Abstract
In patients with primary canaliculitis, conservative medical therapy is associated with a high recurrence rate. Surgical treatments carry a great resolution rate but sometimes can result in the lacrimal pump dysfunction and canalicular scarring. The aim of this study is to introduce a minimally invasive approach, intracanalicular ophthalmic corticosteroid/antibiotic combination ointment infiltration (IOI, intracanalicular ointment infiltration), and to report our preliminary results for treating primary canaliculitis.
In this retrospective, interventional case series, 68 consecutive patients with newly developed primary canaliculitis at a major tertiary eye center between January 2012 and January 2015. Thirty-six patients received conservative medical treatment alone (group 1; 36 eyes). Twenty-two patients and 10 medically uncontrolled patients from group 1 underwent IOI therapy (group 2; 32 eyes). Ten patients and 26 recurrent patients from group 1 and group 2 underwent surgery (group 3; 36 eyes). Patients were followed-up for at least 8 weeks. Clinical characteristics and outcomes were analyzed and compared.
In this study, patients’ age, sex, onset location, and durations of disease among 3 groups showed no significant difference. The resolution rate in group 2 was 72.7% (16/22) for new patients and 68.8% (22/32) for gross patients, respectively, both of which are higher than that of group 1 (22.2%, 10/36) but lower than that of group 3 (100%, 36/36). Of group 3, 2 patients received 2 surgical interventions and resolved finally. Microbiological workup was available in 51 patients. The most common isolates were staphylococcus species (27.9%) and streptococcus species (20%). Canalicular laceration developed in 1 patient during the IOI procedure and 1 patient undergoing surgery. Only 2 had postoperative lacrimal pump dysfunction and 1 had canalicular scarring in group 3.
The IOI may be an effective and minimally invasive technique for treating primary canaliculitis and obviate the need for further intensive surgery.
INTRODUCTION
Primary canaliculitis is an uncommon infectious disease of lacrimal system.1 Although it accounts for <5% of patients with lacrimal disease,2,3 it can be easily misdiagnosed and insufficiently treated in clinic.4 Conservative medical therapy for new onset primary canaliculitis has an acceptable rate of success and was considered as a first-line treatment,4 yet it is often associated with a high recurrence rate.5,6 One major drawback of the medical therapy is that the unique anatomy of lacrimal canaliculi, which is narrow and tortuous compared to the nasalacrimal duct, is a natural barrier to drug administration. In addition, the inflammation associated with primary canaliculitis could induce the mucosal selling, leading to the canalicular obstructions. The concretions, discharge, and infected debris accompanied with the disease may also prevent drugs from eradicating the infection and protect the bacteria within the materials,5 finally resulting in the resistance of the penetration of topical and systemic antibiotics.7 Intracanalicular antibiotic irrigation has been suggested as an alternative to surgery and demonstrates promising initial results; however, this treatment requires multiple irrigations, which may decrease the patients’ compliance.8 Surgical treatments, such as canaliculotomy, punctoplasty, and canalicular curettage, are reported to have a high resolution rate within a short follow-up but possibly result in the lacrimal pump dysfunction and canalicular scarring, which aggravate rather than ameliorate the severity of primary canaliculitis.4,9–11
In this study, the authors developed a new minimally invasive approach, termed intracanalicular ophthalmic corticosteroid/antibiotic combination ointment infiltration (IOI, intracanalicular ointment infiltration), for the treatment of primary canaliculitis. Our purpose was to introduce this approach and to present its preliminary results compared to conservative medical treatment and conventional surgical treatment.
METHODS
This was a retrospective medical record review of consecutive patients undergoing IOI between January 2012 and January 2015. All IOI treatments were performed by the same surgeons (JH and JX) at the Shanghai Eye, Ear, Nose, and Throat Hospital, Fudan University, China. All patients were fully informed of the details and possible complications of the procedure. Patient demographics, clinical presentation, intraoperative findings, microbiological profile based on culture results and clinical outcomes were collected. Written informed consent and Institutional Review Board approval were obtained for this study. The study was conducted in accordance with the Declaration of Helsinki.
Inclusion criteria of canaliculitis were: (1) punctum swelling associated with eyelid thickening and (2) mucopurulent punctal regurgitation or concretions extruding from the punctum.5,6,9,10 Exclusion criteria were: (1) patients with secondary canaliculitis, such as those with punctal plug-induced canaliculitis and (2) patients with dacryocystitis or nasolacrimal obstruction.
