Summary
Introduction
management of intrasubstance meniscal lesions is still controversial. Intrasubstance meniscal lesions can lead to reduced sports activity and meniscal rupture. Physical therapy is often not satisfactory. Therefore new treatment methods are requested. Platelet Rich Plasma (PRP) has the ability to regenerate tissue; this was proved in several experimental studies. Whether percutaneous injections of PRP are effective in intrasubstance meniscal lesions is unknown. We hypothesize that percutaneous PRP injections lead to pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions.
Materials and methods
ten recreational athletes with intrasubstance meniscal lesions (grade II according to Reicher) proven by MR-Imaging (MRI) were treated by percutaneous injections of PRP in the affected meniscal area. Three sequential injections in seven day intervals were performed in every patient. All injections were performed with image converter. Follow-up MRI was done six months after last injection in every patient. Level of sports activity and amount of pain at athletic loads according to numeric rating scale (NRS-11) were noted in each patient before injections and at the time of follow up MRI after six months. The t-test was used to determine statistical differences.
Results
four of ten patients (40%) showed decrease of meniscal lesion in follow up MRI after six months. Nine of ten patients (90%) complained about short episodes of heavy pain after the injections with average NRS-Score of 7.9 at daily loads after the last injection. Six of ten patients (60%) showed Improvement of NRS-Score at final follow up. Average NRS-Score improved significantly (p=0.027) from 6.9 before injections to 4.5 six month after treatment. Six of ten patients (60%) reported increase of sports activity compared to the situation before injections. In four patients (40%) additional surgical treatment was necessary because of persistent knee pain or progression of meniscal lesion.
Conclusions
percutaneous injections of PRP have the ability to achieve pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions. Therefore it could be considered as a treatment option in patients with persisting pain.
Level of evidence
IV.
Keywords: meniscal lesion, PRP, percutaneous, intrasubstance, grade II
Introduction
Meniscal lesions are frequent. The mean annual incidence is about 60–70 per 100,0001, 2. Meniscal lesions are not only painful, but also responsible for long absences from physical activities. Furthermore, it is suggested that meniscal tears may be a risk factor for cartilage deterioration3. Therefore adequate treatment strategies are required.
On MRI imaging, meniscal lesions may be divided into four grades (0–3) according to Reicher et al.4. A grade 1 lesion of the meniscus shows mucoid degeneration without signs of ruptures, i.e. connection to the meniscal surface. Non-surgical intervention with physical therapy is an accepted treatment approach for this kind of lesion5, 6. On the other hand, grade 3 lesions are complete meniscal ruptures with an interruption of the meniscal surface on MRI. Surgical intervention with meniscal repair showed sufficient treatment results and is considered the therapy of choice especially in athletes and active patients. Partial meniscectomy however is the therapy of choice in older and low demand patients7, 8. Treatment concepts for grade 2 lesions are nevertheless still discussed controversial. A grade 2 lesion is consistent with an intrasubstance defect without surface disruption on MRI, but can be considered a pre-stage meniscal rupture. Intrasubstance meniscal lesions can lead to a reduced physical activity and development of complete meniscal rupture1, 9. Conservative treatment is often not satisfactory10, however, in patients with persisting pain despite conservative treatment surgical options are limited since, by definition, there is no complete meniscal rupture6, 10. Therefore, there is a clinical need for new treatment methods for grade 2 lesion.
Percutaneous injection of Platelet Rich Plasma (PRP) might be a promising treatment option for these patients, as it is minimally invasive and shows the ability to regenerate tissue9. PRP is commonly used in many orthopedic applications, especially in the treatment of tendinopathies11–13. The use of PRP in meniscal repair is an area of growing interest but clinical evidence is lacking and only a few studies are existing14–17. Whether percutaneous injections of PRP are effective in intrasubstance meniscal lesions is unknown. We hypothesize that percutaneous PRP injections lead to pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions.
Materials and methods
Ten patients referred to our hospital between 2012 and 2013 were included in this retrospective study. This study had been approved by the institutional review board of the hospital (University Hospital Basel, Switzerland, ID 191/11) before commencement and meets the ethical standards of this journal18.
