Abstract
To date, the effect of tooth loss on all-cause mortality among elderly patients with a different weight group has not been assessed. This retrospective cohort study evaluated the data obtained from a government-sponsored, annual physical examination program for elderly citizens residing in Taipei City during 2005 to 2007, and follow-up to December 31, 2010. We recruited 55,651 eligible citizens of Taipei City aged ≥65 years, including 29,572 men and 26,079 women, in our study. Their mortality data were ascertained based on the national death files. The number of missing teeth was used as a representative of oral health status. We used multivariate Cox proportional hazards regression analysis to determine the association between tooth loss and all-cause mortality. After adjustment for all confounders, the hazard ratios (HRs) of all-cause mortality in participants with no teeth, 1 to 9 teeth, and 10 to 19 teeth were 1.36 [95% confidence interval (CI): 1.15–1.61], 1.24 (95% CI: 1.08–1.42), and 1.19 (95% CI: 1.09–1.31), respectively, compared with participants with 20 or more teeth. A significant positive correlation of body mass index (BMI) with all-cause mortality was found in underweight and overweight elderly patients and was represented as a U-shaped curve. Subgroup analysis revealed a significant positive correlation in underweight (no teeth: HR = 1.49, 95% CI: 1.21–1.83; 1–9 teeth: HR = 1.23, 95% CI: 1.03–1.47; 10–19 teeth: HR = 1.20, 95% CI: 1.06–1.36) and overweight participants (no teeth: HR = 1.37, 95% CI: 1.05–1.79; 1–9 teeth: HR = 1.27, 95% CI: 1.07–1.52). The number of teeth lost is associated with an increased risk of all-cause mortality, particularly for participants with underweight and overweight.
INTRODUCTION
The global prevalence of periodontal disease (PD) is 20% to 50% of the overall population.1–3 This disease is caused by the accumulation of a specific bacterial biofilm around the teeth. The initial presentation is in the form of reversible gingivitis, which can be treated after biofilm removal.4,5 Subsequently, PD progresses with the destruction of the periodontal connective tissue and alveolar bone, which eventually results in tooth loss.6 Dental caries is also a common chronic disease that causes pain and disability across all age groups. If left untreated, dental caries can lead to pain and infection, tooth loss, and edentulism.7–9 The loss of teeth consequently influences the mastication and nutritional status of patients.10
Tooth loss is a crucial oral health problem in the elderly population and correcting this problem may reduce the elevated risk of associated mortality. Several studies have indicated a positive association between tooth loss and mortality among the elderly population. Most of these studies were conducted in countries outside Asia.11–14 In Japan, Ando et al15 conducted a 5.6-year cohort study of 7779 men aged 40 to 79 years, showing that men aged 40 to 64 years with no teeth had significantly higher mortality than that of men with ≥20 teeth; however, no associations were observed between the number of teeth and all-cause mortality among those aged 65 to 79 years. Ansai et al16 conducted a 5.5-year cohort study of 1282 subjects aged 80 years, indicating that tooth loss is a signification predictor of mortality in women, but not men. Another 10-year cohort study of 118 subjects aged 80 years or older by Morita et al17 showed that men with ≥20 teeth had an increased survival rate; however, this was not observed among women. Because of the inconsistent results of previous studies, a large-scale cohort study is required to further investigate the association of the number of teeth with mortality.
Several studies have focused on the association between tooth loss, body mass index (BMI), and mortality worldwide.18 Substantial evidence has suggested a direct association between tooth loss and diseases known to affect mortality,11,19–21 and numerous studies have begun to investigate the role of obesity in periodontitis.22,23 This association is being assessed because both tooth loss and obesity are associated directly with life-threatening diseases, such as cardiovascular diseases and stroke, and other diseases that have been known to affect health and mortality. Therefore, it is crucial to comprehend the interrelationships between tooth loss, BMI, and mortality, and to discover additional supporting evidence to explain this association scientifically and epidemiologically. Several studies have explained the link between tooth loss and diseases such as cardiovascular disease, stroke, and dementia.11,19,20 Moreover, numerous study groups have evaluated population samples to collect statistical data regarding the relationship between tooth loss and obesity.22,23 The collection of statistical information from various populations facilitates contemplating the association between tooth loss and obesity accurately. One study attempted to biologically explain the similarities between them, and reported that they are similar in their responses to inflammation in the body and in disease conditions, and that they are associated.22 The optimal BMI and the effects of tooth loss on the risk of mortality among elderly people remain unclear.
In this retrospective cohort study, we examined whether elderly participants with tooth loss had an increased mortality risk over a follow-up period of 6 years. Given that masticatory function mediates the link among oral health, body weight, and mortality, we expected a positive association between mortality and increased tooth loss. Tooth loss can affect both the dietary intake and nutritional status of elderly people,24,25 thereby influencing body weight and increasing the mortality risk. Therefore, we hypothesized that tooth loss is associated with all-cause mortality among elderly participants with varying BMIs.
