Abstract
Objective
Risk-standardized 30-day mortality and hospital readmission rates for pneumonia are increasingly being tied to hospital reimbursement to incentivize the delivery of high quality care. Such measures may be susceptible to gaming by recoding patients with pneumonia to a primary diagnosis of sepsis or respiratory failure. We sought to determine the degree to which hospitals can game mortality or readmission measures and change their rankings by recoding patients with pneumonia.
Design and Setting
Simulated experimental study of 2,906 US acute care hospitals with at least 25 admissions for pneumonia using 2009 Medicare data.
Participants
Elderly (age ≥ 65 years) Medicare fee-for-service beneficiaries hospitalized with pneumonia. Patients eligible for recoding to sepsis or respiratory failure were those with a principal ICD-9-CM discharge code for pneumonia and secondary codes for respiratory failure or acute organ dysfunction.
Interventions
None
Measurements and Main Results
We measured the number of hospitals that improved their pneumonia mortality or readmission rates after recoding eligible patients. When a sample of 100 hospitals with pneumonia mortality rates above the 50th percentile recoded all eligible patients to sepsis or respiratory failure, 90 hospitals (95% CI: 84 - 95) improved their mortality rate (mean improvement 1.09%, 95% CI: 0.94 – 1.28%) and 41 hospitals dropped below the 50th percentile (95% CI: 33 - 52). When a sample of 100 hospitals with pneumonia readmission rates above the 50th percentile recoded all eligible patients, 66 hospitals (95% CI: 54 - 75) improved their readmission rate (mean improvement 0.34%, 95% CI: 0.19 – 0.45%) and 15 hospitals (95% CI: 9 - 22) dropped below the 50th percentile.
Conclusions
Hospitals can improve apparent pneumonia mortality and readmission rates by recoding pneumonia patients. CMS should consider changes to their methods used to calculate hospital-level pneumonia outcome measures to make them less susceptible to gaming.
MeSH Index Terms: Pneumonia, Sepsis: Quality of Healthcare, Hospital Readmissions, In Silico, Outcome measures
Introduction
Pneumonia is the most common cause of acute hospitalization in the United States (1), yet the quality of care for patients with pneumonia varies widely across hospitals (2-5). In an effort to improve quality, the Centers for Medicare and Medicaid Services (CMS) requires hospitals to publicly report risk-adjusted mortality and readmission rates for pneumonia (6). The Affordable Care Act required implementing the Hospital Readmission Reduction Program (HRRP) and expanded the Hospital Value-Based Purchasing Program (VBP), initiatives formally tying hospital reimbursement to pneumonia readmission and mortality rates (7-9). CMS calculates pneumonia mortality and readmission rates using claims data for patients identified with a principal ICD-9-CM diagnosis code of pneumonia (10). However, patients with pneumonia are increasingly being coded with a principal diagnosis of respiratory failure or severe sepsis (11), and these patients are not included in current hospital mortality and readmission rate calculations.
It is unclear the extent to which pneumonia mortality and readmission measures are sensitive to coding variation and whether hospitals can game these measures. A recent study of 329 hospitals by Rothberg et. al. found that pneumonia mortality rates correlated with how hospitals coded their pneumonia admissions (12). Hospitals coding more patients with pneumonia as a principal diagnosis of sepsis or respiratory failure and secondary diagnosis of pneumonia had lower mortality rates. Because of variation in pneumonia coding practice, the authors recommended that CMS include patients with a principal diagnosis of respiratory failure or sepsis and secondary pneumonia when calculating pneumonia performance measures (12). However, until CMS changes their method of calculating pneumonia performance measures, hospitals may have the ability to game these measures by aggressively (but allowably) coding their most severely ill patients with pneumonia as sepsis or respiratory failure. This practice not only might reduce a hospital's measured pneumonia mortality, it would likely improve Diagnosis-Related Group (DRG) payments for such patients (1). Whether readmission rates could also be improved has not been previously studied.
The current study builds upon the prior work of Rothberg et. al. and evaluates the extent to which hospitals penalized for high pneumonia mortality and readmission rates can improve these rates by recoding patients to a principal diagnosis of sepsis or respiratory failure. We also examine the system-level effects of many hospitals engaged in recoding pneumonia patients at the same time. We hypothesized that a significant fraction of currently penalized hospitals could reduce both their measured 30-day mortality and hospital readmission rates simply by recoding patients with pneumonia who meet criteria for sepsis or respiratory failure. We hypothesized that gains seen by individual hospitals would be reduced if many other hospitals engaged in recoding simultaneously.
