Abstract
Cytotoxic bile acids, such as deoxycholic acid (DCA), are responsible for hepatocyte cell death during intrahepatic cholestasis. The mechanisms responsible for this effect are unclear, and recent studies conflict, pointing to either a modulation of plasma membrane structure or mitochondrial-mediated toxicity through perturbation of mitochondrial outer membrane (MOM) properties. We conducted a comprehensive comparative study of the impact of cytotoxic and cytoprotective bile acids on the membrane structure of different cellular compartments. We show that DCA increases the plasma membrane fluidity of hepatocytes to a minor extent, and that this effect is not correlated with the incidence of apoptosis. Additionally, plasma membrane fluidity recovers to normal values over time suggesting the presence of cellular compensatory mechanisms for this perturbation. Colocalization experiments in living cells confirmed the presence of bile acids within mitochondrial membranes. Experiments with active isolated mitochondria revealed that physiologically active concentrations of DCA change MOM order in a concentration- and time-dependent manner, and that these changes preceded the mitochondrial permeability transition. Importantly, these effects are not observed on liposomes mimicking MOM lipid composition, suggesting that DCA apoptotic activity depends on features of mitochondrial membranes that are absent in protein-free mimetic liposomes, such as the double-membrane structure, lipid asymmetry, or mitochondrial protein environment. In contrast, the mechanism of action of cytoprotective bile acids is likely not associated with changes in cellular membrane structure.
Keywords: apoptosis, bile acids and salts, bile acids and salts/physical chemistry, fluorescence microscopy, membranes/fluidity, membranes, mitochondria
Intrahepatic cholestasis is associated with the accumulation of abnormally high levels of hydrophobic bile acids in the liver, with elevated cytotoxic effects in hepatocytes and bile duct cells (1). Ultimately, bile acid toxicity can result in organ failure (2). Hydrophobic bile acids, such as deoxycholic acid (DCA; supplementary Fig. 1), have been reported to induce apoptosis in hepatocytes at low concentrations (≤100 μM) well below their critical micellar concentration (3), while higher concentrations (≥250 μM) induce cell death by necrosis (4). At submicellar extracellular concentrations (50–100 μM), these molecules have been proposed to activate cell death receptors in a ligand-independent manner (5); induce c-Jun N-terminal kinase 1-mediated activation of p53, elongation factor 2-1, and cyclin D1 expression (3, 6, 7); induce oxidative damage (8); promote B-cell lymphoma 2 (Bcl-2)-associated protein X (Bax) translocation to mitochondria (9); and induce mitochondrial dysfunction (8, 10). Any of these modifications alone are sufficient for caspase activation and initiation of apoptosis (3, 11). However, the precise triggering mechanism responsible for the activation of these apoptotic signaling events is still unknown.
On the other hand, submicellar extracellular concentrations (50–100 μM) of the more hydrophilic bile acids such as ursodeoxycholic acid (UDCA) and tauroursodeoxycholic acid (TUDCA) (supplementary Fig. 1) have the ability to inhibit apoptosis induced by certain agents in both hepatic and nonhepatic cells (10, 12). The UDCA and TUDCA effect seems to be related to the blockage of mitochondrial membrane damage (8), inhibiting disruption of the mitochondrial membrane potential by hydrophobic bile acids, reactive oxygen species production (10), and Bax protein translocation to mitochondria (13).
Activity of both cytotoxic and cytoprotective bile acids is likely to be triggered through two main mechanisms: i) death receptor modulation through changes in plasma membrane organization (extrinsic pathway of apoptosis) and/or ii) induction/inhibition of the membrane permeability transition in mitochondria (intrinsic pathway of apoptosis).
In support of the hypothesis that the plasma membrane is the target of cytotoxic bile acids, a recent study showed that cytotoxic bile acids such as DCA or chenodeoxycholic acid have the ability to disrupt to some extent the membrane-ordering effect induced by cholesterol (Chol) (14). Interestingly, this effect was much less efficient in the Chol-rich liquid-ordered phase (lo), possibly as a consequence of a lower affinity of the bile acids toward more ordered membranes (14–16). This was also recently confirmed in giant plasma membrane vesicles (GPMVs) isolated from rat tumor mast cells (17). The authors have suggested that DCA might interfere with the organization of signaling proteins due to its membrane-disordering effect.
In support of a classical intrinsic apoptotic pathway target, cytoprotective UDCA and TUDCA increased the threshold for apoptosis through inhibition of the mitochondrial permeability transition (MPT) in hepatocytes (10, 13, 18). It is possible that DCA and other cytotoxic bile acids act through activation of intrinsic pathways as well. This hypothesis is supported by evidence showing that hepatocytes deficient in Fas-receptor still undergo cell death after bile duct ligation or in culture after exposure to bile acids, indicating that the extrinsic apoptotic pathway is not essential for cytotoxic action (19). In this case, cytotoxic bile acids could act directly on mitochondrial membranes, either through a change of mitochondrial membrane properties or through a direct increase in the permeability of mitochondrial membranes. A recent study put forward compelling evidence suggesting that cytotoxic bile acids detach the inner boundary membrane from the mitochondrial outer membrane (MOM) and, finally, induce MPT, likely at the remaining contact sites (20).
In this work, we aimed to carry out for the first time a comprehensive characterization of the effect of physiologically active concentrations of cytotoxic and cytoprotective bile acids on the membrane properties of the most likely targets for modulation of cell death by bile acids, the plasma membrane and the mitochondrial membranes. We show that even very high concentrations of both cytotoxic and cytoprotective bile acids only increase plasma membrane fluidity of hepatocytes to a minor extent, and that this effect is not correlated with apoptosis. Additionally, the plasma membrane fluidity recovers to normal (untreated) values during long incubations, suggesting the presence of cellular compensatory mechanisms to maintain plasma membrane integrity. The impact of cytotoxic and cytoprotective bile acids on the average intracellular membrane fluidity is comparable, although for longer incubation times, a dramatic decrease in membrane fluidity is only observed for the cytotoxic DCA. The latter effect is preceded by apoptosis, and it is likely a consequence of the apoptotic process itself. On the other hand, only cytotoxic bile acids had an impact on isolated MOM order, and this effect preceded the onset of mitochondria permeabilization. In addition, we showed that DCA-mediated changes in mitochondrial membrane organization are not observed in protein-free liposomes mimicking mitochondrial membrane lipid composition. These findings identify mitochondrial membranes as a likely target of the cytotoxic bile acid DCA and suggest that the mechanism of action of DCA is associated with changes in mitochondrial membrane features that are absent from protein-free mimetic liposomes.
MATERIALS AND METHODS
Chemicals and reagents
1,2-Dioleoyl-sn-glycero-3-phosphocholine, 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine, l-α-phosphatidylinositol (PI) sodium salt, POPC, N-palmitoyl-d-erythrosphingosylphosphorylcholine, and 1,3-bis(sn-3′-phosphatidyl)-sn-glycerol (cardiolipin, CL) were purchased from Avanti Polar Lipids (Alabaster, AL). Chol was obtained from Sigma-Aldrich (St. Louis, MO). Stock solutions of all lipids were prepared with Uvasol-grade chloroform with the exception of CL, which was prepared in chloroform-methanol (2:1). Both solvents were obtained from Sigma-Aldrich. DCA and TUDCA in sodium salt form, methyl-β-cyclodextrin (CD), NaCl, succinate, and sucrose were purchased from Sigma-Aldrich. UDCA sodium salt was purchased from Santa Cruz Biotechnologies (Santa Cruz, CA), and Tris from Merck (Darmstadt, Germany).
1-[2-Hydroxy-3-(N,N-di-methyl-N-hydroxyethyl)ammoniopropyl]-4-[β-[2-(di-n-butylamino)-6-napthyl] vinyl]pyridinium dibromide (Di-4-ANEPPDHQ), 6-dodecanoyl-2-dimethylaminonaphthalene (Laurdan), [6-amino-9-(2-methoxycarbonylphenyl)xanthen-3-ylidene]azanium (Rho-123), and wheat germ agglutinin conjugated with Alexa Fluor 594 (A594-WGA) were purchased from Invitrogen (Carlsbad, CA). 5(6)-Carboxyfluorescein (CF) was obtained from Sigma-Aldrich. Fluorescently labeled bile acid derivatives were obtained as previously described (14).
Cell culture, isolation of rat primary hepatocytes, and rat liver mitochondria
Primary rat hepatocytes were isolated from the liver of male rats (100–150 g) by collagenase perfusion as previously described (21, 22). After isolation, hepatocytes were resuspended in Complete William’s E medium (Sigma-Aldrich) (23) and plated on PrimariaTM tissue culture dishes (BD Biosciences, San Jose, CA) at 5 × 104 cells/cm2. Cells were maintained at 37°C in a humidified atmosphere of 5% CO2 for 6 h to allow attachment. Plates were then washed with medium to remove dead cells and incubated in Complete William’s E medium. Experiments with hepatocytes were carried out 24 h after plating. HEK293T cells were cultured and maintained in DMEM with 10% FBS and 1% of penicillin-streptomycin (Sigma Chemical Co., St. Louis, MO) at the incubator with controlled temperature (37°C), humidity, and CO2 levels (5%). Low calcium liver mitochondria were isolated from male 200–250 g Sprague-Dawley rats by density gradient centrifugation, as previously published (18, 24). All experiments involving animals were performed by an investigator accredited for directing animal experiments (Federation of Laboratory Animal Science Associations, FELASA level C), in conformity with the Public Health Service Policy on Humane Care and Use of Laboratory Animals, incorporated in the Institute for Laboratory Animal Research’s Guide for the Care and Use of Laboratory Animals. Experiments received prior approval from the Portuguese National Authority for Animal Health.
Cell viability and caspase-3/7 activity measurements
Rat primary hepatocytes were cultured in 96-well assay plates, and the ApoTox-Glo triplex assay (Promega Corp., Madison, WI) was used according to the manufacturer’s protocol. Cell death was also evaluated by the Lactate Dehydrogenase (LDH) assay kit (Sigma) and LDH activity was evaluated in cell culture media. Fluorescence measurements were carried out using a Bio-Rad microplate reader model 680 (Bio-Rad, Hercules, CA).
