Abstract
Objective:
The objective of this prospective, noninterventional, 8-months, observational study was to analyze and compare depression, anxiety, and stress (DAS) levels and their impacting factors in homogenous surviving cancer patients receiving chemotherapy as compared to normal control.
Materials and Methods:
A prospective and descriptive study was carried out jointly by Pharmacology and Oncology departments of a tertiary care center in Malwa region of Punjab. The data was collected by administering the validated questionnaire/response (21-item Depression Anxiety and Stress Scale (DASS-21)) after taking ethical approval and informed consent.
Results:
All eligible 300 subjects participated in the study and they were compared with 300 matched control. The mean age of the cases (cancer patients) and controls was 50.58 ± 13.64 and 46.1 ± 11.78 (mean (M) ± standard deviation (SD)) years. Statistical significant difference was observed in mean ‘scoring of DAS’ in cancer patients when compared with control groups. Anxiety mean scoring showed a statistical significant difference in groups (according to chemotherapy cycles given and duration of disease). Stress was more observed in breast cancer patients.
Conclusion:
Holistic approach in cancer management including psychological evaluation and its solution at appropriate time/stage signifies the need of time as the present study revealed that the percentage of DAS as per the DASS scale was 90, 56, and 28%, respectively. A judicious diagnosis with an apposite intercession including psychological consultation with social support at appropriate time may alleviate the extra burden of psychological disorder, rather enhance the quality of life of cancer-affected rural population.
Keywords: Cancer chemotherapy, DASS-21, Depression, Psycho-oncology, Quality of life
INTRODUCTION
In India, around 2.0–2.5 million people are living with one or another kind of cancer menace, over and above 7–8 lakhs new cases added every year to the existing burden. Data enumerated different cancer prevalence rate gender wise; as among males: 46–122 per 100,000 populations and among females: 57–135 per 100,000 population. Cancer deaths reported per year: 4–5 lakhs.[1]
In northern India, the state of Punjab is experiencing a rising burden of cancer A survey had been conducted by the Department of Health and Family Welfare, Government of Punjab in 2009 in which 7,738 cases of cancer were identified and out of which 245 were only in Faridkot district of Punjab.[1]
Despite modern progress in securing remission and possible cancer cure, it still remains a disease which is connected with hopelessness, pain, fear, and death. Its diagnosis and treatment often produces psychological stress resulting from the authentic symptoms of the disease and deep rooted fear of a silent killer that moves stealthily upon us without warning. Ultimately cancer induces psychological trait that becomes a symbol for grief and pain; that is the reason why psychosocial oncology research studies indicated that a noteworthy percentage of cancer patients at all stages of the sickness have been confronted with psychosocial suffering.[2,3]
Majority of psychological distress encountered are adjustment disorders with depression and/or anxiety, major depression, and delirium. Others (primarily anxiety disorders, behavior disorders, and major depressive disorders) are preexisting conditions often exacerbated by the illness.[4,5] The occurrence of some psychiatric sicknesses (major depression, generalized anxiety, and adjustment disorder) are elevated in patients undergoing radiotherapy (RT) or palliative treatment, terminally-ill patients, and patients experiencing irrepressible pain, which also involve an increased risk for suicidal and disorder psychological behavior.[6]
Some studies anticipated that approximately 20–50% of cancer patients need a psychiatrist for treating major depression or anxiety throughout their cancer experience.[6,7] In the present time; a considerable amount of literature, guidance programs, and research has been evolved with holistic approach to confinement of psychological issues. Acquaintances between psychological and physiological domains of cancer danger and survival are being actively searched through psychoneuroimmunology. Research in these areas is less noticed but with advancement of psychological understanding of disease process; psycho-oncology slowly has become the youngest subspecialty of oncology, as one of the most clearly defined subspecialties of psychiatry.[8,9,10]
There are studies which established the coexistence of depression and cancer, reported prevalence rates of depression for solid tumors ranging from 20 to 50%[11] and in the screening program conducted by Ell and colleagues among low-income women with cancer, the prevalence rate for major depression was 24%.[12] The effects of depression on morbidity/mortality are not definitively established though depression is allied to speedy progression of disease. Possible reasons are neuroimmunological alteration, reduced compliance with treatment, behavioral transformation, and effects of depression on personal, social and family functioning.[13]
