Abstract
Background:
While many pain patients rely on pain-relieving treatments to manage their pain, pain-related research commonly quantifies pain status using validated questionnaires without taking into account that information. This will lead to an underestimate of the burden of pain in the community. To ensure a more accurate assessment of the prevalence and severity of pain, this study aimed to develop a pain management questionnaire and to assess how much population-based pain estimates change when pain management is considered.
Methods:
This study was a cross-sectional population-based study in Grampian, north-east Scotland. A total of 4600 people, aged 25 years and over, were randomly selected from a population sample frame and sent a questionnaire on pain and pain management. Population estimates of pain were determined twice: with the use of standard pain status questionnaires (‘current pain’) and with the use of a newly developed enhanced pain status questionnaire to determine patients’ estimated pain without pain management (‘all pain’).
Results:
The prevalence of current pain was 50.5% (95% CI = 48.0, 52.9). Of those who reported no current pain, 11.6% (95% CI = 9.4, 13.8) reported that they would have had pain had they not managed their pain. Thus, the all pain prevalence was 56.2% (95% CI = 53.7, 58.7). This difference in prevalence rates was statistically significant (difference = 5.7%; 95% CI = 2.2, 9.2). Likewise, participants’ pain severity significantly increased when they estimated their pain without pain management (p < 0.001, Wilcoxon-signed rank test).
Conclusions:
Failure to assess pain management information results in an underestimation of pain prevalence and severity. This should be considered in future epidemiological studies.
Summary points
Pain management information is currently not considered for the assessment of pain in epidemiological population-based studies.
Since pain management can affect people’s pain status drastically, it is likely that we currently underestimate the true burden of pain in studies assessing pain.
Incorporating self-reported pain management information in an epidemiological study of pain led to significantly increased estimates of both pain prevalence and pain severity.
It is therefore crucial to collect and take into account people’s pain management information in future studies for a more accurate measurement of pain.
Keywords: Pain, pain prevalence, pain severity, pain measurement, pain treatment use, epidemiology
Introduction
Patients with pain are commonly reliant on treatments to relieve and manage their pain condition. In a study by Breivik et al.,1 the vast majority of pain patients reported the use of pain treatments (69%) with non-steroidal anti-inflammatory drugs (NSAIDs), paracetamol and weak opioids most commonly reported. The access to pain treatments has become easier for patients with pain. They are not restricted to prescribed treatments but can obtain non-prescribed drugs through multiple sources, like community pharmacies and other retail outlets.2 Moreover, non-pharmacological pain treatments, such as exercise and complementary treatments, have become popular for the management of pain.3
Current pain-related research assesses study participants’ self-reported pain status using validated pain scales without taking into account their pain management. Although pain management is occasionally captured in population studies, it is usually not considered when assessing pain status. Without information on participants’ pain management, a person with self-reported moderate pain and no recent pain treatment use may be considered to have the same pain status as a person with moderate pain, achieved through a complex pain management regime. Nevertheless, it seems evident that the severity of pain (without its management) in the latter is in fact more severe than in the former. In addition to that, participants who report no current pain due to their management are currently not classified as pain patients in these studies. Given that the majority of patients frequently take pain-relieving treatments,4,5 it can be assumed that current population estimates of pain regularly underestimate both the true prevalence and the severity of pain.
The aims of this study were therefore to (1) develop and validate an instrument to collect information on pain management suitable for use in self-complete questionnaires of the type used in population studies and to (2) assess how much population estimates of pain are changed when participants report the pain they believe they would experience in the absence of their pain management.
Methods
Questionnaire development
Two separate questionnaires were developed for this study: (1) a pain management questionnaire to collect information on participants’ recent pain treatment use and (2) an enhanced pain status questionnaire to determine the self-reported pain participants would have had, had they not used pain treatments for its management (‘hypothetical pain’).