The treatment plans included conservative medical therapy (topical antibiotics6 and intracanalicular antibiotic irrigation8) IOI treatment, and surgery (single- or 2-snip punctoplasty and curettage6,10), as shown in Figure 1. Furthermore, complications of the procedures were investigated.
FIGURE 1.
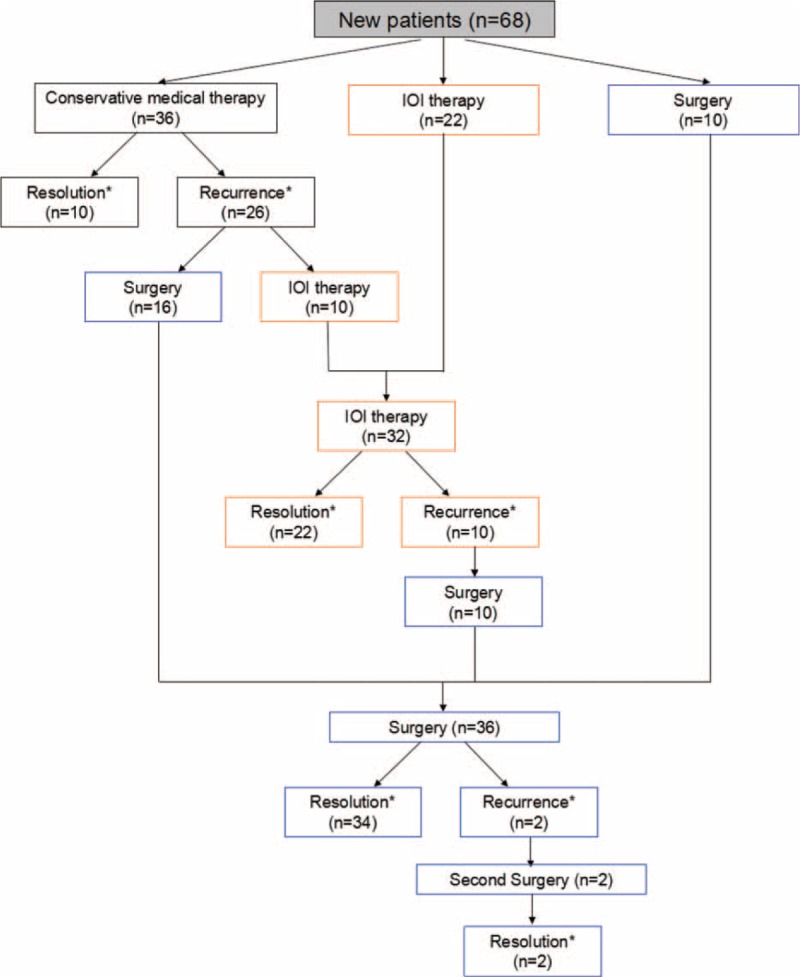
Diagram showing the participation of each group. ∗ For the evaluation of patients’ outcomes, follow-up appointments for at least 8 weeks were required. IOI = intracanalicular ointment infiltration.
The IOI procedure involved the following steps (see Figure 2). At the beginning, 0.5 mL of 2% lidocaine was injected into the lacrimal duct for the infiltration anesthesia. Then, both the upper and lower punctum were dilated. A 23-gauge lacrimal cannula set was used in this procedure. The stainless steel lacrimal cannula is 70.5 mm long with a blunt, conical tip, and an injection orifice on the front side; the cannula is well polished (Figure 2B). The upper and lower canaliculi were probed with this cannula via the punctum. The tip of the cannula passed through canaliculi and entered into dacryocyst and had a hard stop. The ophthalmic tobramycin 0.3%/dexamethasone 0.1% combination ointment (1–1.5 mL, Tobradex®, Alcon) was injected, whereas the tips stay in the dacryocyst. After the ointment flowed out of the upper or lower punctum, the approach was complete. Postoperatively, the patients were prescribed with topical 0.3% tobramycin/0.1% dexamethasone eye drops 4 times per day for 2 weeks, and topical 0.3% tobramycin eye drops 3 times per day for another 2 weeks.
FIGURE 2.
