Abstract
Aim:
This systematic review aimed to establish if cognitive behavioural therapy (CBT) can reduce the physical symptoms of chronic headache and migraines in adults.
Methods:
Evidence from searches of eight databases was systematically sought, appraised and synthesised. Screening of title and abstracts was conducted independently by two reviewers. Full papers were screened, data extracted and quality assessed by one reviewer and checked by a second. Data were synthesised narratively by intervention due to the heterogeneity of the studies. The inclusion criteria specified randomised controlled trials with CBT as an intervention in adults suffering from chronic headaches/migraines not associated with an underlying pathology/medication overuse. CBT was judged on the basis of authors describing the intervention as CBT. The diagnosis of the condition had to be clinician verified. Studies had to include a comparator and employ headache/migraine-specific outcomes such as patient-reported headache days.
Results:
Out of 1126 screened titles and abstracts and 20 assessed full papers, 10 studies met the inclusion criteria of the review. Some studies combined CBT with another intervention, as well as employing varying numbers of comparators. CBT was statistically significantly more effective in improving some headaches-related outcomes in CBT comparisons with waiting lists (three studies), in combination with relaxation compared with relaxation only (three studies) or antidepressant medication (one study), with no statistically significant differences in three studies.
Conclusions:
The findings of this review were mixed, with some studies providing evidence in support of the suggestion that people experiencing headaches or migraines can benefit from CBT, and that CBT can reduce the physical symptoms of headache and migraines. However, methodology inadequacies in the evidence base make it difficult to draw any meaningful conclusions or to make any recommendations.
Keywords: Headache, migraine, cognitive behavioural therapy, systematic review, randomised controlled trial
Headaches are thought to occur regularly in around 46% and migraine in 11% of the population, making it one of the most common neurological problems presented to general practitioners (GPs) and neurologists in the United Kingdom.1 A primary care-based study set in 18 general practices in the south Thames region of England (urban and rural areas) based on 141,100 patients (aged 18 to 75 years) interviewed people reporting problematic experiences of headache in order to establish healthcare use and the cost associated with the provision of services to people with headaches. Extrapolating to the UK population, the authors suggest the total annual cost of migraines and headaches in 2011 was around £4.8 billion (including lost employment), with around £956 million due to healthcare use.2 The authors propose that these figures may be underestimations, as most headaches are self-managed3 and so not reported to GPs. This is supported by other significant organisations4,5 and demonstrates the magnitude of the problem of headaches and migraines in society.
GPs may find the specific diagnosis of headache difficult,6 which may be partly because the aetiology of primary headaches is not well understood or because of a limited understanding of diagnostic classification systems.7 The UKs National Institute of Health and Care Excellence (NICE) published guidelines for the diagnosis and treatment of headaches in 2011 to aid practitioners diagnosis and treatment.7 The NICE guidelines recommend medication for the treatment of chronic headache and migraine and emphasise the prevention of medication overuse. While many headaches can be self-managed with simple analgesics, their efficacy tends to decrease with frequent use8 and overuse can lead to more headaches. Other limitations of pharmacological therapies include the high cost associated with on-going medication, contraindications and medication intolerance.9
While medication is the mainstay of treatment, psychological comorbidity is common in individuals with chronic headache or migraine,10 with a variety of functions such as sleep (fatigue-related problems) and activities such as exercise and emotional experience (stress-related problems) affected.8 In addition, it has been found that the anticipation of a headache can cause significant anxiety between episodes1 and that depression may be three times more common in individuals experiencing severe headaches or migraines than in headache-free individuals,5 although estimates may be unreliable.11 Some of the psychological comorbidity associated with headache or migraine in some individuals may be treatable through psychological interventions. While it is suggested that an effective psychological intervention based on cognitive behavioural principles could substantially improve quality of life for sufferers, the NICE clinical guidelines suggest that there are few data supporting these interventions in the management of chronic headache disorders.7 Interventions such as cognitive behavioural therapy (CBT) include a variety of techniques such as stress management, biofeedback and relaxation, and aim to bring about changes in emotions, cognitions (thoughts) and behaviours (actions), and may be useful through the devolvement of coping mechanisms and life style changes (e.g. diet, sleep). CBT has been found to reduce pain intensity in adults suffering with chronic pain, therefore changing the pain experience.12
CBT has been shown in systematic reviews to be effective in the treatment of chronic pain,12,13 however, these reviews specifically excluded headache suggesting that there are treatment differences13 or that there is a different emphasis in treatment12 and so the potential effectiveness of CBT in headache or migraine is unknown. Current UK national guidelines do not make recommendations on these therapy types due to the lack of evidence.7 Although pain is a biopsychosocial experience, for pragmatic reasons (see the ‘Methods’ section), this review focused only on physical symptoms of pain. The aim of this systematic review was to establish if CBT can reduce the physical symptoms of chronic headache and migraines. CBT may offer a long-term treatment solution for headaches and migraine, and may also eliminate some of the side-effects and costs of medication, as well as other associated health service and personal costs.
Methods
A literature search was conducted using eight electronic databases (AHMED, CINAHL, Embase, Ovid Medline, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations, PsychINFO, the Cochrane library and Web of Science). Databases were searched from 1980 (cognitive and behavioural techniques did not emerge until the 1980s14) to January 2013. Searches were restricted to English language. Biographies of included publications and reviews were hand-searched to identify any potential further studies. For the full search strategy, see Supplementary table.