Confocal and two-photon fluorescence microscopy
All measurements were performed on a Leica TCS SP5 (Leica Microsystems CMS GmbH, Manheim, Germany) inverted confocal microscope (DMI600). Excitation lines were provided by an Argon laser that was focused into the sample by an apochromatic water immersion objective (63×, NA 1.2; Zeiss, Jena, Germany). A 111.4 μm diameter pinhole positioned in front of the image plane blocked out-of-focus signals.
Two-photon excitation measurements of Laurdan were obtained using the same setup coupled to a Ti:sapphire laser (Mai Tai, Spectra-Physics, Darmstadt, Germany) as the excitation source. The excitation wavelength was set to 780 nm and the fluorescence emission of Laurdan was collected at 400–460 nm (I400–460) and 470–530 nm (I470–530). Following incubation with bile acids, rat primary hepatocytes and HEK293T cells were incubated with 5 µM of Laurdan for 15 min. Generalized polarization (GP) images were obtained using homemade software developed in a MATLAB environment (Mathworks, Natick, MA), with the GP value defined as GP = (I400–460 − G· I470–530)/(I400–460 + G· I470–530). Both channel intensities are corrected for background contributions, and the calibration factor G was obtained from imaging Laurdan in DMSO using the same experimental conditions as those set for the samples under study (25).
Colocalization studies with A594-WGA were performed with 633 nm excitation and detection of emission at 695 ± 55 nm. For the colocalization studies between bile acid analogs and the mitochondrial marker, Rho-123, spectral imaging was performed in combination with linear unmixing (26) because the n-(7-nitrobenz-2-oxa-l,3-diazol-4yl) (NBD) and Rho-123 spectra display partially overlapped. Briefly, fluorescence from cells labeled with bile acid analogs and Rho-123 was acquired at different wavelengths for excitation at 458 and 514 nm, and images were computationally processed by a linear unmixing algorithm using the distinct reference spectrum of NBD and Rho-123, which were obtained independently. This procedure was carried out using homemade software created in a MATLAB environment (Mathworks). The product of the difference from the mean (PDM) and Pearson’s correlation coefficient (Rr) (27) parameters were obtained through WCIF ImageJ (http://www.uhnresearch.ca/facilities/wcif/imagej/).
Fluorescence lifetime imaging microscopy
Fluorescence lifetime imaging microscopy (FLIM) of di-4-ANEPPDHQ in HEK293T cells was performed using a Becker and Hickl setup (Berlin, Germany). Two-photon excitation (800 nm) was used to excite di-4-ANEPPDHQ. Two-photon excitation pulses were generated by an Ti:sapphire laser with a pulse frequency of 80 MHz. Emission light was selected with a dichroic beam splitter with an excitation SP700 short-pass filter and an emission 535/85 band-pass filter inserted in front of the photomultiplier and was recorded using a PMC-100-4 cooled high-speed PMT detection head (Becker and Hickl). Images were acquired using a Becker and Hickl SPC 830 module.
The analysis of fluorescence decays was carried out using a nonlinear, least-squares iterative convolution method based on the Marquardt algorithm (28) through the use of the software SPCImage (Beker and Hickl).
MPT detection
MPT was measured spectrophotometrically during 30 min incubations at 37°C using mitochondria (1 mg of protein/ml) suspended in 3 ml of a Chelex-100-treated buffer containing 0.1 M NaCl, 10 mM MOPS, pH 7.4 (10). Mitochondrial swelling was monitored at 540 nm in a Beckman DU 64 spectrophotometer. Basal values of mitochondria absorbance were measured for 5 min.
Lipid vesicle preparation
Large unilamellar vesicles (LUVs; 100 nm) were prepared through extrusion as previously described (29). Vesicles were suspended in Tris buffer (10 mM Tris, 150 mM NaCl at pH 8.0, prepared in Milli-Q water) followed by freeze-thaw cycles and extrusion through polycarbonate filters (100 nm pore size). Liposomes with encapsulated dye were prepared in 10 mM Tris, 150 mM NaCl, 90 mM CF at pH 8.0. Nonencapsulated CF was separated from the liposomes by gel filtration chromatography on a Sephadex G-50 column.
All LUVs were kept at room temperature and in the dark until being used, at most for 48 h after being prepared. Lipid concentrations were determined by phosphorous analysis (30), and Chol concentration was determined gravimetrically.
Membrane fluidity measurements in isolated mitochondria and protein-free liposomes
Fluorescence steady-state measurements of di-4-ANEPPDHQ were performed as previously described (14). The fluorescence intensities were calculated through integration of the emission spectra obtained, and background fluorescence intensity was always subtracted. For measurement of mitochondrial membrane fluidity, isolated rat liver mitochondria were incubated with 5 µM di-4-ANEPPDHQ for 1 h. Unbound probe was removed through a 10 min centrifugation (7,000 g) at 4°C. Fluorescence anisotropy values of di-4-ANEPPDHQ (λexc = 460 nm; λem = 590 nm) were determined after incubating these samples with bile acids at 37°C. Di-4-ANEPPDHQ was incorporated in LUVs mimicking mitochondrial membranes at a probe-to-lipid ratio of 1:200.
Leakage assays in protein-free liposomes
In the CF leakage assay (λexc = 492 nm; λem = 517 nm), LUVs encapsulating CF in suspensions containing 200 μM of lipids were incubated with 100–500 μM of bile acids. Complete (100%) permeabilization was achieved via the addition of Triton X-100 to a final concentration of 1%. Spontaneous leakage was always measured in the absence of bile acids, and experiments were conducted at 25°C. The percentage of CF leakage induced by bile acids was calculated as Leakage (%) = 100 × [(F − F0) − (Fc − F0)]/(Ft − F0), in which F and Ft are the fluorescence intensity prior to and after the addition of the Triton X-100 (after incubation with bile acids), respectively, and F0 and Fc are the fluorescence of intact vesicles before and after the same incubation time. In this way, leakage values were corrected for any intrinsic leakage observed in the absence of bile acids.
RESULTS
Concentration and time-dependent effect of cytotoxic and cytoprotective bile acids on hepatocyte viability and apoptosis
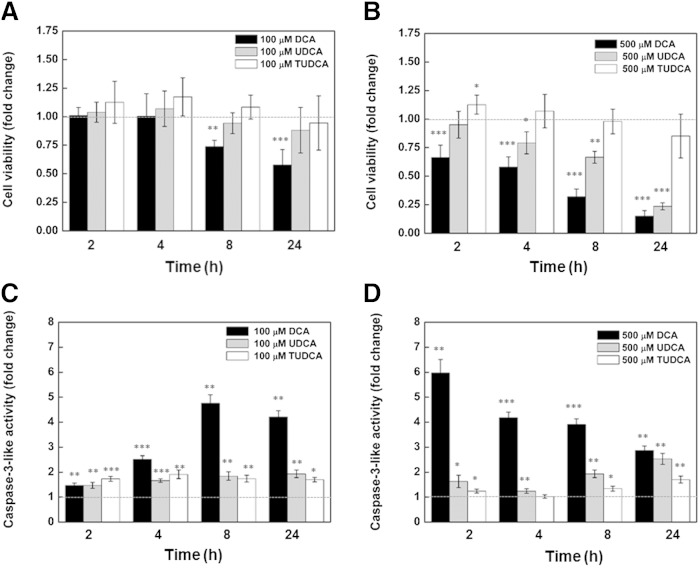
In order to investigate a possible correlation between programmed cell death and changes in hepatocyte membrane order after treatment with bile acids, we first studied the concentration- and time-dependent effect of the cytotoxic and cytoprotective bile acids on cell viability and on the triggering of apoptosis (Fig. 1). Results clearly show that at the lower concentrations used (100 μM), only cells treated with DCA have significantly lower viability and highly upregulated apoptosis over time (Fig. 1A, C). Increased levels of apoptosis during DCA treatment are only detected after an incubation of 4 h (Fig. 1C), and cell viability starts to decrease after this time (Fig. 1A). For a necrosis-inducing concentration of DCA (500 μM), a significant decline in cellular viability and drastically higher apoptosis levels are already detected 2 h after the start of the treatment (Fig. 1B, D). Lower levels of apoptosis were detected for longer incubation times, probably as a result of necrosis. At this higher concentration, UDCA is no longer cytoprotective, and an upregulation of apoptosis is detected as well as a significant decrease in cell viability. TUDCA, on the other hand, did not demonstrate significant toxicity even after 24 h of hepatocyte treatment at 500 μM of the bile acid.
Fig. 1.
Concentration and time dependency of cellular viability and caspase-3-like activity of primary rat hepatocytes in the presence of cytotoxic and cytoprotective bile acids. Cells were isolated as described in Materials and Methods and treated with 100 μM (A, C) or 500 μM (B, D) of DCA (black) or the cytoprotective UDCA (gray)/TUDCA (white) bile acids. Both cellular viability (A, B) and caspase-3-like activity (C, D) in hepatocytes were measured with the ApoTox-Glo triplex assay. Values for both cellular viability and caspase-3-like activity are normalized to control samples from the respective time point. Results are expressed as mean ± SEM fold change of at least three independent experiments. * P < 0.05, ** P < 0.01, and *** P < 0.001 from the respective time point control.
Impact of cytotoxic and cytoprotective bile acids on plasma membrane and intracellular membrane fluidity
Recent results on the interaction of cytotoxic bile acids such as DCA with membrane model systems and on GPMVs (14, 17) have confirmed that apoptosis-inducing bile acids are able to modulate lipid membrane fluidity, suggesting that their physiological activity could be associated with this effect. Different organelles have been anticipated as targets for cytotoxic bile acids, namely, the plasma membrane (17) and the mitochondria (20). Our approach to elucidate this issue was to carry out a quantitative evaluation of the impact of physiologically active DCA concentrations on the membrane order of both these organelles.
Confocal microscopy measurements on rat hepatocytes were carried out using fluorescent probes sensitive to membrane order. Both di-4-ANEPPDHQ (31, 32) and Laurdan (33, 34) have proved to be extremely sensitive to changes in membrane order through changes in their fluorescence emission spectra or lifetimes. Both molecules sense the reorientation of solvent dipoles, whose strength is directly dependent on membrane fluidity, this being related to water penetration within membranes (31, 33). The measurement of shifts in Laurdan emission spectra through ratiometric imaging (25) and changes of di-4-ANEPPDHQ fluorescence lifetime through FLIM (32) are widely used methodologies that allow for a quantitative assessment of membrane order in living cells.