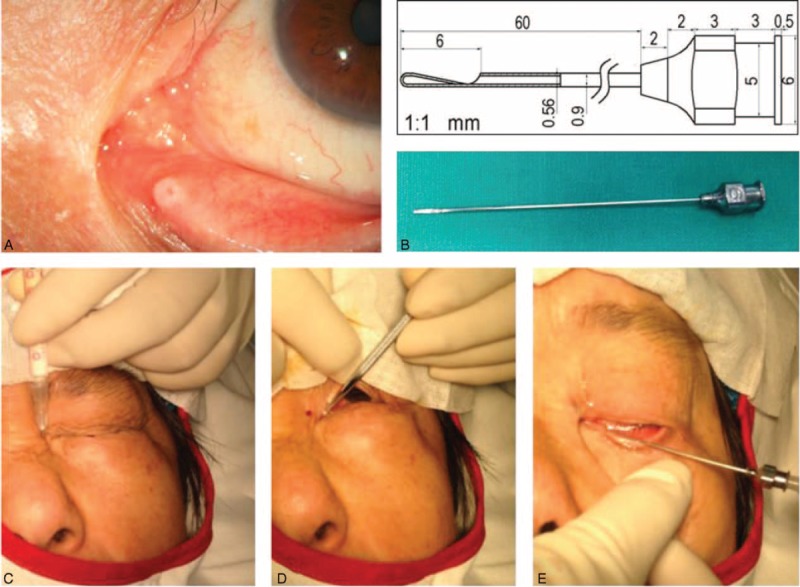
Photographs showing a procedure of IOI therapy. (A) Punctum before the procedure. (B) A modified 23-gauge stainless steel lacrimal cannula, 70.5 mm in length, with a blunt conical tip and an injection orifice on the front side; the cannula was well polished. (C) 0.5 mL of 2% lidocaine was injected into the lacrimal duct for the infiltration anesthesia. (D) Both the upper and lower punctum were dilated. (E) The canaliculi and nasolacrimal duct were probed, and then the tip of the cannula passed through canaliculi and entered into dacryocyst and had a hard stop. The ointment was injected whereas the tips stay in the dacryocyst. IOI = intracanalicular ointment infiltration.
For all groups, patients required follow-up appointments for at least 8 weeks. Postoperative examinations included ocular surface symptoms, signs of canaliculitis, and the treatment response. Resolution was defined as complete relief of inflammatory signs and symptoms following treatment. Complications of these procedures were also investigated. Microbiological culture was performed in the samples from purulent discharge and/or concretions.
An analysis was performed using the statistical software package SPSS for Windows (version 19.0; SPSS, Inc., Chicago, IL). In cases with bilateral onset, only the first eye was enrolled for analysis. The normal distribution data is shown as mean ± standard deviation. The mean values differences among different groups’ parametric data were analyzed using the Mann–Whitney U test. The percentage of parameters between different groups was analyzed with a chi-square test. All of the P values were 2-sided and considered statistically significant when the values were <0.05.
RESULTS
During the study, 68 patient medical records reported a primary canaliculitis (Figure 1). Of these, 36 chose conservative medical therapy (group 1), 22 received IOI (group 2), and 10 underwent surgery (group 3) at baseline. At follow-up, 10 from group 1 converted to group 2 due to the uncontrolled conditions. In addition, 16 from group 1 and 10 from group 2 underwent surgery finally because the recurrence of primary canaliculitis.
Descriptive characteristics of the patients were presented in Table 1. There were 17 (25%) male and 51(75%) female patients. Their mean age was 59.0 ± 12.8 years (range, 33–84 years). The right eye was affected in 36 (52.8%) patients and the left eye in 32 (47.2%). The upper canaliculus was involved in 25 (36.8%) patients, the lower canaliculus in 40 (58.8%) patients, and both canaliculus in 3 (4.4%) patients. The mean time from the onset of symptoms to diagnosis was 5.6 ± 2.3 months (range, 1–9 months). As shown in Table 1, no significant differences in age (P = 0.391), sex (P = 0.843), eyes affected (P = 0.672), canaliculus involved (P = 0.104), or duration of diseases (P = 0.633) among 3 groups were identified.
TABLE 1.
