Abstract
Objective:
To determine whether subjective memory complaints (SMCs) are associated with performance on objective cognitive measures and psychological factors in healthy, community-dwelling older adults.
Method:
The cohort was composed of adults, 65 years and older with no clinical evidence of cognitive impairment (n = 125). Participants were administered: CogState computerized neurocognitive battery, Prospective Retrospective Memory Questionnaire, personality and meaning-in-life measures.
Results:
SMCs were associated with poorer performance on measures of executive function (p = 0.001). SMCs were also associated with impaired delayed recall (p = 0.006) but this did not remain significant after statistical adjustment for multiple comparisons. SMCs were inversely associated with conscientiousness (p = 0.004) and directly associated with neuroticism (p < 0.001). Higher scores on SMCs were associated with higher perceived stress (p = 0.001), and ineffective coping styles (p = 0.001). Factors contributing to meaning-in-life were associated with fewer SMCs (p < 0.05).
Conclusions:
SMCs may reflect early, subtle cognitive changes and are associated with personality traits and meaning-in-life in healthy, older adults.
Keywords: subjective memory complaints, cognitive performance, meaning-in-life, healthy, older adults, personality traits
Introduction
The field of Alzheimer’s disease (AD) is advancing toward earlier detection and diagnosis of the disease. Ultimately, the goal is to identify individuals who are asymptomatic but at risk of developing AD. Subjective memory complaints (SMCs) represent a type of complaint made by individuals with cognitive symptoms or complaints but no clear impairment on objective psychometric testing. Evidence suggests that individuals with SMCs may be at increased risk of dementia, with several studies showing that patients with cognitive complaints have a higher rate of progression to mild cognitive impairment (MCI) or AD than those without. 1 –4 Studies have also reported that, compared to those without cognitive complaints, individuals with SMCs show greater medial temporal lobe atrophy, 5 –8 regional brain hypometabolism, 9 higher prevalence of an AD-like cerebrospinal fluid profile, 10 and more frequent AD pathology at autopsy. 11 As such, SMCs may be a “pre-MCI” stage in the evolution of normal aging to clinical AD and might represent a potential target for intervention trials.
Despite the burgeoning interest, there is still little research on the association between SMCs and cognitive performance in otherwise still healthy, community-dwelling older adults. Although it is generally assumed that individuals with SMCs have relative deficiencies in memory, the extent to which memory complaints reflect a decline in other cognitive domains such as attention, language, and executive function is not established. By definition, individuals with SMCs perform within the “normal range” on standard psychometric measures, although the individuals themselves, close family or friends, report subtle decline in cognitive abilities. The dissociation between patients’ self-assessment and clinical testing may be due to several factors, including lack of sensitivity of psychometric measures, limited sample size, demographics (eg, education), lack of insight, psychiatric symptoms, or personality traits. Standard psychometric tests have poor resolution, particularly in detecting subtle cognitive changes in very early AD. 12 –15 Cognitive reserve factors, such as education level, have also been implicated to account for the discrepancy between subjective complaints and objective cognitive performance, such that individuals with higher education levels can cope longer before manifesting cognitive deficits. 16 Although some studies suggest that negative emotional states and personality traits can also contribute to the dissociation, 17 –19 these studies are limited, with mixed results. 20
The first goal of the present study was to examine the relationship between SMCs and objective cognitive performance using a computerized cognitive battery, with demonstrated sensitivity to subtle changes in cognitive function. 21 –24 We examined a cohort of healthy, community-dwelling older adults with SMCs using this cognitive battery to determine the nature of cognitive deficits in individuals with subjective complaints. The second goal was to examine the association of SMCs with meaning-in-life and personality traits, not as yet reported in the literature, as well as negative emotional states and stress. It was hypothesized that SMCs would be associated with negative emotional states (eg, anxiety and depression), personality traits (eg, neuroticism and conscientiousness), stress, and elements of the meaning-in-life.