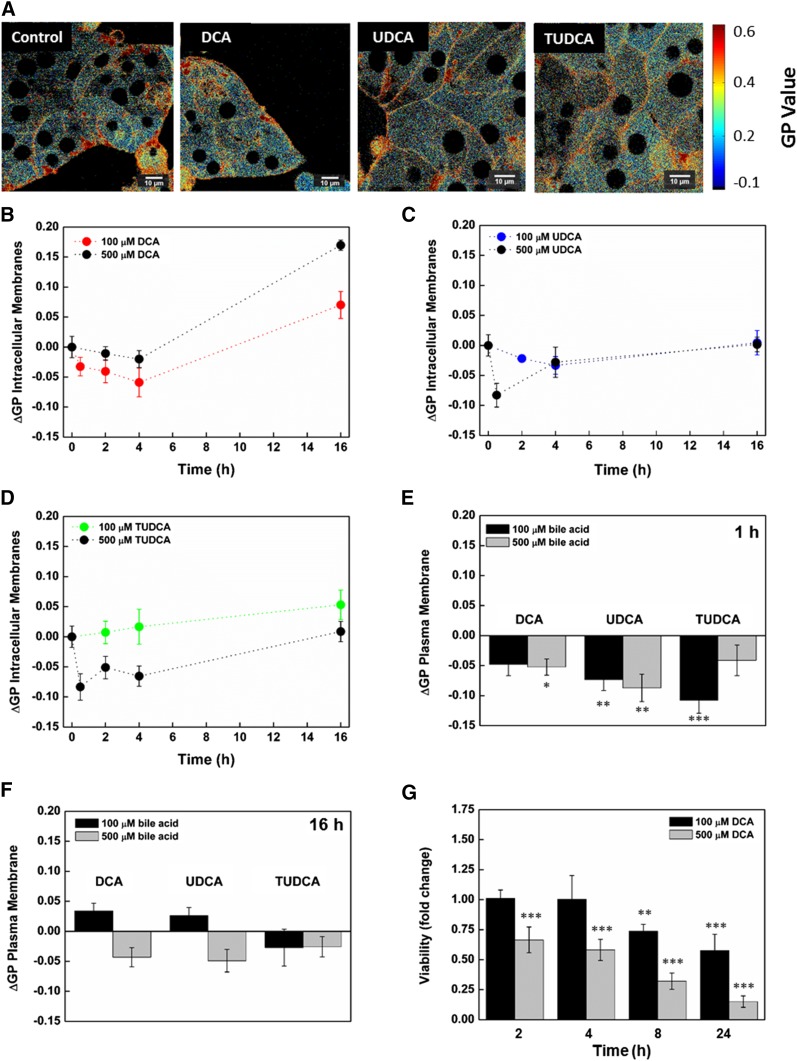
The membrane probe di-4-ANEPPDHQ failed to incorporate in hepatocytes so that only Laurdan was used to detect bile-acid-induced changes in the membrane order of these cells. Laurdan fluorescence emission spectral shifts were quantified through the GP function, and higher GP values are associated with higher membrane ordering. In agreement, higher GP values were measured for the plasma membrane than in intracellular membranes (Fig. 2A and supplementary Fig. 2). This was expected because the Chol concentration is much higher in the plasma membrane. The membrane order of untreated hepatocytes changed over time in a reproducible way (supplementary Fig. 2), probably due to the adaptation of cells to the culture environment. From this experiment, control values are obtained (GPcontrol), this allowing us to determine the relative GP variations (ΔGP = GPbile acid − GPcontrol) for each bile acid and incubation time. These values are shown in Fig. 2B–F. Results are presented for both the average ΔGP of intracellular membranes (Fig. 2B–D) and for the plasma membrane (Fig. 2E, F) of bile-acid-treated hepatocytes compared with untreated cells.
Fig. 2.
Changes in Laurdan GP values in membranes of rat hepatocytes in the presence of DCA and the cytoprotective UDCA/TUDCA bile acids. Laurdan GP values were calculated as described in Materials and Methods. GP images of hepatocytes after 30 min incubation with 100 μM of bile acids (A). Relative changes (ΔGP) between treated and untreated cultures of hepatocytes at different incubation times are shown (B–G). The impact of exposure to bile acids on GP values over time is shown for hepatocyte intracellular membranes in the presence of DCA (B), UDCA (C), and TUDCA (D) at both 100 and 500 μM. The impact of exposure to bile acids on hepatocyte plasma membrane GP values is shown both for 1 h (E) and 16 h (F) incubations. Time dependency of DCA toxicity on isolated hepatocytes at 100 μM (black) and 500 μM (gray) is also shown for comparison (G). Results are expressed as mean ± SEM fold change of at least 12 cells (B–F) or as mean ± SEM fold change of at least three independent experiments (G). * P < 0.05, ** P < 0.01, and *** P < 0.001 from the respective time point control.
After incubation of hepatocytes with 100 μM of DCA during 4 h, only a moderate decrease of GP values in intracellular membranes was observed (Fig. 2B), and longer exposures led to an increase in intracellular membrane order. Exposure to higher (necrosis-inducing) concentrations of DCA (500 μM) virtually eliminated the early decrease in GP values for intracellular membranes and potentiated the late increase in membrane ordering. Incubations of hepatocytes with UDCA and TUDCA at 100 μM had no impact on intracellular membrane fluidity (Fig. 2C, D), although higher concentrations of these bile acids also led to an early decrease in the average intracellular membrane order. However, for both bile acids, Laurdan GP values recovered to control values over time. This recovery is highly indicative of the presence of cellular compensatory mechanisms such as membrane traffic, lipid synthesis, or bile acid efflux, which might contribute to reduce bile-acid-dependent membrane damage. In light of these results, the late increases in GP values observed after long incubations with DCA are likely associated with membrane composition changes resulting from cell death because they are not detected for cytoprotective bile acids, and for 100 μM DCA, this increase in GP values only occurs after the onset of apoptosis (Fig. 1C) and cell death (Fig. 2G).
The impact on hepatocyte plasma membrane order was moderate for all bile acids studied, even at high concentrations and short (Fig. 2E) or long (Fig. 2F) incubation times. Lower hepatocyte plasma membrane order was detected 1 h after incubation with DCA, UDCA, and TUDCA (Fig. 2E), and as observed for intracellular membranes, Laurdan GP recovered over time to values closer to control values (Fig. 2F). Unlike in intracellular membranes, no significant late changes in membrane order were detected for the plasma membrane after DCA treatment, even at necrosis-inducing concentrations (Fig. 2F).
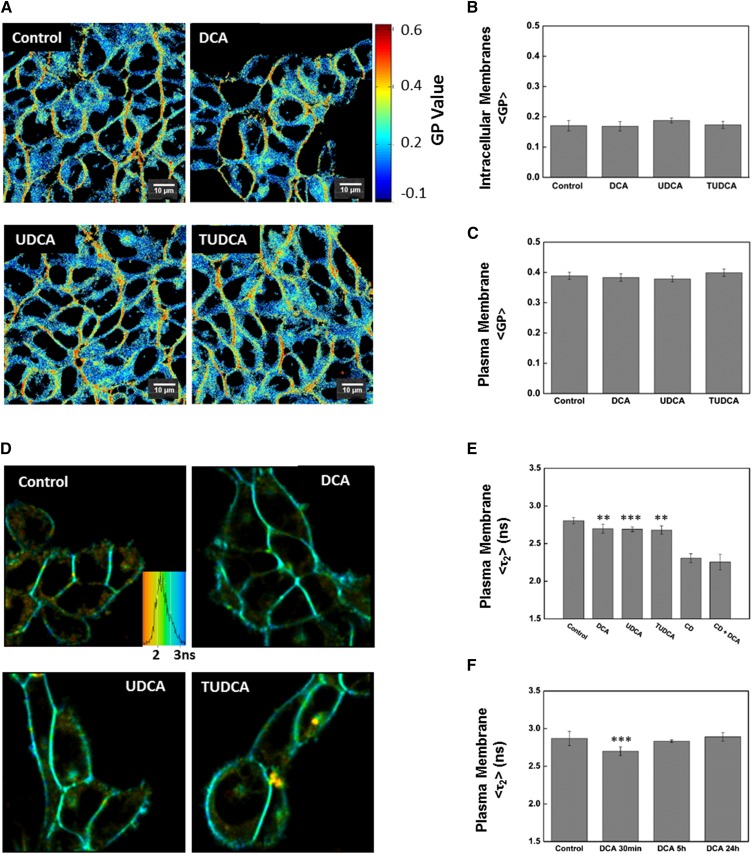
The impact of cytotoxic and cytoprotective bile acids on plasma and intracellular membrane structure was also assessed in HEK293T cells. A much lower intracellular bile acid influx is anticipated for the nonhepatic HEK293T cells, given the absence of the bile acid transporters present in hepatocytes (35), so only the outer leaflet of the plasma membrane is expected to be in contact with a significant concentration of these molecules, eliminating a possible influence of bile acids on mitochondrial membrane properties and on intrinsic apoptotic pathways. In fact, cytotoxicity studies confirmed that this cell line had very low susceptibility for cell death induced by DCA (supplementary Fig. 3). Laurdan GP values in both intracellular and plasma membranes of HEK293T cells after exposure to DCA, UDCA, and TUDCA are shown in Fig. 3A–C. In the absence of significant intracellular influx, no changes in intracellular membrane fluidity are observed (Fig. 3B), and Laurdan GP values for the plasma membrane, which is exposed to bile acids, are largely insensitive to the presence of cytotoxic and cytoprotective bile acids (Fig. 3C).
Fig. 3.
