Abstract
Background:
Musculoskeletal pain in the distal upper limb is relatively common, can be a cause of disability, presents a high cost to society and is clinically important. Previous reviews of prognostic factors have focused on pain in the proximal upper limb, whole upper extremity or isolated regions of the distal upper limb.
Aim:
To identify factors that predict outcome of distal upper limb pain.
Study design:
Systematic review
Method:
Eight bibliographic databases were searched from inception to March 2014. Eligible articles included adults with pain anywhere in the distal upper limb at baseline from randomised controlled trials with a waiting list, expectant policy or usual care group, or observational studies where no treatment or usual care was provided. Data describing the association between a putative prognostic factor and pain or functional outcome at follow-up were required. Quality was assessed using the Quality in Prognostic Studies tool.
Results:
Seven articles reporting on six studies were identified. Heterogeneity of study populations and outcome measures prevented a meta-analysis so a narrative synthesis of results was undertaken. Three factors (being female, a longer duration of the complaint at initial presentation and having musculoskeletal pain in multiple locations) were significantly associated with poor pain outcome in more than one study. Being female was the only factor significantly associated with poor functional outcome in more than one study.
Conclusions:
A range of sociodemographic, pain-related, occupational and psychosocial prognostic factors for distal upper limb pain outcomes were investigated in studies included in the review. However, due to the lack of commonality of factors investigated and lack of consistency of results across studies, there is limited evidence for predictors of distal upper limb pain outcomes. Further research is required to identify prognostic factors of distal upper limb pain, particularly modifiable factors that may influence management.
Keywords: Distal upper limb, musculoskeletal pain, prognosis, prognostic factors, systematic review
Introduction
Musculoskeletal pain in the upper limb is associated with specific and non-specific conditions. In a population survey of working-aged English adults, 48% reported experiencing upper limb pain in the past year,1 with 14% describing persistent pain (>6 months), 10% reporting disabling pain (making it difficult or impossible to sleep, get dressed and do chores)2 and 31% consulting their general practitioner. The UK Labour Force Survey reported approximately 3.8 million lost working days in 2008/2009 due to upper limb musculoskeletal conditions,3 comparable to findings from previous years. Ryall et al.4 found that, of those presenting to primary care or physiotherapy with upper limb pain, 42% reported pain in the distal region (elbow, forearm, wrist and hand), with 48% reporting persistent symptoms and 19% describing unremitting pain a year later. While evidence suggests that distal upper limb pain is relatively common, a cause of disability, costly to society and clinically important, literature focused on prognostic factors is underdeveloped, overshadowed by aetiological5,6 and management research.7–10 Studies of prognostic factors have concentrated on the proximal upper limb11 or pain anywhere in the upper extremity,12–14 often inclusive of neck and back symptoms.15,16 Two reviews restricted to the distal region have investigated elbow complaints17 and hand pain progression in older adults.18 The former included studies of systematic interventions (not reflective of usual care) and the latter comprised cross-sectional investigations only. The aim of this review was to identify and synthesise evidence for prognostic factors of the natural course or conservative management of distal upper limb pain. Knowledge of these factors may assist employers and clinicians in identifying those at higher risk of poor outcome. Elucidation of modifiable predictors could inform management and referral, as well as occupational and public health initiatives. Prognostic factors may be compared to findings for proximal and whole upper limb pain and may be used to support or refute arguments for generic predictors of musculoskeletal pain outcome, regardless of site.
Methods
The review was undertaken in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.19 Eligible studies included adult subjects (⩾18 years) with pain in the elbow, forearm, wrist and/or hand, including specific disorders (e.g. epicondylitis) and non-specific conditions (e.g. elbow complaints). Randomised controlled trials (RCTs) with a waiting list, expectant policy or usual, conservative care group, or observational studies where no or usual conservative treatment was provided, were eligible. Investigation of association between a putative prognostic factor and pain or functional outcome at follow-up was required or raw data from which an association could be determined. Excluded studies included participants with systemic disease (e.g. rheumatoid arthritis), traumatic injury, prior surgery, active/pending compensation claims or studies focused on specific sub-groups (e.g. pregnancy). The search was limited to articles published in English language peer-reviewed journals involving human subjects. A search string, developed in consultation with a medical librarian, was applied to eight databases (Medline, EMBASE, CINAHL, AMED, Web of Science, PsycINFO, the Cochrane Central Register of Controlled Trials and the Cochrane Methodology Register), from inception to March 2014. Three search sets combined terms describing ‘anatomy or pathology’ AND ‘prognosis’ AND ‘symptoms’ (Supplement 1 describes the complete search strategy). Duplicate references were removed and screening was undertaken by one reviewer (D.W.) by title, and then