Summary
The generation of insulin-producing pancreatic β cells from stem cells in vitro would provide an unprecedented cell source for drug discovery and cell transplantation therapy in diabetes. However, insulin-producing cells previously generated from human pluripotent stem cells (hPSC) lack many functional characteristics of bona fide β cells. Here we report a scalable differentiation protocol that can generate hundreds of millions of glucose-responsive β cells from hPSC in vitro. These stem cell derived β cells (SC-β) express markers found in mature β cells, flux Ca2+ in response to glucose, package insulin into secretory granules and secrete quantities of insulin comparable to adult β cells in response to multiple sequential glucose challenges in vitro. Furthermore, these cells secrete human insulin into the serum of mice shortly after transplantation in a glucose-regulated manner, and transplantation of these cells ameliorates hyperglycemia in diabetic mice.
Introduction
The discovery of human pluripotent stem cells (hPSC) opened the possibility of generating replacement cells and tissues in the laboratory that could be used for disease treatment and drug screening. Recent research has moved the stem cell field closer to that goal through development of strategies to generate cells that would otherwise be difficult to obtain, like neurons or cardiomyocytes (Kriks et al., 2011; Shiba et al., 2012; Son et al., 2011). These cells have also been transplanted into animal models, in some cases with a beneficial effect like suppression of arrhythmias with stem cell-derived cardiomyocytes (Shiba et al., 2012), restoration of locomotion after spinal injury with oligodendrocyte progenitors (Keirstead et al., 2005), or improved vision after transplantation of retinal epithelial cells into rodent models of blindness (Lu et al., 2009).
One of the rapidly growing diseases that may be treatable by stem cell derived tissues is diabetes, affecting more than 300 million people worldwide according to the International Diabetes Federation. Type 1 diabetes results from autoimmune destruction of β cells in the pancreatic islet whereas the more common type 2 diabetes results from peripheral tissue insulin resistance and β cell dysfunction. Diabetic patients, particularly those suffering from type 1 diabetes, could potentially be cured through transplantation of new β cells. Patients transplanted with cadaveric human islets can be made insulin independent for five years or longer via this strategy, but this approach is limited because of the scarcity and quality of donor islets (Bellin et al., 2012). The generation of an unlimited supply of human β cells from stem cells could extend this therapy to millions of new patients and be an important test case for translating stem cell biology into the clinic. This is because only a single cell type, the β cell, likely needs to be generated and the mode of delivery is understood: transplantation to a vascularized location within the body with immunoprotection.
Pharmaceutical screening to identify new drugs that improve β cell function, survival, or proliferation is also hindered by limited supplies of islets and high variability due to differential causes of death, donor genetic background, and other factors in their isolation. A consistent, uniform supply of stem cell-derived β cells would provide a unique and valuable drug discovery platform for diabetes. Additionally, genetically diverse stem cell-derived β cells could be used for disease modeling in vitro or in vivo.
Studies on pancreatic development in model organisms (Gamer and Wright, 1995; Henry, 1998; Ninomiay et al., 1999; Apelqvist, A., 1999; Kim et al., 2000; Hebrok et al., 2000; Murtaugh et al., 2003;) identified genes and signals important for the pancreatic lineage, and these have been effectively used to form cells in the β cell lineage in vitro from hPSC. Definitive endoderm and subsequent pancreatic progenitors can now be differentiated with high efficiencies (Kroon et al., 2008; D’Amour et al., 2006; D’Amour et al., 2005; Rezania et al., 2012). These cells can differentiate into functional β cells within three to four months following transplantation into rodents (Kroon et al., 2008; Rezania et al., 2012), indicating that some cells in the preparation contain the developmental potential to develop into β cells if provided enough time and appropriate cues. Unfortunately, the months-long process the cells undergo in vivo is not understood, and it is unclear if this process of in vivo differentiation would also occur in human patients. Attempts to-date at generating insulin-producing (INS+) cells from human pancreatic progenitors in vitro have generated cells with immature or abnormal phenotypes. These cells either fail to perform glucose stimulated insulin secretion in vitro, fail to express appropriate β cell markers such as NKX6-1 or PDX1, abnormally co-express other hormones like glucagon (GCG), fail to function after transplantation in vivo, or display a combination of these abnormal features (D’Amour et al., 2006; Cheng et al., 2012; Hvratin et al., 2014; Narayanan et al., 2013; Xie et al., 2013; Nostro et al., 2011).
Herein we report the discovery of a strategy for large-scale production of functional human β cells from hPSC in vitro. By using sequential modulation of multiple signaling pathways in a 3-dimensional cell culture system, without any transgenes or genetic modification, we generate glucose-responsive, monohormonal insulin-producing cells that show key features of a bona fide β cell including co-expression of key β cell markers and β cell ultrastructure. Furthermore, these cells mimic the function of human islets both in vitro and in vivo. Finally we demonstrate the potential utility of these cells for in vivo transplantation therapy for diabetes.
Results
Generation of Glucose-Sensing Insulin-Secreting β Cells In Vitro
Our strategy to generate functional β cells from hPSC in vitro is outlined in Figure 1A. To produce large numbers, we used a scalable suspension-based culture system that can generate >108 hPSCs and later differentiated cell types (modified from Schulz et al., 2012). Clusters of cells (approximately 100–200 μm in diameter, each cluster containing several hundred cells) from a human embryonic stem cell (hESC) line (HUES8) or 2 human induced pluripotent stem cell (hiPSC) lines (hiPSC-1 and hiPSC-2), were induced into definitive endoderm (>95% SOX17+ cells, DE cells in Figure 1A) and subsequently early pancreatic progenitors (>85% PDX1+ cells, PP1 cells in Figure 1A).
Figure 1. SC-β cells generated in vitro secrete insulin in response to multiple sequential high glucose challenges like primary human β cells.

(A) Schematic of directed differentiation from hPSC into INS+ cells via new or previously published control differentiations.
(B–D) Representative ELISA measurements of secreted human insulin from HUES8 SC-β cells (B), PH cells (C), and primary β (1°β) cells (D) challenged sequentially with 2, 20, 2, 20, 2, and 20mM glucose, with a 30-min incubation for each concentration (see Methods). After sequential low/high glucose challenges, cells were depolarized with 30mM KCl.
(E–G) Box and whisker plots of secreted human insulin from different biological batches of HUES8 (open circles) and hiPSC SC-β (black circles) cells (E; n=12), biological batches of PH cells (F; n=5), and primary β cells (G; n=4). Each circle is the average value for all sequential challenges with 2mM or 20mM glucose in a batch. Insulin secretion at 20mM ranged 0.23–2.7 μIU/103 cells for SC-β cells and 1.5–4.5 μIU/103 cells for human islets, and the stimulation index ranged 0.4–4.1 for SC-β cells and 0.6–4.8 for primary adult. The thick horizontal line indicates the median.
See also Figures S1 and S2A and Table S1.
* p<0.05 when comparing insulin secretion at 20mM vs. 2mM with paired t-test
Act A=Activin A; CHIR=CHIR99021, a GSK3α/β inhibitor; KGF= keratinocyte growth factor or FGF family member 7; RA=Retinoic Acid; SANT1=sonic hedgehog pathway antagonist; LDN=LDN193189, a BMP type 1 receptor inhibitor; PdbU=Phorbol 12,13-dibutyrate, a protein kinase C activator; Alk5i=Alk5 receptor inhibitor II; T3=triiodothyronine, a thyroid hormone; XXI=γ-secretase inhibitor; Betacellulin=EGF family member
Transplantation of pancreatic progenitors expressing PDX1+/NKX6-1+ (PP2 in Figure 1A) into mice gives rise to functional β cells in vivo after 3–4 months (Kroon et al., 2008; Rezania et al., 2012). And previous studies had shown that these PDX1+/NKX6-1+ pancreatic progenitors (PP2) could be further differentiated in vitro into some INS+ cells along with INS+/GCG+ or INS+/SST+ polyhormonal (PH) cells (Nostro et al., 2011; Rezania et al., 2012; Thowfeequ et al., 2007; Aguayo-Mazzucato et al., 2013; D’Amour et al., 2006; Hrvatin et al., 2014). We use the nomenclature PH (polyhormonal, Figure 1A) to refer to this cell population of in vitro differentiated hPSCs. Transcriptional analysis of in vitro differentiated PH cells showed that these cells resemble human fetal and not adult β cells (Hrvatin et al., 2014). Since these PH cells do not show glucose stimulated insulin secretion (GSIS) nor other key properties of bona fide β cells, we returned to the earlier pancreatic progenitor step (PP2) to investigate ways to make NKX6-1+/C-peptide+ (EN cells in Figure 1A) and functional β cells (SC-β cells in Figure 1A).