Methods
Study Cohort
We used Medicare Provider Analysis and Review (MedPAR) and Beneficiary Summary files to identify all acute care hospitalizations for pneumonia among fee-for-service Medicare beneficiaries age 65 years or older in 2009. We defined pneumonia using CMS's definition, which requires the presence of any of the following primary discharge ICD-9-CM diagnosis codes: 480.X, 481, 482.XX, 483.X, 485, 486, or 487.0 (13, 14). Because we wanted to replicate the current CMS methodology for calculating hospital 30-day pneumonia mortality and readmission rates, we did not include patients with a principal diagnosis of sepsis or respiratory failure and secondary pneumonia in our case definition (10,13,14). We followed CMS's inclusion and exclusion criteria for these measures and created separate patient cohorts for analyzing hospital mortality and readmissions (see supplemental digital content).
Pneumonia Admissions Meeting Criteria for Severe Sepsis
We identified patients who also met criteria for either severe sepsis or respiratory failure as those with either a ICD-9-CM procedure code for mechanical ventilation or any other ICD-9-CM diagnosis code for acute organ dysfunction (supplemental digital content eTable 1) (16). This method of identifying patients with severe sepsis has been previously validated against a clinical chart review and used in multiple prior studies (17-19).
Statistical analysis
Hospital 30-day Risk Standardized Mortality (RSMRs) and Readmissions Rates (RSRRs)
We estimated 30-day pneumonia mortality and readmission rates for all hospitals using identical methods to those used in public reporting by CMS (13,14). We used hierarchical logistic regression models to estimate hospital risk standardized mortality and readmission rates, adjusting for age, sex, and hierarchical condition categories (HCC) from the year's prior MedPAR data (20). Hierarchical models allow for the inclusion of a hospital-specific random intercept and are able to isolate the hospital-specific effect on an outcome. A “predicted” probability of the outcome is calculated for each patient using their specific covariates, taking into account the hospital to which they were admitted. The “predicted” probabilities are summed for all patients at each hospital and divided by the sum of “expected” probabilities of the outcome, which are estimated using only patient covariates without accounting for the hospital to which they were admitted. Finally, this ratio is multiplied by the overall mortality or readmission rate to obtain the adjusted hospital specific rate. Because only the point estimate for each hospital is used to calculate penalties under HRRP and VBP, we did not bootstrap these calculations to obtain 95% confidence interval estimates, as is done in Hospital Compare to identify outlier hospitals. Further details of these methods are available in the CMS measures documentation (13,14).
Monte-Carlo Simulations
We performed a series of simulations to understand the extent to which hospitals could improve pneumonia outcomes by recoding eligible patients with pneumonia. In each simulation: (1) we randomly selected from a group of hospitals to recode eligible pneumonia patients as sepsis or respiratory failure (2) we randomly selected patients within these hospitals who met criteria for sepsis or respiratory failure and excluded them from a subsequent readmission or mortality rate calculation by removing them from the numerator and denominator of the calculations. Excluding these patients from the readmission and mortality calculation is what would occur under the current CMS methods if a hospital coded a pneumonia patient as sepsis or respiratory failure in the principal diagnosis field. We then recalculated each hospital's mortality and readmission rates, as described above, and compared these results to the original values. Both hospitals and patients were re-sampled during each subsequent simulation.
In mortality simulations, we selected among hospitals with mortality rates higher than the 50th percentile. These hospitals may be subject to lower reimbursement under CMS' VBP program, and thus have the greatest incentive to improve their mortality rate. In simulations for readmission rates, we selected among hospitals above 50th percentile because these hospitals are penalized for “excess” readmissions under HRRP.
We focused on two parameters during successive runs of the simulation. First, we varied the proportion of eligible patients within a hospital that were recoded to sepsis or respiratory failure, which reflects how aggressively a hospital identifies and recodes all patients eligible for recoding. Second, we varied the total number of hospitals that simultaneously recoded patients. This parameter characterizes how gains among individual hospitals would change when more hospitals engaged in recoding. We performed 100 simulations for each set of parameters. Simulation confidence intervals were calculated using percentiles of the simulated results (21).
Continuous data were compared using t-tests or Wilcoxon rank sum tests as appropriate, categorical data were compared using the chi-squared test or Fishers exact test. P-values < 0.05 were considered significant. All data management and analysis was conducted using SAS 9.2 (SAS Institute, Cary, NC) and Stata 13 (StataCorp, College Station, TX). The institutional review board of the University of Michigan approved the study (HUM00053488).
