Abstract
Esophageal stricture is a severe adverse event after circumferential endoscopic submucosal dissection (ESD). Steroid administration is a new method to prevent stricture formation. We performed a meta-analysis to investigate the efficacy and safety of steroid administration to prevent esophageal stricture after circumferential ESD.
PubMed, the Cochrane Library, EMBASE, Chinese Biomedical Database, and Clinicaltrials.gov were searched. Studies on steroid administration + endoscopic balloon dilation (EBD) versus EBD alone for esophageal stricture were included and pooled analyzed in random-effects models. Besides, subgroup analysis and network analysis were performed to define the influence of ESD type and steroid administration method.
Twelve studies involving 513 patients were included. Meta-analysis showed that steroid administration significantly achieved a lower stricture rate (risk ratio [RR], 0.40; 95% CI, 0.20–0.81) and less required EBD sessions (mean difference [MD], −4.33; 95% CI, −6.10 to −2.57) than control. Subgroup analysis indicated that steroid was effective after both semi- and complete circumferential ESD. Network meta-analysis showed that compared with oral steroid, local injected steroid had a similar effect to prevent stricture (RR, 1.16; 95% CI, 0.48–2.85), whereas a better effect to reduce required EBD sessions (MD, 7.77; 95%CI, 0.26–15.3).
Additional steroid administration is effective to reduce the stricture rate and required EBD sessions. And local injected steroid was superior to oral steroid in EBD reduction, whereas due to the varied method and dose of steroid administration, the finding needs to be clarified in the future.
INTRODUCTION
Esophageal cancer is the eighth most common cancer with an estimated 455,800 new cases and 400,200 deaths in 2012 worldwide, and ∼22% of them were located in eastern Asia and 40% in southern and eastern Africa.1 It is considered to be aggressive that often presents at an advanced stage.2 Besides accurate diagnosis, endoscopic esophageal surgery enables en bloc and complete resection in both endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD).3 However, ESD is always associated with longer operation time and higher complication rate than EMR due to larger resected size, especially when applied to tumor size >20 mm.4 Because esophagus is a narrow and hollow organ, previous studies reported the frequency of stricture ranged from 70% to 90% after semicircumferential esophageal ESD, which usually defected >3/4 of the esophagus circumference.5,6 And the frequency would be even higher to 100% after complete circumferential esophageal ESD.
Endoscopic balloon dilation (EBD) is an effective way to treat post-ESD strictures, while there is a high recurrence.7 As known, repeated EBD sessions would increase relevant complications including perforation and bleeding as well as patients’ uncomfortableness and inconvenience.8 In this case, additional steroid is tried to be administrated to prevent stricture formation and to reduce EBD sessions. In fact, steroid administration is developed to a variety of prevention with conflicting effects and conclusions for a long time. It did not prevent stricture development while might lead to serious adverse events for corrosive esophageal burns,9 and provided limited short- and long-term benefits in lumbar spinal stenosis,10 whereas it seemed to prolong time to stricture recurrence after internal urethrotomy,11 and resulted in striking clinical effects and a significant reduction of restenosis after coronary artery stent implantation.12
Based on current knowledge, the efficacy and safety of additional steroid administration to prevent strictures varied in kinds of diseases and surgeries. Meanwhile, the method of steroid administration would also affect the clinical outcomes. In recent years, several studies have investigated the efficacy of additional steroid administration versus EBD alone to prevent post-ESD strictures with limited sample sizes and inconsistent results.13–24 The purpose of this meta-analysis was to systematically evaluate the efficacy and safety of additional steroid administration for esophageal stricture and the influence of ESD type and steroid administration method.
METHODS
The meta-analysis was performed and reported mainly according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).25 The meta-analysis itself did not involve ethical issue.
Literature Search and Inclusion Criteria
We conducted a comprehensive literature search to identify all relevant studies that investigated the effects of steroid administration including endoscopic local injection, taking oral and superficial application for esophageal stricture after endoscopic circumferential ESD. PubMed, the Cochrane Library, EMBASE, and Chinese Biomedical Literature Database were searched up to March 2015. Language was restricted to English and Chinese. Search terms used were as follows: steroid, corticosteroid, triamcinolone, prednisolone, dexamethasone, esophageal, esophagus, gullet, surgery, esophagectomy, dissection, resection, stricture, stenosis, constriction, straitness, angusty. Related articles function was used, and references in relevant reviews and comparative studies were also screened. The website of Clinicaltrials.gov and Google Scholar were complementally searched to further widen literature search results.
Articles were critically reviewed by 2 researchers for eligibility in the study. Inclusion criteria on study design, participants, interventions, and outcomes were as follows: (1) randomized controlled trials (RCTs) and nonrandomized controlled studies (non-RCTs); (2) participants were patients diagnosed as early esophageal cancer and underwent circumferential ESD; (3) interventions were steroid administration and required EBD in the steroid group, whereas required EBD alone in the control group; (4) outcome measures included the stricture rate, required EBD sessions, and steroid-related complications. Multiple articles published by the same team were carefully compared in aspects of the study duration and case number in order to only include the latest or the most detailed one. Reviews, case series, and patients with esophageal corrosive injury were excluded.
Data Extraction
Two reviewers extracted data independently and cross-checked the items. Data about study characteristics and outcome measures were extracted as follows: (1) first author, publication year, study design, cases in each group, sex and average age of patients, intervention, resected size of esophageal submucosal, and follow-up period; (2) stricture rate, required EBD sessions, and steroid-related complications. Any disagreement was solved though discussion.
Stricture formation was defined as an inability to pass though a standard endoscope of 9.2 to 10 mm diameter with patient's complaint of dysphagia. And required EBD was defined as the number of EBD performed by a balloon dilator and repeated times until the endoscope could pass the former stricture. Semicircumference was defined as dissected margin extending more than two-thirds of esophagus but not the complete esophageal circumference.