MATERIALS AND METHODS
Study Population
In this retrospective cohort study, the cohort comprised 74,223 participants aged ≥55 years from a standard, annul physical examination program for the elderly population, conducted by the Taipei City government during 2005 to 2007. All citizens participated voluntarily, and were encouraged to visit annually, but the present study was conducted using only the results from the initial visits. The demographic and lifestyle data (eg, marital status, education level, smoking status, and alcohol consumption) were collected through self-administered questionnaires. During the medical checkup, blood pressure measurement, blood sample collection, and laboratory analyses were performed for each participant. We excluded 343 participants aged <65 years from the 74,223 participants, and further excluded 18,229 participants with missing survey data regarding BMI (n = 1062), marital status (n = 1427), education level (n = 9441), smoking status (n = 522), alcohol consumption (n = 533), the number of teeth present (n = 36), laboratory data (n = 2460), and details of the dental and prosthetic status (n = 2748). The final analytical sample comprised 55,651 participants, with 29,572 men, and 26,079 women. The data regarding participant identification were removed to ensure participant anonymity throughout the study period. The data acquisition and processing protocol were approved by the Institutional Review Board of Taipei City Hospital (IRB No.: TCHIRB-1030321-W).
Definition of the Number of Teeth
In this program, an oral examination was performed by dentists, which including the details of the dental and prosthetic status of each participant. The number of teeth was used to represent the oral health status and was arbitrarily categorized as follows: no teeth, 1 to 9 teeth, 10 to 19 teeth, and ≥20 teeth. A sensitivity analysis was also performed with the number of teeth as a continuous variable.14,15,26 In this study, missing teeth are defined by sites with nonrepairable roots and missing roots area with no fixed prosthesis present.
Definition of BMI
Both height and weight were measured during the examination by using standardized procedures. BMI was calculated as weight in kilograms divided by height in meters squared. We used the World Health Organization (WHO)-defined BMI-based categories of underweight (BMI < 18.5), normal weight (BMI = 18.5–24.9; reference category), overweight (BMI = 25.0–29.9), and obese (BMI ≥ 30).
Other Confounding Variables
Baseline data were collected, which included age (65–69 years; 70–74 years; 75–79 years; 80–84 years; and ≥85 years), sex, marital status (single; married/cohabiting), education level (none; 1–6 years; 7–12 years; and >12 years), regular dental prophylaxis (yes/no), smoking status in the past 6 months (the participants who had reported smoking every day or some days in the past 6 months were defined as smokers; those who had never smoked in the past 6 months were defined as nonsmokers); alcohol consumption in the past 6 months (the participants who had reported drinking every day or some days in the past 6 months were defined as drinkers; those who did not drink alcohol in the past 6 months were defined as nondrinkers). Diabetes mellitus was defined as either fasting blood sugar ≥126 mg/dL,27 self-report of physician-diagnosed diabetes mellitus, or the use of hypoglycemic medications. Hypertension was defined as either blood pressure >140/90 mm Hg,28 self-report of physician-diagnosed hypertension, or the use of antihypertension medications. Hyperlipidemia was defined as either triglyceride ≥200 mg/dL,29 and total cholesterol ≥200 mg/dL,30 self-report of physician-diagnosed hyperlipidemia, or the use of lipid-lowering medications.
Outcome Variables
We ascertained the vital status of the 55,651 study participants, as of December 31, 2010, through a computerized matching of their cohort IDs with the national death files. Information regarding the cause of death of the participants was coded according to the International Classification of Diseases, Ninth Revision (ICD-9), between 2006 and 2008 (ICD-9: 001-998) or ICD-10, between 2009 and 2010 (ICD-10: A00-Z99).
Statistical Analyses
The proportions of patients with specific numbers of teeth were calculated separately for the various subsamples. A χ2 test was used for single-variable analysis. Cumulative incidence analyses were performed using the Kaplan–Meier method, and the differences between the curves were calculated using the 2-tailed log rank test. We calculated the relative risk of all-cause mortality by using multivariate Cox proportional hazard models. The examination date was considered the time of entry into the study, and the end of follow-up (December 31, 2010) or the date of death, whichever was earlier, was considered the time of exit. The potential risk factors for all-cause mortality, including age, sex, marital status, education level, regular dental prophylaxis, smoking status, alcohol consumption, diabetes mellitus, hypertension, hyperlipidemia, and nonregular dental prophylaxis, were incorporated into the model. Propensity score-based approaches are currently the most effective statistical technologies for addressing selection bias for time-independent treatments.31 Therefore, we used propensity score-based approaches to investigate the causal effects of the number of teeth on mortality given comparable participant characteristics, BMI, lifestyle factors, and laboratory measures. In addition, we considered the number of teeth as a continuous variable and used different tooth loss definitions (eg, patients with partial or complete removable dentures were considered to have no missing teeth for the sensitivity analysis). Stratified Cox proportional hazard regression analysis was used to estimate the effect of the number of teeth on all-cause mortality. We conducted all analyses by using SAS (version 9.3; SAS Institute, Inc., Cary, NC) and STATA (version 13.0; STATA Corp, College Station, TX) statistical software packages.
RESULTS
Participant Characteristics
Table 1 summarizes the proportions of patients with the number of teeth and their baseline characteristics as well as the follow-up duration or mortality rate. The mean age of the participants was 73.34 [standard deviation (SD): 6.28] years. During the 6-year study period, 177,601 person-years of follow-up were recorded, with an average follow-up period of 3.04 (SD: 1.81) years. At the baseline, 81.76% of the elderly patients had 20 teeth or more, 12.07% had 10 to 19 teeth, 4.04% had 1 to 9 teeth, and 2.12% had no teeth. Overall, 3530 (6.34% of all participants) deaths occurred during the 6-year follow-up period. Participants with no teeth exhibited a higher mortality rate (12.53%) than did those with 10 to 19 teeth (8.01%) and those with 20 teeth or more (5.74%). A high prevalence of tooth loss was observed among participants who were men, older, underweight, single, and smokers and those who had lower education levels, diabetes mellitus, hypertension, hyperlipidemia, and nonregular dental prophylaxis.