Results
Patient and hospital characteristics
We identified 319,879 admissions for pneumonia eligible for inclusion in the mortality rate calculation and 345,402 admissions eligible to be included in the readmission rate calculation in 2009. Among hospitals with over 25 eligible admissions, we calculated mortality rates for 2,936 hospitals and readmission rates for 2,950 hospitals (supplemental digital content eFigure 1).
Twenty-eight percent of patients admitted with a principal diagnosis of pneumonia met criteria for sepsis or respiratory failure. Patients meeting criteria were more often male, non-white, and slightly older (Table 1). They were more likely to have congestive heart failure, renal failure, and malignancy. These patients had a markedly higher 30-day all cause mortality rate (17.7% versus 7.2%, p < 0.001), and higher 30-day readmission rate (21.1% versus 16.6%, p < 0.001) among patients who survived the index hospitalization.
Table 1. Characteristics of Medicare beneficiaries admitted with a primary ICD-9-CM diagnosis of pneumonia in 2009.
| Criteria for severe sepsis or respiratory failurea | No (n=253,331) | Yes (n=71,212) |
|---|---|---|
| Patient Characteristics | ||
| % Female | 56.9 | 49.1 |
| % Non-white | 12.1 | 14.3 |
| Age | ||
| 65-74 | 30.3 | 27.3 |
| 75-84 | 36.8 | 37.4 |
| 85 + | 32.9 | 35.3 |
| Comorbidities | ||
| CHF | 38.3 | 46.3 |
| COPD | 46.6 | 43.0 |
| Renal Failure | 21.7 | 71.4 |
| Malignancy | 10.5 | 12.0 |
| History of PNA | 6.2 | 6.9 |
| Admission Type | ||
| Emergent | 73.4 | 78.2 |
| Urgent | 19.5 | 16.8 |
| Admission Source | ||
| ED | 76.4 | 79.1 |
| Outpatient | 17.8 | 13.5 |
| % Admitted to ICU | 8.3 | 26 |
| Outcomes | ||
| Length of Stay, median (IQR) | 4 (3-7) | 6 (4-9) |
| % Discharged to home | 47.6 | 31.8 |
| 30-day Mortality Rate | 9.1 | 21.4 |
| 30-day Readmission Rate | 16.1 | 19.9 |
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; PNA, pneumonia; ED, emergency department; ICU, intensive care unit; IQR, interquartile range.
Results are percentages unless otherwise stated; all comparisons have p values < 0.001.
ICD-9-CM procedure code for mechanical ventilation or secondary diagnosis code for acute organ failure
The mean number of pneumonia admissions per hospital meeting criteria for sepsis or respiratory failure and eligible for recoding was 25, with a range of 0 to 250. Hospitals varied in the percentage of pneumonia patients eligible for recoding, with a median of 21% and interquartile range of 15% to 27% (Figure 1).
Figure 1.
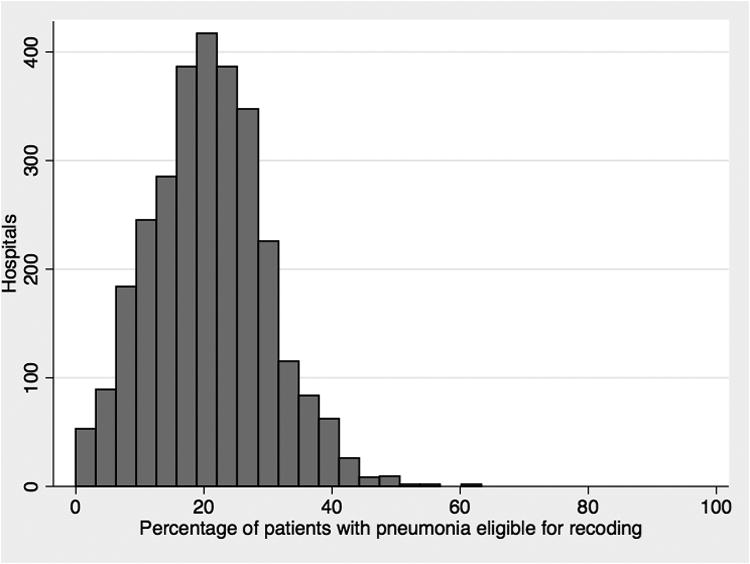
Distribution of patients with pneumonia eligible for recoding to sepsis or respiratory failure among hospitals.
