Abstract
Background:
This study replicates a previous postal survey of general practitioners (GPs) to explore whether attitudes to opioid prescribing have changed at a time when the number of opioid prescriptions issued in primary care has increased.
Methods:
With permission, a 57-item survey instrument previously utilised with GPs in the South-west of England was circulated to 214 GPs in city-centre practices in the East Midlands. The survey instrument included items relating to practice context, prescribing patterns and attitudes about analgesic medication, perceived prescribing frequency and reluctance to prescribe.
Results:
Responses were received from 94 GPs (45%). Almost three-quarters (72.7%) of GPs reported that they sometimes or frequently prescribed strong opioids for chronic non-cancer pain. Over two-thirds (67.8%) reported that they were sometimes or frequently reluctant to prescribe strong opioids for chronic non-cancer pain. No significant relationships were observed between perceived frequency of prescribing and a range of demographic factors; however, concerns about ‘physical dependence’, ‘long-term commitment to prescribing’ and ‘media reports’ were associated with less frequent reported prescribing of, and greater reluctance to prescribe, strong opioids.
Discussion:
Given the national trend for increased opioid prescriptions, it is unsurprising that more frequent self-reported prescribing is reported here; however, increased frequency does not translate into less reluctance about prescribing. The effectiveness of strong opioids for chronic pain is recognised, but concerns about addiction, dependence and misuse inform a reluctance to use strong opioids. These juxtapositions highlight a continued need for clearer understanding of GPs’ perceptions of strong opioids and point to the potential benefit of dedicated guidelines or specialist education and training to address their uncertainties.
Keywords: Chronic pain, general practice, opioids, prescribing practice, analgesics
Introduction
Chronic non-cancer pain (CNCP) is a widespread health problem which affects around 7.8 million people in the United Kingdom.1 Its aetiology may be degenerative, neuralgic, post-surgical or simply unknown; it is most common among those over 50 years, but it may affect all age groups from school children to the most elderly.2 The implications for patients experiencing CNCP can be long term; for one-third of sufferers, it is a lifelong condition,1 and wide-reaching, with potential impact upon employment, mental health and lifestyle.3 The economic impact of CNCP is considerable: in 2010, the total cost of controlled medication prescribed in National Health Service (NHS) primary care was £455,013,758, and the vast majority of these were opioid drugs;4 in 2007, back pain cost the UK economy £12.3 billion, and chronic pain is the second most common reason for claiming incapacity benefit.3
CNCP is a condition which is difficult to manage; 68% of chronic pain sufferers describe times when their pain is not adequately controlled,3 and the quality of long-term pain management is often poor.2 Survey research shows that 81% of general practitioners (GPs) felt patients received suboptimal pain management with effective control in less than half of the cases.5 Analgesic medications are prescribed commonly, and, for carefully selected patients, strong opioids such as morphine sulphate, oxycodone, fentanyl and buprenorphine may play a role in the management of CNCP.6 CNCP is commonly managed in primary care settings, and it has been shown that the use of strong opioids can generate significant uncertainty for both GPs and patients.7–9 Patients are commonly concerned about physical dependence, tolerance and addiction.7,9 GPs share some of these concerns, and comment in both academic journals10–14 and the popular press15–17 illustrates the continued controversy about the use of opioids in the management of CNCP; to borrow from Stannard11 the debate has seemingly turned from ‘why not prescribe opioids?’ to ‘why not to prescribe opioids’.
Despite this, a greater number of opioid prescriptions are being issued4,18 – between 2007 and 2010, primary care prescriptions of the four main strong opioids increased from 4.2 to 5 million.4 Guidelines to support the prescription of opioids19 and changes to the medical school curriculum (to include pain management) may be pertinent in this trend; new formulations of opioid drugs and their promotion by the pharmaceutical industry may also be a factor. Whichever, it is clear that the context of opioid prescribing in general practice is complex.