Methods
Participants
The population consisted of older adults without clinical evidence of cognitive impairment who consented to participate in a longitudinal study of 3 years duration with visits occurring annually. The participants met the following eligibility criteria: (1) age 65 years or older; (2) no clinical evidence of cognitive impairment on a measure of global cognitive functioning Montreal Cognitive Assessment (26-30) 25 ; and (3) no acute or serious medical conditions. Participants were recruited for this baseline visit by the University of Pennsylvania Alzheimer’s Disease Center from its “normal control” cohort and in outreach efforts to a suburban residential setting for independent living, from an Older Adult Registry for African Americans interested in research participation, and other community-dwelling individuals in the greater Philadelphia area. The study population was administered the prescreening Telephone Interview for Cognitive Status to eliminate potential participants who clearly did not meet the protocol requirements. Those with scores >28 were eligible as per established norms for definitely (range 33-41) and probably nonimpaired (range 26-32). 26 The mean for our population was 35 (standard deviation [SD] = 2.6; range 28-41). The review of medical conditions revealed a multitude of age-related illnesses, controlled by treatment and not exclusionary. One individual had significant Parkinson’s disease that precluded writing, and another was undergoing chemotherapy that affected mental clarity. A total of 150 potential participants were approached and screened; of these, 10 withdrew, 12 declined, and 3 did not meet the eligibility criteria. The final sample was 125. There were no significant differences in age, gender, education, or race between the participants and the nonparticipants. The mean age of the cohort was 77 (SD = 7.2; range 65-95). The mean years of education was 16 (SD = 2.8; range 6-20). Women constituted 66% of the sample. The racial distribution was African American: 24% and caucasian: 76% (Table 1). The University of Pennsylvania institutional review board approved the study, and all participants provided informed consent.
Table 1.
Characteristics of the Population (N = 125).
| Characteristic | Number (%) |
|---|---|
| Age, years | |
| 65-74 | 53 (42) |
| 75-84 | 49 (39) |
| 85-95 | 23 (18) |
| Gender | |
| Male | 46 (34) |
| Female | 89 (66) |
| Education, years | |
| ≤12 | 30 (22) |
| 13-17 | 58 (43) |
| >18 | 47 (35) |
| Highest level of occupation | |
| Professionals and technical workers | 73 (57) |
| Managers/administrators, clerical, sales | 45 (35) |
| Operative, service workers | 3 (2) |
| Craftsmen and foremen | 3 (3) |
| Race | |
| Caucasian | 95 (76) |
| African American | 30 (24) |
| Marital status | |
| Married | 73 (54) |
| Widowed | 32 (23) |
| Single, never married | 11 (8) |
| Divorced | 20 (15) |
| Residence | |
| Suburban independent senior living | 52 (42) |
| Urban community residence | 73 (58) |
| Body mass index | |
| Underweight <18.5 | 8 (6) |
| Normal weight 18.5-24.9 | 34 (27) |
| Overweight 25-29.9 | 44 (35) |
| Class I obesity 30-34.9 | 27 (21) |
| Class II obesity 35-39.9 | 5 (4) |
| Class III obesity 40 plus | 9 (7) |
| Tobacco history | |
| Never smoked | 11 (8) |
| Current smoker | 50 (37) |
| Former smoker | 73 (55) |
| Tobacco consumption >1 pack/d | 62 (46) |
| Duration of smoking ≥20 years | 47 (35) |
| Alcohol history | |
| Current drinker | 43 (39) |
| Former drinker | 66 (61) |
| Alcohol consumption ≥3 drinks/d | 7 (11) |
| Duration of drinking ≥20 years | 30 (28) |
Procedures
Subjective Memory Complaints
The SMCs were evaluated with the Prospective Retrospective Memory Questionnaire (PRMQ). 27 The PRMQ contains 16 questions. Participants rated how often each thing happened using a 5-point scale, ranging from (1) never to (5) very often. The minimum score is 16, and the maximum 80. Higher scores on the PRMQ indicate more SMCs. The PRMQ is a measure of self-reported minor memory problems tested in the general population (ages 17-94) for which the reliability and concurrent and predictive validity have been established The mean for the PRMQ is 38.88 (SD = 9.15; range 17-67) for the general adult population aged 18 to 93. 28
