Abstract
Community-based organizations (CBOs) serving persons living with HIV or AIDS face the challenge of an aging population with more chronic diseases. This study assessed cancer programming needs of AIDS service organizations (ASOs) in New York, New Jersey, and Connecticut by conducting a community needs assessment. Sixty (58%) of 103 organizations completed the survey. ASOs conduct activities most related to early steps along the cancer care continuum, but they also express great interest in expanding cancer-focused programming into new areas. ASOs have resources or capacities in assisting HIV+ clients with mental health or substance abuse problems, but there exists a need for funding in undertaking or expanding cancer-focused programs. ASOs are receptive to collaborating with researchers on disseminating cancer prevention and control knowledge in their settings. Community-academic research partnerships enable resonant training and technical assistance methods to be explored that will enhance the abilities of ASOs to bring cancer-related programming to their clients.
Community-based organizations serving persons living with human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS; i.e., PLWHA), face the challenges of serving an aging population. Advances in treatment have resulted in longer life expectancies for PLWHA (Detels et al., 1998; Palella et al., 2006). According to the Centers for Disease Control and Prevention (CDC), the percentage of all people living with AIDS over the age of 50 has risen each year for the past decade, increasing from 17% in 2001 (CDC, 2007) to 35% in 2009 (CDC, 2012), and this is expected to increase to 50% by 2015 (Effros et al., 2008). In 2008, the Antiretroviral Therapy Cohort Collaboration found that life expectancy for HIV-positive people on antiretroviral therapies was in the mid-60s, even for those who started therapy with severely depleted immune systems, while those who began therapy with CD4 counts over 200 per cubic milliliter could live into their 70s (Antiretroviral Therapy Cohort, 2008).
With the aging of the HIV-infected population comes increased risk for diseases associated with aging, such as cancer. As this demographic shift has occurred, non-AIDS defining malignancies (NADMs) including lung, stomach, anal, and liver cancers have overtaken the AIDS-defining malignancies (ADMs) in their impact on AIDS-related mortality (Bonnet et al., 2009; Engels et al., 2008; Shiels et al., 2011). A prospective observational analysis conducted by the CDC from 1992 to 2003 of 54,780 PLWHA showed that PLWHA, when compared with the general population, have a significantly higher risk of colorectal, renal, anal, vaginal, liver, lung, mouth, and throat cancers, as well as melanoma, leukemia, and Hodgkin’s lymphoma (Patel et al., 2008). In some cases, specific behavioral or comorbid factors contribute to increased cancer risk, e.g., tobacco use increases risk for numerous cancers, including lung, renal, mouth, throat, and stomach cancers; concurrent infection with Hepatitis C is a risk factor for liver cancer; and human papillomavirus infection increases risk for cervical, anal, and throat cancers (Martin, Fain, & Klotz, 2008; Silverberg & Abrams, 2007). Other factors that disproportionately affect PLWHA, such as HIV-induced immunosuppression, poverty, and membership in an ethnic or racial minority group, also increase the overall cancer burden in this population (Freeman, Zonszein, Islam, Blank, & Strelnick, 2011; Karpati, Bassett, & McCord, 2006). Thus, it is increasingly important that organizations serving PLWHA be ready to address the cancer concerns within this population.
There is strong interest in the dissemination and implementation of evidence-based knowledge to community settings, where the impact will be greatest. For example, from 2006 to 2008, the Education Network to Advance Cancer Clinical Trials educated staff in community organizations about cancer with the aim of increasing cancer clinical trial enrollment by minority patients (Michaels et al., 2012). In HIV prevention and care, community-based organizations have been a leading force in the development, dissemination, and implementation of best practices in HIV prevention and care, e.g., the CDC’s Diffusion of Effective Interventions (DEBI) program (https://www.effectiveinterventions.org). In addition, AIDS service organizations (ASOs) have been important partners in the recruitment of cohorts for clinical trials and studies on HIV prevention. Given this history and the centrality of ASOs in providing an array of supportive services to PLWHA, ASOs are ideally situated to address emerging issues in the epidemic, such as the growing cancer burden. ASOs, however, comprise a diverse group of organizations providing varied services, ranging from a large menu of different medical and social services to only a single specialized service (Kwait, Valente, & Celentano, 2001). Many ASOs lack sufficient resources, training, and programming to match the needs of aging PLWHA, and cancer concerns may not be salient for PLWHA and the agencies that serve them (Burkhalter et al., 2013). Other organizations providing social and health-supportive services may see PLWHA only as a subset of their larger client population and lack culturally appropriate experience with PLWHA overall (Emlet, Gerkin, & Orel, 2009). Thus, it is critical that the needs and capacities of ASOs to address the growing cancer concerns of PLWHA are better understood so that appropriate interventions can be developed to help ASOs bridge the gap between their HIV/AIDS-focused and cancer-related services and programming.