We first extended the time in culture with the FGF family member KGF, hedgehog inhibitor SANT1, and a low concentration of retinoic acid to generate high levels of NKX6-1+/PDX1+ co-expressing pancreatic progenitor clusters (>55% NKX6-1+/PDX1+ cells, PP2 cells in Figure 1A.) These PP2 cells were the starting point to make differentiated cells that would respond to glucose and mimic natural β cells. Systematic testing of the concentration and exposure time of numerous factors (small molecule agonists and antagonists and assorted growth factors) on pancreatic progenitors (PP2 cells in Figure 1A) led to the development of a new differentiation protocol. This protocol takes 4–5 wk and involves a unique combination of sequential culture steps using factors that affect signaling in numerous pathways, including signaling by wnt, activin, hedgehog, EGF, TGFβ, thyroid hormone, and retinoic acid, as well as γ-secretase inhibition (see Experimental Procedures). In all, we tested over 150 combinations involving over 70 compounds, many of which had been described in the literature as playing a role in pancreatic biology. Most factors and combinations had little appreciable effect on cell function and gene expression, but we were able to develop a protocol using 11 different factors that provided a significant improvement in function and β cell-like gene expression (Table S1).
A key functional feature of a β cell is its ability to repeatedly perform glucose stimulated insulin secretion (GSIS). Nearly all existing directed differentiation protocols generate insulin-expressing cells from hPSC (see PH in Figure 1A) that are defective in GSIS in vitro; these cells fail to respond to even a single glucose challenge. In contrast, the SC-β cells generated from both hESC and hiPSC cells with the new protocol respond to multiple sequential high glucose challenges and depolarization with KCl (Figures 1B, S1, and S2A). This data contrasts with the response of PH cells (Figures 1C), which secrete very low amounts of insulin and are not glucose responsive. SC-β cell clusters and primary adult (cadaveric) islets show a similar response to sequential glucose challenges (compare Figures 1B and D).
Twelve independent differentiation batches of SC-β cells (8 hESC and 4 hiPSC) were tested with three sequential high glucose challenges (3–4 replicates of each) and compared to five batches of PH cell clusters and four sets of cadaveric islets (Figure 1E–G). Because the SC-β cells outperformed PH cells, we compared SC-β cell clusters to primary islet cells. The stimulation index, as calculated by the ratio of insulin secreted in high glucose (20mM) to low glucose (2mM), was similar for SC-β cells and primary adult islets, 2.2±0.3 and 2.1±0.9, respectively.
Some batch-to-batch and donor-to-donor variation is observed for both primary adult β cells and SC-β cells. This variation is not unexpected of islets from cadavers nor for cells taken through a 35-d protocol involving 5 basal media and 11 combinatorially added factors (Figure 1E and G). Some batches of SC-β cells and primary human islets fail to respond to individual glucose challenges (see Figure S1A and C). But overall, SC-β cell clusters and primary islets responded to high glucose challenges at a similar frequency: 75±8% and 72±17%, respectively.
The amount of insulin secreted per cell in response to 20mM glucose by SC-β cells was similar to that secreted by primary adult β cells, averaging 1.6±0.2 and 3.6±0.7 μIU/103 cells, respectively. Notably, some SC-β cell batches secreted as much insulin as cadaveric islets (see Figures 1E and G). Total insulin content per cell was 240±50 μIU/103 cell for SC-β clusters (2 batches) and 200±40 μIU/103 for primary islets (1 batch). The proinsulin to insulin ratio was 0.030±0.001 and 0.029±0.006 for SC-β and primary adult β cells, respectively. Taken together, these data highlight the difference between SC-β and PH cell clusters and suggest that the in vitro function of SC-β cells is similar to their bona fide adult β cell counterparts.
Calcium flux in SC-β cells
We sought to further confirm the in vitro function of SC-β cells by measuring changes in intracellular Ca2+. β cells sense changing glucose levels through calcium signaling; increasing glucose levels leads to membrane depolarization causing an influx of calcium ions which triggers insulin exocytosis (Mohammed et al., 2009). Calcium influx depends on glucose transport and metabolic enzymes as well as functioning potassium ion channels (Rutter and Hodson, 2013). We monitored calcium influx in cell clusters stained with Fluo-4 AM, a cell permeable fluorescent calcium indicator dye, in real-time using fluorescent microscopy (Figure 2A). This method allowed us to analyze calcium flux at both the population and single cell level. The population analysis shows that cells in both SC-β cell clusters and primary adult islets respond to sequential glucose challenges by repeatedly increasing intracellular Ca2+ in a similar manner, consistent with normal glucose responsiveness. In contrast, PH cell clusters displayed an abnormal calcium response, (Figure 2B). Single cell analysis reveals that most individual cells in SC-β cell clusters and primary adult islets respond to 2–3 sequential glucose challenges by fluxing calcium, whereas most cells from PH cell clusters do not (Figure 2C–E). These data show that both the entire population as well as individual cells within the SC-β cell clusters flux calcium similarly to primary human islet cells and further support the conclusion that these SC-β cells function in vitro.
Figure 2. SC-β cells flux cytosolic Ca2+ in response to multiple sequential high glucose challenges like primary human β cells.

(A) Schematic of population level and single cell level detection of cytosolic Ca2+ using Fluo-4 AM staining. Population level measurements were taken on individual whole clusters (marked by large red circle in the schematic), and individual cells within intact clusters (marked by small red circles) were analyzed for single cell analysis.
(B) Representative population measurements of dynamic normalized Fluo-4 fluorescence intensity for HUES8 SC-β cells, primary β cells, and PH cells challenged sequentially with 2, 20, 2, 20, 2, and 20mM glucose and 30mM KCl. The x-axis represents time (in s).
(C) Fluorescence images of Fluo-4 AM staining used in single cell analysis.
(D) Representative images showing single cells that responded to 3 (yellow), 2 (orange), 1 (blue), and 0 (red) glucose challenges.
(E) Quantification of the frequency of SC-β cells (n=156), primary β cells (n=114), and PH cells (n=138) that responded to 20mM glucose.
Scale bar = 100 μm
Stem Cell-Derived β Cells Resemble Primary Human β Cells
The results in Figures 1 and 2 show that SC-β cells display the physiological function in vitro of secreting insulin in response to glucose. We next analyzed protein expression, RNA expression, and ultrastructure of SC-β cells. As with many previously reported hPSC-derived insulin-producing cells, our PH protocol C-peptide+ cells fail to co-express the β cell transcription factor NKX6-1. Conversely, SC-β cells, like islet β cells, stained positive for cytoplasmic C-peptide and the nuclear protein NKX6-1 (Figures 3A and S2B). SC-β cells stain positive for both insulin and C-peptide, a stoichiometric byproduct of proinsulin processing, indicating that the insulin produced comes from cell-endogenous insulin synthesis (data not shown).
Figure 3. SC-β cells express human β cell markers at protein and gene expression level.

(A) Representative immunohistochemistry (IHC) of HUES8 SC-β cells, primary β cells, and PH cells stained for C-peptide (green) and NKX6-1 (red).
(B) Representative IHC of cells stained for C-peptide (green) and PDX1 (red).
(C) Representative IHC of cells stained for C-peptide (green) and glucagon (red) with the corresponding DAPI stain (blue).
Enlarged insets in A, B and C shows staining for transcription factors (NKX6-1 and PDX1) is nuclear and cytoplasmic for C-peptide, except for the PH cells.
(D) Representative flow cytometry dot plots and population percentages of cells stained for C-peptide and NKX6-1. AU = arbitrary units.
(E) Hierarchal clustering based on all genes measured by transcriptional microarray of undifferentiated HUES8, PH cells, fetal β cells, and adult primary β cells sorted for INS (data from Hrvatin et al. 2014), and SC-β cells sorted for INS and NKX6-1.
(F) Heat map of the 100 genes with the most variance across all samples.
All images were taken with a Zeiss LSM 710 confocal microscope.
See also Figures S2B–C, S3, and S4.
CP=C-peptide, SST=somatostatin, GCG=glucagon
Scale bar=100 μm
Nuclear expression of the transcription factor PDX1 is characteristic of human β cells and most PH cells do not co-express PDX1 in C-peptide+ cells (Figure 3B). Both cadaveric islet β cells and SC-β cells co-express this key protein in C-peptide+ cells (Figures 3B and S2C).
Others have noted previously (Bruin et al., 2014; Hrvatin et al., 2014) that most protocols for pancreatic differentiation generate many cells that co-express glucagon and insulin/C-peptide+, and we observed polyhormonal cells in the control PH differentiations. In contrast, the majority of C-peptide+ cells in SC-β differentiations are monohormonal by IHC (Figures 3C and S2D) and flow cytometry (Figure S3). We also observed a minor population of monohormonal SST+ δ cells and GCG+ α cells (Figures 3C, S2D, and S3). There are also a few polyhormonal cells—on average, 7.7±0.7% of C-peptide+ cells co-express glucagon and 4.7±0.1% co-express somatostatin (Figure S3).