Cognitive Testing
The CogState computerized tests have been shown to be valid, reliable, and sensitive to cognitive impairment. 21 –24 Participants were administered the following CogState tests by the trained Geriatric Psychiatrist (SS) over a 35-minute period: Detection task (psychomotor speed), Identification task (attention), One Card Learning task (visual recognition memory), One Back (working memory), Two Back (working memory), Continuous-Paired Associate Learning (CPAL; paired associate learning) task, Groton Maze Learning task (GMLT; executive function), and International Shopping List task (ISLT; verbal learning and memory). The CogState normative data relevant to our findings are as follows. The mean for the GMLT for those 65 to 74 is 64.98 (SD 25.93); for those 75 to 84 is 72.11 (SD 29.01), and for those 85 to 95 is 77.20 (SD 11.54). The mean for the ISLT-delayed age group 65 to 74 is 8.80 (SD 1.94) and for those 75 to 84 is 7.47 (SD 2.57). Histograms were drawn for each outcome variable. Outliers that were 2 or more SDs from the mean were not included in the analysis (1 participant for CPAL and 1 participant for GMLT). Four participants had missing data for ISLT and were removed from the analysis for this task.
Personality Traits
The NEO-Five Factor Inventory assessed 5 dimensions of personality (neuroticism, extraversion, openness, agreeableness, and conscientiousness). Each trait measured the degree individuals agreed with 12 statements rated on a 5-point scale ranging from 0 to 4, with higher scores indicating more of the trait in question. Item scores were summed to yield trait scores that could range from 0 to 48. The psychometric properties of this scale have been extensively documented. 29 Personality traits have been associated with cognitive performance, and our goal was to determine whether they were also associated with SMCs.
Psychological Stress
Psychological distress was assessed using the stress subscale Depression, Anxiety, and Stress Scale (DASS), 30 adaptive and destructive coping styles (Brief Cope), 31 and appraisal of stressful events (Perceived Stress Scale). 32 The mean for the DASS stress subscale from a normative sample between age 50 to 59 was 8.20 (SD 8.64). 33
Mood Measures
The 15-item version Geriatric Depression Scale (GDS) 34 was administered with a cut point of ≥5 suggesting depression. The mean for the DASS depression subscale for a normative sample was 5.28 (SD = 7.80) and DASS anxiety subscale 3.55 (SD = 5.39).
Meaning-in-Life
The Distress Cognition Study Measure 35 measures factors contributing to meaning-in-life (eg, purpose, values, goals, reconciliation with the past, and emotional support) as well as negative interpersonal interactions and recent financial stress. Each factor is measured by the degree to which individuals agreed with the statements rated on a 4-point scale ranging from 1 to 4, with higher scores indicating stronger agreement. Greater meaning-in-life has been associated with reduced risk of MCI and AD in community-dwelling older persons. 36 Our goal was to investigate a possible association between meaning-in-life and SMCs.
Statistical Analysis
Given the sample of 125 participants, and the following assumptions: type I, α, error of 5% and 2-sided tests, this study has 80% power to detect an effect size of 0.25 SD units for continuous covariates. Descriptive statistics were used to characterize the study population. To identify factors associated with cognitive performance, multivariable linear regression models were developed. In linear regression models that adjusted for age, sex, education, race, and multiple comparisons, the PRMQ was entered a an outcome variable, and the CogState tests, personality traits, and psychological stress, mood, and meaning-in-life measures entered as independent variables. Table 2 represents a distinct linear model, with each row representing the association between the outcome measure (PRMQ) and each of the independent variables (eg, CogState subtest). All analyses were performed using Stata Version 12 (StatCorp, College Station, Texas) with 2-tailed tests and a type I error of 0.05.
Table 2.
