Abstract
There has been an increasing focus on determining the psychological mechanisms underlying the broad effects of mindfulness on psychological health. Mindfulness has been posited to be related to the construct of reperceiving or decentering, defined as a shift in perspective associated with decreased attachment to one’s thoughts and emotions. Decentering is proposed to be a meta-mechanism that mobilizes four psychological mechanisms (cognitive flexibility, values clarification, self-regulation, and exposure), which in turn are associated with positive health outcomes. Despite preliminary support for this model, extant studies testing this model have not examined distinct facets of mindfulness. The present study used a multidimensional measure of mindfulness to examine whether this model could account for the associations between ive facets of mindfulness and psychological symptoms (depressive symptoms, stress, anxiety symptoms, alcohol-related problems) in a sample of college students (N = 944). Our findings partially support this model. We found significant double-mediated associations in the expected directions for all outcomes (stress, anxiety symptoms, and depressive symptoms) except alcohol-related problems, and for each of the facets of mindfulness except observing. However, decentering and the specific mechanisms did not fully mediate the associations among mindfulness facets and psychological health outcomes. Experimental and ecological momentary assessment designs are needed to understand the psychological processes that account for the beneficial effects of mindfulness.
Keywords: mindfulness, decentering, depression, anxiety, stress, alcohol-related problems
Introduction
At the heart of Buddhist practices and traditions, mindfulness is often described as of the awareness that comes from paying attention to present moment experience in a purposeful and non-judgmental manner (Bishop et al., 2004; Kabat-Zinn, 1994). Mindfulness-based interventions with the explicit goal of cultivating mindfulness through mindfulness meditation practices have been developed to target chronic pain (Mindfulness Based Stress Reduction, MBSR; Kabat-Zinn, 1990), depressive symptoms (Mindfulness Based Cognitive Therapy, MBCT; Segal, Williams, and Teasdale,2002) and substance misuse (Mindfulness Based Relapse Prevention, MBRP; Witkiewitz, Marlatt, & Walker, 2005). As each of these interventions have been shown to be effective (Chiesa & Serretti, 2013; Grossman, Niemann, Schmidt, & Walach, 2004; Hofmann, Sawyer, Witt, & Oh, 2010), there is an increasing focus on determining the psychological mechanisms through which mindfulness has such broad effects on psychological health. Alongside the development of mindfulness-based interventions, researchers have also studied mindfulness as a dispositional trait (Brown & Ryan, 2003). Importantly, research indicates that meditation experience is positively related to trait mindfulness (Baer et al., 2008) and that trait mindfulness can be increased through mindfulness meditation training (Bowen et al., 2009; Carmody & Baer, 2008). Furthermore, trait mindfulness has been shown to be related to decreased depressive symptoms, anxiety symptoms, stress, and alcohol-related outcomes (Bowlin & Baer, 2012; Cash & Whittingham, 2010; Lyvers, Makin, Toms, Thorberg, & Samios, 2013; Ostafin, Brooks, & Laitem, 2013; Pearson, Brown, Bravo, & Witkiewitz, 2014; Weinstein, Brown, & Ryan, 2009).
One prominent psychological model of the mechanisms of mindfulness on health-related outcomes was proposed by Shapiro and colleagues (2006, 2009; see Figure 1). According to this model, mindfulness is primarily related to the construct of reperceiving, which is proposed to be a meta-mechanism, or a mechanism that mobilizes other mechanisms associated with the health-promoting effects of mindfulness. Shapiro et al. define reperceiving as a shift in perspective associated with decreased attachment to one’s thoughts and emotions, which has been alternatively described as decentering (Fresco et al., 2007), and resembles the construct of cognitive defusion (Hayes, Strosahl, & Wilson, 1999). Shapiro et al. specifically posit that reperceiving leads to changes in at least four additional psychological mechanisms that are putatively more proximal antecedents to improved psychological functioning: values clarification, exposure, self-regulation, and cognitive/behavioral flexibility. Values clarification involves identifying one’s important personal values, which are expected to increase values-consistent behavior. Exposure refers to the ability to allow oneself to endure and “stay with” negative emotional states, and is closely related to the construct of distress tolerance (Simons & Gaher, 2005). Self-regulation refers to the ability to monitor and adapt one’s behavior to changing circumstances in order to achieve relevant goals. Cognitive/behavioral flexibility is described as the ability to process important available information in one’s environment in order to produce appropriate and adaptive behavioral responses.
Figure 1.
Depicts Shapiro et al.’s (2006) theoretical model of mindfulness mechanisms.
To date, there are several studies testing components of Shapiro et al.’s (2006) model. For example, in a sample of novice meditators, researchers have found decentering to increase directly following brief mindful breathing compared to two other stress-reduction techniques (muscle relaxation and loving-kindness meditation; Feldman, Greeson, & Senville, 2010), providing experimental evidence that mindfulness practice specifically (and not stress-reduction more generally) leads to increased decentering. Using a sample of community adults, Carmody, Baer, Lykins, and Olendzki (2009) aimed to test Shapiro et al.’s model by observing changes following an 8-week MBSR course. They found that changes in mindfulness (assessed as a total score of the Five Facet Mindfulness Questionnaire, FFMQ; Baer et al., 2006) and decentering (assessed with the Experiences Questionnaire; Fresco et al., 2007) were strongly collinear so they created a mindfulness/decentering composite change score from pre- to post-MBSR course. This change score inversely predicted a wide range of psychological symptoms. Importantly, purpose in life (values clarification) and environmental mastery (cognitive/behavioral flexibility) were found to significantly mediate the associations between change in mindfulness/decentering and psychological distress (depression, anxiety, and stress), whereas self-regulation and experiential avoidance (exposure) did not.
In a sample of college students, Pearson et al. (2014) tested one aspect of Shapiro et al.’s model by examining decentering and purpose in life as mediators of the associations between trait mindfulness and psychological health outcomes (i.e., depressive symptoms, anxiety symptoms, and alcohol-related problems) in a double-mediated path model (e.g., mindfulness→ decentering→purpose in life→depressive symptoms). They found that decentering alone (in the case of anxiety symptoms) or both decentering and purpose in life (in the case of depressive symptoms and alcohol-related problems) were found to partially mediate the relationship between trait mindfulness and these psychological health outcomes.
