Abstract
The ketogenic diet (KD) is a broad-spectrum therapy for medically intractable epilepsy and is receiving growing attention as a potential treatment for neurological disorders arising in part from bioenergetic dysregulation. The high-fat/low-carbohydrate “classic KD”, as well as dietary variations such as the medium-chain triglyceride diet, the modified Atkins diet, the low-glycemic index treatment, and caloric restriction, enhance cellular metabolic and mitochondrial function. Hence, the broad neuroprotective properties of such therapies may stem from improved cellular metabolism. Data from clinical and preclinical studies indicate that these diets restrict glycolysis and increase fatty acid oxidation, actions which result in ketosis, replenishment of the TCA cycle (i.e., anaplerosis), restoration of neurotransmitter and ion channel function, and enhanced mitochondrial respiration. Further, there is mounting evidence that the KD and its variants can impact key signaling pathways that evolved to sense the energetic state of the cell, and that help maintain cellular homeostasis. These pathways, which include PPARs, AMP-activated kinase, mammalian target of rapamycin, and the sirtuins, have all been recently implicated in the neuroprotective effects of the KD. Further research in this area may lead to future therapeutic strategies aimed at mimicking the pleiotropic neuroprotective effects of the KD.
Keywords: fatty acids, cellular signaling, ketone, oxidative stress
The ketogenic diet (KD) is a high-fat/low-carbohydrate therapy for drug-resistant epilepsy (1, 2), and is increasingly being studied for therapeutic efficacy in a number of neurological disorders, including epilepsy, headache, neurotrauma, Alzheimer’s disease (AD), Parkinson’s disease (PD), sleep disorders, brain cancer, autism, pain, and amyotrophic lateral sclerosis (ALS) (3, 4). This is a result of growing experimental evidence for the broad neuroprotective properties of the KD, and mechanistic linkages to key cellular signaling pathways and fundamental bioenergetics processes, notably within mitochondria (5, 6). In recent years, the field of neurometabolism has been greatly amplified by interest in dietary treatments such as the KD (6), and by the recognition that bioenergetic dysregulation may be a critical pathophysiological factor in diseases of the nervous system (7, 8). Indeed, there is increasing appreciation for the concept of energy failure, principally from mitochondrial dysfunction, as a key mechanism resulting in neuronal death seen in neurodegenerative diseases (8).
That diet and nutrition should influence brain function should not be altogether surprising and much clinical and laboratory data exist linking disturbances in energy metabolism to a variety of clinical disorders (5, 9, 10). Fundamentally, any disease in which the pathogenesis is affected by disturbances in cellular energy utilization, and this could apply to almost every known medical condition, would potentially be amenable to treatments that restore normal metabolism. A common thread of such diet-based therapies for brain diseases is that metabolic substrates and nutrients can exert profound effects on neuronal plasticity, modifying neural circuits and cellular properties to enhance and normalize function. Further, as there is increasing evidence for diet-induced epigenetic mechanisms contributing causally to the development of common chronic diseases (11, 12), greater knowledge of processes and players such as DNA methylation, histone modifications, and noncoding microRNAs will be needed to understand the relationships between energy dysregulation and therapeutic strategies to counter such impairment (11, 13).
This article explores the rationale and evidence for using the KD and related dietary treatments in a broad range of neurological disorders, and highlights novel mechanisms that have been implicated in their actions. However, it is important to recognize that much of the data discussed herein remain preliminary in nature. Nevertheless, the therapeutic potential for dietary therapies for neurological disorders remains almost limitless when viewed from the perspective of salvaging neuronal bioenergetic dysfunction (6, 8, 14).
KD AND EPILEPSY: HISTORICAL ASPECTS
The use of dietary manipulations to treat epilepsy, in particular controlling seizures through sustained fasting, dates back to the time of Hippocrates (15–17). In modern times, reports of modifying diets to treat seizures emerged in the early 20th century both in France and in the United States (15, 17–20). Importantly, in the 1920s, several researchers made significant discoveries regarding the physiological changes associated with the anti-seizure effects of starvation. At Harvard Medical School, Drs. Stanley Cobb and William G. Lennox conducted studies on changes in blood chemistry and metabolism during fasting in epileptic patients (15, 17, 21). They noted that the effects of fasting, such as increases in serum acidosis, were seen within 2–3 days coincident with seizure reductions, and were abolished with carbohydrate intake, but not with a fatty diet (15, 21). During this time, it was also recognized by Dr. R. T. Woodyatt at Rush Medical College that in the fasted state, the body produced ketone bodies [β-hydroxybutyrate (BHB), acetoacetate (ACA), and acetone] through the liver, and that a diet high in fats but low in carbohydrates could replicate this metabolic effect (17, 22). It was then suggested by Dr. Russell Wilder at the Mayo Clinic that consumption of a high-fat/low-carbohydrate diet, and the resulting increase in serum ketone bodies could possibly mimic the effects of starvation and he proposed that this diet should be tested in epileptic patients (23, 24). Subsequently, Dr. Wilder was the first to refer to this special high-fat diet as the “KD” (17). Collectively, Drs. Lennox, Cobb and Wilder believed the KD could be as effective as fasting and more appropriate for long-term suppression of seizures (15, 21, 24).
The first results demonstrating the beneficial effects of the KD on seizure reduction in epileptic children were published by Dr. M. G. Peterman, a pediatrician from the Mayo Clinic (25, 26). And during an era when anti-seizure drugs (ASDs) were scarce, the KD became quickly popularized in large medical centers. However, with the advent of diphenylhydantoin in 1938, the KD quickly fell out of favor due to the simplicity of prescribing an oral medication as opposed to a strict and exacting dietary regimen. Nevertheless, a variation of the KD, i.e., the medium-chain triglyceride (MCT) diet, emerged later as yet another dietary option for medically intractable epilepsy (27), and remains today as an alternative to the classic KD (28).
In recent years, there has been an explosion in clinical use of the KD and of its variants (29, 30), as well as in scientific interest regarding the mechanisms underlying their action (14, 31). Even beyond this resurgence in popularity for epilepsy, the diet has been increasingly found to exert protective effects in a variety of neurological diseases (3, 4) and new mechanistic insights have steadily emerged.
Efficacy in epilepsy: clinical studies
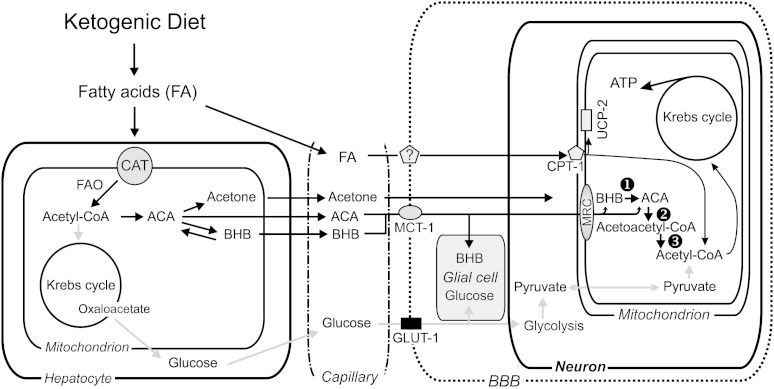
The classic KD utilizes a fat-to-carbohydrate plus protein ratio of 4:1 by weight, with approximately 90% of daily caloric intake coming from fat, and the inclusion of a small amount of protein (∼1 g/kg body weight) to ensure adequate growth in pediatric patients (32–34). A fat-to-carbohydrate ratio of 3:1 may be utilized based on patient’s needs and efficacy, which underscores the importance of the need for a dietician to implement and monitor the patient while on the diet (32–34). The classic KD is primarily based on ingestion of saturated long-chain FAs (32). Upon restriction of carbohydrates, ketogenesis occurs in the liver and ketone bodies are exported to the circulation (Fig. 1). Circulating concentrations of the major ketone bodies, BHB, ACA, and acetone, have been shown to significantly increase within 1–3 days after initiation of the KD.
Fig. 1.
Metabolic pathways involved in KD treatment. CAT, carnitine-acylcarnitine translocase; GLUT-1, glucose transporter-1; BBB, blood-brain barrier; CPT-1, carnitine palmitoyl transferase; numbered black circle 1, 3-hydroxybutyrate dehydrogenase; numbered black circle 2, succinyl-CoA3-oxoacid CoA transferase; numbered black circle 3, mitochondrial acetoacetyl-CoA thiolase; MRC, mitochondrial respiratory complex. Reprinted with permission (180).
A key aspect of the KD includes partial caloric restriction (CR). Prior to starting the diet, a fasting period of 24–48 h is typical (35), but the need for this requirement has been debated (36). An initial period of fasting may accelerate seizure control, and is therefore recommended for patients with a greater need for immediate seizure reduction (37, 38). A decrease in daily caloric intake of 10–25% is typical with the diet. Gluconeogenesis may result from consumption of excess calories, and therefore this slight reduction in calories is thought to increase the efficacy of the diet by maintaining ketosis (14, 39).
After initiation of the diet, seizure control slowly increases within the first few days to weeks (37, 38). This is believed to be due to the gradual elevation of circulating ketone bodies. However, because serum levels of ketone bodies do not correlate tightly with seizure control, it is unknown whether these substrates are directly responsible for the clinical effects observed (32). Despite this uncertainty, it is known that a break from the diet by ingestion of carbohydrates rapidly reverses the anti-seizure effects of the diet. In fact, the onset of seizures can occur less than an hour after administration of glucose (40).
Historically, the KD has been primarily used to treat epilepsy in pediatric patients. Efficacy in seizure control with the KD is assumed to be enhanced in younger patients, and is thought to reflect age-dependent changes in the expression of monocarboxylate transporters which transfer ketone bodies across the blood-brain barrier from the systemic circulation (41, 42) (Fig. 1). However, in spite of the challenges in maintaining the diet in older patients, mostly due to compliance issues, improved seizure control has been reported as well in adolescents and adults (43–45).
Despite numerous clinical reports documenting the efficacy of the KD against intractable epilepsy (32), very few class 1 and 2 studies exist. After nearly a century of use, the strongest evidence only became available as recently as 2008. In this randomized controlled trial of 145 children, aged 2–16 years old with daily seizures and who did not respond to at least two ASDs, it was shown that those who maintained the KD for greater than three months had a significant reduction in the mean percentage of baseline seizures (2). Seven percent of children on the KD demonstrated a greater than 90% reduction in seizures, compared with 0% on the control diet, and there was a more than 50% reduction in seizures in 38% of the patients on the KD versus 6% on the control diet (2).
As the KD is a high-fat diet, concerns exist regarding the development of dyslipidemia, insulin resistance, or increased serum biomarkers for CVD. However, this issue is controversial and definitive clinical data to either support or refute the development of risk factors for metabolic syndrome or CVD in patients on the KD do not exist. In the few studies that have examined CVD or metabolic syndrome risk factors with the KD, the results have been variable. A large study in children found elevated levels of total and LDL cholesterol and triglycerides, with a reduction in HDL cholesterol after 6, 12, and 24 months on the KD (46). However, a longer-term study in children on the KD, for at least 6 years, demonstrated no change in levels of cholesterol or triglycerides compared with baseline values (47). A short-term study in healthy men on the KD for 6 weeks found a decrease in fasting serum insulin levels without a change in estimated insulin resistance, as well as a trend toward increased HDL cholesterol without a change in total and LDL cholesterol concentrations (47). To date, it is not known if the KD leads to the accelerated development of atherosclerotic lesions, arterial stiffness, and vascular endothelial dysfunction in those patients that demonstrate dyslipidemia and elevated levels of CVD risk factors.
Efficacy in epilepsy: preclinical studies
The anti-seizure effects of the KD have been studied in multiple animal models of acute seizures. Rats fed the KD for nearly 2 weeks exhibited increased seizure thresholds after repeated intravenous infusion of pentylenetetrazole (PTZ), a chemoconvulsant that blocks γ-aminobutyric acid (GABA) type A receptors, whereas a 3 week treatment increased thresholds in response to a single exposure to both PTZ and flurothyl, a volatile convulsant (48). The KD also increased resistance in the 6 Hz model of epilepsy in mice, but the effects required 5 days on the diet and protection was lost after 3 weeks (49). Differences in age-dependent protection and latency to seizure control were shown in flurothyl-induced seizures in juvenile and adult mice (50). The KD increased time to the first generalized (clonic) seizure in juvenile mice after 7 and 12 days, but not after 3 days in young mice or after 15 days in adult mice. However, 15 days on the diet protected adult mice against second generalized (tonic extension) seizures, whereas juvenile mice showed no difference after 3, 7, and 12 days on the diet. Additionally, acute administration of the ketone ester R,S-1,3-butanediol ACA diester, which induces ketosis by elevating levels of BHB, ACA, and acetone, increased the latency to seizures induced by central nervous system oxygen toxicity in adult rats (51).
The effect of the KD on the development of chronic seizures has also been examined in various animal models. In an amygdala kindling model, rats were fed the KD 10 days after kindling was complete (52). Following 1 and 2 weeks on the diet, KD-fed rats demonstrated enhanced after-discharge threshold and increased seizure threshold, indicating a protective effect of the diet on seizure activity. However, this effect was lost during weeks 4 and 5. Visuospatial learning and memory, assessed with the Morris water maze during week 3, was not different between groups, and differences in after-discharge duration and clinical seizure duration were also similar at all time-points (52). In the kainic acid (KA) model, several studies have demonstrated variable effects of the KD on epileptogenesis. In young rats treated with KA, initiation of the KD 2 days post-KA reduced spontaneous recurrent seizures during the 8 week dietary treatment period compared with control-fed animals (53). A similar study in young rats treated with KA assessed the effect of the timing of KD initiation on seizure activity and learning and memory, and found the KD reduced spontaneous recurrent seizures when initiated 2 days but not 14 days post-KA (54). However, this did not result in enhanced performance in the Morris water maze test, as rats that started the KD 2 days after KA treatment demonstrated reduced learning and memory, followed by animals that began the KD 14 days post-KA and those fed a control diet (54). These and other studies emphasize the inherent variability of the effects of the KD as a function of the different rodent models used and the heterogeneous methods used for inducing seizures, as well as the dietary protocols adopted.