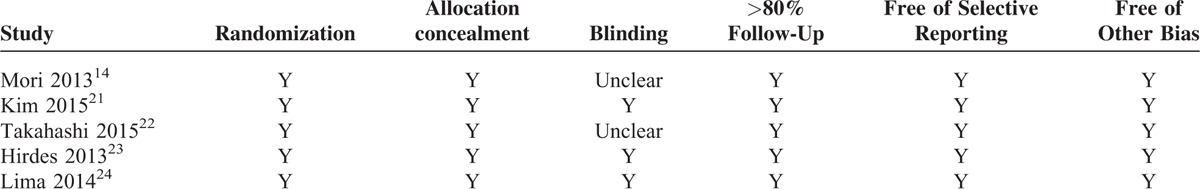
Methodological Quality Assessment
Two methods were adopted to assess methodological quality due to the included study design. The quality of RCTs was assessed by methods recommended by the Cochrane Handbook,26 which included 6 items: randomization, allocation concealment, blinding, lost to follow-up, selective reporting result, and other potential bias. The quality of non-RCTs was assessed by Newcastle–Ottawa scale,27 which had 3 sections: patient selection, comparability of group, and outcome/exposure, with a total of 8 items and 9 stars. A study achieving 5 stars was considered high quality.
Statistical Analysis
Review Manger (Version 5.3, Nordic Cochrane Center, Copenhagen, Denmark) was used to analyze data in the meta-analysis. Data values for pooled analysis were immediately extracted or calculated from the published articles. For overall effects, risk ratios (RR) was adopted to describe dichotomous variables, and mean difference (MD) for continuous variables, both with their respective 95% confidence intervals (95%CI). P < 0.05 was considered significant difference existed. After considering clinical factors by subgroup analysis, statistical heterogeneity across studies was tested by chi-square statistic and presented by the I2 value. Because of the unavoidable heterogeneity across the studies, we only used a random-effects model to analyze data. This provides a more conservative estimate and wider 95%CI.28 Sensitivity analysis was performed by omitting relative poor-quality studies to observe the stability of results and whether they would be influenced by studies with potential bias.13,16,17 Trial sequence analysis (TSA) was also performed to show the changing trend of results according to publication time and to determine whether the total sample size was enough to achieve a real and certain result.29 TSA was performed by TSA software (Version 1.0, Center for Clinical Intervention Research, Copenhagen, Denmark). To compare the influence of different steroid administration methods, we further conducted a network meta-analysis by ITC software (Version 1.0, Canadian Agency for Drugs and Technologies in Health, Ontario, Canada), and it was a useful and effective tool to investigate the preliminary difference between local injected and oral steroid when currently lacking of direct comparison.30
RESULTS
Study Characteristics and Methodological Quality
The literature search identified 412 abstracts for primary review. Finally, 12 studies meeting the inclusion criteria were included for analysis (Fig. 1). There were 5 RCTs,14,21–24 5 cohort studies,15,17–20 and 2 case-control studies.13,16 The combined studies contained 513 patients, of whom 255 are in the steroid group and 258 in the control group. The characteristics of included studies were presented in Table 1. The case number ranged from 14 to 83, with average age in the range from 52 to 75 years. Standard circumferential ESD was performed for the patients, and 8 studies enrolled dissection margins extending over 3/4 of esophageal circumference,13,15–17,18–22 2 studies enrolled over 2/3 of esophageal,14,18 4 studies meanwhile enrolled complete ESD.15,19,20,22 The resected size was also listed in Table 1, and there was no significant difference between the groups in each study. Three kinds of steroid administration methods were included as follows: endoscopic local injection,13,14,16,17,19,21–24 oral,15,18,20 and superficial application,14 as shown in Table 2. Of the RCTs, except 2 of them did not report blinding,14,22 all the other studies were well performed in all the other items; all non-RCTs scored >5 stars,13,15–20 as shown in Tables 3 and 4.
FIGURE 1.
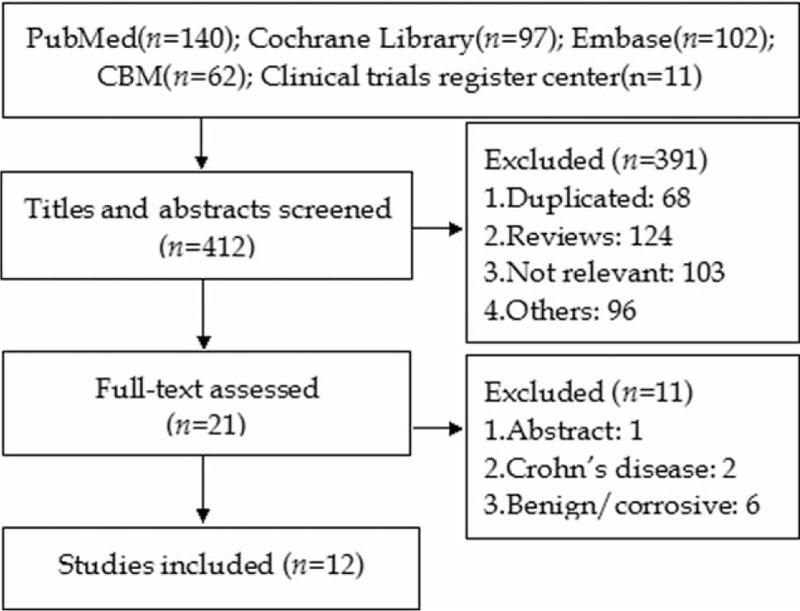
Article identified process from initial search to final decision.
TABLE 1.