In 2009, three New York City-based institutions—Memorial Sloan-Kettering Cancer Center (MSKCC), The City College of New York (CCNY), and Gay Men’s Health Crisis (GMHC)—formed the HIV/AIDS and Cancer Community Research Collaboration (the Collaboration) to assess the cancer programming needs of ASOs and their clients. A first goal of the Collaboration was to conduct a community needs assessment among ASOs. Community needs assessments are conducted in order to identify and examine areas of concern and need in defined communities (Finifter, Jensen, Wilson, & Koenig, 2005), and in undertaking this needs assessment the Collaboration aimed to understand the challenges that community-based ASOs might face in the uptake of cancer programming, as well as the resources and assets they already have that would aid in such efforts. A second aim of the study was to identify characteristics of ASOs that are associated with level of need in order to better target future interventions. This paper reports the findings of a community needs assessment of ASOs in the three states of New York, Connecticut, and New Jersey.
METHODS
SURVEY DEVELOPMENT
To develop the survey, the Collaboration conducted serial focus groups with members of the Collaboration’s Community Advisory Board (CAB), which is comprised by representatives from ten ASOs in the New York metropolitan area (for details see, Burkhalter et al., 2013). Analysis of focus group transcripts identified ASO experiences and perceptions, as well as barriers to and capacities for implementing or expanding cancer-focused programming that spanned cancer prevention, screening, treatment, and survivorship. Focus group findings were used to draft the survey, and published community needs assessments were also examined in order to apply best practices in survey design (Finifter et al., 2005; Orel, 2006). The survey was refined through an iterative process of review and changes in which the research team and the CAB members provided input across several meetings from June through September 2010. The final survey had six sections with a total of 73 items.
The first section of the survey included 17 questions on individual respondents’ sociodemographic and work-related characteristics and additional items about the agencies for which they worked, such as number of employees and clients served. The second survey section had 12 items assessing current cancer-related programs or activities that the agency was undertaking, or, if not, whether they were interested (yes/no) and whether resources were available for implementing the activities (yes/ no). These activities included: (1) assessment of alcohol use and management of alcohol-related problems; (2) assessment of tobacco use and advice/assistance with quitting; (3) referral for cancer screening services; (4) interventions or programs to promote healthy diets; (5) referral to cancer care providers for treatment; (6) education of clients about human papillomavirus (HPV); (7) promotion of physical activity; (8) individual counseling with clients to identify cancer-related risk factors; (9) use of mobile units to provide cancer screening services on-site; and (10) support groups for clients who have had cancer. If an organization provided a service, the respondent was asked what kind of service delivery format was used, e.g., in-person provision of the service, printed educational materials, and community health fairs.
Organizational capacities were assessed with 10 items that queried organizational, staff, and client awareness and knowledge of the impact of cancer on PLWHA, knowledge of health insurance coverage for cancer services such as screening, funding resources, capacity to address mental health and substance abuse problems, the fit of their agency’s mission statement with a focus on cancer care, and whether their initial client assessment could (or does) capture information related to cancer. Respondents used a five-point scale ranging from: completely agree to completely disagree. ASO needs were assessed with a total of 18 items using a three-point response scale of: not at all a need, somewhat of a need, or very much a need. Items assessing interest and readiness in expanding or implementing cancer-focused activities used a four-point response scale ranging from: not at all interested to very much interested. Assessed needs comprised three areas: (1) education and information about cancer (six items; e.g., How much of a need does your agency have for education of clients about cancer concerns for PLWHA, such as risk factors, screening for cancer, cancer treatment or survivorship?); (2) issues around access to culturally competent cancer care (three items; e.g. How much of a need does your agency have for the ability to refer to culturally competent cancer care providers?), and; (3) partnerships with other entities (five items; e.g., How much of a need does your agency have for partnerships with other community-based organizations (CBOs) in order to share knowledge about cancer and HIV/AIDS?). Interest in and readiness to expand or undertake cancer-focused programming or activities were assessed (seven items; e.g., How interested do you believe your organization is in integrating or expanding cancer-focused activities?).
To understand ASO/CBO readiness for the academic-community collaborations that would undertake expansion or initiation of cancer-focused, two items asked about personal and organizational experience with research and whether their experiences were: mostly positive, mixed, positive, and negative, mostly negative, or not applicable. Five items assessed attitudes regarding their organizations’ receptivity to and readiness for research participation. These latter items used a five-point response scale ranging from: completely disagree to completely agree.