abstract. Two reviewers (G.T.J. and K.R.M.) independently screened 10% of search results to ensure consensus. Full-text articles were retrieved for all potentially eligible studies and evaluated against predefined criteria. Reference lists of eligible studies were checked. One reviewer (D.W.) extracted data on study design and duration, the disorder/condition, natural or clinical course, number of participants and attrition, sampling frame, characteristics (age and sex), outcome measures and pain and disability outcome at follow-up. To be defined as a predictor, a factor had to be significant in a multivariable model (significance defined as p ⩽ 0.05 or effect measure confidence interval (CI) not inclusive of 1) in more than one study. In two instances where a study had more than one follow-up point,20–22 or in one study where sub-analyses for different distal regions were presented,23 a factor had to meet the above criteria for any sub-analysis. Methodological quality was assessed by one reviewer (D.W.) using the Quality in Prognostic Studies tool (QuIPS), using criteria published by Hayden et al.24
Results
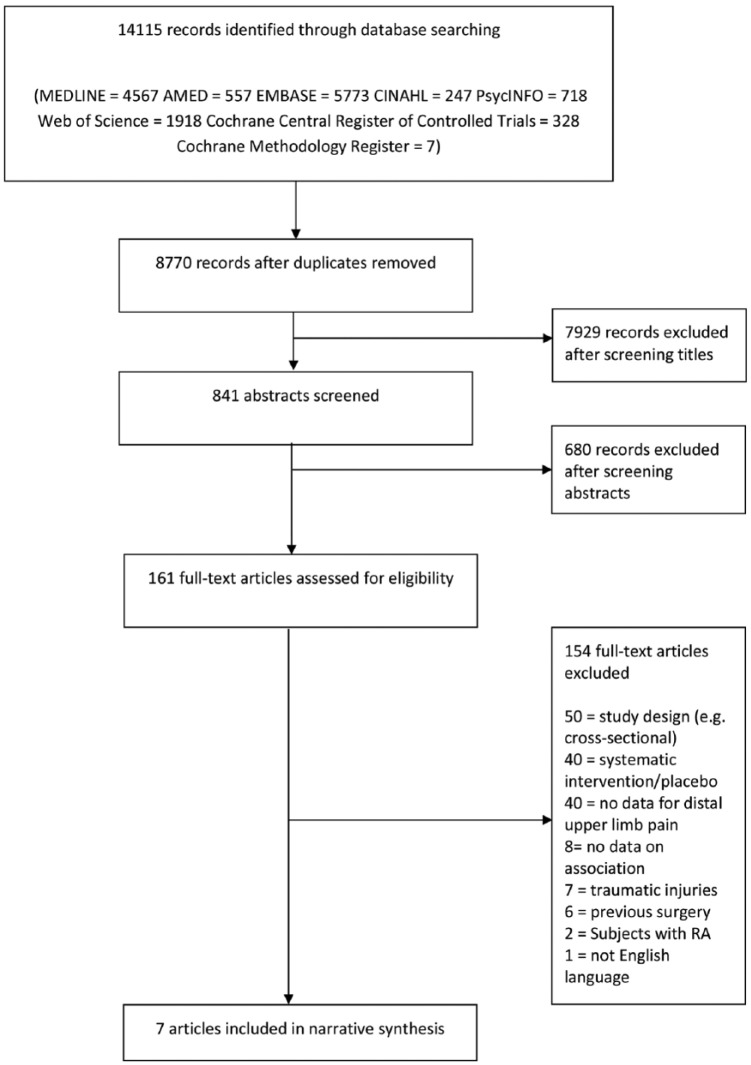
A total of 14,115 references were identified by the search, reduced to 8770 after removing duplicates. After title and abstract screening, 161 full-text articles were retrieved and 154 were excluded after checking eligibility (Figure 1). Seven articles, reporting on six studies, met inclusion criteria. No further studies were identified after checking reference lists.
Figure 1.
Flow of information through different phases of the systematic review.
Study characteristics
All seven identified articles described six prospective cohort studies, three based in the workplace, one in primary care, one in tertiary care and one recruited from a private sports clinic and hospital outpatient department (reported in two articles 20,21). Two studies (three articles) focused on specific disorders (lateral epicondylitis and carpal tunnel syndrome (CTS)) and four studies (four articles) investigated non-specific conditions (elbow complaints, hand pain, finger pain and distal upper limb pain). Study size ranged from 86 to 821 participants.
Outcome measures
Four studies used dichotomous pain outcome measures: a forced choice answer (pain at follow-up, ‘yes’ or ‘no’),25 a question about bothersomeness at follow-up, ‘no’ indicating recovery,22 pain categorised as ‘no’ when zero was reported on a four-point scale,26 and categorised responses from a questionnaire as pain reduction or persistence, based on change at follow-up on a seven-point scale.23 One study created three categories of pain outcome from an 11-point Numerical Rating Scale (NRS):27 no pain (0), moderate pain (1–4), and severe pain (>5). Mean change in pain (standard deviation (SD)) was reported in two studies, measured by visual analogue scale (VAS)20,21 or 11-point NRS.22 Other outcomes were changed in functional limitation/disability (three studies used different instruments: modified pain-free function index,22 Levine Functional Status Scale27 and Disability of the Arm, Shoulder and Hand (DASH)20,21) and job limitation (one study).27 Variation in definitions or thresholds and heterogeneity of study populations and outcome measures prevented a meta-analysis; therefore, a narrative synthesis was undertaken.
Quality assessment
Of the six studies, five were judged to be at low risk of bias and one at moderate risk20,21 (Table 1). One study did not fully state inclusion criteria and failed to provide an adequate description of the baseline sample.23 Another failed to report number of eligible subjects invited to participate.20,21 Four studies failed to describe attempts to collect information from participants who dropped out and five studies did not provide reasons for attrition. However, five of the six studies presented a brief summary of comparison between completers and non-completers, reporting no significant differences for stated characteristics. All studies were at low risk of bias for prognostic factor and outcome measurement. Measurement of confounders and statistical analysis and reporting were also considered to present low risk of bias in all studies.
Table 1.
Quality assessment of included studies (low/moderate/high = risk of bias).
| Study | Study participation | Study attrition | Prognostic factor measurement | Outcome measurement | Consideration of confounders and measurement | Statistical analysis and presentation | Overall risk of bias |
|---|---|---|---|---|---|---|---|
| Padua et al.25 | Low | Low | Low | Low | Low | Low | Low |
| Waugh et al.20,21 | Moderate | Moderate | Low | Low | Low | Low | Moderate |
| Bot et al.22 | Low | Low | Low | Low | Low | Low | Low |
| Lassen et al.23 | Moderate | Low | Low | Low | Low | Low | Low |
| Ding et al.26 | Low | Low | Low | Low | Low | Low | Low |
| Descatha et al.27 | Low | Low | Low | Low | Low | Low | Low |
Pain course
Of the six prospective cohort studies, three were conducted within a clinical setting: conservative care for lateral epicondylitis (follow-up duration 8 weeks and 6 months), conservative care for elbow complaints (follow-up of 3 months and 1 year) and natural course of pain associated with CTS for 1 year after tertiary care referral. Three studies were conducted in an occupational context: distal upper limb pain over 1 year, hand pain over 3 years and finger joint pain over 5 years (Table 2). Within the clinical setting, pain persistence ranged from 8% at 6 months for conservatively treated lateral epicondylitis to 74% for pain associated with the natural history of CTS after referral to tertiary care. Pain persistence in occupational studies decreased as follow-up duration increased: 70% for pain anywhere in the distal upper limb at 1 year, 52% for hand pain at 3 years and 18% for finger joint pain at 5 years.