Anxiety related with cancer intensifies feelings of pain, hampering with sleep habits, causes nausea and vomiting, and negatively affect quality of life.[14] This varied from 0.9 to 49% in one review and large studies using uniform psychiatric examination rather demonstrated lower prevalence rates, from 10 to 30%.[14,15]
Cancer-related stress influence all patients with cancer and harmfully impacts cancer outcomes in terms of response to treatment, quality of life, disease progression, and survival. By and large, stress response engages activation of several body systems including the autonomic nervous system and the hypothalamic–pituitary–adrenal axis. The ‘fight or flight’ response is elicited by the production of mediators such as norepinephrine and epinephrine from the sympathetic nervous system and the adrenal medulla. A growing number of studies have uncovered major role of chronic stress in cancer progression.[16,17]
With above said consideration, the primary objective of the present study was to approximate the depression, anxiety, and stress (DAS) levels in homogenous surviving cancer patients. The secondary objective was to correlate the primary objective with different demographical parameter such as age, gender, duration of cancer diagnosis, chemotherapy cycles, cancer types, etc. In this present study, we planned a self-reported, response-based questionnaire using 21-item Depression Anxiety and Stress scale (DASS-21) which is designed to measure the severity of a range of symptoms common to DAS.[18]
MATERIALS AND METHODS
The present study is a noninterventional, cross-sectional, self-reported based psychological investigation analysis that was carried out at the outpatient clinic of the Oncology Department at GGS Medical College, Faridkot from January 2014 to September 2014. A total of 600 study subjects were evaluated for DAS that included 300 cancer patients and 300 matched controls.
The following inclusion criteria were set before initiation of study: i) Diagnosed with cancer and visiting the institution to receive chemotherapy or adjuvant chemotherapy. ii) No history of other chronic disease such as diabetes and heart disease. iii) No known mental problems or being treated with psychotropic drugs.
A set format of questionnaire containing demographic and psychological questions (DASS-21) was provided to cancer subjects and normal control in their respective understandable language. Before being asked the subjects to participate, a formal consent was obtained from all of them including proper approval from institutional ethics committee. The DASS-21 questionnaire were translated in local understandable language and prevalidated in small cancer sufferer cohort. The response to DASS-21 was collected from the patients of outpatient department during their respective chemotherapy session. Personal details like age, gender, education, occupation, marital status, address, and details of family history; cycles of chemotherapy; duration of diagnosis; etc.; were also collected.
Tools used
The DASS-21 is a 21-item self-report questionnaire designed to measure the severity of a range of symptoms common to DAS. It is a generic scale that shows strong internal consistency and reliability for each subscale (DAS) and it has been prevalidated in cancer patients.
In completing the DASS, the individual is required to indicate the presence of a symptom over the previous week. Each item is scored from 0 (did not apply to me at all over the last week) to 3 (applied to me very much or most of the time over the past week). There are four possible answers in terms of severity or frequency, organized in a scale from 0 to 3. The result is obtained by adding up the scores of the items for each of the three subscales.
The depression subscale assesses symptoms like inertia; anhedonia; dysphoria; lack of interest/involvement; self-depreciation; devaluation of life; and discouragement. The anxiety subscale evaluates excitation of the autonomous nervous system; musculoskeletal effects; situational anxiety; and subjective anxiety experiences. Finally, the stress subscale assesses difficulty to relax; nervous excitation; easy perturbation/agitation; irritability/exaggerated reaction; and impatience.
Calculation of extent of DAS in individual cancer patient is done with corresponding number of questionnaire which is specific (each subclass contained 7 questions) for DAS. Higher score correspond to more severe psychological disorder that is reflected in critical functioning of the DASS is to assess the severity of the core symptoms of DAS.[18]
Statistical analysis
Baseline distinctiveness (demographic, cancer-specific parameter, and DASS scoring) were summarized by descriptive statistics. Frequency, mean, percentages, and standard deviation were calculated as per the study requirement. DASS scoring between groups were compared with analysis of variance (ANOVA) and simple unpaired t-test. All P ≤ 0.05 were considered as significant.