Impact of DCA and cytoprotective bile acids UDCA/TUDCA on the membrane fluidity of HEK293T cells. HEK293T cells were loaded with either 5 µM of Laurdan (A) or 5 µM of di-4-ANEPPDHQ (D) after incubation with 100 µM of bile acids for 30 min at 37°C. Representative Laurdan GP (A) and di-4-ANEPPDHQ fluorescence lifetime (τ) (D) images are shown. Laurdan GP values, di-4-ANEPPDHQ fluorescence lifetimes, and the respective images were obtained as described in Materials and Methods. Average Laurdan GP values after incubation with bile acids are shown for both intracellular (B) and the plasma membranes (C). Average di-4-ANEPPDHQ fluorescence lifetimes are shown for the plasma membrane of HEK293T cells after treatment with bile acids for 30 min. (E). The impact of DCA on the plasma membrane fluidity on HEK293T cells is shown to be time dependent, as fluorescence lifetimes of di-4-ANEPPDHQ return to control values for incubations longer than 5 h (F). Only the value for the longer lifetime component (τ) of di-4-ANEPPDHQ fluorescence decay is shown (E, F) because this component corresponds to ∼97% total fluorescence intensity. Partial Chol extraction from the plasma membrane with 10 mM CD reduced the order of the plasma membrane as expected (CD), but the plasma membrane order remained insensitive to the presence of DCA, even after Chol extraction (CD + DCA). Average GP values are expressed as mean ± SEM from an average of 12 individual cells, and average di-4-ANEPPDHQ fluorescence lifetimes are the average of 50–100 cells.
The alternative sensor for membrane order, di-4-ANEPPDHQ, efficiently incorporated in the plasma membrane of HEK293T cells and was also used to probe for bile-acid-induced changes in plasma membrane properties (Fig. 3D–F). Decreases in membrane ordering are expected to induce a significant decrease in fluorescence lifetime of di-4-ANEPPDHQ in living cells (32), and FLIM measurements were carried out in HEK293T cells before and after a 30 min exposure to bile acids (Fig. 3D). A minor decrease in plasma membrane order after exposure to physiologically active concentrations of bile acids was detectable through di-4-ANEPPDHQ fluorescence lifetimes because incubation of HEK293T cells with DCA, UDCA, and TUDCA induced a small decrease in the fluorescence lifetime of di-4-ANEPPDHQ (Fig. 3E). As previously observed in hepatocytes with Laurdan, after long incubations with bile acids, membrane fluidity returned to control levels (Fig. 3F). The fact that no significant changes in HEK293T plasma membrane fluidity were observed with Laurdan after exposure to bile acids, but some decrease in membrane order is still observed with di-4-ANEPPDHQ, suggests that the impact of bile acids on the plasma membrane is much higher in the bile-acid-exposed outer leaflet, as the translocation of the cationic di-4-ANEPPDHQ across the membrane is very slow, while Laurdan easily flip-flops due to the absence of charge. This is consistent with the absence of bile acid internalization, when only the outer leaflet of the plasma membrane remains exposed to bile acids.
Because Chol was recently shown to modulate the membrane affinity of bile acids (14), the impact of DCA on plasma membrane order was also evaluated after partial Chol depletion with 10 mM CD. This concentration of CD has been reported to remove 30–60% of cellular Chol, depending on cell type, and to disrupt membrane rafts (36). CD treatment reduced plasma membrane order considerably, as reported by the substantial decrease in di-4-ANEPPDHQ fluorescence lifetime, but even after Chol depletion, 100 μM DCA had no major impact on plasma membrane order (Fig. 3E).
The absence of considerable and nontransient modulation of plasma membrane order by DCA is surprising, given the ability of this bile acid to inhibit Chol ordering in membrane model systems (14). Clearly, the minor changes in plasma membrane properties detected upon DCA treatment of hepatocytes are not responsible for its apoptosis/necrosis-promoting effect, because identical relative changes are observed in both DCA-responsive (hepatocytes) and DCA-nonresponsive cells (HEK293T), as well as for noncytotoxic bile acids. These results strongly suggest that changes in plasma membrane order are not the mechanism through which DCA induces apoptosis.
Similarly, the changes detected in intracellular membrane order in hepatocytes after a short incubation period with bile acids were common to all bile acids tested (Fig. 2), and only the onset of apoptosis gave rise to considerable hepatocyte intracellular membrane modifications as revealed by their biophysical parameters. In the absence of apoptosis, both hepatocytes and a nonhepatic cell line were shown to have compensatory mechanisms that led to full abolition of bile acid perturbation of cellular membrane order after long incubations. Thus, it seems evident that the apoptotic modulatory effect of cytoprotective UDCA/TUDCA and cytotoxic DCA is also not the result of indiscriminate changes in the structure of cellular membranes, and more specific mechanisms must account for these effects.
Subcellular distribution of bile acid derivatives
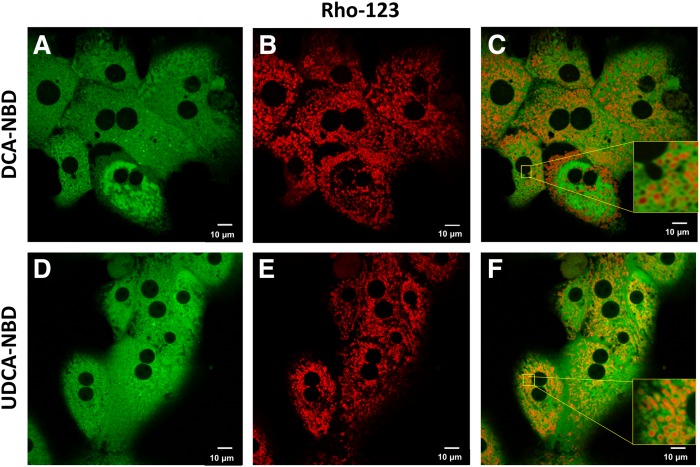
In order to determine whether bile acids have the potential to incorporate in mitochondrial membranes, the distribution of the fluorescent conjugates, DCA-NBD and UDCA-NBD, in living cells was followed through confocal microscopy, both in hepatocytes (Fig. 4) and in HEK293T cells (Fig. 5). Similar fluorescent conjugates of bile acids have been extensively used to study the mechanisms of uptake and excretion of bile acids by hepatocytes (37–40). These bile acid fluorescent analogs were characterized in a previous study, where DCA-NBD and UDCA-NBD were shown to have a superficial location in lipid membranes and to interact preferentially with less ordered liposomes, in agreement with results obtained with unmodified bile acids (14). Thus, the labeled bile acids are expected to be adequate reporters for the intracellular distribution of unmodified bile acids. However, some important differences between the modified and unmodified molecules are still present, namely, because the fluorescent analogs are uncharged, cellular uptake does not require membrane transporters, and uptake by both hepatic and nonhepatic cells (HEK293T) is passive and fast (Figs . 4, 5).
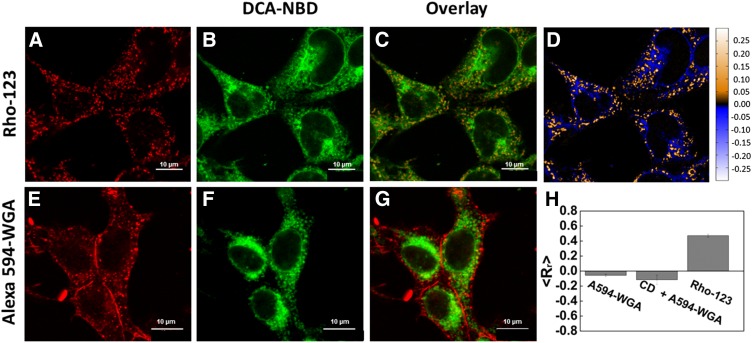
Fig. 4.
Subcellular distribution of bile acid fluorescent analogs in hepatocytes. Representative confocal microscopy analysis of the subcellular distribution of DCA-NBD (A) and UDCA-NBD (D) in hepatocytes after internalization. Rat liver hepatocytes were incubated with 20 μM of bile acid analogs during 30 min at 37°C. Mitochondria were fluorescently stained with 5 μM Rho-123 for 15 min at 37°C (B, E). Overlay images are shown (C, F). Inset images show the presence of bile acid analogs in the outer mitochondrial membrane.
Fig. 5.
Subcellular distribution of DCA-NBD in HEK293T cells. Mitochondria or plasma membranes of HEK293T cells were fluorescently stained with 5 μM Rho-123 (mitochondrial marker) (A) and 130 nM A594-WGA (plasma membrane marker) (E), respectively. The subcellular distribution of 20 µM of DCA-NBD (B, F) in these cells after internalization is also shown by colocalization analysis. Overlay images for DCA-NBD fluorescence and mitochondria (C) or plasma membrane (G) staining are also shown. DCA-NBD distributes through different organelles, including mitochondria, as evidenced by colocalization with mitochondrial membrane marker. As a result, positive PDM (27) values are obtained within the mitochondria, while other intracellular organelles loaded with DCA-NBD present negative PDM values (D). Pearson correlation coefficients (Rr) (27) confirm partial colocalization between DCA-NBD and Rho-123 signals as well as poor colocalization of DCA-NBD with the plasma membrane marker A594-WGA (H). Partial Chol extraction with 10 mM CD did not increase incorporation of DCA-NBD in the plasma membrane (CD + A594-WGA) (H). Results are expressed as mean ± SEM of 50–60 cells.
Rho-123 is a noncytotoxic, cell-permeant, cationic dye that is rapidly sequestered in the matrix space of polarized mitochondria (41). Hepatocytes were incubated with Rho-123 and either DCA-NBD or UDCA-NBD, and the respective fluorescence confocal microscopy images are shown in Fig. 4. Efficient mitochondria labeling by Rho-123 on hepatocytes was observed (Fig. 4B, E), while DCA-NBD and UDCA-NBD were found to incorporate nonspecifically in intracellular membranes. The bile acid analogs exhibit a very limited insertion in the plasma membrane, suggesting a low affinity for this environment. The concentrations of the bile acid analogs in the cytosol are also relatively low. Both bile acid analogs are also clearly shown to insert in the mitochondrial membranes of hepatocytes (Fig. 4C, F, insets). Full overlap of Rho-123 and bile acid-NBD fluorescence is not observed, because Rho-123 is found within the matrix space of mitochondria and the bile acid analogs insert mostly in the outer mitochondrial membranes (supplementary Fig. 4).