Despite preliminary support for Shapiro et al.’s (2006) model of the psychological mechanisms involved with the health-promoting effects of mindfulness, extant studies that have tested Shapiro et al.’s model have not examined distinct facets of mindfulness. Rather than examining mindfulness as a unidimensional construct as in the case of Carmody et al. (2009) and Pearson et al. (2014), the present study used the FFMQ, which assess five distinct aspects of mindfulness: acting with awareness (focusing attention on one’s current activity), non-judging of inner experience (experiencing thoughts/feelings without judging them or criticizing oneself), non-reactivity to inner experience (allowing thoughts/feelings to come and go without reacting to them or getting caught up in them), describing (labeling experiences with words), and observing (noticing internal/external experiences). The purpose of the present study was to examine whether Shapiro et al.’s model could adequately account for the associations between these five facets of mindfulness and psychological health in a sample of college students. Based on previous research (Carmody et al., 2009; Fresco et al., 2007; Pearson et al., 2014) and face validity of the measures, we selected measures to operationalize each of the psychological mechanisms proposed by Shapiro et al. (decentering, values clarification, self-regulation, exposure, and cognitive/behavioral flexibility), and tested these as potential mediators of the effects of facets of mindfulness on psychological symptoms that are particularly prevalent among college students (depressive symptoms, stress, anxiety symptoms, and alcohol-related problems).
Method
Participants
Participants were recruited from Psychology Department participant pools at a large, U.S. southwestern university (n = 663) to “complete a survey using a computer regarding their behavior” and a large, U.S. southeastern university (n = 281) to “complete a survey regarding their personal beliefs and behaviors,” resulting in a total combined sample of 944 college students (605 women, 330 men, 9 unreported). Participants could select multiple racial/ethnic groups that best describe them; participants self-reported their race/ethnicity as White/Caucasian (n = 395; 41.8%), Hispanic/Latino (n = 392; 41.5%), Black/African American (n = 125; 13.2%), American Indian/Alaska Native (n = 63; 6.7%), Asian (n = 58; 6.1%), Native Hawaiian/Pacific Islander (n = 13; 1.4%), and Other (n = 125; 13.2%).
Procedure
Participants signed up to complete the study online from a list of studies available at each of the respective institutions. First, participants read a notification statement or informed consent document that explained the risks and benefits of participating and emphasized their rights to skip any answer or withdrawal from the study at any time. They provided consent to participate by clicking “Next” in the survey. The assessment battery took approximately one hour to complete and participants received course credit for their participation. The studies were approved by the institutional review boards at the respective institutions.
Measures
Mindfulness
Mindfulness was assessed using the 39-item Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006) measured on a 5-point response scale (1 = Never or very rarely true, 5 = Very often or always true). The five facets include acting with awareness (e.g., “It seems I am ‘running on automatic’ without much awareness of what I’m doing,” reverse-coded), non-judging of inner experience, (e.g., “I criticize myself for having irrational or inappropriate emotions,” reverse-coded), non-reactivity to inner experience (e.g., “I perceive my feeling and emotions without having to react to them”), describing (e.g., “I am good at finding the words to describe my feeling”), and observing (e.g., “When I am walking, I deliberately notice the sensations of my body moving”).
Decentering
Decentering was assessed using the 11-item Experiences Questionnaire (EQ; Fresco et al., 2007) measured on a 5-point response scale (1 = Never, 5 = All the time). Example items include, “I can separate myself from my thoughts and my feelings” and “I am consciously aware of a sense of my body as a whole.”
Values Clarification
A component of values clarification (i.e., purpose in life) was assessed using the 7-item Purpose in Life subscale from the Scales of Psychological Well Being questionnaire (SPWB; Ryff, 1989) measured on a 6-point response scale (1 = Strongly Disagree, 6 = Strongly Agree). Example items include “I live life one day at time and don’t really think about the future” and “I have a sense of direction and purpose in life.”
Cognitive/behavioral flexibility
Cognitive/behavioral flexibility was assessed using the 7-item Environmental Mastery subscale of the Scales of Psychological Well Being questionnaire (SPWB, Ryff, 1989) measured on a 6-point response scale (1 = Strongly Disagree, 6 = Strongly Agree). Example items include, “I am quite good at managing the many responsibilities of my daily life” and “I often feel overwhelmed by my responsibilities” (reverse-coded).
Self-regulation
Self-regulation was assessed using the 31-item Short Self-Regulation Questionnaire (SSRQ; Carey et al., 2004) measured on a 5-point response scale (1 = Strongly Disagree, 5 = Strongly Agree). Example items include, “I set goals for myself and keep track of my progress” and “I usually think before I act.”
Exposure
Exposure was assessed through the conceptually similar construct of distress intolerance using the 15-item Distress Tolerance Scale (DTS, Simons & Gaher, 2005) measured on a 5-point response scale (1 = Strongly Disagree, 5 = Strongly Agree). Example items include, “Feeling distressed or upset is unbearable to me” and “I can’t handle feeling distressed or upset.”
Depressive symptoms
Depressive symptoms were assessed using the 20-item Center for Epidemiological Studies Depression-Revised (CESD-R; Eaton, Muntaner, Smith, Tien, & Ybarra,2004) measured on a 5-point response scale (1 = Not at all or Less than 1 day, 1 = 1–2 Days, 2 = 3–4 Days, 3 = 5–7 Days, 4 = Nearly Every day for 2 weeks). Example items include, “I felt depressed” and “I lost interest in my usual activities.”
Stress
Stress was assessed using the 14-item Perceived Stress Scale (PSS; Cohen, Kamarck, & Merlmelstein, 1983) measured on a 5-point response scale (1 = Never, 5 = Very Often). Example items include, “In the last month, how often have you found that you could not cope with all the things you had to do?” and “ In the last month, how often have you felt difficulties were piling up so high that you could not overcome them?”
Anxiety symptoms
Anxiety symptoms (i.e., worry) was assessed using the 16-item Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec,1990) measured on a 5-point response scale (1 = not at all typical of me, 5 = very typical of me). Although five items on the PSWQ are reversed-coded, our exploratory factor analysis revealed that these items did not load strongly (<.40) on a single factor; rather, they loaded together on a second factor. Given our aim of examining a single factor of anxiety symptoms, these items were dropped, and the remaining 11 items were used. Example items include, “My worries overwhelm me” and “Once I start worrying, I cannot stop”.
Alcohol-related problems
Alcohol-related problems were assessed using the 24-item Brief-Young Adult Alcohol Consequences Questionnaire (B-YAACQ; Kahler, Strong, & Read, 2005). Individuals responded on a checklist response format indicating whether they experienced a specific consequence in the past month. Non-drinkers were given a score of ‘0’ to reflect the absence of alcohol-related problems. Example items include, “I have had a hangover (headache, sick stomach) the morning after I had been drinking” and “I have passed out from drinking.”