Previous works by McCracken et al.7,8 and Hutchinson et al.9 have attempted to shed light upon this by considering GPs’ prescribing patterns and their attitudes towards opioid medication. Both studies demonstrate a complex relationship between GP demographics, GP attitudes and GP prescribing practice; both studies highlight that significant numbers of GPs do not prescribe opioids/strong opioids (25%/42%). Although limited in scope, these studies suggest that younger GPs, male GPs and GPs in full-time practice are more likely to prescribe opioids. Formal training was seen to impact positively upon opioid prescribing, although use of formal guidelines did not.8 Unsurprisingly, those less concerned about the use of opioid drugs and those who view them as appropriate for CNCP also prescribe them more frequently.8
Previous research has highlighted an uncertainty about opioid prescription which persists; for GPs, this includes concerns about professional competency (through a lack of training and prescribing guidelines), concerns relating to patient behaviour (such as addiction and the need for long-term commitment) and concerns about the risk of strong opioids; for patients, concerns may include addiction, perceptions of others and experience of side effects.7–14 There is a growing concern about the use of opioids (alongside their increased use) which indicates the need for further research to uncover and understand prescribing patterns. This study builds upon the work previously undertaken by McCracken et al.7,8 by (1) exploring whether attitudes to opioid prescribing have changed over time, given increases in the number of opioid prescriptions issued in primary care and (2) exploring changes in attitudes and patterns of prescribing with a different demographic and socio-economic profile of GPs since previous research had a limited geographic scope.
Methods
Sample selection
Using the NHS choices website,20 all GPs in NHS Nottingham City Primary Care Trust region were identified. At the time of the study, NHS Nottingham City Primary Care Trust (PCT) provided healthcare to a population of approximately 350,000 people including 62 medical practices with 214 GPs (NHS Nottingham City Clinical Commissioning Group is now responsible for commissioning healthcare in this region). Nottingham City is part of a larger urban conurbation (population is excess of 600,000) and is a city marked by significant deprivation; a quarter of the city’s population reside in areas in the most 10% deprived in England. It is an ethnically diverse city with 25% residents from Black or minority ethnic groups. Health inequalities are prominent and life expectancy lags behind the national average; in the most disadvantaged parts of the city men live on average 9.2 years fewer than the national average and women 8 years fewer.21
Questionnaire development
The questionnaire was developed by McCracken et al.8 to investigate patterns of prescription and concern about opioid analgesics for chronic non-malignant pain in general practice in the South West of England. It was informed by both literature review and the clinical practice of the original research team (GPs and psychologists with extensive clinical experience of chronic pain management). It is used here with permission and without alteration to enable direct comparison of data across regions and at different times.
The survey was a 57-item instrument designed to gather data regarding GPs, the situation of their practice, perceived patterns of prescribing analgesic medications, their concerns and attitudes about analgesic medications. It was organised into three sections: (1) Questions about yourself and your practice, (2) Treating chronic pain at your practice, and (2) Your prescribing of analgesic medications for chronic pain. Self-reported frequency of prescribing ‘strong opioids’, ‘weak opioids’, ‘non-steroidal anti-inflammatory drugs (NSAIDs)’ and other drugs for chronic non-malignant pain was measured on a Likert-type scale with responses including ‘always’, ‘frequently’, ‘sometimes’, ‘rarely’, ‘never’ or ‘unsure’. Reluctance to prescribe opioid analgesics for chronic non-malignant pain, cancer pain and acute pain was measured using the same scale. Attitudes and beliefs about prescribing opioid analgesic were considered in a number of ways across the instrument including questions relating to perceptions of appropriateness, effectiveness, social pressure and adverse effects. A total of 15 key ‘rationally derived attitude and belief items’8 were rated on a five point scale (Figure 1) with responses ‘often true’, ‘almost always true’ or ‘always true’ taken to indicate the respondents’ endorsement of the statement.
Figure 1.