SAMPLE
As there are no definitive criteria for what constitutes an ASO, we established a priori guidelines for the purpose of this study. Organizations had to be community-based, nonprofit, and indicate a primary focus on providing HIV/AIDS-related services, typically social services. Medical providers, clinics, or hospitals were not included. To identify a broad ASO sample, the research team searched the current lists of HIV/AIDS service providers from the public health departments of New York, New Jersey, and Connecticut to identify 149 potential candidate organizations for survey participation. Of these 149 organizations, 41 were excluded because they offered very few HIV/AIDS services, were concerned primarily with HIV prevention for at-risk populations, or were part of or affiliated with medical institutions. For the remaining 108 ASOs, organizational websites were used to identify a contact person, usually an Executive Director, Program Director, or an individual with similar responsibilities within the organization. Through this process, five organizations were found to be either unreachable or ineligible, leaving a final sample of 103 ASOs.
PROCEDURE
Staff reached out to organizational contacts at the 103 ASOs by mail, e-mail, and telephone to solicit their interest in participating in the survey. In order to assure the anonymity of all responses, organizational contacts were asked to complete an Agency Contact Information sheet with their phone number, email, and postal mailing addresses and to identify a knowledgeable and experienced staff member within their organization whom they would ask to complete the survey. This procedure assured the anonymity of respondents while providing a means to communicate with organizational contacts in the event that questions about the survey arose. All participating organizations were offered a $50 donation upon completion of the survey. The study protocol was reviewed by the Institutional Review Boards at both MSKCC and CCNY and found to be research exempt from the requirement for HIPAA authorization and informed consent. The study’s primary community partner, Gay Men’s Health Crisis (GMHC), accepted these IRB decisions in the absence of an established IRB.
STATISTICAL ANALYSIS
Descriptive statistics were calculated using SPSS (v. 21). T-tests were performed to compare characteristics of ASOs responding to the survey to those ASOs that did not respond. To examine the relationship between ASO characteristics and type and level of needs, correspondence analysis was used—a multidimensional, nonlinear, descriptive technique for categorical data. The categorical data, in this instance, comprised 16 contingency tables of agency characteristic categories by agency need/ interest categories. The four candidates for agency characteristics were size of staff, number of clients served, size of budget, and geographical location. The four categories of need and interest were education and information, culturally competent cancer care, partnerships, and interests and readiness. The first step in the analysis was calculating the chi-square statistic for each contingency table and then dividing it by the total sample size to determine a measure of variance known as inertia. The larger the inertia, the stronger the relationship it indicates between the agency characteristic and the level of agency need or interest.
RESULTS
RESPONSE
Of the final sample of 103 organizations, 60 (58%) completed the survey. In order to check for any systematic bias between the responding and non-responding organizations, we used Guidestar, an online database of public government documents filed by nonprofit organizations (http://www.guidestar.org/), to gather descriptive information about the sample of 103 ASOs. For 96 of the 103 organizations, Guidestar was able to provide access to the IRS 990 forms filed by this sample of ASOs, and data on numbers of staff and volunteers and total revenue were used to compare study participating and nonparticipating organizations. Responding organizations on average had fewer staff members, fewer volunteers, and less total revenue than non-respondents, but these differences were not statistically significant (p > .05).
INDIVIDUAL RESPONDENT AND ORGANIZATIONAL CHARACTERISTICS
Characteristics of individual ASO employees completing the survey are as follows: 55% female and 45% male, with a mean age of 48.3 years (range 24 to 68 years), and 65% were white, 27% Black, 12% Hispanic, and 3% Asian/Pacific Islander. Most employees (80%) had graduate degrees, 13% had college degrees, and 7% with high school degrees. Staff were employed at their agency a mean of 10.5 years, had been in their current roles a mean of 8.1 years, and most (90%) were in administration or management positions. Table 1 shows the characteristics of the responding agencies. Median total staff size (both full- and part-time) was 42, with a range of 1 to 1,451. Thirty-three (55%) of the organizations surveyed had 50 or fewer employees, nine (15%) had between 51 and 100, and 15 (25%) had more than 100, and data were missing for three organizations. Organizational size was defined as number of part- and full-time staff, and a dichotomous variable of organizational size was used for subsequent analyses, with those having > 100 staff (large) compared to those with ≤ 100 staff (small). New York-based ASOs comprised 57% of the total, with the remainder evenly split between Connecticut and New Jersey. Nearly a quarter (23%) of all ASOs surveyed was in New York City, with another 38% in large cities throughout the tri-state area, and 38% in smaller cities and rural areas.
TABLE 1.