Subjective Memory Complaints and Their Associations With Cognitive Performance (N = 125).a
| CogState Subtest | Coefficient | Standard Error | R 2 | 95% Confidence Interval | P |
|---|---|---|---|---|---|
| Executive function | 0.098 | 0.028 | .0964 | 0.043 to 0.153 | .001 b |
| Verbal memory immediate | 0.209 | 0.135 | .0199 | −0.477 to 0.593 | .13 |
| Verbal memory delay recall | 0.927 | 0.329 | .0633 | −1.599 to −0.274 | .006 |
| Paired associate learning | 5.380 | 5.576 | .0079 | −5.663 to 16.423 | .33 |
| Detection task | 1.252 | 2.235 | .0027 | −3.176 to 5.679 | .57 |
| Identification task | 1.392 | 3.064 | .0018 | −4.677 to 7.461 | .45 |
| One Back | −1.800 | 3.123 | .0028 | −7.986 to 4.384 | .57 |
| Two Back | 0.405 | 3.746 | .0001 | −7.014 to 7.825 | .91 |
| One Card Learning task | −6.042 | 5.602 | .0098 | −17.138 to 5.054 | .28 |
a Subjective memory complaints are measured by the Prospective Retrospective Memory Questionnaire (PRMQ). Objective Cognitive Performance was measured using the CogState a computerized neurocognitive battery of tests. Performance was calculated for Executive Function by totaling the errors and for Verbal Memory by totaling the number of correct responses. Each row represents a distinct linear regression analysis with 1 outcome and 1 independent variable. Errors in executive function increased as subjective memory complaints increased. Delayed recall on verbal memory (International Shopping List task) declined with higher scores on the PRMQ. No other significant associations were found for the following administered tests: working memory (One Back and Two Back), continuous paired associate learning, the detection task for psychomotor speed, the 1 card learning task for visual recognition memory, and identification for attention.
b Statistically significant after adjustment for multiple comparisons using a Bonferroni adjustment of 0.05/9 = 0.005 as the threshold for significance.
Results
Characteristics of the Study Population
There were 125 participants in the study. The mean age of the cohort was 77 (SD = 7.2; range 65-95). The mean years of education was 16 (SD = 2.8; range 6-20). The majority were women and married. Most participants engaged in occupations of high mental demands. The racial distribution reflects the population in the Delaware Valley (African American: 24% and caucasian: 76%). The mean number of years of education was significantly higher for caucasians than African Americans (15.9, 14.2, t = 2.98, degrees of freedom (df) = 123; P = .004.) Yet, there were no statistically significant differences by race in their cognitive performance on the CogState tests associated with SMCs, executive function (14, 16.5, t = −1.63, df = 117, P = .107), or delayed verbal memory (7.79, 7.72, t = 1.073, df = 117, P = .286). The participants were health conscious being former smokers and former drinkers with a mean body mass index of 28.5 in the overweight but not obese class (SD = 6.2; range 18-58; Table 1).