TABLE 1.
Baseline Characteristic of Participants
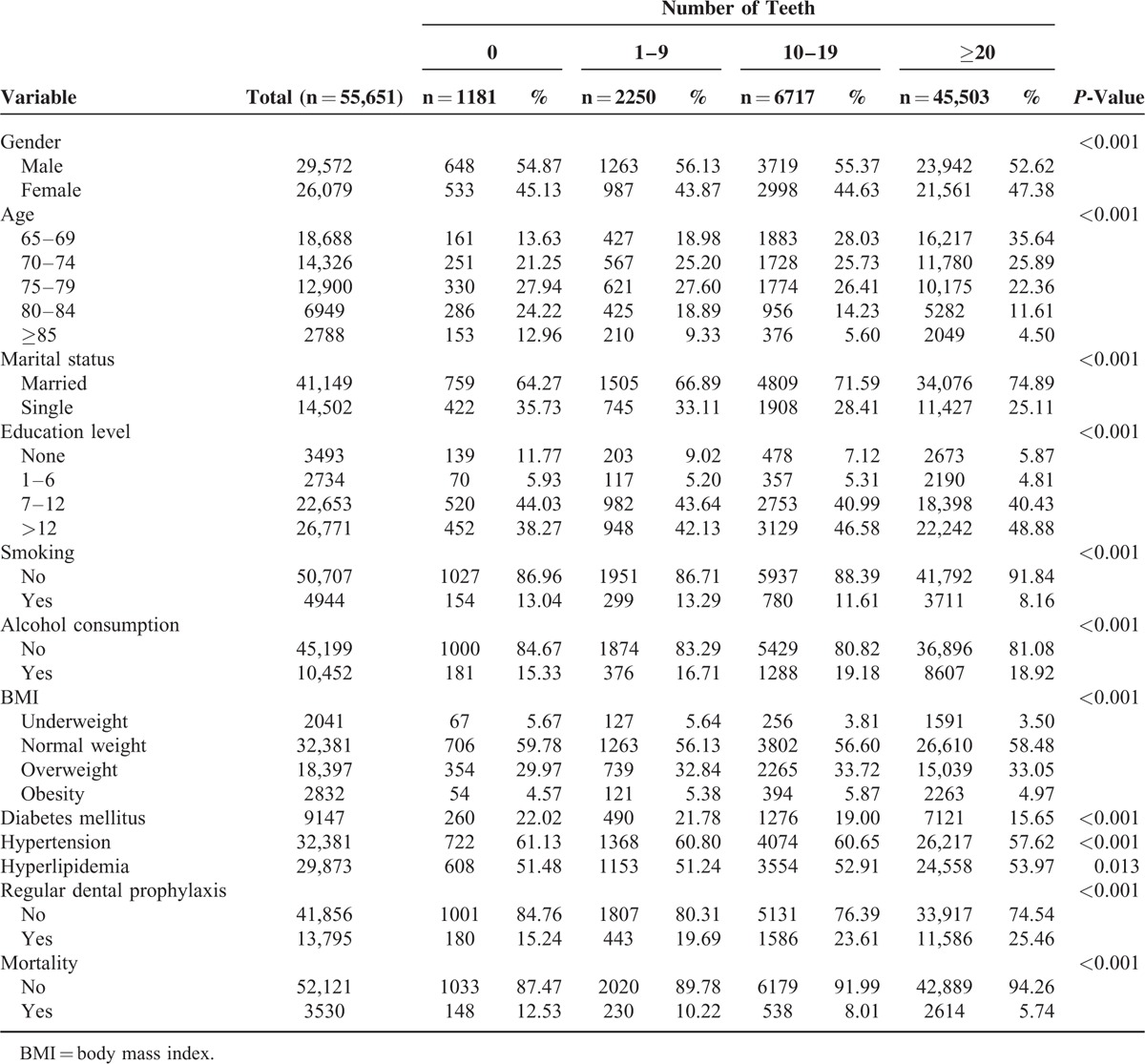
Association Between the Number of Teeth and Mortality
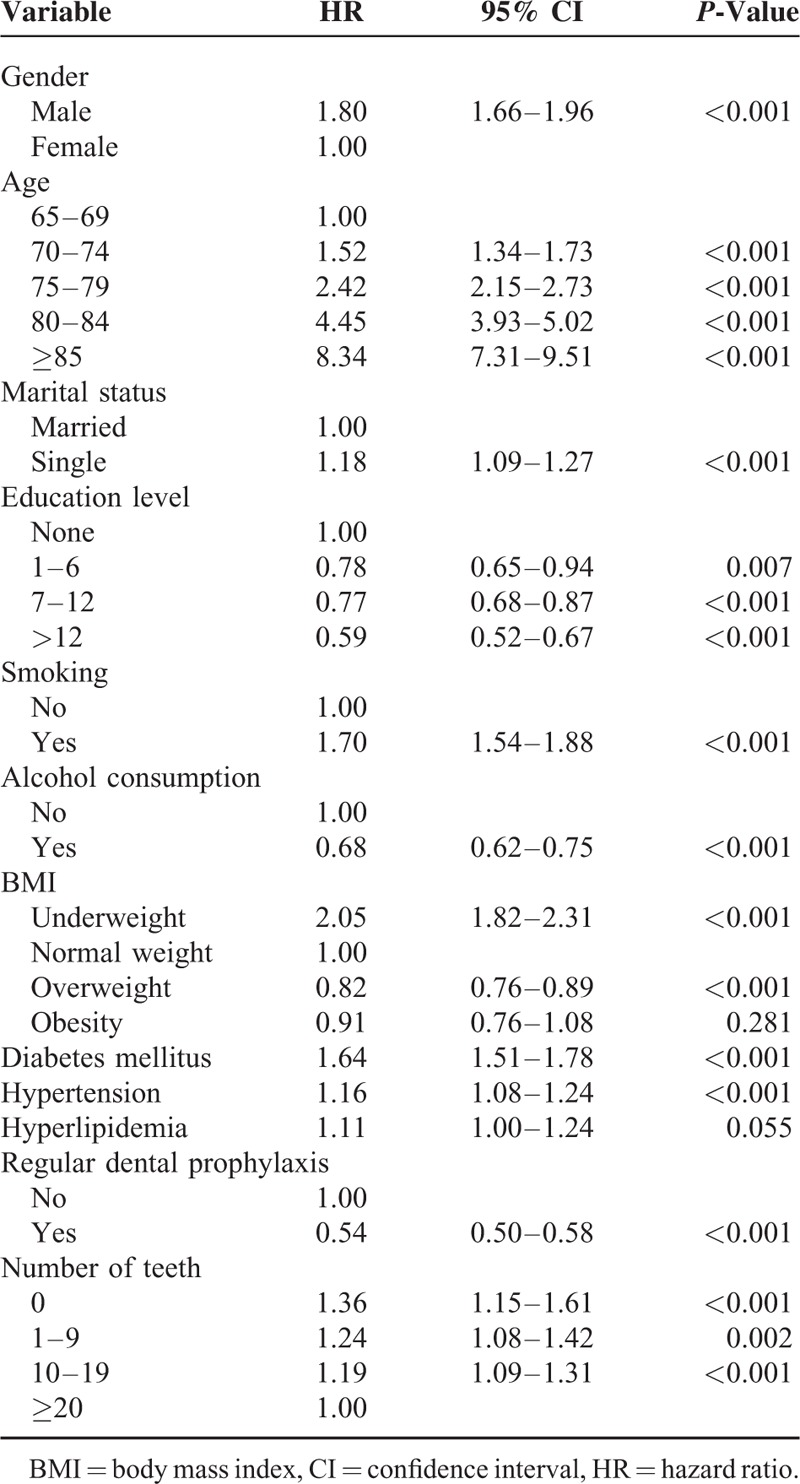
We observed a positive association between the number of teeth lost and all-cause mortality (Figure 1). After control for other covariates, participants with a high number of teeth lost exhibited significantly higher hazard ratios (HRs) for all-cause mortality (no teeth: HR = 1.36, 95% confidence interval (CI): 1.15–1.61; 1–9 teeth: HR = 1.24, 95% CI: 1.08–1.42; 10–19 teeth: HR = 1.19, 95% CI: 1.09–1.31) (Table 2). Multivariate Cox proportional hazard analysis identified the male sex (HR = 1.80, 95% CI: 1.66–1.96), an