-B-039-006), Tseng-Lien Lin Foundation and the Katsuzo and Kiyo Aoshima Funds, Japan.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Donnan GA, Fisher M, Macleod M, et al. Stroke. Lancet 2008; 371:1612–1623. [DOI] [PubMed] [Google Scholar]
- 2.Rothwell PM, Algra A, Amarenco P. Medical treatment in acute and long-term secondary prevention after transient ischaemic attack and ischaemic stroke. Lancet 2011; 377:1681–1692. [DOI] [PubMed] [Google Scholar]
- 3.Hong KS, Yegiaian S, Lee M, et al. Declining stroke and vascular event recurrence rates in secondary prevention trials over the past 50 years and consequences for current trial design. Circulation 2011; 123:2111–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McArthur KS, Quinn TJ, Higgins P, et al. Post-acute care and secondary prevention after ischaemic stroke. BMJ 2011; 342:d2083. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein LB, Rothwell PM. Advances in prevention and health services delivery 2010-2011. Stroke 2012; 43:298–299. [DOI] [PubMed] [Google Scholar]
- 6.Abbott AL. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Stroke 2009; 40:e573–e583. [DOI] [PubMed] [Google Scholar]
- 7.Fonarow GC, Reeves MJ, Smith EE, et al. Characteristics, performance measures, and in-hospital outcomes of the first 1 million stroke and transient ischemic attack admissions in get with the guidelines-stroke. Circ Cardiovasc Qual Outcomes 2010; 3:291–302. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh FI, Lien LM, Chen ST, et al. Get With the Guidelines-Stroke performance indicators: surveillance of stroke care in the Taiwan Stroke Registry: get With the Guidelines-Stroke in Taiwan. Circulation 2010; 122:1116–1123. [DOI] [PubMed] [Google Scholar]
- 9.Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol 2006; 164:487–496. [DOI] [PubMed] [Google Scholar]
- 10.Wei YC, Sun MF, Chang KC, et al. Pilot scheme of health policy in stroke adjuvant acupuncture therapy for acute and subacute ischemic stroke in Taiwan. Evid Based Complement Alternat Med 2011; 2011:689813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hawk C, Ndetan H, Evans MW., Jr Potential role of complementary and alternative health care providers in chronic disease prevention and health promotion: an analysis of National Health Interview Survey data. Prev Med 2012; 54:18–22. [DOI] [PubMed] [Google Scholar]
- 12.Berman BM, Langevin HM, Witt CM, et al. Acupuncture for chronic low back pain. New Engl J Med 2010; 363:454–461. [DOI] [PubMed] [Google Scholar]
- 13.Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med 2009; 169:858–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu H, Tang J, Lin X, et al. Acupuncture for stroke rehabilitation. Stroke 2008; 39:517–518. [Google Scholar]
- 15.Wu P, Mills E, Moher D, et al. Acupuncture in poststroke rehabilitation: a systematic review and meta-analysis of randomized trials. Stroke 2010; 41:e171–e179. [DOI] [PubMed] [Google Scholar]
- 16.Sze FK, Wong E, Or KK, et al. Does acupuncture improve motor recovery after stroke? A meta-analysis of randomized controlled trials. Stroke 2002; 33:2604–2619. [DOI] [PubMed] [Google Scholar]
- 17.Kong JC, Lee MS, Shin BC, et al. Acupuncture for functional recovery after stroke: a systematic review of sham-controlled randomized clinical trials. CMAJ 2010; 182:1723–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim MK, Choi TY, Lee MS, et al. Contralateral acupuncture versus ipsilateral acupuncture in the rehabilitation of post-stroke hemiplegic patients: a systematic review. BMC Complement Altern Med 2010; 10:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 2011; 378:1244–1253. [DOI] [PubMed] [Google Scholar]