In order to be included in the review, studies had to be randomised controlled trials (RCTs). Abstracts or conference presentations were only included if they presented sufficient details to allow an appraisal of the methodology and assessment of the results. Studies had to include CBT as an intervention in an adult population suffering from headaches or migraines not associated with an underlying pathology or due to medication overuse, provide headache/migraine inclusion criterion or classification and state the frequency and duration of the condition or describe the condition as chronic, and the headache/migraine diagnosis had to be clinician verified. CBT was judged on the basis of authors describing the intervention as CBT. Studies describing the intervention as cognitive therapy (CT) due to the age of the publication were included if the intervention included a cognitive (e.g. re-conceptualisation) and a behavioural (e.g. skills acquisition or skills consolidation) element. Studies had to include a comparator (any), and headache-specific outcomes (patient-reported headache days, headache-specific quality of life, migraine disability assessment, headache/migraine frequency or intensity, functional status and resource use). In scoping searches for this review, we identified that there was no consensus in the measurement tools employed to measure psychological aspects of the pain experience. To aid interpretation of the results of these studies, we therefore focussed our review on physical reported outcomes of pain only, although we acknowledge that pain is not a purely physical experience. Author-designed participant-reported outcomes were also not included in the review, since the validity and clinical interpretation of some of these measures are unreliable.
Title and abstract screening was conducted by two reviewers independently using the above criteria. Inclusion criteria to full papers were applied, data extracted and study quality assessed by one reviewer and checked by a second. Methodological and study quality were assessed based on criteria published for systematic reviews by the Centre for Reviews and Dissemination (CRD).15 Disagreements were resolved through discussion between the reviewers or if necessary through arbitration by a third reviewer. Experts in CBT were consulted for input into the review.
Studies were synthesised narratively with tabulation of results of all included studies. The RCTs were heterogeneous in their interventions and comparators; meta-analysis was therefore not appropriate.
Results
A total of 1126 titles and abstracts were screened and 1106 references excluded at title and abstract stage. We retrieved 20 full papers, excluded nine papers for various reasons (see Figure 1) and included 10 studies based on 11 publications in the review.
Figure 1.
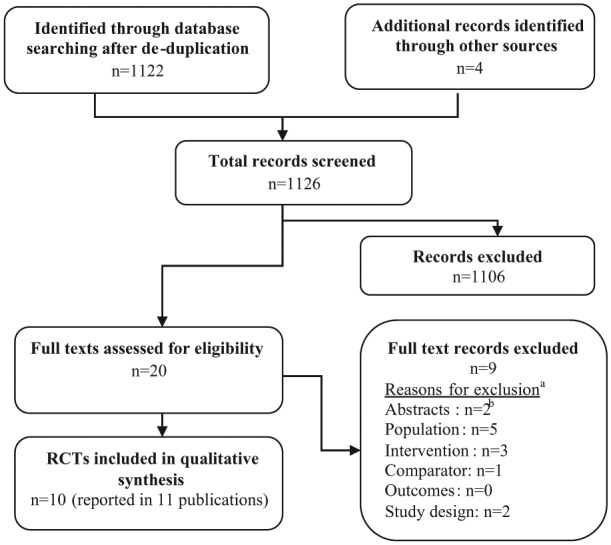
Flow chart for the identification of studies.
aPapers could be excluded for more than one reason, only the main reason is stated.
bExcluded due to insufficient information.
Of the 10 included studies, six employed mixed interventions (see Table 1), of which four studies combined some form of CBT with relaxation (Blanchard et al.,16 Holroyd et al.,17 Mosley et al.,18 Tobin et al.19), one with biofeedback (Blanchard et al.20) and the remaining study with placebo (Holroyd et al.21,22). In addition, one study allowed additional physical treatments such as pain medication, nerve blocks, acupuncture, massage and physical therapy for both the CBT and the wailing list control group (Basler et al.23). Two of the studies evaluated clinic-based CBT with self-managed CBT (Martin et al.,24 Richardson and McGrath25). For ease of comparison, all interventions are abbreviated CBT and for simplicity the two types of biofeedback (temporal pulse amplitude biofeedback training and thermal biofeedback) are referred to as just biofeedback. For details of the interventions and comparators employed in the studies, see Table 1.
Table 1.
Main characteristics of included studies.