Demographic Data of 68 Consecutive Patients With Primary Canaliculitis
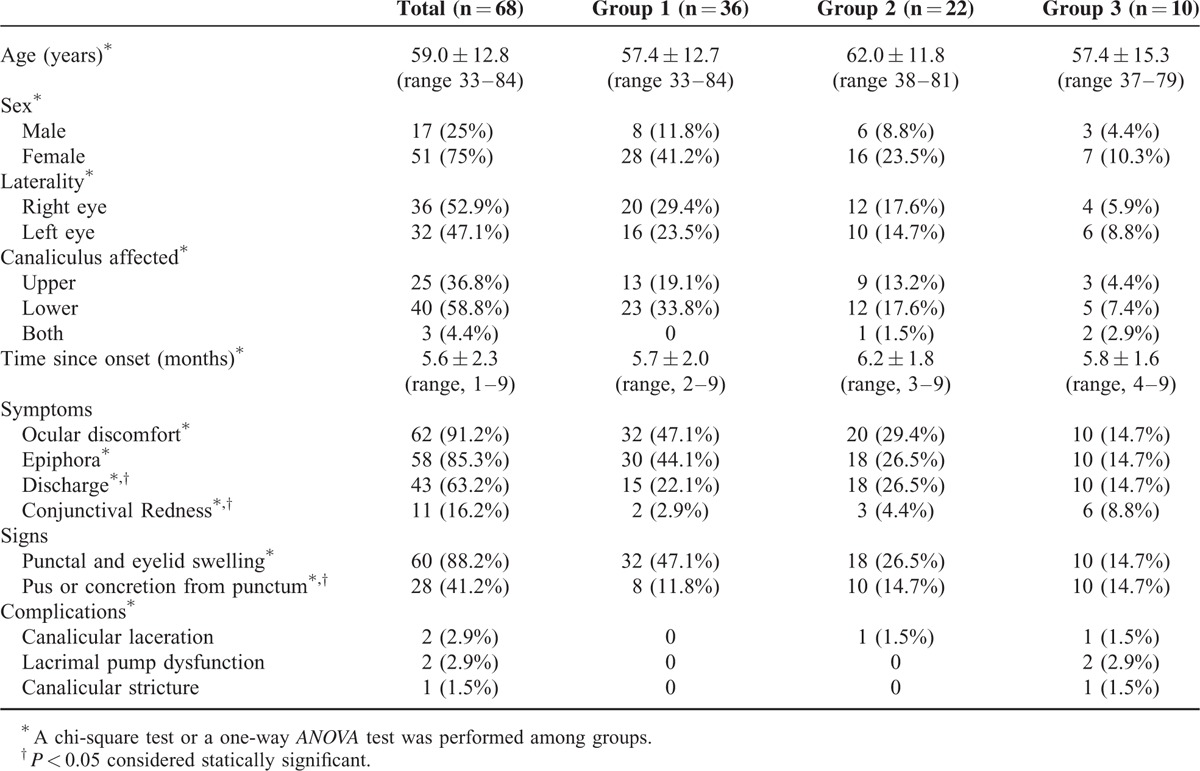
The clinical presentations in these 68 patients are also summarized in Table 1. Ocular discomfort was the most common presenting symptom noted in 62 (91.2%) patients, followed by epiphora (58, 85.3%), discharge (43, 63.2%), and conjunctival redness (11, 16.2%). The primary sign was punctal and eyelid swelling in 60 (88.2%) patients; the other sign was pus or concretion from punctum (28, 41.2%). In our case series, patients with discharge (P < 0.001), conjunctival redness (P < 0.01), or pus or concretion from punctum (P < 0.001) are more likely to receive IOI therapy or to undergo surgery.
Eight weeks after the initial procedure, resolution of newly developed patients was noted in 27.8% (10/36) of group 1, 72.7% (16/22) of group 2, and 100% (10/10) of group 3, respectively. Because some recurrent patients converted to group 2 or group 3, we also calculated gross resolution rates of these 2 groups, which changed to 68.8% (22/32) in group 2 but remained the same as 100% (36/36) in group 3. However, it should be noted that 5.6% (2/36) patients of group 3 received 2 surgical interventions, and both of them resolved finally. The response to treatments is summarized in Table 2. Our statistical analysis showed that the resolution rate in group 2 did not change significantly even after it enrolled medically uncontrolled patients from group 1 (P = 0.753).
TABLE 2.