Characteristic of the Included Studies
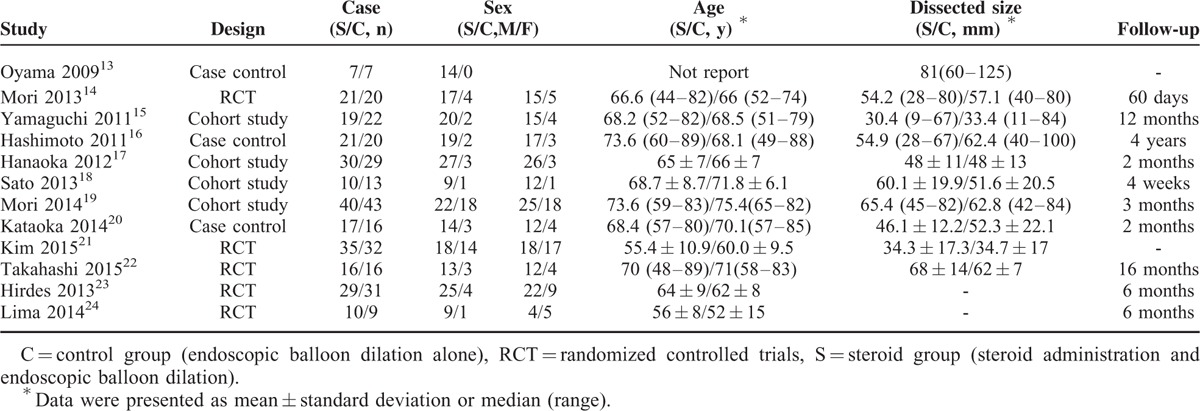
TABLE 2.
Methods of Injected and Oral Steroid Described in the Studies
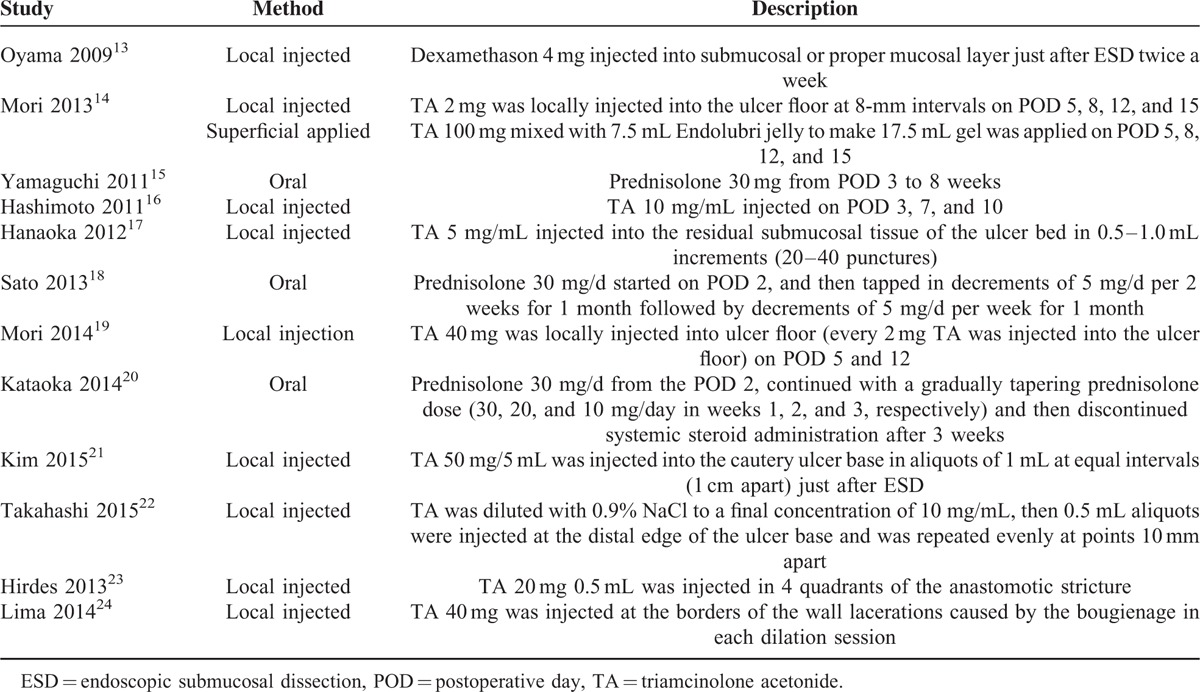
TABLE 3.
Quality Assessment Result Based on Newcastle-Ottawa Quality Assessment Scale
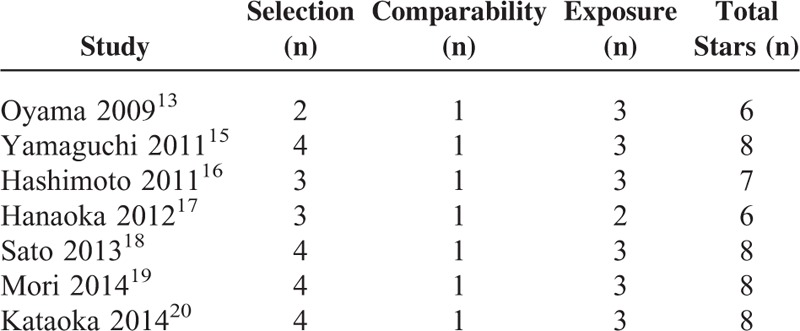
TABLE 4.