Table 2.
Data extraction.
| Authors | Follow-up duration | Condition | Natural history or conservative treatment | Participants and sampling frame | Baseline characteristics, mean (SD) unless otherwise stated | Outcome measures | Results at follow-up, mean (SD) unless otherwise stated |
|---|---|---|---|---|---|---|---|
| Padua et al.25 | 10–15 months | Idiopathic carpal tunnel syndrome (CTS) | Natural history (untreated) | Baseline: 330 | Total cohort (n = 330) | Boston Carpal Tunnel Questionnaire | Results for untreated cohort (n = 196) At follow-up: Improvement in pain (% of hands): 26% |
| Follow-up: 264 (80%)196 subjects untreated throughout follow-up | Age: 51.9 (13.8) | Historic and Objective scale (Hi-Ob). 2 domains: Clinical history and objective findings; Pain (yes or no) | Baseline painful hands: 57% | ||||
| Patients referred to multiple centres for neurophysiological testing in Italy | Female: 83% | Electrodiagnostic evaluation | Follow-up painful hands: 43% (p = 0.009) | ||||
| Untreated cohort (n = 196) | (Comparison at the patient level also demonstrated significant improvement in pain, p = 0.038. No further data provided.) | ||||||
| Age: 52.0 (13.4) | Worsening pain: 12% | ||||||
| Female: 82% | Stationary pain: 62% | ||||||
| Waugh et al.20,21 | 8 weeks and 6 months | Lateral epicondylitis | Conservative treatment: physiotherapy | Baseline: 86 | Age: 44 (8) | Disability of the Arm, Shoulder and Hand (DASH) (30-item questionnaire scored out of 100. Higher score = greater disability) | DASH |
| Follow-up at 8 weeks: 83 (97%) | Female: 57% (at 8 weeks); 60% (at 6 months) | Pain visual analogue scale (VAS) (100 mm vertical line) | DASH 0 at 6 months (no disability) = 20% | ||||
| Follow-up at 6 months: 60 (70%)Nine private sports medicine clinics and two hospital outpatient departments in Canada | Question regarding recovery of symptoms | DASH 10 at 6 months (no or minimal) = 67% | |||||
| DASH > 40 at 6 months (moderate to high) = 6.7% | |||||||
| Pain VAS | |||||||
| Pain VAS 0 mm (no pain) at 6 months = 38% | |||||||
| Pain VAS ⩽10 mm (no or minimal) = 65% | |||||||
| Pain VAS >60 mm (mod. to severe) = 5% | |||||||
| Recovery of symptoms | |||||||
| Symptoms consistently improving: 80% | |||||||
| Symptoms completely resolved: 33% | |||||||
| No improvement of symptoms: 6.7% | |||||||
| Worsening of symptoms: 1.7% | |||||||
| Bot et al.22 | 3 months and 1 year | Elbow complaints | Authors assumption: In most cases, initial treatment based on an expectant policy. | Baseline: 1813-month follow-up: 157 (87%)12-month follow-up: 152 (84%) | Age: 47.9 (11.6)Female: 66% | Patient-perceived recovery (Yes or No. No = recovered) | Recovery: 3 months = 13%; 12 months = 34% |
| General practice in the Netherlands | Change in pain intensity (Pain during previous 24 hours, 11-point Numerical Rating Scale) | Of those not fully recovered, substantial improvement: 3 months = 24%; 12 months = 21% | |||||
| Change in functional disability(modified pain-free function index, 10-item scale, score range 0–100) | Of those not fully recovered, some improvement: 3 months = 37%; 12 months = 25% | ||||||
| Reduction in pain intensity3 months: 1.3 (2.3) points 12 months: 2.1 (2.6) points (p < 0.01) | |||||||
| Reduction in disability (SD) 3 months: 6.3 (16.2) points 12 months: 11.9 (21.2) points (p < 0.01) | |||||||
| Lassen et al.23 | 1 year | ‘Severe’ elbow, forearm and hand pain (right side only) | No intervention. | Baseline: 821Follow-up: 673 (82%)Technicians (computer users) working in DenmarkNUDATA study | From NUDATA study (baseline n = 6943)Age: 41.7 (8.9)Female: 64%. | Self-reported pain questionnaire (pain reduction versus pain persistence. Pain or discomfort in the right elbow, forearm or wrist-hand in past 12 months captured by a 7-point scale) | Persistent pain |
| Elbow: 68% | |||||||
| Forearm: 67% | |||||||
| Wrist-hand: 74% | |||||||
| Persistent ‘severe’ pain in one region: 70% | |||||||
| Persistent ‘severe’ pain in two regions: 64% | |||||||
| Persistent ‘severe’ pain in three regions: 70% | |||||||
| Ding et al.26 | 5 years | Finger joint pain | No intervention. | Baseline: 543 | Age: 54 (5) | Subject-reported location and severity of hand joint pain in last 30 days (4-point scale: 0 = no pain, 3 = severe. Categorised as no pain (0) or pain (⩾1)) | Persistent pain in ⩾1 joint in right hand: 23.0% |
| 5-year follow-up: 482 (88.8%; inclusive of those with and without pain at baseline and follow-up)Female dentists and teachers in Finland | Female: 100% | Persistent pain in ⩾1 joint in left hand: 14.1% | |||||
| Recovery (pain at baseline only) (right hand): 8.3% | |||||||
| Recovery (pain at baseline only) (left hand): 12.0% | |||||||
| Descatha et al.27 | 3 years | CTS symptoms and other hand pain | No intervention. | Baseline: 1553-year follow-up: 155 (100%) | Age: 29.51 (9.16) | Persistence of pain: Severe hand pain at follow-up (⩾5 on an 11-point Numerical Rating Scale in last 30 days. Moderate pain: 1–4; No pain: 0) | Severe pain at follow-up: 32.9% |
| Industrial workers in North America (high and low hand-intensive jobs) | Female: 25% | Change in functional status (Levine Functional Status Scale, 5-point scale) | Moderate pain at follow-up: 18.7% | ||||
| Predictors of Carpal Tunnel Syndrome (PrediCTS) study | Change in job limitation (dichotomous composite outcome) | No pain at follow-up: 48.4% | |||||
| 11.6% reported functional status limitations | |||||||
| 21.9% reported job limitations at follow-up |
Prognostic factors
Multiple linear, logistic and Cox regression were used to analyse prognostic factors depending on the nature of the outcome variable. In total, associations between 58 different factors and outcomes were investigated across the six studies. There was a lack of commonality of factors investigated, with 42 (72%) investigated in only one study (Table 3). Sixteen factors were examined in two or more studies and only six factors were investigated by three or more studies: age, sex, body mass index, pain severity and duration, and other pain sites. Two studies included all covariates in regression models and four used selection procedures to determine inclusion (Table 4).