All pain management approaches were included in the pain management questionnaire (e.g. pharmacological and non-pharmacological). A stem question was placed at the beginning of the pain management questionnaire to determine any recent pain treatment use (Figure 1). Three comprehensive treatment lists were developed to gather information on (1) prescribed, (2) non-prescribed and (3) other treatments (covering complementary treatments and exercise). The lists contained pain treatments commonly used by people experiencing pain in the United Kingdom. The individual questionnaire items were selected with the aid of a pharmacist (author C.M.B.). The final version of the questionnaire was also reviewed for completeness by a general practitioner. Below each treatment section, participants were provided with the option to add any other pain treatments that were not included in the lists.
Figure 1.
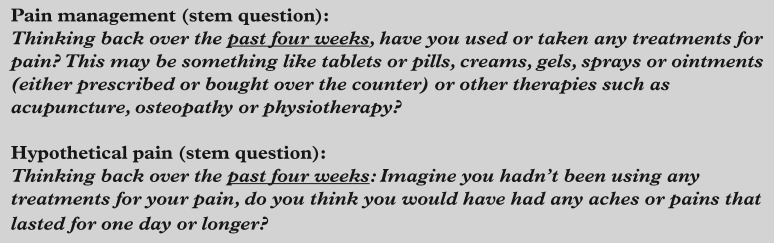
Questionnaire stem questions.
The pain management questionnaire was sent to a random sample of 150 research volunteers who had participated in a previous population study and reported pain at that time.6 A subsample of the questionnaire respondents (n = 25) participated in a subsequent face-to-face interview. They were asked to bring with them all the treatments that they had been using for their pain management within the past 4 weeks. The agreement between the list of treatments collected in the paper questionnaire and those identified at the interview was assessed using the Prevalence and Bias Adjusted Kappa (PABAK).7 Moreover, the questionnaire’s sensitivity and specificity were examined. Overall, the PABAK suggested ‘almost perfect’ agreement (k = 0.95) and the questionnaire’s sensitivity and specificity were high (88.0% and 98.3%, respectively).
Based on two widely used questionnaires for pain (including pain location (body manikins) and the Chronic Pain Grade (CPG)8), an enhanced pain status questionnaire was developed to estimate participants’ hypothetical pain in a state without pain management. This was piloted with the University of Aberdeen Service User Group (people with chronic pain) which led to further modifications to the instrument. This identified the complexity of the concept of imagining the presence and severity of hypothetical pain. Therefore, questions with a recall period of more than 1 month were removed and a small paragraph was included at the beginning of the questionnaire section in order to help participants to imagine their hypothetical pain:
In this section we ask you about any pain you think you would have if you weren’t managing your pain with the treatments reported above. You might find it easier to answer the following questions when thinking back to a situation when you had forgotten to use your pain treatments.
The final version of the instrument contained four questions to assess the prevalence, the location and the severity of participants’ hypothetical pain. The stem question to identify with hypothetical pain is displayed in Figure 1.
Population study
A random sample of 4600 National Health Service (NHS) residents in Grampian (north of Scotland, UK) aged 25 years and over was selected from Health Board records. Potential participants were sent a letter informing them that they had been selected for the study, followed by the survey pack 1 week later. Each survey pack consisted of an invitation letter, an information sheet, the questionnaire and a pre-paid reply envelope. A third mailing was undertaken to follow up non-respondents with a reminder mailing 3 weeks after the first contact (or 2 weeks after the questionnaire distribution).
The study questionnaire consisted of five sections to collect information on participants’ (1) demographic characteristics (date of birth, gender and educational background), (2) health status (36-Item Short Form Health Survey (SF-36) version 29), (3) pain status (including pain location (body manikins) and CPG) and (if applicable) their (4) pain management and (5) pain without pain management (hypothetical pain). Additionally, information on the area of residence (categorized as rural vs urban) was available from the data for all persons in the sample. All participants were asked to answer the pain management stem question at the beginning of the pain management questionnaire. Those who reported no pain management in the past 4 weeks were instructed to skip the remaining questionnaire sections; those who completed the questions on their pain management went on to the enhanced pain status questionnaire.