Quality Assessment Result Based on Methods Recommended by Cochrane Handbook
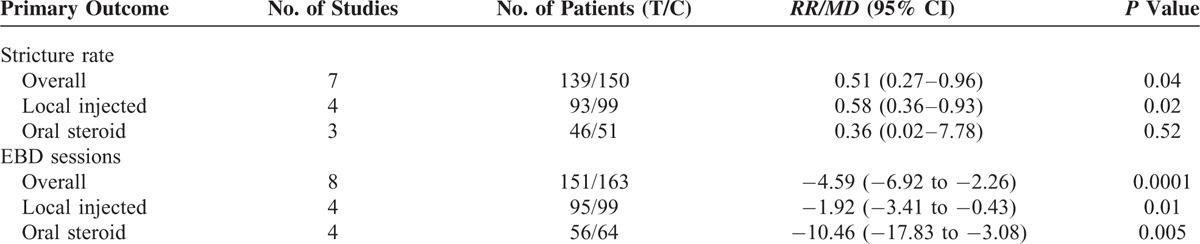
Stricture Rate
Nine studies reported the stricture rate after treatment.15–20,22–24 The average rate of stricture rate was 64% in the control group, and 29% in the steroid group. The pooled estimate showed a significantly lower stricture rate in the steroid group than that in the control group (RR, 0.40; 95% CI, 0.20–0.81). Subgroup analysis was done after identifying the steroid administration method. The result revealed that the reduced stricture rate was mostly contributed by local injected steroid (RR, 0.42; 95% CI, 0.24–0.73) other than oral steroid (RR, 0.36; 95% CI, 0.02–7.78) (Fig. 2).
FIGURE 2.
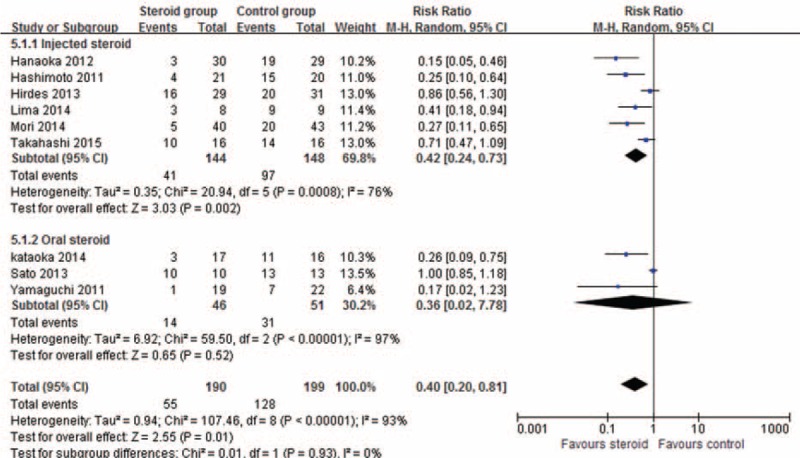
Forest plot showed that steroid administration led to a significantly lower stricture rate than control (RR, 0.40; 95% CI, 0.20–0.81), and the lower stricture rate was mostly contributed by local steroid injection (RR, 0.42; 95% CI, 0.24–0.73) other than oral steroid (RR 0.36, 95% CI, 0.02–7.78). CI = confidence interval; M-H = Mantel Haenszel, RR = risk ratio.
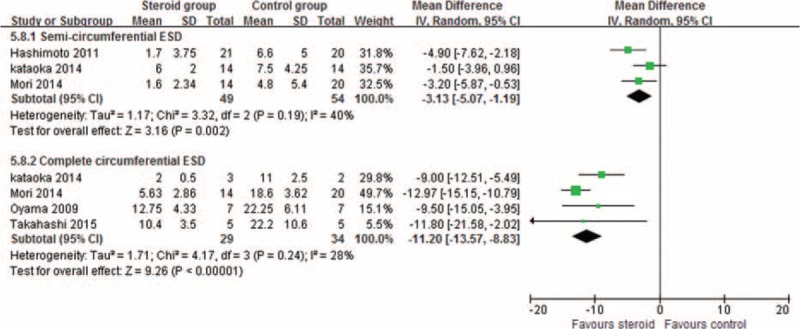
Required EBD Sessions
The required EBD sessions were reported in 11 studies during follow-up.13,15–24 Meta-analysis showed a significantly reduced EBD sessions in the steroid group than that in the control group (MD, −4.33; 95% CI, −6.10 to −2.57). Subgroup analysis was done after identifying the steroid administration method. The result revealed that both local injected steroid (MD, −2.69; 95% CI, −4.12 to −1.26) and oral steroid (MD, −10.46; 95% CI, −17.83 to −3.08) were effective to reduce EBD sessions (Fig. 3).
FIGURE 3.
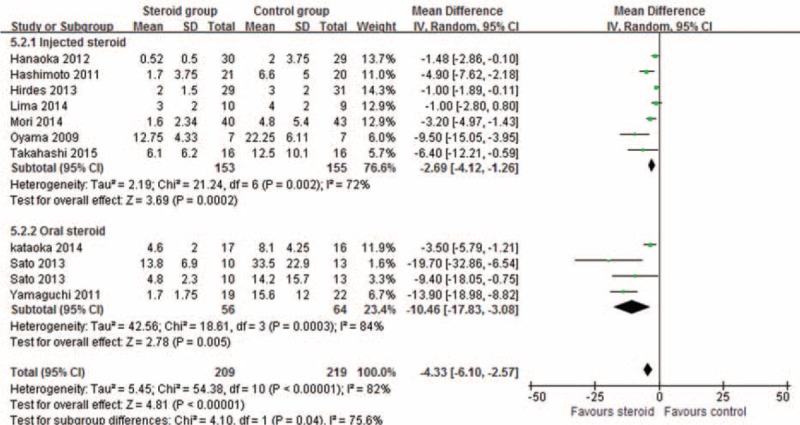
Forest plot showed that steroid significantly reduced EBD sessions than control (MD, −4.33; 95% CI, −6.10 to −2.57), and both local injected (MD, −2.69; 95% CI, −4.12 to −1.26) and oral steroid (MD, −10.46; 95% CI, −17.83 to −3.08) were effective to reduce EBD sessions. CI = confidence interval, EBD = endoscopic balloon dilation, MD = mean difference, M–H = Mantel Haenszel.