older age, a lower education level, a single status (HR = 1.18, 95% CI: 1.09–1.27), smoking (HR = 1.70, 95% CI: 1.54–1.88), diabetes mellitus (HR = 1.64; 95% CI: 1.51–1.78), and hypertension (HR = 1.16, 95% CI: 1.08–1.24) as independent risk factors for mortality. Participants with regular dental prophylaxis had lower mortality (HR = 0.54, 95% CI: 0.50–0.58) than did participants with nonregular dental prophylaxis. Among the BMI-based categories, underweight participants exhibited a significantly higher mortality risk compared with that of normal weight participants (HR = 2.05, 95% CI: 1.82–2.31).
FIGURE 1.
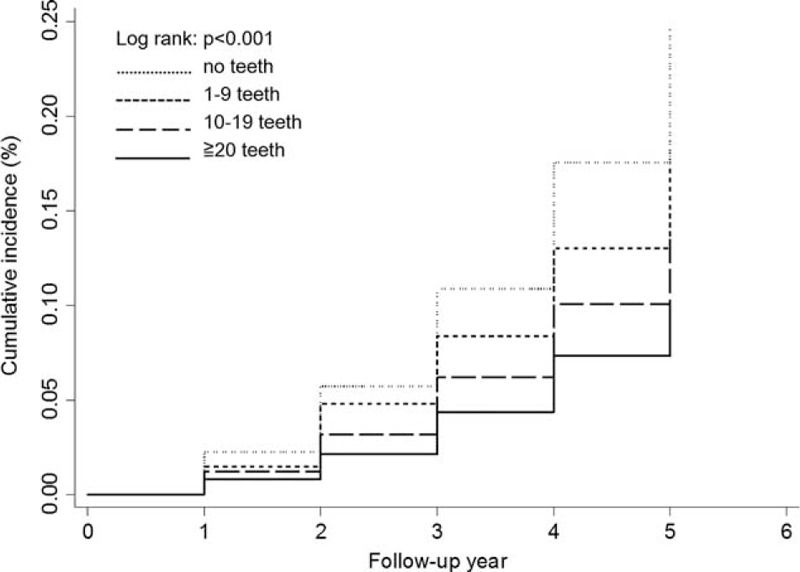
Six-year cumulative incidences of all-cause mortality.