Characteristics of Responding AIDS Service Organizations
| Characteristics | Frequency | Percentage |
|---|---|---|
| Location of the organization | ||
| New York | 34 | 57 |
| New Jersey | 13 | 22 |
| Connecticut | 13 | 22 |
| Agency experience in cancer services | ||
| None | 24 | 40 |
| Prevention | 34 | 57 |
| Screening | 22 | 37 |
| Treatment | 7 | 12 |
| Survivorship | 4 | 7 |
| Research | 1 | 2 |
| Other (education, caregiver groups) | 2 | 3 |
| Median | Range | |
| Full-time staff | 34 | 0 to 768 |
| Part-time staff | 4 | 0 to 683 |
| Total staff | 42 | 1 to 1451 |
| Volunteers | 12 | 0 to 600 |
| Client base size | 1,000 | 20 to 35,000 |
INTEREST AND EXPERIENCE WITH CANCER-RELATED ACTIVITIES AND SERVICES
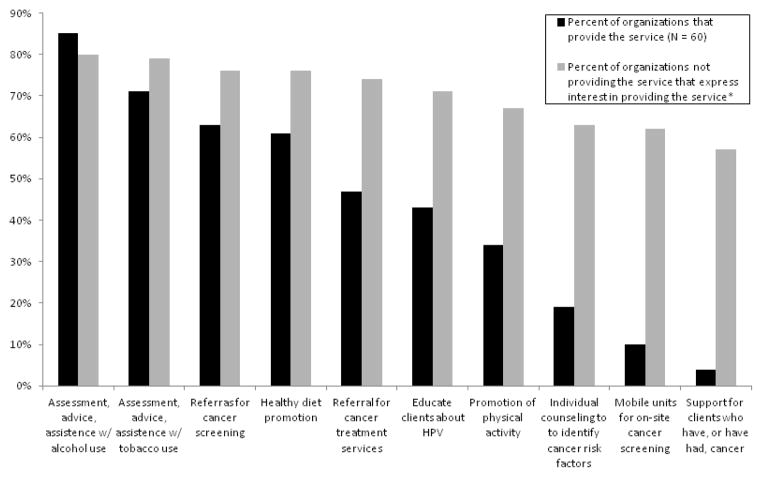
Ten cancer-related activities were queried in the survey, and Figure 1 illustrates the levels of agency experience in providing these, or interest in doing so when not providing them. Screening and assistance with treatment for alcohol (85%) and tobacco use (71%) were the most frequently reported services, followed by cancer-related referrals to other agencies or health care providers (63%), and healthy diet programs (61%). With the exception of tobacco use, however, risk factors specifically related to cancer were not as frequently assessed at client intake: diet (55%), physical activity/exercise (44%), personal history of cancer (42%), HPV infection status (38%), family history of cancer (25%), and sun protection (5%). When compared by staff size (data not shown), the larger organizations were more likely (80%, n = 15) to report experience providing cancer-related activities than smaller organizations (50%, n = 42). Among ASOs that provided cancer-related activities, the only statistically-significant difference by size was related to the provision of individual counseling regarding cancer-related risk factors, with 47% of large organizations providing this activity as opposed to only 10% of smaller organizations (p = .005). A separate set of questions (not shown) asked about the formats agencies preferred for the delivery of cancer programming that they currently engaged in. In this, agencies preferred formats that were generally less labor-intensive and targeted to larger audiences, such as the provision of printed educational materials (36%), health fairs (33%), educational presentations to groups of clients or staff (32%), and mass media or community outreach campaigns (10%).
FIGURE 1.
Levels of Experience and Interest in Cancer-Related Programming. *For this response, n = the number of organizations not providing the service already, which varies for each category from 9 (alcohol assessment & assistance) to 55 (support groups for clients w/ cancer).
With regard to the ten cancer programming activities, we asked organizations that were not currently offering those programs if they have any interest in so doing. Across all ten categories of activities, interest ranged from 80% of organizations (n = 9) showing an interest in assessing alcohol use to 57% (n = 55) interested in using mobile units for cancer screening. When organizations expressing interest in providing a cancer-related services that they did not currently offer were added together with those already performing the service, about 80% or more of the ASOs surveyed would be providing cancer-related activities if it were possible to do so. On the question of interest, however, there was a higher than expected level of missing data and incomplete responses. Of the organizations that did not have experience in one of the items in Figure 1 (up to 55 organizations depending on the activity), 16 had missing responses in their answers to the question whether they would have interest in taking up that activity. Among those 16, the average number of missing responses was 4 (range: 1–11).