| Author, country, (sample size); F-up; Mean age; Headache diagnosis; Mean years of pain | Intervention/interventions (sample size); duration | Comparator/s (sample size) |
|---|---|---|
| Basler et al.,23 Germany (n = 126); F-up: 6 months. Mean age: 40.0 years (SD = 11.4). Headache diagnosis: 26% migraine, 36% tension headache, 37% both. Mean years of pain: 14.2 (SD = 11.0). |
CBT (+ physical treatments such as pain medication, nerve blocks, acupuncture, massage and physical therapy) (n = 50); Treatment duration: 12 weeks (12 sessions, 5–8 patients per group) |
1. Waiting list control (+ physical treatments such as pain medication, nerve blocks, acupuncture, massage and physical therapy) (n = 38) |
| Blanchard et al.,16 USA (n = 77); F-up: 12 weeks. Mean age: 38.6 years (range = 21–67). Headache diagnosis: tension headache. Mean years of pain: 14.1 (SD = 10.6–14.1). |
CBT (cognitive therapy) + relaxation (progressive muscle relaxation) (n = 17); Treatment duration: 8 weeks (11 sessions, not reported but suggests individual sessions) |
1. Relaxation (progressive muscle relaxation) (n = 19) 2. Placebo (pseudo-medication) (n = 16) 3. Waiting list control (headache monitoring) (n = 15) |
| Blanchard et al.,20 USA (n = 148); F-up: 12 weeks. Mean age: 38.6 years (range = 21–61). Headache diagnosis: 64% migraine or mixed migraine; 36% tension headache. Mean years of pain: 15.6 (SD = 8.6–12.4). |
CBT (cognitive therapy) + biofeedback (thermal biofeedback) (n = 30); Treatment duration: 8 weeks (16 sessions, not reported but suggests individual sessions) |
1. Relaxation training + biofeedback (thermal biofeedback) (n = 32) 2. Placebo (pseudo-medication) (n = 24) 3. Waiting list control (headache monitoring) (n = 30) |
| Holroyd et al.,17 USA (n = 41); F-up: 12 weeks. Mean age: 32.3 years (range = 19–55). Headache diagnosis: recurrent tension headache. Mean years of pain: 10.7 (range = 1–28). |
CBT + relaxation (n = 19); Treatment duration: 8 weeks (3 sessions, individual) |
1. Antidepressant medication (amitriptyline) (n = 17) |
| Holroyd et al.,21,22 USA (n = 203); F-up:6 months. Mean age: 37 years (SD = 0.85). Headache diagnosis: chronic tension-type headache. Mean years of pain: 12.6 (SD = 0.79). |
CBT (stress management therapy) + placebo (n = 38); Treatment duration: 8 weeks (3 sessions, not reported but suggests individual sessions) |
1. CBT (stress management therapy) + antidepressant medicationa (n = 45) 2. Antidepressant medicationa (n = 48) 3. Placebo (n = 38) |
| Martin et al.,24 Australia (n = 64); F-up: 4 + 12 months. Mean age: 38.4 (SD: CBT 9.81, SM-CBT 8.41). Headache diagnosis: migraine CBT 50.0%/SM-CBT 37.9%; tension headache CBT 26.9%/ SM-CBT 41.4%; mixed CBT 23.1%/ SM-CBT 20.7%. Mean years of pain: 16.5 (SD: CBT 8.88, SM-CBT 11.71) |
Clinic-based CBT (n = 31); Treatment duration: 12 weeks (12 sessions, 4–6 patients per group) |
1. Self-managed CBT (n = 31) |
| Martin et al.,26 Australia (n = 64); F-up: 12 months. Mean age: 44.0 (SD = 9.6). Headache diagnosis: 59% migraine, 41% tension-type headache. Mean years of pain: 24.7 (SD = 11.7). |
CBT (n = 20); Treatment duration: 8 weeks (8 sessions, unclear if individual or group treatment) |
1. Biofeedback (temporal pulse amplitude biofeedback training. (n = 19) 2. Waiting list control (n = 12) |
| Mosley et al.,18 USA (n = 37); F-up: 12 weeks + 4 months. Mean age: 68 years (range = 60–78). Headache diagnosis: recurrent tension headache. Mean years of pain: 37 (range = 9–55). |
CBT + relaxation (n = 11); Treatment duration: 12 weeks (12 sessions, group treatment – number of patients per group not reported) |
1. Relaxation (n = 10) 2. Waiting list control (n = 9) |
| Richardson and McGrath,25 Canada (n = 51); F-up:6 months. Mean age: 35.6 (range = 23–48). Headache diagnosis: common migraine (not classic migraine). Mean years of pain: 16.7 (range = 2–40). |
Clinic-based CBT (n = 15) Treatment duration: 8 weeks (8 sessions, unclear if individual or group treatment) |
1. Self-managed CBT (n = 15) 2. Waiting list control (n = 17) |
| Tobin et al.,19 USA (n = 27); F-up: 3 months. Mean age: 28 (SD = 6.6). Headache diagnosis: recurrent tension headache. Mean years of pain: 8 (SD = 5.7). |
CBT + relaxation (n = 12); Treatment duration: 8 weeks (3 sessions, unclear if individual or group treatment) |
1. Relaxation (n = 12) |
CBT: cognitive behavioural therapy; SD: standard deviation; F-up: follow-up.
Some studies had more than one follow-up point. The results for the follow-up point with the most complete data are reported. For detailed data extraction forms, please contact the corresponding author.
Amitriptyline or nortriptyline.
Four of the studies had one comparator (Basler et al.,23 Holroyd et al.,17 Martin et al.,24 Tobin et al.19), three had two comparators (Martin et al.,26 Mosley et al.,18 Richardson and McGrath25) and the remaining three studies had four comparators (Blanchard et al.,16 Blanchard et al.,20 Holroyd et al.21,22). Other active treatment comparators included relaxation in three studies (Blanchard et al.,16 Mosley et al.,18 Tobin et al.19), and one study each of combined relaxation with biofeedback (Blanchard et al.20), combined CBT with antidepressants (Holroyd et al.21,22), antidepressants (Holroyd et al.17) and biofeedback (Martin et al.26). Relaxation and biofeedback could therefore be part of the intervention or a comparator, making comparison between studies difficult. Five studies included non-treatment comparators such as a waiting list control group (Blanchard et al.,16 Blanchard et al.,20 Martin et al.,26 Mosley et al.,18 Richardson and McGrath25) and three studies a placebo group (Blanchard et al.,16 Blanchard et al.,20 Holroyd et al.21,22). The most complete results were reported for 3 months post-treatment in three studies21,23,25 and 6 months in seven studies.16–20,24,26
Quality assessment
Overall, the assessment of study quality suggests that results of the included RCTs should be interpreted with caution as there is some evidence of potential risk of bias. Study quality varied between studies. In eight out of the 10 categories, one or more of the studies provided insufficient information to allow for a conclusion about the potential risk of bias to be reached and only four categories included studies that seemed to have methods that would minimise potential bias adequately (see Table 2). Selection bias is unknown or likely in all of these studies.