Permissions
For the study, permission was obtained from Institutional Review Board and Ethics Committee. Written informed consent was obtained from all patients before participation.
RESULTS
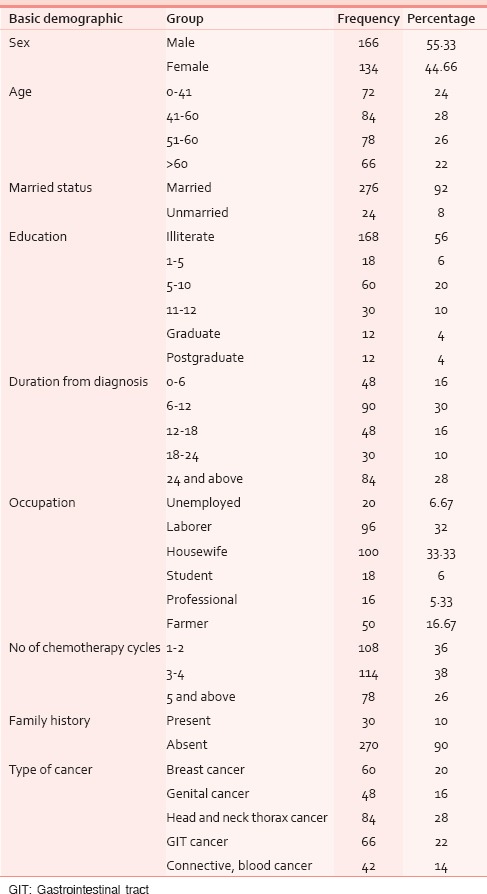
All 600 eligible study subjects participated in the study with 300 cancer patients and 300 matched controls. The mean age of the cases (cancer patients) and controls was 50.58 ± 13.64 and 46.1 ± 11.78 (mean (M) ± standard deviation (SD)) years with most common age group being 41–50 years with male preponderance (52%) in patients group and in control group was 0–40 years with male preponderance. Out of the total subjects, 56% were illiterate and majority was (33.33%) housewife by occupation as shown in Table 1. Out of our 300 cancer patients, 28% were suffering from head and neck thorax cancer followed by gastrointestinal tract (GIT; 22%) and breast (20%). Family history was seen only in 10%, in which no significant hereditary correlation was observed. As per the chemotherapy session's progress, we divided the patients in three subgroups; the first group had 108 patients and received one to two chemotherapy cycles, the second group had 114 patients and received three to four chemotherapy cycles, and third group had 78 patients and received more than five chemotherapy cycles.
Table 1.
Baseline assessment
As per the DASS-21 scoring system described in DASS-21 scale scoring manual, a high scale score represents a high level of symptomatology related to DAS. M and SD of individual item (DAS) were calculated and compared with age, duration of diagnosis, gender, type of cancer, chemotherapy cycles, and 300 matched controls.[19] As shown in Table 2, the statistical significance was tested by ANOVA and unpaired t-test as applicable.
Table 2.
Comparison of depression, anxiety, and stress with different variable
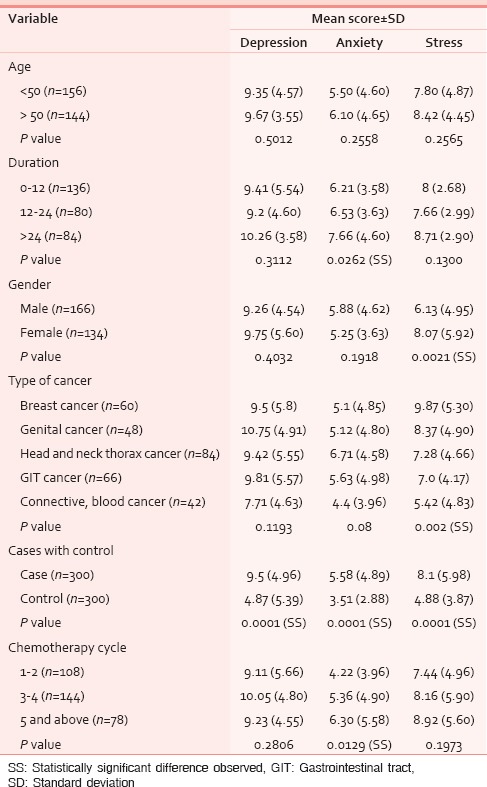
Final calculation of DASS scoring results showed that statistical significant difference was observed in mean scoring of DAS in 300 cases and 300 control groups. As shown in Table 2. Apart from above anxiety mean scoring in three groups (according to chemotherapy cycles given) and three groups according to duration of diagnosis has shown a statistical significance difference among groups [Table 2]. Gender wise, female patients experienced more stress than male cancer patients. A significant difference was noted in mean stress score in different cancer type with more stress in breast cancer patients and lower with blood and connective tissue cancer. No significance difference was noted according to different age group in cancer patients.