Patient's eligible for recoding are those with a principal ICD-9-CM diagnosis code for pneumonia and an ICD-9-CM procedure code for mechanical ventilation or secondary diagnosis codes for acute organ failure.
Mortality rate changes after recoding
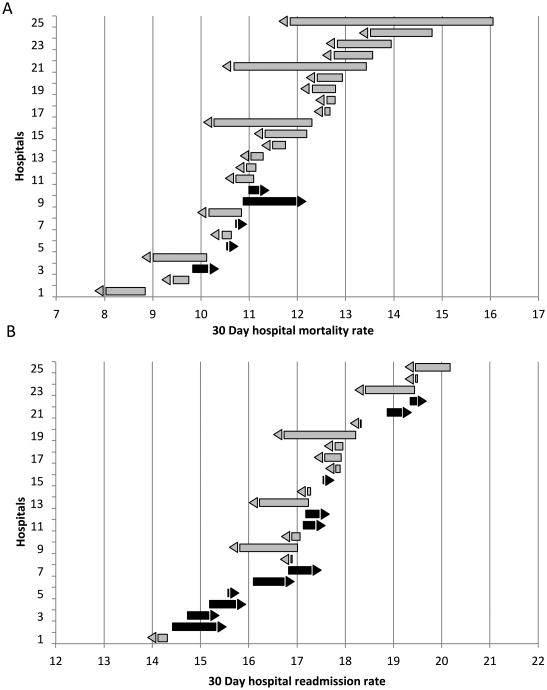
To illustrate the range of effect on mortality rates after individual hospitals recoded patients, we performed simulations by randomly selecting 25 hospitals to recode all their eligible patients to a principal diagnosis of sepsis or respiratory failure (Figure 2A). Among the 25 hospitals, 19 improved (95% CI: 16 - 23) after recoding, with a mean improvement in their morality rate of 0.94 percentage points (95% CI: 0.67 – 1.38). Among hospitals that worsened after recoding, their mortality rate increased by a mean of 0.21 percentage points (95% CI: 0.05 – 0.46)
Figure 2.
Change in hospital-level pneumonia 30-day morality and 30-day hospital readmission rates after recoding eligible patients.
Change in (A) pneumonia 30-day mortality rate and (B) pneumonia 30-day hospital readmission rate when 25 randomly selected hospitals identify and recode all eligible patients with pneumonia to a primary diagnosis of sepsis or respiratory failure. Data are from representative simulations. Arrows show direction of change in the outcome but do not contribute to degree of change. Patient's eligible for recoding are those with a principal ICD-9-CM diagnosis code for pneumonia and ICD-9-CM procedure code for mechanical ventilation or secondary diagnosis code for acute organ failure.
Hospitals with the greatest incentive to improve mortality (i.e. those above the 50th percentile) were able to significantly reduce their mortality rates as well (Table 2). For example, when 100 hospitals (7% of hospitals above the 50th percentile) engaged in recoding, they improved their mortality rate on average by 0.54 percentage points (95% CI: 0.42% - 0.66%) and 1.09 percentage points (95% CI: 0.94% - 1.28%) after recoding half or all of their eligible patients, respectively. Overall, 90 out of 100 of these hospitals experienced some improvement after recoding all eligible patients (95% CI: 84 - 95). Forty-one successfully dropped below the 50th percentile (95% CI: 33 – 52), potentially improving their reimbursement under VBP. To attain these gains, the median number of patients a hospital recoded was 18 (9 – 31, IQR). While many hospitals improved their rankings and dropped to below the 50th percentile, other hospitals that did not recode patients worsened, moving above the 50th percentile. Also, when a higher number of hospitals engaged in recoding the improvements seen by individual hospitals were reduced (online supplemental eTable 2 and eFigure 2). For example, when 500 hospitals above the 50th percentile for mortality recoded all eligible patients, only 35 per 100 dropped below the 50th percentile (compared with 41 dropping below the 50th percentile when 100 hospitals engaged in recoding).