All patients were recreational level athletes and forced to quit sport activities because of pain within the knee joint at athletic loads. Activities included alpine skiing, cross country skiing, cycling and running. Inclusion criteria were: Patient age ≥18 years, persistent knee joint pain for at least six months and evidence of intramural meniscal lesion grade 2 according to Reicher et al.4 on MRI. All patients failed a six month course of conservative treatment, including activity modification with sport cessation, physiotherapy, and NSAID. Exclusion criteria included osteoarthritis with a Kellgren-Lawrence stadium >2, medial or lateral deviation of the mechanical axis >10mm, prior knee injury or meniscal lesion, generalized inflammatory arthritis, systemic diseases, pregnancy, severe infection, known malignancy, bleeding disorders or anticoagulation, previous knee surgery, ESWT, corticosteroid injection into the knee joint and finally nerve-related symptoms such as radiculopathy.
The Arthrex ACP Double Syringe System™ was used to obtain PRP. This system includes one outer 10 ml syringe. Within this outer syringe, a commercially available 5 ml syringe is connected. Ten millilitres of autologous blood was taken from the antecubital vein with the outer syringe and placed into the Arthrex Centrifuge (Rotofix) and centrifuged for five minutes at 1,500 rpm. During the extracorporeal blood processing, 2 ml of acid-citrate-dextrose (ACD) solution was used to prevent clotting. The system allows supernatant (PRP) transfer from the 10 ml outer syringe into the 5 ml syringe under aseptic conditions. Harvest volume averaged between 2–5 ml. Acquired PRP contained reduced levels of leukocytes compared to the baseline of the whole blood. It could be classified as PRP type 3a according to Mishra et al.19. PRP was prepared fresh at each time and was injected within 30 minutes. Three sequential injections with seven-day intervals were performed in each patient. All injections were performed under fluoroscopy. The injection technique has been standardized in a preceding cadaver trial to ensure correct injection in the different meniscal areas (data not shown). All injections were performed on an outpatient basis. The injection point was the medial or lateral joint space. The joint space was detected with fluoroscopy in anterior-posterior (AP) projection. In mediolateral (ML) projection the syringe was placed according to the affected area to the anterior, intermediate or posterior part of the meniscus. Correct AP projection was ensured by reference to the tibia plateau and femoral notch. Correct ML projection was ensured based on the distal femur with condyles superimposed and joint space free of superimposition. Meniscal tissue was identified by increase and loss of resistance.
After PRP injection, patients remained in the outpatient clinic until pain was considered tolerable and were followed in the outpatient clinic or by telephone interview to detect possible side effects. All patients were allowed to bear full weight, but were advised to avoid physical activities, such as running or jumping, for at least four weeks after the last injection. Ice packs and medication with paracetamol were allowed for post injection pain. NSAID were not allowed for 6 months. Physical therapy was not prescribed during recovery from the injections.
Before treatment and at 6 months follow-up patients were asked to rate their pain on a numeric rating scale (NRS-11) during individual athletic loads, with zero indicating no pain and ten the worst pain imaginable. The t-test was used for statistical analysis with the level of significance set to p<0.05.
MRI of the respective knee joint was performed prior to the first and 6 months after the last injection. All ten patients were imaged on the same 1.5-T MRI scanner (Avanto; Siemens Medical Systems, Erlangen, Germany) using an 8-channel phased-array extremity coil. All MRI examinations consisted of an axial frequency-selective fat-suppressed T2-weighted fast spin-echo (FSE) sequence, a coronal intermediate- weighted FSE sequence, a coronal frequency-selective fat-suppressed intermediate-weighted FSE sequence, a sagittal intermediate-weighted FSE sequence and a sagittal frequency-selective fat suppressed T2-weighted FSE sequence. A section thickness of 3 mm was used. To assure that the slices used for the evaluation of the progression of the meniscal lesion were taken through the same part of the meniscus, the patient was placed in a standardized position and wore a knee splint for reproducible alignment of the leg. Halt of progression was determined when the same grade of meniscal lesion according to Reicher et al.4 was present during follow up examination with same or less size and signal intensity of the lesion. Imaging evaluation was per-formed in a blinded manner by two independent, experienced radiologists.