TABLE 2.
Multivariate Cox Proportional Model of Factors Associated With All-Cause Mortality
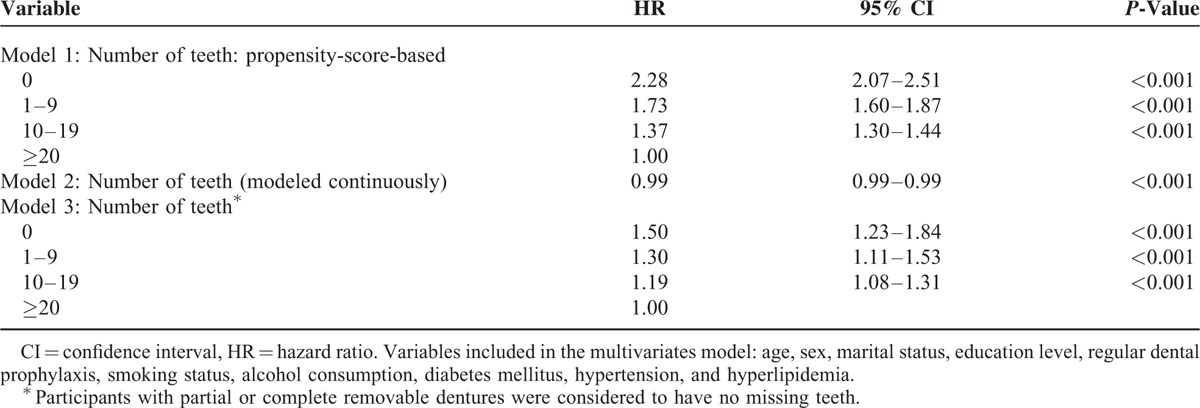
Sensitivity Analysis of Associations Between the Number of Teeth and Mortality
The results of the sensitivity analysis of the associations between the number of teeth and mortality are shown in Table 3. Propensity score-based approaches for investigating the causal effects of the number of teeth on mortality revealed a significant association between the number of teeth and all-cause mortality (no teeth: HR = 2.28, 95% CI: 2.07–2.51; 1–9 teeth: HR = 1.73, 95% CI: 1.60–1.87; and 10–19 teeth: HR = 1.37, 95% CI: 1.30–1.44). When the number of teeth was considered a continuous variable, participants with all numbers of teeth had a significantly decreased all-cause mortality risk (HR = 0.99, 95% CI: 0.99–0.99). In our study, 32.8% of participants wore partial or complete removable dentures. We also used different definitions of the number of teeth (eg, participants with partial or complete removable dentures were considered to have no missing teeth for the sensitivity analysis), and the results remained robust (no teeth: HR = 1.50, 95% CI: 1.23–1.84; 1–9 teeth: HR = 1.30, 95% CI: 1.11–1.53; 10–19 teeth: HR = 1.19, 95% CI: 1.08–1.31).
TABLE 3.
Sensitivity Analysis of the Associations Between the Number of Teeth and Mortality
Subgroup Analysis of Associations Between the Number of Teeth and Mortality
The results of the subgroup analyses are shown in Figure 2. The HRs exhibited similar trends for each subgroup. Among the male participants, those with <20 teeth where significantly associated with increased all-cause mortality (no teeth: HR = 1.38, 95% CI: 1.13–1.68; 1–9 teeth: HR = 1.38, 95% CI: 1.18–1.62; 10–19 teeth: HR = 1.24, 95% CI: 1.11–1.38). Among the underweight participants, a significant association was observed between the number of teeth lost and all-cause mortality (no teeth: HR = 1.49, 95% CI: 1.21–1.83; 1–9 teeth: HR = 1.23, 95% CI: 1.03–1.47; 10–19 teeth: HR = 1.20, 95% CI: 1.06–1.36). Among the overweight participants, those with <10 teeth exhibited a significantly high mortality risk (no teeth: HR = 1.37, 95% CI: 1.05–1.79; 1–9 teeth: HR = 1.27, 95% CI: 1.07–1.52). Among the normal weight and obese participants, no significant association was observed between the number of teeth and all-cause mortality.
FIGURE 2.