Table 2.
Quality assessment of included studies.
| Authors | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bias | Basler et al.23 | Blanchard et al.16 | Blanchard et al.20 | Holroyd et al.17 | Holroyd et al.21 | Martin et al.24 | Martin et al.26 | Mosley et al.18 | Richardson and McGrath.25 | Tobin et al.19 |
| Random sequence generation? | U | I | U | I | U | U | U | I | U | I |
| Allocation concealment? | U | U | U | U | U | U | U | U | U | U |
| Groups similar at the outset? | A | I | A | A | A | A | A | A | A | A |
| Performance bias: blinding of car providers? | U | U | U | U | P | U | U | U | U | U |
| Performance bias: blinding of participants? | U | U | U | U | P | U | U | U | U | U |
| Detection bias: blinding of outcome assessors? | U | U | U | U | U | U | U | U | U | U |
| Unexpected imbalances in drop-outs between groups? | A | A | I | A | I | I | A | I | I | A |
| Free of selective reporting? | U | U | I | U | U | I | U | U | U | U |
| ITT analysis? | I | I | I | I | A | I | I | I | I | U |
| Did the analysis account for missing data? | U | I | I | P | A | I | I | I | I | U |
A: adequate; I: inadequate; P: partial; U: unknown/unclear.
For ease of comparison, the outcome data of the studies are grouped by their main comparator. Some studies had more than one follow-up point and the results for the follow-up point reporting the most comprehensive data are reported. Due to minimal reporting of adverse events (tricyclic antidepressants) limited to two studies, data have been omitted from this article.17,21
CBT versus waiting list control
This comparison was reported by three studies.23,25,26 At follow-up in the study by Basler et al.,23 the waiting list control group had also received CBT and data were amalgamated; hence, post-treatment and not follow-up data (4 weeks) are reported here. Martin et al.26 reported results for more than one follow-up point and the latest follow-up point of 12 months is reported (see Supplementary table). The study by Richardson and McGrath25 only reported results for subgroups of ‘more severe’ and ‘less severe’ resulting in very small participant numbers at 8 weeks post-treatment, and it is unclear if the study was powered for this type of comparison. Other comparator treatments included in two of the studies (biofeedback26 and self-management CBT25) are discussed below.
CBT was statistically significantly more effective compared to a waiting list in reducing headache intensity in one (post-hoc comparison)25 out of two studies,23,25 in reducing headache frequency25 and headache-free days,23 each reported by one study (see Table 3). CBT was statistically significantly less effective in the reduction of headache intensity (one study23), headache activity (one study26), responder rate (two studies25,26) and in pain medication (one study23) when compared to a waiting list group – although only one of the three studies reported a statistical comparison for pain medication. However, results must be treated with caution as there were issues around the risk of bias in all three trials, drop-outs were excluded from the results in all three trials, there was a failure to report p values in a number of instances and two studies had very low participant numbers25,26
Table 3.
CBT versus waiting list control.
| Outcome, study | Results, n (SD); p value |
|---|---|
| Headache intensity | |
| Basler et al.23 | CBT 3.52 (1.56), WL 3.66 (1.35); nsa |
| Richardson and McGrath25 | More severe: CBT 3.49 (0.63), WL 4.09 (0.61)a |
| Less severe: CBT 2.75 (1.23), WL 3.16 (0.37)a | |
| Headache activity | |
| Martin et al.26 | CBT 0.207 (0.225), WL 0.434 (0.737); p = 0.057b |
| Headache frequency | |
| Richardson and McGrath25 | More severe: CBT 12.14 (4.95), WL 18.67 (8.65)a |
| Less severe: CBT 5.00 (3.38), WL 11.13 (8.46)a | |
| Headache-free days | |
| Basler et al.23 | CBT 3.00 (2.32), WL 3.07 (2.23); p < 0.05 |
| Responder rate | |
| Martin et al.26 | >50% reduction in headache rating, n (%): CBT 14 (77.8), WL 3 (23.1); nsa |
| >50% reduction medication use, n (%): CBT 11 (61.1), WL (36.4); nsa | |
| Richardson and McGrath25 | ⩾50% reduction in headache activity, n (%): CBT 7c (47), WL 3c (18); nsa |
| Medication used | |
| Basler et al.23 | CBT 1.06 (1.09), WL 1.77 (1.66)a |
SD: standard deviation; CBT: cognitive behavioural therapy. NS: not significant. WL: waiting list.
No p value reported.
Covariate adjusted post-treatment.
Calculated by reviewer.