Results
4 women and 6 men with a mean age of 53.3±13.9 years were included in this study. Mean symptom duration, from the beginning of symptoms to enrolment in the study, was 7.1±0.96 months. Average NRS-Score prior to injection was 6.9±0.99. In MR-imaging all patients showed grade 2 meniscal lesion with preserved meniscal surface and intrasubstance signal abnormality (Tab. 1).
Table 1.
Patients characteristics before and after injections. (Tx: treatment)
| NRS-Score (before Tx) | NRS-Score (6 months after Tx) | Meniscal lesion (before Tx, MRI) | Meniscal lesion (6 months after Tx, MRI) | Decline of intrasubstance signal (MRI) | |
|---|---|---|---|---|---|
| Patient 1 | 6 | 0 | IIb | I | Yes |
| Patient 2 | 7 | 8 | IIb | III | No |
| Patient 3 | 8 | 8 | IIb | III | No |
| Patient 4 | 6 | 6 | IIb | IIb | No |
| Patient 5 | 9 | 5 | IIb | IIb | No |
| Patient 6 | 6 | 2 | IIa | IIa | Yes |
| Patient 7 | 7 | 1 | IIb | IIb | Yes |
| Patient 8 | 7 | 8 | IIb | IIb | No |
| Patient 9 | 7 | 3 | IIb | IIa | Yes |
| Patient 10 | 6 | 4 | IIb | IIb | No |
| Mean (SD) | 6.9 (0.99) | 4.5 (2.99) | IIb | IIb | |
|
| |||||
| p=0.027 | p=0.889 | ||||
Three sequential injections with seven-day intervals were performed in every patient. Maximal 0.5 – 1 ml of PRP could be injected in the meniscal tissue limited by a growing resistance. No systemic or local complications were noted at any time. Six of ten patients (60%) showed Improvement of NRS-Score at athletic loads at final follow up. One patient showed decline of NRS from 7 to 1, another patient from 6 to 0 (Tab. 1). Six of ten patients (60%) reported increase of sports activity compared to the situation before injections and returned to previous sports activity level. Average NRS-Score six months after treatment was reduced significantly (p=0.027) to 4.5 (Tab. 1). Four of ten patients (40%) showed a decrease of meniscal lesion in follow up MRI after six months with decline of intrasubstance signal alteration in sagittal and coronal planes (Figs. 1–4). Nevertheless two patients (20%) showed progression of meniscal lesion in follow up MRI six months after injections with a defect of the meniscal surface. In four patients (40%) additional surgical treatment was necessary because of persistent knee pain at athletic loads and in daily routine. Post procedural pain was reported by almost all patients (90%), with an average NRS score of 7.9 at daily loads after the last injection. All patients required icepack treatment and analgesia with paracetamol. Post treatment pain resolved in three patients (30%) only 5 five days after infiltration.