Subgroup Analysis According to ESD Type
Specific data on the stricture rate and EBD sessions according to semicircumferential ESD and complete ESD were reported by 6 studies.13,15,16,19,20,22 Subgroup analysis of 3 studies showed that steroid administration achieved a lower stricture rate after both semi-ESD (RR, 0.25; 95% CI, 0.12–0.51) and complete ESD (RR, 0.37; 95% CI, 0.21–0.66)(Fig. 4). Subgroup analysis demonstrated that steroid administration reduced the EBD sessions after both semicircumferential ESD (MD, −3.13; 95% CI, −5.07 to −1.19) and complete ESD (MD, −11.20; 95% CI, −13.57–8.83) during follow-up (Fig. 5).
FIGURE 4.
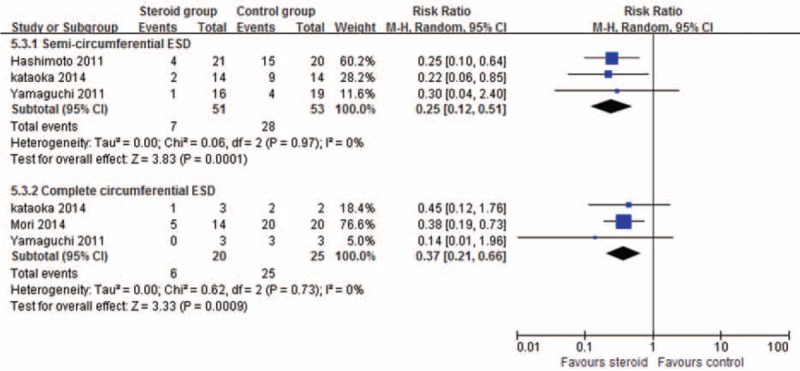
Forest plot showed that steroid achieved a lower stricture rate after both semicircumferential ESD (RR, 0.25; 95% CI, 0.12–0.51) and complete ESD (RR, 0.37; 95% CI, 0.21–0.66). CI = confidence interval, ESD = endoscopic submucosal dissection, M–H = Mantel Haenszel, RR = risk ratio.
FIGURE 5.
Forest plot showed that steroid reduced the EBD sessions after both semicircumferential ESD (MD, −3.13; 95% CI, −5.07 to −1.19) and complete ESD (MD, −11.20; 95% CI, −13.57–8.83). CI = confidence interval, EBD = endoscopic balloon dilation, ESD = endoscopic submucosal dissection, M–H = Mantel Haenszel.
Sensitivity Analysis
The sensitivity analysis results were listed in Table 5. After omitting 3 relatively poor-quality studies (stars < 8),13,16,17 meta-analysis result showed a similar trend in aspects of stricture rate (RR, 0.51; 95%CI, 0.27–0.96) and required EBD sessions (MD, −4.59, 95%CI, −6.92 to −2.26). Data were analyzed in random-effects models, and restricted studies did not alter the results compared with those mentioned above.
TABLE 5.
Sensitivity Analysis Result After Omitting 3 Relatively Poor-Quality Studies
Trial Sequence Analysis Avoiding False Positive
We performed TSA on the data of pooled estimate. After adjusting the heterogeneity across the included studies, all information sizes were derived to ensure a maximum type I error of 1% and a maximum type II error of 10%. The result showed that the Z-curve crossed the 2 monitoring boundaries constructed from the information size calculations, thereby confirming that steroid administration could reduce the stricture rate and required EBD sessions although the meta-analysis also did not reach required information size for required EBD sessions analysis (Figs. 6 and 7).
FIGURE 6.
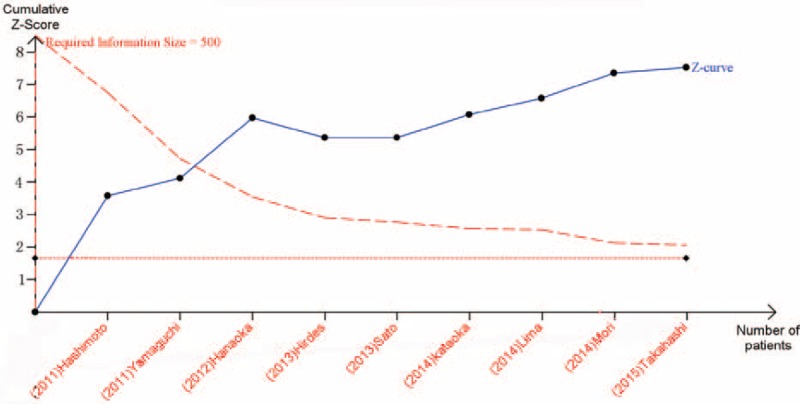
TSA result showed that the Z-curve crossed the monitoring boundaries constructed from the information size calculation to ensure a maximum type I error of 1% and a maximum type II error of 10% for the stricture rate. TSA = trial sequence analysis.
FIGURE 7.