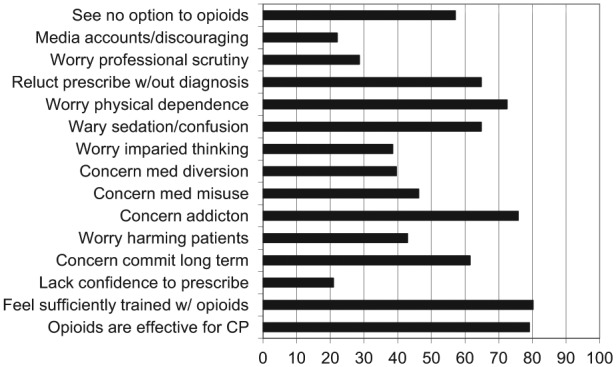
Percentage of general practitioners endorsing each survey item regarding attitudes and concerns about strong opioids as ‘often’, ‘almost always’ or ‘always true’ (N = 91).
w/out = without; med = medical; commit = committing; CP = chronic pain.
Study protocol and data collection
Correspondence with the local ethics committee established that formal ethical approval was not required for this study; local research governance procedures for the relevant region were followed. In February 2011, a questionnaire survey and postage-paid reply envelope were mailed to 214 GPs from 62 practices in Nottingham City together with a covering letter providing information about the study. Two follow-up reminders were posted to non-responders at 3-week intervals, and informed consent was taken to be return of the form. Four replies indicated that GPs no longer practised in the region, and completed questionnaires were received from 94 GPs, giving an overall response rate of 45%.
Analysis
Data were handled using SPSS PAS-W version 19.0. Analysis included descriptive statistics, chi-square test and Wilcoxon’s signed-rank test.
Results
Of those who responded, 38% were male (n = 36) and 53% female (n = 50; eight did not report their gender); age ranged from 29.3 to 69.5 years (n = 82, mean = 48.6 years, standard deviation (SD) = 9.6 years); 95% worked in urban areas and 5% in mixed urban/rural areas. The majority of respondents (85%, n = 73) obtained their primary medical qualification in the United Kingdom, with the remainder obtaining their qualification elsewhere (15%, n = 13). Over two-thirds of respondents described themselves as White (69%), with the remainder describing themselves as Indian (17%), Pakistani (5%), Black African (1%), other Asian (1%) or other (7%). Respondents reported having spent between 1 and 34 years working in general practice (mean years = 17, SD = 8).
Treating chronic pain
Only 11% of GPs reported completing some type of speciality training in chronic pain management; this included courses on medicines, palliative care and general pain management.
Excluding analgesic medication, acupuncture (25%, n = 23) was the most frequently reported treatment offered, with no other complementary therapies reported. Of the conventional therapies, 20% (n = 18), 15% (n = 14) and 12% (n = 11) of GPs indicated that they provided counselling, physiotherapy and psychological treatments within their practice, respectively. Just 22% of respondents (n = 20) reported they had a defined protocol or care pathway for referral of patients to secondary care chronic pain management services.
Prescribing of analgesic medications for chronic pain
Of the GPs, 60% reported that they sometimes prescribed strong opioids for chronic non-malignant pain, 27% reported rarely and 13% reported frequently. Reported prescribing of strong opioids was less frequent than reported prescribing of other analgesic medications (Figure 2): Wilcoxon’s matched-pairs signed-rank tests showed that these frequency ratings differed significantly from the ratings for the reported prescription of weak opioids (Z = −7.34, p < 0.001), NSAIDs (Z = −6.30, p < 0.001) and tricyclic antidepressants (Z = −7.30, p < 0.001).
Figure 2.
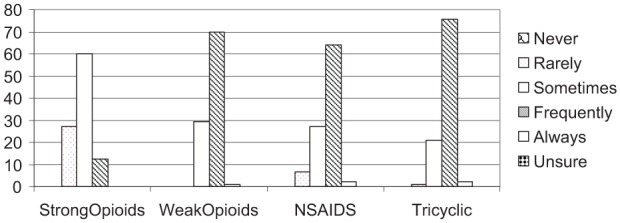
Survey results demonstrating percentages of general practitioners prescribing four common classes of analgesic medications for chronic non-malignant pain (N = 91).