The most parsimonious explanation is that the SC-β cells can be found within the NKX6-1+/C-peptide+ monohormonal population. Flow cytometry reveals that the new protocol produces an average of 33±2% (n=12) NKX6-1+/C-peptide+ cells, similar to the 26±3% (n=3) average observed in cadaveric islets (Figures 3D and S2E). The remainder of cells in the SC-β clusters are either endocrine cells (α or δ cells that express the hormones GCG or SST) or PDX1+ pancreatic progenitors that have not differentiated into endocrine cells. We did not observe any residual cells expressing pluripotency markers such as OCT4. The non-β cells within a human islet differ from SC-β cell clusters, having higher proportions of α and δ cells.
The improved protein expression of several key β cell markers indicates that the transcriptional network of SC-β cells better matches that of human islet β cells. Recent work had demonstrated that INS+ PH cells, generated by previous protocols, do not resemble adult islet INS+ β cells (Hrvatin et al., 2014; Xie et al., 2013). Microarray analysis of sorted INS+ cells generated with previous protocols showed that they cluster with fetal β cells rather than functional adult human β cells.
To compare SC-β cells to adult human islets, we sorted out INS+/NKX6-1+ cells from SC-β cell differentiations and performed global gene expression analysis. The SC-β cells clustered with adult β cells, unlike fetal β cells or INS+ PH cells (Hrvatin et al., 2014) (Figure 3E–F). Furthermore, expression of many canonical β cell genes, such as PDX1, MNX1, and SLC30A8 (ZNT8), were more similar between SC-β cells and adult β cells than PH cells while others, such as KLF9, PCSK1, and PCSK2, are still differentially expressed (Figure S4). We conclude that SC-β cells made ex vivo are most similar, but not completely identical, to cadaveric β cells by transcriptional analysis.
SC-β cell ultrastructure
In light of the observation that SC-β cells secrete insulin in a physiological manner in vitro, we hypothesized that SC-β cells might also package insulin protein into secretory granules as do primary β cells. β cells package insulin into secretory granules that initially appear as pale grey cores surrounded by a small electron-lucent area or light halo and these condense into granules with dark polygonal crystalline cores surrounded by a light halo (Deconinck et al., 1971; Like et al., 1972). Previous studies of INS+ cells showed abnormal granules that resemble alpha-like granules with round cores surrounded by a dark grey halo (PH cells, D’Amour et al., 2006; Deconinck et al., 1971; Like et al., 1972) and/or abnormal granules of indistinct hormonal character. We recapitulated these results with our control protocol, producing INS+ cells that had abnormal and alpha-like granules and few, if any, β cell granules (Figures 4A–B). In contrast, our new differentiation strategy generates SC-β cells that package and crystallize insulin protein into granules that are structurally similar to primary β cell insulin granules. Both developing insulin granules and mature, crystallized insulin granules are observed in SC-β cells and primary human β cells. SC-β cells and primary β cells averaged 66±11 and 77±8 insulin granules per cell, respectively (Figure 4C). Immunogold labeling with particles against insulin and glucagon showed that granules in the PH cells contained both insulin and glucagon protein, whereas primary human β cell and SC-β cell granules contained only insulin (Figure 4D). Thus, this key ultrastructural feature of adult human β cells is mirrored in SC-β cells.
Figure 4. SC-β cell insulin granules are structurally similar to primary human β cell granules.

(A) Electron microscopy images of granules within sectioned cells, highlighting representative crystallized insulin granules (red), early insulin granules (yellow), and mixed endocrine granules (blue) found in HUES8 SC-β cells, primary β cells, and PH cells. Scale bar=500 nm.
(B) Higher magnification images of granules highlighted in (A). Scale bar=500 nm.
(C) Box and whisker plot of the number of insulin and early insulin granules per cell. The cross indicates mean and the thick horizontal line indicates median. n=24 cells from 2 batches of differentiation for HUES8 SC-β cells, and n=30 cells from 2 donors of primary human β cells. PH cells are not shown because no mature insulin or early insulin granules were observed.
(D) Electron microscopy images of cells labeled with immunogold staining showing granules that contain insulin (smaller 5 nm black dots) and/or glucagon (larger 15 nm black dots). Representative immunogold particles are highlighted with red arrows (insulin) and blue arrows (glucagon). Scale bar=100 nm.
Stem Cell-Derived β Cells Function in vivo After Transplantation
To test their capacity to function in vivo, we transplanted SC-β cells under the kidney capsule of immunocompromised mice (Figure 5 and Tables S2 and S3). When primary human islets (500 ieq, or islet equivalents) are transplanted, human insulin is detected in the serum of glucose challenged mice within 2 wk (Figure 5A). Conversely, when 5 million pancreatic progenitor cells are transplanted into mice no insulin is detected at 2 wk post-transplant (data not shown) (Kroon et al., 2008; Schulz et al., 2012; Rezania et al., 2012). A portion of the cells in this pancreatic progenitor population will differentiate further and secrete insulin, but only after a 3–4 month long ill-understood maturation phase in vivo.
Figure 5. Transplanted SC-β cells function rapidly in vivo.
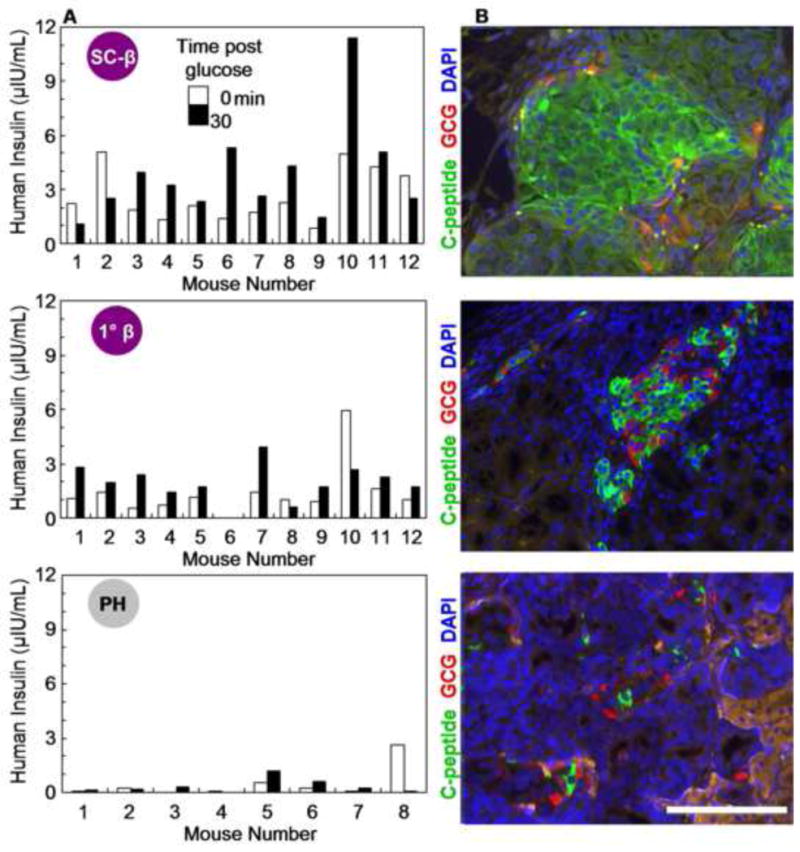
(A) ELISA measurements of human insulin from the serum of individual mice transplanted with comparable numbers of HUES8 SC-β cells (5×106 cells), primary human β cells (500–1000 IEQ), or PH cells (5×106 cells). Measurements were taken before (white bars) and 30 min after (black bars) a glucose injection of mice 2 wk post-transplantation.
(B) Representative IHC of cells 2 wk post-transplantation in (A) stained with C-peptide (green) and glucagon (GCG; red) to confirm presence of graft.
All images were taken with a Olympus IX51 microscope.
See also Figure S5 and Tables S2 and S3.
Scale bar=100 μm
We tested whether insulin is detectable in serum of animals transplanted with 5 million SC-β cells sooner than 3–4 months. After a brief surgical recovery period (2 wk), mice transplanted with SC-β cells were injected with glucose and serum was collected 30 min later. ELISA measurement of human insulin in the serum revealed that SC-β cells from both hESC and hiPSC secrete insulin into the host bloodstream within 2 wk, the earliest post-transplantation time point tested (Figures 5A). As a control, we also transplanted the same number of PH cells and pancreatic progenitors, neither of which secreted significant levels of insulin in vivo within 2 wk, as has been previously published (Kroon et al., 2008) (data not shown and Figure 5A). To test whether the SC-β cells secrete insulin in response to glucose, we measured human insulin in the bloodstream of a subset of mice both before (0 min) and after (30 min) an acute glucose challenge. 73% of SC-β cell transplanted mice (27/37 animals) showed increased human insulin in the bloodstream after a glucose challenge, 2 wk post-transplant (Figure 5A and Tables S2 and S3). By comparison, 75% of mice transplanted with human islets (9/12 animals) showed increased human insulin secretion after the glucose challenge. This increase in human insulin with transplanted SC-β cells is statistically significant (p=0.0008). As another measure of in vivo GSIS, the average ratio of insulin secreted after the glucose challenge compared to before the it was 1.9 ± 0.3 for islet transplants and 1.7 ± 0.2 for SC-β cell transplants. These in vivo stimulation indices ranged from 0.4 – 4.3 for islet transplants and from 0.5 – 3.8 for SC-β cell transplants (Tables S2 and S3).
