Abstract
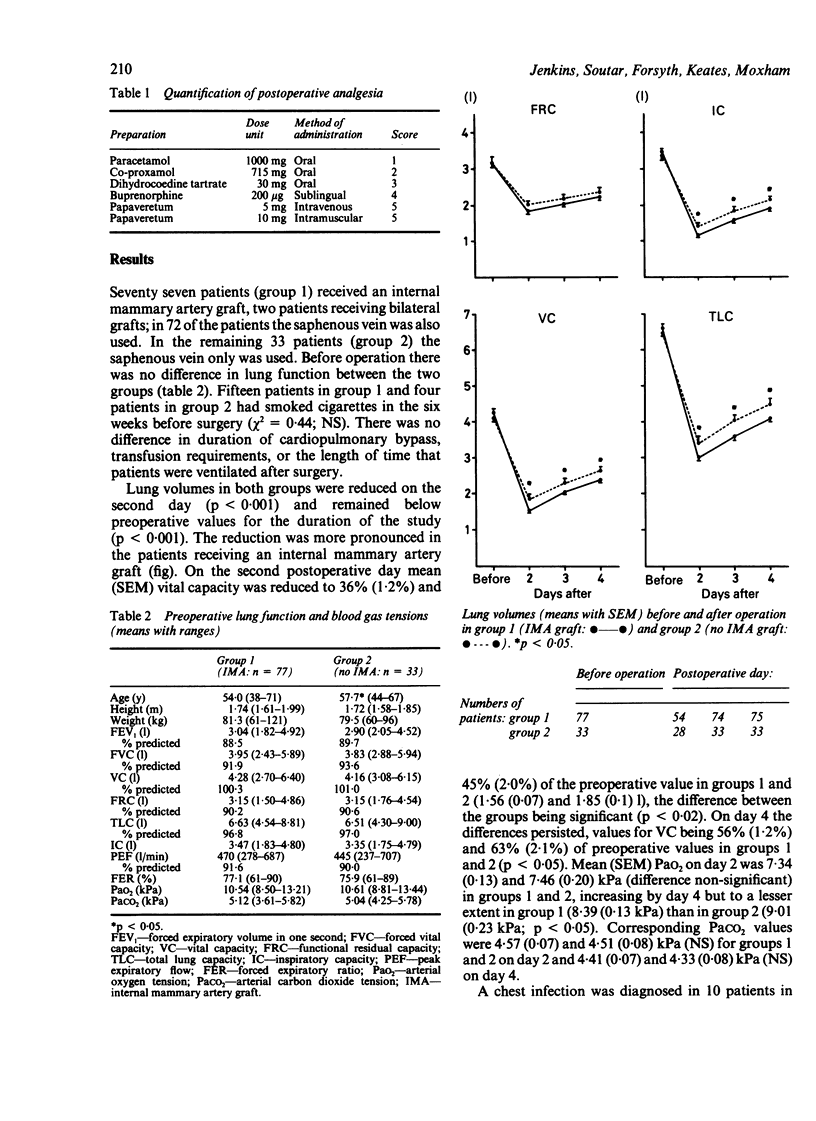
Lung volumes and arterial blood gas tensions in patients undergoing coronary artery surgery were compared in 77 patients given an internal mammary artery graft (group 1) and 33 patients given a saphenous vein graft only (group 2). Patients in both groups developed a severe restrictive ventilatory defect after surgery, more pronounced in those receiving an internal mammary artery graft. Mean (SEM) vital capacity in groups 1 and 2 was reduced to 36% (1.2%) and 45% (2.0%) of preoperative values on the second postoperative day (1.56 and 1.85 1 respectively), with some recovery by day 4 to 56% (1.2%) and 63% (2.1%) of preoperative values. The mean (SEM) arterial oxygen tension was 7.34 (0.13) kPa for group 1 and 7.46 (0.20) kPa for group 2 on day 2, rising to 8.39 (0.13) and 9.01 (0.23) kPa on day 4. Analgesic requirements were greater in the group receiving an internal mammary artery graft. Possible explanations for the differences between the effects of the two grafts include the higher frequency of pleurotomy, the placing of pleural drains, and additional surgical trauma when internal mammary artery grafts are used.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BLAIR E., HICKAM J. B. The effect of change in body position on lung volume and intrapulmonary gas mixing in normal subjects. J Clin Invest. 1955 Mar;34(3):383–389. doi: 10.1172/JCI103086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess G. E., 3rd, Cooper J. R., Jr, Marino R. J., Peuler M. J., Mills N. L., Ochsner J. L. Pulmonary effect of pleurotomy during and after coronary artery bypass with internal mammary artery versus saphenous vein grafts. J Thorac Cardiovasc Surg. 1978 Aug;76(2):230–234. [PubMed] [Google Scholar]
- Jenkins S. C., Barnes N. C., Moxham J. Evaluation of a hand-held spirometer, the Respiradyne, for the measurement of forced expiratory volume in the first second (FEV1), forced vital capacity (FVC) and peak expiratory flow rate (PEFR). Br J Dis Chest. 1988 Jan;82(1):70–75. doi: 10.1016/0007-0971(88)90010-1. [DOI] [PubMed] [Google Scholar]
- Loop F. D., Lytle B. W., Cosgrove D. M., Stewart R. W., Goormastic M., Williams G. W., Golding L. A., Gill C. C., Taylor P. C., Sheldon W. C. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986 Jan 2;314(1):1–6. doi: 10.1056/NEJM198601023140101. [DOI] [PubMed] [Google Scholar]
- Spencer F. C. The internal mammary artery: the ideal coronary bypass graft? N Engl J Med. 1986 Jan 2;314(1):50–51. doi: 10.1056/NEJM198601023140109. [DOI] [PubMed] [Google Scholar]
- Spiro S. G., Dowdeswell I. R. Arterialized ear lobe blood samples for blood gas tensions. Br J Dis Chest. 1976 Oct;70(4):263–268. doi: 10.1016/0007-0971(76)90042-5. [DOI] [PubMed] [Google Scholar]


