Abstract
Background
The proportion of older people is increasing, therefore their place of residence and place of care at the end of life are becoming increasingly important.
Aim
To compare aspects of end-of-life care among older people in residential homes and home settings in the Netherlands.
Design and setting
Nationwide representative mortality follow-back study among GPs in the Netherlands.
Method
The study included patients aged ≥65 years who died non-suddenly, whose longest place of residence in their last year of life was at home or in a residential home (n = 498). Differences were analysed using Pearson’s χ2 test, Mann-Whitney U tests, and multivariate logistic regression.
Results
Controlling for the differences between the populations in home settings and residential homes, no differences were found in treatment goals, communication about end-of-life care, or use of specialised palliative care between the two settings. However, people living in a residential home were more likely to have received palliative care from a GP than people living at home (OR 2.84, 95% confidence interval [CI] = 1.41 to 5.07). In residential homes, people more often experienced no transfer between care settings (OR 2.76, 95% CI = 1.35 to 5.63) and no hospitalisations (OR 2.2, 95% CI = 1.04 to 4.67) in the last 3 months of life, and died in hospital less often (OR 0.78, 95% CI = 0.63 to 0.97) than those people living at home.
Conclusion
Despite similar treatment goals, care in residential homes seems more successful in avoiding transfers and hospitalisation at the end of life. Especially since older people are encouraged to stay at home longer, measures should be taken to ensure they are not at higher risk of transfers and hospitalisations in this setting.
Keywords: end of life care, general practitioner, palliative care, residential facilities, terminal care
INTRODUCTION
The population of Europe is ageing, with the proportion of those living beyond 60 years increasing each year.1 As a result, there is a growing need for care over a longer period of time, increasing the burden on healthcare systems.2–4 To limit this burden, policy initiatives encourage people to stay at home longer and make less use of relatively expensive institutionalised care.1,5,6
In the Netherlands, older people who are severely care-dependent most often live in nursing homes, where they are cared for by an in-house physician and nursing staff. Older people with lower care needs may either live at home or in a residential home. Residential homes provide continuous on-site nursing care with activities of daily living such as eating or bathing, but do not have on-site medical care and only some provide psychogeriatric care for people with dementia. In both settings care is provided primarily by GPs, who are considered to be appropriate caregivers for many situations including care at the end of life.
Although many people would prefer to die at home, a sizeable percentage would prefer to die in a residential home.7,8 Although it is known that a person’s quality of life in the final phase of life and quality of death can be affected by the care setting, studies often do not directly compare care setting or place of residence.9 Those that do make a direct comparison focus primarily on subjective measures of care, such as the family’s satisfaction with care.10 How the care received by older people living at home compares with that received by those living in a residential home is yet unknown.
Several aspects of end-of-life care that influence its quality might differ depending on the care setting or place of residence of a patient. One of these is recognising when aggressive or curative treatment or hospitalisation is no longer beneficial,11–13 because hospitalisations may complicate care provision and result in a lower quality of death.14 Recognising when the end of life is near has been shown to reduce the chance of hospitalisation in the last month of life, as has having a palliative treatment aim.15 Likewise, the provision of palliative care has been shown to reduce the number of hospitalisations.16,17 These three aspects of care: having a palliative treatment aim, following up with providing palliative care, and reducing unnecessary hospitalisations near the end of life, all play an important role in the quality of end-of-life care and should be present in all care settings.
The aim of this study was to examine and compare different aspects of end-of-life care in the last 3 months of life among older people in residential homes and home settings in the Netherlands. Specific research questions include:
are there population differences between older people in home settings and older people in residential homes?
do treatment goals in the last 3 months of life differ between people in home settings and people in residential homes?
are there differences in palliative care provision for people in home settings and people in residential homes?
do transitions between care settings and hospitalisations in the last 3 months of life differ between people in home settings and people in residential homes?