NSAIDS: non-steroidal anti-inflammatory drugs.
More than half of the GPs (53%) reported they were sometimes reluctant to prescribe strong opioids for CNCP, 24% reported rarely, 16% frequently, 4% never and 3% always reluctant to prescribe. Greater reluctance was reported in the use of strong opioids for CNCP than for use in cancer pain (Figure 3): Wilcoxon tests showed that these reluctance ratings were significantly different from those for cancer pain (Z = −8.07, p < 0.001), but not different from those for acute pain (Z = −0.25, p = 0.98).
Figure 3.
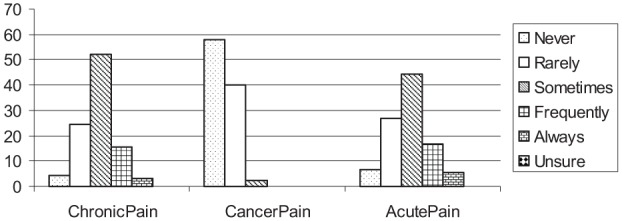
Survey results demonstrating percentages of general practitioners reporting reluctance to prescribe strong opioids for non-malignant pain, cancer pain and acute pain (N = 91).
More than half of the respondents (57%) reported that they followed guidelines or recommendations for the prescribing of medication for chronic pain; just under half (43%) reported either that they did not follow guidelines (27%) or that they were unsure (16%). Of the 57% who reported following guidelines, only a minority of GPs indicated which ones they used and these varied. Where reported, the National Institute for Clinical Excellence (NICE) guideline was the most commonly identified, followed by the World Health Organization guidelines and then the British National Formulary (BMF). Also cited were hospital guidelines, local Primary Care Trust guidelines, hospice guidelines and the Bandolier Pain Ladder.
GP and practice characteristics associated with strong opioid prescription for chronic pain
Analyses were conducted to examine potential correlates of perceived frequency of prescribing. Spearman’s correlation coefficients showed that there was no significant relationship between perceived frequency of prescribing and GP age, years in practice, number of GPs in the practice, approximate patient list size or practice location. Those who reported a greater reluctance to prescribe in turn reported prescribing less frequently (p < 0.001). Chi-square tests showed that there was no relationship between gender and perceived frequency of prescribing.
There were no significant differences in the perceived frequency of prescribing between GPs who were full-time and those who were part-time, χ2 (2, N = 88) = 0.57, p = 0.75. In this sample, GPs who had speciality training did not differ significantly in their perceived frequency of prescribing from those who had not, χ2 (2, N = 87) = 2.33, p = 0.31. The use of practice guidelines was unrelated to perceived frequency of prescribing, χ2 (4, N = 84) = 1.02, p = 0.90.
GP and practice characteristics associated with reluctance to prescribe opioids
Analyses were conducted to examine potential correlates of reluctance to prescribe strong opioids. As with the perceived frequency of prescribing data, ratings of reluctance were unrelated to GP gender, χ2 (4, N = 85) = 5.56, p = 0.24. Work hours (part-time or full-time) was unrelated to reluctance to prescribe, χ2 (4, N = 90) = 2.97, p = 0.56. GPs who had specialty training did not differ in their level of reluctance from those who had not had any training, χ2 (4, N = 89) = 3.24, p = 0.58. The use of practice guidelines was unrelated to reluctance to prescribe strong opioids, χ2 (8, N = 86) = 8.38, p = 0.40, as was practice location, χ2 (4, N = 88) = 6.19, p = 0.19.