Table 3.
Putative prognostic factors investigated across all studies.
| Idiopathic carpal tunnel syndrome (CTS) |
Lateral epicondylitis |
Elbow complaints |
Distal upper limb pain |
Finger joint pain |
CTS and hand pain |
|
|---|---|---|---|---|---|---|
| Padua et al.25 | Waugh et al.20,21 | Bot et al.22 | Lassen et al.23 | Ding et al.26 | Descatha et al.27 | |
| Sociodemographic factors | ||||||
| Age | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Sex | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Body mass index | ✓ | ✓ | ✓ | |||
| Handedness | ✓ | |||||
| Marital status | ✓ | |||||
| Having children in the household | ✓ | |||||
| Smoking status | ✓ | ✓ | ||||
| Education level | ✓ | ✓ | ||||
| Complaint characteristics | ||||||
| Duration | ✓ | ✓ | ✓ | |||
| Presumed cause | ✓ | |||||
| Previous history | ✓ | ✓ | ||||
| Uni- or bilaterality | ✓ | ✓ | ||||
| Complaint on dominant side | ✓ | |||||
| Symptoms experienced | ✓ | ✓ | ||||
| Frequency of discomfort | ✓ | |||||
| Severity of pain at baseline | ✓ | ✓ | ✓ | |||
| Site of lesion | ✓ | ✓ | ||||
| Other musculoskeletal complaints | ✓ | ✓ | ✓ | |||
| Non-musculoskeletal complaints | ✓ | ✓ | ||||
| Symptoms of CTS without nerve conduction studies | ✓ | |||||
| Abnormal upper limb neurodynamics | ✓ | |||||
| Confirmed CTS | ✓ | |||||
| Radiographic osteoarthritis | ✓ | |||||
| Pain anywhere in the distal upper limb | ✓ | |||||
| Phalen test result | ✓ | |||||
| Occupational | ||||||
| Physical work exposures | ✓ | ✓ | ||||
| Social support at work | ✓ | |||||
| Employment status | ✓ | |||||
| Occupation (teacher vs dentist) | ✓ | |||||
| Mouse time | ✓ | |||||
| Keyboard time | ✓ | |||||
| Support during mouse use | ✓ | |||||
| Support during keyboard use | ✓ | |||||
| ‘Abnormal’ mouse position | ✓ | |||||
| ‘Abnormal’ keyboard position | ✓ | |||||
| Chair adjustment | ✓ | |||||
| Desk adjustment | ✓ | |||||
| Dissatisfaction with workplace | ✓ | |||||
| Job demands | ✓ | |||||
| Job control | ✓ | |||||
| Job strain | ✓ | |||||
| Time pressure | ✓ | |||||
| Functional status and physical activity | ||||||
| Baseline functional status/disability | ✓ | ✓ | ||||
| Norm for physical activity | ✓ | |||||
| American College of Sports Medicine position stand | ✓ | |||||
| Leisure time physical activities | ✓ | |||||
| Baseline leisure time hand activity | ✓ | |||||
| Hand stress (work and leisure) | ✓ | |||||
| Psychosocial factors | ||||||
| Distress | ✓ | |||||
| Coping | ✓ | |||||
| Kinesiophobia | ✓ | |||||
| Negative affectivity | ✓ | |||||
| Type A behaviour | ✓ | |||||
| Social support | ✓ | ✓ | ||||
| General health | ||||||
| Vitality | ✓ | |||||
| Perceived general health | ✓ | |||||
| Perceived overall quality of life | ✓ | |||||
| Use of analgesics | ✓ | |||||
Table 4.
Covariates included in multivariable models in more than one study – pain.