How this fits in
A growing proportion of older people require care in a variety of settings, with care at home being stipulated as desirable for both the patient and the healthcare system. Studies investigating the effect of setting on quality of end-of-life care have so far focused on subjective measures of care, such as the family’s satisfaction with care, or have not directly compared care settings. The current research directly compares several objective measures of the care received by older patients living at home and living in a residential home. Knowing how end-of-life care for older people differs between settings can help inform clinicians and policy-makers of the potential benefits and pitfalls of specific places of care.
METHOD
Study design and data collection
The data used in this study were collected via the Netherlands Institute of Health Services Research (NIVEL) Primary Care Database, Sentinel Practices, operating since 1970. The network is managed to encompass a sample of 0.8% of the Dutch population, which is representative in terms of age, sex, and population density. GPs are invited to participate on the basis of their practice population characteristics so that the sample remains representative. On accepting the invitation, GPs first participate in a 2-month trial period to assess their reporting accuracy and motivation before becoming regular participants (registering 26 weeks or more of one year, usually for several years). Participating GPs record demographic and care characteristics for all deaths of practice patients using a standardised registration form within 1 week of the patient’s death.18 Participating GPs gave written informed consent at the beginning of each registration year, having been informed of the study objectives and procedures. All patient data were recorded anonymously.
Sample
There were 801 patients who died in the 40 participating GP practices between 1 January 2011 and 31 December 2012.19 All patients who died non-suddenly aged ≥65 years and whose longest place of residence in the last year of life had been a home setting (either their own home or a relative’s home) or a residential home were included, comprising a total sample of 498 patients.
Measurements
Demographic characteristics included sex, age at time of death, cause of death, having dementia, main place of residence in the last year of life, and place of death. In addition, several care characteristics were registered:
Treatment goals
GPs were asked to indicate the importance of a palliative, curative, or life-prolonging treatment goal 2–3 months before death, 2–4 weeks before death, and 1 week before death on a 5-point Likert scale ranging from ‘not important at all’ to ‘very important’. Scores of 4 and 5 were interpreted as that treatment goal being ‘important’.
Palliative care provisions
GPs were asked to indicate whether their patient had received palliative care provided by the GPs themselves, by a GP with formal palliative care training, or by any of a number of specialised palliative care services. Options were: by a palliative care consultant; in a hospice; in a palliative care unit in a hospital; in a palliative care unit in a residential, care, or nursing home; and ‘other’. If a specialised palliative care service had been used, GPs were asked to indicate how many days before death palliative care was first provided. GPs were also asked if the patient had ever expressed a preference for a place of death, a proxy decision-maker, or about any medical end-of-life treatments.
Care trajectories
GPs were asked to indicate when patients were transferred between care settings during the last 3 months of life, and how long patients stayed at each care setting. GPs could give details on a maximum of four care settings and three transitions.
Analyses
Differences between groups were tested using Pearson’s χ2 test or Mann–Whitney U tests. Multivariate logistic regression was used to analyse associations between longest place of residence (as dependent variable) and several care characteristics, while controlling for age, sex, cancer or non-cancer, and having dementia or not. Robust standard errors were used to account for clustering within GP practices. All analyses were performed using Stata (version 12).
RESULTS
Population differences between residential settings
The study included 400 people aged ≥65 years living at home in the last year of life, and 98 who lived in a residential home (Table 1). The average age at death of people living at home was 81 years (SD 23) compared with 87 years (SD 7) for those in a residential home (P = 0.02). Of those living at home, 43% were females compared with 63% of those in a residential home (P<0.001). There were significant differences between the two groups in cause of death (P<0.001). People living at home were more likely to have died of cancer (54%) compared with those in a residential home (25%), whereas those in a residential home were more likely to have died of cardiovascular disease (15% versus 25%), respiratory disease (5% versus 11%), or old age (11% versus 24%). Residents of a residential home were more likely to have dementia (P<0.001), with 16% having mild dementia and 17% having severe dementia, compared with 8% and 5%, respectively, for those living at home.
Table 1.