Variations on the KD
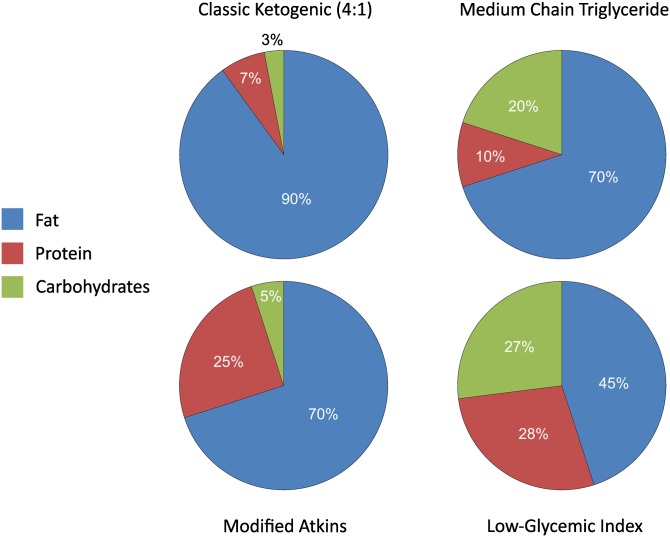
Notwithstanding the documented efficacy of the KD against seizure disorders, implementation remains challenging (e.g., poor compliance due to lack of palatability and concerns regarding long-term health consequences such as increases in cholesterol and triglycerides, slow growth in pediatric patients, etc.) (37, 55, 56). Hence, clinical researchers have sought alternative therapies that retain anti-seizure effects yet are devoid of these limitations. In addition to the MCT diet, two distinct variations on the KD theme include the modified Atkins diet (MAD) and the low-glycemic index treatment (LGIT) (57) (Fig. 2). Finally, there is CR, a dietary practice known to reduce the progression of many age-related diseases. Interestingly, this particular dietary strategy, which the KD was originally designed to mimic, has been an intense focus for researchers interested in the mechanisms underlying aging/longevity, neurological diseases, and a host of other conditions (58–60).
Fig. 2.
Comparison of four major KDs. Pie-charts depict relative proportion of calories provided by fat, protein, and carbohydrates for the classic KD (4:1 ratio by weight of fats to carbohydrate plus protein), the MCT diet, the MAD, and the LGIT.
The MCT diet
The MCT diet, which, as the name implies, utilizes MCTs as the fat component, was first described in 1971 and was reported to induce anti-seizure effects similar to the classic KD (27, 40). In an initial comparison of children under 10 years of age on a 60% MCT diet with the classic 3:1 KD, circulating levels of BHB were found to be similar (27, 40). MCTs produce a higher level of ketosis compared with long-chain triglycerides, and this allows for a decrease in the intake of these fats and a greater consumption of carbohydrates and protein on this modified diet (28).
The first long-term randomized trial compared the effects of the classic KD and the MCT diet in children with intractable epilepsy after 3, 6, and 12 months on these regimens (28). The 4:1 classic KD was used for the majority of the children, although some children were on a 3:1 ratio. The MCT diet was composed of ∼15% carbohydrates, ∼10% protein, 30% long-chain FAs, and 40–45% MCT fat. There were no differences between dietary groups in percent reduction in baseline seizures after 3, 6, and 12 months. Additionally, no differences were found between the two diets in those achieving seizure reductions greater than 50 or 90%. Serum levels of ACA and BHB were greater in children on the classic KD after 3 and 6 months, but only levels of ACA remained elevated in those on the KD after 12 months (28).
The MAD
The MAD was designed to mimic the high-fat KD while allowing more liberalized intake of protein, fluids, and calories to increase compliance, especially in adults (56) (Fig. 2). However, the MAD still relies on carbohydrate restriction, initially 10 g/day in children and 15 g/day in adults; this can be increased to 20–30 g/day after a couple months on the diet depending on seizure control (56). The MAD was originally developed at the Johns Hopkins Hospital and is considered to be a “modified” version of the original Atkins diet because weight loss is not the principal goal and protein intake is liberalized (56).
Seizure control with the MAD was originally shown in six children and adults with intractable epilepsy (61). In the five patients able to maintain ketosis for 6–24 months, three demonstrated a significant reduction in seizures and the opportunity to reduce concomitant ASDs (61). Following this initial report, the Dr. Robert C. Atkins Foundation sponsored the first prospective study on the MAD in 20 children who experienced at least three seizures per week and had prior use of at least two ASDs (62). In those that maintained the diet for at least 6 months, 4 became seizure-free, 13 (65%) had a greater than 50% reduction in seizures, and 7 (35%) demonstrated a greater than 90% decrease (62). Efficacy of the MAD on seizure control in adults was also shown in a prospective study of 30 adults with at least weekly seizures and previous use of at least two ASDs (55). Of those that maintained the diet, a greater than 50% reduction in seizures was found in 14 (47%) patients after 3 months and in 10 (33%) adults after 6 months (55).
The LGIT
The glycemic index (GI) is a measure of the rise in circulating levels of glucose in response to ingestion of a specific food. The index estimates how each gram of available carbohydrate in a food source will elevate levels of blood glucose compared with the consumption of pure glucose, which is assigned a GI of 100. The rationale for the LGIT was based on the clinical observation that the KD led to a sustained drop in blood glucose levels and on laboratory studies showing decreased seizure susceptibility in epileptic mice induced by CR (63). The LGIT prevents large postprandial increases in blood glucose, resulting in more stable circulating levels of glucose, and in early studies has been shown to provide seizure control in a broad range of patients (64, 65). This diet also allows for a greater intake of carbohydrates (∼40–60 g/day), but this is restricted to those foods with a GI of <50 (64, 65). Total caloric intake is determined based on patient’s needs, with 20–30% of calories coming from protein and the remaining 60% from fats (64) (Fig. 2).
In an initial study of 20 epileptic patients (5–34 years old), 10 out of 20 patients demonstrated a >90% seizure reduction while on the LGIT, despite achieving lower levels of circulating ketone bodies (65). In a larger cohort of children on the LGIT, 89% of whom failed to respond to at least three ASDs, seizure frequencies were reduced by greater than 50% in 42, 50, 54, 64, and 66% of patients after 1, 3, 6, 9, and 12 months of treatment, respectively (29). This study also showed an inverse relation between efficacy of the diet and serum glucose at certain time-points, but did not find a correlation between seizure reduction and circulating levels of BHB during follow-ups (29).
CR
As the KD was originally designed to mimic the effects of fasting, it was postulated that CR (or intermittent fasting) might provide similar results without the need for a large regular intake of fats. CR involves a reduction in total daily caloric intake below the ad libitum level without the risk of malnutrition (58, 66). CR is well-known to ameliorate many age-related and metabolic diseases, and is the only natural method known to increase life-span across multiple species (60). As such, comparisons of the KD and CR on seizure control have been performed in animal models of epilepsy. However, clinical studies involving CR or intermittent fasting for epilepsy have yet to be conducted (67).
A study in rats of varying ages treated with a mild calorically restricted standard chow diet (90% of recommended daily calories) and an isocaloric KD showed protection against PTZ-induced seizures (68). Rats fed the isocaloric KD exhibited a greater threshold to PTZ-induced seizures compared with CR-standard chow animals, which in turn demonstrated greater protection than those fed the same standard chow ad libitum (68).
In the EL genetic mouse model of epilepsy, CR (15 or 30%) delayed the development and frequency of seizures in both juvenile and adult animals (63). Additionally, when compared with a previous study by the same group that utilized the typical KD in EL mice (69), the authors found that the mild form of CR (15%) resulted in greater protection than the KD in juvenile mice. A follow-up study in adult EL mice showed that CR in the context of both a KD and a high-carbohydrate/low-fat diet reduced seizure susceptibility (70), leading the authors to conclude that restriction of calories, not the composition of the diet per se, is the key determinant of seizure control.
MECHANISTIC OVERVIEW: KETOGENESIS
Sustained intake of a high-fat/low-carbohydrate diet increases the rates of FA oxidation (FAO) and gluconeogenesis. The end product of FAO is acetyl-CoA, which can enter the TCA cycle and reacts with oxaloacetate to form citrate. However, under these metabolic conditions, oxaloacetate is also diverted to gluconeogenesis, and is therefore exported out of the mitochondria after conversion to aspartate by aspartate aminotransferase, in a process that requires glutamate, which is subsequently transformed to α-ketoglutarate. In the liver, increased production of acetyl-CoA results in levels that exceed the amount of oxaloacetate available for entry into the TCA cycle, and ketogenesis is then initiated when two acetyl-CoA molecules are combined to form acetoacetyl-CoA (Fig. 1). Acetoacetyl-CoA is then condensed with another molecule of acetyl-CoA to form HMG-CoA, in a nonreversible step catalyzed by the rate-limiting enzyme HMG-CoA synthase 2 (HMG-CoAS2). The ketone body ACA is then produced via the breakdown of HMG-CoA, releasing a molecule of acetyl-CoA. ACA can be further reduced to the ketone body BHB by BHB dehydrogenase in a reaction that is coupled to the ratio of the oxidized to reduced forms of NAD+, i.e., NAD+/NADH, and the spontaneous decarboxylation of ACA can yield acetone, another ketone body. BHB and ACA are the major ketone bodies, and levels of BHB have been shown to greatly exceed those of ACA in tissues and the circulation making it the predominant ketone body (71, 72). All three ketone bodies can then be exported from the liver into the circulation for uptake by tissues with high-metabolic demands, such as the heart, skeletal muscle, and the brain. In extra-hepatic tissues, BHB dehydrogenase catalyzes the first reaction in ketone body oxidation from BHB to ACA, which makes it an important regulator of mitochondrial NAD+/NADH status (73). In the second reaction of ketone body oxidation, ACA is then converted to acetoacetyl-CoA by succinyl-CoA3-oxoacid CoA transferase in a reaction that transfers a molecule of CoA from succinyl-CoA and therefore also yields succinate. It is important to note that deficiency of the enzyme succinyl-CoA3-oxoacid CoA transferase has been observed in rare cases and this can result in ketoacidosis, seizures, and other pathologies due to an inability to oxidize ketone bodies (73). In the final step of ketone body oxidation, mitochondrial acetoacetyl-CoA thiolase converts acetoacetyl-CoA to two molecules of acetyl-CoA for incorporation into the TCA cycle by citrate synthase (73).
Ketone bodies
The earliest demonstration of ketone bodies inducing anti-seizure effects was made by Keith in the 1930s. ACA was shown to protect against thujone-induced seizures in rabbits (74). This was followed decades later by two additional studies demonstrating in vivo anti-seizure effects of ketone bodies (75, 76). In the Frings audiogenic seizure-susceptible mouse (a model of sensory-evoked reflex seizures), acute administration of acetone and ACA led to an elevation in seizure threshold, whereas the more prevalent ketone body, BHB, had no effect on sound-induced seizures. In a separate study, acetone displayed dose-dependent anti-seizure effects in four diverse rodent models of epilepsy, including maximal electroshock seizures, subcutaneous PTZ, amygdala kindling, and the AY-9944 (an inhibitor of cholesterol biosynthesis) model of atypical absence seizures (76). Curiously, studies showing anti-seizure properties of the major ketone, BHB, have not yet been forthcoming.
Neurotransmitters and ion channel regulation
One hypothesis for KD action involves changes in the levels of certain neurotransmitters (NTs) as a result of altered synthesis and/or clearance from the synaptic cleft. The production of the major excitatory NT glutamate is paradoxically linked to the synthesis of the main inhibitory NT GABA via the action of the biosynthetic enzyme for GABA, glutamate decarboxylase (GAD). The KD has been proposed to alter the metabolism of glutamate, in response to ketosis, resulting in increased levels of GABA and enhanced inhibitory neurotransmission (77).
Glutamate is cleared from the synaptic space by astrocytes, which convert glutamate to glutamine through the action of the glial enzyme glutamine synthetase. Glutamine is then exported to neurons where it is hydrolyzed to glutamate and can then either be converted to GABA or transaminated to aspartate in a reaction that also requires oxaloacetate. Because the KD induces metabolic changes that require available oxaloacetate to condense with acetyl-CoA for incorporation into the TCA cycle, the production of aspartate from glutamate is reduced. This may result in enhanced flux through GAD to increase the synthesis of GABA (77).
In children fed the KD, cerebrospinal fluid levels of GABA were increased, but without a change in glutamate concentrations (78). However, rats fed the KD for 3 weeks showed a reduction in brain glutamate levels, with no change in GABA (79). Another study in rats fed the KD for 3 weeks found increased levels of glutamate and glutamine in the hippocampus, but this was also associated with an overall decrease in the transcripts of genes involved in synaptic transmission (48). Further, using both mild CR (i.e., 90% of daily energy requirements or 10% CR) and an isocaloric KD, investigators found significant increases in the mRNA expression of both isoforms of GAD (GAD65 and GAD67) in several brain regions and independent of ketogenic effects (80). Additionally, reduced levels of aspartate were found in a mouse model of ketosis, along with the expected increases in acetyl-CoA, with no change in the levels of GABA and glutamate (77). However, this same study also showed increases in glutamine and GABA upon infusion of the nitrogen donors alanine or leucine (77).
As another component of the NT theory, it was hypothesized that the KD might also enhance reuptake of glutamate from the synaptic cleft by astrocytes (81). However, in rats fed a KD for 4–5 weeks, there were no differences in the levels of brain glutamate transporters and no change in the reuptake activity of glutamate (81). With regard to glutamatergic neurotransmission, a recent study demonstrated a possible alternative mechanism through which the KD could suppress neuronal excitability. The ketone bodies, BHB and ACA, were shown to directly influence presynaptic glutamate release by directly competing with Cl− for allosteric activation of vesicular glutamate transporters, resulting in diminished release of glutamate (82). In the same study, direct application of the potassium channel blocker 4-aminopyridine to rat brain in vivo evoked seizures with concurrent secretion of glutamate, and these effects were blocked by ACA (82).
Notwithstanding these observations, whether ketone bodies exert direct effects on excitatory or inhibitory neurotransmission remains controversial. In the hippocampus, BHB and ACA did not acutely affect GABAA, α-amino-3-hydroxy-5-methylisoxazole-4-propionate, N-methyl-D-aspartate, kainate, or glycine receptors (83). However, ACA and BHB were later shown in vitro to reduce the spontaneous firing rate of GABAergic neurons in the substantia nigra pars reticulata, a putative subcortical seizure gate, and this action was dependent on opening of KATP channels and GABAB receptor activation (84). The same group then showed that the open probability of KATP channels in the hippocampus in vitro was enhanced in the presence of BHB (85). Further support for ketone body effects on neuronal excitability was recently demonstrated in sympathetic neurons in vitro. Here, BHB was shown to be an agonist of the FFA receptor 3, through which inhibition of N-type Ca2+ channels was documented (86). Interestingly, the short-chain FAs, acetate, propionate, and butyrate, are known agonists of FFA receptor 3.