Response to Treatments for Primary Canaliculitis
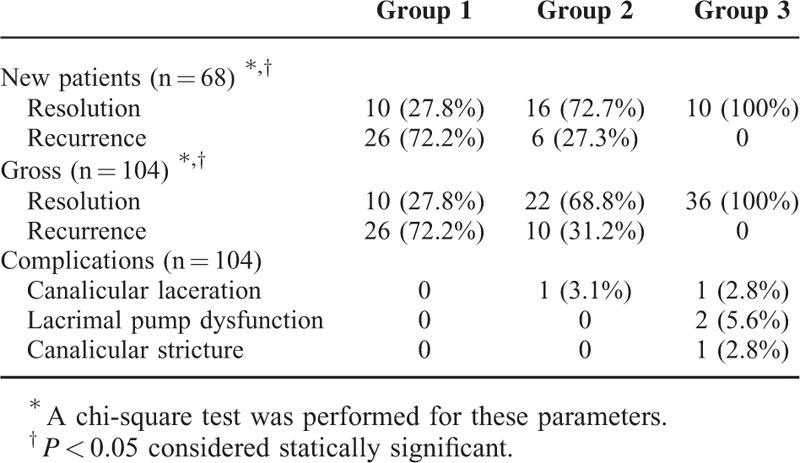
Two patients had intraoperative canalicular laceration, whereas 3 had postoperative epiphora. Two of these 3 patients with epiphora were considered as lacrimal pump dysfunction due to the snip of punctum in the surgery, whereas another one patient developed canalicular stricture at the final follow-up. This patient with canalicular stricture was noted to have both of canaliculus affected with mucopurulent discharge on preoperative examinations, and sulfur granules and concretions were found during the surgery. Although an additional lacrimal intubation surgery was recommended, this patient declined further therapy.
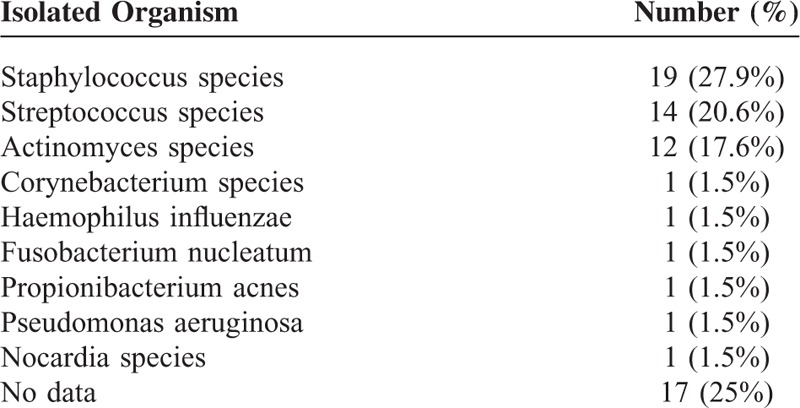
Microbiologic cultures were available in the medical records of 75% (51/68) of patients. The most common organisms grown in culture were staphylococcus species (27.9%), followed by streptococcus species (20.6%), and actinomyces species (17.6%). Details of the microbiological profile are summarized in Table 3.
TABLE 3.
Microbiological Profile of 68 Consecutive Patients With Primary Canaliculitis
DISCUSSION
In this study, 72.7% (16/22) of newly developed patients with primary canaliculitis were cured with IOI therapy. After we enrolled 10 additional recurrent patients from group 1, the resolution rate in this group was still 68.8% (22/32). The pilot treatment results of IOI therapy were better than those seen in patients with conservative medical therapy but worse than those seen in patients undergoing surgery. The exact mechanism why the resolution rate of IOI therapy was higher than conservative medical therapy remains unknown. Indeed, group 1 and group 2 mostly used the same antibiotics regimen (tobramycin). One possible reason is that IOI therapy dramatically increases the local drug concentration by infiltrating the ointment directly to the canaliculus and uses the tobramycin combined with corticosteroids. It has been reported that although topical corticosteroids alone was not successful for the treatment of canaliculitis,12 it was effective when combined with tobramycin.13 In addition, the microbiologic profile analysis showed that staphylococcus species, streptococcus species, and actinomyces species were 3 main organisms identified in our case series. Zhang et al14 and Sun et al15 found that ocular bacterial isolates susceptibility to tobramycin was mild or moderate sensitive in China. However, Gram-positive bacteria were more likely reported to be resistant to tobramycin.16–18 This may explain why the recurrence rate was still 31.2% (10/32) in group 2. One advantage of IOI therapy is that it preserves the structure and function of punctum and canaliculus; therefore, its complications were relatively few compared to the invasive surgery. The limitation of this approach needs to be noted. As a minimally invasive therapy, debris, concretions, or granules can be left in the canaliculus behind unintentionally. The complete removal of these materials often requires an intensive surgery.