Characteristics of the study population (n = 498)a
| Home setting (n= 400) | Residential home (n= 98) | ||
|---|---|---|---|
|
| |||
| n (%) | n (%) | P-value | |
| Age at death (mean, SD) | 81 (23) | 87 (7) | 0.02 |
|
| |||
| Sex, female | 171 (43) | 62 (63) | <0.001 |
|
| |||
| Cause of death | |||
| Malignancies | 216 (54) | 24 (25) | <0.001 |
| Cardiovascular disease | 61 (15) | 24 (25) | |
| Respiratory disease | 21 (5) | 11 (11) | |
| Disease of nervous system | 7 (2) | 2 (2) | |
| Stroke (CVA) | 22 (6) | 2 (2) | |
| Old age | 44 (11) | 23 (24) | |
| Other | 27 (7) | 11 (11) | |
|
| |||
| Dementia | |||
| None | 334 (88) | 57 (66) | <0.001 |
| Mild | 29 (8) | 14 (16) | |
| Severe | 18 (5) | 15 (17) | |
Missing data for: cause of death n=3, dementia n=31. CVA = cerebrovascular accident.
Treatment goals in the last 3 months of life
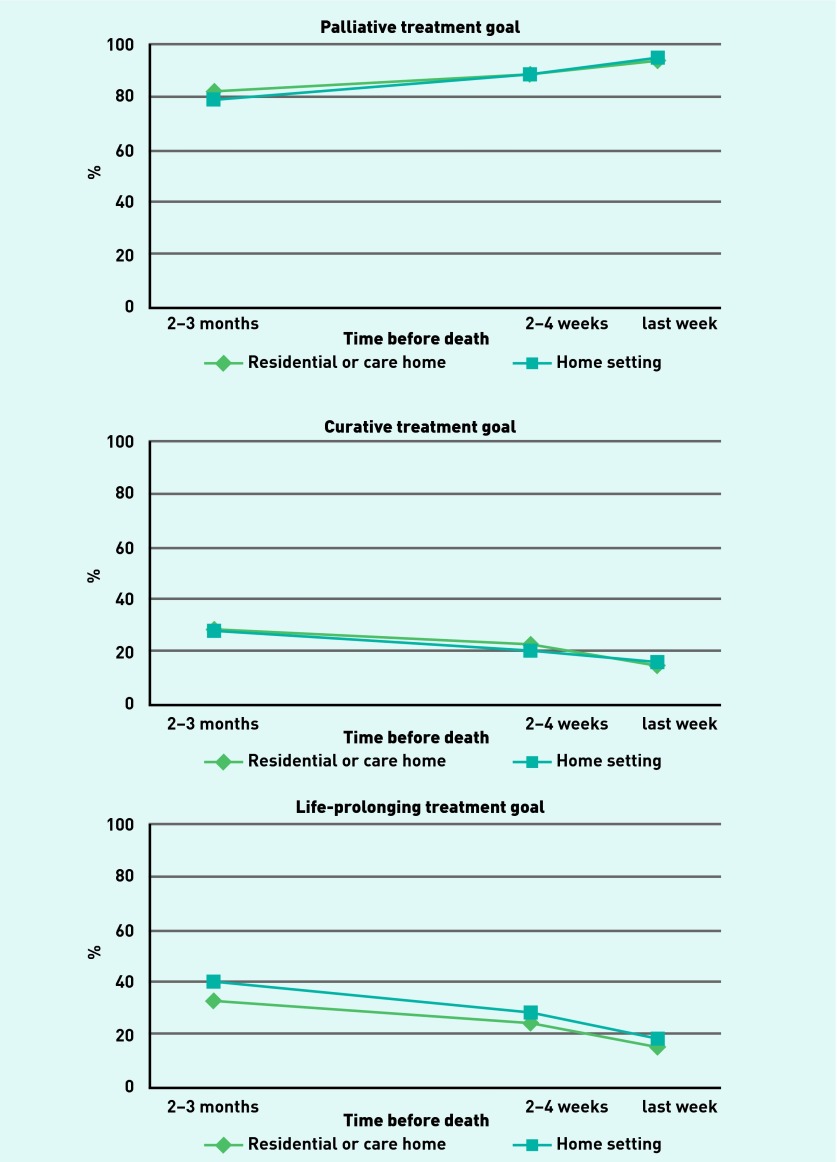
In the 2 to 3 months before death, a palliative treatment goal was considered important for 79% of those living at home and 82% of those in a residential home (Figure 1). This increased to 95% and 94%, respectively, in the last week of life. Two to 3 months before death a curative treatment goal was considered important for 29% of those living at home and 30% of those in a residential home, decreasing to 17% and 15%, respectively, in the last week of life. A life-prolonging treatment goal was considered important in the last 2–3 months of life for 40% of those living at home and 33% of those in a residential home, decreasing to 19% and 15%, respectively, in the last week of life. There were no significant differences in treatment goals between the two groups at any time point, either in bivariate analyses or after controlling for patient characteristics.