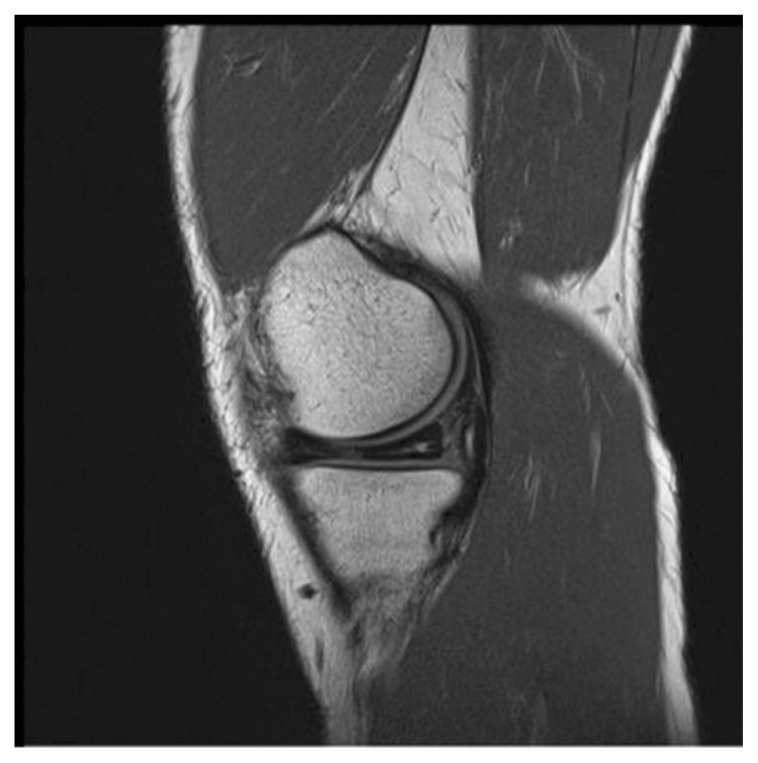
Figure 1.
Meniscal lesion before injections (patient 7).
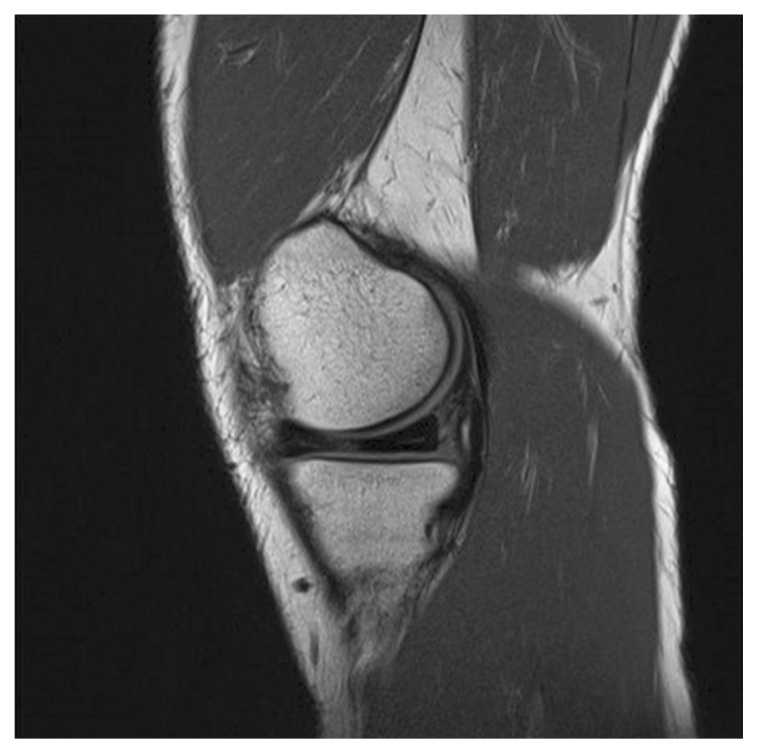
Figure 2.
Meniscal lesion 6 months after injections (patient 7).
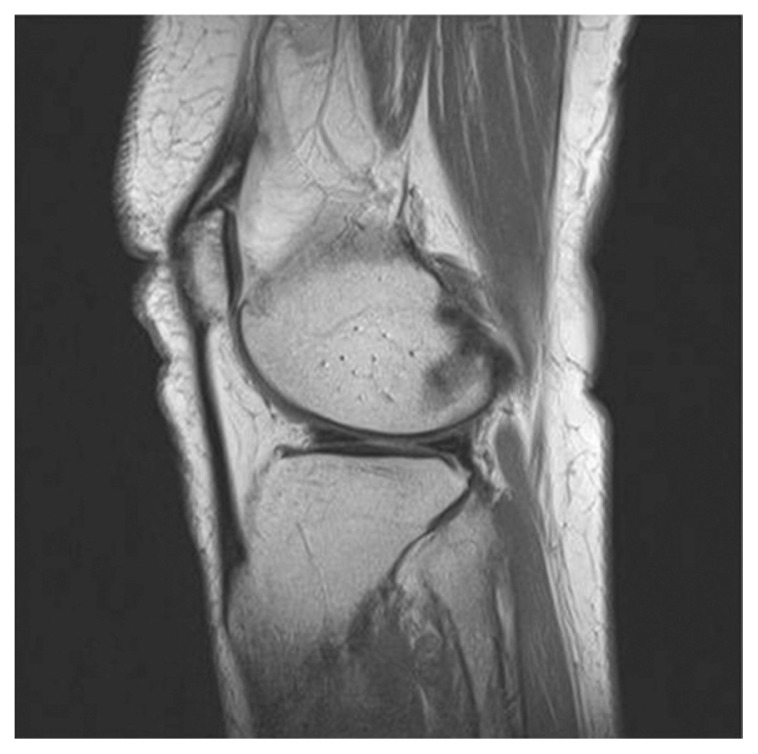
Figure 3.