CBT plus relaxation versus relaxation
Three RCTs compared CBT plus relaxation with relaxation only (Table 4).16,18,19 Apart from relaxation, Mosley et al.18 included a waiting list group as a second comparator, while Blanchard et al.16 included a waiting list and a placebo group as comparators (see Supplementary table). Both Blanchard et al.16 and Mosley et al.18 reported post-treatment data only. All three studies excluded drop-outs from the results.
Table 4.
CBT plus relaxation versus relaxation.
| Outcome | Results, n (SD); p value |
|---|---|
| Headache intensity | |
| Mosley et al.18 | CBT + RLX 3.73 (2.73), RLX 5.29 (3.51); p < 0.05 |
| Tobin et al.19 | CBT + RLX 2.91 (2.42), RLX 4.60 (2.89); p < 0.05 |
| Headache activity | |
| Blanchard et al.16 | CBT + RLX 3.20 (3.70), RLX 3.82 (2.59); p = 0.001 |
| Tobin et al.19 | CBT + RLX0.68 (0.95), RLX 3.10 (1.75); p < 0.05 |
| Headache-free days | |
| Tobin et al.19 | CBT + RLX 5.77 (2.07), RLX 3.59 (3.17); p < 0.05 |
| Responder rate | |
| Blanchard et al.16 | ⩾50% improvement, n (%): CBT + RLX 10 (62.5), RLX 6 (31.6); nsa |
| Mosley et al.18 | >50% improvement, n (%): CBT + RLX 7b (63.6), RLX 4b (40); nsa |
| Medication use | |
| Mosley et al.18 | CBT + RLX 2.18 (1.72), RLX 3.90 (4.43); p < 0.01 |
CBT: cognitive behavioural therapy. NS: not significant. RLX: relaxation.
No p values reported.
Calculated by reviewer.
Combined CBT plus relaxation was statistically significantly more effective in reducing headache intensity18,19 and headache activity16,19 compared to relaxation in the two studies reporting this outcome, in reducing headache frequency in one study reporting this outcome,19 and in one out of three studies in reducing medication use.18 The intervention did not have a statistically significantly better responder rate in the two studies reporting this outcome.16,18 It should be noted that in the study by Tobin et al.19 only four participants reported regularly taking prescribed medication and the variable was excluded from analysis, while the study by Blanchard et al.16 did not report a statistical comparison between the active treatment groups. Results must be treated with caution as all three studies excluded drop-outs from the results and had low participant numbers per treatment group.16,18,19
CBT plus relaxation versus antidepressants (amitriptyline)
One study reported a comparison of CBT plus relaxation with antidepressant medication.17 Holroyd et al.17 assessed headache-related outcomes at 12 weeks post-treatment. While authors stated that all statistical analyses were based on an intention to treat principle, the reported data excluded drop-outs.
CBT plus relaxation was statistically significantly more effective in reducing the mean level of headache pain when compared with amitriptyline, increasing headache-free days and had a better responder rate (statistically significantly more likely to be categorised as moderately or substantially improved), but this was not so in the reduction of medication use or headache peak (see Table 5). Caution in the interpretation of the results is required, and as the study had a small sample size (CBT plus relaxation n = 19, Medication n = 17), there were imbalances in headache medication use at baseline (amitriptyline group nearly double to that in the CBT plus relaxation group) and the study had a high drop-out rate (12%). This was nearly four times higher in amitriptyline group and may have been related to possible side-effects of the antidepressant medication.
Table 5.
CBT plus relaxation versus antidepressants (amitriptyline) – Holroyd et al.17
| Outcome | Results, n (SD); p value |
|---|---|
| Headache intensity | CBT + RLX 4.33 (2.35), AM 4.55 (1.98); nsa |
| Headache index | CBT + RLX 0.96 (0.65), AM 1.49 (1.11); p < 0.001 |
| Headache-free days | CBT + RLX 54.7 (27.5), AM 42.3 (32.9); p < 0.05 |
| Responder rate | Moderately (33–66% reduction) or substantially improved (>66% reduction), n (%) CBT + RLX17 (90), AM 9 (53); p < 0.05 |
| Medication use | CBT + RLX0.26 (0.52), AM 0.82 (1.17); nsa |
SD: standard deviation; AM: amitriptyline. CBT: cognitive behavioural therapy. NS: not significant. RLX: relaxation.
No p value reported.
CBT plus placebo versus CBT plus antidepressants (amitriptyline or nortriptyline)
The study by Holroyd et al.21 compared CBT plus placebo with CBT plus antidepressants, antidepressants alone or placebo (Table 6). While p values were reported, data were presented in graph format and means were estimated from the graphs by reviewers (see Supplementary table). The authors noted that the trial did not have enough power to detect small treatment effects.
Table 6.
| Outcome | Results, mean ratinga |
|---|---|
| Headache index | CBT + PL1.9, AD 1.65 |
| Days of least moderate pain | Pain rating mean ⩾5: CBT + PL 6.6, AD 6.6 |
| Responder rate | >50% reduction in headache index scores, n/N (%): CBT + PL17/49 (35), AD 34/53 (64); p = 0.006 |
| Medication index | CBT + PL 29, AD 23 |
AD: antidepressants. CBT: cognitive behavioural therapy. PL: placebo.
Data (mean rating) estimated from graph by reviewer.