Figure 1.
Percentage of patients for whom a palliative, curative, and life-prolonging treatment goal was important during last 3 months of life in home settings and residential homes.
Palliative care provision and communication in the last 3 months of life
Those in a residential home setting were more likely to have received palliative care from their GP (58%) than those living at home (53%, OR 2.84, 95% CI = 1.41 to 5.07) (Table 2). Likewise, palliative care from a GP with formal palliative care training was provided more often to those in a residential home (24%) than those living at home (7%, OR 6.26, 95% CI = 2.88 to 13.66). There were no significant differences in overall frequency of care received from specialised palliative care initiatives, although only those living at home received specialised care in a palliative care unit in a hospital (1%) or from other sources (6%). Specialised palliative care was initiated a median of 14 days before death for those living at home, and 12 days before death for those in a residential home.
Table 2.
Palliative care provision and communication at the end of life of patients in home settings and residential homes (n = 498)a
| Home setting (n= 400) | Residential home (n= 98) | OR (95% CI)b | |
|---|---|---|---|
|
| |||
| n (%) | n (%) | ||
| Palliative care provided by GP | 208 (53) | 56 (58) | 2.84 (1.41 to 5.07) |
| By GP with formal palliative care training | 19 (7) | 16 (24) | 6.26 (2.88 to 13.66) |
|
| |||
| Specialised palliative care initiatives | |||
| Any specialised palliative care | 93 (26) | 10 (12) | 0.57 (0.32 to 1.07) |
| Palliative care consultant | 28 (11) | 3 (5) | 1.47 (0.41 to 5.33) |
| Hospice | 16 (6) | 3 (5) | 1.29 (0.29 to 5.65) |
| Palliative care unit in a hospital | 3 (1) | – | – |
| In-house palliative care service in residential/care/nursing home | 15 (6) | 3 (5) | 0.695 (0.14 to 3.48) |
| Other | 24 (6) | – | – |
|
| |||
| Initiation of palliative care in days before death (median) | 14 | 12 | 1.005 (0.997 to 1.01) |
|
| |||
| GP was aware of patient’s preference | |||
| About a medical end-of-life treatment | 204 (52) | 49 (51) | 1.56 (0.85 to 2.86) |
| For place of death | 224 (56) | 53 (55) | 1.55 (0.67 to 3.61) |
| For proxy decision-maker | 113 (29) | 25 (26) | 1.27 (0.77 to 2.1) |
Missing data for: palliative care received n=28, initiation of palliative care in days before death n=218, preference end-of-life treatment n=7, preference place of death n= 3, preference proxy n=7.
Multivariate logistic regression controlling for age, cancer/non-cancer, dementia, and sex. Reference group is home setting.
The GPs were aware of their patients’ preference about a medical end-of-life treatment in 52% of cases for those living at home and 51% of cases for those in a residential home. The patient’s preference for a place of death was known in 56% of cases for those living at home and 55% of cases for those in a residential home. The patient had expressed a preference for a proxy decision-maker in 29% of cases for those living at home and 26% of cases for those in a residential home. There were no significant differences between groups in the GPs’ awareness of patients’ preferences.