Figure 1 indicates the mean score of DAS in graphical outline. As per the Figure 2; severity scoring pointed out 18, 66, and 120 cancer patients with normal level of DAS, respectively. On higher side 120, 66, and 6 patients’ experienced severe DAS, respectively. Only 12 cancer patients had shown extremely severe anxiety level.
Figure 1.
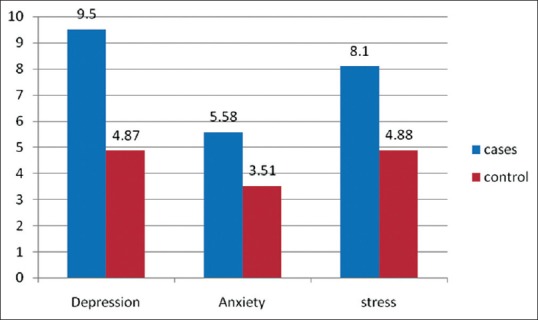
Mean score of depression, anxiety, and stress among cancer patients and control
Figure 2.

Severity of depression, anxiety, and stress according to DASS-21 scale. DASS-21 = 21-item Depression Anxiety Stress Scale
DISCUSSION AND CONCLUSION
In this study, the range of DAS (symptomatic only excluding milder cases) as per the DASS-21 scale was 90, 56, and 28%, respectively. In the present study, the higher depression and anxiety prevalence had similarities with other researches who worked on psychological disorder related to cancer.[20,21]
The present study also highlighted the strong correlation between cancer and psychological disorder and this strong evidence is supported by Spiegel et al., who reported strong evidence of cancer–depression association, with depression prevalence from 20 to 50% in sizeable tumors.[22]
There is a strong link between psychological factors such as stress, depression, and social isolation with disease progression. Sustained activation of negative affective pathways may be the strongest links in cancer progression as seen in chronicity of negative effect due to depression and hopelessness.[19,23]
The psychological analysis according to cancer type showed a distinctive pattern, that is, more prevalence of DAS in patients suffering from cancer of head and neck, breast, and genital tract. More stress was noticed in female gender due to breast and genital cancer that could be due to concerns regarding disfigurement, self-image, and effect on sex drive. These findings are in concordance with study done by Nikbakhsh et al.[24]
In contrast, DAS was much lower in hematological malignancies (non-Hodgkin’ lymphoma and Hodgkin's lymphoma) as these malignancies are internal and the symptom is very vague, no external disfigurement is visible. Similar view is shared by Prieto et al., who stated that a sample of hematological inpatients prevalence of major depression was 9% than what we have seen in other categories.[10,11,13]
The several studies and review are not in accordance to our findings; they either show higher or lower prevalence of DAS and potential explanations for this range could be the characterization of morbid anxiety, the range of self-report measures applied, social and financial status, demographic factors, and aspects of cancer diagnosis and treatment that may be associated with morbid anxiety.[11,12,25] As in our study, most of the cancer patients belongs to low socioeconomic strata and health insurance cover is very rare in this rural population, so financial difficulties are very widespread distinguishing of these patients which further add up disease unrelated psychological strain.