While authors reported statistically significant differences for the CBT plus placebo group compared with placebo alone in headache activity and headache-free days, no statistical comparison of CBT plus placebo with CBT plus antidepressants was reported for these outcomes (see Supplementary table for other comparators). For the responder rate, CBT plus antidepressants was statistically superior to antidepressants alone (p = 0.006). The study had an overall drop-out rate of 29% at 6 months follow-up, which was highest in the placebo group (46%) followed by the CBT plus placebo (31%) and differences were statistically significant (p = 0.01).
CBT versus CBT self-management
Two studies compared clinic-based CBT with a self-managed form of CBT.24,25 The study by Martin et al.24 reported data at several time points, with 12-month follow-up data reported here. Richardson and McGrath25 had an additional waiting list control arm (reported above). As previously mentioned, the authors grouped the majority of their results into subgroups of ‘more severe’ and ‘less severe’, leading to very small sample sizes per subgroup.
There were no statistically significant differences between treatment arms for any of the outcomes (see Table 7). It is unclear if the study by Richardson and McGrath25 had enough power to detect differences in the very small reported subgroups as already stated. Authors attributed the lack of statistical difference in the responder rate to the small sample size and therefore low power. Authors also stated that medication use was only recorded for half of the participants (8–9 per treatment group) due to ‘an administrative error’ and warned that results must be treated with caution. Both studies excluded drop-outs from their reported results.
Table 7.
CBT versus CBT self-management.
| Outcome | Results, mean (SD) |
|---|---|
| Headache intensity | |
| Richardson and McGrath25 | More severe: CBT 3.03 (0.38), CBT-SM 3.47 (0.50); nsa |
| Less severe: CBT 3.13 (0.96), CBT-SM 2.95 (1.17); nsa | |
| Headache activity | |
| Martin et al.24 | CBT 0.31c,CBT-SM 0.37c, nsa |
| Headache-frequency | |
| Richardson and McGrath25 | More severe: CBT 11.86 (2.67), CBT-SM 14.33 (6.50); nsa |
| Less severe: CBT 5.86 (1.77), CBT-SM 5.25 (1.83); nsa | |
| Responder rate | |
| Richardson and McGrath25 | ⩾50% reduction in headache activity: CBT 7b (47), CBT-SM 5b (33); nsa |
| Pain medication index | |
| Richardson % McGrath25 | CBT 51.11 (77.56), CBT-SM 25.00 (35.53); nsa |
CBT: cognitive behavioural therapy. CBT-SM: cognitive behavioural therapy-self-managed. NS: not significant.
No p value reported.
Data estimated from graph by reviewer.
Calculated by reviewer.
CBT versus biofeedback
One study by Martin et al.26 reported a comparison between CBT and temporal pulse amplitude biofeedback, with the addition of a waiting list control group (reported above). The study had a small sample size (CBT n = 18, BF n = 19). Reported results excluded data for drop-outs, resulting in an even smaller sample size (CBT n = 10, BF n = 11) at 12 weeks follow-up (see Supplementary table). As previously stated, the authors reported results for more than one follow-up point and the latest follow-up point of 12 months is reported here.
There were no statistically significant differences between the treatment groups for headache activity (see Table 8). No statistical comparison for pain medication use or responder rate (headache ratings and pain medication) was reported. Authors state that there was no significant association between treatment condition and the presence of clinically significant change (p value not reported). Results should be interpreted with caution, as data for drop-outs were excluded and results were based on a small sample size.
Table 8.
CBT versus biofeedback – Martin et al.26
| Outcome | Results, mean (SD); p value |
|---|---|
| Headache activity | CBT 0.207 (0.225), BF 0.364 (0.506); p = 0.057a |
| Responder rate | >50% reduction in headache rating: CBT 14 (77.8), BF12 (63.2) >50% reduction medication use: CBT 11 (61.1), BF 11 (57.9) |
| Medication use (pill count) | CBT 1.26 (1.87), BF 1.05 (1.95) |
BF: biofeedback. CBT: cognitive behavioural therapy.
Covariate adjusted post-treatment.
CBT plus biofeedback versus relaxation plus biofeedback
One study assessed this comparison, with the additional of a placebo and a waiting list control group as comparators (see Supplementary table). Blanchard et al.20 reported statistical comparisons between the treatment groups through an analysis of variance. While authors reported data for more than one time point (no data reported for 12 months follow-up), the most complete results were for 12 weeks post-treatment (reported here).
There were no statistical comparisons between the active treatment groups. Visual inspection of the data would appear to show lower average daily headache activity (see Table 9), a greater responder rate and a lower pain medication index for the CBT plus biofeedback group at 12 weeks follow-up, but it is unclear if this is statistically significant. For medication use, authors stated that both biofeedback groups (as well as the placebo group, see Supplementary table) showed significant reductions in medication use at 12 weeks post-treatment, but adding CBT yielded no advantage. Drop-outs were excluded from the reported data.
Table 9.
CBT plus biofeedback versus BF plus relaxation – Blanchard et al.20
| Outcome | Results, mean (SD) |
|---|---|
| Headache activity | CBT + BF 1.90 (2.16), BF + RLX 2.05 (2.22) |
| Responder rate | ⩾50% improvement, n (%): CBT + BF 15 (50.0); BF + RLX 17 (53.1) |
| Pain medication index | CBT + BF 8.4 (13.6), BF + RLX 11.2 (21.9) |
BF + RLX: biofeedback plus relaxation. CBT + BF: cognitive behavioural therapy plus biofeedback.