Transitions between care settings in the last 3 months of life
People living in a residential home had not experienced any transitions between care settings in the last 3 months of life in 69% of cases, compared with 46% of those living at home (OR 2.76, 95% CI = 1.35 to 5.63) (Table 3). For 17% of those in a residential home and 34% of those living at home, there was one transition in the last 3 months of life (OR 0.29, 95% CI = 0.12 to 0.67). There were no significant differences between the groups for those who experienced two or more transitions. The most frequent care trajectory for those who experienced at least one transition was to move from their place of residence to hospital, occurring in 25% of cases for those living at home and 10% of cases for those in a residential home (OR 0.25, 95% CI = 0.11 to 0.58). In the last week of life, 22% of those living at home and 15% of those in a residential home were transferred to another care setting.
Table 3.
Transitions between care settings in the last 3 months of life and place of death of people in home settings and residential homes (n = 498)a
| Home setting (n= 400) | Residential home (n= 98) | OR (95% CI)b | |
|---|---|---|---|
|
| |||
| n (%) | n (%) | ||
| Transitions between care settings | |||
| Number of transitions in the last 3 months of lifec | |||
| None | 183 (46) | 68 (69) | 2.76 (1.35 to 5.63) |
| 1 | 134 (34) | 17 (17) | 0.29 (0.12 to 0.67) |
| 2 | 61 (15) | 11 (11) | 0.77 (0.32 to 1.81) |
| 3 or more | 22 (6) | 2 (2) | 0.36 (0.05 to 2.38) |
|
| |||
| Type of trajectory in the last 3 months of lifed | |||
| Residence → Hospital | 100 (25) | 10 (10) | 0.25 (0.11 to 0.58) |
| Residence → Hospital → Residence | 33 (8) | 7 (7) | 1.38 (0.51 to 3.74) |
| Residence → Hospital → Residence → Hospital | 8 (2) | 1 (1) | 0.63 (0.05 to 8.4) |
| Hospital → Residence | 8 (2) | – | – |
| Residence → Palliative care unit/hospice | 13 (3) | – | – |
| Residence → Hospital → Palliative care unit/hospice | 12 (3) | – | – |
|
| |||
| Transferred in last week of life | 87 (22) | 15 (15) | 0.61 (0.25 to 1.52) |
|
| |||
| Hospitalisations | |||
| Number of hospitalisations in last 3 months of lifec | |||
| None | 211 (53) | 71 (72) | 2.2 (1.04 to 4.67) |
| 1 | 169 (42) | 25 (26) | 0.46 (0.21 to 1.03) |
| 2 | 20 (5) | 2 (2) | 0.76 (0.32 to 1.803) |
|
| |||
| If hospitalised, number of days (mean, SD) | 12.2 (12.5) | 10.6 (10.7) | 0.97 (0.91 to 1.02) |
|
| |||
| Death in hospital | 119 (30) | 16 (16) | 0.78 (0.63 to 0.97) |
|
| |||
| Died at place of preference | 176 (79) | 41 (79) | 0.88 (0.38 to 2.02) |
Missing data for: transitions n=4, place of death n= 4, number of days hospitalised n=11, died at place of preference n=265.
Multivariate logistic regression controlling for age, cancer, dementia, and sex. Reference group is home setting.
Reference categories as follows: none versus any; 1, 2, or 3 or more versus none.
Only trajectories that applied to more than 1% of people in either group are shown.