Outcome measures
The primary outcome measures were pain prevalence and pain severity. Both outcomes were assessed twice: in the current state, regardless of whether or not the participants used pain management (current pain), and in a hypothetical state without the effect of their pain management (hypothetical pain). The pain severity of participants who reported current pain was assessed using the CPG which categorizes pain status into five different grades, ranging from Grade 0 (no pain) to Grade 4 (high disability – severely limiting). Chronic widespread pain was measured using the American College of Rheumatology (ACR) definition in the 1990 criteria for fibromyalgia:10 Pain in the axial skeleton and in at least two contralateral body quadrants that had persisted for 3 months or longer. The first question of the CPG was altered for inclusion in the enhanced pain status questionnaire to determine participants’ hypothetical pain severity on a 11-point numerical scale:
Imagine you weren’t using any treatments for your pain: How do you think you would rate your pain on a 0-10 scale at the present time, where 0 is ‘no pain’ and 10 is ‘pain as bad as could be’? Please circle one number only.
The secondary outcome measures were demographic and health-related risk markers for pain.
Analysis
Respondents’ personal characteristics, their current pain status and recent pain management were summarized and reported. The prevalence of ‘current pain ’ (proportion of respondents reporting current pain) and ‘all pain ’ (proportion of respondents reporting either current pain and/or hypothetical pain) were determined and compared. The difference in prevalence rates and its 95% confidence interval (CI) were reported. Pain severity with and without consideration of participants’ pain management was explored among persons who provided both estimates (current and hypothetical pain severity). These estimates were reported as medians and interquartile ranges (IQRs). The difference between current and hypothetical pain severity was assessed with the Wilcoxon-signed rank test. Using Poisson regression, associations between pain and risk markers (as measured by questions of the SF-36) were explored for current pain and all pain.
Results
Respondents’ demographic characteristics
Overall, 1604 participants returned a completed questionnaire (response rate = 36.3%). The proportion of females among respondents was 55.3%, and the median age was 55 years (IQR: 44, 65). When compared to non-respondents, respondents were significantly more likely to be female, of older age and living in a rural area (all p < 0.001).
Respondents’ pain status
Out of 1604 questionnaire respondents, 1579 provided information on their current pain status. Of those, 797 reported current pain prevalence (50.5%). Respondents most commonly reported arm/shoulder pain (23.2%) and lower back pain (22.3%), followed by knee pain (16.8%). The ratio between those reporting regional versus widespread pain was approximately 2:1. Among those with widespread pain, the vast majority confirmed that it was a chronic condition (86.8%). Participants’ disability status due to pain was low in the majority of patients (75.1%, CPG 1 + 2), with approximately one-third having high pain intensity. Highly disabling pain was experienced by 20.2% of patients (CPG 3 + 4), with more than half of these reporting severe limitations (Table 1).
Table 1.
Self-reported current pain status.
| Variable | n (%) | |
|---|---|---|
| Pain prevalence (past 4 weeks) | Yes | 797 (50.5) |
| No | 782 (49.5) | |
| Total | 1579 (100.0) | |
| Type of pain | No pain | 782 (49.5) |
| Regional pain | 570 (36.1) | |
| Widespread pain (of which chronic) | 227 (14.4) (197 (86.8)) | |
| Total | 1579 (100.0) | |
| Pain severity (CPG) | No pain | 1 (0.1) |
| Low disability – low intensity (Grade 1) | 392 (49.2) | |
| Low disability – high intensity (Grade 2) | 206 (25.9) | |
| High disability – moderately limiting (Grade 3) | 71 (8.9) | |
| High disability – severely limiting (Grade 4) | 90 (11.3) | |
| Missing information | 37 (4.6) | |
| Total | 797 (100.0) | |
CPG: Chronic Pain Grade.