GP attitudes and beliefs
Most GPs believed that opioids are effective for chronic pain (79%). A total of 80% felt sufficiently trained in the prescription of opioids. Three-quarters of respondents expressed concerns about addiction (76%) and physical dependence (73%). Two-thirds (66%) reported reluctance to prescribe when a clear diagnosis was absent. Almost two-thirds were worried about patients experiencing sedation and confusion (65%), and 38% were concerned about patients experiencing impaired thinking. Over half (58%) reported seeing no option but to prescribe opioids for some patients. Just under half of the GPs expressed concerns about medical misuse (47%), medical diversion (40%) and harming patients (43%). In all, 62% were concerned about a long-term commitment to prescribing opioids and 29% were worried about professional scrutiny. Around one-fifth (22%) reported they found media coverage of cases of inappropriate opioid use discouraging. More than one in five GPs (21%) indicated they lacked confidence in the area of prescribing analgesics.
Associations between GP attitudes and beliefs, and opioid prescribing
The associations between the 15 GP attitudes and concerns and the GPs’ frequency of prescribing and reluctance to prescribe strong opioid analgesics for chronic non-malignant pain were examined (Table 1).
Table 1.
Correlations of GPs’ attitudes and concerns towards strong opioids for chronic non-malignant pain with the frequency of prescribing and reluctance to prescribe them.
| GP attitudes and concerns | Correlation results |
|
|---|---|---|
| Frequency of prescribing (r) | Reluctance to prescribe (r) | |
| Opioids are effective for chronic pain | −0.17 | 0.28** |
| Feel sufficiently trained with opioids | −0.21 | 0.32** |
| Lack confidence to prescribe | 0.10 | −0.09 |
| Concern about commitment in long term | 0.26* | −0.49** |
| Worry about harming patient | 0.11 | −0.32** |
| Concern about addiction | 0.16 | −0.46** |
| Concern about medication misuse | 0.17 | −0.12 |
| Concern about medication diversion | 0.03 | −0.18 |
| Worry about impaired thinking | 0.11 | −0.21* |
| Worry about sedation or confusion | 0.21 | −0.12 |
| Worry about physical dependence | 0.26* | −0.29* |
| Reluctance to prescribe without diagnosis | 0.09 | −0.46** |
| Worry about professional scrutiny | 0.21 | 0.20 |
| Discouraged by media accounts | 0.26* | 0.23* |
| See no other option | −0.01 | 0.11 |
p < 0.05, **p < 0.01.
Each of the attitude and concern items is rated on a scale from 0 (never true) to 5 (always true), and the frequency and reluctance items are rated on a six-point scale including ‘always’, ‘frequently’, ‘sometimes’, ‘rarely’ and ‘never’.
Only 3 of the 15 attitude and concern items were significantly correlated with perceived frequency of prescribing opioids at a Bonferroni-corrected α level of p < 0.003 (0.05/15). These three correlates are ‘concern about a long-term commitment to prescribing opioids’, ‘worry about physical dependence’ and ‘discouraged by media accounts’. The higher the GPs’ levels of concern about long-term commitment and worry about patients becoming physically dependent, and the more discouraged about media accounts of medical misuse of opioids, the less frequently they reported prescribing strong opioids.
The correlation results demonstrate that the attitude and concern items were more highly associated with the reluctance ratings than the perceived frequency of prescribing. Of the 15 attitude and concern items, 9 achieved significant correlations with reluctance to prescribe strong opioids, 6 of which reached p < 0.001 level. The strongest correlate was ‘concern about a long-term commitment to prescribing strong opioids’, followed by ‘concern about addiction’ and ‘reluctance to prescribe without a diagnosis’. GPs who reported these concerns to a greater degree were more reluctant to prescribe opioids. Degree of feeling sufficiently trained to prescribe opioids and a worry about harming patients were both moderately sized but significant predictors of reluctance to prescribe. When the GPs felt they were sufficiently trained and were less worried about harming patients, they were less reluctant to prescribe.