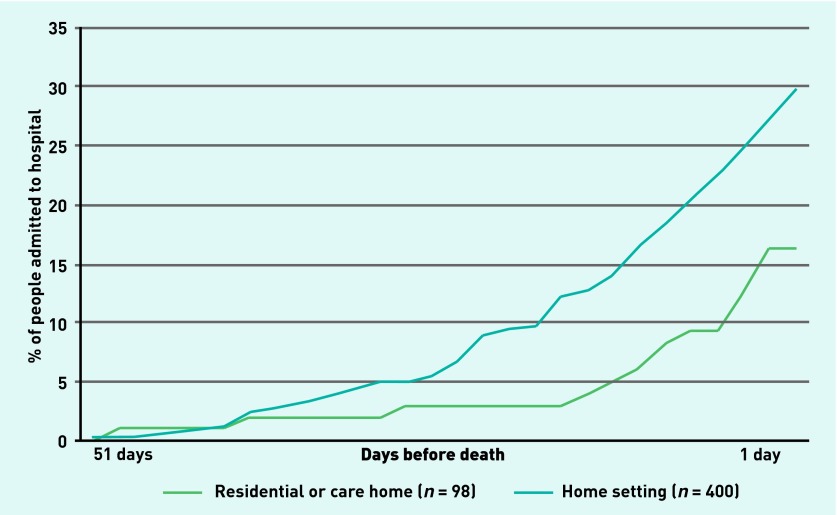
Hospitalisations in the last 3 months of life were less frequent for those in a residential home, where 72% were not hospitalised during this time, than for those living at home, where 53% were not hospitalised (OR 2.2, 95% CI = 1.04 to 4.67). People living at home who were hospitalised, spent a total average of 12 days (SD 12.5) in hospital, compared with an average of 11 days (SD 11) for those in a residential home. People in a residential home were less likely to die in hospital (16% of cases) than people living at home (30% of cases; OR 0.78, 95% CI = 0.63 to 0.97). In both groups, 79% of people died at their place of preference.
The maximum length of hospital stay for those whose stay ended in death in hospital was 51 days (Figure 2). Those living at home were more likely to be admitted to hospital longer before death than those in a residential home (OR 1.1 per day, 95% CI = 1.01 to 1.19).
Figure 2.
Timing of hospitalisation in days before death for patients who died in hospital from home settings and from residential homes (n = 498).
DISCUSSION
Summary
This study found that home settings and residential homes cater to different populations in terms of age, sex, cause of death, and having dementia. Of the three aspects mentioned earlier as playing a role in the quality of end-of-life care, recognising a palliative treatment goal did not differ between settings after controlling for patient characteristics. The provision of palliative care apparently did differ, with people living in a residential home significantly more likely to receive palliative care from a GP with or without formal palliative care training than people living at home. In contrast, people living at home received palliative care from a larger variety of specialised palliative care providers than those living in a residential home. Furthermore, people living in a residential home had lower odds of transfers and hospitalisation near the end of life, and of dying in hospital, than people living at home.
Strengths and limitations
To the authors’ knowledge, this nationwide representative study is the first to compare directly end-of-life care received by older patients living at home and those living in a residential home. By investigating objective measures of care, this knowledge adds to and improves on studies focusing on subjective measures such as the family’s satisfaction with care.
As this study was retrospective in nature, the participating GPs may have experienced recall bias in answering, especially for questions regarding aspects of care occurring long before death. This risk was minimised by having the survey completed within 1 week of death. Due to the nature of the data, it was not possible to ascertain the degree to which people were supported by or received care from informal caregivers, such as a spouse or children. Finally, it is important to realise that this study pertains to people living at home or in a residential home and does not include those living in a nursing home, although this distinction in long-term care structures may be different in other European countries.