Another link between the KD and KATP channels was recently revealed. BCL-2-associated agonist of cell death (BAD), a member of the Bcl-2 proteins that govern apoptotic cell death, was found to mediate a switch in the oxidative metabolism of glucose versus ketone bodies, as neurons and astrocytes from Bad−/− or BadS155A mice exhibited reduced mitochondrial oxidative metabolism of glucose, but enhanced mitochondrial respiration in the presence of BHB (87). Interestingly, this change in metabolism was implicated in neuronal excitability, as Bad−/− or BadS155A mice also demonstrated increased resistance to KA- and PTZ-induced seizures, effects that required the opening of KATP channels (87). While KATP channel opening induced by low ATP levels is indeed an intriguing mechanism that couples the metabolic state of the cell to neuronal excitability, the fact that the KD and ketone bodies actually increase ATP production needs to be reconciled with the KATP channel hypothesis (84, 88, 89).
Increases in the levels of the purine nucleotide adenosine may also potently modulate neuronal activity. Adenosine is produced from ATP and itself produces anti-seizure effects through activation of inhibitory adenosine A1 receptors (A1Rs) (90). As the KD increases levels of ATP (88, 89), elevated neuronal or astrocytic release and subsequent hydrolysis to adenosine in the synapse may subsequently result in enhanced activation of A1Rs (91). In mice, targeted deletion of A1Rs (i.e., A1R+/− and A1R−/−) or increased expression of adenosine kinase (Adk-Tg), an enzyme that enhances clearance of adenosine, causes spontaneous electrographic seizures (92). A 3 week treatment with a KD led to decreased electrographic seizures in Adk-Tg and A1R+/− mice, but not in animals missing A1Rs (A1R−/−), indicating that adenosine may be an important mediator of the KD’s anti-seizure effects (92).
Bioenergetic and mitochondrial changes
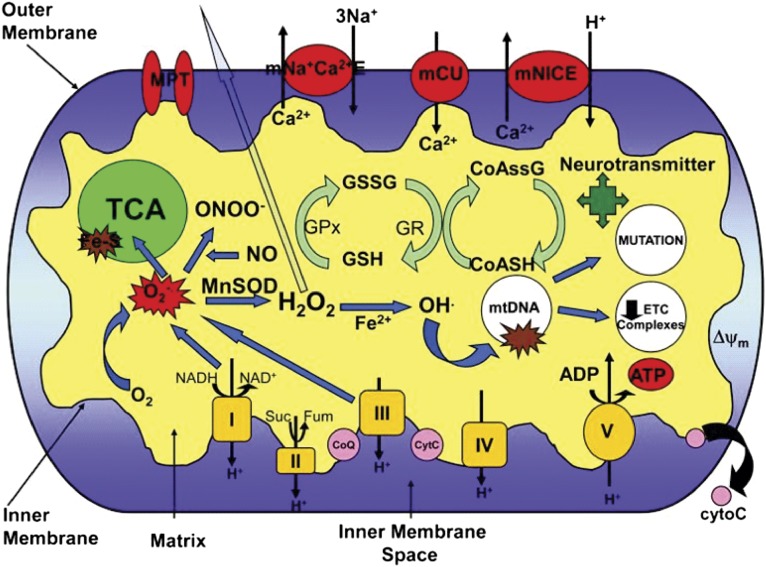
Pathological changes in mitochondrial energy metabolism and reactive oxygen species (ROS) production are known to occur with epileptogenesis, and intriguingly the KD has been found to profoundly affect these processes (93). In addition to enhancing energy reserves, ATP levels, and the expression of many enzymes involved in multiple metabolic pathways in the mitochondria, the KD has also been shown to increase mitochondrial biogenesis in the hippocampus (48). Additionally, multiple studies have demonstrated elevated antioxidant activity, diminished production of ROS, and decreased ROS-induced damage with the KD (6, 14, 94). Figure 3 summarizes the substrates and pathways linking mitochondrial redox changes to the TCA cycle and respiratory chain function. Impairment of mitochondrial bioenergetics capacity can critically affect apoptosis, neuronal excitability, and seizure susceptibility.
Fig. 3.
Mitochondrial function and neuronal excitability. Various aspects of the mitochondria can lead to impairment of its bioenergetic capacity affecting neuronal excitability, apoptosis, and an increase in seizure susceptibility. O2·, production by complex I and III of the ETC leads to the production of ONOO−, in a reaction with NO, and H2O2 through dismutation by the antioxidant MnSOD (SOD2). H2O2 is membrane-permeable and able to diffuse out of the mitochondria causing widespread oxidative damage. Excessive O2·, production also damages Fe-S-containing enzymes involved in the TCA cycle such as aconitase. OH· can be formed from H2O2 through Fenton chemistry and lead to further oxidative damage of macromolecules such as ETC complexes and mtDNA. Oxidative damage to mtDNA can lead to increased mutation rates and a decrease in ETC subunit expression encoded by the mitochondrial genome. Alterations in the redox status of GSH/GSSG and CoASH/CoASSG can cause an inability to protect against the deleterious effects of ROS. Modification of NT biosynthesis within the mitochondria can affect levels of neuronal excitability/inhibition. Oxidative damage to these targets can result in increased neuronal excitability resulting from decreased ΔΨ and ATP levels affecting the Na+/K+-ATPase and the release of cytochrome C, leading to apoptosis. mNa+C2+E, mitochondrial sodium calcium exchanger; mCU, mitochondrial calcium uniporter; mNICE, mitochondrial sodium independent calcium exchanger; CoASSG, CoA glutathione disulfide; GR, glutathione reductase; GPx, glutathione peroxidase; cytoC, cytochrome C; Suc, succinate; Fum, fumarate. Reprinted with permission (181).
Antioxidant activity, ROS, and the redox state
Several studies indicate that the KD decreases the production of ROS and limits ROS-mediated damage, possibly by enhancing antioxidant activity. One study in rats fed the KD for 8 weeks demonstrated tissue-specific alterations in antioxidant status and oxidative damage (95). Specifically, no changes were found in the cerebral cortex, however lipid peroxidation, assessed as thiobarbituric acid reactive substances, was increased in the cerebellum in KD-fed rats versus controls and this was associated with decreased total antioxidant reactivity in this tissue. Additionally, in the hippocampus, thiobarbituric acid reactive substances were unchanged and the overall antioxidant status was elevated with the KD, as indicated by enhanced total antioxidant reactivity and glutathione peroxidase activities despite a reduction in the activity of catalase (95). This study highlights the disparities in susceptibility to oxidative damage in various brain regions, possibly as a result of differential effects of the KD on antioxidant enzyme activities in certain tissues.
The KD has also been shown to change the mitochondrial production of hydrogen peroxide (H2O2) as a function of treatment duration. A decrease in substrate-driven mitochondrial H2O2 production was shown in rats after 3 weeks on the diet, and this was associated with increased mitochondrial GSH levels, depletion of which is known to occur with seizures (96). The increase in GSH was associated with elevated activity of the rate-limiting enzyme in GSH biosynthesis, glutamate cysteine ligase (GCL), and enhanced expression of the GCL catalytic subunit and the GCL modulatory subunit in rats fed the KD (96).
The increase in GSH and levels of the GCL subunits, GCL catalytic subunit and GCL modulatory subunit, observed by Jarrett et al. (96) prompted an investigation to examine the role of nuclear factor erythroid 2-related factor 2 (Nrf2), as activation of this redox-sensitive transcription factor is the primary mechanism that induces this antioxidant pathway (97). Nrf2 is activated by cellular stress and initiates transcription of a diverse set of genes, such as antioxidant defense, drug transporters, metabolic enzymes, and transcription factors, by binding to the antioxidant or electrophile response elements (98). This study demonstrated that production of mitochondrial-derived H2O2 was initially enhanced after 1 day on the diet, but was significantly decreased at the 3 week time-point (97). This initial increase in H2O2 was accompanied by an elevation in the lipid peroxidation product 4-hydroxy-2-nonenal (4-HNE), both of which stimulate Nrf2 activity through oxidation of the inhibitory binding partner Kelch-like ECH-associated protein 1 (Keap1), resulting in the release and nuclear translocation of Nrf2 (99). The acute rise in H2O2 and 4-HNE with the KD coincided with increased hippocampal nuclear expression of Nrf2 after 1 week on the KD, indicative of enhanced Nrf2 activation. Levels of Nrf2 remained elevated after 3 weeks on the KD and this was associated with increased activity of NAD(P)H:quinone oxidoreductase, a prototypical Nrf2 target. Although GSH was depleted in liver homogenates at all time-points examined (3 days, 1 week, 3 weeks), levels of reduced CoA (CoASH), a measure of mitochondrial antioxidant capacity, was decreased at 3 days, but elevated after 3 weeks. Likewise in the liver, nuclear extracts demonstrated increased Nrf2 expression after 1 and 3 weeks on the diet, accompanied by elevations in both NAD(P)H:quinone oxidoreductase activity and the expression of Nrf2 target heme oxygenase-1 after 3 weeks on the diet (97). Interestingly, a recent study found that increasing Nrf2 expression in a rat model of temporal lobe epilepsy decreased spontaneous seizures (100).
Acute application of the ketone bodies BHB and ACA in hippocampal slices enhanced catalase activity in response to H2O2 (89) and decreased oxidation of carboxy-2′,7′-dichlorodihydrofluorescein diacetate, a dye often used as an indicator of intracellular ROS (101). In isolated mitochondria, ACA and BHB have been shown to decrease ROS levels in response to glutamate by enhancing oxidation of NADH (102). Additionally, ACA and BHB reduced mitochondrial ROS both basally and in response to the ATP synthase inhibitor oligomycin (103).
A possible mechanism mediating the decrease in mitochondrial ROS production with the KD is enhanced expression of uncoupling proteins (UCPs). Increased activity of UCPs can diminish the mitochondrial membrane potential (ΔΨ) resulting in a decrease in ROS production, and this has been associated with increased resistance to KA-induced seizures (104). Additionally, FA can induce increases in UCP expression possibly through enhanced activity of transcription factors, such as the PPAR and forkhead box (FOX) families of transcription factors (105). In mice fed the KD, UCP activity was enhanced, and this was associated with increased levels of UCP2, UCP4, and UCP5 in the hippocampus (106). Additionally, ROS production, assessed in the presence of oligomycin to maximize ΔΨ, was reduced in mice fed the KD (106).
Recently, BHB was shown to be an inhibitor of class I histone deacetylases (HDACs) in vitro and in vivo (107), and this activity was associated with increased resistance to oxidative stress. Specifically, BHB increased acetylation of histone H3 lysine 9 and histone H3 lysine 14 and enhanced transcription of genes regulated by FOXO3A, including the antioxidant enzymes manganese superoxide dismutase (MnSOD) and catalase. Further, BHB (administered in vivo for 24 h via an osmotic pump) decreased protein carbonylation, 4-HNE, and lipid peroxides in the kidney. Although the authors did not report such effects in neuronal tissue or cells, it is possible that direct inhibition of HDACs and the ensuing transcriptional changes may mediate some of the antioxidant effects known to occur in the brain with the KD.
Mitochondrial permeability transition
ACA and BHB both blocked neuronal death in response to diamide, a mitochondrial permeability transition (mPT) activator, in a mechanism independent of oxidative stress. Additionally, ACA and BHB mimicked the effects of the mPT blocker, cyclosporin A, as all three increased the threshold for calcium-induced mPT opening (103). More recently, it was shown that prolonged in vitro “seizure-like” activity induced with low-Mg2+ in rat glioneuronal cocultures resulted in depolarization of ΔΨ and mPT opening, with subsequent cell death (108). These effects were reversed with mPT inhibition by cyclosporin A. In spite of these observations, the causal relationships between mPT, the KD, and epilepsy have yet to be clearly delineated.
Glycolytic restriction/diversion
A key feature of the KD is a relative reduction in glycolysis and an increase in nonglucose sources of fuel through the oxidation of FA and ketone bodies which ultimately feed the TCA cycle through a process known as anaplerosis (i.e., the replenishing of depleted metabolic cycle intermediates). Glycolytic restriction is thought to be an important mechanism mediating the anti-seizure properties of the KD. As mentioned above, CR has been shown in a mouse model of epilepsy to render anti-seizure, and possibly anti-epileptogenic, effects (70). The earliest clinical observation supporting this notion is the rapid reversal of seizure control upon ingestion of carbohydrates or glucose in patients on the KD (40). Additionally, studies utilizing labeled metabolic precursors have shown reduced oxidative metabolism of glucose (77, 79).
Use of glycolytic inhibitors has enabled further insights into this possible mechanism for seizure control. In vitro application of 2-deoxy-D-glucose (2-DG), an inhibitor of phosphoglucose isomerase, resulted in anti-seizure effects against the GABAA receptor antagonist bicuculline, 4-aminopyridine, and increased extracellular K+ (109). Additionally, in vivo administration of 2-DG reduced seizures induced by audiogenic and 6 Hz stimulation in mice (109) and chronically in a rat kindling model (109, 110). The anti-seizure effects of 2-DG may be partially mediated by changes in the expression of genes encoding brain-derived neurotrophic factor (BDNF) and its receptor TrkB, both of which are regulated by the activity of the transcription factor, neuron restrictive silencing factor (NRSF), which represses transcription by binding to the neuron restrictive silencing element in promoter regions (110). NRSF transcriptional repression was enhanced by 2-DG, and this was associated with a reduction in acetylation and an increase in methylation of histone H3 lysine 9 at the neuron restrictive silencing element promoter, epigenetic modifications associated with suppression of gene transcription. NRSF-mediated repression required an interaction with the transcriptional corepressor, carboxyl-terminal binding protein (CtBP), that was disrupted with increasing concentrations of NADH, a cofactor that is elevated upon increased glycolytic flux. This suggests that the anti-seizure actions of 2-DG may be mediated by a decrease in cytosolic and nuclear levels of NADH and subsequent influences on histone modifications (110).
Interestingly, changes in histone acetylation have also been shown to be mediated by the activity of ATP-citrate lyase, which converts glucose-derived citrate to acetyl-CoA (111). Enhanced flux of acetyl-CoA from ATP-citrate lyase increased acetylation of H3 and this resulted in increased expression of glycolytic enzymes. This effect was found to be specific for acetyl-CoA produced from glycolysis, as changes in histone acetylation did not occur in cells supplemented with FAs under glucose-replete conditions (111).