Patients in the present study were mostly the middle-aged and elderly, which is consistent with previous reports.5,6,8–10,19 Similar to their findings, most of primary canaliculitis patients in the present study were women (75%).5,6,9–11 The mean time from onset to diagnosis of primary canaliculitis was 5.6 ± 2.3 months (range, 1–9 months) months, which was also comparable with their reports.5,6,8–11 Although ocular discomfort and epiphora were the most common symptoms in our study, different from studies which have identified discharge as the most common symptom,1,3,10,11 we found that punctal and eyelid swelling and pus or concretion from punctum were still the primary clinical signs, which were traditionally considered as hallmarks of canaliculitis. Lin et al identified the presence of concretions from canaliculus as a predictive risk factor for the recurrence in patients either receiving conservative medical therapy or surgical treatments.11 In regard to this finding, such patients with pus or concretion from punctum were not commonly treated with conservative medical therapy in our clinical practice. Our statistical analysis also demonstrated that patients with discharge, conjunctival redness, or pus or concretion from punctum are more likely to receive IOI therapy or undergo surgery in our case series.
Successful initial resolution with conservative medical therapy has been reported between 20% and 100%.1,5,9,11 In our study, conservative medical therapy resulted in as high as 62.2% of the recurrence in new primary canaliculitis patients. It should be noted that we did not apply the canalicular expression to patients in group 1, which could possibly increase the resolution rate further. However, because of the presence of concretions, this improvement may also be limited. Not surprisingly, single surgical intervention in group 3 had a high resolution rate (94.4%, 34/36) at the 8 weeks follow-up. Two cases of recurrence were noted. However, after the secondary surgical intervention, both of them resolved finally. The excellent clinical outcome of surgery is similar to previous reports.2,5,7,10,11,19 Complications of surgical intervention includes the injury to the canalicular mucus (canalicular stricture), the damage to the punctum (lacrimal pump dysfunction), and canalicular laceration. The complication rate of group 3 (4/36) was higher than that of group 2 (1/32), although no significant difference was found (P = 0.360).
There are several limitations in our study. As a retrospective study, it is not allowed us to collect data that was not mentioned in the medical records, which may result in a documentation bias. Because most of patients in group 2 and group 3 were treated in an outpatient department, their compliance was poor and became a significant issue for regular check-ups. We have to set the final follow-up time as 8 weeks because the lacrimal outflow system was syringed routinely at this time point. After that, patients who had no signs of canaliculitis were usually not asked for further follow-up. Finally, as our study is not a randomized study, there is a possibility of a selection bias. It seems that milder cases were more likely to undergo conservative medical therapy. This selection bias, however, does not change our conclusions. Indeed, random assignment of the patients would have even worsened the outcomes of group 1.
IOI therapy is an effective, minimally invasive, and easy-to-perform approach for patients with primary canaliculitis, which may obviate the need for surgical interventions. This is the first case series that demonstrates its preliminary clinical outcomes. The resolution rate of IOI therapy was higher than those seen that of conservative medical therapy but still remained lower than that of conventional surgery. However, because this procedure makes very limited damage to the canalicular structure and function, it could be the third way for primary canaliculitis beyond conservative medical therapy and surgical intervention. Prospective, randomized, controlled studies with long follow-ups are warranted to demonstrate the best indications for this approach.
Footnotes
Abbreviation: IOI = intracanalicular ointment infiltration.