| Idiopathic carpal tunnel syndrome (CTS) |
Lateral epicondylitis |
Elbow complaints |
Distal upper limb, elbow, forearm and wrist-hand pain |
Finger joint pain |
CTS and hand pain |
|
|---|---|---|---|---|---|---|
| Padua et al.25 | Waugh et al.20,21 | Bot et al.22 | Lassen et al.23 | Ding et al.26 | Descatha et al.27 | |
| Analysis | Multiple logistic regression | Multiple linear regression | Multiple linear regression | Multiple logistic regression | Multivariable Cox regression | Multivariable Cox regression |
| Follow-up duration | 10–15 months | 8 weeks; 6 months | 3 months; 12 months | 1 year | 5 years | 3 years |
| Selection procedure for multivariable model | Forward likelihood-ratio method | p ⩽ 0.50 required for entry of variable into model | p < 0.2 (forced into model: age, sex, baseline pain and disability, duration) | p ⩽ 0.25 required for entry of variable into model | None | None |
| Then, manual backward selection, retaining factors p < 0.10 (Wald) | ||||||
| Covariate | ||||||
| Female | Not stated | ✓ | ✓ | ✓ | ✓ | |
| Higher age | Not stated | ✓ | ✓ | ✓ | ✓ | ✓ |
| Longer duration | ✓ | ✓ | ||||
| More severe baseline pain | ✓ | ✓ | ✓ | |||
| Multiple MSK complaints | ✓ | ✓ | ||||
| Low level of social support | ✓ | ✓ | ||||
| Previous history | Not stated | ✓ | ✓ | |||
Pain
Twenty prognostic factors were significantly associated with poor pain outcome. Only three were reported by more than one study: being female, longer duration and multi-site pain. Being female was a significant predictor of poor pain outcome at 8 weeks for conservatively managed lateral epicondylitis, but not at 6 months.20,21 Being female was also a significant predictor of poor pain outcome of elbow complaints in primary care at 3 months, but not at 1 year.22 In contrast, being female was a significant predictor of persistent elbow pain in the workplace at 1 year (odds ratio (OR) = 2.52, 95% CI = 1.30–4.91, n = 289).23 Longer duration of the complaint at initial presentation was a significant predictor of poor pain outcome in two clinical studies,22,25 and reporting pain in multiple regions was a significant predictor of poor pain outcome in two studies.22,23 Greater severity of baseline pain predicted a contradictory pain outcome in two clinical studies; poor prognosis for lateral epicondylitis at 8 weeks20 and elbow complaint improvement at 3 months and 1 year22 (Table 5).
Table 5.
Prognostic factors of distal upper limb pain: pain outcomes.
| Idiopathic carpal tunnel syndrome (CTS) |
Lateral epicondylitis |
Elbow complaints |
Distal upper limb, elbow, forearm and wrist-hand pain |
|
|---|---|---|---|---|
| Padua et al.25 | Waugh et al.20,21 | Bot et al.22 | Lassen et al.23 | |
| Female | – | Negative prognostic factor | Negative prognostic factor | Negative prognostic factor |
| 8 weeks: b = 9.28 (0.13 – 18.43), p = 0.04 | 3 months: b = −0.94 (−1.57 – −0.31), p = 0.00 | Elbow pain, 1 year: Odds ratio (OR) = 2.52 (1.30–4.91) | ||
| Longer duration | Negative prognostic factor | – | Negative prognostic factor | – |
| OR for improvement at 10–15 month follow-up Hands: OR = 0.84 (0.71–0.99) p = 0.05 Patients: OR = 0.80 (0.63–1.02) p = 0.053 | >6 months duration 3 months: b = −2.19 (−3.70 – −0.68) p = 0.00 | |||
| 12 months: b = −2.36 (−4.14 – −0.59) p = 0.00 | ||||
| Greater severity | – | Negative prognostic factor | Positive prognostic factor | – |
| 8 weeks: b = 0.19 (0.01 – 0.27) p = 0.05 | 3 months: b = 0.56 (0.42 – 0.71) p = 0.00 | |||
| 12 months: b = 0.62 (0.45 – 0.79) p = 0.00 | ||||
| Multiple MSK complaints | – | – | Negative prognostic factor | Negative prognostic factor |
| 3 months: b = −0.98 (−1.83 – −0.12) p = 0.03 | 1–2 other regions Forearm: OR = 17.1 (2.72 – 334) Distal upper limb: OR = 3.43 (1.27–10.3) | |||
| 12 months: b = −1.23 (−2.14 – −0.31) p = 0.01 | 3–4 other regions Forearm: OR = 13.7 (2.32–262) Distal upper limb: OR = 4.63 (1.75–13.7) | |||
| >5 other regions Forearm: OR = 21.7 (3.47–425) Distal upper limb: OR = 6.13 (2.21–18.9) |
Seventeen factors were significant predictors of poor pain outcome in one study only. Higher age predicted persistent elbow complaints at 3 months, but not 1 year22 and was not a significant predictor in four other studies.20,23,26,27 Nerve symptoms predicted poor pain outcome associated with lateral epicondylitis at 8 weeks but not 6 months.20,21 A positive Phalen test for CTS was a significant predictor of poor pain outcome at 10–15 months.25 Medium and low levels of social support predicted persistent elbow complaints at 3 months in a primary care setting.22 However, low level of social support was not a significant predictor of persistent pain related to CTS in an occupational context.27 Having a history of the complaint predicted persistent elbow complaints at 1 year,22 but not pain associated with lateral epicondylitis at 6 months.21 Using worrying and retreating as coping strategies and having a tendency to self-massage the hands predicted persistent elbow complaints at 1 year. Retreating as a coping strategy predicted poor outcome at 3 months in the same study.22 In pathology-specific studies, confirmed CTS predicted pain at 3 years27 and radiographic evidence of osteoarthritis (OA) predicted finger joint pain at 5 years.26 Single-study findings for occupational factors included having an unadjusted desk, forearm/wrist support during mouse use, high time pressure at work (forearm, wrist/hand and distal upper limb pain respectively at 1 year23) and having a repetitive job, defined as performing the same task ⩾25 hours/week (pain associated with lateral epicondylitis at 6 months21). Type A behaviour predicted poor outcome of wrist/hand and distal upper limb pain at 1 year.23 Having the complaint on the dominant side and reporting more fear avoidance were significant predictors of elbow complaint improvement at 3 months but not 1 year.22
Disability
Thirteen factors were significantly associated with poor functional outcome. However, the only factor identified more than once was female gender. It predicted persistent hand disability at 3 years in an occupational setting27 and poor functional outcome for conservative management of lateral epicondylitis at 8 weeks.20 In the latter study, being female was no longer a significant predictor at 6 months. A greater level of disability at baseline predicted contradictory clinical outcomes in two different studies, indicating poor prognosis for lateral epicondylitis at 8 weeks and 6 months20,21 and positive outcome for elbow complaints at 3 months and 1 year22 (Table 6).
Table 6.