- 20.Boysen G, Krarup LH. Benefits of physical activity for stroke survivors. Expert Rev Neurother 2009; 9:147–149. [DOI] [PubMed] [Google Scholar]
- 21.Flachskampf FA, Gallasch J, Gefeller O, et al. Randomized trial of acupuncture to lower blood pressure. Circulation 2007; 115:3121–3129. [DOI] [PubMed] [Google Scholar]
- 22.Kim DD, Pica AM, Duran RG, et al. Acupuncture reduces experimental renovascular hypertension through mechanisms involving nitric oxide synthases. Microcirculation 2006; 13:577–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsuchiya M, Sato EF, Inoue M, et al. Acupuncture enhances generation of nitric oxide and increases local circulation. Anesth Analg 2007; 104:301–307. [DOI] [PubMed] [Google Scholar]
- 24.Cabioğlu MT, Ergene N. Electroacupuncture therapy for weight loss reduces serum total cholesterol, triglycerides, and LDL cholesterol levels in obese women. Am J Chin Med 2005; 33:525–533. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh CH. The effects of auricular acupuncture on weight loss and serum lipid levels in overweight adolescents. Am J Chin Med 2010; 38:675–682. [DOI] [PubMed] [Google Scholar]
- 26.Wang Q, Peng Y, Chen S, et al. Pretreatment with electroacupuncture induces rapid tolerance to focal cerebral ischemia through regulation of endocannabinoid system. Stroke 2009; 40:2157–2164. [DOI] [PubMed] [Google Scholar]
- 27.Chen HF, Lee SP, Li CY. Sex differences in the incidence of hemorrhagic and ischemic stroke among diabetics in Taiwan. J Womens Health 2009; 18:647–654. [DOI] [PubMed] [Google Scholar]
- 28.Liao CC, Chou YC, Yeh CC, et al. Stroke risk and outcomes in patients with traumatic brain injury: 2 nationwide studies. Mayo Clin Proc 2014; 89:163–172. [DOI] [PubMed] [Google Scholar]
- 29.Liao CC, Lin CS, Shih CC, et al. Increased risk of fracture and postfracture adverse events in patients with diabetes: 2 nationwide population-based retrospective cohort studies. Diabetes Care 2014; 37:2246–2252. [DOI] [PubMed] [Google Scholar]
- 30.Liao CC, Shen WW, Chang CC, et al. Surgical adverse outcomes in patients with schizophrenia: a population-based study. Ann Surg 2013; 257:433–438. [DOI] [PubMed] [Google Scholar]
- 31.Milionis HJ, Giannopoulos S, Kosmidou M, et al. Statin therapy after first stroke reduces 10-year stroke recurrence and improves survival. Neurology 2009; 72:1816–1822. [DOI] [PubMed] [Google Scholar]
- 32.Sacco RL, Diener HC, Yusuf S, et al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med 2008; 359:1238–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohr JP, Thompson JL, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med 2001; 345:1444–1451. [DOI] [PubMed] [Google Scholar]
- 34.Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006; 333:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolf PA, D’Agostino RB, Belanger AJ, et al. Probability of stroke: a risk profile from the Framingham Study. Stroke 1991; 22:312–318. [DOI] [PubMed] [Google Scholar]
- 36.Feigin VL, Lawes CM, Bennett DA, et al. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2003; 2:43–53. [DOI] [PubMed] [Google Scholar]
- 37.Gordon NF, Gulanick M, Costa F, et al. Physical activity and exercise recommendations for stroke survivors: an American Heart Association Scientific Statement from the council on clinical cardiology, subcommittee on exercise, cardiac rehabilitation, and prevention; the council on cardiovascular nursing; the council on nutrition, physical activity, and metabolism; and the stroke council. Circulation 2004; 109:2031–2041. [DOI] [PubMed] [Google Scholar]
- 38.Choi DC, Lee JY, Moon YJ, et al. Acupuncture-mediated inhibition of inflammation facilities significant functional recovery after spinal cord injury. Neurobiol Dis 2010; 39:272–282. [DOI] [PubMed] [Google Scholar]