Funding/support: the authors were supported by grants from the Key Clinic Medicine Research Program, the Ministry of Health, China (201302015); the National Science and Technology Research Program, the Ministry of Science and Technology, China (2012BAI08B01); the National Natural Science Foundation of China (81170817, 81200658, 81300735, 81270978, U1205025, and 81330022); the Scientific Research Program, Science and Technology Commission of Shanghai Municipality, Shanghai (13441900900, 13430720400); the Chinese Postdoctoral Fund (XMU135890); and the New Technology Joint Research Project in Shanghai Hospitals (SHDC12014114). The sponsor or funding organization had no role in the design or conduct of this research.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Anand S, Hollingworth K, Kumar V, et al. Canaliculitis: the incidence of long-term epiphora following canaliculotomy. Orbit 2004; 23:19–26. [DOI] [PubMed] [Google Scholar]
- 2.Demant E, Hurwitz JJ. Canaliculitis: review of 12 cases. Can J Ophthalmol 1980; 15:73–75. [PubMed] [Google Scholar]
- 3.Zaldivar RA, Bradley EA. Primary canaliculitis. Ophthal Plast Reconstr Surg 2009; 25:481–484. [DOI] [PubMed] [Google Scholar]
- 4.Freedman JR, Markert MS, Cohen AJ. Primary and secondary lacrimal canaliculitis: a review of literature. Surv Ophthalmol 2011; 56:336–347. [DOI] [PubMed] [Google Scholar]
- 5.Vécsei VP, Huber-Spitzy V, Arocker-Mettinger E, et al. Canaliculitis: difficulties in diagnosis, differential diagnosis and comparison between conservative and surgical treatment. Ophthalmologica 1994; 208:314–317. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Q, Xu B, Li XX, et al. Clinical characteristics, treatment patterns, and outcomes of primary canaliculitis among patients in Beijing, China. Biomed Res Int 2015; 2015:904756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pavilack MA, Frueh BR. Through curettage in the treatment of chronic canaliculitis. Arch Ophthalmol 1992; 110:200–202. [DOI] [PubMed] [Google Scholar]
- 8.Mohan ER, Kabra S, Udhay P, et al. Intracanalicular antibiotics may obviate the need for surgical management of chronic suppurative canaliculitis. Indian J Ophthalmol 2008; 56:338–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaliki S, Ali MJ, Honavar SG, et al. Primary canaliculitis: clinical features, microbiological profile, and management outcome. Ophthal Plast Reconstr Surg 2012; 28:355–360. [DOI] [PubMed] [Google Scholar]
- 10.Lee MJ, Choung HK, Kim NJ, et al. One-snip punctoplasty and canalicular curettage through the punctum: a minimally invasive surgical procedure for primary canaliculitis. Ophthalmology 2009; 116:2027–2030. [DOI] [PubMed] [Google Scholar]
- 11.Lin SC, Kao SC, Tsai CC, et al. Clinical characteristics and factors associated the outcome of lacrimal canaliculitis. Acta Ophthalmol 2011; 89:759–763. [DOI] [PubMed] [Google Scholar]
- 12.Briscoe D, Edelstein E, Zacharopoulos I, et al. Actinomyces canaliculitis: diagnosis of a masquerading disease. Graefes Arch Clin Exp Ophthalmol 2004; 242:682–686. [DOI] [PubMed] [Google Scholar]
- 13.Chen SX, Lee GA. SmartPlug in the management of severe dry eye syndrome. Cornea 2007; 26:534–538. [DOI] [PubMed] [Google Scholar]
- 14.Zhang C, Liang Y, Deng S, et al. Distribution of bacterial keratitis and emerging resistance to antibiotics in China from 2001 to 2004. Clin Ophthalmol 2008; 2:575–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun ST, Wang LY, Zhang YQ, et al. The changes of ocular bacterial isolates and in vitro antimicrobial susceptibility in the past six years. Zhonghua Yan Ke Za Zhi 2012; 48:542–547. [PubMed] [Google Scholar]
- 16.Blanco AR, Sudano Roccaro A, Spoto CG, et al. Susceptibility of methicillin-resistant Staphylococci clinical isolates to netilmicin and other antibiotics commonly used in ophthalmic therapy. Curr Eye Res 2013; 38:811–816. [DOI] [PubMed] [Google Scholar]
- 17.Galvis V, Tello A, Guerra A, et al. Antibiotic susceptibility patterns of bacteria isolated from keratitis and intraocular infections at Fundación Oftalmológica de Santander (FOSCAL), Floridablanca, Colombia. Biomedica 2014; 34 Suppl 1:23–33. [DOI] [PubMed] [Google Scholar]
- 18.Long C, Liu B, Xu C, et al. Causative organisms of post-traumatic endophthalmitis: a 20-year retrospective study. BMC Ophthalmol 2014; 14:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hussain I, Bonshek RE, Loudon K, et al. Canalicular infection caused by actinomyces. Eye (Lond) 1993; 7:542–544. [DOI] [PubMed] [Google Scholar]