Meniscal lesion before injections (patient 1).
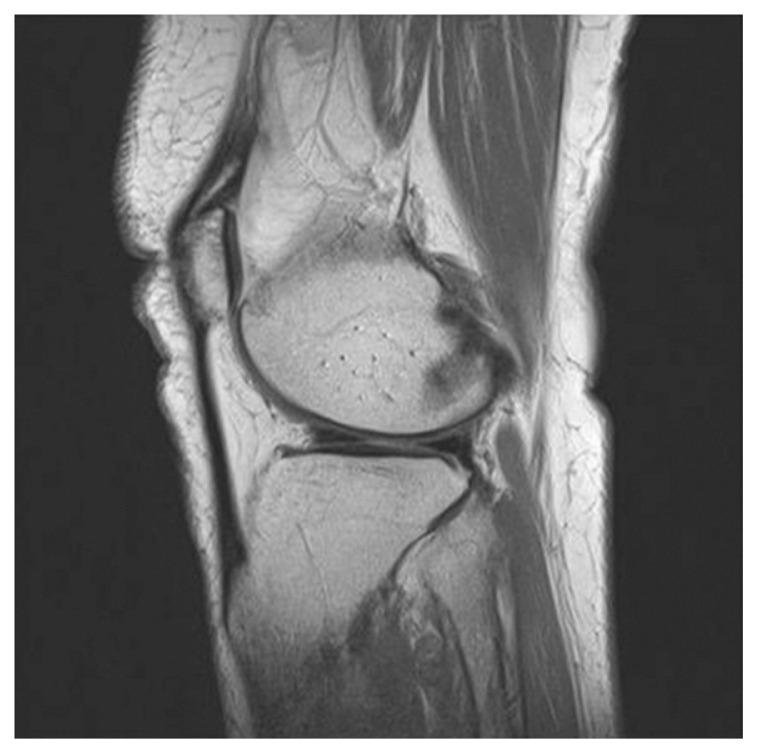
Figure 4.
Meniscal lesion 6 months after injections (patient 1).
Discussion
Percutaneous injections of PRP have the ability to achieve pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions. In the present study 60% of patients showed a significant improvement of NRS score and increase of sports activity after injection. In 40% of patients decrease of meniscal lesion could be seen on MRI.