Acetyl-CoA has yet another role as the cofactor for acetylation of the ε-lysine residues on histones and nonhistone enzymes by lysine acetyltransferases (KATs) (112). Three families of KATs have been found to alter the acetylation state of a diverse group of substrates with varying influences on cellular functions (112). However, these three families of KATs have primarily been localized to the nucleo-cytoplasmic compartments and a mitochondrial KAT has yet to be confirmed despite estimates that 65% of mitochondrial proteins are acetylated, especially those involved in energy metabolism and antioxidant defenses (112, 113). Recently, it was shown that the high alkaline pH of the mitochondria in the presence of elevated levels of acetyl-CoA allows for nonenzymatic acetylation to occur in vitro (114). This has led to speculation that compartmental differences in acetyl-CoA concentration can direct changes in acetylation (112).
Fructose-1,6-bisphosphate also inhibits glycolysis by diverting the metabolism of glucose to the pentose phosphate pathway and also affords broad anti-seizure effects in vivo (115). Fructose-1,6-bisphosphate was shown to provide the greatest protection when compared with the KD, 2-DG, and the commonly prescribed ASD valproic acid in the pilocarpine-, KA-, and PTZ-induced seizure models in rats (115). Surprisingly, the KD did not demonstrate anti-seizure activity in this study, and 2-DG was only protective in the pilocarpine model, whereas valproic acid demonstrated limited protection in all three models.
FAO
Intake of a high-fat diet, such as the KD, inherently increases the rate of FAO and this also changes the levels and types of PUFAs in the circulation, liver, and brain. These alterations in PUFAs are a result of endogenous production and export of these FAs into the circulation, because large quantities of these lipids are not a typical component of the KD (116). PUFAs are known to possess neuroprotective properties (117); therefore, it has been speculated that this lipid species may mediate the anti-seizure effects of the KD.
In pediatric patients with epilepsy, 3–4 weeks of KD treatment led to elevations in circulating levels of BHB, cortisol, and FFAs (116). Most PUFAs were also increased in the serum, including the triglyceride and phospholipid forms of linoleic acid, arachidonic acid (AA), and DHA; triglyceride levels of stearic acid; and palmitic acid in phospholipids (116). Additionally, these alterations in FAs were associated with seizure reduction in 78% of the children. Interestingly, seizure control was correlated with circulating AA levels, but not electroencephalogram changes (116).
Whether PUFA supplementation can render anti-seizure effects remains controversial. Supplementation with 5 g of omega-3 PUFAs for 6 months appeared to reduce the frequency and severity of seizures in a small observational study (118). However, in a 12 week randomized placebo-controlled parallel group study in adults with epilepsy, administration of EPA and DHA (1 g EPA, 0.7 g DHA daily) reduced seizure frequency for the first 6 weeks of treatment, but this effect did not persist in spite of sustained increases in DHA and EPA and decreases in AA and linoleic acid in the plasma (119). In a further randomized, blinded trial of PUFA supplementation (EPA plus DHA, 2.2 mg/day in a 3:2 ratio over 12 weeks) in adults with uncontrolled epilepsy, there was a lack of clear efficacy when compared with the placebo (120). However, it is unclear whether different doses, duration, or ratios of PUFAs might have been effective.
In rats fed the KD, there were marked reductions of PUFA levels in plasma and adipose tissue, but enhanced mobilization of the PUFAs AA and DHA to the liver and brain (121). This was accompanied by an initial increase in the plasma levels of BHB, followed by a reduction by day 10 of the diet. Following a calorie-restricted KD, mRNA expression of the rate-limiting enzyme for ketone body production, HMG-CoAS2, was found to increase in both liver and brain, in contrast to isocaloric standard chow which showed enhanced expression only in the liver (122). Collectively, these and other animal studies suggest that diet-induced changes in brain content and metabolism of PUFAs may be important contributors to the anti-seizure effects of the KD (123).
Bioenergetic reserve and mitochondrial respiration
Alterations in bioenergetic metabolites by the KD have been shown in several animal studies. DeVivo et al. (88) first demonstrated significant increases in ATP and the ATP/ADP ratio (and other parameters of bioenergetic reserve capacity) in the brain of rats fed the KD for 3 weeks. Further, decreases in creatine with no change in phosphocreatine were noted in this study. However, while a later study failed to confirm elevations in ATP and ATP/ADP ratios, the KD was shown to increase the ratio of phosphocreatine-to-creatine (48). In vitro studies have further supported the concept that KD metabolites can enhance bioenergetic function. For example, BHB and ACA prevented depletion of ATP in hippocampal slices in response to H2O2 and inhibitors of complex I (rotenone) and complex II (3-nitropropionic acid) of the electron transport chain (ETC) (89). In a mouse model of global cerebral ischemia, administration of BHB immediately following bilateral common carotid artery ligation ameliorated the decline in tissue levels of ATP (124). Thus, collectively, there is both in vivo and in vitro evidence for the KD and ketone bodies enhancing ATP production in the brain.
Consistent with the KD’s favorable effects on energy production, changes in the expression of enzymes involved in metabolic pathways have also been reported. Two studies revealed changes in gene expression in the hippocampus of mice and rats fed the KD (48, 125) and both demonstrated enhanced expression of numerous enzymes involved in mitochondrial metabolism (125), such as the TCA cycle and oxidative phosphorylation (48). However, there was not complete concordance with respect to the gene expression changes for all metabolic enzymes (48).
Mitochondrial respiration and ETC activity have been shown to be elevated in animals fed the KD or with in vitro application of ketone bodies. BHB increased oxygen consumption and ATP production in purified mitochondria in the presence of two inhibitors of complex I, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) and rotenone (126). Further, in a model of glutamate excitotoxicity, ACA and BHB increased complex I-driven oxygen consumption through increased NADH oxidation (102).
TCA cycle effects and anaplerosis
As numerous studies have shown that the KD can increase ATP levels, bioenergetic capacity, and transcription of enzymes in energy-producing pathways, it is also likely that levels of metabolic intermediates may be altered. Specifically, the KD may enhance neuronal ATP production through refilling of TCA cycle intermediates from the increase in acetyl-CoA levels from the oxidation of ketone bodies. These actions may contribute to anti-seizure effects. In this regard, the anaplerotic substrate, triheptanoin, has been shown to raise seizure thresholds in mouse seizure models, and to help restore levels of TCA intermediates (127, 128). Further, replenishment of the TCA cycle may counter seizure-induced energy failure and augment inhibitory neurotransmission (129). For example, α-ketoglutarate, which serves a dual function as a TCA cycle intermediate and as the immediate precursor to glutamate which can be converted to GABA, directly links anaplerosis to neuronal excitability (129).
ACTIVATION OF ENERGY-SENSING SIGNALING PATHWAYS
It is well-established that multiple signaling pathways have evolved to sense states of diminished energy stores, such as seen during exercise and CR, and that activation of these pathways results in restoration of cellular homeostasis and integrity (60, 130). Data regarding the association of the KD with these energy-sensing pathways are limited, but the similarities between the protective mechanisms evoked by the KD and those known to be influenced by these pathways indicates substantial overlap in their mechanisms and downstream effects.
PPARs
The PPAR family of nuclear receptors represents one signaling pathway that may mediate some of the beneficial effects of the KD (131). PPARs are transcription factors that bind to the PPAR response element of promoter regions. They include three isoforms: PPARα, PPARγ, and PPARβ/δ (131). FAs are endogenous ligands for PPARs and PPAR agonists are used in the treatment of lipid disorders such as type II diabetes mellitus and high cholesterol (131). The induction of FAO is a known metabolic effect of PPAR activation, which renders these transcription factors an attractive mediator for the clinical effects of the KD.
Fenofibrate, a PPARα agonist, was shown to exhibit anti-seizure properties similar to the KD (132). Rats fed the KD and a diet containing fenofibrate showed increased threshold to PTZ-induced seizures and an increased latency to spike-and-wave discharges lasting longer than 5 min in the lithium-pilocarpine model, compared with control-fed animals (132). In a separate study, acute injection of the PPARγ agonist (N-[9-fluorenylmethoxycarbonyl]-)-l-leucine protected adult magnesium-deficient mice against audiogenic seizures, and this was reversed by administration of the PPARγ antagonist GW9662 (133). In contrast, FMOC-L-leucine did not exhibit anti-seizure activity in another seizure model, the 6 Hz test, and another PPARγ ligand, rosiglitazone, did not reduce audiogenic seizures (133). Rosiglitazone has been shown to reduce oxidative stress in the lithium-pilocarpine model of epilepsy, and this was associated with an amelioration of neuronal death in the hippocampus and an enhancement of superoxide dismutase (SOD) activity and levels of GSH, as well as a reduction in the Nrf2 target, heme oxygenase-1 (134). Further, the PPARα-selective agonist ciprofibrate was shown to selectively increase mRNA levels of HMG-CoAS2, the rate-limiting enzyme in the production of ketone bodies, and that of two other known PPARα targets, acyl CoA oxidase and medium-chain acyl-CoA dehydrogenase (135).
AMP-activated kinase
AMP-activated kinase (AMPK) is induced by low levels of AMP and inhibited by high concentrations of ATP; therefore, AMPK functions as a direct sensor of the energy state of the cell. Activation of AMPK leads to the phosphorylation of multiple substrates, resulting in concurrent inhibition of anabolic pathways and increases in catabolic metabolism to enhance the production of ATP (136). These effects are known to include an upregulation of FAO and increased mitochondrial biogenesis (136). Similar to PPARs, agonists of AMPK are used to treat type II diabetes mellitus and metabolic syndrome (136).
The KD increased AMPK activity in the liver and skeletal muscle of mice, and this was associated with increased gene expression of enzymes involved in FAO and a reduction in transcript levels of enzymes in lipid synthesis pathways in the liver (137). Increased activation of AMPK was also found in the liver of rats on the KD, but this was not associated with enhanced activation in the brain (138).
Mammalian target of rapamycin
The mammalian target of rapamycin (mTOR) is another protein kinase that exerts multiple effects on energy metabolism through the actions of two distinct complexes, mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2) (139). Unlike the PPARs and AMPK, however, mTOR is activated during high-energy states and this results in an induction of protein synthesis and mRNA translation, among other actions that promote growth and cellular proliferation (139). Importantly, AMPK inhibits mTORC1 through direct phosphorylation of both a subunit of this complex and an upstream regulatory protein (139). In rats, the KD inhibited activation of the mTOR pathway in the liver and brain (138). Additionally, in the KA model, enhanced activation of mTOR was found in the hippocampus of rats fed a standard diet and this effect was blocked after 7 days on the KD (138). Given that mTOR inhibition is believed to retard the processes of epileptogenesis (140) and that the KD can decrease mTOR signaling, it is conceivable that metabolism-based treatments could render anti-epileptogenic effects.
Sirtuins
The sirtuins (SIRTs) 1–7 are a family of NAD+-dependent enzymes known to influence multiple aspects of cellular homeostasis, including metabolism and antioxidant activity. The SIRTs were originally classified as class III HDACs; however, it is now known that individual isoforms also demonstrate desuccinylase, demalonylase, and ADP-ribosyltransferase activities (60). The SIRTs are direct sensors of the energetic and redox state of the cell, principally through NAD+, which is required for their catalytic activity. Additionally, the beneficial effects of CR may be mediated by the SIRTs, as well as the AMPK and mTOR pathways (66, 141). The diversity and abundance of their histone and nonhistone substrates, as well as their specific localization within different cellular compartments reflect the extent of their broad influence on energy metabolism (66, 142). Collectively, the SIRTs are known to enhance oxidative phosphorylation and reduce glycolysis, in addition to providing increased resistance to oxidative stress (60). The substantial overlap in the activities of these regulators of cellular homeostasis with the known mechanisms of the KD suggests possible involvement of the SIRTs in the effects of this dietary modification. Certainly, the observation that BHB is an HDAC inhibitor (107) is compelling in this regard.
One study examined levels of SIRT1 and SIRT3 in interscapular brown adipose tissue from mice on the KD for 1 month (143). Protein expression of SIRT1 was elevated, but levels of SIRT3 were reduced compared with mice on a standard diet (143). A separate study examining gene expression changes in the hippocampus of rats fed the KD for 3 weeks found increased levels of Sirt5, although this was reported in the supplemental results section and not discussed by the authors (48).
Further, SIRT3 and SIRT5, major regulators of mitochondrial energy metabolism, exhibit extensive regulation of the acetylation and succinylation state of numerous enzymes in the TCA cycle, FAO, and ketogenesis (144, 145). Interestingly, the activity of the rate-limiting enzyme in ketogenesis, HMG-CoAS2, is regulated by both deacetylation through SIRT3 and desuccinylation by SIRT5, two posttranslational modifications thought to inhibit enzymatic activity (144–146). Finally, separate studies in Sirt3−/− and Sirt5−/− mice demonstrated reductions in the circulating levels of BHB under fasting, but not basal, conditions (145, 146).
EVIDENCE AND IMPLICATIONS FOR OTHER NEUROLOGICAL DISORDERS
Mitochondrial dysfunction in neurological diseases
Mitochondrial dysfunction has recently been recognized as a common mechanism underlying many neurological disorders (7, 8, 147, 148). The role for mitochondrial energetics and signaling as important mediators of neuronal death, a common feature of neurodegenerative diseases (149), is increasingly being understood. Specific pathological changes include a reduction in ATP production via oxidative phosphorylation or direct inhibition of specific complexes of the ETC, and elevations in the production of mitochondrial-derived ROS, which can alter cellular signaling. Additionally, given the similar mechanisms of these processes in neurodegenerative diseases and the beneficial effects of the KD and ketone bodies on multiple aspects of mitochondrial function, there has been an increase in the use of metabolism-based treatments for neurological diseases (3, 4).
AD
AD is characterized by an accumulation of neurofibrillary tangles and amyloid plaques comprised of misfolded aggregates of tau and amyloid-β (Aβ) proteins, respectively, resulting in neuronal death (130). AD is an age-related neurodegenerative disease and is known to arise from both genetic and environmental influences. Older adults with AD are at increased risk for the development of epilepsy and similar mechanisms, such as deficits in mitochondrial energy metabolism and elevations in oxidative stress, are thought to contribute to both pathological states (130, 150). Therefore, there is growing interest in the use of the KD to delay the progression of AD.