Other weaker but significant predictors were ‘worry about physical dependence’, ‘opioids are effective for chronic pain’, ‘discouraged by media accounts’ and ‘worry about impaired thinking’. When the GPs were more concerned about patients becoming physically dependent on opioids and about opioids impairing patients’ thinking, they were more reluctant to prescribe opioids. Also, when they were more discouraged by the media accounts of medical misuse of opioids, they were more reluctant to prescribe. When GPs felt that opioids were effective for treating chronic pain, they were less reluctant to prescribe.
Discussion
This work marks a timely repeat of McCracken et al.’s8 previous review of GP prescribing and attitudes towards strong opioid medication. Conducted at a time when opioid prescriptions are on the increase in the United Kingdom,4,22 when campaigning organisations are calling for improved management of CNCP1,23 and when media reports highlight concern about strong opioid drugs,15–17 this study provides pertinent insight into an important and contentious topic.
Given the nationwide trend for increased willingness to prescribe opioids for chronic pain,24 perhaps fuelled by aggressive pharmaceutical marketing,25 it is unsurprising that GPs here reported more frequent prescribing of opioids for CNCP. Almost three-quarters of our sample reported that they sometimes or frequently prescribed opioids for CNCP, and no GP never prescribes; in the previous study, more than 4 in 10 reported that they rarely or never prescribed. Previous demographic differences in prescribing patterns appear to have diminished and we found no difference in the perceived prescribing frequencies of male and female GPs, full- and part-time GPs, and older and younger GPs. GPs who are less reluctant about prescribing opioids do report prescribing more frequently, but overall prescribing appears to be greater in recent years with no clear demographic trends. More GPs reported accessing prescribing guidelines (57% compared with 43%), although it should be noted that the most frequently cited26 is for neuropathic pain which contains little information on opioids; more specific guidelines from the British Pain Society19 and Royal College of Anaesthetists were not identified here. Only 1 in 10 of our GPs had received formal training in pain management (comparable with the earlier study), and neither formal training nor guideline use was related to perceived frequency of prescribing in our study.
While our sample suggests marked changes in the frequency of reported prescribing a reported reluctance to prescribe persists. In both studies approximately half of GPs described being sometimes reluctant to prescribe opioids and around one in five always or frequently reluctant. As with McCracken et al.’s8 previous study reluctance to prescribe is more strongly correlated to GP attitudes and concerns than perceived frequency of prescribing. Across both studies, a number of concerns and attitudes are consistently related to a reluctance to prescribe – concerns about addiction, about commitment in the long-term and about prescribing without diagnoses being the strongest and most consistent across the two studies. Concerns about addiction and physical dependence are stronger in our sample, and almost twice as many GPs are now concerned about opioids being diverted for non-medicinal use by others, compared with the previous survey.8 This finding is not unexpected given the media attention in recent years surrounding the ‘prescription opioid crisis’ – prescription drug misuse and dependence, coupled with steep increases in opioid-related mortality.27
Despite these concerns, most GPs feel that opioids are effective in cases of CNCP. In our sample, more GPs feel sufficiently trained to prescribe opioids and there is less reluctance to prescribe without diagnosis. Each of these attitudes is inversely correlated with reluctance to prescribe, but none are significantly related to reported frequency of prescription. Relationships between perceived prescribing frequency and GP attitudes and concerns are weaker in our study than the previous work with one notable exception. Here, feeling discouraged by media accounts demonstrates a stronger correlation with reduced prescribing than in the earlier study (it is also significantly correlated to increased reluctance to prescribe). The impact of the media may be important in understanding why the reluctance to prescribe opioids has not diminished at a time when the number of opioid prescriptions has increased.