Cancer patients undergoing first chemotherapy cycles have shown lower levels of psychological issues compared to successive chemotherapy cycles. The explanation may be that as they are exposed to various adverse effects in initial chemo cycles like vomiting, diarrhea, dry mouth, pain, weakness, anxiety, lack of sleep, neuropathy, and anorexia; which leads to higher levels of psychological fear problems as they are offered the next higher treatment cycles as shown in the Table 2, where DAS score raised with the number of chemotherapy cycles proceeding with time.
This study showed clearly higher prevalence of depression and anxiety and stress disorders among cancer patients in comparison to matched-control patients. Different age groups did not influence the occurrence of DAS.
It is anticipated that the conclusion of this study will lead to identify the level of psychological distress and complicated needs to solve the problems reported by these complex population of cancer patients. The level of psychological distress is alarmingly high and needs to be addressed by all healthcare professionals involved in the follow-up care. The high prevalence and association with outcome justifies future research regarding the management of DAS in cancer-affected population. We think that this study needs to be extensive in the future to engage more patients and need to evaluate the results with prescribed psychiatric intervention in early stages of cancer management that may be in a shape of bigger robust clinical examination with larger study samples in multiple settings.
CONCLUSION
A comprehensive assault by cancer disrupts the normal well-being of patients or we can say that cancer is an important health issue influencing psychological balance that may further aggravate the disease progression. The frequently considered efficacy criteria of cancer cure therapy is somewhat deficient; as we have seen in present study the actual burden of psychological disorder (DAS) despite advance care of the cancer patients. Holistic approach (including psychological evaluation and its solution at appropriate time/stage) signifies the need of time as the present study revealed, the range of DAS (symptomatic only excluding milder cases) as per the DASS-21 scale was 90, 56, and 28%, respectively. DASS score differs with type of cancer, the numbers of chemotherapy cycle patients were subjected to, duration of diagnosis, and wildly differ with the matched control that itself demonstrates the varied type of psychological interventions needed as per the individuals need. A judicious diagnosis with a apposite intercession including psychological consultation with social support at appropriate time may alleviate the taboo of cancer as a deadly and fatal disease in our rural population.
Footnotes
Source of Support: Study funded by STS 2014 Indian Council of Medical Research Project.
Conflict of Interest: None declared.
REFERENCES
- 1.Project Proposal September 2012. State Health Systems Resource Centre National Rural Health Mission. Department of Health and Family Welfare, Government of Punjab. [Last accessed on 2014 Sep 08]. Available from: Pbhealth.gov.in/Final%20State%20Proposal.pdf .
- 2.Lesko LM. Psychologic issues. In: De Vita VT Jr, Hellman S, Rosenberg SA, editors. Cancer: Principles and Practice of Oncology. 5th ed. Vol. 2. Philadelphia: Lippincott-Ravewn; 1997. pp. 2879–91. [Google Scholar]
- 3.Parker PA, Baile WF, de Moor C, Cohen L. Psychosocial and demographic predictors of quality of life in a large sample of cancer patients. Psychooncology. 2003;12:183–93. doi: 10.1002/pon.635. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal A, Syed GM, Siddiqui KS. Mental disorders in cancer patients: Observations at a tertiary care center in Pakistan. Pak J Med Sci. 2002;18:109–16. [Google Scholar]
- 5.Rouhani M, Holland JC. Psychiatric aspects of cancer. In: Gelder MG, Lopez-Ibor JJ, Andreasen NC, editors. New Oxford Textbook of Psychiatry. Vol. 2. Oxford: Oxford University Press; 2000. pp. 1178–85. [Google Scholar]
- 6.Chochinov HM. Depression in cancer patients. Lancet Oncol. 2001;2:599–606. doi: 10.1016/S1470-2045(01)00456-9. [DOI] [PubMed] [Google Scholar]