Interaction of bile acid analogs with mitochondria is not specific to hepatocytes, as it is also observed in HEK293T cells. In these cells, DCA-NBD fluorescence is also found in mitochondria as evidenced by partial colocalization of Rho-123 marker and DCA-NBD (Fig. 5C). This partial colocalization is confirmed and quantified through calculation of PDMs (Fig. 5D) and of the Pearson’s correlation coefficient (<Rr>) of the two signals (Fig. 5H). Although this colocalization is clear, DCA-NBD fluorescence is again observed throughout different intracellular compartments, revealing no apparent specific enrichment (Fig. 5B, F). As in hepatocytes, very little DCA-NBD fluorescence is detected in the plasma membrane (Fig. 5E–H).
Previous work with model membranes showed that membrane ordering and Chol concentration dramatically influenced the partition of both cytotoxic and cytoprotective bile acids to lipid membranes (14). The preference of DCA-NBD for intracellular membranes, which present significantly lower Chol concentration compared with the plasma membrane, suggested that this property could contribute to define the preferential sites for accumulation of bile acids intracellularly. However, Chol depletion and membrane raft disruption with 10 mM CD had no impact on the concentration of DCA-NBD in the plasma membrane (Fig. 5H). Thus, it is unlikely that exclusion of bile acids from the plasma membrane is solely dictated by differences in Chol concentration, and other unknown factors are expected to be responsible for this effect.
The results for the subcellular distribution of UDCA-NBD after uptake in HEK293T cells are largely analogous to those obtained with DCA-NBD (supplementary Fig. 5). Cytoprotective UDCA-NBD is also found in mitochondrial membranes, while very little UDCA-NBD is detected at the plasma membrane. These results reinforce the notion that apoptosis modulation by bile acids is likely not the result of changes in plasma membrane organization.
Impact of cytotoxic and cytoprotective bile acids on mitochondrial membranes
The ability of bile acid conjugates to bind to mitochondria was also confirmed through steady-state fluorescence intensity measurements of bile acid fluorescent analogs. Incubation of both DCA-NBD and UDCA-NBD with freshly isolated liver mitochondria resulted in an increase in fluorescence intensity of the labeled bile acids, which is clear evidence of interaction (supplementary Fig. 6).
Given the presence of both classes of bile acids in the mitochondrial membrane during incubation of living cells, there is a strong potential for modulation of mitochondrial membrane properties. Because the integrity of mitochondrial membranes is essential for cellular survival, these changes might also potentially lead to an activation/inhibition of MPT. Importantly, changes in mitochondrial membrane fluidity have been correlated with differential Bax activation and apoptosis (42) and import of glutathione into the mitochondria (43). Recently, it was demonstrated through electron microscopy of isolated mitochondria that after exposure to toxic concentrations of bile acids, mitochondria undergo a dramatic reorganization of the MOM before the onset of MPT, suggesting that the MOM is the major target site for cytotoxic bile acids within mitochondria (20). Previous studies have also identified changes in average membrane fluidity of isolated mitochondria after exposure to toxic bile acids (44). Here, we aimed to follow in real time the changes in MOM properties and correlate these changes with the onset of MPT. Although during in vivo cholestasis, the total intracellular concentrations of bile acids in hepatocytes are reported to be ∼800 µM (45, 46), it is difficult to estimate the intracellular concentration of free bile acids as a significant population is expected to be complexed with membranes and proteins. For this reason, we chose to carry out measurements with isolated mitochondria at identical concentrations as used in the other experiments, so that direct comparisons for membrane sensitivity to DCA insertion could be established.
Measurements of MOM fluidity in functional freshly isolated mitochondria were carried out using di-4-ANEPPDHQ (Fig. 6), whose fluorescence properties have been shown to be extremely sensitive to membrane composition and order (25). Although the MOM is permeable to small hydrophilic molecules due to the presence of mitochondrial porins (47), di-4-ANEPPDHQ is expected to selectively stain the MOM, as a result of the presence of two cationic groups and a large hydrophobic moiety in this molecule, which drastically minimize flip-flop across membranes (31) and porin transport (47), respectively. The fluorescent membrane probe readily incorporated in isolated mitochondria and unbound di-4-ANEPPDHQ was removed through centrifugation. Fluorescence anisotropy of membrane-inserted probes such as di-4-ANEPPDHQ is ideally suited to follow changes in membrane structure/dynamics. In fact, because rotation of these molecules is hindered within membranes, any structural or dynamical change in membrane properties will affect the rotational freedom of the molecule, and this is easily detected through steady-state fluorescence anisotropy (<r>) measurements. The fluorescence anisotropy of di-4-ANEPPDHQ within isolated mitochondria was measured to be <r > ∼0.24 (Fig. 6).
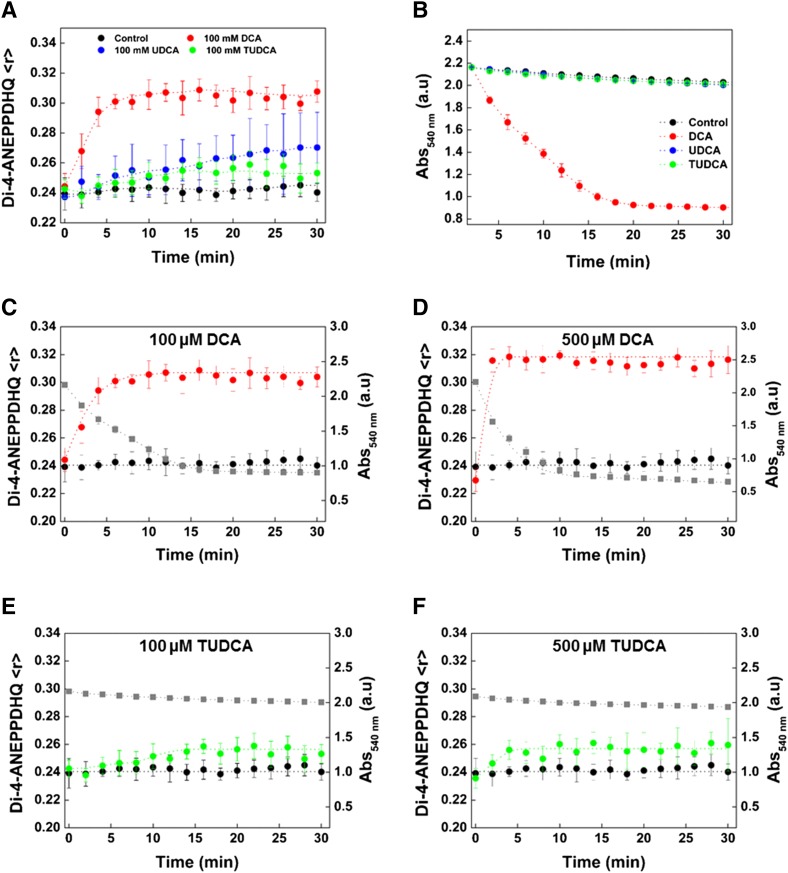
Fig. 6.
DCA induces changes in MOM structure, which precede the onset of MPT. Comparison between changes in membrane order of freshly isolated rat liver mitochondria over time after exposure to DCA (red), UDCA (blue), and TUDCA (green) at 100 μM (A). Mitochondrial membrane order in freshly isolated rat liver mitochondria was monitored through fluorescence anisotropy measurements of di-4-ANEPPDHQ after removal of unbound membrane probe by centrifugation. Control values (untreated samples) are shown in black. Detection of mitochondrial swelling after exposure of isolated rat liver mitochondria to DCA (red), UDCA (blue), and TUDCA (green) at 100 μM (B). Control values are shown in black. Mitochondrial swelling was detected through changes in optical density (OD) at 540 nm. Changes in the fluorescence anisotropy of di-4-ANEPPDHQ (red) and mitochondrial swelling (gray) for isolated mitochondria in the presence of 100 μM DCA (C) and 500 μM DCA (D). Results for mitochondrial membrane order (green) and mitochondrial swelling (gray) for isolated mitochondria in the presence of 100 μM TUDCA (E) and 500 μM TUDCA (F).Control values for di-4-ANEPPDHQ fluorescence anisotropy are shown in black.
The fluorescence anisotropy (<r>) of di-4-ANEPPDHQ within MOM increased immediately after exposure of isolated mitochondria to DCA in a concentration-dependent manner. At lower concentrations of DCA (100 μM), the fluorescence anisotropy of di-4-ANEPPDHQ stabilized at <r > ∼0.30, 10 min after the start of the incubation, while for necrosis-inducing concentrations (500 μM), the fluorescence anisotropy reached <r > ∼0.32, just 2 min after the start of the incubation (Fig. 6 C, D). The fluorescence anisotropy is dependent on both rotational motions and on the fluorescence lifetime of the fluorophore, as described by Perrin’s equation (48), but although a minor fluorescence quenching of di-4-ANEPPDHQ is observed in the presence of DCA (5–10%, depending on [DCA]), this is insufficient to produce the observed changes in fluorescence anisotropy [50–62% fluorescence quenching would be necessary to induce the observed increases in <r> as dictated by Perrin’s equation (48)]. Therefore, the increase in fluorescence anisotropy of di-4-ANEPPDHQ within the MOM observed after exposure to DCA is a result of decreased anisotropic rotational motions within the membrane and reflects considerable changes in MOM structure and dynamics. A shift of di-4-ANEPPDHQ fluorescence emission spectra to shorter wavelengths is also observed after exposure to DCA, which is consistent with a less polar environment (supplementary Fig. 7).
The increase in di-4-ANEPPDHQ fluorescence anisotropy in the presence of DCA is considerably faster than the swelling of mitochondria, as detected by changes in OD at 540 nm (Fig. 6B–D), suggesting that the structural changes observed in the MOM precede activation of MPT. On the other hand, UDCA and TUDCA only induced minor increases in the fluorescence anisotropy of di-4-ANEPPDHQ (Fig. 6A, E, F) and did not lead to activation of MPT, as no swelling was detected (Fig. 6B).