Statistical Analysis
To test the theoretical model proposed by Shapiro and colleagues (2006; Figure 1), structural equation modeling using Mplus 7 (Muthén & Muthén, 1998–2012) was conducted. We proposed a structural model in which five distinct aspects of mindfulness (acting with awareness, non-judging of inner experience, non-reactivity to inner experience, describing, and observing) were examined as statistical predictors of decentering, four psychological mechanisms (self-regulation, purpose in life, distress intolerance, cognitive flexibility), and psychological health outcomes (depressive symptoms, stress, anxiety symptoms, and alcohol-related problems). Decentering was modeled as a predictor of the four psychological mechanisms and psychological health outcomes. Furthermore, the four psychological mechanisms were modeled as the most proximal predictors of the psychological health outcomes. Gender, race, ethnicity, age, and school were included as covariate predictors of all variables in the model. To evaluate overall model fit, we used model fit criteria suggested by Hu and Bentler (1999) including the Comparative Fit Index (CFI) > .95, Tucker-Lewis Index (TLI) > .95, Root Mean Square Error of Approximation (RMSEA) < .06, and Standardized Root Mean Square Residual (SRMR) < .08.
To reduce the complexity of the model and improve model fit, we followed the item-to-construct balance approach described by Little, Cunningham, Shahar, and Widaman (2002) to create parcels for multi-item inventories. We extracted a single factor in exploratory factor analyses (EFAs) for each latent construct, sorted the items from highest to lowest factor loadings, and created three to four balanced parcels by pairing items with the highest factor loadings with items with the lowest factor loadings. We also used these EFAs to ensure that each subscale was unidimensional, which is requisite for using parceling. Supplementary Table 1 shows the correlations among the parcels used as indicators of the latent factors in the model.
We examined the total, direct, and indirect effects of each predictor variable on outcomes using bias-corrected bootstrapped estimates (Efron & Tibshirani, 1993) based on 10,000 bootstrapped samples, which provides a powerful test of mediation (Fritz & MacKinnon, 2007) and is robust to small departures from normality (Erceg-Hurn & Mirosevich, 2008). Parameters were estimated using maximum likelihood estimation, and missing data were handled using full information maximum likelihood, which is more efficient and has less bias than alternative procedures (Enders, 2001; Enders & Bandalos, 2001). Statistical significance was determined by 95% bias-corrected bootstrapped confidence intervals that do not contain zero.
Results
After item parceling, our SEM model provided decent fit to the data, CFI = .941, TLI = .931, RMSEA = .044 (90% CI [.042, .046], SRMR = .048, χ2(1041) = 2882.18, p < .001. Although CFI and TLI did not exceed .95, RMSEA and SRMR were well under values indicative of good model fit. Table 1 summarizes the correlations among all latent variables in the model. Table 2 summarizes the total, total indirect, specific indirect, and direct effects of the five facets of mindfulness and decentering on psychological mechanisms and psychological health outcomes.
Table 1.
Correlations among latent variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Acting with Awareness | ---- | ||||||||||
| 2. Non-judging | .544 | ---- | |||||||||
| 3. Non-reactivity | .000 | −.031 | ---- | ||||||||
| 4. Describing | .358 | .199 | .375 | ---- | |||||||
| 5. Observing | −.180 | −.377 | .486 | .261 | ---- | ||||||
| 6. Decentering | .365 | .381 | .532 | .462 | .182 | ---- | |||||
| 7. Mechanisms Latent Variable | .597 | .414 | .308 | .459 | .126 | .562 | ---- | ||||
| 8. Distress Intolerance | −.476 | −.557 | −.212 | −.260 | .118 | −.446 | −.534 | ---- | |||
| 9. Depressive Symptoms | −.508 | −.523 | −.149 | −.268 | .116 | −.438 | −.566 | .558 | ---- | ||
| 10. Stress | −.579 | −.561 | −.198 | −.256 | .212 | .212 | −.569 | .658 | .695 | ---- | |
| 11. Anxiety Symptoms | −.423 | −.496 | −.223 | −.233 | .094 | −.435 | −.368 | .596 | .512 | .687 | ---- |
| 12. Alcohol-Related Problems | −.193 | −.142 | −.038 | −.030 | .077 | −.483 | −.569 | .658 | .223 | .227 | .107 |
Note. Significant effects (p < .05) are bolded for emphasis.
Table 2.
Summary of total, indirect, and direct effects of mindfulness facets and decentering on depression, stress, anxiety, and alcohol-related problems
| Outcome Variables: | Depressive Symptoms | Stress | Anxiety Symptoms | Alcohol-Related Problems | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Predictor Variable: Acting with Awareness | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI |
| Total | −.299 | −.349 | −.379,−.219 | −.374 | −.398 | −.467,−.281 | −.211 | −.356 | −.291,−.131 | −.192 | −.055 | −.287,−.098 |
| Total indirecta | −.194 | −.227 | −.252,−.136 | −.183 | −.195 | −.251,−.116 | −.071 | −.119 | −.128,−.014 | −.038 | −.011 | −.096,.020 |
| Decentering | −.013 | −.016 | −.031,.004 | −.010 | −.011 | −.030,.009 | −.018 | −.031 | −.035,−.002 | −.005 | −.001 | −.022,.011 |
| Mechanisms Latent Variable | −.120 | −.140 | −.017,−.078 | −.097 | −.103 | −.155,−.039 | .027 | .046 | −.018,.073 | −.007 | −.002 | .063,.048 |
| Distress Intolerance | −.044 | −.052 | −.068,−.021 | −.060 | −.064 | −.094,−.026 | −.074 | −.124 | −.107,−.040 | −.022 | −.006 | −.044,.000 |