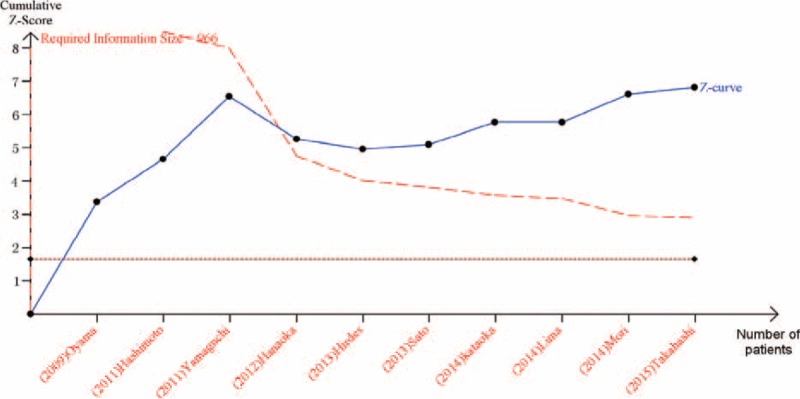
TSA result showed that the Z-curve crossed the monitoring boundaries constructed from the information size calculation to ensure a maximum type I error of 1% and a maximum type II error of 10% for required EBD sessions. EBD = endoscopic balloon dilation, TSA = trial sequence analysis.
Network Meta-Analysis According to the Steroid Administration Method
We conducted a network meta-analysis because of lacking direct comparison of local injected and oral steroid currently. Through comparing the estimates, network meta-analysis showed that local injected steroid had a similar effect to prevent stricture formation (RR, 1.16; 95% CI, 0.48–2.85), whereas a better effect to reduce required EBD sessions than oral steroid (MD, 7.77; 95%CI, 0.26–15.3).
Steroid-Related Complications
Five studies reported steroid-related complications, which included pneumomediastinum (0/1), deep submucosal tear (1/0), tarry stool (1/0), perforation (2/0), and bleeding (2/0). Meta-analysis showed that steroid administration did not raise more concerns than control (RR, 2.01; 95% CI, 0.49–8.25) (Figs. 4–7).
DISCUSSION
Esophageal ESD is established as a useful treatment for early stage esophageal cancer with a low risk of lymph node metastases, and now there is a widespread application of ESD also for superficial squamous cell neoplasms.21 However, this procedure has kinds of complications, especially post-ESD stricture occurred in average 16.7% of total patients.31 For patients with high-risk factors including: (1) dissected margins extending more than three-fourths of the esophageal circumference, (2) a long axis of dissected size >30 mm, (3) dissected site located in upper esophageal; the stricture rate after preventive EBD was still having a high rate of 59%.32
Lacking of clear underlying mechanism of stricture formation, excessive collagen in scars during the wound-healing process of esophageal mucosal and muscle is a major cause of concerns currently.33 Because the scar healing is a physiological process starting on granulation tissue formation, an early and immediate steroid administration after ESD would suppress the level of injury-induced inflammation, and slow-down the process of granulation tissue formation.34 Then a persistence of steroid may further inhibit collagen synthesis and cross-linking, meanwhile enhance collagen breakdown in granulation tissue.35,36 However, whether evidences from clinic were in accordance with these? We reviewed the literature to determine the efficacy of additional steroid administration and compare the difference between kinds of administration methods.
Meta-analysis of RCTs is mostly preferred to meta-analysis of RCTs and non-RCTs, but to date there are only 5 RCTs containing <100 cases in each group. Hirdes et al stated that at least 200 to 750 patients had to be included and analyzed to detect a significant reduction of stricture rate of 10 to 20% by using a 2-side α of 0.05 and a power of 80%.23 And we calculated that sample size may be at least to 400 patients to detect a significant reduction of EBD sessions in this case. So, a meta-analysis including limited studies and patients would be seriously influenced by a type I error or a type II error.37 For the surgical procedure and objective measurement, a well-conducted meta-analysis of RCTs and high-quality non-RCTs can be a good alternative.38
In our meta-analysis, the stricture rate and required EBD sessions are key indicators to assess the efficacy of steroid administration. The estimates of pooled stricture rate and required EBD sessions both were significantly reduced in patients with high risk of post-ESD stricture formation. Further subgroup analysis revealed that the efficacy of steroid is similar after semi-ESD and complete ESD, whereas the efficacy of injected and oral steroid seemed to be a little different. The results were strengthened by TSA and sensitivity analysis, whereas pooled estimates of oral steroid only included 3 studies and had a relative wide 95% CI.
After efficacy confirmed, the choice of administration method of steroid including local injected, oral, and superficially applied should be made. In the absence of quantitative and direct-comparison studies, our network meta-analysis was the first indicating a superiority of local injected to oral steroid in required EBD sessions reduction, and a similarity between them in stricture rate reduction. Meanwhile, local injected steroid was intended for really more patients than oral steroid: (1) diabetes mellitus patients; (2) patients suffered cardiovascular/cerebrovascular disease and taking anticoagulants at higher risk of uncontrollable bleeding, although the prothrombin time-internationalized ratio (PT-INR) levels were <3.0;8,39 (3) patients tired of long-term steroid taking; (4) aged patients concerned about systematic steroid adverse events. Some studies mentioned that local injected steroid might potentially increase risks of perforation, bleeding, and back-pack pain associated with EBD, whereas currently it lacked data supporting. And all these concerns would be eliminated though a superficially applied steroid gel, which might also have similar efficacy to prevent strictures.8
Implications of the study results for the clinical practice for esophageal stricture after semi- and complete ESD and surgery should be mentioned. Standard EBD remains the first choice for stricture treatment, as it could be applied to most of patients with satisfied efficacy and safety. Other newly developed treatment of radial incision and cutting is performing the clinical phase II/III study,40 and autologous oral mucosal sheets or an extracellular matrix scaffold material only achieved promising experimentally primarily results.41 Self-expandable metal stents or biodegradable stents seemed to be more suitable for anastomotic stricture and cicatricial stricture by esophagitis because of its invasive and high cost.42 Our meta-analysis demonstrated the efficacy of steroid administration to prevent stricture, especially for local injected steroid for patients with high risks after ESD. Thus, for the selected patients, steroid was a prevention with promising efficacy and full feasibility. And as EBD was performed according to the diagnosis and patient's demands, the complicated effect of mechanical dilation by endoscopic balloon as well as medical effects of steroid should also be noticed. Besides, for some complex stricture, the newly developed treatments may be an alternative. As local injected steroid needed additional injection, we currently evaluated and investigated a possibility of using a submucosal injection solution containing steroid to prevent stricture formation at not early stage but ahead of stage for patients with high risk.