Self-reported pain management
Out of the 1604 respondents, 930 (58.0%) managed their pain within the past 4 weeks. Of these, more than 70% reported the use of any prescribed or non-prescribed pain treatments. The most commonly reported treatments were non-prescribed tablets and capsules (73.6%), followed by prescribed NSAIDs and non-opioids (52.3%, both). Non-prescribed creams and ointments were used more frequently than those prescribed by a health practitioner (22.0% vs 11.8%). Approximately one in four pain treatment users reported any exercise or complementary treatments to manage their pain (24.9%). Most commonly reported treatments were massage (8.9%), physiotherapy (7.7%), transcutaneous electrical nerve stimulation (TENS) machine (2.9%) or yoga (2.6%). Few respondents reported the use of other complementary therapies, such as hypnotherapy, Alexander technique or homeopathy.
Pain prevalence with and without considering self-reported pain management
The prevalence of current pain was 50.5% (95% CI = 48.0, 52.9). Of the respondents who reported no current pain, 91 (11.6%; 95% CI = 9.4, 13.8) reported hypothetical pain (Figure 2). Hence, the prevalence of all pain was 56.2% (95% CI = 53.7, 58.7). The difference in population estimates of pain prevalence was statistically significant (difference = 5.7%; 95% CI = 2.2, 9.2).
Figure 2.
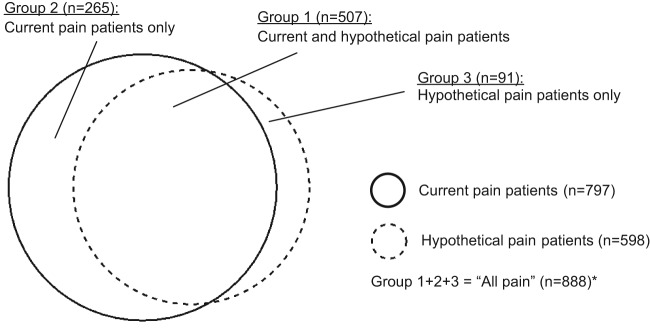
Patients reporting current and/or hypothetical pain. *25 patients with current pain did not answer the question on hypothetical pain.
Pain severity with and without considering self-reported pain management
Out of the 507 respondents that reported current and hypothetical pain (Figure 2), 500 completed the question on pain severity twice: before and after considering the effect of their pain management. In 100 cases (20.0%), the participants indicated that their pain severity would not have changed had they not managed their pain with pain-relieving treatments. The majority of patients (n = 376, 75.2%) reported that they would have had more severe pain if they had not used any treatments for its management. On average, the pain severity increased by 3 points on a 11-point numerical rating scale when the pain patients considered their pain management (current pain severity, median: 3, IQR: 2, 6; hypothetical pain severity, median: 6, IQR: 4, 8). The change of participants’ self-reported pain severity was statistically significant (Wilcoxon-signed rank test; p < 0.001).
Risk markers for pain
Low educational background (defined as no educational background or secondary school) was significantly associated with current pain (incidence rate ratio (IRR) = 1.11; 95% CI = 1.01, 1.23) but not significantly associated with the prevalence of all pain (IRR = 1.05; 95% CI = 0.96, 1.15). Furthermore, the risk of reporting current and all pain was higher among females, older respondents and those living in urban areas. However, none of these associations proved to be statistically significant (Table 2). It was observed that nearly all associations between demographic risk factors and pain prevalence were stronger for current pain when compared to all pain.
Table 2.
Risk markers for pain prevalence – demographic factors.