For comparison purposes, protein-free liposomes mimetic of MOM were also prepared with a lipid composition of phosphatidylcholine (PC)/phosphatidylethanolamine (PE)/PI/CL/Chol (48:25:12:6:9) (49–53). Mitochondrial phospholipid composition varies little among different cells, and although the concentration of CL at the MOM is still a controversial subject (51, 53), the presence of significant concentrations of this lipid at mitochondrial contact sites has been extensively confirmed (50, 53). The fluorescence anisotropy of di-4-ANEPPDHQ within MOM mimetic liposomes is significantly higher (<r > ∼0.30) than the value obtained for di-4-ANEPPDHQ within isolated mitochondria (Fig. 7). Because the fluorescence anisotropy of di-4-ANEPPDHQ exhibited very little sensitivity to small changes in the proportion of the lipid components of liposomes mimetic of MOM (results not shown), the observed differences cannot be attributed to the uncertainty in mitochondrial membrane lipid composition and must be associated either with differences in structure (absence of mitochondrial double-membrane structure in protein-free liposomes mimetic of MOM), with the asymmetric distribution of lipids in mitochondrial membranes, or with the presence of proteins within the MOM (53).
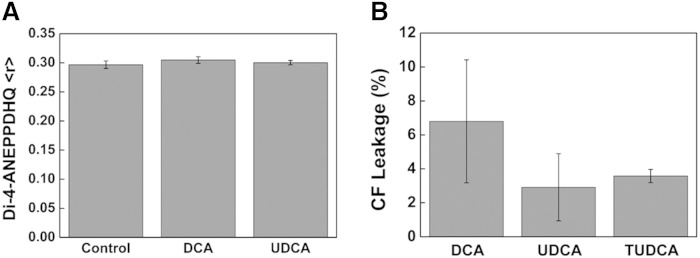
Fig. 7.
Impact of bile acids on membrane fluidity and permeability of liposomes mimicking MOM composition. Fluorescence anisotropy measurements of di-4-ANEPPDHQ within protein-free liposomes mimicking MOM lipid composition (PC/PE/PI/CL/Chol, 48:25:12:6:9) (A). Measurements in the presence of 500 μM of DCA or UDCA were carried out after a 15 min incubation with the bile acid. MOM biomimetic liposomes were loaded with 90 mM CF (under fluorescence self-quenching conditions) and exposed for 1 h at room temperature to 100 μM of DCA, UDCA, and TUDCA at room temperature (B). Results are shown for the increase in CF leakage from liposomes. The increase in CF fluorescence intensity is proportional to the fraction of CF released and can be used to evaluate liposome permeability as described in Materials and Methods.
The specific nature of the structural changes detected in the MOM after exposure to DCA are unclear because no alteration in di-4-ANEPPDHQ fluorescence anisotropy is observed in protein-free liposomes mimicking the MOM lipid composition after exposure to DCA, even at high concentrations (Fig. 7A). No changes in di-4-ANEPPDHQ fluorescence emission spectra after incubation with DCA were identified as well (results not shown). MOM mimetic liposomes were loaded with CF under fluorescence self-quenching conditions and were exposed for 1 h to 100 μM of DCA, UDCA, and TUDCA. The increase in fluorescence intensity is proportional to the fraction of CF released and can be used to estimate liposome permeability to small molecules (% CF leakage). At apoptotic concentrations of DCA, the permeability of these protein-free liposomes mimicking MOM lipid composition was only marginally increased, without significant differences between cytotoxic and cytoprotective bile acids (Fig. 7B and supplementary Fig. 8).
These results are strongly supportive of the notion that DCA, in the range of concentrations where it is physiologically active, does not increase mitochondrial membrane permeability through direct modulation of the mitochondrial lipid structure, and DCA apoptotic activity depends on features of mitochondrial membranes that are absent from protein-free mimetic liposomes, namely, the mitochondrial double-membrane structure, the asymmetric distribution of lipids, or the mitochondrial protein environment.
DISCUSSION
Cytotoxic bile acids have been shown to induce cell death through multiple pathways, depending on their concentrations (3, 4), but the corresponding mechanism of action of these molecules is still highly ambiguous and a matter of much debate, as the target of these molecules has recently been alternatively suggested to be the plasma membrane (17) or the MOM (20). Our previous studies have demonstrated that at physiologically active concentrations, cytotoxic bile acids have the potential to modulate the structure of lipid membranes, but only for certain lipidic compositions, namely, in the presence of low concentrations of Chol (14). These results confirmed that the mechanism of action of cytotoxic bile acids could be associated with modulation of membrane properties but did not offer any information on the cellular target of these molecules. In order to address this issue, we aimed here to carry out a comprehensive study on the impact of physiologically active concentrations of the cytotoxic bile acid DCA on the membrane structure of both the plasma membrane and the MOM of isolated hepatocytes. Because the detection of membrane structural changes is not by itself evidence that the impacted organelle is the site of action of DCA, we also carried out time-dependent quantitative measurements of membrane fluidity (both on live cells and isolated organelles), cell death, apoptosis, and mitochondrial swelling, which allowed for correlations to be established. Both concentrations of DCA previously shown to induce apoptosis (100 μM) and necrosis (500 μM) were tested to probe for distinctive patterns of membrane perturbation associated with each of the cell death pathways. Experiments were also always carried out in parallel with cytoprotective bile acids for comparison.
Our results clearly show that the fluidity of the plasma membrane increases after exposure to DCA or to the cytoprotective UDCA or TUDCA, as evaluated from changes in Laurdan GP values (Fig. 2E). A similar effect is also observed for HEK293T cells (Fig. 3E), which are not susceptible to DCA-induced cell death and for which a much lower bile-acid influx is expected, given the absence of the bile acid transporters. As a result of the lower intracellular concentrations of bile acids within these cells, the membrane order of the outer leaflet of the plasma membrane seems to be more sensitive to the presence of bile acids than the inner leaflet. However, plasma membrane fluidity for both cell types quickly recovered to control values after <5 h of incubation (Figs. 2F, 3F), suggesting that efficient cellular mechanisms are present to compensate for this effect. Such compensatory mechanisms were also previously observed when cytotoxic bile acids induced a much larger impact on isolated GPMVs than on the plasma membrane of living cells (17). Although we cannot totally exclude an effect of bile acids on very specific plasma membrane components, these results strongly suggest that nonspecific changes in plasma membrane biophysical properties are not the mechanism through which DCA induces apoptosis in healthy hepatocytes. These results were further supported by the detection through confocal microscopy of very low levels of bile acid fluorescent analogs in the plasma membrane of hepatocytes (Fig. 4).
For hepatocyte intracellular membranes, the average membrane fluidity also increases initially (Laurdan ΔGP decreases) after incubation with both cytoprotective and cytotoxic bile acids (Fig. 2B–D). As in the plasma membrane, membrane fluidity recovers to control values for cytoprotective bile acids, suggesting similar compensatory effects. However, only for the cytotoxic DCA, a late decrease in membrane fluidity (Laurdan ΔGP increases) is observed (Fig. 2B). This is associated with compositional changes in intracellular membranes of dead/dying cells, because they only occur after the onset of apoptosis and cell death (Figs. 1C, 2G). Again, the impact of DCA and the nontoxic bile acid TUDCA on the average intracellular membrane fluidity (before the onset of apoptosis and cell death) suggests that the overall decrease in membrane fluidity detected shortly after incubation with DCA is not responsible for the activation of cell death pathways.
Because neither changes in plasma membrane structure nor generalized changes in intracellular membrane fluidity are responsible for the physiological impact of DCA, activation of cell death must be associated with an alternative target. Confocal microscopy measurements with both bile acid fluorescent analogs studied (DCA-NBD and UDCA-NBD) showed no evidence of enrichment in specific organelles. However, mitochondria were shown here to incorporate significant levels of these molecules. Given that resistance to cytotoxic bile acids by specific cell types has been associated with both upregulation of Bcl-2 proteins (54, 55) and changes in mitochondria membrane composition (56), and that cytotoxic bile acids have been shown to induce MPT, cytochrome c release from isolated mitochondria, and changes in MOM morphology (20, 57), it is reasonable to assume that mitochondrial membranes are a likely target for these molecules.
After incubation of isolated mitochondria with DCA, both time- and concentration-dependent perturbations of MOM structure were detected, as revealed by fluorescence anisotropy measurements of di-4-ANEPPDHQ (Fig. 6). These membrane changes preceded the MPT and are likely related to the previously observed morphological changes in MOM morphology during incubation of isolated mitochondria with toxic bile acids (20). Importantly, cytoprotective bile acids were not able to alter mitochondrial membrane structure, unlike what has been observed previously for other organelles (Fig. 2). Thus, our results strongly suggest that unlike the plasma membrane, the MOM structure is specifically modified by cytotoxic bile acids. The protein and lipid makeup of these two compartments is drastically different (52, 58), which could justify the much greater affinity of bile acid analogs for the mitochondrial membranes (Figs. 4, 5). These results are consistent with a mechanism of action involving triggering of cell death through a mitochondria-dependent pathway. This would be in agreement with reports showing that changes in mitochondrial membrane properties are correlated with differential Bax activation and apoptosis (42) and import of glutathione into the mitochondria (43). Such modulation of cell death by modification of MOM structure could also help explain why cytotoxic bile acids induce the mitochondrial translocation of Bcl-2 proteins (3, 7, 59, 60). In this case, the extent of mitochondria membrane perturbation by cytotoxic bile acids could contribute to the definition of cell death pathway, as apoptotic and necrotic-inducing concentrations of DCA perturbed the MOM to different degrees (Fig. 7). Our data also show that the changes in mitochondrial membrane fluidity and permeability induced by DCA were not reproduced in protein-free liposomes with a lipidic composition mimetic of the MOM. These results indicate that the DCA apoptotic activity depends on features of mitochondrial membranes that are absent from protein-free mimetic liposomes, such as the double-membrane structure, lipid asymmetry, or the mitochondrial protein environment. It is also relevant that both cytoprotective bile acids used in this work did not induce significant nontransient changes in any of the cellular membranes studied. Therefore, their mechanism of action is likely not associated with direct perturbation of the membrane fluidity of either the plasma membrane or the mitochondria.