Prognostic factors of distal upper limb pain: disability outcomes.
| Lateral epicondylitis |
Elbow complaints |
Carpal Tunnel Syndrome and hand pain |
|
|---|---|---|---|
| Waugh et al.20,21 | Bot et al.22 | Descatha et al.27 | |
| Female | Negative prognostic factor | – | Negative prognostic factor |
| 8 weeks: b = 10.62 (5.02–16.22) p < 0.01 | Odds ratio = 2.51 (1.07–5.92) | ||
| 6 months: b = 0.8 (−4.4–6.0) p = 0.75 | |||
| Greater disability | Negative prognostic factor | Positive prognostic factor | – |
| 8 weeks: b = 0.62 (0.44–0.80) p<0.01 | 3 months: b = 0.58 (0.45–0.72) p = 0.00 | ||
| 6 months: b = 0.5 (0.3–0.6) p < 0.01 | 12 months: b = 0.71 (0.54–0.87) p = 0.00 |
Twelve factors predicted poor functional outcome in one study only. Being unemployed, having children in the household, more severe pain at baseline and less social support predicted poor functional outcome related to elbow complaints at 3 months but not 1 year.22 In the same study, longer duration of the complaint, multiple musculoskeletal complaints and using retreating as a coping strategy predicted poor functional outcome at both 3 months and 1 year. Predictors of poor functional outcome significant at 1 year only in this study were having a previous history of the complaint and worrying more. In a study of lateral epicondylitis, nerve symptoms predicted poor functional outcome at 8 weeks but not 6 months.20,21 In the same study, having a repetitive job predicted poor functional outcome at 6 months but not 8 weeks. Descatha et al.27 reported that electrophysiologically confirmed CTS was a predictor of poor functional outcome of hand pain associated with CTS at 3 years. Presuming the cause of the complaint was an accident was the only predictor of improved functional outcome (elbow complaints at 3 months).22
Discussion
The aim of this review was to identify significant predictors of distal upper limb pain outcomes that have been identified by more than one study. For completeness, we have also described instances where a factor was a significant predictor in one study and not confirmed in other studies or only investigated once. In accordance with our aim, results that have been replicated have been given more weight in our interpretation of the literature. We found that 16 prognostic factors for distal upper limb pain have been examined in two or more studies and only 6 have been investigated by three or more studies, namely age, sex, BMI, severity and duration of pain at baseline and multi-site musculoskeletal pain. Given inconsistent results across identified studies in this review, there is therefore insufficient evidence to enable prediction of distal upper limb pain outcomes from presenting characteristics. Being female was the only consistently significant predictor of poor pain and functional outcome. This limited finding is most likely due to a particular lack of investigation of prognostic factors for functional outcomes. Of 23 putative prognostic markers of poor functional outcome identified as being explored in the literature, the majority (17) were investigated only once. A focus on functional outcomes in future studies will assist corroborative identification of potentially modifiable predictors of pain-related disability.
Our findings suggest that, during an episode of conservative care, immediate improvements in female patients may not be observed, but improvement within a year is likely. However, within occupational contexts, being female predicted persistent elbow pain at 1 year23 and hand disability at 3 years.27 Having multiple musculoskeletal complaints and a longer duration of the complaint also predicted poor long-term pain outcome. Previous research not restricted to the distal upper limb has identified greater severity of pain and disability at baseline as predictive of poor outcome.11,16,28–30 Yet, this current review found contradictory evidence. Waugh et al.20,21 identified greater baseline severity as indicative of poor outcome, in opposition to the findings of Bot et al.22 The latter authors measured change in pain/disability; individuals with greater baseline severity had more scope for reduction, even though, when compared to those with low baseline scores, they may have a poorer prognosis. A reduction of one point on the 11-point NRS used by these authors represents the minimum clinically important change.22,31,32 Consequently, having a higher score at baseline could result in clinically important change and a statistically improved outcome. However, final pain score should be considered to inform prognostic interpretation.
Both specific and non-specific pain-related conditions of the distal upper limb are included in this review. The heterogeneity of pathologies and difference in study populations may support arguments against collating prognostic evidence for pain anywhere in the distal upper limb. However, given the wider literature that suggests common prognostic factors for chronic pain, regardless of anatomical location,33,34 or factors predictive of persistent pain in the whole upper limb,35,36 our approach (elbow, forearm and hand only) is composite yet conservative. The review criteria included a range of symptom severities and healthcare-seeking behaviours. This included observational studies in occupational contexts where information about treatment or management was either not collected or analysed, and clinical studies where an expectant policy may have been undertaken (comparable to natural history). This diversity meant that factors investigated were often specific to particular settings. While the predictive significance of diagnostically confirmed CTS,25 or radiographic evidence of OA26 may be important, these findings are only generalisable to similar patient groups. Such factors were only investigated in one study and therefore did not reach the threshold to be included in the review synthesis. However, factors not pathology-specific and investigated only once also significantly predicted poor outcome. These included psychosocial and occupational factors, both identified as important predictors of chronic pain in other regi-ons.11,12,14,35–37 This review reveals a paucity of evidence for these potentially modifiable factors in distal upper limb pain prognosis. An earlier review of elbow complaints17 proposed psychosocial factors as putative predictors. The only study in this review that investigated generic elbow conditions22 considered such factors, finding negative coping strategies and fear avoidance beliefs as indicative of poor outcome. It is reasonable to suggest that persistence of pain in the distal upper limb outwith the elbow may also be affected by psychosocial and occupational factors.
The lack of evidence for prognostic factors for distal upper limb pain outcomes may be attributable to issues with statistical power. From the wider literature, Spreeuwers et al.36 indicated that limited cases of distal upper limb pain prevented separate analysis, and Punnett et al.38 described the necessity of combining different sites to reach required power. Three articles in this review22,23,27 used data from large observational studies, increasing the likelihood of including individuals with persistent distal upper limb pain or disability, thereby increasing predictive power. This limitation may be overcome through purposeful recruitment or adoption of agreed protocols, facilitating data pooling for future systematic reviews and meta-analyses.