| Decentering-Mechanisms Latent Variable | −.011 | −.013 | −.019,−.003 | −.009 | −.009 | −.017,−.001 | .003 | .004 | −.002,.007 | −.001 | .000 | −.006,.005 |
| Decentering-Distress Intolerance | −.005 | −.006 | −.010,−.001 | −.007 | −.007 | −.013,−.001 | −.009 | −.014 | −.016,−.001 | −.003 | −.001 | −.006,.001 |
| Direct | −.105 | −.122 | −.190,−.020 | −.191 | −.203 | −.301,−.081 | −.140 | −.237 | −.231,−.049 | −.154 | −.044 | −.271,−.037 |
| Outcome Variables: | Depressive Symptoms | Stress | Anxiety Symptoms | Alcohol-Related Problems | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Predictor Variable: Non-judging | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI |
| Total | −.354 | −.358 | −.433,−.275 | −.307 | −.283 | −.409,−.206 | −.381 | −.559 | −.472,−.291 | −.036 | −.009 | −.137,.065 |
| Total indirecta | −.178 | −.178 | −.231,−.120 | −.191 | −.177 | −.252,−.131 | −.181 | −.266 | −.236,−.127 | −.061 | −.015 | −.111,−.011 |
| Decentering | −.028 | −.028 | −.062,.006 | −.022 | −.020 | −.058,.014 | −.038 | −.056 | −.067,−.009 | −.011 | −.003 | −.044,.022 |
| Mechanisms Latent Variable | −.031 | −.031 | −.058,−.003 | −.025 | −.023 | −.051,.001 | .007 | .010 | −.007,.021 | −.002 | .000 | −.017,.013 |
| Distress Intolerance | −.083 | −.084 | −.121,−.045 | −.112 | −.103 | −.159,−.064 | −.138 | −.202 | −.186,.089 | −.041 | −.010 | −.080,−.003 |
| Decentering-Mechanisms Latent Variable | −.023 | −.023 | −.019,−.003 | −.019 | −.017 | −.033,−.005 | .005 | .008 | −.004,.014 | −.001 | .000 | −.012,.010 |
| Decentering-Distress Intolerance | −.011 | −.011 | −.036,−.012 | −.014 | −.013 | −.026,−.003 | −.018 | −.026 | −.030,−.005 | −.005 | −.001 | −.012,.001 |
| Direct | −.179 | −.181 | −.266,−.092 | −.116 | −.107 | −.222,−.009 | −.200 | −.293 | −.301,−.099 | .025 | .006 | −.088,.138 |
| Outcome Variables: | Depressive Symptoms | Stress | Anxiety Symptoms | Alcohol-Related Problems | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Predictor Variable: Non-reactivity | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI |
| Total | −.141 | −.206 | −.230,−.052 | −.239 | −.318 | −.333,−.145 | −.217 | −.459 | −.303,−.131 | −.090 | −.032 | −.203,.023 |
| Total indirecta | −.147 | −.215 | −.204,−.091 | −.145 | −.193 | −.207,−.083 | −.124 | −.262 | −.178,−.070 | −.044 | −.016 | −.094,.006 |
| Decentering | −.040 | −.058 | −.089,.009 | −.031 | −.041 | −.084,.022 | −.054 | −.114 | −.096,−.013 | −.015 | −.005 | −.063,.032 |
| Mechanisms Latent Variable | −.025 | −.036 | −.057,.007 | −.020 | −.027 | −.046,.006 | .006 | .012 | −.007,.019 | −.002 | −.001 | −.015,.012 |
| Distress Intolerance | −.035 | −.051 | −.061,−.009 | −.047 | −.062 | −.081,−.013 | −.058 | −.122 | −.097,−.018 | −.017 | −.006 | −.036,.002 |
| Decentering-Mechanisms Latent Variable | −.033 | −.048 | −.052,−.013 | −.026 | −.035 | −.047,−.006 | .007 | .016 | −.006,.020 | −.002 | −.001 | −.018,.014 |
| Decentering-Distress Intolerance | −.015 | −.022 | −.026,−.004 | −.021 | −.027 | −.036,−.005 | −.025 | −.054 | −.043,−.008 | −.008 | −.003 | −.017,.001 |
| Direct | .006 | .009 | −.089,.102 | −.094 | −.125 | −.205,.018 | −.093 | −.196 | −.184,−.002 | −.046 | −.016 | −.173,.081 |
| Outcome Variables: | Depressive Symptoms | Stress | Anxiety Symptoms | Alcohol-Related Problems | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Predictor Variable: Describing | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI |
| Total | −.042 | −.049 | −.120,.037 | −.008 | −.009 | −.100,.084 | .010 | .017 | −.069,.088 | .050 | .014 | −.038,.138 |
| Total indirecta | −.068 | −.080 | −.110,−.026 | −.057 | −.060 | −.098,−.015 | −.020 | −.033 | −.057,.017 | −.012 | −.003 | −.040,.017 |
| Decentering | −.018 | −.021 | −.040,.005 | −.014 | −.015 | −.037,.009 | −.024 | −.041 | −.044,−.004 | −.007 | −.002 | −.028,.015 |
| Mechanisms Latent Variable | −.032 | −.038 | −.058,−.007 | −.026 | −.028 | −.050,−.002 | .007 | .012 | −.007,.021 | −.002 | −.001 | −.018,.009 |
| Distress Intolerance | .003 | .004 | −.014,.020 | .004 | .004 | −.019,.027 | .005 | .009 | −.023,.033 | .002 | .000 | −.008,.009 |
| Decentering-Mechanisms Latent Variable | −.014 | −.017 | −.024,−.004 | −.012 | −.012 | −.022,−.002 | .003 | .006 | −.004,.009 | −.001 | .000 | −.008,.001 |
| Decentering-Distress Intolerance | −.007 | −.008 | −.012,−.001 | −.009 | −.010 | −.017,−.002 | −.011 | −.019 | −.020,−.003 | −.003 | −.001 | −.008,.006 |
| Direct | .026 | .031 | −.046,.099 | .048 | .052 | −.036,.133 | .029 | .050 | −.047,.106 | .061 | .018 | −.026,.149 |
| Outcome Variables: | Depressive Symptoms | Stress | Anxiety Symptoms | Alcohol-Related Problems | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Predictor Variable: Observing | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI |
| Total | .007 | .009 | −.081,.095 | .136 | .164 | .032,.241 | .002 | .004 | −.094,.098 | .048 | .015 | −.073,.169 |
| Total indirecta | −.029 | −.039 | −.072,−.013 | −.019 | −.022 | −.063,.026 | .015 | .028 | −.025,.054 | .000 | .000 | −.022,.023 |
| Decentering | −.006 | −.008 | −.018,.006 | −.005 | −.006 | −.016,.007 | −.008 | −.016 | −.022,.005 | −.002 | −.001 | −.012,.007 |
| Mechanisms Latent Variable | −.028 | −.037 | −.055,−.001 | −.022 | −.027 | −.048,.003 | .006 | .012 | −.007,.019 | −.002 | −.001 | −.016,.013 |
| Distress Intolerance | .012 | .015 | −.010,.033 | .016 | .019 | −.012,.044 | .019 | .037 | −.015,.053 | .006 | .002 | −.006,.018 |