Table 2. Improved pneumonia 30-day mortality and hospital readmission rates when hospitals above the 50th percentile recoded patients to a primary diagnosis of sepsis or respiratory failure.
| When 100 hospitals with mortality rates above the 50th percentile recoded patients | After half of eligible patients recoded | After all eligible patients recoded |
|---|---|---|
| Average percent decrease in mortality rate among the hospitals (95% CI) | 0.54 (0.42-0.66) | 1.09 (0.94-1.28) |
| Number who improved out of 100 hospitals (95% CI) | 81 (73-88) | 90 (84-95) |
| Number who dropped below the 50th percentile out of 100 hospitals (95% CI) | 22 (15-29) | 41 (33-52) |
| Number of patient's recoded per hospital (median, IQR) | 9 (5-16) | 18 (9-31) |
| When 100 hospitals with readmission rates above the 50th percentile recoded patients | After recoding half of eligible patients | After recoding all eligible patients |
| Average percent decrease in readmission rate among the hospitals (95% CI) | 0.16 (0.09-0.25) | 0.34 (0.19-0.45) |
| Number who improved out of 100 hospitals (95% CI) | 61 (51-70) | 66 (54-75) |
| Number who dropped below the 50th percentile out of 100 hospitals (95% CI) | 10 (4-16) | 15 (9-22) |
| Number of patient's recoded per hospital (median, IQR) | 9 (4-16) | 17 (9-32) |
Results are means and 95% confidence interval estimates from Monte-Carlo simulations unless otherwise stated. Confidence intervals are percentiles of the simulated results. In each simulation: (1) 100 hospitals are selected to recode patients (2) among selected hospitals, 50% or 100% of patients with pneumonia and organ failure are dropped (recoded) and the mortality or readmission rate is re-calculated. Patients eligible for recoding are those with a primary ICD-9-CM code for pneumonia and ICD-9-CM procedure code for mechanical ventilation or secondary code for acute organ failure
Readmission rate changes after recoding
To illustrate the range of effect on readmission rates after recoding, we randomly selected 25 hospitals to recode all their eligible patients to sepsis or respiratory failure (Figure 2B). Among the 25 hospitals, 13 improved their readmission rates after recoding (95% CI: 9 - 18). Among the hospitals that improved, their readmission rate decreased by an average of 0.50 percentage points (95% CI: 0.31 – 0.77) while among the hospitals that worsened, their readmission rate increased by an average of 0.30 percentage points (95% CI: 0.17 – 0.44).
Hospitals with the greatest incentive to reduce their hospital readmission rates (i.e. those above the 50th percentile) also improved by recoding eligible patients (Table 2). For example, if 100 hospitals (7% of the group) recoded patients, their readmission rates decreased on average by 0.16 percentage points (95% CI: 0.09% - 0.25%) and 0.34 percentages points (95% CI: 0.19% - 0.45%) after recoding half or all their eligible patients respectively. Sixty-six out of the 100 hospitals improved overall (95% CI: 54 - 75) after recoded all eligible patients, and 15 of 100 dropped to below the 50th percentile (95% CI: 9 - 22), effectively excluding themselves from CMS's pneumonia readmission penalties. Similarly to the mortality analysis, although these hospitals improved, other hospitals not recoding patients worsened, moving above the 50th percentile. In simulations where a larger number of hospitals recoded patients, the associated gains for individual hospitals engaging in recoding were slightly less, for example, 14 per 100 hospitals dropped below the 50th percentile when 500 hospitals engaged in recoding (supplemental online eTable 2).
Population effects of recoding pneumonia patients
Both population-level pneumonia morality rates and readmission rates decreased when a large numbers of hospitals adopted the practice of recoding patients (Table 3). When 50% of the overall hospital cohort (1458 hospitals) recoded all eligible patients, the overall mortality rate dropped from 11.8% to 10.6% and the readmission rate dropped from 17.1% to 16.8%. Although both hospitals that recoded patients as well as those who did not recode patients improved, gains were greater for hospitals that recoded patients. At the same time, the rankings of hospitals that recoded patients improved while the ranking of hospitals that did not recode patients worsened. Among hospital rankings for mortality, hospitals that recoded improved their ranking by 242 places on average, while hospitals that did not recode worsened their ranking by 241 places on average.