Smidt et al.39 and Bisset et al.10 have both published secondary analyses of RCTs, pooling data to investigate conservatively treated epicondylitis, both excluded from this review due to the systematic nature of interventions. However, their results corroborate some of our findings. Smidt et al.39 reported that greater pain severity, longer duration and concomitant shoulder pain predicted poor outcome at 1 month, with greater pain severity and longer duration remaining significant at 6 months; greater pain severity, longer duration and concomitant neck pain were predictive of poor outcome at 1 year. Sex, however, was not a strong predictor of outcome. In Bisset et al.,10 greater severity of pain predicted poor outcome at 6 weeks and being employed predicted improvement at 1 year. Workplace and psychosocial factors were not investigated in the trials that supplied data for these secondary analyses. However, Haahr and Andersen’s9 RCT of occupational factors and epicondylitis, excluded from this review due to the systematic intervention, found that after adjustment for the intervention, high physical strain at work (OR = 2.3, CI = 1.1–1.5) and dominant-side complaint (OR = 3.1, CI = 1.4–6.8) significantly predicted high pain score at 1 year. If included in this review, the latter finding would contradict some of the findings of Bot et al.22 Acknowledging Haahr and Anderson’s report, Bot et al. propose differences in study population and study duration as possible explanations.
This report reveals a gap in the literature while providing some evidence for predictors of poor outcome and suggesting future areas of the study. Some authors have proposed that location of musculoskeletal pain is less important than other factors in determining persistence.33,34 This review reveals further research is required to identify prognostic factors for distal upper limb pain to support or refute such arguments. A limitation of this review is the reductive identification of prognostic factors, based on reaching significance in multivariable models. This prevented consideration of trends and may have introduced uncertainty with regard to factors found to have no association to outcome. Another potential limitation may come from excluding studies with active/pending legal compensation claims. This criterion was informed by evidence that suggests litigation has a negative impact on outcome.40,41 However, on repeating the search to identify articles that had been excluded for this reason, no additional studies met all other criteria for inclusion in this review. Finally, there remains the possibility of publication bias. Rather than selective dissemination of results, it seems more likely that research focused on distal upper limb pain has either not been undertaken, or sub-analyses have not been completed due to inadequate sample size needed to reach necessary power.
Conclusion
A range of prognostic factors for distal upper limb pain outcomes have been investigated. However, there is a lack of consistency of factors examined and results obtained. Female gender, longer duration of pain and multiple pain locations have been found to be repeatedly associated with poor distal upper limb pain or disability outcomes. Further research is required to corroborate existing findings and identify modifiable predictors of poor outcome. This would enable clinicians to provide better advice to patients about likely prognosis and could inform the development of targeted management strategies and public and occupational health initiatives.
Acknowledgments
Mel Bickerton, Information Consultant at the University of Aberdeen, provided assistance with the development of the search strategy.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: D.W. was funded by a University of Aberdeen Institute of Applied Health Sciences PhD studentship.
References
- 1. Palmer KT, Calnan M, Wainwright D, et al. Upper limb pain in primary care: health beliefs, somatic distress, consulting and patient satisfaction. Fam Pract 2006; 23(6): 609–617. [DOI] [PubMed] [Google Scholar]
- 2. Palmer KT, Calnan M, Wainwright D, et al. Disabling musculoskeletal pain and its relation to somatization: a community-based postal survey. Occup Med 2005; 55(8): 612–617. [DOI] [PubMed] [Google Scholar]
- 3. Health and Safety Executive. Self-reported work-related illness and workplace injuries in 2008/09: results from the Labour Force Survey, http://www.hse.gov.uk/statistics/lfs/lfs0809.pdf (2011, accessed 5 July 2014).
- 4. Ryall C, Coggon D, Peveler R, et al. A prospective cohort study of arm pain in primary care and physiotherapy – prognostic determinants. Rheumatology 2007; 46(3): 508–515. [DOI] [PubMed] [Google Scholar]
- 5. Macfarlane GJ, Hunt IM, Silman AJ. Role of mechanical and psychosocial factors in the onset of forearm pain: prospective population based study. BMJ 2000; 321(7262): 676–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kryger AI, Andersen JH, Lassen CF, et al. Does computer use pose an occupational hazard for forearm pain; from the NUDATA study. Occup Environ Med 2003; 60(11): e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bisset L, Beller E, Jull G, et al. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ 2006; 333(7575): 939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smidt N, van der Windt DA, Assendelft WJ, et al. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002; 359(9307): 657–662. [DOI] [PubMed] [Google Scholar]
- 9. Haahr JP, Andersen JH. Prognostic factors in lateral epicondylitis: a randomized trial with one-year follow-up in 266 new cases treated with minimal occupational intervention or the usual approach in general practice. Rheumatology 2003; 42(10): 1216–1225. [DOI] [PubMed] [Google Scholar]
- 10. Bisset L, Smidt N, Van der Windt DA, et al. Conservative treatments for tennis elbow do subgroups of patients respond differently? Rheumatology 2007; 46(10): 1601–1605. [DOI] [PubMed] [Google Scholar]
- 11. Kuijpers T, Van Der Windt DAWM, Van Der Heijden GJMG, et al. Systematic review of prognostic cohort studies on shoulder disorders. Pain 2004; 109(3): 420–431. [DOI] [PubMed] [Google Scholar]
- 12. Van Eijsden-Besseling MD, van den Bergh KA, Staal JB, et al. The influence of work and treatment related factors on clinical status and disability in patients with non-specific work-related upper limb disorders. Work 2010; 37(4): 425–432. [DOI] [PubMed] [Google Scholar]