| Decentering-Mechanisms Latent Variable | −.005 | −.007 | −.013,.003 | −.004 | −.005 | −.011,.003 | .001 | .002 | −.002,.004 | .000 | .000 | −.003,.003 |
| Decentering-Distress Intolerance | −.002 | −.003 | −.006,.002 | −.003 | −.004 | −.008,.002 | −.004 | −.007 | −.010,.002 | −.001 | .000 | −.003,.001 |
| Direct | .036 | .048 | −.044,.117 | .155 | .186 | .058,−.253 | −.013 | −.024 | −.104,.079 | .048 | .015 | −.072,.168 |
| Outcome Variables: | Depressive Symptoms | Stress | Anxiety Symptoms | Alcohol-Related Problems | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Predictor Variable: Decentering | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | B | 95% CI |
| Total | −.205 | −.237 | −.322,−.088 | −.182 | −.192 | −.298,−.067 | −.169 | −.282 | −.264,−.073 | −.059 | −.016 | −.163,−.046 |
| Total indirecta | −.112 | −.129 | −.160,−.065 | −.110 | −.116 | −.166,−.054 | −.042 | −.070 | −.089,.005 | −.022 | −.006 | −.061,.016 |
| Mechanisms Latent Variable | −.076 | −.088 | −.116,−.036 | −.062 | −.065 | −.106,−.017 | .017 | .029 | −.012,.047 | −.005 | −.001 | −.041,.031 |
| Distress Intolerance | −.036 | −.041 | −.060,−.011 | −.048 | −.051 | −.082,−.014 | −.059 | −.099 | −.097,−.021 | −.018 | −.005 | −.038,.003 |
| Direct | −.093 | −.107 | −.203,.017 | −.072 | −.076 | −.192,.047 | −.127 | −.212 | −.218,−.036 | −.036 | −.010 | −.146,.074 |
Note. Significant effects are in bold typeface for emphasis and were determined by a 95% bias-corrected bootstrapped confidence interval (based on 10,000 bootstrapped samples) that does not contain zero. All results come from a single structural equation model.
Reflects the combined indirect effects via decentering, mechanisms latent variable, distress tolerance, decentering via mechanisms latent variable, and decentering via distress tolerance.).
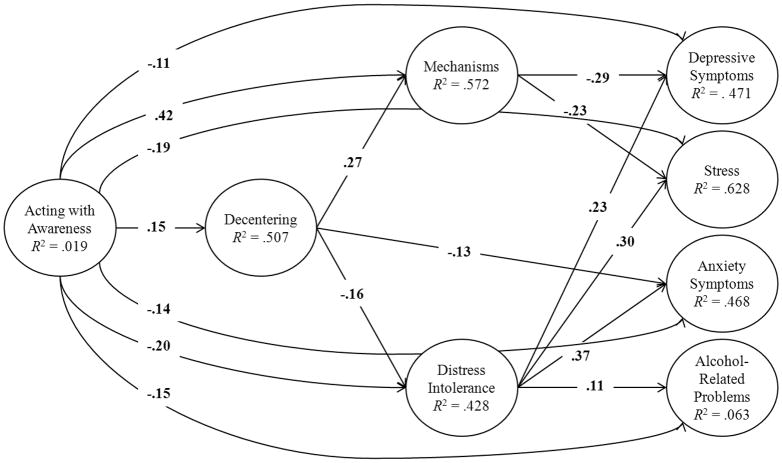
Three of the psychological mechanism variables (environmental mastery, purpose in life and self-regulation) were all highly correlated with each other (rs > .700); thus, we created a second-order “mechanisms” latent variable to reduce issues of multicollinearity. Initial testing of the complete model revealed multiple suppression effects (i.e., the total effects of specific mechanisms variables on outcomes were opposite in direction to the direct effects of those variables on psychological health outcomes). Thus, the results are described with a higher-order mechanisms latent variable and distress intolerance as the two most proximal predictors of outcomes. Although a single SEM model was conducted with all five facets of mindfulness predicting outcomes (see Supplementary Figure 1) to investigate the unique direct and indirect associations of mindfulness facets on proposed mediators and outcomes, for reasons of parsimony, we present separate tables for the acting with awareness (Figure 2) and non-judging facets of mindfulness (Figure 3). For the remaining facets, results are described in the text.
Figure 2.
Depicts the unique direct associations of acting with awareness on decentering, mechanisms (self-regulation, cognitive/behavioral flexibility, and purpose in life), and health-related outcomes controlling for the other mindfulness facets and demographic covariates. Although not shown for reasons of parsimony, the mechanisms latent variable was allowed to correlate with distress intolerance, acting with awareness was allowed to correlate with the other four facets of mindfulness, and demographic covariates (gender, race, ethnicity, age, and school) were included as covariate predictors of all variables in the model and allowed to correlate with each other.
Figure 3.
Depicts the unique direct associations of non-judging of experience on decentering, mechanisms (self-regulation, cognitive/behavioral flexibility, and purpose in life), and health-related outcomes controlling for the other mindfulness facets and demographic covariates. Although not shown for reasons of parsimony, the mechanisms latent variable was allowed to correlate with distress intolerance, non-judging was allowed to correlate with the other four facets of mindfulness, and demographic covariates (gender, race, ethnicity, age, and school) were included as covariate predictors of all variables in the model and allowed to correlate with each other.
Direct effects
Acting with awareness
As shown in Figure 2, the acting with awareness facet of mindfulness was modestly associated with higher decentering (β = .15), modestly associated with lower levels of distress intolerance (β = −.20), and moderately associated with higher levels of the latent mechanisms variable (β = .42). Acting with awareness had significant direct associations with all psychological health outcomes, that is, lower levels of depressive symptoms (β = −.11), stress (β = −.19), anxiety symptoms (β = −.14), and alcohol-related problems (β = −.15).
Non-judging
As shown in Figure 3, the non-judging facet of mindfulness was moderately associated with higher decentering (β = .30), moderately associated with lower levels of distress intolerance (β = −.37), and modestly associated with higher levels of mechanisms (β = .11). Non-judging had a modest direct association with lower levels of depressive symptoms (β = −.18), stress (β = −.12), and anxiety symptoms (β = −.20), but a non-significant direct association with alcohol-related problems (β = .03).