After 2 wk post transplantation, animals were sacrificed and the engrafted kidneys were removed for histology. IHC showed that both SC-β cell and human islet grafts contain C-peptide+ cells adjacent to the mouse kidney (Figures 5B and S5). Analysis of C-peptide and glucagon staining further revealed that the SC-β cells remained monohormonal after transplantation (Figures 5B and S5). A minor population of GCG+ cells, which was observed before transplantation (Figures 3C, S2D, and S3), was also observed in the grafts (Figures 5B and S5).
Utility of Stem Cell-Derived β Cells for Treating Diabetes
A major challenge for the stem cell field has been to generate differentiated cells that mimic their normal, in vivo counterparts. We examined how useful SC-β cells would be as a cell therapy in a diabetic animal model. One useful diabetes model is the Akita mouse (Yoshioka et al., 1997), which has a mutation in the insulin gene, leading to protein misfolding, irreversible β cell failure, and progressively severe hyperglycemia. Immunodeficient NOD-Rag1null IL2rgnull Ins2Akita (NRG-Akita) mice can be restored to normoglycemia via mouse or human islet transplantation (Brehm et al., 2010).
We tested whether SC-β cells could also function to control diabetic hyperglycemia. Transplantation of SC-β cells, but not PH cells, into the kidney capsule of NRG-Akita mice rapidly reversed the progressively worsening hyperglycemia observed in these animals (Figure 6A). Fasting blood glucose measurements of mice transplanted with SC-β cells averaged <200 mg/dl, whereas those transplanted with control PH cells showed progressively higher blood glucose levels that approached 600 mg/dL, as has been observed for non-transplanted NRG-Akita mice (Figure 6A) (Brehm et al., 2010). Mice that received SC-β cells also rapidly cleared glucose from the blood after a glucose injection, similar to the glucose clearance found in a separate independent cohort of NRG-Akita mice transplanted with 4000 IEQ of human islets (Figures 6B). We measured human insulin in the bloodstream 18 wk after transplantation and found mice that received SC-β cells maintained human insulin secretion (Figure 6C).
Figure 6. Transplanted SC-β cells rapidly ameliorates hyperglycemia in diabetic mice.

(A) Fasting blood glucose measurements of progressively diabetic NRG-Akita mice transplanted with HUES8 SC-β cells (5×106 cells; open circles; n=6) or PH cells (5×106 cells; closed square; n=6 for 0, 18, and 28 d and n=4 for 53, 84 and 112 d). Glucose measurements were saturated at 600mg/dL. *p<0.05 comparing the 2 cell groups on the same d with unpaired t-test. Data presented as mean±SEM.
(B) Blood glucose measurements of mice that have been transplanted 137 d prior with HUES8 SC-β cells (n=5) or PH cells (n=1) and a separate independent cohort of mice transplanted 34 d prior with human islets (4000 IEQ; closed triangle; n=6). Note: It was not possible to coordinate receipt of human cadaveric islets and the production of SC-β cells. So the data in Figure 6B come from a different animal cohort. One mouse that received HUES8 SC-β cells died after a blood draw taken in (C), and 5 mice that received PH cells died over the duration of the observation period. Data presented as mean±SEM.
(C) ELISA measurements of human insulin from the serum of individual mice transplanted with HUES8 SC-β cells (n=6) or PH cells (n=2). Mice were fasted for 16 hr and then blood glucose was measured before (white bars) and 30 min after (black bars) a glucose injection of mice, 126 d post-transplantation. p<0.05 for transplanted HUES8 SC-β cells insulin concentration 30 min vs. 0 min after glucose injection with paired t-test.
Mice transplanted with SC-β cells also survived better than control mice: 2/6 mice that received PH cells died within eight wk of transplantation compared to 0/6 mice that received SC-β cells. By the end of more than 4 months observation post transplantation, 5/6 mice that received PH cells died compared to 1/6 mice that received SC-β cells. Thus SC-β cells are capable of secreting insulin and rapidly ameliorating progressive hyperglycemia in a diabetic mouse model.
Discussion
Here we show that functional human SC-β cells can be directly generated from human pluripotent stem cells in vitro. The data presented demonstrate that these cells function similarly to primary human β cells both in vitro and in vivo post-transplantation. These cells can be generated without genetic modification and in large numbers (billions of cells). While not all of the cells present at the end of the protocol are SC-β cells, the percentage of NKX6-1+/C-peptide+ cells in the cluspters is similar to that found in human islets, and the size of the clusters is comparable, though slightly larger on average than human islets (approximately 200–250 μm diameter vs 100–150 μm diameter). This is all accomplished ex vivo by the addition of defined factors, without the addition of mesenchymal or endothelial cells that normally accompany β cell development.
Although we observed that the global gene expression patterns of SC-β cells are more similar to adult human β cells than to fetal β cells, or previously produced INS+ cells, gene expression differences still remain. One possibility is that additional modifications to the culture media or added factors could shift the cells even closer to primary β cells. Another possibility is that gene expression patterns in cadaveric β cells result from varied causes of death of the donors, the isolation and recovery process, or shipping, or arise from the influence of adjacent non-endocrine cells. Future studies will include a more detailed analysis of the gene expression differences between SC-β and primary β cells. Two differentiated β cell markers UCN3 (Blum et al., 2012) and MAFA (Aguayo-Mazzucato et. al., 2013) were not investigated because of the low sensitivity of the probes on the DNA microarray. Looking ahead, it may be possible to use the approach developed here to improve the number of SC-β cells formed, as well as altering the differentiation of pancreatic endocrine progenitors to produce all the other endocrine hormone cell types (α, γ, δ, ε) and reconstruct the proportions found in human islets.
A preparation of monohormonal cells that respond to a single glucose challenge has been previously reported, but those cells were not shown to express the key β cell identity marker NKX6-1 nor function in vivo (Cheng 2012.) Recent work has shown that differentiation protocols that generate higher levels of NKX6-1 lead to better outcomes for the pancreatic progenitor transplants (Rezania et al., 2013). Conditional knock-out studies have shown that NKX6-1 is necessary for β cell function in adult mouse islets, suggesting that co-expression of these factors in SC-β cells may be part of the reason for their functional abilities (Taylor et al., 2013). Despite the potential malleability of gene expression levels, we consider the key feature of β cells to be their function, i.e. their ability to repeatedly respond to glucose by secreting insulin in a way that can be quantified and observed in vivo and in vitro. The characterization of SC-β cell physiology can be extended in future studies by performing a time course of insulin synthesis and secretion and determining how long these cells maintain this phenotype in vitro and in vivo.
We note that the insulin detected in serum of transplanted SC-β cells was generally lower than that of animals transplanted with cadaveric donor islets on a per cell basis (Tables S2 and S3). One possibility is that the other cell types in islets, mesenchyme, endothelial cells, or other endocrine cell types, may help engraftment or the vascularization necessary for glucose and insulin exchange from the mouse vasculature. Another possibility is that the slightly larger size of the SC-β clusters compared to the human islets we received may influence relative insulin amounts secreted, as it has been observed that smaller islets secrete more insulin per cell than larger islets (Fujita et al., 2011). Nonetheless, the fact that transplantation of SC-β cells consistently results in rapid and glucose responsive insulin production and that these cells function to treat diabetes in a mouse model is encouraging.
The results described here suggest that SC-β cells present an opportunity for cell therapy. Limited supplies of donated cadaveric islets and the very small amount of human β cell replication achieved in vitro have severely limited human β cell supplies to-date. This limitation has restricted transplantation options for patients as well as high throughput drug screening and disease modeling. A single 68 kg (150lb) patient requires roughly 340–750 million transplanted islet cells to effectively resolve type 1 diabetes via islet transplantation (McCall and Shapiro, 2012; Shapiro et al., 2006). The strategy we describe here may address this limitation as it utilizes a renewable cell source and a scalable method, with cells grown 300 million at a time in suspension in a single 500ml flask. Thus one or 2 flasks may be sufficient for treatment of a patient. An additional clinical advantage of SC-β cells compared to previously proposed therapies using pancreatic progenitors is that these cells do not require an extended post-transplantation period before observing insulin production. Immediate insulin production makes it theoretically possible to reduce patient exogenous insulin requirements from the first few days post-transplantation.