| Risk marker | Pain patients – ‘current pain’ (%) | Crude IRR (95% CI) | Pain patients – ‘all pain’ (%) | Crude IRR (95% CI) | |
|---|---|---|---|---|---|
| Gender | Male | 340 (42.7) | 1.00 | 379 (42.7) | 1.00 |
| Female | 457 (57.3) | 1.08 (0.98; 1.20) | 509 (57.3) | 1.08 (0.99, 1.18) | |
| Total | 797 (100.00) | 888 (100.00) | |||
| Age | 25–34 years | 75 (9.4) | 1.00 | 91 (10.3) | 1.00 |
| 35–44 years | 117 (14.7) | 1.04 (0.84; 1.29) | 133 (15.0) | 0.98 (0.82, 1.17) | |
| 45–54 years | 184 (23.1) | 1.17 (0.96; 1.42) | 199 (22.4) | 1.04 (0.88, 1.23) | |
| 55–64 years | 199 (25.0) | 1.17 (0.97, 1.42) | 219 (24.7) | 1.06 (0.90, 1.25) | |
| 65–74 years | 145 (18.2) | 1.14 (0.93, 1.40) | 160 (18.0) | 1.04 (0.87, 1.23) | |
| 75–84 years | 59 (7.4) | 1.17 (0.91, 1.49) | 65 (7.3) | 1.06 (0.86, 1.31) | |
| 85–94 years | 18 (2.3) | 1.34 (0.96, 1.88) | 21 (2.4) | 1.29 (0.98, 1.70) | |
| Total | 797 (100.0) | 888 (100.0) | |||
| Education | ≥Vocational qualification | 485 (60.8) | 1.00 | 553 (62.3) | 1.00 |
| No education/Secondary School | 303 (38.0) | 1.11 (1.01; 1.23) | 326 (36.7) | 1.05 (0.96; 1.15) | |
| Missing information | 9 (1.1) | 9 (1.0) | |||
| Total | 797 (100.0) | 892 (100.0) | |||
| Area of residence | Urban | 364 (45.7) | 1.00 | 401 (45.2) | 1.00 |
| Rural | 426 (53.5%) | 1.02 (0.92; 1.12) | 479 (53.9) | 1.04 (0.95; 1.14) | |
| Missing information | 7 (0.9) | 8 (0.9) | |||
| Total | 797 (100.0) | 888 (100.0) | |||
IRR: incidence rate ratio; CI: confidence interval.
A significant dose–risk relationship was determined between participants’ self-reported general health and the prevalence of any pain outcome (non-parametric test for trend; p < 0.001). Those who reported poor health had an almost 3-fold increased risk (all pain) or a 3.5-fold increased risk (current pain) of reporting pain when compared to those who were in excellent health (Table 3). Similar results were determined for participants’ self-reported vitality: the lower the level of energy, the higher was the risk of reporting current and all pain. Comparable dose–risk relationships were determined when the associations of pain prevalence with participants’ mental health, physical functioning and social functioning were explored (non-parametric test for trend; p < 0.001). The risk of reporting current and all pain was doubled when respondents reported any depressive symptoms, and almost doubled when limited physical and social functioning were reported (Table 3). All health-related risk factors were stronger predictors for current pain when compared to all pain.
Table 3.
Risk markers for pain prevalence – health-related factors.
| Risk marker | Pain patients – ‘current pain’ (%) | Crude IRR (95% CI) | Pain patients – ‘all pain’ (%) | Crude IRR (95% CI) | |
|---|---|---|---|---|---|
| General health | Excellent | 54 (6.8) | 1.00 | 67 (7.6) | 1.00 |
| Very good | 249 (31.2) | 1.54 (1.20, 1.98) | 291 (32.8) | 1.45 (1.17, 1.80) | |
| Good | 318 (39.9) | 2.37 (1.86, 3.01) | 346 (39.0) | 2.08 (1.69, 2.55) | |
| Fair | 124 (15.6) | 2.83 (2.21, 3.62) | 131 (14.8) | 2.41 (1.94, 2.98) | |
| Poor | 52 (6.5) | 3.51 (2.76, 4.48) | 53 (6.0) | 2.89 (2.34, 3.56) | |
| Total | 797 (100.0) | 888 (100.0) | |||
| High level of energy | All of the time | 23 (2.9) | 1.00 | 25 (2.8) | 1.00 |
| Most of the time | 283 (35.5) | 1.45 (1.01, 2.08) | 329 (37.1) | 1.55 (1.10, 2.18) | |
| Some of the time | 265 (33.3) | 2.27 (1.58, 3.25) | 291 (32.8) | 2.29 (1.63, 3.22) | |
| A little of the time | 132 (16.6) | 2.92 (2.03, 4.19) | 141 (15.9) | 2.87 (2.04, 4.03) | |
| None of the time | 92 (11.5) | 2.96 (2.05, 4.26) | 99 (11.2) | 2.93 (2.08, 4.12) | |
| Missing information | 2 (0.3) | 3 (0.3) | |||
| Total | 797 (100.0) | 888 (100.0) | |||
| Feeling calm and peaceful | All of the time | 45 (5.7) | 1.00 | 53 (6.0) | 1.00 |
| Most of the time | 365 (45.8) | 1.30 (1.01, 1.67) | 410 (46.2) | 1.24 (0.996, 1.55) | |
| Some of the time | 206 (25.9) | 1.67 (1.29, 2.15) | 230 (25.9) | 1.58 (1.26, 1.98) | |
| A little of the time | 126 (15.8) | 2.10 (1.63, 2.72) | 135 (15.2) | 1.91 (1.53, 2.40) | |
| None of the time | 52 (6.5) | 2.23 (1.70, 2.93) | 55 (6.2) | 2.00 (1.57, 2.54) | |