- 7.Carlson LE, Bultz BD. Benefits of psychosocial oncology care: Improved quality of life and medical cost offset. Health Qual Life Outcomes. 2003;1:8. doi: 10.1186/1477-7525-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carvalho MM. Psycho oncology: History, characteristic and challenge. Psicol USP. 2002;13:151–66. [Google Scholar]
- 9.Holland JC. History of psycho oncology: Overcoming attitudinal and conceptual barriers. Psychosom Med. 2002;64:206–21. doi: 10.1097/00006842-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Grassi L, Gritti P, Rigatelli M, Gala C. Psychosocial problems secondary to cancer: An Italian multicentre survey of consultation-liaison psychiatry in oncology. Italian Consultation-Liaison Group. Eur J Cancer. 2000;36:579–85. doi: 10.1016/s0959-8049(99)00285-3. [DOI] [PubMed] [Google Scholar]
- 11.Sharpe M, Strong V, Allen K, Rush R, Postma K, Tulloh A, et al. Major depression in outpatients attending a regional cancer centre: Screening and unmet treatment needs. Br J Cancer. 2004;90:314–20. doi: 10.1038/sj.bjc.6601578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ell K, Sanchez K, Vourlekis B, Lee PJ, Dwight-Johnson M, Lagomasino I, et al. Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecologic cancer. J Clin Oncol. 2005;23:3052–60. doi: 10.1200/JCO.2005.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prieto JM, Atala J, Blanch J, Carreras E, Rovira M, Cirera E, et al. Role of depression as a predictor of mortality among cancer patients after stem-cell transplantation. J Clin Oncol. 2005;23:6063–71. doi: 10.1200/JCO.2005.05.751. [DOI] [PubMed] [Google Scholar]
- 14.Stark DP, House A. Anxiety in cancer patients. Br J Cancer. 2000;83:1261–7. doi: 10.1054/bjoc.2000.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van't Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological squeal of cancer diagnosis: A meta-analytical review of 58 studies after 1980. Psychosom Med. 1997;59:280–93. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Antoni MH, Lutgendorf SK, Cole SW, Dhabhar FS, Sephton SE, McDonald PG, et al. The influence of bio-behavioral factors on tumor biology: Pathways and mechanisms. Nat Rev Cancer. 2006;6:240–8. doi: 10.1038/nrc1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lutgendorf SK, De Geest K, Bender D, Ahmed A, Goodheart MJ, Dahmoush L, et al. Social influences on clinical outcomes of ovarian cancer patients. J Clin Oncol. 2012;30:2885–90. doi: 10.1200/JCO.2011.39.4411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lovibond SH, Lovibond PF. 2nd ed. Sydney: Psychology Foundation; 1995. “Manual for the Depression Anxiety Stress Scales”. Available from The Psychology Foundation, Room 1005 Mathews Building, University of New South Wales, NSW 2052, Australia. [Google Scholar]
- 19.Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer. 2009;115:5349–61. doi: 10.1002/cncr.24561. [DOI] [PubMed] [Google Scholar]
- 20.Thalén-Lindström A, Larsson G, Glimelius B, Johonsson B. Anxiety and depression in oncology patients; A longitudinal study of a screening, assessment and psychosocial support intervention. Acta Oncol. 2013;52:118–27. doi: 10.3109/0284186X.2012.707785. [DOI] [PubMed] [Google Scholar]
- 21.Step MM, Kypriotakis GM, Rose JH. An exploration of the relative influence of patient's age and cancer recurrence status on symptom distress, anxiety, and depression over time. J Psychosoc Oncol. 2013;31:168–90. doi: 10.1080/07347332.2012.761318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spiegel D, Giese-Davis J. Depression and cancer: Mechanisms and disease progression. Biol Psychiatry. 2003;54:269–82. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- 23.Stommel M, Given BA, Given CW. Depression and functional status as predictors of death among cancer patients. Cancer. 2002;94:2719–27. doi: 10.1002/cncr.10533. [DOI] [PubMed] [Google Scholar]
- 24.Nikbakhsh N, Moudi S, Abbasian S, Khafri S. Prevalence of depression and anxiety among cancer patients Caspian. J Intern Med. 2014;5:167–70. [PMC free article] [PubMed] [Google Scholar]
- 25.Atesci FC, Oguzhanoglu NK, Baltalarli B, Karada F, Ozdel O, Karagöz N. Psychiatric disorders in cancer patients and associated factors. Turk Psikiyatri Derg. 2003;14:145–52. [PubMed] [Google Scholar]