In fasted patients with AD or mild cognitive impairment, acute ingestion of a MCT drink increased BHB levels and cognitive function compared with the placebo (151). Further, in a separate study of older adults with mild cognitive impairment, a low-carbohydrate (5–10% of calories) diet for 6 weeks enhanced a measure of verbal memory versus preintervention scores, whereas there was no change in those assigned to the high-carbohydrate (50% of calories) diet (152). Additionally, the improvement in memory in those on the low-carbohydrate diet was positively correlated with levels of urinary ketones (152). Finally, Henderson et al. (153) treated 152 patients having mild-to-moderate AD daily with 20 g of MCT for 3 months, and found that MCT-treated patients [lacking the apoE epsilon 4 (APOE4) allele] achieved significantly higher Alzheimer’s Disease Assessment Scale-cognitive subscale scores at two different time-points versus placebo-treated controls. Interestingly, postdose serum BHB levels correlated positively with improvement in Alzheimer’s Disease Assessment Scale-cognitive subscale scores.
However, in a mouse model of AD, consumption of a KD high in saturated FAs for 43 days reduced total levels of Aβ but did not affect cognitive function (154). The lack of an effect on cognitive function in this study could be a result of the short duration of the diet or due to a reduction in the level of ketosis from day 16 to day 27 following the introduction of standard chow to mitigate the level of weight loss in mice fed the KD. In vitro, BHB reduced hippocampal neuronal cell death from exposure to the proteolytic fragment of the β-chain of the amyloid precursor protein, Aβ1-42 (155). Additionally, it has been shown that a ketone ester diet lessens amyloid and tau pathologies and improves learning and memory performance in a mouse model of AD (156). Taken together, there are an increasing number of studies pointing to the neuroprotective benefits of the KD and its metabolic substrates.
PD
The hallmark neuropathological finding in PD is the degeneration of dopaminergic neurons in the substantia nigra. A main mechanism thought to contribute to this excitotoxic cell death is defects in complex I of the ETC (149). Hence, it follows that metabolism of ketone bodies may circumvent this deficit and allow for oxidative phosphorylation to occur, possibly by enhancing the activity of complex II in the ETC (3). This was shown in vitro in isolated brain mitochondria from mice as BHB ameliorated the decline in oxygen consumption and ATP production in response to 1-methyl-4-phenylpyridinium, the active metabolite of MPTP, a complex I inhibitor commonly used to model PD, and rotenone, another inhibitor of complex I, and these effects were blocked by inhibitors of complexes II and III, 3-nitropropionic acid and antimycin A, respectively (126). The authors speculated that the ability to bypass complex I inhibition was due to the metabolism of BHB into succinate, which can feed directly into complex II and was also shown to be elevated in vivo in mice with BHB infusion and complex II inhibition (126). Additionally, these authors also showed that following treatment with MPTP, BHB reduced dopaminergic neuronal cell death in substantia nigra pars compacta in vivo, and this was associated with increased levels of dopamine and improved rotarod performance, demonstrating an attenuation of motor deficits (126). Further, BHB has also been demonstrated to decrease cell death in vitro in mesencephalic neurons exposed to 1-methyl-4-phenylpyridinium (155).
In PD patients treated with the KD for 4 weeks, scores on the Unified Parkinson’s Disease Rating Scale improved, although this study had a very small sample size and did not include controls (157). Moreover, this study showed that switching MUFAs and PUFAs for saturated fats prevented the increase in cholesterol expected from intake of a high-fat diet (157). In a prospective study of older adults, increased consumption of total fats, MUFAs, and PUFAs was associated with a lower risk of PD (158).
Brain cancer
Cancer cells are known to undergo dramatic metabolic alterations, including a preference for ATP production via glycolysis and enhanced lactic acid production, despite the presence of oxygen for oxidative phosphorylation (159). This shift in metabolism was first noted by Otto Warburg and was subsequently coined the “Warburg effect” (160). Defects in mitochondrial function resulting in diminished oxidative phosphorylation are thought to be main contributors to cancer cell metabolism. Because cancer cells preferentially use glucose for energy, and the KD reduces glycolytic flux and enhances oxidative metabolism, high-fat KDs may represent potentially viable treatments to limit oncogenesis (161). Indeed, this conceptual approach was demonstrated in a compelling manner in a mouse astrocytoma model, indicating that plasma glucose is an accurate predictor of tumor growth more than the specific origin of dietary calories (162).
In a later study employing a mouse model of malignant glioma, the KD decreased tumor growth and improved survival, and this was associated with a reduction in tissue levels of ROS (163). Additionally, the KD induced gene expression changes in the tumor tissue to more closely resemble the pattern found in normal brain. Further, the KD also caused an upregulation of enzymes involved in oxidative stress resistance, such as glutathione peroxidase 7 and peroxiredoxin 4, in tumor tissue, but not normal specimens (163). The authors speculated that the effects of the KD are not just due to reductions in glucose, but alterations in cellular signaling pathways associated with enhanced homeostasis, and this leads to increased survival and reduced tumor growth.
The same research group later showed in the identical model that administration of Ketocal®, a commercially available 4:1 KD, greatly increased survival (164). When Ketocal® was given in conjunction with radiation therapy, a supra-additive effect was found as visualization of tumor cells diminished below the levels of detection in 9 out of 11 animals. Further, when these animals were placed back on a standard diet, no regrowth of tumors was found after 100 days (164).
In a more recent immunohistochemical analysis of malignant gliomas compared with adjacent “normal” brain tissue from adults, expression levels of cytosolic glycolytic enzymes and mitochondrial ketolytic enzymes were found to be altered (165). The most frequent pattern observed in the brain tumor tissue was an upregulation of the cytosolic glycolytic enzymes with a reduction in the levels of the mitochondrial ketolytic enzymes. This study suggests the potential utility of the KD as a therapeutic intervention in patients with low levels of ketolytic enzymes in tumor tissues.
Neurotrauma
Acute neurotrauma results in metabolic changes in the brain, including diminished glycolysis, and also activates excitotoxic and neuroinflammatory cascades (166, 167). In spite of the glycolytic restriction observed, the KD, through a multiplicity of other neuroprotective mechanisms, may counter the pathophysiological changes seen after traumatic brain injury (TBI). In an animal model of TBI, cortical contusion volume was reduced in rats fed the KD (168). Further, infusion of BHB 3 h after injury increased cerebral uptake of BHB and ameliorated the injury-induced reduction in cortical ATP levels (169). A recent study in a rat model of TBI demonstrated that the KD decreased mRNA levels of Bax, a Bcl-2 protein mediating apoptosis, and reduced cerebral edema and apoptosis (170). Additionally, initiation of the KD 4 days before insulin-induced hypoglycemia reduced neuronal death in rats (171). Further support for a metabolic approach toward TBI treatment is provided by Davis et al. (172), who showed that fasting for 24 h following controlled cortical impact in rats resulted in increased tissue sparing and improvements in mitochondrial function, and that these effects were a result of ketones and not hypoglycemia.
ALS
Mitochondrial dysfunction is also thought to contribute to the progression of ALS, a disease characterized by degeneration of motor neurons in the cortex and spinal cord (173). In ALS mice, the KD improved motor function, as evidenced by increased time to failure on rotorod performance and this was associated with preservation of motor neurons in the ventral horn of the spinal cord (174). In mitochondria isolated from the spinal cord of a transgenic mouse model of ALS (SOD1-G93A), addition of BHB in vitro enhanced ATP production and this effect was maintained in the presence of the complex I inhibitor rotenone, but not the complex II inhibitor malonate (174). Additionally, the preservation of ATP levels by BHB was associated with increased neuronal survival in the presence of rotenone, but not malonate (174).
Pain and inflammation
Multiple lines of experimental evidence suggest shared fundamental mechanisms responsible for chronic pain syndromes and epilepsy, particularly the involvement of cellular membrane-bound ion channels (175). Specifically, both chronic pain and epilepsy are characterized by enhanced neuronal excitability, and whatever the relevant mechanisms may be, metabolic approaches toward treatment (e.g., the KD, inhibition of glycolysis through fasting or 2-DG, etc.) can alleviate neuropathic pain (14, 176). Additionally, ASDs are often prescribed for chronic pain, further suggesting similarities in the pathophysiology of these two disorders (177). In juvenile and adult rats, the KD reduced pain, as assessed by increased latency to hind-paw withdrawal in a test of thermal nociception, and inflammation, as measured by hind-paw swelling in response to injection of the immune-potentiator, Freund’s complete adjuvant (176). Despite attaining similar levels of circulating ketone bodies, the anti-inflammatory and hypo-algesic effects of the KD were more prominent in juvenile mice (176).
Other disorders
There are a number of other reports suggesting that the KD (or other dietary manipulations) can effectively treat diverse neurological disorders such as autism and migraine. In the BTBR mouse, an inbred model that recapitulates the core behavioral features of autism spectrum disorder, and that does not exhibit altered susceptibility to seizures, the KD increased sociability and communication while reducing repetitive behaviors (178). A small study examined the use of the MAD in treating chronic headaches in adolescents and demonstrated reduced headache severity in the three patients that completed the study (179). However, the MAD did not reduce headache frequency; unfortunately, the small study size and limited number of patients completing the 3 month study prevent any definitive conclusions from being reached (179).
SUMMARY
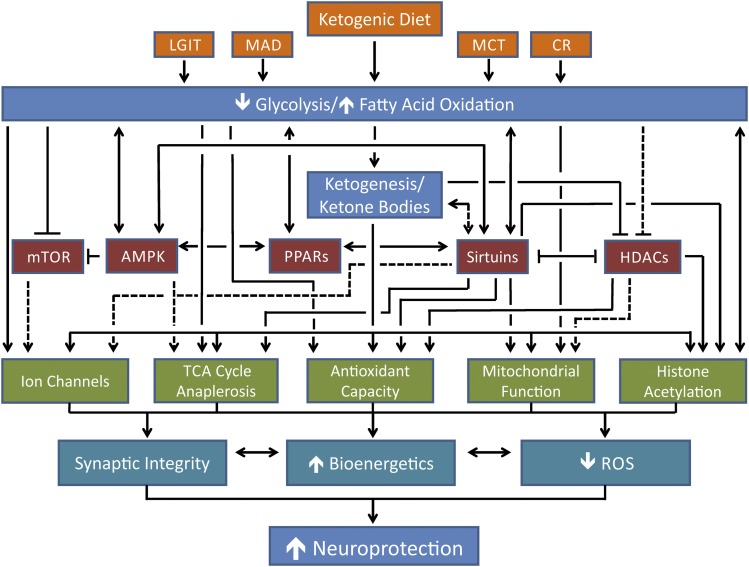
The KD is a broad-spectrum therapy for multiple forms of epilepsy in both children and adults. The utility of the KD and variations of this diet for the treatment of a variety of neurodegenerative disorders suggests common central mechanisms that restore imbalances in energy metabolism (Fig. 4). The numerous mechanisms known to partially mediate the effects of the KD (such as increases in FAO, reductions in glycolysis, an enhancement of the cellular responses to oxidative stress, etc.) indicate that manipulation of these specific pathways may represent an attractive paradigm for experimental therapeutics. Specifically, bioenergetic substrates and enzymes may be desirable drug targets for the treatment of many neurological diseases. Additionally, the signaling pathways that evolved to sense the cellular energetic state and provide resistance to metabolic stress may provide the best means to mimic the KD. Future research in this burgeoning area may lead to the elucidation of additional novel mechanisms that mediate the pleiotropic neuroprotective effects of the KD.
Fig. 4.
Proposed mechanisms for the neuroprotective effects of the KD and its variants. The dietary interventions are shown in orange; the metabolic effects of the diets are shown in blue; the energy-sensing pathways that may mediate the effects of the dietary alterations are shown in red; the cellular effects resulting from the diets and/or the energy-sensing pathways are shown in green; and the broad protective effects of the diets and the resulting cellular effects are in shown cyan. Solid black lines indicate links proven in the literature; dashed black lines represent possible, but as yet unproven, links. Further details are provided in the text.
Footnotes
Abbreviations:
- AA
- arachidonic acid
- ACA
- acetoacetate
- AD
- Alzheimer’s disease
- ALS
- amyotrophic lateral sclerosis
- AMPK
- AMP-activated kinase
- ASD
- anti-seizure drug
- Aβ
- amyloid-β
- A1R
- adenosine A1 receptor
- BHB
- β-hydroxybutyrate
- CoASH
- reduced CoA
- CR
- caloric restriction
- ETC
- electron transport chain
- FAO
- fatty acid oxidation
- GABA
- γ-aminobutyric acid
- GAD
- glutamate decarboxylase
- GCL
- glutamate cysteine ligase
- GCLM
- glutamate cysteine ligase modulatory subunit
- GI
- glycemic index
- HDAC
- histone deacetylase
- HMG-CoAS2
- HMG-CoA synthase 2
- KA
- kainic acid
- KAT
- lysine acetyltransferase
- KD
- ketogenic diet
- LGIT
- low-glycemic index treatment
- MAD
- modified Atkins diet
- MCT
- medium-chain triglyceride
- MnSOD
- manganese superoxide dismutase
- mPT
- mitochondrial permeability transition
- MPTP
- 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- mTOR
- mammalian target of rapamycin
- mTORC1
- mammalian target of rapamycin complex 1
- mTORC2
- mammalian target of rapamycin complex 2
- Nrf2
- nuclear factor erythroid 2-related factor 2
- NRSF
- neuron restrictive silencing factor
- NT
- neurotransmitter
- PD
- Parkinson’s disease
- PTZ
- pentylenetetrazole
- ROS
- reactive oxygen species
- SIRT
- sirtuin
- SOD
- superoxide dismutase
- TBI
- traumatic brain injury
- UCP
- uncoupling protein
- VPA
- valproic acid
- 2-DG
- 2-deoxy-D-glucose
- 4-HNE
- 4-hydroxy-2-nonenal
- ΔΨ
- mitochondrial membrane potential
This work is supported by grants from the NIH RO1 NS039587 and NS086423 (M.P.), and the Canadian Institutes of Health Research (J.M.R.).