Several anabolic growth factors have been identified in meniscal tissue repair and regeneration such as basic fibroblast growth factor, TGF-b1, bone morphogenic proteins, insulin-like growth factor-I, vascular endothelial growth factor and PDGF-AB20. PRP is an autologous source of these and other growth factors and might be a promising treatment option in meniscal lesions. In this present study it could be shown that the usage of PRP for intrasubstance meniscal lesions (grade 2) might be beneficial. To date, only a few studies have evaluated the use of PRP for meniscal applications14–17. Ishida et al.16 investigated the use of PRP for meniscal tissue regeneration in an animal trial. Tissue defects treated with PRP showed significantly greater scores for the number of fibro-chondrocytes and production of extracellular matrix compared to platelet poor Plasma (PPP) and controls. The results of this study led the authors to conclude that PRP enhances the healing properties of the inner, avascular meniscus. Moreover a recent clinical trial reported the improved outcome results after open meniscal repair and addition of PRP compared to open meniscal repair alone14. These results are consistent with the results of our present study. However, intrasubstance lesions are considered a special kind of meniscal tear and the evidence for treatment options of these kind of meniscal lesions is rare4, 10, 21. Previous studies often reported unsatisfactory results after conservative treatment7, 10. In contrast, operative intervention with arthroscopic needling or partial menisectomy showed good results in an earlier study10. However, these methods contain inherent perioperative risks. Furthermore, partial menisectomy is a final treatment option and should be reserved for patients with instable meniscus lesions in the white-white area without healing tendency5, 6. As opposed to this, percutaneous injections of PRP represent a low invasive treatment option with combination of growth factor application and meniscal trephination. This percutaneous technique is, if appropriately used, safe, without any considerable risks and can lead to satisfactory clinical results. Therefore it could be used as a first step procedure or at least temporizing treatment option in patients with persisting meniscal pain. However it should be noted that in four patients of present study percutaneous injections remained unsuccessful requiring later surgical treatment. Moreover high post procedural pain was reported in almost all patients with a temporary increase of NRS. The Authors interpreted that pain as a volume-induced post procedural pain attributable to the inability of the rigid meniscal tissue to absorb the load of fluid. On the other hand, this pain can also be caused by leukocytes contained in the PRP22. However, in this present study leucocyte poor PRP was used, which limits possibility of leucocytes induced pain. Nonetheless usage of leucocyte filters for preparation of PRP might be considered in future to further prevent this side effect22–24.
Obviously the present study contains several limitations. Firstly it remains uncertain whether the plasma was always applied in the damaged meniscal area with the percutaneous technique. Usage of a dye such as a radio-contrast agent might be considered in future studies to improve verification of PRP application. This however would further reduce the possible amount of PRP injected within the meniscus. Moreover, knee pain might not only be caused by the meniscal pathology alone, but also, due to the age distribution, by early osteoarthritic changes. PRP showed efficacy in osteoarthritic knee pathology in earlier studies23 and may actually decrease the pain and inflammation even without healing the meniscus in some patients. However, patients with significant osteoarthritic changes (> Kellgren-Lawrence grade 2) were not included in this present study. Moreover further investigations with controlled trials are preferable to validate the significance of this therapeutic tool. Especially the comparison between PRP injections, steroid injections and needling alone seems interesting and should be focused in future studies.
Conclusion
Percutaneous injections of PRP have the ability to achieve pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions. Therefore it could be considered at least as a temporizing treatment option in patients with persisting pain.
References
- 1.Hede A, Jensen DB, Blyme P, Sonne-Holm S. Epidemiology of meniscal lesions in the knee. 1,215 open operations in Copenhagen 1982–84. Acta Orthop Scand. 1990;61(5):435–437. doi: 10.3109/17453679008993557. [DOI] [PubMed] [Google Scholar]