- 13. Van Eijsden-Besseling MD, van den Bergh KA, Staal JB, et al. The course of nonspecific work-related upper limb disorders and the influence of demographic factors, psychologic factors, and physical fitness on clinical status and disability. Arch Phys Med Rehabil 2010; 91(6): 862–867. [DOI] [PubMed] [Google Scholar]
- 14. Palmer KT, Reading I, Linaker C, et al. Population-based cohort study of incident and persistent arm pain: role of mental health, self-rated health and health beliefs. Pain 2008; 136(1–2): 30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cole DC, Hudak PL. Prognosis of nonspecific work-related musculoskeletal disorders of the neck and upper extremity. Am J Ind Med 1996; 29(6): 657–668. [DOI] [PubMed] [Google Scholar]
- 16. Estlander A, Takala EDM, ViikariJuntura EDM. Do psychological factors predict changes in musculoskeletal pain? A prospective, two-year follow-up study of a working population. J Occup Environ Med 1998; 40(5): 445–453. [DOI] [PubMed] [Google Scholar]
- 17. Hudak PL, Cole DC, Haines AT. Understanding prognosis to improve rehabilitation: the example of lateral elbow pain. Arch Phys Med Rehabil 1996; 77(6): 586–593. [DOI] [PubMed] [Google Scholar]
- 18. Nicholls EE, van der Windt DA, Jordan JL, et al. Factors associated with the severity and progression of self-reported hand pain and functional difficulty in community-dwelling older adults: a systematic review. Musculoskeletal Care 2012; 10(1): 51–62. [DOI] [PubMed] [Google Scholar]
- 19. Moher D, Liberati ADH, Tetzlaff JBS, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151(4): 264–269. [DOI] [PubMed] [Google Scholar]
- 20. Waugh EJ, Jaglal SB, Davis AM, et al. Factors associated with prognosis of lateral epicondylitis after 8 weeks of physical therapy. Arch Phys Med Rehabil 2004; 85(2): 308–318. [DOI] [PubMed] [Google Scholar]
- 21. Waugh EJ, Jaglal SB, Davis, et al. Computer use associated with poor long-term prognosis of conservatively managed lateral epicondylalgia. J Orthop Sports Phys Ther 2004; 34(12): 770–780. [DOI] [PubMed] [Google Scholar]
- 22. Bot SD, van der Waal JM, Terwee CB, et al. Course and prognosis of elbow complaints: a cohort study in general practice. Ann Rheum Dis 2005; 64(9): 1331–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lassen CF, Mikkelsen S, Kryger AI, et al. Risk factors for persistent elbow, forearm and hand pain among computer workers. Scand J Work Environ Health 2005; 31(2): 122–131. [DOI] [PubMed] [Google Scholar]
- 24. Hayden JADC, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med 2013; 158(4): 280–286. [DOI] [PubMed] [Google Scholar]
- 25. Padua L, Padua R, Aprile I, et al. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology 2001; 56(11): 1459–1466. [DOI] [PubMed] [Google Scholar]
- 26. Ding H, Solovieva S, Leino-Arjas P. Determinants of incident and persistent finger joint pain during a 5-year follow-up among female dentists and teachers. J Epidemiol Community 2011; 65: A262. [DOI] [PubMed] [Google Scholar]
- 27. Descatha A, Dale AM, Franzblau A, et al. Natural history and predictors of long-term pain and function among workers with hand symptoms. Arch Phys Med Rehabil 2013; 94(7): 1293–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Feuerstein M, Huang GD, Haufler AJ, et al. Development of a screen for predicting clinical outcomes in patients with work-related upper extremity disorders. J Occup Environ Med 2000; 42(7): 749–761. [DOI] [PubMed] [Google Scholar]
- 29. Karjalainen K, Malmivaara A, Mutanen P, et al. Outcome determinants of subacute low back pain. Spine 2003; 28(23): 2634–2640. [DOI] [PubMed] [Google Scholar]
- 30. Klenerman LC, Slade PD, Stanley IMFRCGP, et al. The prediction of chronicity in patients with an acute attack of low back pain in a general practice setting. Spine 1995; 20(Suppl. 4): 478–484. [DOI] [PubMed] [Google Scholar]
- 31. Cepeda MS, Africano JM, Polo R, et al. What decline in pain intensity is meaningful to patients with acute pain? Pain 2003; 105(1–2): 151–157. [DOI] [PubMed] [Google Scholar]
- 32. Salaffi F, Stancati A, Silvestri CA, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004; 8(4): 283–291. [DOI] [PubMed] [Google Scholar]
- 33. Henschke N, Ostelo RW, Terwee CB, et al. Identifying generic predictors of outcome in patients presenting to primary care with nonspinal musculoskeletal pain. Arthritis Care Res 2012; 64(8): 1217–1224. [DOI] [PubMed] [Google Scholar]
- 34. Mallen CD, Peat G, Thomas E, et al. Prognostic factors for musculoskeletal pain in primary care: a systematic review. Br J Gen Pract 2007; 57(541): 655–661. [PMC free article] [PubMed] [Google Scholar]
- 35. Feleus A, van Dalen T, Bierma-Zeinstra SM, et al. Kinesiophobia in patients with non-traumatic arm, neck and shoulder complaints: a prospective cohort study in general practice. BMC Musculoskelet Disord 2007; 8: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Spreeuwers D, de Boer AG, Verbeek JH, et al. Work-related upper extremity disorders: one-year follow-up in an occupational diseases registry. Int Arch Occup Environ Health 2011; 84(7): 789–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Palmer KT. Diagnosing soft tissue rheumatic disorders of the upper limb in epidemiological studies of vibration-exposed populations. Int Arch Occup Environ Health 2008; 81(5): 575–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Punnett L, Gold J, Katz JN, et al. Ergonomic stressors and upper extremity musculoskeletal disorders in automobile manufacturing: a one year follow up study. Occup Environ Med 2004; 61(8): 668–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Smidt N, Lewis M, Van Der Windt DA, et al. Lateral epicondylitis in general practice: course and prognostic indicators of outcome. J Rheumatol 2006; 33(10): 2053–2059. [PubMed] [Google Scholar]
- 40. Rasmussen C, Rechter L, Schmidt I, et al. The association of the involvement of financial compensation with the outcome of cervicobrachial pain that is treated conservatively. Rheumatology 2001; 40(5): 552–554. [DOI] [PubMed] [Google Scholar]
- 41. Landers MR, Cheung W, Miller D, et al. Workers’ compensation and litigation status influence the functional outcome of patients with neck pain. Clin J Pain 2007; 23(8): 676–682. [DOI] [PubMed] [Google Scholar]