Table 3. Population-based effects after half of studied hospitals recoded all eligible patients with pneumonia to sepsis or respiratory failure.
| Before recoding | After recoding | |
|---|---|---|
| Number of Pneumonia hospitalizations | N=320,650 | N=285,527 |
| Risk standardized Mortality (overall) | 11.7 | 10.6 |
| Mortality for Hospitals that recoded | 11.8 | 10.2 |
| Mean change in ranking | improved by 235 | |
| Mortality for Hospitals that did not recode | 11.8 | 11.0 |
| Mean change in ranking | worsened by 235 | |
| Risk standardized readmission (overall) | 17 | 16.7 |
| Readmission For hospitals that recoded | 17.1 | 16.7 |
| Mean change in ranking | improved by 37 | |
| Readmission For hospitals that did not recode | 17.1 | 16.8 |
| Mean change in ranking | worsened by 37 |
Results are percentages unless otherwise stated. Patients eligible for recoding are those with a primary ICD-9-CM diagnosis code for pneumonia and ICD-9-CM procedure code for mechanical ventilation or secondary diagnosis code for acute organ failure
Discussion
In this study, we explored whether hospitals can improve their publically reported pneumonia outcome measures by gaming, i.e. recoding eligible patients with pneumonia to a principal diagnosis of sepsis or respiratory failure. We found the opportunity for improvement to be substantial—a large number of hospitals above the 50th percentile for mortality, and many hospitals above the 50th percentile for readmission dropped to below the 50th percentile after recoding eligible patients. A hospital's ability to improve, however, depended both on how aggressively they identified all patients eligible for recoding, as well as the behavior of other hospitals within the system. As more hospitals engaged in recoding overall, or as fewer eligible patients were recoded at an individual hospital, the ability for an individual hospital to improve their mortality or readmission rates diminished but never disappeared.
Despite attempts to risk-adjust pneumonia mortality and readmission rates, patients with sepsis or respiratory failure have a higher severity of illness that is not fully captured in current CMS risk adjustment methods. By definition, patients meeting criteria for sepsis or respiratory failure have acute organ dysfunction (22), but current CMS risk-adjustment only includes age, sex, and comorbidities. As a consequence, hospitals able to exclude this sicker population from their denominator appear to have better outcomes. Importantly, removing this sickest group of pneumonia patients by up-coding is a perfectly acceptable practice given their current claims-based definitions and the current international consensus conference definition of sepsis (22).
Our study confirms recent data linking hospitals' coding practice for pneumonia to pneumonia-specific mortality and makes significant additional contributions to previous work. We show for the first time that coding practice can affect pneumonia readmission rates; and in investigating the system-wide impact of this practice, found that hospitals not engaged in recoding could potentially be harmed. Rothberg and colleagues examined the Premier Perspective database and demonstrated that a hospital's coding practice for pneumonia was associated with its reported in-hospital mortality (12). An important limitation of this study was its focus on in-hospital mortality, an outcome influenced by hospital discharge practice and thus may not accurately reflect the quality of care delivered during hospitalization (23). In the current study, we demonstrated that pneumonia coding had a similar influence on the preferred measure of 30-day mortality in the Medicare population.
Our results have important financial implications for hospitals caring for patients with pneumonia. Currently, hospitals with excessive readmission rates for pneumonia, congestive heart failure, or acute myocardial infarction are at risk for up to 2% cuts to their yearly Medicare reimbursement, increasing to up to 3% in 2015 under the hospital readmission reduction program (8). Similarly, poor performers with respect to mortality for these conditions are also subject to a 1% cut increasing to 2% by 2017 under the value based purchasing program (24). Recoding pneumonia patients could reduce a hospitals financial risks and increase DRG-based payment given the higher cost for sepsis (mean inpatient costs $18,600) and respiratory failure (mean inpatient costs $21,700) relative to pneumonia (mean inpatient costs $9,500) (1). Adequately performing hospitals may feel pressure as the distribution of outcomes changes when greater numbers of hospitals engage in recoding. These high performing hospitals may be subject to penalties because they now appear “worse” than their peers.
Given these strong financial incentives, and the greater awareness and push for early identification and treatment of sepsis (25), we suspect more patients with pneumonia will be labeled as sepsis. This potential for shifts in coding practice across all hospitals may be important sources of variation in both case definition and outcomes of sepsis and pneumonia that need to be accounted for in future longitudinal studies of patients with pneumonia or when assessing the effectiveness of measures like Hospital Compare, HRRP, or VBP initiatives. An apparent improvement in mortality or readmission rates after institution of these measures may be detected simply because the sickest patients are now labeled with other diagnoses—the so-called “Will Rogers” phenomenon (26).