ORGANIZATIONAL CAPACITIES
ASO capacities are presented in Table 2. ASOs reported a relatively high capacity to help clients address their substance abuse and mental health problems (90% and 88%, respectively). Only about half (55%) of agencies agreed partly or completely that their clients are aware and knowledgeable of their personal cancer risks and the impact of cancer on PLWHA. On the other hand, about two-thirds (66%) reported that their staff and organizational leadership were knowledgeable of cancer concerns for their clients. About two-thirds (63%) of staff was knowledgeable about health insurance coverage for cancer services, but a smaller percentage was knowledgeable about free or low cost cancer screening services (57%). Only about 7% of organizations agreed at any level that their organization had funding to support cancer-focused activities or services.
TABLE 2.
Current Organizational Cancer-Related Knowledge and Capacities
| Disagree (%) | Neither Agree nor Disagree (%) | Agree (%) | |
|---|---|---|---|
| Our clients have knowledge about… | |||
| Impact of cancer on PLWHA | 35 | 10 | 55 |
| Personal cancer risks | 38 | 11 | 48 |
| Our staff/organization has knowledge about… | |||
| Aging of HIV/AIDS population and the opportunity to re-focus services | 3 | 10 | 86 |
| Cancer concerns/risks on PLWHA | 20 | 14 | 66 |
| Health insurance coverage for cancer services | 29 | 8 | 63 |
| Free/low cost cancer screening services | 33 | 10 | 57 |
| Our organization can… | |||
| Help clients address their substance use problems | 7 | 3 | 90 |
| Help clients address their mental health problems | 10 | 2 | 88 |
| Support integration of cancer-related services (through mission statement) | 28 | 24 | 48 |
| Capture information related to cancer concerns | 17 | 8 | 75 |
PERCEIVED NEEDS FOR THE PROVISION OF CANCER-RELATED PROGRAMMING
Table 3 shows results for the assessment of organizational needs in the uptake or expansion of cancer-related programming. Across all need categories, a large majority of organizations perceived some need or great need. Agencies were most likely to report great need in the areas of education of clients and staff about cancer concerns for PLWHA (58% and 54%, respectively) and for information on links between cancer and HIV/AIDS and the specific impact of cancer on their organizations’ clients (64% and 61%, respectively). In addition, 95% of ASOs indicated that there was some or great need to involve public health agencies, such as the city or state departments of health, to provide them with financial and logistical support for implementing new or expanded cancer-focused programs. By contrast, the lowest need was for the involvement of local businesses, such as beauty or barber shops to spread the message about cancer (29% reported great need and 34% reported no need).
TABLE 3.
Organizational Needs for the Uptake of Cancer Programming
| Organizational Needs | No Need (%) | Some Need (%) | Great Need (%) |
|---|---|---|---|
| Education on cancer concerns among PLWHA for… | |||
| Clients | 5 | 37 | 58 |
| Staff | 5 | 41 | 54 |
| Leadership | 17 | 46 | 37 |
| Information/data on… | |||
| Cancer treatment/prevention clinical research trials | 7 | 56 | 37 |
| Links between HIV/AIDS and cancer | 5 | 31 | 64 |
| Impact of cancer on PLWHA clients | 5 | 33 | 61 |
| Ability to refer… | |||
| To culturally competent cancer providers | 17 | 41 | 42 |
| Undocumented/uninsured clients to cancer care | 10 | 37 | 53 |
| Ways to strengthen clients/medical provider relationship | 7 | 47 | 46 |
| Relationships/partnerships with… | |||
| Community businesses (to spread message about cancer risk for PLWHA) | 34 | 37 | 29 |
| Cancer care providers (for information and referrals) | 7 | 49 | 44 |
| Other CBOs (for knowledge sharing on HIV/AIDS and cancer) | 19 | 44 | 37 |
| Public health agencies (for support to expand services to include cancer) | 5 | 34 | 61 |
| Community volunteers (for implementation of cancer-related activities) | 24 | 32 | 44 |
The only factor that differentiated the organizations’ level of needs was organizational size. Correspondence analysis demonstrated consistent and statistically significant differences (p values ≤ .05) between small and large organizations. Smaller ASOs expressed greater needs on almost every item in the areas of education and information, culturally competent cancer care, and partnerships. Larger agencies perceived less need across all categories surveyed, but the difference was mainly a reduction of degree, from great need to some need, for the larger organizations.
RESEARCH PARTICIPATION
Overall, 71% of respondents reported that either they or their organizations, or both, had some experience with research. Only 27% reported that neither they nor their agency had any research experience. Among those with research experience, 58% reported that the experience was mostly positive, while the remaining 42% reported a mixture of both positive and negative experiences. None of the respondents had mostly negative research experience. Some 42% of respondents partly or completely disagreed with the statement that “working with academic, medical, or other kinds of research organizations is a one-way street where ‘we give, they take,’” 29% neither agreed nor disagreed, and 29% partly agreed with the statement. A majority of respondents agreed that “research partners will engage my organization as an active participant in research” (54.2%); and that “research partnerships with my organization will have our best interests and those of our clients in mind” (66.1%). Over half of respondents (61%) disagreed with the statement that “I do not believe that results of research partnerships my organization may form will be of practical use to my organization.” Nearly two-thirds of agencies agreed somewhat or completely that “my organization is prepared to be an active partner in research projects with outside organizations.”