REFERENCES
- 1.Vining E. P., Freeman J. M., Ballaban-Gil K., Camfield C. S., Camfield P. R., Holmes G. L., Shinnar S., Shuman R., Trevathan E., Wheless J. W. 1998. A multicenter study of the efficacy of the ketogenic diet. Arch. Neurol. 55: 1433–1437. [DOI] [PubMed] [Google Scholar]
- 2.Neal E. G., Chaffe H., Schwartz R. H., Lawson M. S., Edwards N., Fitzsimmons G., Whitney A., Cross J. H. 2008. The ketogenic diet for the treatment of childhood epilepsy: a randomised controlled trial. Lancet Neurol. 7: 500–506. [DOI] [PubMed] [Google Scholar]
- 3.Stafstrom C. E., Rho J. M. 2012. The ketogenic diet as a treatment paradigm for diverse neurological disorders. Front. Pharmacol. 3: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barañano K. W., Hartman A. L. 2008. The ketogenic diet: uses in epilepsy and other neurologic illnesses. Curr. Treat. Options Neurol. 10: 410–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waldbaum S., Patel M. 2010. Mitochondrial dysfunction and oxidative stress: a contributing link to acquired epilepsy? J. Bioenerg. Biomembr. 42: 449–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Milder J., Patel M. 2012. Modulation of oxidative stress and mitochondrial function by the ketogenic diet. Epilepsy Res. 100: 295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin M. T., Beal M. F. 2006. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 443: 787–795. [DOI] [PubMed] [Google Scholar]
- 8.Pathak D., Berthet A., Nakamura K. 2013. Energy failure: does it contribute to neurodegeneration? Ann. Neurol. 74: 506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roth J., Szulc A. L., Danoff A. 2011. Energy, evolution, and human diseases: an overview. Am. J. Clin. Nutr. 93: 875S–883S. [DOI] [PubMed] [Google Scholar]
- 10.Schiff M., Benit P., Coulibaly A., Loublier S., El-Khoury R., Rustin P. 2011. Mitochondrial response to controlled nutrition in health and disease. Nutr. Rev. 69: 65–75. [DOI] [PubMed] [Google Scholar]
- 11.McKay J. A., Mathers J. C. 2011. Diet induced epigenetic changes and their implications for health. Acta Physiol. (Oxf.). 202: 103–118. [DOI] [PubMed] [Google Scholar]
- 12.Roopra A., Dingledine R., Hsieh J. 2012. Epigenetics and epilepsy. Epilepsia. 53(Suppl 9): 2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Urdinguio R. G., Sanchez-Mut J. V., Esteller M. 2009. Epigenetic mechanisms in neurological diseases: genes, syndromes, and therapies. Lancet Neurol. 8: 1056–1072. [DOI] [PubMed] [Google Scholar]
- 14.Masino S. A., Rho J. M. 2012. Mechanisms of ketogenic diet action. In Jasper’s Basic Mechanisms of the Epilepsies. J. L. Noebels, M. Avoli, M. A. Rogawski, et al., editors. Oxford University Press, Bethesda, MD. [Google Scholar]
- 15.Lennox W. G., Cobb S. 1928. Epilepsy: from the standpoint of physiology and treatment. Medicine. 7: 105–290. [Google Scholar]
- 16.Bailey E. E., Pfeifer H. H., Thiele E. A. 2005. The use of diet in the treatment of epilepsy. Epilepsy Behav. 6: 4–8. [DOI] [PubMed] [Google Scholar]
- 17.Wheless J. W. 2008. History of the ketogenic diet. Epilepsia. 49(Suppl 8): 3–5. [DOI] [PubMed] [Google Scholar]
- 18.Conklin H. W. 1922. Cause and treatment of epilepsy. J. Am. Osteopath. Assoc. 26: 11–14. [Google Scholar]
- 19.Guelpa G., Marie A. 1911. La lutte contre l’epilepsie par la desintoxication et par la reeducation alimentaire. Revue de Therapie Medico-Chirurgicale. 78: 8–13. [Google Scholar]
- 20.Geyelin H. R. 1921. Fasting as a method for treating epilepsy. Med. Rec. 99: 1037–1039. [Google Scholar]
- 21.Lennox W. G., Cobb S. 1928. Studies in epilepsy: VIII. The clinical effects of fasting. Arch. Neurol. Psychiatry. 20: 771–779. [Google Scholar]
- 22.Woodyatt R. T. 1921. Objects and method of diet adjustment in diabetics. Arch. Intern. Med. 28: 125–141. [Google Scholar]
- 23.Wilder R. M. 1921. The effect of ketonemia on the course of epilepsy. Mayo Clinic Bulletin. 2: 307. [Google Scholar]
- 24.Wilder R. M. 1922. The threshold of ketogenesis. J. Biol. Chem. 52: 393–401. [Google Scholar]
- 25.Peterman M. G. 1925. The ketogenic diet in epilepsy. J. Am. Med. Assoc. 84: 1979–1983. [Google Scholar]
- 26.Peterman M. G. 1924. The ketogenic diet in the treatment of epilepsy: a preliminary report. Am. J. Dis. Child. 28: 28–33. [Google Scholar]
- 27.Huttenlocher P. R., Wilbourn A. J., Signore J. M. 1971. Medium-chain triglycerides as a therapy for intractable childhood epilepsy. Neurology. 21: 1097–1103. [DOI] [PubMed] [Google Scholar]
- 28.Neal E. G., Chaffe H., Schwartz R. H., Lawson M. S., Edwards N., Fitzsimmons G., Whitney A., Cross J. H. 2009. A randomized trial of classical and medium-chain triglyceride ketogenic diets in the treatment of childhood epilepsy. Epilepsia. 50: 1109–1117. [DOI] [PubMed] [Google Scholar]
- 29.Muzykewicz D. A., Lyczkowski D. A., Memon N., Conant K. D., Pfeifer H. H., Thiele E. A. 2009. Efficacy, safety, and tolerability of the low glycemic index treatment in pediatric epilepsy. Epilepsia. 50: 1118–1126. [DOI] [PubMed] [Google Scholar]
- 30.Kossoff E. H., Cervenka M. C., Henry B. J., Haney C. A., Turner Z. 2013. A decade of the modified Atkins diet (2003–2013): Results, insights, and future directions. Epilepsy Behav. 29: 437–442. [DOI] [PubMed] [Google Scholar]
- 31.Lutas A., Yellen G. 2013. The ketogenic diet: metabolic influences on brain excitability and epilepsy. Trends Neurosci. 36: 32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kossoff E. H., Rho J. M. 2009. Ketogenic diets: evidence for short- and long-term efficacy. Neurotherapeutics. 6: 406–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kossoff E. H., Zupec-Kania B. A., Rho J. M. 2009. Ketogenic diets: an update for child neurologists. J. Child Neurol. 24: 979–988. [DOI] [PubMed] [Google Scholar]
- 34.Kossoff E. H., Zupec-Kania B. A., Amark P. E., Ballaban-Gil K. R., Christina Bergqvist A. G., Blackford R., Buchhalter J. R., Caraballo R. H., Helen Cross J., Dahlin M. G., et al. 2009. Optimal clinical management of children receiving the ketogenic diet: recommendations of the International Ketogenic Diet Study Group. Epilepsia. 50: 304–317. [DOI] [PubMed] [Google Scholar]
- 35.Freeman J. M., Kossoff E. H., Hartman A. L. 2007. The ketogenic diet: one decade later. Pediatrics. 119: 535–543. [DOI] [PubMed] [Google Scholar]
- 36.Bergqvist A. G., Schall J. I., Gallagher P. R., Cnaan A., Stallings V. A. 2005. Fasting versus gradual initiation of the ketogenic diet: a prospective, randomized clinical trial of efficacy. Epilepsia. 46: 1810–1819. [DOI] [PubMed] [Google Scholar]
- 37.Kossoff E. H., Laux L. C., Blackford R., Morrison P. F., Pyzik P. L., Hamdy R. M., Turner Z., Nordli D. R., Jr 2008. When do seizures usually improve with the ketogenic diet? Epilepsia. 49: 329–333. [DOI] [PubMed] [Google Scholar]
- 38.Freeman J. M., Vining E. P. 1999. Seizures decrease rapidly after fasting: preliminary studies of the ketogenic diet. Arch. Pediatr. Adolesc. Med. 153: 946–949. [DOI] [PubMed] [Google Scholar]
- 39.Bough K. J., Rho J. M. 2007. Anticonvulsant mechanisms of the ketogenic diet. Epilepsia. 48: 43–58. [DOI] [PubMed] [Google Scholar]
- 40.Huttenlocher P. R. 1976. Ketonemia and seizures: metabolic and anticonvulsant effects of two ketogenic diets in childhood epilepsy. Pediatr. Res. 10: 536–540. [DOI] [PubMed] [Google Scholar]
- 41.Pierre K., Pellerin L. 2005. Monocarboxylate transporters in the central nervous system: distribution, regulation and function. J. Neurochem. 94: 1–14. [DOI] [PubMed] [Google Scholar]
- 42.Prins M. L. 2008. Cerebral metabolic adaptation and ketone metabolism after brain injury. J. Cereb. Blood Flow Metab. 28: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mady M. A., Kossoff E. H., McGregor A. L., Wheless J. W., Pyzik P. L., Freeman J. M. 2003. The ketogenic diet: adolescents can do it, too. Epilepsia. 44: 847–851. [DOI] [PubMed] [Google Scholar]
- 44.Klein P., Janousek J., Barber A., Weissberger R. 2010. Ketogenic diet treatment in adults with refractory epilepsy. Epilepsy Behav. 19: 575–579. [DOI] [PubMed] [Google Scholar]
- 45.Payne N. E., Cross J. H., Sander J. W., Sisodiya S. M. 2011. The ketogenic and related diets in adolescents and adults–a review. Epilepsia. 52: 1941–1948. [DOI] [PubMed] [Google Scholar]
- 46.Kwiterovich P. O., Jr, Vining E. P., Pyzik P., Skolasky R., Jr, Freeman J. M. 2003. Effect of a high-fat ketogenic diet on plasma levels of lipids, lipoproteins, and apolipoproteins in children. JAMA. 290: 912–920. [DOI] [PubMed] [Google Scholar]
- 47.Groesbeck D. K., Bluml R. M., Kossoff E. H. 2006. Long-term use of the ketogenic diet in the treatment of epilepsy. Dev. Med. Child Neurol. 48: 978–981. [DOI] [PubMed] [Google Scholar]
- 48.Bough K. J., Wetherington J., Hassel B., Pare J. F., Gawryluk J. W., Greene J. G., Shaw R., Smith Y., Geiger J. D., Dingledine R. J. 2006. Mitochondrial biogenesis in the anticonvulsant mechanism of the ketogenic diet. Ann. Neurol. 60: 223–235. [DOI] [PubMed] [Google Scholar]
- 49.Hartman A. L., Lyle M., Rogawski M. A., Gasior M. 2008. Efficacy of the ketogenic diet in the 6-Hz seizure test. Epilepsia. 49: 334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rho J. M., Kim D. W., Robbins C. A., Anderson G. D., Schwartzkroin P. A. 1999. Age-dependent differences in flurothyl seizure sensitivity in mice treated with a ketogenic diet. Epilepsy Res. 37: 233–240. [DOI] [PubMed] [Google Scholar]
- 51.D’Agostino D. P., Pilla R., Held H. E., Landon C. S., Puchowicz M., Brunengraber H., Ari C., Arnold P., Dean J. B. 2013. Therapeutic ketosis with ketone ester delays central nervous system oxygen toxicity seizures in rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 304: R829–R836. [DOI] [PubMed] [Google Scholar]
- 52.Hori A., Tandon P., Holmes G. L., Stafstrom C. E. 1997. Ketogenic diet: effects on expression of kindled seizures and behavior in adult rats. Epilepsia. 38: 750–758. [DOI] [PubMed] [Google Scholar]
- 53.Xu X. P., Sun R. P., Jin R. F. 2006. Effect of ketogenic diet on hippocampus mossy fiber sprouting and GluR5 expression in kainic acid induced rat model. Chin. Med. J. (Engl.). 119: 1925–1929. [PubMed] [Google Scholar]
- 54.Su S. W., Cilio M. R., Sogawa Y., Silveira D. C., Holmes G. L., Stafstrom C. E. 2000. Timing of ketogenic diet initiation in an experimental epilepsy model. Brain Res. Dev. Brain Res. 125: 131–138. [Erratum. 2001. Brain Res. Dev. Brain Res. 128: 197.] [DOI] [PubMed] [Google Scholar]
- 55.Kossoff E. H., Rowley H., Sinha S. R., Vining E. P. 2008. A prospective study of the modified Atkins diet for intractable epilepsy in adults. Epilepsia. 49: 316–319. [DOI] [PubMed] [Google Scholar]
- 56.Kossoff E. H., Dorward J. L. 2008. The modified Atkins diet. Epilepsia. 49(Suppl 8): 37–41. [DOI] [PubMed] [Google Scholar]
- 57.Cross J. H., Neal E. G. 2008. The ketogenic diet–update on recent clinical trials. Epilepsia. 49(Suppl 8): 6–10. [DOI] [PubMed] [Google Scholar]
- 58.Bishop N. A., Guarente L. 2007. Genetic links between diet and lifespan: shared mechanisms from yeast to humans. Nat. Rev. Genet. 8: 835–844. [DOI] [PubMed] [Google Scholar]
- 59.Fusco S., Pani G. 2013. Brain response to calorie restriction. Cell. Mol. Life Sci. 70: 3157–3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Libert S., Guarente L. 2013. Metabolic and neuropsychiatric effects of calorie restriction and sirtuins. Annu. Rev. Physiol. 75: 669–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kossoff E. H., Krauss G. L., McGrogan J. R., Freeman J. M. 2003. Efficacy of the Atkins diet as therapy for intractable epilepsy. Neurology. 61: 1789–1791. [DOI] [PubMed] [Google Scholar]
- 62.Kossoff E. H., McGrogan J. R., Bluml R. M., Pillas D. J., Rubenstein J. E., Vining E. P. 2006. A modified Atkins diet is effective for the treatment of intractable pediatric epilepsy. Epilepsia. 47: 421–424. [DOI] [PubMed] [Google Scholar]
- 63.Greene A. E., Todorova M. T., McGowan R., Seyfried T. N. 2001. Caloric restriction inhibits seizure susceptibility in epileptic EL mice by reducing blood glucose. Epilepsia. 42: 1371–1378. [DOI] [PubMed] [Google Scholar]
- 64.Pfeifer H. H., Lyczkowski D. A., Thiele E. A. 2008. Low glycemic index treatment: implementation and new insights into efficacy. Epilepsia. 49(Suppl 8): 42–45. [DOI] [PubMed] [Google Scholar]
- 65.Pfeifer H. H., Thiele E. A. 2005. Low-glycemic-index treatment: a liberalized ketogenic diet for treatment of intractable epilepsy. Neurology. 65: 1810–1812. [DOI] [PubMed] [Google Scholar]
- 66.Guarente L. 2013. Calorie restriction and sirtuins revisited. Genes Dev. 27: 2072–2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hartman A. L., Stafstrom C. E. 2013. Harnessing the power of metabolism for seizure prevention: focus on dietary treatments. Epilepsy Behav. 26: 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bough K. J., Valiyil R., Han F. T., Eagles D. A. 1999. Seizure resistance is dependent upon age and calorie restriction in rats fed a ketogenic diet. Epilepsy Res. 35: 21–28. [DOI] [PubMed] [Google Scholar]