These cells also present new opportunities for β cell studies. A single flask could provide enough cells for screening 30,000 compounds in a 384 well format seeded with 10,000 cells per well. Unlike primary human β cells, SC-β cells can also be generated from pluripotent cells of any desired genetic background. hiPSC, which function like hESC, can be generated from any fibroblasts or other somatic cell types through introduction of a small set of pluripotency genes (Takahashi 2006). hiPSC cells from patients with diabetes or other metabolic syndromes have been derived. Work in progress in our laboratory has demonstrated that this protocol can be applied to differentiate SC-β cells from diabetic hiPSC lines, which could be used for disease modeling and the study of β cell function or susceptibility to stress or immune attack. Furthermore, technologies like TALEN and CRISPR enable genome editing of hESC or hiPSC cells to test variants identified by genome wide association studies (GWAS). SC-β cell drug responses could be compared between genetically matched pairs of mutant and non-mutant β cells (Ding et al., 2013). Identification and testing of novel biomarkers for β cell function or pharmacogenetics is also enabled by the combination of these technologies. Thus SC-β cells provide a new platform for in vitro drug discovery and characterization for human metabolism and diabetes.
The generation of SC-β cells provides a potentially useful step towards the generation of islets and pancreatic organs. Incorporating pancreatic niche cells, such as mesenchymal or endothelial cells, into cultures of stem cell derived pancreatic cells may be beneficial (Sneddon et al., 2012; Lammert et al., 2001). Other evidence suggests that the presence of α and γ cells may be important for precise tuning of normal β cell function (Rodriguez-Diaz et al., 2011). Tissue engineering of a pancreatic organ will require incorporation of exocrine and ductal tissue, possibly in a specified architecture. Much work remains to be done to achieve any of these therapeutic, disease modeling, drug discovery, or tissue engineering goals but the generation of SC-β cells represents a step forward towards making a clinical impact with stem cell biology.
Experimental Procedures
Cell culture
Undifferentiated hPSC lines were maintained in mTeSR1 (StemCell Technologies Inc.) in 500ml spinner flasks (Corning, VWR) placed on a 9-Position stir plate (Chemglass) set at rotation rate of 70rpm in a 37°C incubator, 5% CO2, and 100% humidity. The human embryonic stem cell line HUES8 and 2 hiPSC cell lines (hiPSC-1 and hiPSC-2) were utilized for all experiments shown. HUES8 cells are part of the NIH human embryonic stem cell registry eligible for NIH funding and differentiate well into multiple lineages (Chetty et al., 2013).
Using significant modifications of previously published protocols (Schulz et al., 2012; Rezania et al., 2012; Hrvatin et al., 2014), populations of DE, PGT and PP1 cells were generated as described below. For initiation of SC-β cell differentiation, HUES8, hiPSC-1, or hiPSC-2 cells were seeded at 6×105 cells/ml in mTeSR1 media+10μM Y27632. The differentiation was started 48 hr later for HUES8 and 72 hr later for hiPSC-1 and hiPSC-2 by changing media to Day media. Media changes were as follows – Day 1: S1+100ng/ml ActivinA (R&D Systems)+3μM Chir99021 (Stemgent). Day 2: S1+100ng/ml ActivinA. Days 4, 6: S2+50ng/ml KGF (Peprotech). Days 7, 8: S3+50ng/ml KGF+0.25μM Sant1 (Sigma)+2μM RA (Sigma)+200nM LDN193189 (only Day 7) (Sigma)+500nM PdBU (EMD Millipore). Days 9, 11, 13: S3+50 ng/ml KGF+0.25μM Sant1+100nM RA. Days 14, 16: S5+0.25μM Sant1+100nM RA+1μM XXI (EMD Millipore)+10μM Alk5i II (Axxora)+1μM T3 (EMD Millipore)+20ng/ml Betacellulin (Thermo Fisher Scientific). Days 18, 20: S5+25nM RA+1μM XXI+10μM Alk5i II+1μM T3+20ng/ml Betacellulin. Days 21–35 (change every 2nd day): S6+10μM Alk5i II+1μM T3. In the final stage, cells were analyzed between 28–33 d of the protocol.
For generation of PH protocol cells, HUES8 was used, and the same differentiation protocol was followed until d 14. On d 14 and 16, cells were fed with S3+1μM Alk5i II, 200nM LDN193189, and 100nM RA (Rezania et al., 2012). On d 18 and onward, cells were fed every other d with S3+100nM RA. Cells were maintained in this media until experimental analysis. Cells were maintained in culture and tested after the same number of days in differentiation media as the SC-β cells to control for the impact of time in culture.
Glucose stimulated insulin secretion
Human islets (~500 IEQ, Prodo Laboratories) or differentiated PH or SC-β cells (~5×105 cells between 28–35 d of differentiation) were sampled. Clusters were washed with Krebs (Krb) buffer and then pre-incubated in low (2mM) glucose Krb for 2 hr to remove residual insulin. Clusters were washed 2 times in Krb, incubated in low glucose Krb for 30 min, and supernatant collected. Then clusters were washed 2 times in Krb, incubated in high glucose Krb for 30 min, and supernatant collected. This sequence was repeated 2 additional times. Finally, clusters incubated in Krb containing 2mM glucose and 30mM KCl (depolarization challenge) for 30 min, then supernatant collected. Clusters were then dispersed into single cells using TrypLE Express (Life Technologies) and cell number was counted automatically by a Vi-Cell (Beckman Coulter). Supernatant samples containing secreted insulin were processed using the Human Ultrasensitive Insulin ELISA (ALPCO Diagnostics).
Proinsulin and insulin content measurements
Acid-ethanol extraction was used to extract protein, and proinsulin and insulin contact measured using intact human proinsulin (BioVendor) and human Ultrasensitive Insulin ELISA kits.
Calcium imaging
Clusters were attached to plates coated with hESC-qualified Matrigel (BD Biosciences). After incubation and attachment, the wells were washed with Krb buffer, incubated with Fluo4-AM (Life Technologies) for 45 min, washed with Krb buffer, and then incubated further in 37°C incubator for additional 15 min without the dye. Clusters were then immediately staged on an AxioZoom V16 microscope (Carl Zeiss) for acquisition of high resolution time series imaging.
Time series images were acquired at single cell resolution of 80x magnification, every 17 s. Progression of glucose challenges and time of the stimulation during imaging was as follows: 5 min in low (2mM) glucose Krb, wash, 5 min high (20mM) glucose Krb, and wash. This sequential treatment was repeated 2 more times, then a final 5-min incubation 2mM glucose Krb containing 30mM KCl was performed. Images were analyzed using ImageJ/Fiji. Analysis of the cluster was done by the measurement of the average fluorescence intensity of the whole cluster (population analysis) or average fluorescence intensity of the individual cells within the cluster (single cell analysis).
Immunohistochemistry
Differentiated cell clusters or islets were fixed with 4% PFA for 1 hr at room temperature (RT), washed, embedded in Histogel (Thermo), and sectioned for histological analysis. Before staining, paraffin was removed from sections using Histoclear (Thermoscientific), rehydrated, and underwent antigen retrieval by treatment with 0.1M EDTA (Ambion) in pressure cooker (Proteogenix) for 2 hr. For staining, slides were blocked with PBS+0.1% Triton X-100 (VWR)+5% donkey serum (Jackson Immunoresearch) for 1 hr at RT, incubated with primary antibodies overnight at 4°C, washed, incubated with secondary antibody incubation for 2 hr at RT, and washed. For imaging, samples were mounted in Vectashield (Vector Laboratories), covered with coverslips, and sealed with nail polish. Representative images were taken using an Olympus IX51 Microscope or Zeiss LSM 510 or 710 confocal microscope.
Flow cytometry
Differentiated cell clusters or islets were dispersed into single-cell suspension by incubation in TrypLE Express at 37°C, fixed with 4% PFA on ice for 30 min, washed once in PBS, and incubated in blocking buffer (PBS+0.1% TritonX100+5% donkey serum) on ice for 1 hr. Cells were then resuspended in blocking buffer with primary antibodies and incubated at 4°C overnight. Cells were washed twice in blocking buffer and then incubated in blocking buffer with secondary antibodies on ice for 2 hr. Cells were then washed thrice and analyzed using the LSR-II flow cytometer (BD Biosciences). Analysis of the results was performed using FlowJo software.
Gene expression analysis of sorted cells
To analyze global gene expression of SC-β cells, we used a recently described fixation and sorting strategy to isolate NKX6-1+/INS+ SC-β cells from the heterogenous cell clusters (Hrvatin et al., 2014). In brief, dispersed and fixed cells were incubated with primary antibodies for 30 min in buffer containing RNasin, washed twice, and then incubated with secondary antibodies in buffer containing RNasin for 30 min each. After antibody staining, cells were sorted by fluorescence activated cell sorting. RNA was extracted with the RecoverAll Total Nucleic Acid Isolation Kit (Ambion). The Illumina TotalPrep RNA Amplification Kit (Life Technologies) was used to make cRNA, which was run on Human HT-12 Expression BeadChips (Illumina) using the Whole-Genome Expression Direct Hybridization kit (Illumina). Chips were scanned on the Illumina Beadstation 500. These SC-β cell microarray data and the previously published hPSC, PH, fetal β and adult β cell data (Hrvatin et al., 2014) were imported into the R statistical computing platform using the programming packages lumi and EMA. Samples were analyzed by hierarchial clustering using Pearson’s correlation and Ward linkage. The pattern of clustering was robust to other distance and linkage metrics. Microarray data will be uploaded to publicly available databases.