Comparison with existing literature
The higher transfer rates of those living at home require attention because there is a trend towards encouraging older people to stay at home longer in an effort to decrease the growing burden on the long-term care system.1,6 Although there have been many initiatives to decrease unnecessary hospitalisations from long-term care settings,20,21 less attention has been paid to hospitalisations from a home setting, although these too are unnecessary or avoidable in some cases.15 The availability of primary care (particularly GP care) has been shown to decrease avoidable hospitalisations both in general21,22 and specifically from long-term care settings.23,24
Implications for practice
The fact that those people living in a residential home receive palliative care more than twice as often from their GP as those living at home, and more frequently receive specialised palliative care from a GP with formal palliative care training, could be both a cause and an effect of their lower transfer and hospitalisation rates at the end of life. GPs serving the population of a residential home may be more experienced and more confident in serving the care needs of someone at the end of life, making them less likely to transfer patients or have them hospitalised at the end of life. Alternatively, if there is more reluctance to transfer older patients from a residential home to hospital than those living at home — possibly because they are more frail — the GP automatically becomes the designated person for providing palliative care.
The lower transfer rates of older people in a residential home may also be a consequence of their symptoms being investigated to a lesser degree, to avoid burdensome interventions not in the patient’s best interests. Conditions potentially requiring hospital care, such as cancer, could then go undiagnosed. Older people living at home may also have more need for a transfer to a different care setting or to hospital because organising home care 24 hours per day can be difficult, especially at short notice. Initiatives aimed at improving the provision of palliative care in home settings specifically,25 or in addition to other settings,26,27 may prove valuable in decreasing this risk.
Acknowledgments
The authors acknowledge other collaborators of EURO IMPACT (further details of these are available from the authors on request).
Funding
EURO IMPACT — European Intersectorial and Multidisciplinary Palliative Care Research Training was funded by the European Union Seventh Framework Programme (FP7/2007–2013, grant number 264697).
Ethical approval
Ethical approval is not required for posthumous collection of anonymous patient data in the Netherlands.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Social Protection Committee. European Commission . Adequate social protection for long-term care needs in an ageing society. Brussels: European Commission; 2014. [Google Scholar]
- 2.Polder JJ, Barendregt JJ, Van Oers H. Health care costs in the last year of life: the Dutch experience. Soc Sci Med. 2006;63(7):1720–1731. doi: 10.1016/j.socscimed.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Langton JM, Blanch B, Drew AK, et al. Retrospective studies of end-of-life resource utilization and costs in cancer care using health administrative data: a systematic review. Palliat Med. 2014;28(10):1167–1196. doi: 10.1177/0269216314533813. [DOI] [PubMed] [Google Scholar]
- 4.Curtis JR, Engelberg RA, Bensink ME, Ramsey SD. End-of-life care in the intensive care unit: can we simultaneously increase quality and reduce costs? Am J Respir Crit Care Med. 2012;186(7):587–592. doi: 10.1164/rccm.201206-1020CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardiner C, Brereton L, Frey R, et al. Exploring the financial impact of caring for family members receiving palliative and end-of-life care: a systematic review of the literature. Palliat Med. 2014;28(5):375–390. doi: 10.1177/0269216313510588. [DOI] [PubMed] [Google Scholar]
- 6.Rijksoverheid [Dutch Parliament] Elderly live independently longer [In Dutch] http://www.rijksoverheid.nl/onderwerpen/ouderenzorg/ouderen-langer-zelfstandig-wonen (accessed 28 Aug 2015).