In light of the opportunity to avoid financial penalties by recoding patients with pneumonia, CMS should consider changing their method for calculating hospital risk-adjusted mortality and readmission rates for pneumonia. One potential approach would be to include organ failure codes in the risk adjustment models. However, we do not favor this approach because it would potentially limit the measures ability to detect poor performing hospitals. For example, if hospitals poorly manage pneumonia their patients may develop more organ dysfunction. Adjusting for the organ dysfunction in this setting would effectively undermine CMS's intent to penalize hospitals that deliver poor care. A second approach would be to include patients with a primary diagnosis of sepsis or respiratory failure and secondary pneumonia in the case definition. However, this population is more heterogeneous and includes patients who developed pneumonia as a complication of their hospitalization. Perhaps the optimal solution would incorporate present on admission codes, which have been included as part of Medicare data since mid-2008 (27,28). These codes would catch patients admitted with pneumonia if their primary diagnosis was sepsis or respiratory failure, while ensuring that the pneumonia did not develop during the course of the hospitalization, consistent with CMS's original goal.
Our current study has several limitations. We were unable to determine if hospitals are currently recoding patients with pneumonia to improve their reported outcomes, instead we were only able to explore scenarios that assess how easily this could occur. Wide variability in how hospitals code patients with pneumonia, however, suggests that some hospitals may be working harder than others to up-code eligible patients. There may be other reasons for coding variation between hospitals. For example, some hospitals may have a more developed coding infrastructure, and patients at those hospitals may be more likely to be coded as sepsis if they meet criteria. In addition, we used only a single years worth of Medicare data in our simulations, in contrast to Medicare's methods, where three years of data are used to calculate hospital outcomes. This raises the potential that the observed changes in outcomes may be larger than what is possible in practice. Also, the financial benefits that hospitals gain through recoding may take longer to be realized. Finally, we were unable to directly estimate the financial gains that would result from changes in mortality and readmission rates for PNA. Pneumonia outcomes are only two of several factors included in the calculation of hospital penalties by CMS in the HRRP and VBP programs (9,29).
Conclusion
In this paper, we showed that currently penalized hospitals have the ability to improve their pneumonia mortality and readmission rates through gaming, by simply re-labeling their sickest patients with pneumonia to sepsis or respiratory failure. We also showed the significant system-level effects of this practice—that overall mortality and readmission rates will drop, and hospitals not engaged in recoding may be harmed. We believe the incentives for hospitals to engage in recoding their sickest patients with pneumonia is simply too great for them not to adopt the practice. CMS should carefully weigh potential changes to their method of calculating pneumonia outcome measures to make them less susceptible to gaming and more reflective of the true differences in quality of care provided to patients with pneumonia.
Supplementary Material
Acknowledgments
Financial Support: Supported by grants to Dr. Sjoding, NIH T32HL007749, Dr. Iwashyna from the Department of Veterans Affairs Health Services Research & Development Services - IIR 11-109 and National Institute of Aging (R21AG044752), Dr. Dimick from the National Institute of Aging (R01AG039434), and Dr. Cooke from the Agency for Healthcare Research and Quality (K08HS020672). These views expressed herein do not necessarily represent the views of the United States Government. Dr. Dimick is a consultant and equity owner of ArborMetrix, Inc, which provides software and analytics for measuring hospital quality and efficiency. The company had no role in the study herein.
Copyright form disclosures: Dr. Sjoding received support for article research from the National Institutes of Health (NIH). Dr. Iwashyna disclosed government work. Dr. Dimick consulted for, is employed by, and has stock with ArborMetrix (Equity owner). He received support for article research from the NIH. His institution received grant support from the NIH (RO1) and RO1/R21. Dr. Cooke received support for article research from the Agency for Healthcare Research and Quality. His institution received grant support from the AHRQ (K08HS020672).
Footnotes
Conflict of Interest Disclosure: No author's have conflicts of interest to disclose
References
- 1.Torio C, Andrews R. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. [Accessed May 23, 2013];Statistical Brief #160. https://http://www.hcup-us.ahrq.gov/reports/statbriefs/sb160.pdf. [PubMed]
- 2.Meehan TP, Fine MJ, Krumholz HM, et al. Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA : the journal of the American Medical Association. 1997 Dec 17;278(23):2080–2084. [PubMed] [Google Scholar]
- 3.Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: A profile at state and national levels. JAMA : the journal of the American Medical Association. 2000 Oct 4;284(13):1670–1676. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- 4.Lindenauer PK, Bernheim SM, Grady JN, et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for medicare beneficiaries with pneumonia. Journal of hospital medicine : an official publication of the Society of Hospital Medicine. 2010 Jul-Aug;5(6):E12–18. doi: 10.1002/jhm.822. [DOI] [PubMed] [Google Scholar]
- 5.Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals--the Hospital Quality Alliance program. The New England journal of medicine. 2005 Jul 21;353(3):265–274. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. Hospital Compare. [Accessed April 7, 2014]; http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalCompare.html.