Several limitations of the study need to be considered: (1) the meta-analysis included non-RCTs, although comparable baseline reported, potential bias might be concerned in patients grouping. (2) ESD was performed in difference centers, surgeon's experience and operation technique could to some extent influence the complication rate as well as the stricture rate, and these were inevitable in surgical studies with a long interval. (3) The kind, method, and dose of administrated steroid varied in studies; although subgroup analysis was performed, this might be still the major source of heterogeneity. A recommended administration protocol in the future may be useful to surgeons who were not familiar and expert with this. (4) Resected site of the esophagus was also an important factor of stricture formation, whereas the mostly included was ESD performed in the middle or lower part of the esophagus. And without detailed description, this might induce a lower stricture rate in the meta-analysis. (5) Most studies were conducted in Japan. We failed to include Japanese publications, so selection bias of articles might exist. (5) Publication bias might exist although comprehensive literature search was conducted, as some negative results may not be published.
In conclusion, there are a little number of RCTs to evaluate the efficacy of steroid to prevent stricture after ESD, and the meta-analysis is partly influenced by non-RCTs. Steroid administration, especially local injected steroid, shows promising efficacy for stricture prevention, with a significantly reduced stricture rate and required EBD sessions during follow-up.
Footnotes
Abbreviations: EBD = endoscopic Balloon dilation, ESD = endoscopic submucosal dissection, MD = mean difference, RCT = randomized controlled trials, RR = risk ratio, TSA = trial sequence analysis.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA 2015; 65:87–108. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA 2011; 61:69–90. [DOI] [PubMed] [Google Scholar]
- 3.Cao Y, Liao C, Tan A, et al. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 2009; 41:751–757. [DOI] [PubMed] [Google Scholar]
- 4.Huai ZY, Feng Xian W, Chang Jiang L, et al. Submucosal injection solution for endoscopic resection in gastrointestinal tract: a traditional and network meta-analysis. Gastroenterol Res Practice 2015; ID 702768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ono S, Fujishiro M, Niimi K, et al. Predictors of postoperative stricture after esophageal endoscopic submucosal dissection for superficial squamous cell neoplasms. Endoscopy 2009; 41:661–665. [DOI] [PubMed] [Google Scholar]
- 6.Katada C, Muto M, Manabe T, et al. Esophageal stenosis after endoscopic mucosal resection of superficial esophageal lesions. Gastrointest Endosc 2003; 57:165–169. [DOI] [PubMed] [Google Scholar]
- 7.Ezoe Y, Muto M, Horimatsu T, et al. Efficacy of preventive endoscopic balloon dilation for esophageal stricture after endoscopic resection. J Clin Gastroenterol 2011; 45:222–227. [DOI] [PubMed] [Google Scholar]
- 8.Yoda Y, Yano T, Kaneda K, et al. Endoscopic balloon dilatation for benign fibrotic strictures after curative nonsurgical treatment for esophageal cancer. Surg Endosc 2012; 26:2877–2883. [DOI] [PubMed] [Google Scholar]
- 9.Pelclová D, Navrátil T. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev 2005; 24:125–129. [DOI] [PubMed] [Google Scholar]
- 10.Liu K, Liu P, Liu R, et al. Steroid for epidural injection in spinal stenosis: a systematic review and meta-analysis. Drug Des Devel Ther 2015; 9:707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang K, Qi E, Zhang Y, et al. Efficacy and safety of local steroids for urethra strictures: a systematic review and meta-analysis. J Endourol 2014; 28:962–968. [DOI] [PubMed] [Google Scholar]
- 12.Versaci F, Gaspardone A, Tomai F, et al. Immunosuppressive therapy for the prevention of restenosis after coronary artery stent implantation (IMPRESS study). J Am College Cardiol 2002; 40:1935–1942. [DOI] [PubMed] [Google Scholar]
- 13.Oyama T, Kitamura Y. The prevention of stricture after circumferential esophageal endoscopic submucosal dissection—can steroid injection reduce the number of balloon dilatation? Gastrointest Endosc 2009; 69:AB359. [Google Scholar]
- 14.Mori H, Rafiq K, Kobara H, et al. Steroid permeation into the artificial ulcer by combined steroid gel application and balloon dilatation: prevention of esophageal stricture. J Gastroenterol Hepatol 2013; 28:999–1003. [DOI] [PubMed] [Google Scholar]
- 15.Yamaguchi N, Isomoto H, Nakayama T, et al. Usefulness of oral prednisolone in the treatment of esophageal stricture after endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma. Gastrointest Endosc 2011; 73:1115–1121. [DOI] [PubMed] [Google Scholar]
- 16.Hashimoto S, Kobayashi M, Takeuchi M, et al. The efficacy of endoscopic triamcinolone injection for the prevention of esophageal stricture after endoscopic submucosal dissection. Gastrointest Endosc 2011; 74:1389–1393. [DOI] [PubMed] [Google Scholar]
- 17.Hanaoka N, Ishihara R, Takeuchi Y, et al. Intralesional steroid injection to prevent stricture after endoscopic submucosal dissection for esophageal cancer: a controlled prospective study. Endoscopy 2012; 44:1007. [DOI] [PubMed] [Google Scholar]