Subjective Memory Complaints and Their Associations
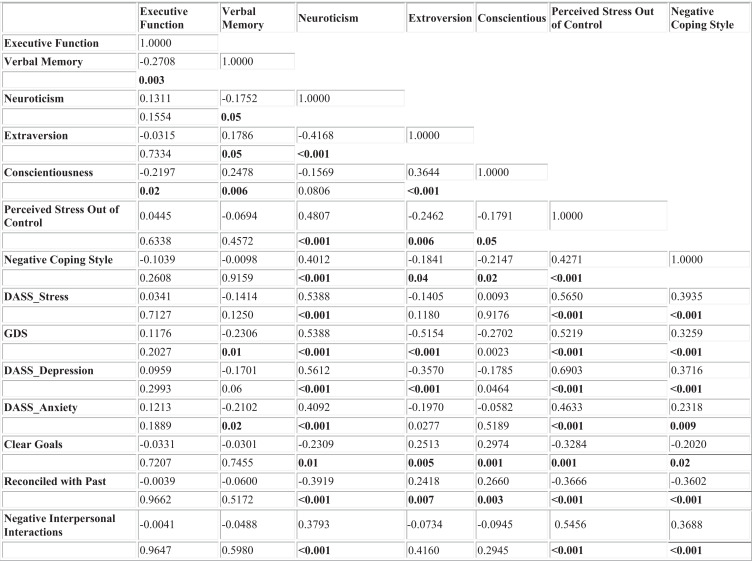
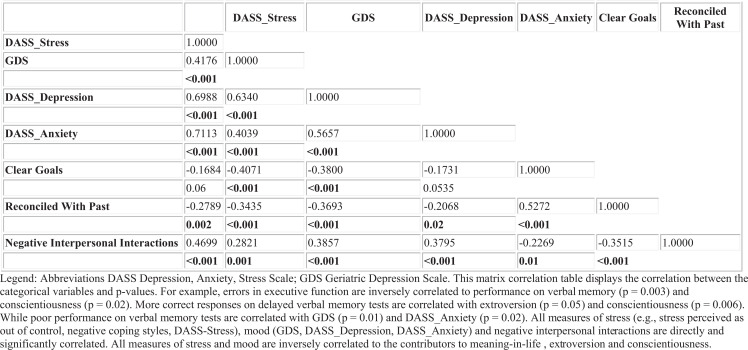
The mean score on the PRMQ in our population was 36 (SD = 8.8; range 20-69) similar to that in the literature. 36 The mean scores on the GMLT and the ISLT delayed were also similar to that reported by CogState. Table 3 displays the mean, SD, and range for each categorical variable significantly associated with SMCs. The Pearson’s correlation table for continuous variables in Appendix A corroborates the associations revealed by the regression models.
Table 3.
Descriptive Statistics for Categorical Variables Significantly Associated With the PRMQ (N = 125).
| Variables | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|
| CogState | ||||
| Executive Function | 82.647 | 27.874 | 37 | 218 |
| Verbal Memory Delayed | 7.655 | 2.392 | 2 | 12 |
| Personality traits | ||||
| Neuroticism | 16.232 | 7.533 | 0 | 40 |
| Extraversion | 28.032 | 5.982 | 12 | 46 |
| Conscientiousness | 35.352 | 5.229 | 21 | 47 |
| Psychological stress | ||||
| Perceived stress: out of control | 7.902 | 4.951 | 0 | 21 |
| Negative coping style | 13.216 | 2.884 | 9 | 21 |
| DASS: stress | 6.552 | 6.716 | 0 | 35 |
| Mood measures | ||||
| Geriatric Depression Scale | 2.456 | 2.529 | 0 | 12 |
| DASS: depression | 4.36 | 5.692 | 0 | 28 |
| DASS: anxiety | 3.128 | 4.096 | 0 | 23 |
| Meaning-in-Life | ||||
| Clear goals | 9.2 | 2.345 | 0 | 12 |
| Reconciled with the past | 13 | 2.609 | 0 | 16 |
| Negative interpersonal interaction | 11.952 | 3.377 | 7 | 23 |
Abbreviations: DASS, Depression, Anxiety, and Stress Scale; PRMQ, Prospective Retrospective Memory Questionnaire.
Subjective Memory Complaints and Cognitive Performance
As Table 2 indicates, although higher scores on the PRMQ are significantly correlated with poor performance on memory measures, such as verbal memory delayed recall, a significant association beyond the memory domain was also observed for executive function.
Subjective Memory Complaints, Cognitive Performance Personality Traits
Subjective memory complaints were also significantly associated with personality traits, where higher PRMQ scores were related to lower scores on extraversion, conscientiousness, and higher scores on neuroticism (Table 4).
We also compared performance on CogState measures to personality traits. Significant associations were observed for GMLT (executive function), where more errors were related to higher scores on neuroticism (coefficient 0.594; standard error 0.284, 95% confidence interval [CI] 0.031 to 1.157; P = .04). Furthermore, greater accuracy on the ISLT (verbal memory) was associated with extroversion (coefficient 0.081; standard error 0.037, 95% CI 0.006 to 0.156; P = .03) and conscientiousness (coefficient 0.133; standard error 0.042, 95% CI 0.049 to 0.217; P = .002).