Electron microscopy
To analyze granular ultrastructure, cadaveric pancreatic islets or differentiated hPSC were fixed at RT for 2 hr with a mixture containing 1.25% PFA, 2.5% glutaraldehyde, and 0.03% picric acid in 0.1M sodium cocodylate buffer (pH 7.4). Samples were then washed in 0.1M cacodylate buffer and post-fixed at RT with a mixture of 1% OsO4/1.5% KFeCN6 once for 2 hr then once for 1 hr. After washing with water, samples were stained in 1% aqueous uranyl acetate for 1 hr, washed, and subsequently dehydrated. An 1 hr incubation in propyleneoxide was followed by infiltration overnight in a 1:1 mixture of propyleneoxide and TAAB Epon (Marivac Canada Inc. St. Laurent, Canada), after which samples were embedded in TAAB Epon. Cut sections were then stained with 0.2% lead citrate. A JEOL 1200EX Transmission electron microscope or a TecnaiG2 Spirit BioTWIN was used to analyze the samples. For determination of granular protein composition, immunogold labeling was performed on cadaveric pancreatic islets or differentiated clusters.
Transplantation studies
Immunodeficient SCID-Beige mice, aged 8–10 wk, were procured from Taconic or The Jackson Laboratory, and NOD.Cg-Rag1tm1Mom IL2rgtm1Wjl Ins2Akita (NRG-Akita), aged 8–12 wk, were generously provided by Dr. Leonard D. Shultz of The Jackson Laboratory, Bar Harbor, ME. Human islets (500-1000IEQ per animal for SCID-Beige or 4000IEQ per animal for NRG-Akita mice) or hPSC derived cell clusters (5 million cells per animal) were loaded into catheter for cell delivery below the kidney capsule of mice.
At select times, mice were analyzed by performing a glucose challenge, measuring blood glucose, and collecting serum to measure human insulin. After fasting the mice for 16 hr overnight, mice were injected intraperitoneal (IP) with 2g D-(+)-glucose/1 kg body weight and blood glucose measured and serum collected at 0 and 30 min post glucose injection. Serum human insulin levels were quantified using the Human Ultrasensitive Insulin ELISA. Kidneys containing the grafts were dissected from the mice, fixed in 4% PFA overnight, embedded in paraffin, and sectioned for histological analysis. IHC analysis was performed as described above. All experiments were in accordance with the guidelines of the appropriate committee.
Statistical analysis
Statistical analysis was performed by using unpaired and paired t-tests. Box and whisker plots were generated with BoxPlorR (http://boxplot.tyerslab.com/) using default settings for box and whisker length.
Supplementary Material
Additional representative examples of in vitro-derived HUES8 SC-β cell insulin secretion in response to multiple sequential high glucose challenges. Some examples were chosen to illustrate the occasional failure of both SC-β and primary β cells to respond to high glucose that was observed. Three additional representative ELISA measurements of HUES8 SC-β cells (A), PH cells (B), and primary β cells (C) challenged sequentially with 2, 20, 2, 20, 2, and 20 mM glucose, with a 30-minute incubation for each concentration, are shown (see Methods). After sequential low/high glucose challenges, cells were depolarized with 30 mM KCl. Related to Figure 1.
Table S1. Differentiation factors used in steps 3, 4, 5, and 6
Table S2. ELISA measurements of human insulin from the serum of mice transplanted with HUES8 SC-β cells, primary β cells, and PH cells
Table S3. ELISA measurements of human insulin from the serum of mice transplanted with hiPSC-derived SC-β cells
SC-β cells can be generated from other hPSC lines in vitro.
(A) Representative ELISA measurements of secreted human insulin from hiPSC SC-β cells generated from two hiPSC lines (hiPSC-1 and hiPSC-2) challenged sequentially with 2, 20, 2, 20, 2, and 20 mM glucose, with a 30-minute incubation for each concentration (see Methods). After sequential low/high glucose challenges, cells were depolarized with 30 mM KCl.
(B) Representative immunohistochemistry of cells stained for C-peptide (green) and NKX6-1 (red).
(C) Representative immunohistochemistry of cells stained for C-peptide (green) and PDX1 (red).
(D) Representative immunohistochemistry of cells stained for C-peptide (green) and glucagon (red) with the corresponding DAPI stain (blue).
Enlarged insets in B, C and D shows staining for transcription factors (NKX6-1 and PDX1) is nuclear and cytoplasmic for C-peptide, except for the PH cells.
(E) Representative flow cytometry dot plots and population percentages of cells stained for C-peptide and NKX6-1. AU = arbitrary units.
All images were taken with a Olympus IX51 microscope.
Scale bar = 100 μm
Protocol for making SC-β cells produced low percentages of SST and GCG expressing cells. Representative flow cytometry dot plots and population percentages of HUES8 SC-β, primary human β cells, and PH cell populations are shown.
(A) Stained for C-peptide and GCG.
(B) Stained for C-peptide and SST.
(C) Stained for SST and GCG.
Related to Figure 3.
SST=somatostatin; GCG=glucagon ; AU=arbitrary units
SC-β cells have gene expression comparable to human β cells and different from PH cells. Select genes measured by transcriptional microarray of PH cells (n=2) and adult primary β cells (n=4) sorted for INS (data from Hrvatin et al. 2014) and HUES8 SC-β cells (n=2) sorted for INS and NKX6-1. Data shown as mean±SEM. * indicates p<0.05 comparing to adult primary β cells. Related to Figure 3.
SC-β cells grafts contain large regions of C-peptide-expressing cells. Low magnification images of histological sections of HUES8 SC-β and PH cells transplanted into mice two weeks prior are shown. Grafts were stained with DAPI (blue), C-peptide (green), and GCG (red). The yellow/dim green tissue on the right side of each image is the autofluorescent mouse kidney tissue and is marked with an asterisk. Transplantation of PH cells resulted in large masses/tumors in the majority of the mice at later times, but this was not observed with transplantation of SC-β cells. A much larger number of transplants and more extensive histological examination will be needed to assess the possibility of undesired cell growth in the grafts. All images were taken with an Olympus IX51 microscope. Scale bar = 200 μm. Related to Figure 5.
Highlights.
Stem cell-derived β (SC-β) cells secret insulin upon glucose stimulation in vitro
SC-β cells resemble human islet β cells by gene expression and ultrastructure
SC-β cell transplantation ameliorates hyperglycemia in mice
SC-β cells provide a platform for therapeutic development and disease modeling
Acknowledgments
We thank Chunhui Xie, Eliza Scadden, and Isaac Alter for excellent technical assistance, Maria Ericsson, Elizabeth Benecchi, and Louise Trakimas from the HMS Conventional Electron Microscopy Facility for assistance with electron microscopy, and Dena Cohen, Jeffrey Davis, Adam Roose, Barak Blum and the Greiner and BetaLogics laboratories for helpful discussions. We also thank the members of the Harvard Stem Cell Institute Histology Core and Flow Cytometry Core facilities for invaluable assistance. The NRG-Akita mice were generously provided by Dr. Leonard Shultz, J.R.M. was supported by a fellowship from the Harvard Stem Cell Institute. Q.P.P was supported by a fellowship from the Juvenile Diabetes Research Foundation. D.A.M. is an Investigator of the Howard Hughes Medical Institute. This work was supported by grants from the Harvard Stem Cell Institute, NIH, Helmsley Charitable Trust, the JPB Foundation and the generosity of M. and A. Barry.