DISCUSSION
To our knowledge, this is the first reported study to examine ASO interests, needs, capacities, and readiness to address the growing cancer needs of their clients. This study has identified five principal findings with regard to ASOs’ readiness and needs to implement or expand cancer programming. First, ASOs currently conduct activities most related to the early steps along the cancer care continuum, i.e., cancer prevention, such as assessing alcohol and tobacco use and promoting a healthy diet, as well as providing referrals for cancer screening. Second, ASOs are highly interested in providing services they do not currently offer, such as tobacco screening and assessment and education about HPV infection. Third, ASOs have notable resources or capacities in the areas of assisting HIV+ clients with mental health or substance abuse problems, but for undertaking or expanding cancer-focused programs, there is a marked need for funding. Fourth, ASOs express a strong need for education and information about the links between HIV/AIDS and cancer and the impact of cancer on their specific client population. Fifth, there is an overall positive receptivity to collaborating with researchers focused on the dissemination of cancer prevention and control knowledge in their settings.
Understanding the needs and capacities of CBOs that serve PLWHA will be increasingly important over the next decade. Mayberry et al. (2009), report that there is an important relationship between health at the individual and community/ population levels and suggest a potential role for CBOs to promote health, prevent disease, and address racial, ethnic, and socio-economic disparities in local communities. At the same time, federal funding streams for HIV/AIDS programming are becoming more closely tied to the geography of HIV/AIDS prevalence and incidence, privileging organizations from the 12 cities of highest prevalence/incidence (Valdiserri, 2011). Organizations in smaller cities, suburbs, and rural areas (outside of the HIV hot spots in the Deep South) thus face an increasingly challenging funding landscape.
As ASOs deal with changes in the funding landscape and emerging issues of cancer and aging among PLWHA, a growing number of organizations providing care for aging populations also serve PLWHA as a secondary client base. In one survey of Area Agencies on Aging in Washington State, 84% of responding agencies agreed that serving HIV-infected older adults was consistent with their mission, but few indicated that they had substantial experience with this population (Emlet et al., 2009). This raises issues not only of cultural competence with the high-prevalence HIV-positive populations (gay and bisexual men, women of color) but also of appropriate training in the particular ways in which cancer impacts PLWHA. These agencies would face specific issues of education and information on the differences between AIDS-defining and non-AIDS defining malignancies, as well as the differential rates of risk and incidence for some cancers among PLWHA.
Of note, smaller ASOs reported greater levels of need than larger ASOs in addressing their clients’ cancer concerns. Although the distribution of different cancer-related activities across organizations did not vary by size, larger organizations expressed much less need for partnerships with other organizations and health care providers, possibly indicating that even when they do not provide a service, their staff feel confident they can refer the client to another organization that can. Taken together, the findings suggest overall that most ASOs will be receptive to interventions to enable them to undertake a wider range of cancer-related activities for their clients with HIV/AIDS, but efforts to expand the uptake of cancer-related activities need to provide adequate resources and should specially target smaller agencies in an effort to ameliorate the disparities between large and small organizations.
Efforts to increase cancer-related programming will require training, further research, and capacity assessments. The findings that over half of respondents had a history of mostly positive research experiences and had positive attitudes regarding potential research collaborations bode well for future efforts to promote cancer programming, especially if interventions incorporate CBPR methods and provide ASOs with information about the linkages of HIV and cancer and its importance to their clients. A CBPR approach will also help to address ASO concerns that research sometimes results in creating data that do not serve their organizational needs (Burkhalter, et al., 2013).
The Collaboration’s needs assessment was conducted with ASOs in the tri-state area, and the results are therefore not generalizable across the country. However, the metropolitan New York region across the three states holds the second highest concentration of HIV and AIDS nationally (CDC, 2013) and, for this reason, ASOs in this region most likely demonstrate the diversity of issues and challenges faced in the field. We purposely excluded organizations providing medical services from the survey, which may have limited our understanding of the cancer-related programming that is available to PLWHA outside of ASOs. Given the importance of ASOs and social services to most PLWHA, especially those of lower socioeconomic status, however, our needs assessment captures the landscape of cancer-related programming as it is available to the PLWHA who are in the most precarious positions for health management and cancer risks.