- 7.Lausch K, Shigekawa E, Stroumsa D, Tabak R. An In-depth Look at Six Cost Containment Programs in the Affordable Care Act. [Accessed June 16, 2014];2014 http://www.chrt.org/assets/policy-papers/CHRT-An-In-depth-Look-at-Six-Cost-Containment-Programs-in-the-ACA.pdf.
- 8.James J. Medicare Hospital Readmission Reduction Program. [Accessed June 18, 2014];Health Policy Briefs. 2013 https://http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=102.
- 9.Centers for Medicare & Medicaid Services. Hospital Value-Based Purchasing. [Accessed June 12, 2014]; http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html?redirect=/hospital-value-based-purchasing.
- 10.Bratzler DW, Normand SL, Wang Y, et al. An administrative claims model for profiling hospital 30-day mortality rates for pneumonia patients. PloS one. 2011;6(4):e17401. doi: 10.1371/journal.pone.0017401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003-2009. JAMA : the journal of the American Medical Association. 2012 Apr 4;307(13):1405–1413. doi: 10.1001/jama.2012.384. [DOI] [PubMed] [Google Scholar]
- 12.Rotherberg MB, Pekow PS, Priya A, Lindenauer PK. Variation in Diagnostic Coding of Patients with Pneumonia and Its Association with Hospital Risk-Standardized Mortality Rates. Annals of internal medicine. 2014;160(6):380–388. doi: 10.7326/M13-1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grady JN, Lin Z, Wang Y, et al. 2013 Measure Updates and Specifications: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measures. [Accessed June 3, 2014];2013 http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic/Page/QnetTier3&cid=1163010421830.
- 14.Grady JN, Zhenqui L, Wang Y, et al. 2013 Measures updates and specifications report: hospital-level 30-day risk-standardized readmission measures for acute myocardial infarction, heart failure, and pneumonia. [Accessed June 4, 2014];2013 https://http://www.qualitynet.org/dcs/ContentServer?cid=1219069855841&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page.
- 15.AHRQ. Clinical Classification Software. [Accessed Febuary 7, 2014];2014 http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 16.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Critical care medicine. 2001 Jul;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Iwashyna TJ, Odden A, Rohde J, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Medical care. 2014 Jun;52(6):e39–43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA : the journal of the American Medical Association. 2010 Oct 27;304(16):1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prescott HC, Langa KM, Lui V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. American Journal of Respiratory and Critical Care Medicine. 2014 Jul 1;190(1):62–69. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li P, Kim MM, Doshi JA. Comparison of the performance of the CMS Hierarchical Condition Category (CMS-HCC) risk adjuster with the Charlson and Elixhauser comorbidity measures in predicting mortality. BMC health services research. 2010;10:245. doi: 10.1186/1472-6963-10-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burton A, Altman DG, Royston P, Holder RL. The design of simulation studies in medical statistics. Statistics in medicine. 2006 Dec 30;25(24):4279–4292. doi: 10.1002/sim.2673. [DOI] [PubMed] [Google Scholar]
- 22.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Critical care medicine. 2003 Apr;31(4):1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 23.Drye EE, Normand SL, Wang Y, et al. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Annals of internal medicine. 2012 Jan 3;156(1 Pt 1):19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Medicare & Medicaid Services. Medicare program; hospital inpatient value-based purchasing program; final rule. Fed Regist. 2011;76(88):26490–26547. [PubMed] [Google Scholar]
- 25.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Critical care medicine. 2013 Feb;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 26.Feinstein AR, Sosin DM, Wells CK. The Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. The New England journal of medicine. 1985 Jun 20;312(25):1604–1608. doi: 10.1056/NEJM198506203122504. [DOI] [PubMed] [Google Scholar]
- 27.Wright S. Memorandum Report: Assessment of Hospital Reporting of Present on Admission Indicators on Medicare Claims. [Accessed June 15, 2014];2012 https://oig.hhs.gov/oei/reports/oei-06-09-00310.pdf.
- 28.Goldman LE, Chu PW, Osmond D, Bindman A. The accuracy of present-on-admission reporting in administrative data. Health services research. 2011 Dec;46(6pt1):1946–1962. doi: 10.1111/j.1475-6773.2011.01300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services. Readmission Reduction Program. [Accessed June 23, 2014]; http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.