- 7.Abarshi E, Onwuteaka-Philipsen B, Donker G, et al. General practitioner awareness of preferred place of death and correlates of dying in a preferred place: a nationwide mortality follow-back study in the Netherlands. J Pain Symptom Manage. 2009;38(4):568–577. doi: 10.1016/j.jpainsymman.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Gomes B, Higginson IJ, Calanzani N, et al. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol. 2012;23(8):2006–2015. doi: 10.1093/annonc/mdr602. [DOI] [PubMed] [Google Scholar]
- 9.Mezey M, Dubler NN, Mitty E, Brody AA. What impact do setting and transitions have on the quality of life at the end of life and the quality of the dying process? Gerontologist. 2002;42(Suppl 3):54–67. doi: 10.1093/geront/42.suppl_3.54. [DOI] [PubMed] [Google Scholar]
- 10.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 11.Raijmakers N, Galushko M, Domeisen F, et al. Quality indicators for care of cancer patients in their last days of life: literature update and experts’ evaluation. J Palliat Med. 2012;15(3):308–316. doi: 10.1089/jpm.2011.0393. [DOI] [PubMed] [Google Scholar]
- 12.De Roo ML, Leemans K, Claessen SJ, et al. Quality indicators for palliative care: update of a systematic review. J Pain Symptom Manage. 2013;46(4):556–572. doi: 10.1016/j.jpainsymman.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Pasman HR, Brandt HE, Deliens L, Francke AL. Quality indicators for palliative care: a systematic review. J Pain Symptom Manage. 2009;38(1):145–156. doi: 10.1016/j.jpainsymman.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 14.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 15.De Korte-Verhoef R. Reasons and avoidability of hospitalisations at the end of life. Perspectives of GPs, nurses and family carers. PhD thesis, Vrije Universiteit, 2014. [Google Scholar]
- 16.Higginson IJ, Evans CJ. What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J. 2010;16(5):423–435. doi: 10.1097/PPO.0b013e3181f684e5. [DOI] [PubMed] [Google Scholar]
- 17.Zimmermann C, Riechelmann R, Krzyzanowska M, et al. Effectiveness of specialized palliative care: a systematic review. JAMA. 2008;299(14):1698–1709. doi: 10.1001/jama.299.14.1698. [DOI] [PubMed] [Google Scholar]
- 18.Van den Block L, Onwuteaka-Philipsen B, Meeussen K, et al. Nationwide continuous monitoring of end-of-life care via representative networks of general practitioners in Europe. BMC Fam Pract. 2013;14(1):73. doi: 10.1186/1471-2296-14-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donker GA. Continue Morbiditeits Registratie Peilstations Nederland 2012. Utrecht: NIVEL; 2013. [Google Scholar]
- 20.Konetzka RT, Spector W, Limcangco MR. Reducing hospitalizations from long-term care settings. Med Care Res Rev. 2008;65(1):40–66. doi: 10.1177/1077558707307569. [DOI] [PubMed] [Google Scholar]
- 21.Rosano A, Loha CA, Falvo R, et al. The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health. 2013;23(3):356–360. doi: 10.1093/eurpub/cks053. [DOI] [PubMed] [Google Scholar]
- 22.Onwuteaka-Philipsen BD, De Korte-Verhoef MC, Schweitzer BP, et al. Generalist primary and palliative care is associated with few hospitalisations in the last month of life. Eur J Palliat Care; 14th World Congress of the European Association for Palliative Care: Building Bridges; 8–10 May 2015; Copenhagen. 2015. [Abstract]. [Google Scholar]
- 23.Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs: [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp 760–761] J Am Geriatr Soc. 2010;58(4):627–635. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- 24.Kaspers PJ, Pasman HR, Onwuteaka-Philipsen BD, Deeg DJ. Changes over a decade in end-of-life care and transfers during the last 3 months of life: a repeated survey among proxies of deceased older people. Palliat Med. 2013;27(6):544–552. doi: 10.1177/0269216312457212. [DOI] [PubMed] [Google Scholar]
- 25.van der Plas AG, Hagens M, Pasman HR, et al. PaTz groups for primary palliative care: reinventing cooperation between general practitioners and district nurses in palliative care: an evaluation study combining data from focus groups and a questionnaire. BMC Fam Pract. 2014;15(1):14. doi: 10.1186/1471-2296-15-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaw KL, Clifford C, Thomas K, Meehan H. Review: improving end-of-life care: a critical review of the gold standards framework in primary care. Palliat Med. 2010;24(3):317–329. doi: 10.1177/0269216310362005. [DOI] [PubMed] [Google Scholar]
- 27.Mahmood-Yousuf K, Munday D, King N, Dale J. Interprofessional relationships and communication in primary palliative care: impact of the Gold Standards Framework. Br J Gen Pract. 2008 doi: 10.3399/bjgp08X279760. [DOI] [PMC free article] [PubMed] [Google Scholar]