Non-reactivity
The non-reactivity facet of mindfulness was moderately associated with higher decentering (β = .43), modestly associated with lower levels of distress intolerance (β = −.16), and was not significantly related to mechanisms (β = .09). Non-reactivity had a modest direct association with lower levels of anxiety symptoms (β = −.09), but non-significant direct associations with depressive symptoms (β = .01), stress (β = −.09), and alcohol-related problems (β = −.05).
Describing
The describing facet of mindfulness was modestly associated with higher decentering (β = .19), modestly associated with higher levels of mechanisms (β = .11), and was not significantly related to distress intolerance (β = .01). Describing did not have any significant direct associations with any of the psychological health outcomes [depressive symptoms (β = .03), stress (β = .05), anxiety symptoms (β = .03), alcohol-related problems (β = .06)].
Observe
The observing facet of mindfulness was not significantly associated with decentering (β = .07) or distress intolerance (β = .05), but was modestly associated with higher levels of mechanisms (β = .10). Observing had a modest direct association with higher levels of stress (β = .15), but non-significant direct associations with depressive symptoms (β = .04), anxiety symptoms (β = −.01), and alcohol-related problems (β = .05).
Decentering
As shown in both of the preceding figures, decentering was modestly associated with higher levels of mechanisms (β = .27) and lower levels of distress intolerance (β = −.16). With regards to psychological health outcomes, decentering had a modest direct association with lower levels of anxiety symptoms (β = −.13), but non-significant direct associations with depressive symptoms (β = −.09), stress (β = −.07), and alcohol-related problems (β = −.04).
Specific mechanisms
The higher-order mechanisms latent variable was modestly associated with lower levels of depressive symptoms (β = −.29) and stress (β = −.23), but not significantly associated with anxiety symptoms (β = .07) and alcohol-related problems (β = −.02). Distress intolerance had direct associations with higher levels of stress (β = .30), anxiety symptoms (β = .37), depressive symptoms (β = .23), and alcohol-related problems (β = .11).
Indirect effects
Decentering as a meta-mechanism
With regards to the associations between mindfulness facets and the higher-order mechanisms latent variable, decentering at least partially mediated the effects of three of the five facets of mindfulness: acting with awareness, describing, and non-judging. With regards to the associations between mindfulness facets and distress intolerance, decentering at least partially mediated the effects of four of the five facets of mindfulness: non-reactivity, acting with awareness, describing, and non-judging. Decentering also directly mediated the associations between these four mindfulness facets and anxiety symptoms.
Specific mechanisms
The higher-order mechanisms latent variable significantly mediated the associations between decentering and two psychological health outcomes: depressive symptoms and stress. Distress intolerance significantly mediated the associations between decentering and three psychological health outcomes: depressive symptoms, anxiety symptoms, and stress. Mechanisms significantly mediated the associations between four mindfulness facets (observing, acting with awareness, describing, and non-judging) and depressive symptoms as well two facets (acting with awareness, describing) and stress. Distress intolerance significantly mediated the associations between three mindfulness facets (non-reactive, acting with awareness, non-judging) and depressive symptoms, three mindfulness facets (non-reactive, acting with awareness, non-judging) and stress, and three facets of mindfulness (non-reactivity, acting with awareness, and non-judging) and anxiety symptoms.
Double-mediated paths
Shapiro et al.’s (2006) model specifically predicts double-mediated associations such that mindfulness is associated with increased decentering, which is associated with increased specific mechanisms, which in turn is associated with decreased psychological symptoms (e.g., mindfulness facets → decentering → mechanisms → depressive symptoms). The double-mediated paths through decentering and the higher-order mechanisms latent variable were significant for the associations of four facets of mindfulness (non-reactivity, acting with awareness, describing, and non-judging) with both depressive symptoms and stress. The double-mediated paths through decentering and distress intolerance were significant for the associations of the same four facets of mindfulness with depressive symptoms, anxiety symptoms, and stress. There were significant double-mediated associations for all outcomes except alcohol-related problems, and for each of the facets of mindfulness except observing.
Discussion
The purpose of the present study was to examine a psychological model of the putative mechanisms through which mindfulness has health-promoting effects. Specifically, based on Shapiro et al. (2006), we examined how five facets of trait mindfulness (Baer et al., 2006) relate to depressive symptoms, stress, anxiety symptoms, and alcohol-related problems via decentering and four conceptually distinct psychological constructs expected to be proximal predictors of psychological health outcomes including values clarification (purpose in life), self-regulation, cognitive/behavioral flexibility, and exposure (distress intolerance).
Consistent with Shapiro et al.’s theoretical model, four of the five mindfulness facets were predictive of having less attachment to one’s experiences (i.e., higher reperceiving or decentering), which in turn was related to other putatively more proximal mechanisms, which were in turn related to psychological health outcomes. Further, we found double-mediated paths consistent with the model for four of the five facets of mindfulness such that mindfulness facets predicted higher decentering, which in turn predicted specific psychological mechanisms, which in turn predicted psychological health outcomes. Finally, the overall model had strong predictive utility as it explained substantial portions of variance in decentering (50.7%), the higher-order mechanisms latent variable (57.2%), distress intolerance (42.8%), depressive symptoms (47.1%), stress (62.8%), and anxiety symptoms (46.8%). However, decentering did not fully mediate many of the associations between mindfulness facets on other psychological mechanisms and psychological health outcomes. Further, none of the mediators fully accounted for the associations between mindfulness facets and psychological health outcomes. Finally, the model only accounted for 6.3% of the variance in alcohol-related problems. Together, these results suggest that there are constructs missing from the model that must more fully explain the associations between mindfulness facets and psychological health outcomes.
Many of our specific findings were consistent with previous studies. For example, consistent with Pearson et al. (2014), we found that acting with awareness was directly related to each of the mechanisms in the expected direction and inversely related to each of the psychological health outcomes even when controlling for four other facets of mindfulness. Consistent with a study examining the five mindfulness facets as they relate to anxiety and depressive symptoms in a treatment-seeking sample (Desrosiers, Klemanski, & Nolen-Hoeksema, 2013), we found both non-judging and non-reactivity to inner experience to have negative associations (direct and/or indirect) with anxiety and depressive symptoms. Interestingly, we found that the observing facet of mindfulness was positively related to stress, and negatively correlated with some of the other mindfulness facets. Previous research has found the observing facet to be negatively (but non-significantly) correlated with non-judging of inner experience in samples without meditation experience (Baer et al., 2006), and positively related to psychological symptoms (e.g., Baer et al., 2006; Leigh, Bowen, & Marlatt, 2005; Leigh & Neighbors, 2009). Specifically, it appears that higher observing may be naturally associated with higher judgment until mindfulness practice (e.g., mindfulness meditation) is used to cultivate a non-judgmental attitude that co-occurs with increased observing.