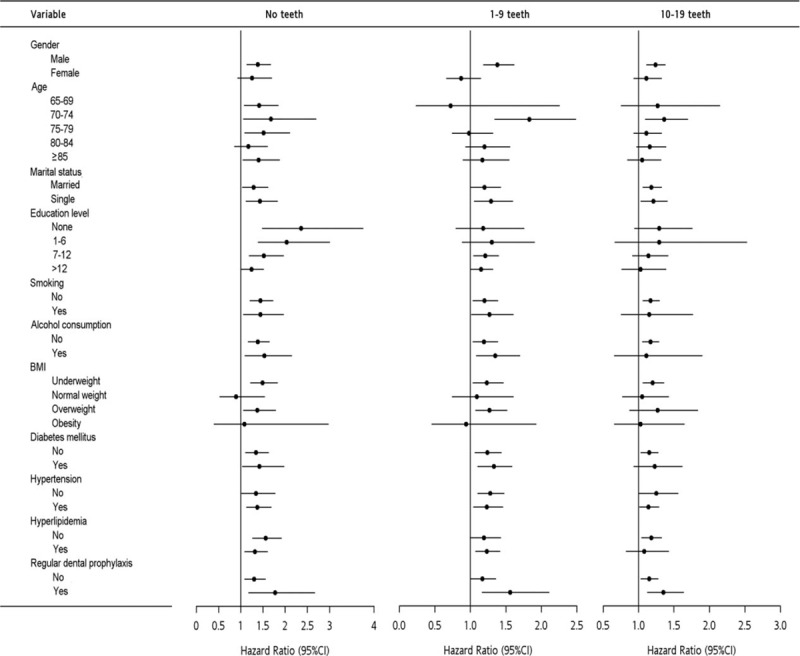
Subgroup analysis of all-cause mortality.
DISCUSSION
In this study, we demonstrated an association between the number of teeth lost and an increased risk of all-cause mortality. The patients who had lost 11 to 20 and >20 teeth, particularly underweight participants, exhibited a significantly higher risk of all-cause mortality compared with those who had lost 0 to 10 teeth. Although previous studies have investigated the relationship between tooth loss and all-cause mortality, they have not included the category of BMI.26,32,33 In addition, despite the inclusion of BMI,12–14,16,20 no subgroup analysis has been conducted by categorizing overweight and underweight participants, despite such associations being able to be determined, because both stroke and dementia have been associated with being underweight. Tooth loss influences mastication and nutritional status.10 Poor nutrition may be related to being underweight. Moreover, tooth loss can be associated with being underweight based on the overlapping diseases that occur under both these conditions. Thus, it is crucial to understand the relationship between these diseases and tooth loss, and their effects on mortality through statistical analyses.
Our findings demonstrated an association between the number of teeth lost and an increased risk of all-cause mortality. Most previous studies in countries other than Asian have evaluated the relationship between tooth loss and a single cause of mortality. Tooth loss is a risk indicator for various diseases such as cardiovascular disease,33,34 stroke,11 and dementia.35,36 Several recent studies have proposed that oral diseases may lead to systemic inflammation,11,37,38 as indicated by increased C-reactive protein levels. Inflammation, possibly within the central nervous system, is believed to play a pivotal role in the pathogenesis of dementia37 and stroke.39
Our study found that male participants aged 65 years or older with less than 20 teeth were significantly associated with increased all-cause mortality, which is consistent with the findings of the previous study by Morita et al,17 but inconsistent with those of other Asian cohort studies by Ando et al15 and Ansai et al.16 The prevalence of participants with less than 20 teeth in these 2 studies was higher than 50%, which is much higher than that in our study (6.17% had lost >20 teeth). These participants might represent a group of frailer elderly people, which may explain the different observation in our study.
In our study, the loss of 11 to 20 and >20 teeth was associated with an increased risk of all-cause mortality among underweight patients. Previous studies have found an association between being underweight and increased mortality.40–43 Tooth loss influences dietary choices; older people with many missing teeth consume less meat, fruit, beans, and oils, and primarily obtain their required energy from solid fats, alcohol, and added sugar. Therefore, tooth loss can affect both the dietary intake and nutritional status of such people,24,25 thereby increasing the risk of mortality. Although we did not find a dose–effect relationship between tooth loss and mortality among the underweight participants, we obtained a significant HR when tooth loss was treated as a continuous variable.
Socioeconomic status (SES) may be a crucial confounder for not only prosthodontic replacement but also mortality. A meta-analysis by Polzer et al18 indicated that if published results are not adjusted for SES, the effect of missing prosthodontic replacement on mortality is likely to be overestimated. Although dental services are covered by the National Health Insurance program in Taiwan, prosthodontic replacement is not included. In this study, we adjusted only for the education level, which was used as a proxy of SES. We cannot rule out the possibility that SES had a residual confounding effect.
By contrast, subgroup analysis showed that overweight participants with severe tooth loss had an increase of 27% to 37% in mortality, with overweight participants having a lower risk of mortality (18% reduction in mortality). The impact of severe tooth loss on mortality cannot be ignored. Therefore, not only underweight participants but also overweight participants should pay attention to oral hygiene to reduce the risk of tooth loss. In addition, the obese participants exhibited an association between tooth loss and mortality, but this association was statistically nonsignificant. Based on our results, we recommend that public health efforts include population-wide strategies and resources to ensure that oral health programs are available from early life onward, with the aim of reducing the prevalence of tooth loss and mortality.