| Missing information | 3 (0.4) | 5 (0.6) | |||
| Total | 797 (100.0) | 888 (100.0) | |||
| Limited in walking more than one mile | Not limited at all | 494 (62.0) | 1.00 | 566 (63.7) | 1.00 |
| Limited a little | 159 (20.0) | 1.68 (1.51, 1.87) | 169 (19.0) | 1.56 (1.42, 1.71) | |
| Limited a lot | 139 (17.4) | 1.81 (1.63, 2.01) | 147 (16.6) | 1.67 (1.52, 1.83) | |
| Missing information | 5 (0.6) | 6 (0.7) | |||
| Total | 797 (100.0) | 888 (100.0) | |||
| Health interferes with social activities | Not at all | 439 (55.1) | 1.00 | 503 (56.6) | 1.00 |
| Slightly | 185 (23.2) | 1.50 (1.33, 1.68) | 202 (22.8) | 1.43 (1.29, 1.58) | |
| Moderately | 65 (8.2) | 1.78 (1.54, 2.05) | 70 (7.9) | 1.67 (1.48, 1.89) | |
| Quite a bit | 69 (8.7) | 1.93 (1.70, 2.20) | 72 (8.1) | 1.76 (1.57, 1.97) | |
| Extremely | 37 (4.7) | 1.94 (1.65, 2.27) | 39 (4.4) | 1.78 (1.55, 2.05) | |
| Missing information | 2 (0.3) | 2 (0.2) | |||
| Total | 797 (100.0) | 888 (100.0) | |||
IRR: incidence rate ratio; CI: confidence interval.
Discussion
Incorporating self-reported pain management information in an epidemiological study of pain led to significantly increased estimates of both pain prevalence (5.7%) and pain severity. Furthermore, the associations between demographic and health-related risk markers and the prevalence of pain attenuated slightly after identifying patients with hypothetical pain.
The strengths of this study were the recruitment of a large population-based sample and the thorough development of the questionnaires. Furthermore, we believe that this is the first study that has estimated the prevalence and severity of pain in a general population, in consideration of participants’ self-reported pain management. Nevertheless, there are some limitations to the study that need to be addressed. First, the response rate was modest. Only 1604 out of 4600 selected persons completed and returned a questionnaire (36%). In order to examine whether non-response bias was introduced, the results were weighted back to the study population on the basis of their gender, age and area of residence (data not shown). Differences in prevalence estimates were small and not statistically significant. Likewise, the adjusted model on health-related risk factors for pain differed marginally when compared to the crude analysis. Based on the assumption that late respondents resemble non-respondents, a second approach to estimate the effect of non-response was undertaken by comparing early and late respondents (data not shown). On the whole, the pain prevalence in both groups differed minimally, with late respondents demonstrating a lower prevalence rate. Furthermore, there was no consistent pattern of early respondents reporting poorer health than late respondents or vice versa. There was therefore no evidence to imply that the findings of this study were affected by non-response bias. Nevertheless, it cannot be discounted that there may have been other factors associated with questionnaire response which were not captured in the questionnaire. Second, the study was affected by misclassification. With the inclusion of the enhanced pain status questionnaire, pain was assessed twice for all participants with current pain and pain management. As per the data provided, 108 out of the 601 patients who reported current pain symptoms and pain management did not report any hypothetical pain (18%). This is logically counter-intuitive and unlikely to be true. Since the hypothetical pain status questionnaire was used to identify the pain patients that were not captured by the standard pain status questionnaire, the misclassification should not have had an effect on the measurement of pain prevalence. It might, however, have had an effect on the estimated pain severity. Given that 108 failed to report hypothetical pain (and therefore also failed to provide an estimate for their hypothetical pain severity), the estimate of participants’ hypothetical pain severity may be an inaccurate reflection of the truth. Nevertheless, it is unlikely that the established increase in pain severity due to the absence of pain management would change substantially.