Limitations
The present study was limited by the cross-sectional survey design, prohibiting the demonstration of temporal precedence, which is requisite for making causal inferences. Relatedly, numerous alternative models could have provided equivalent or better fit to the data. Together, these limitations point to the necessity of examining Shapiro et al.’s (2006) model using experimental designs that can rule out ‘third variable’ explanations for these observed associations and can examine the temporal sequence of changes in the psychological constructs examined in the present study.
There are numerous limitations in our specific test derived from Shapiro et al.’s (2006) model that warrant mention. First, we used a multidimensional operationalization of dispositional mindfulness using the FFMQ (Baer et al., 2006), whereas Shapiro et al. argue that the three axioms of mindfulness (intention, attention, and attitude) cannot be segregated, but must be examined as an integrated whole. Thus, it appears that our operationalization may be at odds with their conceptualization. Second, we selected a single measure meant to capture a primary aspect of each of the psychological constructs proposed in the model. There are numerous alternative operationalizations. For example, we chose a measure of distress intolerance to capture the construct of exposure, whereas Carmody et al. (2009) used a measure of experiential avoidance. Thus, until definitive, validated measures of each of the constructs proposed in Shapiro et al.’s model are developed, additional operationalizations ought to be examined. Consistent with Carmody et al. (2009), we operationalized values clarification with a measure of purpose in life. However, more specific assessments of values and the degree to which one engages in values-consistent behavior would be one alternative way of operationalizing this construct. Third, we selected measures to capture four conceptually distinct psychological mechanisms, but found that three of these specific mechanisms were not sufficiently empirically distinct for SEM model testing. To overcome the problems associated with multicollinearity, we formed a higher-order latent variable defined by the three lower-order latent variables of self-regulation, cognitive/behavioral flexibility, and purpose in life. For lack of a better term, we have labeled this latent variable the ‘mechanisms’ latent variable. However, it is not clear what term best captures a psychological construct defined by these three conceptually distinct constructs. Fourth, although we used Shapiro et al.’s (2006) model as the basis of examining the mediated paths between facets of mindfulness and psychological health outcomes, we did not have hypotheses regarding which specific facets of mindfulness would be mediated by which specific mechanisms. Thus, our results should be considered preliminary and warrant replication. Finally, we are unable to determine the extent to which our findings generalize to other non-college student populations. We selected four psychological health outcomes that show sufficient variation in college student samples. For example, we used the experience of common, negative alcohol-related consequences as an index of problematic alcohol use, and found only weak prediction of this outcome in this sample. Findings may be entirely different when examining, for example, severity of substance dependence in a clinical context. Studies testing psychological models of mindfulness in clinical populations are sorely needed.
Clinical Implications
Despite the limitations of the present study, we believe our findings may have important implications for mindfulness-based interventions. Specifically, by determining the unique direct and indirect paths by which distinct facets of mindfulness relate to psychological health outcomes, we gain some insight into how mindfulness-based interventions may be effective. For example, non-judging of inner experience was most substantially related to exposure, which was substantially related to stress and anxiety symptoms. Thus, mindfulness-based interventions that focus specifically on cultivating non-judgment of inner experience may be most effective for reducing anxiety symptoms. Although most interventions that use mindfulness meditation as a core component use a range of distinct meditation techniques (e.g., sitting meditation, body scan, loving-kindness meditation), a logical next step in experimental research is to determine the specific sequelae of each of these distinct mindfulness techniques. For example, if loving-kindness meditation is most effective at cultivating non-judgment of inner experience, focusing specifically on this technique may be the most effective in allowing greater exposure to and better management of anxiety symptoms. Relatedly, specific mindfulness techniques can be geared toward individuals with particular needs. For example, if body scan is found to be most effective at increasing acting with awareness, an interventionist can predominantly use this technique among individuals who are particular low in this facet of mindfulness.
Conclusions
As acknowledged by Shapiro et al. (2006, 2009), their model is a model of the possible mechanisms of the heath-promoting effects of mindfulness, not the model, and thus was put forth tentatively. Although we found mixed support for this model, we found the model to have predictive utility and it is a useful starting point in the testing of psychological mechanisms of the beneficial effects of mindfulness. However, our results suggest that the model needs to be expanded. Although many of the models that have been proposed regarding the mechanisms of mindfulness focus on different levels of analyses (e.g., psychological versus neurophysiological), we need to identify the extent to which Shapiro et al.’s model is complementary or contradictory to other proposed models of the mechanisms of mindfulness (Baer, 2003; Hölzel et al., 2011; Kerr, Sacchet, Lazar, Moore, & Jones, 2013; Malinowski, 2013). Contradictory models can be tested against one another in a number of ways to determine the model with the most predictive utility, the best causal evidence, and/or the most clinical utility. Despite the preliminary nature of the present study’s findings, combining our results with studies that map specific mindfulness techniques to specific facets of mindfulness holds incredible promise for refining and tailoring mindfulness-based interventions for a variety of psychological health outcomes.
Supplementary Material
Supplementary Table 1. Descriptive statistics and correlations among all observed variables.
Supplementary Figure 1. Depicts the significant relationships (p < .05) in the estimated structural equation model (N = 944). The disturbances among health outcomes (depression, stress, anxiety, and alcohol-related problems), among the five facets of mindfulness, and among ‘mechanisms’ and distress tolerance were allowed to correlate. Non-significant paths as well as factor loadings to parcels are not shown in the figure for reasons of parsimony. Significant effects of the covariates as well as disturbances are available from the authors upon request.