Our study has several limitations. First, information on other confounding factors that might affect tooth loss and mortality, such as dementia, cerebrovascular disease, stroke, and cancer, was not available. Although our analyses were adjusted for common chronic health conditions and baseline patient characteristics, it is possible that subclinical diseases or other diseases not measured contribute to decreased survival. Additional studies are required to evaluate the impact of this confounder on the association between tooth loss and mortality. Second, information bias in subject characteristics and comorbidities cannot be avoided in studies using self-report questionnaires. However, the comorbidities in this study were combined with data on laboratory parameters, reducing the possibility of recall bias. Third, we used the baseline examination data to represent all of the participants in the cohort. These data may have changed with time, thus conferring complex effects on the respective mortality rates. However, our results demonstrate the value of a single determination of tooth loss in predicting the risk of mortality. Fourth, the participants in our study may not be representative of the general population. However, because the risk comparison was based on internal comparisons, the calculated relative risks are a reasonable estimate of those in the general population. Finally, a total of 20% of the people had missing survey data and laboratory data. Underweight people and those with tooth loss >20 were more likely to have missing data. Because mortality was more prevalent among these groups than among those with complete information, our findings underestimate the true differences and are conservative.
In conclusion, the number of teeth lost is associated with an increased risk of all-cause mortality. All-cause mortality includes causes such as cardiovascular disease, stroke, and dementia, and these diseases are strongly associated with tooth loss and being underweight. Tooth loss could lead directly to influence dietary choices or poor digestion, thus resulting in becoming underweight. This might explain the association between the increased risk of all-cause mortality and tooth loss, particularly in underweight people. Our results indicated a bidirectional relationship between all-cause mortality and tooth loss, and further research must be conducted to explore the mechanisms underlying the empirical associations observed in our study.
Acknowledgments
This study is based (in part) on data from the Taipei City Public Health Database provided by the Department of Health, Taipei City Government, and managed by Databank for Public Health Analysis. The interpretation and conclusions contained herein do not represent those of Department of Health, Taipei City Government, or Databank for Public Health Analysis.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, HR = hazard ratio, ICD = International Classification of Diseases, PD = periodontal disease, SD = standard deviation, SES = socioeconomic status.
The authors have no funding and conflicts of interest to disclose.
This study was supported by the Department of Health, Taipei City Government (10401-62-061).
REFERENCES
- 1.Albandar JM, Rams TE. Global epidemiology of periodontal diseases: an overview. Periodontol 2000 2002; 29:7–10. [DOI] [PubMed] [Google Scholar]
- 2.Albandar JM. Underestimation of periodontitis in NHANES surveys. J Periodontol 2011; 82:337–341. [DOI] [PubMed] [Google Scholar]
- 3.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 2007; 11:1–92. [PubMed] [Google Scholar]
- 4.Petersen PE, Ogawa H. Strengthening the prevention of periodontal disease: the WHO approach. J Periodontol 2005; 76:2187–2193. [DOI] [PubMed] [Google Scholar]
- 5.Paster BJ, Boches SK, Galvin JL, et al. Bacterial diversity in human subgingival plaque. J Bacteriol 2001; 183:3770–3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet 2005; 366:1809–1820. [DOI] [PubMed] [Google Scholar]
- 7.Baelum V, Fejerskov O. Tooth loss as related to dental caries and periodontal breakdown in adult Tanzanians. Community Dent Oral Epidemiol 1986; 14:353–357. [DOI] [PubMed] [Google Scholar]
- 8.Beltran-Aguilar ED, Barker LK, Canto MT, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis—United States, 1988–1994 and 1999–2002. MMWR Surveill Summ 2005; 54:1–43. [PubMed] [Google Scholar]
- 9.Kida IA, Astrom AN, Strand GV, et al. Clinical and socio-behavioral correlates of tooth loss: a study of older adults in Tanzania. BMC Oral Health 2006; 6:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimazaki Y, Soh I, Saito T, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res 2001; 80:340–345. [DOI] [PubMed] [Google Scholar]
- 11.Watt RG, Tsakos G, de Oliveira C, et al. Tooth loss and cardiovascular disease mortality risk—results from the Scottish Health Survey. PLoS One 2012; 7:e30797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Padilha DM, Hilgert JB, Hugo FN, et al. Number of teeth and mortality risk in the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci 2008; 63:739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osterberg T, Carlsson GE, Sundh V, et al. Number of teeth—a predictor of mortality in the elderly? A population study in three Nordic localities. Acta Odontol Scand 2007; 65:335–340. [DOI] [PubMed] [Google Scholar]
- 14.Osterberg T, Carlsson GE, Sundh V, et al. Number of teeth—a predictor of mortality in 70-year-old subjects. Community Dent Oral Epidemiol 2008; 36:258–268. [DOI] [PubMed] [Google Scholar]