There are other factors that may influence GPs’ prescribing patterns, such as lack of pharmacological alternatives and a lack of concrete guidelines to inform opioid use. Continued uncertainty about opioids might suggest that GPs prescribe despite their concerns and not because of a commitment to their use. More than half of the GPs surveyed here indicated that they often perceive no alternative but to prescribe opioid medication, and only four non-pharmacological treatment alternatives were proposed by GPs in this survey, each available in only small number of practices. This is consistent with previous findings8 and indicates that while the number of formulations of opioids may be increasing, the use of alternative therapies and non-pharmacological pain management strategies is not. Continued uncertainty in managing opioid prescriptions may also stem from a lack of clear formal support and guidelines. Few GPs in our sample reported having received formal training, few adhered to a formal pathway for treating CNCP and most of those who utilised guidelines referred to NICE guidelines, which are of limited application in the management of opioid prescriptions. It may be relevant that, at the time of data collection, pain management lay outside the Quality and Outcomes (QOF) Framework for General Medical Services; inclusion of pain management in such a framework might generate greater scrutiny, more clarity and more consistency in opioid prescribing and management. In summary, therefore, it appears that changes in perceived prescribing frequency have not been matched by changes in prescribing support for GPs; this might be addressed through (1) inclusion of pain management in QOF,1 (2) advocating the provision, use and adoption of ‘good practice’ guidelines for opioid prescription and (3) enhanced and increased provision of pain management education and training. The need for increased training and support for GPs regarding opioid prescribing is now being recognised, and it has been suggested that training and education are acceptable to GPs and may increase knowledge about opioids and reduce concerns about prescribing, but does not appear to influence prescribing behaviour or GP well-being (related to prescribing).28
The findings of this study are limited to retrospective reports of prescribing practices, rather than objective observations of prescribing behaviour. Our response rate was relatively low and we do not have data on non-responders. However, low response rates are a common challenge in research with GPs; our response rate was greater than that of McCracken et al.,8 and previous studies have had comparable response rates without showing evidence of responder bias.29
Conclusion
Despite changes to the context of opioid prescribing in the United Kingdom, the findings of this survey are similar to those of previous studies that have attempted to shed light on GP experiences and attitudes towards opioid prescribing for CNCP.8,9 The frequency of prescribing has increased, but concerns about opioid use and a reluctance to prescribe persist for many GPs, and importantly persist for GPs with varying levels of prior training and experience and from diverse demographics. This juxtaposition points to the continued need for greater clarity in our understanding of how GPs perceive the benefits and challenges of opioid use. It also points to an ongoing need for more explicit guidance in the process of opioid prescribing – guidelines such as those generated for the management of opioids in palliative care30 would be a positive step forward. Additional training and educational provision in pain management and in the management of opioid prescriptions may be required to support GPs to feel more confident in their prescribing.
Acknowledgments
The authors would like to thank the GPs who participated in the study and Sally Zhou for assistance with data handling.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Chief Medical Officer. CMO annual report 2008. London: Department of Health, 2009. [Google Scholar]
- 2. Elliot A, Smith B, Hannafor P, et al. The course of chronic pain in the community: the results of a four year follow-up. Pain 2002; 99: 299–307. [DOI] [PubMed] [Google Scholar]
- 3. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10(4): 287–333. [DOI] [PubMed] [Google Scholar]
- 4. Care Quality Commission. The safer management of controlled drugs – annual report 2010. Newcastle upon Tyne: Care Quality Commission, 2011. [Google Scholar]
- 5. Stannard C, Johnson M. Chronic pain management – can we do better. Curr Med Res Opin 2003; 19: 703–706. [DOI] [PubMed] [Google Scholar]
- 6. Kalso E, Edwards J, Moore R, et al. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain 2004; 112: 372–380. [DOI] [PubMed] [Google Scholar]
- 7. McCracken L, Hoskins J, Eccleston C. Concerns about medication and medication use in chronic pain. J Pain 2006; 7: 726–734. [DOI] [PubMed] [Google Scholar]
- 8. McCracken L, Velleman S, Eccleston C. Patterns of prescription and concern about opioid analgesics for chronic non-malignant pain in general practice. Prim Health Care Res Dev 2008; 9: 146–156. [Google Scholar]
- 9. Hutchinson K, Moreland A, Williams A, et al. Exploring beliefs and practice of opioids prescribing for persistent non-cancer pain by general practitioners. Eur J Pain 2007; 11: 93–98. [DOI] [PubMed] [Google Scholar]
- 10. Knaggs R. Guest Editorial. Br J Pain 2012; 6: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stannard C. Opioid prescribing in the UK: can we avert a public health disaster? Br J Pain 2012; 6: 7–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dhalla I, Persaud N, Juurlink D. Facing up to the prescription opioid crisis. BMJ 2011; 343: d5142. [DOI] [PubMed] [Google Scholar]
- 13. Grady D, Berkowitz S, Katz MH. Opioids for chronic pain. Arch Intern Med 2011; 171(16): 1426–1427. [DOI] [PubMed] [Google Scholar]
- 14. Katz MH. Long-term opioid treatment of nonmalignant pain: a believer loses his faith. Arch Intern Med 2010; 170(16): 1422–1424. [DOI] [PubMed] [Google Scholar]
- 15. Kloth D. America’s fatal addiction to prescription drugs. The Guardian, 10 June 2011. Available at http://www.theguardian.com/commentisfree/cifamerica/2011/jun/10/prescription-drug-abuse (accessed 22 March 2015).