Contributor Information
David B. Brown, Center on Alcoholism, Substance Abuse, and Addictions, Department of Psychology, University of New Mexico, 2650 Yale Blvd SE, MSC 11-6280, Albuquerque, NM, 87106
Adrian J. Bravo, Department of Psychology, Old Dominion University, Norfolk, VA
Corey R. Roos, Center on Alcoholism, Substance Abuse, and Addictions, Department of Psychology, University of New Mexico, 2650 Yale Blvd SE, MSC 11-6280, Albuquerque, NM, 87106
Matthew R. Pearson, Email: mateo.pearson@gmail.com, Center on Alcoholism, Substance Abuse, and Addictions, Department of Psychology, University of New Mexico, 2650 Yale Blvd SE, MSC 11-6280, Albuquerque, NM, 87106
References
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical psychology: Science and practice. 2003;10(2):125–143. doi: 10.1093/clipsy/bpg015. [DOI] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Williams JMG. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed Operational Definition. Clinical Psychology: Science and Practice. 2004;11:230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Marlatt A. Mindfulness-based relapse prevention use disorders: A pilot efficacy trial. Substance Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlin SL, Baer RA. Relationships between mindfulness, self-control, and psychological functioning. Personality and Individual Difference. 2012;52:411–415. doi: 10.1016/j.paid.2011.10.050. [DOI] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Cash M, Whittingham K. What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness. 2010;1:177–182. doi: 10.1007/s12671-010-0023-4. [DOI] [Google Scholar]
- Carey KB, Neal DJ, Collins SE. A psychometric analysis of the self-regulation questionnaire. Addictive Behaviors. 2004;29(2):253–260. doi: 10.1016/j.addbeh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer R. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA, Lykins B, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2009;65:613–626. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use and Misuse. 2013;49:492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. doi: http://dx.doi.org/10.2307/2136404. [PubMed] [Google Scholar]
- Desrosiers A, Klemanski DH, Nolen-Hoeksema S. Mapping mindfulness facets onto dimensions of anxiety and depression. Behavior Therapy. 2013;44:373–384. doi: 10.1016/j.beth.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M. Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R) In: The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. 3. Maruish ME, editor. Mahwah, NJ: Lawrence Erlbaum; 2004. pp. 363–377. [Google Scholar]
- Efron B, Tibshirani RJ. An introduction to the bootstrap. Vol. 57. CRC press; 1994. [Google Scholar]
- Ekholm E. Influence of the recall period on self-reported alcohol intake. European Journal of Clinical Nutrition. 2004;58:60–63. doi: 10.1038/sj.ejcn.1601746. [DOI] [PubMed] [Google Scholar]
- Enders CK. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychological methods. 2001;6(4):352. doi: 10.1037/1082-989X.6.4.352. [DOI] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [Google Scholar]
- Erceg-Hurn DM, Mirosevich VM. Modern robust statistical methods: an easy way to maximize the accuracy and power of your research. American Psychologist. 2008;63(7):591. doi: 10.1037/0003-066X.63.7.591. [DOI] [PubMed] [Google Scholar]
- Feldman G, Greeson J, Senville J. Differential effects of mindful breathing, progressive muscle relaxation, and loving-kindness meditation on decentering and negative reactions to repetitive thoughts. Behaviour Research and Therapy. 2010;48:1002–1011. doi: 10.1016/j.brat.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, Van Dulmen MHM, Segal ZV, Ma SH, Teasdale JD, Williams JMG. Initial psychometric properties of the experiences questionnaire: Validation of a self-report measure of decentering. Behavior Therapy. 2007;38:234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford; 1999. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your mind and body to face stress, pain, and illness. New York: Delacorte; 1990. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion Books; 1994. [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The brief young adult alcohol consequences questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29:1180–1189. doi: 10.1097/01.ALC.0000171940.95813.A5. [DOI] [PubMed] [Google Scholar]
- Keng S, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review. 2011;31:1041–1056. doi: 10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr CE, Sacchet MD, Lazar SW, Moore CI, Jones SR. Mindfulness starts with the body: somatosensory attention and top-down modulation of cortical alpha rhythms in mindfulness meditation. Frontiers in human neuroscience. 2013;7 doi: 10.3389/fnhum.2013.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh J, Bowen S, Marlatt A. Spirituality, mindfulness and substance abuse. Addictive Behaviors. 2005;30:1335–1341. doi: 10.1016/j.addbeh.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Leigh J, Neighbors C. Enhancement motives mediate the positive association between mind/body awareness and college student drinking. Journal of Social Clinical Psychology. 2009;28:650–669. doi: 10.1521/jscp.2009.28.5.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling. 2002;9:151–173. doi: 10.1207/S15328007SEM0902_1. [DOI] [Google Scholar]
- LyversMMakin C, Toms E, Thorberg FA, Samios C. Trait mindfulness in relation to emotional self-regulation and executive function. Mindfulness. 2013 doi: 10.1007/s12671-013-0213-y. [DOI] [Google Scholar]
- Malinowski P. Neural mechanisms of attentional control in mindfulness meditation. Frontiers in neuroscience. 2013;7 doi: 10.3389/fnins.2013.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn state worry questionnaire. Behavior Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Ostafin BD, Brooks JJ, Laitem M. Affective reactivity mediates an inverse relation between mindfulness and anxiety. Mindfulness. 2013 doi: 10.1007/s12671-013-0206-x. [DOI] [Google Scholar]
- Pearson MR, Brown DB, Bravo AJ, Witkiewitz K. Staying in the moment and finding purpose: The associations of trait mindfulness, decentering, and purpose in life with depressive symptoms, anxiety symptoms, and alcohol-related problems. Mindfulness. 2014 doi: 10.1007/s12671-014-0300-8. [DOI] [Google Scholar]
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57:1069–1081. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: Guilford Press; 2002. [Google Scholar]
- Shapiro S. The integration of mindfulness and psychology. Journal of Clinical Psychology. 2009;65:555–560. doi: 10.1002/jclp.20602. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. Journal of Clinical Psychology. 2006;62:373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. doi: 10.1007/s11031-005-7955-3. [DOI] [Google Scholar]
- Van Dam NT, Earleywine M. Validation of the center of epidemiologic studies depression scale-revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry Research. 2011;186:128–132. doi: 10.1016/j.psychres.2010.08.018. [DOI] [PubMed] [Google Scholar]
- Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. Journal of Research in Personality. 2009;43:374–385. doi: 10.1016/j.jrp.2008.12.008. [DOI] [Google Scholar]
- Witkiewitz K, Marlatt GA, Walker D. Mindfulness-based relapse prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy: An International Quarterly. 2005;19:211–228. doi: 10.1891/jcop.2005.19.3.211. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Descriptive statistics and correlations among all observed variables.
Supplementary Figure 1. Depicts the significant relationships (p < .05) in the estimated structural equation model (N = 944). The disturbances among health outcomes (depression, stress, anxiety, and alcohol-related problems), among the five facets of mindfulness, and among ‘mechanisms’ and distress tolerance were allowed to correlate. Non-significant paths as well as factor loadings to parcels are not shown in the figure for reasons of parsimony. Significant effects of the covariates as well as disturbances are available from the authors upon request.