- 15.Ando A, Tanno K, Ohsawa M, et al. Associations of number of teeth with risks for all-cause mortality and cause-specific mortality in middle-aged and elderly men in the northern part of Japan: the Iwate-KENCO study. Community Dent Oral Epidemiol 2014; 42:358–365. [DOI] [PubMed] [Google Scholar]
- 16.Ansai T, Takata Y, Soh I, et al. Relationship between tooth loss and mortality in 80-year-old Japanese community-dwelling subjects. BMC Public Health 2010; 10:386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morita I, Nakagaki H, Kato K, et al. Relationship between survival rates and numbers of natural teeth in an elderly Japanese population. Gerodontology 2006; 23:214–218. [DOI] [PubMed] [Google Scholar]
- 18.Polzer I, Schwahn C, Volzke H, et al. The association of tooth loss with all-cause and circulatory mortality. Is there a benefit of replaced teeth? A systematic review and meta-analysis. Clin Oral Investig 2012; 16:333–351. [DOI] [PubMed] [Google Scholar]
- 19.Uppoor AS, Lohi HS, Nayak D. Periodontitis and Alzheimer's disease: oral systemic link still on the rise? Gerodontology 2013; 30:239–242. [DOI] [PubMed] [Google Scholar]
- 20.Abnet CC, Qiao YL, Dawsey SM, et al. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int J Epidemiol 2005; 34:467–474. [DOI] [PubMed] [Google Scholar]
- 21.Hayasaka K, Tomata Y, Aida J, et al. Tooth loss and mortality in elderly Japanese adults: effect of oral care. J Am Geriatr Soc 2013; 61:815–820. [DOI] [PubMed] [Google Scholar]
- 22.Krejci CB, Bissada NF. Obesity and periodontitis: a link. Gen Dent 2013; 61:60–63.quiz 4. [PubMed] [Google Scholar]
- 23.Khader YS, Bawadi HA, Haroun TF, et al. The association between periodontal disease and obesity among adults in Jordan. J Clin Periodontol 2009; 36:18–24. [DOI] [PubMed] [Google Scholar]
- 24.Savoca MR, Arcury TA, Leng X, et al. Severe tooth loss in older adults as a key indicator of compromised dietary quality. Public Health Nutr 2010; 13:466–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perera R, Ekanayake L. Relationship between nutritional status and tooth loss in an older population from Sri Lanka. Gerodontology 2012; 29:e566–e570. [DOI] [PubMed] [Google Scholar]
- 26.Holm-Pedersen P, Schultz-Larsen K, Christiansen N, et al. Tooth loss and subsequent disability and mortality in old age. J Am Geriatr Soc 2008; 56:429–435. [DOI] [PubMed] [Google Scholar]
- 27.Boden-Albala B, Cammack S, Chong J, et al. Diabetes, fasting glucose levels, and risk of ischemic stroke and vascular events: findings from the Northern Manhattan Study (NOMAS). Diabetes Care 2008; 31:1132–1137. [DOI] [PubMed] [Google Scholar]
- 28.Kelly TN, Gu D, Chen J, et al. Hypertension subtype and risk of cardiovascular disease in Chinese adults. Circulation 2008; 118:1558–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Third Report of the National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143–3421. [PubMed] [Google Scholar]
- 30.Jacobs D, Blackburn H, Higgins M, et al. Report of the Conference on Low Blood Cholesterol: Mortality Associations. Circulation 1992; 86:1046–1060. [DOI] [PubMed] [Google Scholar]
- 31.Newgard CD, Hedges JR, Arthur M, et al. Advanced statistics: the propensity score—a method for estimating treatment effect in observational research. Acad Emerg Med 2004; 11:953–961. [DOI] [PubMed] [Google Scholar]
- 32.Jansson L, Lavstedt S, Frithiof L. Relationship between oral health and mortality rate. J Clin Periodontol 2002; 29:1029–1034. [DOI] [PubMed] [Google Scholar]
- 33.Tu YK, Galobardes B, Smith GD, et al. Associations between tooth loss and mortality patterns in the Glasgow Alumni Cohort. Heart 2007; 93:1098–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwahn C, Polzer I, Haring R, et al. Missing, unreplaced teeth and risk of all-cause and cardiovascular mortality. Int J Cardiol 2013; 167:1430–1437. [DOI] [PubMed] [Google Scholar]
- 35.Kim JM, Stewart R, Prince M, et al. Dental health, nutritional status and recent-onset dementia in a Korean community population. Int J Geriatr Psychiatry 2007; 22:850–855. [DOI] [PubMed] [Google Scholar]
- 36.Steele J. Tooth loss may be more frequent in older people with a genetic predisposition towards dementia. J Evid Based Dent Pract 2008; 8:253–254. [DOI] [PubMed] [Google Scholar]
- 37.Kamer AR, Craig RG, Dasanayake AP, et al. Inflammation and Alzheimer's disease: possible role of periodontal diseases. Alzheimers Dement 2008; 4:242–250. [DOI] [PubMed] [Google Scholar]
- 38.Bahekar AA, Singh S, Saha S, et al. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J 2007; 154:830–837. [DOI] [PubMed] [Google Scholar]
- 39.Lee YL, Hu HY, Huang N, et al. Dental prophylaxis and periodontal treatment are protective factors to ischemic stroke. Stroke 2013; 44:1026–1030. [DOI] [PubMed] [Google Scholar]
- 40.Flegal KM, Graubard BI, Williamson DF, et al. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 2007; 298:2028–2037. [DOI] [PubMed] [Google Scholar]
- 41.Nagai M, Kuriyama S, Kakizaki M, et al. Effect of age on the association between body mass index and all-cause mortality: the Ohsaki cohort study. J Epidemiol 2010; 20:398–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang Y, Wang Y, Qain Y, et al. Association of body mass index with cause specific deaths in Chinese elderly hypertensive patients: Minhang community study. PLoS One 2013; 8:e71223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu CY, Chou YC, Huang N, et al. Association of body mass index with all-cause and cardiovascular disease mortality in the elderly. PLoS One 2014; 9:e102589. [DOI] [PMC free article] [PubMed] [Google Scholar]