In this report, we aimed to clarify the current ambiguity on the possible cellular targets of cytotoxic bile acids. The application in this study of a reductionist approach relying on the use of cell cultures, isolated mitochondria, and protein-free liposomes has its limitations because, in vivo, the membranes of the different cellular organelles will be exposed to a considerably more complex mixture of bile acids, as well as to a much greater heterogeneity in both protein-bile acid and lipid-bile acid complexes. However, the results presented here strongly suggest that mitochondrial membranes are more susceptible to DCA-induced structural changes than the plasma membrane and support a model of mitochondria-dependent pathway for cell death modulation by DCA, induced by perturbation of the mitochondrial membrane environment.
We show that while both toxic (DCA) and nontoxic bile acids (UDCA, TUDCA) induce an increase in the average membrane fluidity of hepatocytes, these effects are transient and not correlated with apoptosis. Importantly, the plasma membrane is only moderately affected by both classes of bile acids, including in nonhepatic cells, which are not susceptible to apoptosis by DCA. On the other hand, MOM structure is shown to be heavily perturbed in the presence of DCA, while only marginally sensitive to the presence of nontoxic concentrations of UDCA/TUDCA. MOM perturbation by DCA also precedes the onset of MPT, suggesting a possible link between the two processes.
Supplementary Material
Footnotes
Abbreviations:
- A594-WGA
- Alexa Fluor 594 conjugate of wheat germ agglutinin
- Bax
- Bcl-2-associated X protein
- Bcl-2
- B-cell lymphoma 2
- CD
- methyl-β-cyclodextrin
- CF
- 5(6)-carboxyfluorescein
- Chol
- cholesterol
- CL
- cardiolipin [1,3-bis(sn-3′-phosphatidyl)-sn-glycerol]
- DCA
- deoxycholic acid
- di-4-ANEPPDHQ
- 1-[2-hydroxy-3-(N,N-di-methyl-N-hydroxyethyl)ammoniopropyl]-4-[β-[2-(di-n-butylamino)-6-napthyl] vinyl]pyridinium dibromide
- FLIM
- fluorescence lifetime imaging microscopy
- GP
- generalized polarization
- GPMV
- giant plasma membrane vesicle
- Laurdan
- 6-dodecanoyl-2-dimethylaminonaphthalene
- LUV
- large unilamellar vesicle
- MOM
- mitochondrial outer membrane
- MPT
- mitochondrial permeability transition
- NBD
- n-(7-nitrobenz-2-oxa-l,3-diazol-4yl)
- PDM
- product of the difference from the mean
- PI
- l-α-phosphatidylinositol
- Rho-123
- 6-amino-9-(2-methoxycarbonylphenyl)xanthen-3-ylidene]azanium
- TUDCA
- tauroursodeoxycholic acid
- UDCA
- ursodeoxycholic acid
This work was supported by Fundação para a Ciência e Tecnologia, Portugal (FCT) Project References RECI/CTM-POL/0342/2012 and PTDC/QUI -BIO/119494/2010, and by FCT Fellowships SFRH/BD/92398/2013 (T.S.), SFRH/BPD/92409/2013 (S.N.P.), and SFRH/BPD/64320/2009 (F.F.).
The online version of this article (available at http://www.jlr.org) contains a supplement.
REFERENCES
- 1.Schmucker D. L., Ohta M., Kanai S., Sato Y. K. K. 1990. Hepatic injury induced by bile salts: correlation between biochemical and morphological events. Hepatology. 12: 1216–1221. [DOI] [PubMed] [Google Scholar]
- 2.Yamazaki M., Miyake M., Sato H., Masutomi N., Tsutsui N., Adam K.-P., Alexander D. C., Lawton K. A., Milburn M. V., Ryals J. A., et al. 2013. Perturbation of bile acid homeostasis is an early pathogenesis event of drug induced liver injury in rats. Toxicol. Appl. Pharmacol. 268: 79–89. [DOI] [PubMed] [Google Scholar]
- 3.Castro R. E., Amaral J. D., Solá S., Kren B. T., Steer C. J., Rodrigues C. M. P. 2007. Differential regulation of cyclin D1 and cell death by bile acids in primary rat hepatocytes. Am. J. Physiol. Gastrointest. Liver Physiol. 293: G327–G334. [DOI] [PubMed] [Google Scholar]
- 4.Gumpricht E., Devereaux M. W., Dahl R. H., Sokol R. J. 2000. Glutathione status of isolated rat hepatocytes affects bile acid-induced cellular necrosis but not apoptosis. Toxicol. Appl. Pharmacol. 164: 102–111. [DOI] [PubMed] [Google Scholar]
- 5.Faubion W. A., Guicciardi M. E., Miyoshi H., Bronk S. F., Roberts P. J., Svingen P. A., Kaufmann S. H., Gores G. J. 1999. Toxic bile salts induce rodent hepatocyte apoptosis via direct activation of Fas. J. Clin. Invest. 103: 137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferreira D. M. S., Afonso M. B., Rodrigues P. M., Simão A. L., Pereira D. M., Borralho P. M., Rodrigues C. M. P., Castro R. E. 2014. c-Jun N-terminal kinase 1/c-Jun activation of the p53/microRNA 34a/sirtuin 1 pathway contributes to apoptosis induced by deoxycholic acid in rat liver. Mol. Cell. Biol. 34: 1100–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webster C. R. L., Johnston A. N., Anwer M. S. 2014. Protein kinase C delta protects against bile acid apoptosis by suppressing proapoptotic JNK and BIM pathways in human and rat hepatocytes. Am. J. Physiol. Gastrointest. Liver Physiol. 307: G1207–G1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodrigues C. M. P., Fan G., Wong P. Y., Kren B. T., Steer C. J. 1998. Ursodeoxycholic acid may inhibit deoxycholic acid-induced apoptosis by modulating mitochondrial transmembrane potential and reactive oxygen species production. Mol. Med. 4: 165–178. [PMC free article] [PubMed] [Google Scholar]
- 9.Amaral J. D., Castro R. E., Solá S., Steer C. J., Rodrigues C. M. P. 2007. p53 is a key molecular target of ursodeoxycholic acid in regulating apoptosis. J. Biol. Chem. 282: 34250–34259. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues C. M. P., Fan G., Ma X., Kren B. T., Steer C. J., Wong P. Y. 1998. A novel role for ursodeoxycholic acid in inhibiting apoptosis by modulating mitochondrial membrane perturbation. J. Clin. Invest. 101: 2790–2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amaral J. D., Castro R. E., Steer C. J., Rodrigues C. M. P. 2009. p53 and the regulation of hepatocyte apoptosis: implications for disease pathogenesis. Trends Mol. Med. 15: 531–541. [DOI] [PubMed] [Google Scholar]
- 12.Amaral J. D., Viana R. J. S., Ramalho R. M., Steer C. J., Rodrigues C. M. P. 2009. Bile acids: regulation of apoptosis by ursodeoxycholic acid. J. Lipid Res. 50: 1721–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodrigues C. M., Ma X., Linehan-Stieers C., Fan G., Kren B. T., Steer C. J. 1999. Ursodeoxycholic acid prevents cytochrome c release in apoptosis by inhibiting mitochondrial membrane depolarization and channel formation. Cell Death Differ. 6: 842–854. [DOI] [PubMed] [Google Scholar]
- 14.Mello-Vieira J., Sousa T., Coutinho A., Fedorov A., Lucas S. D., Moreira R., Castro R. E., Rodrigues C. M. P., Prieto M., Fernandes F. 2013. Cytotoxic bile acids, but not cytoprotective species, inhibit the ordering effect of cholesterol in model membranes at physiologically active concentrations. Biochim. Biophys. Acta. 1828: 2152–2163. [DOI] [PubMed] [Google Scholar]
- 15.Mohapatra M., Mishra A. K. 2011. Effect of submicellar concentrations of conjugated and unconjugated bile salts on the lipid bilayer membrane. Langmuir. 27: 13461–13467. [DOI] [PubMed] [Google Scholar]
- 16.Coreta-Gomes F. M., Martins P. A. T., Velázquez-Campoy A., Vaz W. L. C., Geraldes C. F. G., Moreno M. J. 2015. Interaction of bile salts with model membranes mimicking the gastrointestinal epithelium: a study by isothermal titration calorimetry. Langmuir. 31: 9097–9104. [DOI] [PubMed] [Google Scholar]
- 17.Zhou Y., Maxwell K. N., Sezgin E., Lu M., Liang H., Hancock J. F., Dial E. J., Lichtenberger L. M., Levental I. 2013. Bile acids modulate signaling by functional perturbation of plasma membrane domains. J. Biol. Chem. 288: 35660–35670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Botla R., Spivey J., Aguilar H., Bronk S., Gores G. 1995. Ursodeoxycholate (UDCA) inhibits the mitochondrial membrane permeability transition induced by glycochenodeoxycholate: a mechanism of UDCA cytoprotection. J. Pharmacol. Exp. Ther. 272: 930–938. [PubMed] [Google Scholar]
- 19.Nalapareddy P. D., Schüngel S., Hong J-Y., Manns M. P., Jaeschke H., Vogel A. 2009. The BH3-only protein bid does not mediate death-receptor-induced liver injury in obstructive cholestasis. Am. J. Pathol. 175: 1077–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulz S., Schmitt S., Wimmer R., Aichler M., Eisenhofer S., Lichtmannegger J., Eberhagen C., Artmann R., Tookos F., Walch A., et al. 2013. Progressive stages of mitochondrial destruction caused by cell toxic bile salts. Biochim. Biophys. Acta. 1828: 2121–2133. [DOI] [PubMed] [Google Scholar]
- 21.Mariash C. N., Seelig S., Schwartz H. L., Oppenheimer J. H. 1986. Rapid synergistic interaction between thyroid hormone and carbohydrate on mRNAS14 induction. J. Biol. Chem. 261: 9583–9586. [PubMed] [Google Scholar]