Footnotes
Author Contributions
All authors contributed to conception and design of experiments. Individual experimental contributions are as follows: F.W.P, J.R.M., M.G., and M.S. were primarily responsible for the experiments shown in Figures 1, 3, 5, and S1-5 and Tables S1–3; J.R. for Figure 2; A.V.D. for Figure 4; and D.G. for Figure 6. F.W.P, J.R.M, M.G., and D.A.M. wrote the manuscript. All authors reviewed, edited, and approved the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aguayo-Mazzucato C, Zavacki AM, Marinelarena A, Hollister-Lock J, Khattabi IE, Marsili A, Weir GC, Sharma A, Larsen PR, Bonner-Weir S. Thyroid Hormone Promotes Postnatal Rat Pancreatic β-Cell Development and Glucose-Responsive Insulin Secretion Through MAFA. Diabetes. 2013;62:1569–580. doi: 10.2337/db12-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apelqvist A, Li H, Sommer L, Beatus P, Anderson DJ, Honjo T, Hrabe de Angelis M, Lendahl U, Edlund H. Nature. 1999;400:877–881. doi: 10.1038/23716. [DOI] [PubMed] [Google Scholar]
- Bellin MD, Barton FB, Heitman A, Harmon J, Balamurugan AN, Kandaswamy R, Sutherland DE, Alejandro R, Hering BJ. Potent Induction Immunotherapy Promotes Long-Term Insulin Independence After Islet Transplantation in Type 1 Diabetes. American Journal of Transplantation. 2012;12:1576–583. doi: 10.1111/j.1600-6143.2011.03977.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum B, Hrvatin SS, Schuetz C, Bonal C, Rezania A, Melton DA. Functional beta-cell maturation is marked by an increased glucose threshold and by expression of urocortin 3. Nat Biotechnol. 2012 Feb 26;30(3):261–4. doi: 10.1038/nbt.2141. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehm MA, Bortell R, Diiorio P, Leif J, Laning J, Cuthbert A, Yang C, Herlihy M, Burzenski L, et al. Human Immune System Development and Rejection of Human Islet Allografts in Spontaneously Diabetic NOD-Rag1null IL2r{gamma} Ins2Akita Mice. Diabetes. 2010;59:2265–2270. doi: 10.2337/db10-0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brelje TC, Stout LE, Bhagroo NV, Sorenson RL. Distinctive roles for prolactin and growth hormone in the activation of signal transducer and activator of transcription 5 in pancreatic islets of langerhans. Endocrinology. 2004;145:4162–175. doi: 10.1210/en.2004-0201. [DOI] [PubMed] [Google Scholar]
- Bruin JE, Erener S, Vela J, Hu X, Johnson JD, Kurata HT, Lynn FC, Piret JM, Asadi A, et al. Characterization of polyhormonal insulin-producing cells derived in vitro from human embryonic stem cells. Stem Cell Res. 2014;12:194–208. doi: 10.1016/j.scr.2013.10.003. [DOI] [PubMed] [Google Scholar]
- Cheng X, Ying L, Lu L, Galvão AM, Mills JA, Lin HC, Kotton DN, Shen SS, Nostro MC, et al. Self-renewing endodermal progenitor lines generated from human pluripotent stem cells. Cell Stem Cell. 2012;10:371–384. doi: 10.1016/j.stem.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty S, Pagliuca FW, Honore C, Kweudjeu A, Rezania A, Melton DA. A simple tool to improve pluripotent stem cell differentiation. Nat Methods. 2013;10:553–56. doi: 10.1038/nmeth.2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amour KA, Agulnick AD, Eliazer S, Kelly OG, Kroon E, Baetge EE. Efficient differentiation of human embryonic stem cells to definitive endoderm. Nat Biotechnol. 2005;23:1534–541. doi: 10.1038/nbt1163. [DOI] [PubMed] [Google Scholar]
- D’Amour KA, Bang AG, Eliazer S, Kelly OG, Agulnick AD, Smart NG, Moorman MA, Kroon E, Carpenter MK, Baetge EE. Production of pancreatic hormone--expressing endocrine cells from human embryonic stem cells. Nat Biotechnol. 2006;24:1392–1401. doi: 10.1038/nbt1259. [DOI] [PubMed] [Google Scholar]
- Deconinck JF, Potvliege PR, Gepts W. The ultrastructure of the human pancreatic islets. Diabetologia. 1971;7:266–282. doi: 10.1007/BF01211879. [DOI] [PubMed] [Google Scholar]
- Ding Q, Lee YK, Schaefer EK, Peters D, Veres A, Kim K, Kuperwasser N, Motola D, Meissner T, et al. A TALEN Genome-Editing System for Generating Human Stem Cell-Based Disease Models. Cell Stem Cell. 2013;12:238–251. doi: 10.1016/j.stem.2012.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita Y, Takita M, Shimoda M, Itoh T, Sugimoto K, Noguchi H, Naziruddin B, Levy MF, Matsumoto S. Large human islets secrete less insulin per islet equivalent than smaller islets in vitro. Islets. 2011;3:1–5. doi: 10.4161/isl.3.1.14131. [DOI] [PubMed] [Google Scholar]
- Gamer LW, Wright CV. Autonomous endodermal determination in Xenopus: regulation of expression of the pancreatic gene XlHbox 8. Dev Biol. 1995;171:240–251. doi: 10.1006/dbio.1995.1275. [DOI] [PubMed] [Google Scholar]
- Hebrok M, Kim S, St-Jacques B, McMahon A, Melton DA. Regulation of pancreas development by hedgehog signaling. Development. 2000;127:4905–4913. doi: 10.1242/dev.127.22.4905. [DOI] [PubMed] [Google Scholar]
- Henry GL, Melton DA. Mixer, a novel homeobox gene, is required for endoderm development. Science. 1998;281:91–96. doi: 10.1126/science.281.5373.91. [DOI] [PubMed] [Google Scholar]
- Hrvatin S, O’Donnell CW, Deng F, Millman JR, Pagliuca FW, DiIorio P, Rezania A, Gifford DK, Melton DA. Differentiated human stem cells resemble fetal, not adult, β cells. Proc Natl Acad Sci USA. 2014:201400709. doi: 10.1073/pnas.1400709111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SK, Hebrok M, Li E, Oh SP, Schrewe H, Harmon EB, Lee JS, Melton DA. Activin receptor patterning of foregut organogenesis. Genes Dev. 2000;14:1866–1871. [PMC free article] [PubMed] [Google Scholar]
- Keirstead HS, Nistor G, Bernal G, Totoiu M, Cloutier F, Sharp K, Steward O. Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants remyelinate and restore locomotion after spinal cord injury. The Journal of Neuroscience. 2005;25:4694–4705. doi: 10.1523/JNEUROSCI.0311-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriks S, Shim JW, Piao J, Ganat YM, Wakeman DR, Xie Z, Carrillo-Reid L, Auyeung G, Antonacci C, Buch A. Dopamine neurons derived from human ES cells efficiently engraft in animal models of Parkinson/’s disease. Nature. 2011;480:547–551. doi: 10.1038/nature10648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, Young H, Richardson M, Smart NG, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26:443–452. doi: 10.1038/nbt1393. [DOI] [PubMed] [Google Scholar]
- Labriola L, Montor WR, Krogh K, Lojudice FH, Genzini T, Goldberg AC, Eliaschewitz FG, Sogayar MC. Beneficial effects of prolactin and laminin on human pancreatic islet-cell cultures. Mol Cell Endocrinol. 2007;263:120–133. doi: 10.1016/j.mce.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Lammert E, Cleaver O, Melton D. Induction of pancreatic differentiation by signals from blood vessels. Science. 2001;294:564–67. doi: 10.1126/science.1064344. [DOI] [PubMed] [Google Scholar]
- Like AA, Orci L. Embryogenesis of the human pancreatic islets: a light and electron microscopic study. Diabetes. 1972;21:511–534. doi: 10.2337/diab.21.2.s511. [DOI] [PubMed] [Google Scholar]
- Lu B, Malcuit C, Wang S, Girman S, Francis P, Lemieux L, Lanza R, Lund R. Long-term safety and function of RPE from human embryonic stem cells in preclinical models of macular degeneration. Stem Cells. 2009;27:2126–135. doi: 10.1002/stem.149. [DOI] [PubMed] [Google Scholar]
- Matschinsky FM. Assessing the potential of glucokinase activators in diabetes therapy. Nature Reviews Drug Discovery. 2009;8:399–416. doi: 10.1038/nrd2850. [DOI] [PubMed] [Google Scholar]
- McCall M, Shapiro AMJ. Update on Islet Transplantation. Cold Spring Harb Perspect Med. 2012;2:a007823. doi: 10.1101/cshperspect.a007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modi P. Diabetes beyond insulin: review of new drugs for treatment of diabetes mellitus. Curr Drug Discov Technol. 2007;4:39–47. doi: 10.2174/157016307781115476. [DOI] [PubMed] [Google Scholar]
- Mohammed JS, Wang Y, Harvat TA, Oberholzer J, Eddington DT. Microfluidic device for multimodal characterization of pancreatic islets. Lab Chip. 2009;9:97–106. doi: 10.1039/b809590f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murtaugh LC, Stanger BZ, Kwan KM, Melton DA. Notch signaling controls multiple steps of pancreatic differentiation. Proc Natl Acad Sci USA. 2003;100:14920–14925. doi: 10.1073/pnas.2436557100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayanan K, Lim VY, Shen J, Tan ZW, Rajendran D, Luo SC, Gao S, Wan CA, Ying J. Extracellular matrix-mediated differentiation of human embryonic stem cells: Differentiation to insulin-secreting beta cells. Tissue Eng Part A. 2013;20:424–433. doi: 10.1089/ten.TEA.2013.0257. [DOI] [PubMed] [Google Scholar]