- 69.Todorova M. T., Tandon P., Madore R. A., Stafstrom C. E., Seyfried T. N. 2000. The ketogenic diet inhibits epileptogenesis in EL mice: a genetic model for idiopathic epilepsy. Epilepsia. 41: 933–940. [DOI] [PubMed] [Google Scholar]
- 70.Mantis J. G., Centeno N. A., Todorova M. T., McGowan R., Seyfried T. N. 2004. Management of multifactorial idiopathic epilepsy in EL mice with caloric restriction and the ketogenic diet: role of glucose and ketone bodies. Nutr. Metab. (Lond). 1: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Greene A. E., Todorova M. T., Seyfried T. N. 2003. Perspectives on the metabolic management of epilepsy through dietary reduction of glucose and elevation of ketone bodies. J. Neurochem. 86: 529–537. [DOI] [PubMed] [Google Scholar]
- 72.Veech R. L., Chance B., Kashiwaya Y., Lardy H. A., Cahill G. F., Jr 2001. Ketone bodies, potential therapeutic uses. IUBMB Life. 51: 241–247. [DOI] [PubMed] [Google Scholar]
- 73.Cotter D. G., Schugar R. C., Crawford P. A. 2013. Ketone body metabolism and cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 304: H1060–H1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Keith H. M. 1933. Factors influencing experimentally produced convulsions. Arch. Neurol. Psychiatry. 29: 148–154. [Google Scholar]
- 75.Rho J. M., Anderson G. D., Donevan S. D., White H. S. 2002. Acetoacetate, acetone, and dibenzylamine (a contaminant in l-(+)-beta-hydroxybutyrate) exhibit direct anticonvulsant actions in vivo. Epilepsia. 43: 358–361. [DOI] [PubMed] [Google Scholar]
- 76.Likhodii S. S., Serbanescu I., Cortez M. A., Murphy P., Snead O. C., III, Burnham W. M. 2003. Anticonvulsant properties of acetone, a brain ketone elevated by the ketogenic diet. Ann. Neurol. 54: 219–226. [DOI] [PubMed] [Google Scholar]
- 77.Yudkoff M., Daikhin Y., Nissim I., Horyn O., Lazarow A., Luhovyy B., Wehrli S. 2005. Response of brain amino acid metabolism to ketosis. Neurochem. Int. 47: 119–128. [DOI] [PubMed] [Google Scholar]
- 78.Dahlin M., Elfving A., Ungerstedt U., Amark P. 2005. The ketogenic diet influences the levels of excitatory and inhibitory amino acids in the CSF in children with refractory epilepsy. Epilepsy Res. 64: 115–125. [DOI] [PubMed] [Google Scholar]
- 79.Melø T. M., Nehlig A., Sonnewald U. 2006. Neuronal-glial interactions in rats fed a ketogenic diet. Neurochem. Int. 48: 498–507. [DOI] [PubMed] [Google Scholar]
- 80.Cheng C. M., Hicks K., Wang J., Eagles D. A., Bondy C. A. 2004. Caloric restriction augments brain glutamic acid decarboxylase-65 and -67 expression. J. Neurosci. Res. 77: 270–276. [DOI] [PubMed] [Google Scholar]
- 81.Bough K. J., Paquet M., Pare J. F., Hassel B., Smith Y., Hall R. A., Dingledine R. 2007. Evidence against enhanced glutamate transport in the anticonvulsant mechanism of the ketogenic diet. Epilepsy Res. 74: 232–236. [DOI] [PubMed] [Google Scholar]
- 82.Juge N., Gray J. A., Omote H., Miyaji T., Inoue T., Hara C., Uneyama H., Edwards R. H., Nicoll R. A., Moriyama Y. 2010. Metabolic control of vesicular glutamate transport and release. Neuron. 68: 99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thio L. L., Wong M., Yamada K. A. 2000. Ketone bodies do not directly alter excitatory or inhibitory hippocampal synaptic transmission. Neurology. 54: 325–331. [DOI] [PubMed] [Google Scholar]
- 84.Ma W., Berg J., Yellen G. 2007. Ketogenic diet metabolites reduce firing in central neurons by opening K(ATP) channels. J. Neurosci. 27: 3618–3625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tanner G. R., Lutas A., Martinez-Francois J. R., Yellen G. 2011. Single K ATP channel opening in response to action potential firing in mouse dentate granule neurons. J. Neurosci. 31: 8689–8696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Won Y. J., Lu V. B., Puhl H. L., III, Ikeda S. R. 2013. β-Hydroxybutyrate modulates N-type calcium channels in rat sympathetic neurons by acting as an agonist for the G-protein-coupled receptor FFA3. J. Neurosci. 33: 19314–19325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Giménez-Cassina A., Martínez-Francois J. R., Fisher J. K., Szlyk B., Polak K., Wiwczar J., Tanner G. R., Lutas A., Yellen G., Danial N. N. 2012. BAD-dependent regulation of fuel metabolism and K(ATP) channel activity confers resistance to epileptic seizures. Neuron. 74: 719–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.DeVivo D. C., Leckie M. P., Ferrendelli J. S., McDougal D. B., Jr 1978. Chronic ketosis and cerebral metabolism. Ann. Neurol. 3: 331–337. [DOI] [PubMed] [Google Scholar]
- 89.Kim do Y., Vallejo J., Rho J. M. 2010. Ketones prevent synaptic dysfunction induced by mitochondrial respiratory complex inhibitors. J. Neurochem. 114: 130–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Masino S. A., Kawamura M., Jr, Ruskin D. N., Geiger J. D., Boison D. 2012. Purines and neuronal excitability: links to the ketogenic diet. Epilepsy Res. 100: 229–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pascual O., Casper K. B., Kubera C., Zhang J., Revilla-Sanchez R., Sul J. Y., Takano H., Moss S. J., McCarthy K., Haydon P. G. 2005. Astrocytic purinergic signaling coordinates synaptic networks. Science. 310: 113–116. [DOI] [PubMed] [Google Scholar]
- 92.Masino S. A., Li T., Theofilas P., Sandau U. S., Ruskin D. N., Fredholm B. B., Geiger J. D., Aronica E., Boison D. 2011. A ketogenic diet suppresses seizures in mice through adenosine A(1) receptors. J. Clin. Invest. 121: 2679–2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rowley S., Patel M. 2013. Mitochondrial involvement and oxidative stress in temporal lobe epilepsy. Free Radic. Biol. Med. 62: 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Veech R. L. 2004. The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot. Essent. Fatty Acids. 70: 309–319. [DOI] [PubMed] [Google Scholar]
- 95.Ziegler D. R., Ribeiro L. C., Hagenn M., Siqueira I. R., Araujo E., Torres I. L., Gottfried C., Netto C. A., Goncalves C. A. 2003. Ketogenic diet increases glutathione peroxidase activity in rat hippocampus. Neurochem. Res. 28: 1793–1797. [DOI] [PubMed] [Google Scholar]
- 96.Jarrett S. G., Milder J. B., Liang L. P., Patel M. 2008. The ketogenic diet increases mitochondrial glutathione levels. J. Neurochem. 106: 1044–1051. [DOI] [PubMed] [Google Scholar]
- 97.Milder J. B., Liang L. P., Patel M. 2010. Acute oxidative stress and systemic Nrf2 activation by the ketogenic diet. Neurobiol. Dis. 40: 238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Suzuki T., Motohashi H., Yamamoto M. 2013. Toward clinical application of the Keap1-Nrf2 pathway. Trends Pharmacol. Sci. 34: 340–346. [DOI] [PubMed] [Google Scholar]
- 99.Sekhar K. R., Rachakonda G., Freeman M. L. 2010. Cysteine-based regulation of the CUL3 adaptor protein Keap1. Toxicol. Appl. Pharmacol. 244: 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mazzuferi M., Kumar G., van Eyll J., Danis B., Foerch P., Kaminski R. M. 2013. Nrf2 defense pathway: Experimental evidence for its protective role in epilepsy. Ann. Neurol. 74: 560–568. [DOI] [PubMed] [Google Scholar]
- 101.Maalouf M., Rho J. M. 2008. Oxidative impairment of hippocampal long-term potentiation involves activation of protein phosphatase 2A and is prevented by ketone bodies. J. Neurosci. Res. 86: 3322–3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maalouf M., Sullivan P. G., Davis L., Kim D. Y., Rho J. M. 2007. Ketones inhibit mitochondrial production of reactive oxygen species production following glutamate excitotoxicity by increasing NADH oxidation. Neuroscience. 145: 256–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kim do Y., Davis L. M., Sullivan P. G., Maalouf M., Simeone T. A., van Brederode J., Rho J. M. 2007. Ketone bodies are protective against oxidative stress in neocortical neurons. J. Neurochem. 101: 1316–1326. [DOI] [PubMed] [Google Scholar]
- 104.Sullivan P. G., Dube C., Dorenbos K., Steward O., Baram T. Z. 2003. Mitochondrial uncoupling protein-2 protects the immature brain from excitotoxic neuronal death. Ann. Neurol. 53: 711–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Azzu V., Brand M. D. 2010. The on-off switches of the mitochondrial uncoupling proteins. Trends Biochem. Sci. 35: 298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sullivan P. G., Rippy N. A., Dorenbos K., Concepcion R. C., Agarwal A. K., Rho J. M. 2004. The ketogenic diet increases mitochondrial uncoupling protein levels and activity. Ann. Neurol. 55: 576–580. [DOI] [PubMed] [Google Scholar]
- 107.Shimazu T., Hirschey M. D., Newman J., He W., Shirakawa K., Le Moan N., Grueter C. A., Lim H., Saunders L. R., Stevens R. D., et al. 2013. Suppression of oxidative stress by beta-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 339: 211–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kovac S., Domijan A. M., Walker M. C., Abramov A. Y. 2012. Prolonged seizure activity impairs mitochondrial bioenergetics and induces cell death. J. Cell Sci. 125: 1796–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stafstrom C. E., Ockuly J. C., Murphree L., Valley M. T., Roopra A., Sutula T. P. 2009. Anticonvulsant and antiepileptic actions of 2-deoxy-D-glucose in epilepsy models. Ann. Neurol. 65: 435–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Garriga-Canut M., Schoenike B., Qazi R., Bergendahl K., Daley T. J., Pfender R. M., Morrison J. F., Ockuly J., Stafstrom C., Sutula T., Roopra A. 2006. 2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CtBP-dependent metabolic regulation of chromatin structure. Nat. Neurosci. 9: 1382–1387. [DOI] [PubMed] [Google Scholar]
- 111.Wellen K. E., Hatzivassiliou G., Sachdeva U. M., Bui T. V., Cross J. R., Thompson C. B. 2009. ATP-citrate lyase links cellular metabolism to histone acetylation. Science. 324: 1076–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Albaugh B. N., Arnold K. M., Denu J. M. 2011. KAT(ching) metabolism by the tail: insight into the links between lysine acetyltransferases and metabolism. ChemBioChem. 12: 290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hebert A. S., Dittenhafer-Reed K. E., Yu W., Bailey D. J., Selen E. S., Boersma M. D., Carson J. J., Tonelli M., Balloon A. J., Higbee A. J., et al. 2013. Calorie restriction and SIRT3 trigger global reprogramming of the mitochondrial protein acetylome. Mol. Cell. 49: 186–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wagner G. R., Payne R. M. 2013. Widespread and enzyme-independent Nε-acetylation and Nε-succinylation of proteins in the chemical conditions of the mitochondrial matrix. J. Biol. Chem. 288: 29036–29045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lian X. Y., Khan F. A., Stringer J. L. 2007. Fructose-1,6-bisphosphate has anticonvulsant activity in models of acute seizures in adult rats. J. Neurosci. 27: 12007–12011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fraser D. D., Whiting S., Andrew R. D., Macdonald E. A., Musa-Veloso K., Cunnane S. C. 2003. Elevated polyunsaturated fatty acids in blood serum obtained from children on the ketogenic diet. Neurology. 60: 1026–1029. [DOI] [PubMed] [Google Scholar]
- 117.Michael-Titus A. T., Priestley J. V. 2014. Omega-3 fatty acids and traumatic neurological injury: from neuroprotection to neuroplasticity? Trends Neurosci. 37: 30–38. [DOI] [PubMed] [Google Scholar]
- 118.Schlanger S., Shinitzky M., Yam D. 2002. Diet enriched with omega-3 fatty acids alleviates convulsion symptoms in epilepsy patients. Epilepsia. 43: 103–104. [DOI] [PubMed] [Google Scholar]
- 119.Yuen A. W., Sander J. W., Fluegel D., Patsalos P. N., Bell G. S., Johnson T., Koepp M. J. 2005. Omega-3 fatty acid supplementation in patients with chronic epilepsy: a randomized trial. Epilepsy Behav. 7: 253–258. [DOI] [PubMed] [Google Scholar]
- 120.Bromfield E., Dworetzky B., Hurwitz S., Eluri Z., Lane L., Replansky S., Mostofsky D. 2008. A randomized trial of polyunsaturated fatty acids for refractory epilepsy. Epilepsy Behav. 12: 187–190. [DOI] [PubMed] [Google Scholar]
- 121.Taha A. Y., Ryan M. A., Cunnane S. C. 2005. Despite transient ketosis, the classic high-fat ketogenic diet induces marked changes in fatty acid metabolism in rats. Metabolism. 54: 1127–1132. [DOI] [PubMed] [Google Scholar]
- 122.Cullingford T. E., Eagles D. A., Sato H. 2002. The ketogenic diet upregulates expression of the gene encoding the key ketogenic enzyme mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase in rat brain. Epilepsy Res. 49: 99–107. [DOI] [PubMed] [Google Scholar]
- 123.Taha A. Y., Burnham W. M., Auvin S. 2010. Polyunsaturated fatty acids and epilepsy. Epilepsia. 51: 1348–1358. [DOI] [PubMed] [Google Scholar]
- 124.Suzuki M., Sato K., Dohi S., Sato T., Matsuura A., Hiraide A. 2001. Effect of beta-hydroxybutyrate, a cerebral function improving agent, on cerebral hypoxia, anoxia and ischemia in mice and rats. Jpn. J. Pharmacol. 87: 143–150. [DOI] [PubMed] [Google Scholar]