- 22.Castro R. E., Ferreira D. M. S., Zhang X., Borralho P. M., Sarver A. L., Zeng Y., Steer C. J., Kren B. T., Rodrigues C. M. P. 2010. Identification of microRNAs during rat liver regeneration after partial hepatectomy and modulation by ursodeoxycholic acid. Am. J. Physiol. Gastrointest. Liver Physiol. 299: G887–G897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Castro R. E., Ferreira D. M. S., Afonso M. B., Borralho P. M., Machado M. V., Cortez-Pinto H., Rodrigues C. M. P. 2013. miR-34a/SIRT1/p53 is suppressed by ursodeoxycholic acid in the rat liver and activated by disease severity in human non-alcoholic fatty liver disease. J. Hepatol. 58: 119–125. [DOI] [PubMed] [Google Scholar]
- 24.Walajtys-Rhode E., Zapatero J., Moehren G., Hoek J. B. 1992. The role of the matrix calcium level in the enhancement of mitochondrial pyruvate carboxylation by glucagon pretreatment. J. Biol. Chem. 267: 370–379. [PubMed] [Google Scholar]
- 25.Owen D. M., Rentero C., Magenau A., Abu-Siniyeh A., Gaus K. 2012. Quantitative imaging of membrane lipid order in cells and organisms. Nat. Protoc. 7: 24–35. [DOI] [PubMed] [Google Scholar]
- 26.Zimmermann T., Rietdorf J., Pepperkok R. 2003. Spectral imaging and its applications in live cell microscopy. FEBS Lett. 546: 87–92. [DOI] [PubMed] [Google Scholar]
- 27.Wu Y., Zinchuk V., Grossenbacher-Zinchuk O., Stefani E. 2012. Critical evaluation of quantitative colocalization analysis in confocal fluorescence microscopy. Interdiscip. Sci. 4: 27–37. [DOI] [PubMed] [Google Scholar]
- 28.Marquardt D. W. 1963. An algorithm for least-squares estimation of nonlinear parameters. J. Soc. Ind. Appl. Math. 11: 431–441. [Google Scholar]
- 29.Sarmento M. J., Coutinho A., Fedorov A., Prieto M., Fernandes F. 2014. Ca(2+) induces PI(4,5)P2 clusters on lipid bilayers at physiological PI(4,5)P2 and Ca(2+) concentrations. Biochim. Biophys. Acta. 1838: 822–830. [DOI] [PubMed] [Google Scholar]
- 30.McClare C. W. 1971. An accurate and convenient organic phosphorus assay. Anal. Biochem. 39: 527–530. [DOI] [PubMed] [Google Scholar]
- 31.Jin L., Millard A. C., Wuskell J. P., Dong X., Wu D., Clark H. A., Loew L. M. 2006. Characterization and application of a new optical probe for membrane lipid domains. Biophys. J. 90: 2563–2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owen D. M., Lanigan P. M. P., Dunsby C., Munro I., Grant D., Neil M. A. A., French P. M. W., Magee A. I. 2006. Fluorescence lifetime imaging provides enhanced contrast when imaging the phase-sensitive dye di-4-ANEPPDHQ in model membranes and live cells. Biophys. J. 90: L80–L82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parasassi T., Gratton E. 1995. Membrane lipid domains and dynamics as detected by Laurdan fluorescence. J. Fluoresc. 5: 59–69. [DOI] [PubMed] [Google Scholar]
- 34.Pinto S. N., Fernandes F., Fedorov A., Futerman A. H., Silva L. C., Prieto M. 2013. A combined fluorescence spectroscopy, confocal and 2-photon microscopy approach to re-evaluate the properties of sphingolipid domains. Biochim. Biophys. Acta. 1828: 2099–2110. [DOI] [PubMed] [Google Scholar]
- 35.Dawson P. A., Lan T., Rao A. 2009. Bile acid transporters. J. Lipid Res. 50: 2340–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zidovetzki R., Levitan I. 2007. Use of cyclodextrins to manipulate plasma membrane cholesterol content: evidence, misconceptions and control strategies. Biochim. Biophys. Acta. 1768: 1311–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Holzinger F., Schteingart C. D., Ton-Nu H. T., Cerrè C., Steinbach J. H., Yeh H. Z., Hofmann A. F. 1998. Transport of fluorescent bile acids by the isolated perfused rat liver: kinetics, sequestration, and mobilization. Hepatology. 28: 510–520. [DOI] [PubMed] [Google Scholar]
- 38.de Waart D. R., Häusler S., Vlaming M. L., Kunne C., Hänggi E., Gruss H. J., Oude Elferink R. P., Stieger B. 2010. Hepatic transport mechanisms of cholyl-L-lysyl-fluorescein. J Pharmacol. Exp. Ther. 334: 78–86. [DOI] [PubMed] [Google Scholar]
- 39.Bravo P., Bender V., Cassio D. 1998. Efficient in vitro vectorial transport of a fluorescent conjugated bile acid analogue by polarized hepatic hybrid WIF-B and WIF-B9 cells. Hepatology. 27: 576–583. [DOI] [PubMed] [Google Scholar]
- 40.Kitamura T., Gatmaitan Z., Arias I. M. 1990. Serial quantitative image analysis and confocal microscopy of hepatic uptake, intracellular distribution and biliary secretion of a fluorescent bile acid analog in rat hepatocyte doublets. Hepatology. 12: 1358–1364. [DOI] [PubMed] [Google Scholar]
- 41.Kim M., Cooper D. D., Hayes S. F., Spangrude G. J. 1998. Rhodamine-123 staining in hematopoietic stem cells of young mice indicates mitochondrial activation rather than dye efflux. Blood. 91: 4106–4117. [PubMed] [Google Scholar]
- 42.Lucken-Ardjomande S., Montessuit S., Martinou J-C. 2008. Bax activation and stress-induced apoptosis delayed by the accumulation of cholesterol in mitochondrial membranes. Cell Death Differ. 15: 484–493. [DOI] [PubMed] [Google Scholar]
- 43.Marí M., Caballero F., Colell A., Morales A., Caballeria J., Fernandez A., Enrich C., Fernandez-Checa J. C., García-Ruiz C. 2006. Mitochondrial free cholesterol loading sensitizes to TNF- and Fas-mediated steatohepatitis. Cell Metab. 4: 185–198. [DOI] [PubMed] [Google Scholar]
- 44.Solá S., Brito M. A., Brites D., Moura J. J. G., Rodrigues C. M. P. 2002. Membrane structural changes support the involvement of mitochondria in the bile salt-induced apoptosis of rat hepatocytes. Clin. Sci. (Lond.). 103: 475–485. [DOI] [PubMed] [Google Scholar]
- 45.Benz C., Angermüller S., Otto G., Sauer P., Stremmel W., Stiehl A. 2000. Effect of tauroursodeoxycholic acid on bile acid-induced apoptosis in primary human hepatocytes. Eur. J. Clin. Invest. 30: 203–209. [DOI] [PubMed] [Google Scholar]
- 46.Rolo A. P., Oliveira P. J., Moreno A. J., Palmeira C. M. 2000. Bile acids affect liver mitochondrial bioenergetics: possible relevance for cholestasis therapy. Toxicol. Sci. 57: 177–185. [DOI] [PubMed] [Google Scholar]
- 47.Benz R. 1994. Permeation of hydrophilic solutes through mitochondrial outer membranes: review on mitochondrial porins. Biochim. Biophys. Acta . 1197: 167–196. [DOI] [PubMed] [Google Scholar]
- 48.Lakowicz J. R. 2006. Principles of Fluorescence Spectroscopy. Springer, New York. [Google Scholar]
- 49.Lucken-Ardjomande S., Montessuit S., Martinou J-C. 2008. Contributions to Bax insertion and oligomerization of lipids of the mitochondrial outer membrane. Cell Death Differ. 15: 929–937. [DOI] [PubMed] [Google Scholar]
- 50.Daum G., Graz T. U. 1985. Lipids of mitochondria. Biochim. Biophys. Acta. 822: 1–42. [DOI] [PubMed] [Google Scholar]
- 51.Gebert N., Joshi A. S., Kutik S., Becker T., McKenzie M., Guan X. L., Mooga V. P., Stroud D. A., Kulkarni G., Wenk M. R., et al. 2009. Mitochondrial cardiolipin involved in outer-membrane protein biogenesis: implications for Barth syndrome. Curr. Biol. 19: 2133–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Osman C., Voelker D. R., Langer T. 2011. Making heads or tails of phospholipids in mitochondria. J. Cell Biol. 192: 7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ardail D., Privat J-P., Egret-Charlier M., Levrat C., Lerme F., Louisot P. 1990. Mitochondrial contact sites. J. Biol. Chem. 265: 18797–18802. [PubMed] [Google Scholar]
- 54.Barrasa J. I., Santiago-Gómez A., Olmo N., Lizarbe M. A., Turnay J. 2012. Resistance to butyrate impairs bile acid-induced apoptosis in human colon adenocarcinoma cells via up-regulation of Bcl-2 and inactivation of Bax. Biochim. Biophys. Acta. 1823: 2201–2209. [DOI] [PubMed] [Google Scholar]
- 55.Powell A. A., LaRue J. M., Batta A. K., Martinez J. D. 2001. Bile acid hydrophobicity is correlated with induction of apoptosis and/or growth arrest in HCT116 cells. Biochem. J. 356: 481–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gumpricht E., Devereaux M. W., Dahl R., Soden J. S., Sparagna G. C., Leonard S. W., Traber M. G., Sokol R. J. 2008. Resistance of young rat hepatic mitochondria to bile acid- induced permeability transition: potential role of alpha-tocopherol. Pediatr. Res. 64: 498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rolo A. P., Oliveira P. J., Moreno A. J., Palmeira C. M. 2003. Chenodeoxycholate induction of mitochondrial permeability transition pore is associated with increased membrane fluidity and cytochrome c release: protective role of carvedilol. Mitochondrion. 2: 305–311. [DOI] [PubMed] [Google Scholar]
- 58.van Meer G., Voelker D. R., Feigenson G. W. 2008. Membrane lipids: where they are and how they behave. Nat. Rev. Mol. Cell Biol. 9: 112–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Webster C. R. L., Usechak P., Anwer M. S. 2002. cAMP inhibits bile acid-induced apoptosis by blocking caspase activation and cytochrome c release. Am. J. Physiol. Gastrointest. Liver Physiol. 283: G727–G738. [DOI] [PubMed] [Google Scholar]
- 60.Denk G. U., Kleiss C. P., Wimmer R., Vennegeerts T., Reiter F. P., Schulz S., Zischka H., Rust C. 2012. Tauro-beta-muricholic acid restricts bile acid-induced hepatocellular apoptosis by preserving the mitochondrial membrane potential. Biochem. Biophys. Res. Commun. 424: 758–764. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.