The survey was self-reported by one staff member at the responding organization who had enough experience and seniority to accurately characterize the organization’s interests, needs, and readiness on issues of cancer programming. Because we did not screen respondents, some survey results may reflect the individual’s perception of his or her organization with some degree of personal bias. ASO staff respondent demographics (65% white, 35% nonwhite) reflected general population norms, with Blacks/African Americans somewhat over-represented (U.S. Census Bureau, 2013). They did not reflect the community demographics of PLWHA, which are approximately 44% Black/African American, 33% white, 19% Latino, and just over 3% for all other demographic categories (CDC, 2012). Although it is unclear how respondent demographics correspond with the demographics of ASO staff members nationally and in the tri-state area, respondents were more diverse than the current general population workforce profile (Bureau of Labor Statistics, U.S. Department of Labor, 2012). Additionally, there was a higher rate of missing data when we asked respondents about interest in cancer-related activities that they were not currently providing, suggesting some caution in interpreting these findings.
As the present Collaboration indicates, community-academic research partnerships hold much potential to explore resonant training and technical assistance methods that will enhance the abilities of ASOs of all sizes to bring cancer-related programming to their clients. We have begun to use the results of this tri-state needs assessment to create other cancer-focused education programs for ASOs that are focusing on primary prevention, including a tobacco cessation intervention and training program and a program of training ASO staff on helping to refer clients to clinical trials sponsored by the AIDS Malignancy Consortium.
Acknowledgments
This research was supported by a grant from the National Cancer Institute (3U54CA137788-02S1).
The authors wish to thank the members of the HIV/AIDS and Cancer Community Research Collaboration Community Advisory Board and the HIV/AIDS service organization staff members who participated in this study. We wish to acknowledge the assistance of Christopher Webster in the preparation of the manuscript.
Contributor Information
John A. Guidry, Gay Men’s Health Crisis
Erica I. Lubetkin, Sophie Davis School of Biomedical Education, City College of New York
Geoffrey W. Corner, Department of Psychiatry & Behavioral Sciences, Memorial Sloan-Kettering Cancer Center
Jennifer Lord-Bessen, Department of Psychiatry & Behavioral Sciences, Memorial Sloan-Kettering Cancer Center
Mark Kornegay, Gay Men’s Health Crisis.
Jack E. Burkhalter, Department of Psychiatry & Behavioral Sciences, Memorial Sloan-Kettering Cancer Center
References
- Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: A collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnet F, Burty C, Lewden C, Costagliola D, May T, Bouteloup V, Morlat P. Changes in cancer mortality among HIV-infected patients: The Mortalité 2005 Survey. Clinical Infectious Diseases. 2009;48:633–639. doi: 10.1086/596766. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics U.S. Department of Labor. Occupational Outlook Handbook, 2012–2013 Edition, Projections Overview. 2012 Retrieved October 23, 2013 from http://www.bls.gov/ooh/about/projections-overview.htm.
- Burkhalter JE, Cahill S, Shuk E, Guidry J, Corner G, Berk A, Lubetkin E. At the intersection of HIV/AIDS and cancer: A qualitative needs assessment of community-based HIV/AIDS service organizations. Health Education & Behavior. 2013;40:493–503. doi: 10.1177/1090198112459049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report 2005: Cases of HIV infection and AIDS in the United States and dependent areas. 2007 Retrieved from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/pdf/2005SurveillanceReport.pdf.
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report. 2012 Retrieved February 18, 2013, from http://www.cdc.gov/hiv/pdf/statistics_2011_HIV_Surveillance_Report_vol_23.pdf.