Using the standard pain status questionnaires, pain in the past 4 weeks, lasting for 1 day or longer was reported by 50.5% of the participants. This prevalence rate was somewhat lower than those determined in previous studies which used the same pain questionnaire within their population samples. In a study by Hunt et al.,11 the prevalence of pain was explored in a general population near Manchester. The authors found a pain prevalence of 57% within the past month. Another study by Macfarlane et al.6 found a pain prevalence of 63% in their population sample in Aberdeen and North Cheshire. The crude prevalence rate of chronic widespread pain in the current study was 12.5%. The results were in line with similar studies previously conducted in the United Kingdom, such as that of Hunt et al.11 who determined a chronic pain prevalence of 12.9% in their population sample in Manchester or Croft et al.12 who reported a prevalence of 11.2%. In the review by Harstall and Ospina,13 the authors established a weighted chronic pain prevalence of 11.8% across studies using the ACR definition and criteria for fibromyalgia10. In accordance with results of a number of earlier studies,14,15 the prevalence of pain was associated with several demographic and health-related risk markers, such as lower education and (albeit not statistically significant) older age, female gender and rural residence. Moreover, pain was highly associated with poor health reports, underpinning the findings of previous studies.16–18
The enhanced pain status questionnaire identified 91 participants who reported no current pain but imagined that they would have had any pain had they not managed it with the treatments reported in the questionnaire (hypothetical pain patients). When these patients were included in the risk markers analysis, the strength of the associations between pain prevalence and any risk marker variable decreased. The participants with hypothetical pain were therefore somewhat healthier when compared to those with current pain. These findings are plausible and support the construct validity of the questionnaire. The results of the enhanced pain status questionnaire also gave some insight into the efficacy of participants’ pain management. Interestingly, a large proportion of ‘all pain’ sufferers reported ‘current’ pain despite a high report of pain management. On average, these patients estimated that their ‘current’ pain was significantly reduced by their pain management (3 points on a numerical scale). Only a minority of ‘all pain’ patients gained complete pain relief through their pain management (5.7%).
It has been demonstrated that pain management is vital for pain patients and associated with a significant reduction of their pain severity scores. Hence, the collection and consideration of pain management information in population-based studies is crucial. If it is not feasible to gather detailed information on patients’ pain management, researchers should make an effort to collect information on participants’ pain status in a state without their pain management. This will ensure a more accurate estimation of the burden of pain and allow the comparisons of pain patients who manage and who do not manage their pain.
To the best of our knowledge, this is the first study to estimate people’s pain status, taking into account their pain management. We have established that pain management has a significant impact on people’s pain experience and therefore on their self-reported pain status. As a consequence, pain management information should routinely be collected in future studies assessing pain.
Acknowledgments
We would like to thank everyone who was involved in the study, including Professor Sir Lewis Ritchie (Director of Public Health, NHS Grampian), John Lemon (University of Aberdeen), Dr Fiona Garton (University of Aberdeen) and the Aberdeen Service User Group. Finally, we would like to acknowledge all data entry clerks (Maxx Livingstone, Rory Macfarlane, Georgia Mannion-Krase and Hazel Reilly) and participants of the study. We would also like to thank the Aberdeen Service Users Group of the Institute of Applied Health Sciences, University of Aberdeen. This study was conceived by G.J.M., G.T.J. and C.M.B. It was planned by all the authors and E.F. conducted the study. E.F. drafted the manuscript and all other authors critically reviewed the manuscript and provided important intellectual content.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study was approved by the North of Scotland National Health Service Research Ethics Committee (REC reference: 12/NS/0079).