Discussion
Headaches and migraines present an important health problem and while they are generally not life threatening, they are a cause of personal and social burden, with substantial economic impact.27 CBT could offer an effective treatment countering the burden and impact; however, making general recommendations on the basis of the findings of these included studies is difficult, as the evidence is limited by poor methodology.
Where CBT was compared with a waiting list control, results were mixed with some showing more effective results for those treated with CBT on some outcomes but not others. For CBT plus relaxation compared with relaxation alone, the findings of this review provide some support for CBT above and beyond common therapeutic factors. CBT plus relaxation was generally more effective than antidepressants alone. However, negative side effects of antidepressant medication may have confounded outcomes, reflecting the possibility that adverse side effects for some individuals counter any possible benefits in others. Similarly, where CBT plus placebo was compared with CBT plus antidepressants, CBT plus antidepressants was not statistically superior to CBT plus placebo in any of the outcomes. These findings provide no support for the addition of antidepressants to CBT. While no statistical comparisons were reported where CBT plus biofeedback was compared with relaxation plus biofeedback, when CBT alone was compared with biofeedback, statistical differences were not in support of CBT. These findings suggest that individuals can benefit from structured therapeutic interventions without CBT-specific ingredients. Lastly, where clinic-based CBT was compared with self-managed CBT, one treatment was not statistically more effective that the other and these findings suggest that individuals can benefit from structured psycho-therapeutic interventions even without the benefit of common therapeutic factors associated with therapist contact.
The findings of this review are in line with the NICE guidelines, in that there is limited evidence for the efficacy of CBT as a treatment for headaches/migraines, although the former was not based on the findings of a systematic review. Differences in treatment outcomes may be due to variations in the components of CBT employed in these studies or differences in the way the therapy was implemented. Often in studies of this type, newly qualified practitioners implement the therapeutic treatments. In addition, it has been found that maintenance of coping skills after completing CBT is variable, with individuals often experiencing a decline in therapeutic benefit within several weeks.28 Longer term follow-up would therefore be of interest because as with all chronic conditions, sickness-behaviours have become embedded over a long period of time. Individuals may therefore need longer to establish changes in order to benefit from the therapy. Some suggest that treatments like CBT were never intended to change enduring personality processes and that changes in personality processes and traits are difficult to achieve in short time periods.29 This may mean that in chronic conditions such as headaches and migraines longer periods of therapy are needed. Lastly, there was a lack of consensus in how the same or similar outcomes were measured in these studies, combined with a lack of statistical comparison to other active treatment comparators employed in the studies. A comparison of CBT with other active psychotherapies would allow exploration of the relative contributions made by therapeutic contact and CBT-based techniques.
This systematic review used standard rigorous methods for evidence synthesis and evidence for clinical effectiveness was systematically sought and appraised and synthesised. Experts in CBT have been consulted for input into the review. Quantitative pooling of outcomes across clinical effectiveness studies in a meta-analysis was not possible due to large differences in interventions and comparators, as well as differences in the way outcomes were presented. Results of the RCTs should be interpreted with caution as no high quality contemporary evidence was identified for CBT. Known methodological problems in this type of research include difficulties in blinding trials; the absence of standardisation and detailed description of patient groups, interventions, delivery of interventions and outcome measures; the inclusion of self-selected patients30 and the use of waiting list control groups.
Limitations of this review are the inclusion of some relatively old studies with a potential uncertain or high risk of bias, small number of participants and generally sub-optimal reporting. In addition, some studies conducted a large number of statistical tests regardless of their small sample size, without addressing the increased possibility of statistical error. Finally, we focused on non-psychological outcomes for pragmatic reasons because the nature of the patient-reported outcome measures was inconsistent across studies.
Conclusion
Overall, these findings were mixed, with some studies providing evidence in support of the suggestion that people experiencing headaches or migraines can benefit from CBT, and that CBT can reduce the physical symptoms of headache and migraines. However, all the results must be interpreted with caution due to the lack of statistical power and methodological limitations of the studies, as well as the large number of different interventions and comparators employed in these studies.
Suggested research priorities
It has been suggested that a study of a CBT for headache/migraine in primary care might be beneficial.2 The study should follow rigorous methods, employ standardised outcome measure with long-term follow-up, use an active comparator, with CBT based on step-wise treatment to enable the identification of the specific component/components that may be responsible for reducing any improvements in headaches/migraines symptoms.
Acknowledgments
We would like to thank Karen Welch (Information Specialist, SHTAC) for developing the search strategies and downloading the references.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. National Institute for Health and Care Excellence. Headaches in young people and adults (QS42), http://publications.nice.org.uk/headaches-in-young-people-and-adults-qs42#ftn.footnote_2 (2013, accessed 30 August 2013).
- 2. McCrone P, Seed PT, Dowson AJ, et al. Service use and costs for people with headache: a UK primary care study. J Headache Pain 2011; 12(6): 617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morrell DC, Wale CJ. Symptoms perceived and recorded by patients. J R Coll Gen Pract 1976; 26(167): 398–403. [PMC free article] [PubMed] [Google Scholar]
- 4. British Association for the Study of Headache (BASH). Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache and medication-overuse headache. 3rd ed Available at: http://www.bash.org.uk/wp-content/uploads/2012/07/10102-BASH-Guidelines-update-2_v5-1-indd.pdf (2010, accessed 3 September 2013).