- 16. Pilkington E. Pharmageddon: how America got hooked on killer prescription drugs. The Guardian, 9 June 2011. [Google Scholar]
- 17. Campbell D. Millions ‘lending’ prescription drugs. The Observer, 30 May 2010. Available at http://www.theguardian.com/uk/2010/may/30/millions-lend-prescription-drugs-survey (accessed 22 March 2015).
- 18. Boudreau D, Korff MV, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf 2009; 18(12): 1166–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. British Pain Society. Opioids for persistent pain: good practice. London: British Pain Society, 2010. [Google Scholar]
- 20. NHS choices. NHS Nottingham City PCT, http://www.nhs.uk/Services/Trusts/GPs/DefaultView.aspx?id=89662 (2012, accessed 1 February 2012).
- 21. NHS Nottingham City CCG. Annual report 2011–2012. London: Department of Health, 2012. [Google Scholar]
- 22. Zin CS, Chen LC, Knaggs RD. Changes in trends and pattern of strong opioid prescribing in primary care. Eur J Pain 2014; 18(9): 1343–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chronic Pain Policy Coalition. A new pain manifesto. London: Chronic Pain Policy Coalition, 2007. [Google Scholar]
- 24. Dhalla IA. Facing up to the prescription opioid crisis. BMJ 2011; 343: d5142. [DOI] [PubMed] [Google Scholar]
- 25. Van Zee A. The promotion and marketing of oxycontin: commercial triumph, public health tragedy. Am J Public Health 2009; 99: 221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. National Institute for Health and Clinical Excellence. Clinical guideline 96-neuropathic pain: the pharmacological management of neuropathic pain in adults in non-specialist settings. Manchester: National Institute for Health and Clinical Excellence, 2010. [PubMed] [Google Scholar]
- 27. Winstock A, Bell J, Borschmann R. Editorial: opioids in the UK: what’s the problem? BMJ 2013; 347: f5108. [DOI] [PubMed] [Google Scholar]
- 28. McCracken LM, Boichat C, Eccleston C. Training for general practitioners in opioid prescribing for chronic pain based on practice guidelines: a randomised pilot and feasibility trial. J Pain 2012; 13(1): 32–40. [DOI] [PubMed] [Google Scholar]
- 29. Robertson J, Walkom EJ, McGettigan P. Response rates and representativeness: a lottery incentive improves physician return rates. Pharmacoepidemiol Drug Saf 2005; 14(8): 571–577. [DOI] [PubMed] [Google Scholar]
- 30. National Institute for Health and Clinical Excellence. Clinical guideline 140-opioids in palliative care: safe and effective prescribing of strong opioids for pain in palliative care of adults. Manchester: National Institute for Health and Clinical Excellence, 2012. [Google Scholar]