- Ninomiya H, Takahashi S, Tanegashima K, Yokota C, Asashima M. Endoderm differentiation and inductive effect of activin-treated ectoderm in Xenopus. Dev Growth Differ. 1999;41:391–400. doi: 10.1046/j.1440-169x.1999.00449.x. [DOI] [PubMed] [Google Scholar]
- Nostro MC, Sarangi F, Ogawa S, Holtzinger A, Corneo B, Li X, Micallef SJ, Park IH, Basford C, et al. Stage-specific signaling through TGF{beta} family members and WNT regulates patterning and pancreatic specification of human pluripotent stem cells. Development. 2011;138:861–871. doi: 10.1242/dev.055236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JA, Brelje TC, Sorenson RL. Adaptation of islets of Langerhans to pregnancy: increased islet cell proliferation and insulin secretion correlates with the onset of placental lactogen secretion. Endocrinology. 1992;130:1459–466. doi: 10.1210/endo.130.3.1537300. [DOI] [PubMed] [Google Scholar]
- Rezania A, Bruin JE, Riedel MJ, Mojibian M, Asadi A, Xu J, Gauvin R, Narayan K, Karanu F, et al. Maturation of Human Embryonic Stem–Cell Derived Pancreatic Progenitors Into Functional Islets Capable of Treating Pre-existing Diabetes in Mice. Diabetes. 2012;61:2016–029. doi: 10.2337/db11-1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezania A, Bruin JE, Xu J, Narayan K, Fox JK, O’Neil JJ, Kieffer TJ. Enrichment of human embryonic stem cell-derived NKX6.1-expressing pancreatic progenitor cells accelerates the maturation of insulin-secreting cells in vivo. Stem Cells. 2013;31:2432–442. doi: 10.1002/stem.1489. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Diaz R, Dando R, Jacques-Silva MC, Fachado A, Molina J, Abdulreda MH, Ricordi C, Roper SD, Berggren PO, Caicedo A. Alpha cells secrete acetylcholine as a non-neuronal paracrine signal priming beta cell function in humans. Nat Med. 2011;17:888–892. doi: 10.1038/nm.2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter GA, Hodson DJ. Minireview: Intraislet Regulation of Insulin Secretion in Humans. Molecular Endocrinology. 2013;27:1984–995. doi: 10.1210/me.2013-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz TC, Lynn FC, Young HY, Agulnick AD, Babin MJ, Baetge EE, Bang AG, Bhoumik A, Cepa I, et al. A Scalable System for Production of Functional Pancreatic Progenitors from Human Embryonic Stem Cells. PLoS ONE. 2012;7:e37004. doi: 10.1371/journal.pone.0037004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro AM, Ricordi C, Hering BJ, Auchincloss H, Lindblad R, Robertson RP, Secchi A, Brendel MD, Berney T, et al. International trial of the Edmonton protocol for islet transplantation. N Engl J Med. 2006;355:1318–330. doi: 10.1056/NEJMoa061267. [DOI] [PubMed] [Google Scholar]
- Shiba Y, Fernandes S, Zhu WZ, Filice D, Muskheli V, Kim J, Palpant NJ, Gantz J, Moyes KW, Reinecke H. Human ES-cell-derived cardiomyocytes electrically couple and suppress arrhythmias in injured hearts. Nature. 2012;489:322–25. doi: 10.1038/nature11317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sneddon JB, Borowiak M, Melton DA. Self-renewal of embryonic-stem-cell-derived progenitors by organ-matched mesenchyme. Nature. 2012;491:765–68. doi: 10.1038/nature11463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son EY, Ichida JK, Wainger BJ, Toma JS, Rafuse VF, Woolf CJ, Eggan K. Conversion of mouse and human fibroblasts into functional spinal motor neurons. Cell Stem Cell. 2011;9:205–218. doi: 10.1016/j.stem.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- Taylor BL, Liu FF, Sander M. Nkx6.1 Is Essential for Maintaining the Functional State of Pancreatic Beta Cells. Cell Rep. 2013;4:1262–275. doi: 10.1016/j.celrep.2013.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thowfeequ S, Ralphs KL, Yu W, Slack JMW, Tosh D. Betacellulin inhibits amylase and glucagon production and promotes beta cell differentiation in mouse embryonic pancreas. Diabetologia. 2007;50:1688–697. doi: 10.1007/s00125-007-0724-y. [DOI] [PubMed] [Google Scholar]
- Vetere A, Choudhary A, Burns SM, Wagner BK. Targeting the pancreatic β-cell to treat diabetes. Nature Reviews Drug Discovery. 2014 doi: 10.1038/nrd4231. [DOI] [PubMed] [Google Scholar]
- Xie R, Everett LJ, Lim HW, Patel NA, Schug J, Kroon E, Kelly OG, Wang A, D’Amour KA, et al. Dynamic Chromatin Remodeling Mediated by Polycomb Proteins Orchestrates Pancreatic Differentiation of Human Embryonic Stem Cells. Cell Stem Cell. 2013;12:224–237. doi: 10.1016/j.stem.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshioka M, Kayo T, Ikeda T, Koizuni A. A novel locus, Mody4, distal to D7Mit189 on chromosome 7 determines early-onset NIDDM in nonobese C57BL/6 (Akita) mutant mice. Diabetes. 1997;46:887–894. doi: 10.2337/diab.46.5.887. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional representative examples of in vitro-derived HUES8 SC-β cell insulin secretion in response to multiple sequential high glucose challenges. Some examples were chosen to illustrate the occasional failure of both SC-β and primary β cells to respond to high glucose that was observed. Three additional representative ELISA measurements of HUES8 SC-β cells (A), PH cells (B), and primary β cells (C) challenged sequentially with 2, 20, 2, 20, 2, and 20 mM glucose, with a 30-minute incubation for each concentration, are shown (see Methods). After sequential low/high glucose challenges, cells were depolarized with 30 mM KCl. Related to Figure 1.
Table S1. Differentiation factors used in steps 3, 4, 5, and 6
Table S2. ELISA measurements of human insulin from the serum of mice transplanted with HUES8 SC-β cells, primary β cells, and PH cells
Table S3. ELISA measurements of human insulin from the serum of mice transplanted with hiPSC-derived SC-β cells
SC-β cells can be generated from other hPSC lines in vitro.
(A) Representative ELISA measurements of secreted human insulin from hiPSC SC-β cells generated from two hiPSC lines (hiPSC-1 and hiPSC-2) challenged sequentially with 2, 20, 2, 20, 2, and 20 mM glucose, with a 30-minute incubation for each concentration (see Methods). After sequential low/high glucose challenges, cells were depolarized with 30 mM KCl.
(B) Representative immunohistochemistry of cells stained for C-peptide (green) and NKX6-1 (red).
(C) Representative immunohistochemistry of cells stained for C-peptide (green) and PDX1 (red).
(D) Representative immunohistochemistry of cells stained for C-peptide (green) and glucagon (red) with the corresponding DAPI stain (blue).
Enlarged insets in B, C and D shows staining for transcription factors (NKX6-1 and PDX1) is nuclear and cytoplasmic for C-peptide, except for the PH cells.
(E) Representative flow cytometry dot plots and population percentages of cells stained for C-peptide and NKX6-1. AU = arbitrary units.
All images were taken with a Olympus IX51 microscope.
Scale bar = 100 μm
Protocol for making SC-β cells produced low percentages of SST and GCG expressing cells. Representative flow cytometry dot plots and population percentages of HUES8 SC-β, primary human β cells, and PH cell populations are shown.
(A) Stained for C-peptide and GCG.
(B) Stained for C-peptide and SST.
(C) Stained for SST and GCG.
Related to Figure 3.
SST=somatostatin; GCG=glucagon ; AU=arbitrary units
SC-β cells have gene expression comparable to human β cells and different from PH cells. Select genes measured by transcriptional microarray of PH cells (n=2) and adult primary β cells (n=4) sorted for INS (data from Hrvatin et al. 2014) and HUES8 SC-β cells (n=2) sorted for INS and NKX6-1. Data shown as mean±SEM. * indicates p<0.05 comparing to adult primary β cells. Related to Figure 3.
SC-β cells grafts contain large regions of C-peptide-expressing cells. Low magnification images of histological sections of HUES8 SC-β and PH cells transplanted into mice two weeks prior are shown. Grafts were stained with DAPI (blue), C-peptide (green), and GCG (red). The yellow/dim green tissue on the right side of each image is the autofluorescent mouse kidney tissue and is marked with an asterisk. Transplantation of PH cells resulted in large masses/tumors in the majority of the mice at later times, but this was not observed with transplantation of SC-β cells. A much larger number of transplants and more extensive histological examination will be needed to assess the possibility of undesired cell growth in the grafts. All images were taken with an Olympus IX51 microscope. Scale bar = 200 μm. Related to Figure 5.