- 5. World Health Organization. Headache disorders. WHO factsheet number 277, http://www.who.int/mediacentre/factsheets/fs277/en/ (2012, accessed 30 August 2013).
- 6. Watson DP. Easing the pain: challenges and opportunities in headache management. Br J Gen Pract 2008; 58(547): 77–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Institute for Health and Care Excellence. Headaches: diagnosis and management of headaches in young people and adults (CG150), http://publications.nice.org.uk/headaches-cg150 (2012, accessed 5 September 2013).
- 8. Bendtsen L. Drug and nondrug treatment in tension-type headache. Ther Adv Neurol Disord 2009; 2(3): 155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lemstra M, Stewart B, Olszynski WP. Effectiveness of multidisciplinary intervention in the treatment of migraine: a randomized clinical trial. Headache 2002; 42(9): 845–854. [DOI] [PubMed] [Google Scholar]
- 10. D’Amico D, Libro G, Prudenzano MP, et al. Stress and chronic headache. J Headache Pain 2000; 1(1): S49–S52. [Google Scholar]
- 11. Pincus T, Williams AC, Vogel S, et al. The development and testing of the depression, anxiety, and positive outlook scale (DAPOS). Pain 2004; 109(1–2): 181–188. [DOI] [PubMed] [Google Scholar]
- 12. Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 1999; 80(1–2): 1–13. [DOI] [PubMed] [Google Scholar]
- 13. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2013; 11: CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rachman S. Psychological treatment of anxiety: the evolution of behavior therapy and cognitive behavior therapy. Annu Rev Clin Psychol 2009; 5: 97–119. [DOI] [PubMed] [Google Scholar]
- 15. Centre for Reviews and Dissemination. Systematic reviews: CRD’s guidance for undertaking reviews in health care. 3rd ed. York: York Publishing Services Ltd., CRD, 2009. [Google Scholar]
- 16. Blanchard EB, Appelbaum KA, Radnitz CL, et al. Placebo-controlled evaluation of abbreviated progressive muscle-relaxation and of relaxation combined with cognitive therapy in the treatment of tension headache. J Consult Clin Psychol 1990; 58(2): 210–215. [DOI] [PubMed] [Google Scholar]
- 17. Holroyd KA, Nash JM, Pingel JD, et al. A comparison of pharmacological (amitriptyline HCL) and nonpharmacological (cognitive-behavioral) therapies for chronic tension headaches. J Consult Clin Psychol 1991; 59(3): 387–393. [DOI] [PubMed] [Google Scholar]
- 18. Mosley TH, Grothues CA, Meeks WM. Treatment of tension headache in the elderly: a controlled evaluation of relaxation training and relaxation training combined with cognitive-behavior therapy. J Clin Geropsychol 1995; 1(3): 175–188. [Google Scholar]
- 19. Tobin DL, Holroyd KA, Baker A, et al. Development and clinical trial of a minimal contact, cognitive-behavioral treatment of tension headache. Cogn Ther Res 1988; 12(4): 325–339. [Google Scholar]
- 20. Blanchard EB, Appelbaum KA, Radnitz CL, et al. A controlled evaluation of thermal biofeedback and thermal biofeedback combined with cognitive therapy in the treatment of vascular headache. J Consult Clin Psychol 1990; 58(2): 216–224. [DOI] [PubMed] [Google Scholar]
- 21. Holroyd KA, O’Donnell FJ, Stensland M, et al. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA 2001; 285(17): 2208–2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Holroyd KA, Labus JS, Carlson B. Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: the role of disorder severity and psychiatric comorbidity. Pain 2009; 143(3): 213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Basler HD, Jakle C, Kroner HB. Cognitive-behavioral therapy for chronic headache at German pain centers. Int J Rehabil Health 1996; 2(4): 235–252. [Google Scholar]
- 24. Martin PR, Nathan PR, Milech D, et al. Cognitive therapy vs. self-management training in the treatment of chronic headaches. Br J Clin Psychol 1989; 28(Pt 4): 347–361. [DOI] [PubMed] [Google Scholar]
- 25. Richardson GM, McGrath PJ. Cognitive-behavioral therapy for migraine headaches: a minimal-therapist-contact approach versus a clinic-based approach. Headache 1989; 29(6): 352–357. [DOI] [PubMed] [Google Scholar]
- 26. Martin PR, Forsyth MR, Reece J. Cognitive-behavioral therapy versus temporal pulse amplitude biofeedback training for recurrent headache. Behav Ther 2007; 38(4): 350–363. [DOI] [PubMed] [Google Scholar]
- 27. Kernick D, Stapley S, Hamilton W. GPs’ classification of headache: is primary headache underdiagnosed? Br J Gen Pract 2008; 58(547): 102–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Naylor MR, Keefe FJ, Brigidi B, et al. Therapeutic interactive voice response for chronic pain reduction and relapse prevention. Pain 2008; 134(3): 335–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Westen D, Novotny CM, Thompson-Brenner H. The empirical status of empirically supported psychotherapies: assumptions, findings, and reporting in controlled clinical trials. Psychol Bull 2004; 130(4): 631–663. [DOI] [PubMed] [Google Scholar]
- 30. Symvoulakis EK, Clark LV, Dowson AJ, et al. Headache: a ‘suitable case’ for behavioural treatment in primary care? Br J Gen Pract 2007; 57(536): 231–237. [PMC free article] [PubMed] [Google Scholar]