- 2.Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31(12):1644–1648. doi: 10.1097/00005373-199112000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Ding C, Martel-Pelletier J, Pelletier JP. Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: c cross sectional study. J Rheumatolo. 2007;34:776–784. [PubMed] [Google Scholar]
- 4.Reicher MA, Hartzman S, Duckwiler GR, Bassett LW, Anderson LJ, Gold RH. Meniscal injuries: detection using MR imaging. Radiology. 1986;159(3):753–757. doi: 10.1148/radiology.159.3.3754645. [DOI] [PubMed] [Google Scholar]
- 5.Katz JN, Brophy RH, Chaisson CE, de Chaves L. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–1684. doi: 10.1056/NEJMoa1301408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacDonald PB. Arthroscopic partial meniscectomy was not more effective than physical therapy for meniscal tear and knee osteoarthritis. J Bone Joint Surg Am. 2013;95(22):2058. doi: 10.2106/JBJS.9522.ebo745. [DOI] [PubMed] [Google Scholar]
- 7.Laible C, Stein DA, Kiridly DN. Meniscal repair. J Am Acad Orthop Surg. 2013;21(4):2014–2013. doi: 10.5435/JAAOS-21-04-204. [DOI] [PubMed] [Google Scholar]
- 8.Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Boint Joint Surg Am. 2012;94(24):2222–2227. doi: 10.2106/JBJS.K.01584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489–496. doi: 10.1016/j.joms.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Biedert RM. Treatment of intrasubstance meniscal lesions: a randomized prospective study of four different methods. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):104–108. doi: 10.1007/s001670050195. [DOI] [PubMed] [Google Scholar]
- 11.Barrett SE, Erredge ES. Growth factors for chronic plantar fasciitis. Podiatry Today. 2004;17:37–42. [Google Scholar]
- 12.Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34:1774–1778. doi: 10.1177/0363546506288850. [DOI] [PubMed] [Google Scholar]
- 13.Scioli M. Treatment of recalcitrant enthesopathy of the hip with platelet rich plasma- a report of three cases. Clin Orthop Soc News. 2006;6:6–7. [Google Scholar]
- 14.Pujol N, Salle De Chou E, Boisrenoult P, Beaufils P. Platelet-rich plasma for open meniscal repair in young patients: any benefit? Knee Surg Sports Traumatol Arthrosc. 2015;23:51–58. doi: 10.1007/s00167-014-3417-3. [DOI] [PubMed] [Google Scholar]
- 15.Hutchinson ID, Rodeo SA, Perrone GS, Murray MM. Can platelet-rich plasma enhance anterior cruciate ligament and meniscal repair? J Knee Surg. 2014;28:19–28. doi: 10.1055/s-0034-1387166. [DOI] [PubMed] [Google Scholar]
- 16.Ishida K, Kuroda R, Miwa M. The regenerative effects of platelet-rich plasma on meniscal cells in vitro and its in vivo application with biodegradable gelatin hydrogel. Tissue Eng. 2007;13:1103–1112. doi: 10.1089/ten.2006.0193. [DOI] [PubMed] [Google Scholar]
- 17.Zellner J, Mueller M, Berner A. Role of mesenchymal stem cells in tissue engineering of meniscus. J Biomed Mater Res A. 2010;94:1150–1161. doi: 10.1002/jbm.a.32796. [DOI] [PubMed] [Google Scholar]
- 18.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal. Basic principles and recommendations in clinical and field science research. MLTJ. 2013;4:250–252. [PMC free article] [PubMed] [Google Scholar]
- 19.Mishra A, Harmon K, Woodall J, Vieira A. Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol. 2012;13(7):1185–1195. doi: 10.2174/138920112800624283. [DOI] [PubMed] [Google Scholar]
- 20.Bhargava MM, Attia ET, Murrell GA. The effect of cytokines on the proliferation and migration of bovine meniscal cells. Am J Sports Med. 1999;27:636–643. doi: 10.1177/03635465990270051601. [DOI] [PubMed] [Google Scholar]
- 21.Biedert RM. Intrasubstance meniscal tears. Clinical aspects and the role of MRI. Arch Orthop Trauma Surg. 1993;112(3):142–147. doi: 10.1007/BF00449992. [DOI] [PubMed] [Google Scholar]
- 22.Dragoo JL, Braun HJ, Durham JL, Ridley BA, Odegaard JI, Luong R, Arnoczky SP. Comparison of the acute inflammatory response of two commercial platelet-rich plasma systems in healthy rabbit tendons. Am J Sports Med. 2012;40(6):1274–1281. doi: 10.1177/0363546512442334. [DOI] [PubMed] [Google Scholar]
- 23.Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013;41(2):356–364. doi: 10.1177/0363546512471299. [DOI] [PubMed] [Google Scholar]
- 24.Behera P, Dhillon M, Aggarwal S, Marwaha N, Prakash M. Leukocyte-poor platelet-rich plasma versus bupivacaine for recalcitrant lateral epicondylar tendinopathy. J Orthop Surg (Hong Kong) 2015;23(1):6–10. doi: 10.1177/230949901502300102. [DOI] [PubMed] [Google Scholar]