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: We would like to thank the Institute of Applied Health Sciences (IAHS) at the University of Aberdeen for funding the PhD studentship of E.F.
References
- 1. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10: 287–333. [DOI] [PubMed] [Google Scholar]
- 2. Bond C, Hannaford P. Issues related to monitoring the safety of over-the-counter (OTC) medicines. Drug Saf 2003; 26: 1065–1074. [DOI] [PubMed] [Google Scholar]
- 3. Ernst E. Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination. Vaccine 2001; 20 Suppl 1: S90–S93. [DOI] [PubMed] [Google Scholar]
- 4. Fouladbakhsh JM, Vallerand AH, Jenuwine ES. Self-treatment of pain among adolescents in an urban community. Pain Manag Nurs 2012; 13: 80–93. [DOI] [PubMed] [Google Scholar]
- 5. Haetzman M, Elliott A, Smith B, et al. Chronic pain and the use of conventional and alternative therapy. Fam Pract 2003; 20: 147–154. [DOI] [PubMed] [Google Scholar]
- 6. Macfarlane GJ, Beasley M, Jones EA, et al. The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain 2012; 153: 27–32. [DOI] [PubMed] [Google Scholar]
- 7. Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol 1993; 46: 423–429. [DOI] [PubMed] [Google Scholar]
- 8. Von Korff M, Dworkin SF, Le Resche L. Graded chronic pain status: an epidemiologic evaluation. Pain 1990; 40: 279–291. [DOI] [PubMed] [Google Scholar]
- 9. Ware JE, Kosinski M, Dewey JE. How to score version 2 of the SF-36 health survey: standard & acute forms. Lincoln, RI: QualityMetric Incorporated, 2000. [Google Scholar]
- 10. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum 1990; 33: 160–172. [DOI] [PubMed] [Google Scholar]
- 11. Hunt I, Silman A, Benjamin S, et al. The prevalence and associated features of chronic widespread pain in the community using the ‘Manchester’ definition of chronic widespread pain. Rheumatology 1999; 38: 275–279. [DOI] [PubMed] [Google Scholar]
- 12. Croft P, Rigby A, Boswell R, et al. The prevalence of chronic widespread pain in the general population. J Rheumatol 1993; 20: 710–713. [PubMed] [Google Scholar]
- 13. Harstall C, Ospina M. How prevalent is chronic pain. Pain Clin Updat 2003; 11: 1–4. [Google Scholar]
- 14. Bergman S, Herrström P, Jacobsson LT, et al. Chronic widespread pain: a three year followup of pain distribution and risk factors. J Rheumatol 2002; 29: 818–825. [PubMed] [Google Scholar]
- 15. Reisbord LS, Greenland S. Factors associated with self-reported back-pain prevalence: a populationdashbased study. J Chronic Dis 1985; 38: 691–702. [DOI] [PubMed] [Google Scholar]
- 16. Arnold LM, Witzeman KA, Swank ML, et al. Health-related quality of life using the SF-36 in patients with bipolar disorder compared with patients with chronic back pain and the general population. J Affect Disord 2000; 57: 235–239. [DOI] [PubMed] [Google Scholar]
- 17. Bergman S, Jacobsson LT, Herrström P, et al. Health status as measured by SF-36 reflects changes and predicts outcome in chronic musculoskeletal pain: a 3-year follow up study in the general population. Pain 2004; 108: 115–123. [DOI] [PubMed] [Google Scholar]
- 18. Mäntyselkä PT, Turunen JH, Ahonen RS, et al. Chronic pain and poor self-rated health. JAMA 2003; 290: 2435–2442. [DOI] [PubMed] [Google Scholar]