- 125.Noh H. S., Lee H. P., Kim D. W., Kang S. S., Cho G. J., Rho J. M., Choi W. S. 2004. A cDNA microarray analysis of gene expression profiles in rat hippocampus following a ketogenic diet. Brain Res. Mol. Brain Res. 129: 80–87. [DOI] [PubMed] [Google Scholar]
- 126.Tieu K., Perier C., Caspersen C., Teismann P., Wu D. C., Yan S. D., Naini A., Vila M., Jackson-Lewis V., Ramasamy R., et al. 2003. D-beta-hydroxybutyrate rescues mitochondrial respiration and mitigates features of Parkinson disease. J. Clin. Invest. 112: 892–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Willis S., Stoll J., Sweetman L., Borges K. 2010. Anticonvulsant effects of a triheptanoin diet in two mouse chronic seizure models. Neurobiol. Dis. 40: 565–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hadera M. G., Smeland O. B., McDonald T. S., Tan K. N., Sonnewald U., Borges K. 2014. Triheptanoin partially restores levels of tricarboxylic acid cycle intermediates in the mouse pilocarpine model of epilepsy. J. Neurochem. 129: 107–119. [DOI] [PubMed] [Google Scholar]
- 129.Kovac S., Abramov A. Y., Walker M. C. 2013. Energy depletion in seizures: anaplerosis as a strategy for future therapies. Neuropharmacology. 69: 96–104. [DOI] [PubMed] [Google Scholar]
- 130.Mattson M. P. 2012. Energy intake and exercise as determinants of brain health and vulnerability to injury and disease. Cell Metab. 16: 706–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sampath H., Ntambi J. M. 2005. Polyunsaturated fatty acid regulation of genes of lipid metabolism. Annu. Rev. Nutr. 25: 317–340. [DOI] [PubMed] [Google Scholar]
- 132.Porta N., Vallee L., Lecointe C., Bouchaert E., Staels B., Bordet R., Auvin S. 2009. Fenofibrate, a peroxisome proliferator-activated receptor-alpha agonist, exerts anticonvulsive properties. Epilepsia. 50: 943–948. [DOI] [PubMed] [Google Scholar]
- 133.Maurois P., Rocchi S., Pages N., Bac P., Stables J. P., Gressens P., Vamecq J. 2008. The PPARgamma agonist FMOC-L-leucine protects both mature and immature brain. Biomed. Pharmacother. 62: 259–263. [DOI] [PubMed] [Google Scholar]
- 134.Yu X., Shao X. G., Sun H., Li Y. N., Yang J., Deng Y. C., Huang Y. G. 2008. Activation of cerebral peroxisome proliferator-activated receptors gamma exerts neuroprotection by inhibiting oxidative stress following pilocarpine-induced status epilepticus. Brain Res. 1200: 146–158. [DOI] [PubMed] [Google Scholar]
- 135.Cullingford T. E., Dolphin C. T., Sato H. 2002. The peroxisome proliferator-activated receptor alpha-selective activator ciprofibrate upregulates expression of genes encoding fatty acid oxidation and ketogenesis enzymes in rat brain. Neuropharmacology. 42: 724–730. [DOI] [PubMed] [Google Scholar]
- 136.Hardie D. G., Sakamoto K. 2006. AMPK: a key sensor of fuel and energy status in skeletal muscle. Physiology (Bethesda). 21: 48–60. [DOI] [PubMed] [Google Scholar]
- 137.Kennedy A. R., Pissios P., Otu H., Roberson R., Xue B., Asakura K., Furukawa N., Marino F. E., Liu F. F., Kahn B. B., et al. 2007. A high-fat, ketogenic diet induces a unique metabolic state in mice. Am. J. Physiol. Endocrinol. Metab. 292: E1724–E1739. [Erratum. 2009. Am. J. Physiol. Endocrinol. Metab. 296: E1179.] [DOI] [PubMed] [Google Scholar]
- 138.McDaniel S. S., Rensing N. R., Thio L. L., Yamada K. A., Wong M. 2011. The ketogenic diet inhibits the mammalian target of rapamycin (mTOR) pathway. Epilepsia. 52: e7–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Johnson S. C., Rabinovitch P. S., Kaeberlein M. 2013. mTOR is a key modulator of ageing and age-related disease. Nature. 493: 338–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wong M. 2013. Mammalian target of rapamycin (mTOR) pathways in neurological diseases. Biomed. J. 36: 40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Houtkooper R. H., Williams R. W., Auwerx J. 2010. Metabolic networks of longevity. Cell. 142: 9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Houtkooper R. H., Pirinen E., Auwerx J. 2012. Sirtuins as regulators of metabolism and healthspan. Nat. Rev. Mol. Cell Biol. 13: 225–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Srivastava S., Baxa U., Niu G., Chen X., Veech R. L. 2013. A ketogenic diet increases brown adipose tissue mitochondrial proteins and UCP1 levels in mice. IUBMB Life. 65: 58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rardin M. J., Newman J. C., Held J. M., Cusack M. P., Sorensen D. J., Li B., Schilling B., Mooney S. D., Kahn C. R., Verdin E., et al. 2013. Label-free quantitative proteomics of the lysine acetylome in mitochondria identifies substrates of SIRT3 in metabolic pathways. Proc. Natl. Acad. Sci. USA. 110: 6601–6606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rardin M. J., He W., Nishida Y., Newman J. C., Carrico C., Danielson S. R., Guo A., Gut P., Sahu A. K., Li B., et al. 2013. SIRT5 regulates the mitochondrial lysine succinylome and metabolic networks. Cell Metab. 18: 920–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shimazu T., Hirschey M. D., Hua L., Dittenhafer-Reed K. E., Schwer B., Lombard D. B., Li Y., Bunkenborg J., Alt F. W., Denu J. M., et al. 2010. SIRT3 deacetylates mitochondrial 3-hydroxy-3-methylglutaryl CoA synthase 2 and regulates ketone body production. Cell Metab. 12: 654–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.de Castro I. P., Martins L. M., Tufi R. 2010. Mitochondrial quality control and neurological disease: an emerging connection. Expert Rev. Mol. Med. 12: e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Calì T., Ottolini D., Brini M. 2012. Mitochondrial Ca(2+) and neurodegeneration. Cell Calcium. 52: 73–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Johri A., Beal M. F. 2012. Mitochondrial dysfunction in neurodegenerative diseases. J. Pharmacol. Exp. Ther. 342: 619–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Palop J. J., Mucke L. 2009. Epilepsy and cognitive impairments in Alzheimer disease. Arch. Neurol. 66: 435–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Reger M. A., Henderson S. T., Hale C., Cholerton B., Baker L. D., Watson G. S., Hyde K., Chapman D., Craft S. 2004. Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. Neurobiol. Aging. 25: 311–314. [DOI] [PubMed] [Google Scholar]
- 152.Krikorian R., Shidler M. D., Dangelo K., Couch S. C., Benoit S. C., Clegg D. J. 2012. Dietary ketosis enhances memory in mild cognitive impairment. Neurobiol. Aging. 33: 425.e19–425.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Henderson S. T., Vogel J. L., Barr L. J., Garvin F., Jones J. J., Costantini L. C. 2009. Study of the ketogenic agent AC-1202 in mild to moderate Alzheimer’s disease: a randomized, double-blind, placebo-controlled, multicenter trial. Nutr. Metab. (Lond). 6: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Van der Auwera I., Wera S., Van Leuven F., Henderson S. T. 2005. A ketogenic diet reduces amyloid beta 40 and 42 in a mouse model of Alzheimer’s disease. Nutr. Metab. (Lond). 2: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kashiwaya Y., Takeshima T., Mori N., Nakashima K., Clarke K., Veech R. L. 2000. D-beta-hydroxybutyrate protects neurons in models of Alzheimer’s and Parkinson’s disease. Proc. Natl. Acad. Sci. USA. 97: 5440–5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kashiwaya Y., Bergman C., Lee J. H., Wan R., King M. T., Mughal M. R., Okun E., Clarke K., Mattson M. P., Veech R. L. 2013. A ketone ester diet exhibits anxiolytic and cognition-sparing properties, and lessens amyloid and tau pathologies in a mouse model of Alzheimer’s disease. Neurobiol. Aging. 34: 1530–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Vanitallie T. B., Nonas C., Di Rocco A., Boyar K., Hyams K., Heymsfield S. B. 2005. Treatment of Parkinson disease with diet-induced hyperketonemia: a feasibility study. Neurology. 64: 728–730. [DOI] [PubMed] [Google Scholar]
- 158.de Lau L. M., Bornebroek M., Witteman J. C., Hofman A., Koudstaal P. J., Breteler M. M. 2005. Dietary fatty acids and the risk of Parkinson disease: the Rotterdam study. Neurology. 64: 2040–2045. [DOI] [PubMed] [Google Scholar]
- 159.Seyfried T. N., Shelton L. M. 2010. Cancer as a metabolic disease. Nutr. Metab. (Lond). 7: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Warburg O. 1956. On the origin of cancer cells. Science. 123: 309–314. [DOI] [PubMed] [Google Scholar]
- 161.Seyfried T. N., Kiebish M. A., Marsh J., Shelton L. M., Huysentruyt L. C., Mukherjee P. 2011. Metabolic management of brain cancer. Biochim. Biophys. Acta. 1807: 577–594. [DOI] [PubMed] [Google Scholar]
- 162.Seyfried T. N., Sanderson T. M., El-Abbadi M. M., McGowan R., Mukherjee P. 2003. Role of glucose and ketone bodies in the metabolic control of experimental brain cancer. Br. J. Cancer. 89: 1375–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Stafford P., Abdelwahab M. G., Kim do Y., Preul M. C., Rho J. M., Scheck A. C. 2010. The ketogenic diet reverses gene expression patterns and reduces reactive oxygen species levels when used as an adjuvant therapy for glioma. Nutr. Metab. (Lond). 7: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Abdelwahab M. G., Fenton K. E., Preul M. C., Rho J. M., Lynch A., Stafford P., Scheck A. C. 2012. The ketogenic diet is an effective adjuvant to radiation therapy for the treatment of malignant glioma. PLoS ONE. 7: e36197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Chang H. T., Olson L. K., Schwartz K. A. 2013. Ketolytic and glycolytic enzymatic expression profiles in malignant gliomas: implication for ketogenic diet therapy. Nutr. Metab. (Lond). 10: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Babikian T., Prins M. L., Cai Y., Barkhoudarian G., Hartonian I., Hovda D. A., Giza C. C. 2010. Molecular and physiological responses to juvenile traumatic brain injury: focus on growth and metabolism. Dev. Neurosci. 32: 431–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Algattas H., Huang J. H. 2014. Traumatic brain injury pathophysiology and treatments: early, intermediate, and late phases post-injury. Int. J. Mol. Sci. 15: 309–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Prins M. L., Fujima L. S., Hovda D. A. 2005. Age-dependent reduction of cortical contusion volume by ketones after traumatic brain injury. J. Neurosci. Res. 82: 413–420. [DOI] [PubMed] [Google Scholar]
- 169.Prins M. L., Lee S. M., Fujima L. S., Hovda D. A. 2004. Increased cerebral uptake and oxidation of exogenous betaHB improves ATP following traumatic brain injury in adult rats. J. Neurochem. 90: 666–672. [DOI] [PubMed] [Google Scholar]
- 170.Hu Z. G., Wang H. D., Qiao L., Yan W., Tan Q. F., Yin H. X. 2009. The protective effect of the ketogenic diet on traumatic brain injury-induced cell death in juvenile rats. Brain Inj. 23: 459–465. [DOI] [PubMed] [Google Scholar]
- 171.Yamada K. A., Rensing N., Thio L. L. 2005. Ketogenic diet reduces hypoglycemia-induced neuronal death in young rats. Neurosci. Lett. 385: 210–214. [DOI] [PubMed] [Google Scholar]
- 172.Davis L. M., Pauly J. R., Readnower R. D., Rho J. M., Sullivan P. G. 2008. Fasting is neuroprotective following traumatic brain injury. J. Neurosci. Res. 86: 1812–1822. [DOI] [PubMed] [Google Scholar]
- 173.Rothstein J. D. 2009. Current hypotheses for the underlying biology of amyotrophic lateral sclerosis. Ann. Neurol. 65(Suppl 1): S3–S9. [DOI] [PubMed] [Google Scholar]
- 174.Zhao Z., Lange D. J., Voustianiouk A., MacGrogan D., Ho L., Suh J., Humala N., Thiyagarajan M., Wang J., Pasinetti G. M. 2006. A ketogenic diet as a potential novel therapeutic intervention in amyotrophic lateral sclerosis. BMC Neurosci. 7: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Bialer M. 2012. Why are antiepileptic drugs used for nonepileptic conditions? Epilepsia. 53(Suppl 7): 26–33. [DOI] [PubMed] [Google Scholar]
- 176.Ruskin D. N., Kawamura M., Masino S. A. 2009. Reduced pain and inflammation in juvenile and adult rats fed a ketogenic diet. PLoS ONE. 4: e8349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Masino S. A., Ruskin D. N. 2013. Ketogenic diets and pain. J. Child Neurol. 28: 993–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Ruskin D. N., Svedova J., Cote J. L., Sandau U., Rho J. M., Kawamura M., Jr, Boison D., Masino S. A. 2013. Ketogenic diet improves core symptoms of autism in BTBR mice. PLoS ONE. 8: e65021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kossoff E. H., Huffman J., Turner Z., Gladstein J. 2010. Use of the modified Atkins diet for adolescents with chronic daily headache. Cephalalgia. 30: 1014–1016. [DOI] [PubMed] [Google Scholar]
- 180.Kim do Y., Rho J. M. 2008. The ketogenic diet and epilepsy. Curr. Opin. Clin. Nutr. Metab. Care. 11: 113–120. [DOI] [PubMed] [Google Scholar]
- 181.Waldbaum S., Patel M. 2010. Mitochondria, oxidative stress, and temporal lobe epilepsy. Epilepsy Res. 88: 23–45. [DOI] [PMC free article] [PubMed] [Google Scholar]