- 18.Sato H, Inoue H, Kobayashi Y, et al. Control of severe strictures after circumferential endoscopic submucosal dissection for esophageal carcinoma: oral steroid therapy with balloon dilation or balloon dilation alone. Gastrointest Endosc 2013; 78:250–257. [DOI] [PubMed] [Google Scholar]
- 19.Mori H, Kobara H, Rafiq K, et al. Local steroid injection prevent deformity and stenosis of stomach after large endoscopic submucosal dissection. Am J Digest Dis 2014; 1:136–142. [Google Scholar]
- 20.Kataoka M, Anzai S, Shirasaki T, et al. Efficacy of short period, low dose oral prednisolone for the prevention of stricture after circumferential endoscopic submucosal dissection (ESD) for esophageal cancer. Endosc Int Open 2014; (EFirst). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim B, Lee H, Chung H, et al. The efficacy of topical bupivacaine and triamcinolone acetonide injection in the relief of pain after endoscopic submucosal dissection for gastric neoplasia: a randomized double-blind, placebo-controlled trial. Surg Endosc 2014; 1–9. [DOI] [PubMed] [Google Scholar]
- 22.Takahashi H, Arimura Y, Okahara S, et al. A randomized controlled trial of endoscopic steroid injection for prophylaxis of esophageal stenoses after extensive endoscopic submucosal dissection. BMC Gastroenterol 2015; 15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirdes MMC, van Hooft JE, Koornstra JJ, et al. Endoscopic corticosteroid injections do not reduce dysphagia after endoscopic dilation therapy in patients with benign esophagogastric anastomotic strictures. Clin Gastroenterol Hepatol 2013; 11:795-801. e1. [DOI] [PubMed] [Google Scholar]
- 24.Lima PJ, Bonotto ML, Hahn GD, et al. A prospective randomized trial of intralesional triamcinolone injections after endoscopic dilation for complex esophagogastric anastomotic strictures. Surg Endosc 2014; 1–5. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8:336–341. [DOI] [PubMed] [Google Scholar]
- 26.The Cochrane Collaboration, 2011, Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1. 0 [updated March 2011]. 2014; www.cochrane-handbook.org. [Google Scholar]
- 27.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25:603–605. [DOI] [PubMed] [Google Scholar]
- 28.Berlin JA, Laird NM, Sacks HS. A comparison of statistical methods for combining event rates from clinical trials. Stat Med 1989; 8:141–151. [DOI] [PubMed] [Google Scholar]
- 29.Wetterslev J, Thorlund K, Brok J, et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 2008; 61:64–75. [DOI] [PubMed] [Google Scholar]
- 30.Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med 2002; 21:2313–2324. [DOI] [PubMed] [Google Scholar]
- 31.Kishida Y, Kakushima N, Kawata N, et al. Complications of endoscopic dilation for esophageal stenosis after endoscopic submucosal dissection of superficial esophageal cancer. Surg Endosc 2014; 1–7. [DOI] [PubMed] [Google Scholar]
- 32.Ezoe Y, Muto M, Horimatsu T, et al. Efficacy of preventive endoscopic balloon dilation for esophageal stricture after endoscopic resection. J Clin Gastroenterol 2011; 45:222–227. [DOI] [PubMed] [Google Scholar]
- 33.Ramage JI, Jr, Rumalla A, Baron TH, et al. A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection therapy for recalcitrant esophageal peptic strictures. Am J Gastroenterol 2005; 100:2419–2425. [DOI] [PubMed] [Google Scholar]
- 34.Carrico TJ, Mehrhof AI, Jr, Cohen IK. Biology of wound healing. Surg Clin North Am 1984; 64:721–733. [DOI] [PubMed] [Google Scholar]
- 35.Kochhar R, Makharia GK. Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc 2002; 56:829–834. [DOI] [PubMed] [Google Scholar]
- 36.Russell SB, Trupin JS, Myers JC, et al. Differential glucocorticoid regulation of collagen mRNAs in human dermal fibroblasts. Keloid-derived and fetal fibroblasts are refractory to down-regulation. J Biol Chem 1989; 264:13730–13735. [PubMed] [Google Scholar]
- 37.Siddique S, Kottewar S, Theivanayagam S, et al. Tu1372 Steroid Use for prevention of strictures post endoscopic submucosal dissection: a meta analysis. Gastrointest Endosc 2014; 79:AB516. [Google Scholar]
- 38.Abraham NS, Byrne CM, Young JM, et al. Meta-analysis of non-randomized comparative studies of the short-term outcomes of laparoscopic resection for colorectal cancer. ANZ J Surg 2007; 77:508. [DOI] [PubMed] [Google Scholar]
- 39.Choudari CP, Rajgopal C, Palmer KR. Acute gastrointestinal haemorrhage in anticoagulated patients: diagnoses and response to endoscopic treatment. Gut 1994; 35:464–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kataoka K, Aoyama I, Mizusawa J, et al. A randomized controlled Phase II/III study comparing endoscopic balloon dilation combined with steroid injection versus radial incision and cutting combined with steroid injection for refractory anastomotic stricture after esophagectomy: Japan Clinical Oncology Group Study JCOG1207. Jpn J Clin Oncol 2015; 45:385–389. [DOI] [PubMed] [Google Scholar]
- 41.Ohki T, Yamato M, Ota M, et al. Prevention of esophageal stricture after endoscopic submucosal dissection using tissue-engineered cell sheets. Gastroenterology 2012; 143:582-588. e2. [DOI] [PubMed] [Google Scholar]
- 42.Karbowski M, Schembre D, Kozarek R, et al. Polyflex self-expanding, removable plastic stents: assessment of treatment efficacy and safety in a variety of benign and malignant conditions of the esophagus. Surg Endosc 2008; 22:1326–1333. [DOI] [PubMed] [Google Scholar]