- Centers for Disease Control and Prevention. Diagnosed HIV infection among adults and adolescents in metropolitan statistical areas—United States and Puerto Rico, 2011. HIV Surveillance Supplemental Report. 2013;18(8) http://www.cdc.gov/hiv/library/reports/surveillance. [Google Scholar]
- Detels R, Muñoz A, McFarlane G, Kingsley LA, Margolick JB, Giorgi J, Phair JP. Effectiveness of potent antiretro-viral therapy on time to AIDS and death in men with known HIV infection duration. Journal of the American Medical Association. 1998;280:1497–1503. doi: 10.1001/jama.280.17.1497. [DOI] [PubMed] [Google Scholar]
- Effros RB, Fletcher CV, Gebo K, Halter JB, Hazzard WR, Horne FM, High KP. Aging and infectious diseases: Workshop on HIV infection and aging: What is known and future research directions. Clinical Infectious Diseases. 2008;47:542–553. doi: 10.1086/590150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emlet CA, Gerkin A, Orel N. The graying of HIV/AIDS: Preparedness and needs of the aging network in a changing epidemic. Journal of Gerontological Social Work. 2009;52:803–814. doi: 10.1080/01634370903202900. [DOI] [PubMed] [Google Scholar]
- Engels EA, Biggar RJ, Hall HI, Cross H, Crutchfield A, Finch JL, Goedert JJ. Cancer risk in people infected with human immunodeficiency virus in the United States. International Journal of Cancer. 2008;123:187–194. doi: 10.1002/ijc.23487. [DOI] [PubMed] [Google Scholar]
- Finifter DH, Jensen CJ, Wilson CE, Koenig BL. A comprehensive, multitiered, targeted community needs assessment model: Methodology, dissemination, and implementation. Family and Community Health. 2005;28:293–306. doi: 10.1097/00003727-200510000-00003. [DOI] [PubMed] [Google Scholar]
- Freeman K, Zonszein J, Islam N, Blank AE, Strelnick AH. Mortality trends and disparities among racial/ethnic and sex subgroups in New York City, 1990 to 2000. Journal of Immigrant and Minority Health. 2011;13:546–554. doi: 10.1007/s10903-010-9345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpati AM, Bassett MT, McCord C. Neighbourhood mortality inequalities in New York City, 1989–1991 and 1999–2001. Journal of Epidemiology and Community Health. 2006;60:1060–1064. doi: 10.1136/jech.2006.047100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwait J, Valente TW, Celentano DD. Interorganizational relationships among HIV/AIDS service organizations in Baltimore: a network analysis. Journal of Urban Health. 2001;78:468–487. doi: 10.1093/jurban/78.3.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin CP, Fain MJ, Klotz SA. The older HIV-positive adult: A critical review of the medical literature. American Journal of Medicine. 2008;121:1032–1037. doi: 10.1016/j.amjmed.2008.08.009. [DOI] [PubMed] [Google Scholar]
- Mayberry RM, Daniels P, Yancey EM, Akintobi TH, Berry J, Clark N, Dawaghreh A. Enhancing community-based organizations’ capacity for HIV/ AIDS education and prevention. Evaluation and Program Planning. 2009;32:213–220. doi: 10.1016/j.evalprogplan.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels M, Weiss ES, Guidry JA, Blakeney N, Swords L, Gibbs B, Patel S. The promise of community-based advocacy and education efforts for increasing cancer clinical trials accrual. Journal of Cancer Education. 2012;27:67–74. doi: 10.1007/s13187-011-0271-6. [DOI] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene. HIV Epidemiology and Field Services Program Semiannual Report: Covering January 1 2009_ December 31, 2009. 2010 Oct; Retrieved from http://www.nyc.gov/html/doh/downloads/pdf/dires/2010_2nd_semi_rpt.pdf.
- Orel N. Community needs assessment: Documenting the need for affirmative services for LGB older adults. In: Kimmel DC, Rose T, David S, editors. Lesbian, gay, bisexual, and transgender aging: Research and clinical perspectives. New York: Columbia University Press; 2006. pp. 227–246. [Google Scholar]
- Palella FJ, Jr, Baker RK, Moorman AC, Chmiel JS, Wood KC, Brooks JT, Holmberg SD. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. Journal of Acquired Immune Deficiency Syndromes. 2006;43:27–34. doi: 10.1097/01.qai.0000233310.90484.16. [DOI] [PubMed] [Google Scholar]
- Patel P, Hanson DL, Sullivan PS, Novak RM, Moorman AC, Tong TC, Brooks JT. Incidence of types of cancer among HIV-infected persons compared with the general population in the United States, 1992–2003. Annals of Internal Medicine. 2008;148:728–736. doi: 10.7326/0003-4819-148-10-200805200-00005. [DOI] [PubMed] [Google Scholar]
- Shiels MS, Pfeiffer RM, Gail MH, Hall HI, Li J, Chaturvedi AK, Engels EA. Cancer burden in the HIV-infected population in the United States. Journal of the National Cancer Institute. 2011;103:753–762. doi: 10.1093/jnci/djr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverberg MJ, Abrams DI. AIDS-defining and non-AIDS-defining malignancies: Cancer occurrence in the antiretroviral therapy era. Current Opinion in Oncology. 2007;19:446–451. doi: 10.1097/CCO.0b013e3282c8c90d. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. State and County QuickFacts. 2013 Last Revised: Thursday, 27-Jun-2013 Retrieved October 21, 2013, from http://quickfacts.census.gov/qfd/states/00000.html.
- Valdiserri R. CDC launches enhanced comprehensive HIV prevention planning (ECHPP) web page. 2011 Jul 20; Retrieved from http://blog.aids.gov/2011/07/cdc-launches-enhanced-comprehensive-hiv-prevention-planning-echpp-web-page.html.