Subjective Memory Complaints, Cognitive Performance, Psychological Stress, Mood Measures, and Meaning-in-Life
Higher PRMQ scores were associated with higher scores on all measures of stress, stress perceived as out of control, negative coping style, and the DASS stress subscale. Higher PRMQ scores were also associated with subclinical depression and anxiety as measured by the DASS subscales and the GDS. It is noteworthy that our population had lower mean scores on the DASS subscales than the normative sample (Table 3). The GDS scores were well below the cut point of ≥5. Yet the associations persist.
Clear goals and being reconciled with the past were associated with lower PRMQ scores, whereas negative interpersonal relations were associated with higher scores (Table 4).
Table 4.
Subjective Memory Complaints and Their Associations With Personality Traits, Psychological Stress, Mood Measures, and Meaning-in-Life (N = 125).
| Coefficient | Standard Error | R 2 | 95% Confidence Interval | P | |
|---|---|---|---|---|---|
| Personality traits | |||||
| Neuroticism | 0.506 | 0.099 | .1686 | 0.310 to 0.701 | <.001 b |
| Extraversion | −0.471 | 0.130 | .1123 | −0.729 to −0.213 | <.001 b |
| Conscientiousness | −0.449 | 0.151 | .0653 | −0.749 to 0.149 | .004 b |
| Openness | 0.006 | 0.138 | .0000 | −0.267 to 0.278 | .967 |
| Agreeableness | 0.011 | 0.163 | .0000 | −0.31 to 0.333 | .947 |
| Psychological stress | |||||
| Perceived stress: out of control | 0.552 | 0.159 | .1084 | 0.236 to 0.869 | <.001 b |
| Negative coping style | 0.849 | 0.264 | .0776 | 0.327 to 1.371 | .002 b |
| DASS: stress | 0.418 | 0.111 | .1019 | 0.196 to 0.639 | <.001 b |
| Mood measures | |||||
| Geriatric Depression Scale | 1.216 | 0.201 | .1359 | 0.821 to 1.611 | <.001 b |
| DASS: depression | 0.489 | 0.137 | .1088 | 0.218 to 0.760 | <.001 b |
| DASS: anxiety | 0.757 | 0.188 | .1019 | 0.385 to 1.129 | <.001 b |
| Meaning-in-life | |||||
| Clear goals | −0.858 | 0.341 | .6742 | −1.532 to −0.184 | .01 |
| Reconciled with the past | −1.195 | 0.295 | .3345 | −1.78 to −0.612 | <.001 b |
| Negative interpersonal score | 0.814 | 0.231 | .0449 | 0.357 to 1.272 | .001 b |
| Acknowledged value system | −0.499 | 0.371 | .0145 | −1.234 to 0.236 | .182 |
| Sense of purpose | −0.488 | 0.266 | .0266 | −1.016 to 0.039 | .069 |
| Emotional support | −0.401 | 0.249 | .0207 | −0.895 to 0.092 | .110 |
Abbreviations: DASS, Depression, Anxiety, and Stress Scale; PRMQ, Prospective Retrospective Memory Questionnaire.
a Each row represents a distinct linear regression analysis with 1 outcome and 1 independent variable (eg, total score of the PRMQ and neuroticism domain score). Subjective memory complaints (SMCs) were significantly and inversely associated with extraversion and conscientiousness and directly associated with neuroticism. The greater the number of SMCs, the higher the scores on stress perceived as out of control and negative coping style, stress levels, and mood. Factors contributing to purpose in life such as clear goals and being reconciled with the past were associated with fewer subjective memory complaints, whereas negative interpersonal relations were associated with more SMCs.
b The specific result within each domain (personality trait, psychological stress, etc) was statistically significant after adjustment for multiple comparisons. Adjustments were made using a Bonferroni method with 0.05/n, where n is the number of comparisons within each domain, as the threshold for significance.
Associations were also observed between mood measures and CogState tasks. For example, a greater number of errors on the GMLT were associated with higher scores on the DASS depression subscale (coefficient 1.112; standard error 0.478, 95% CI 0.165 to 2.058; P = .02), the DASS anxiety (coefficient 1.988; standard error 0.585; 95% CI 0.828 to 3.148; P = .001), and the GDS (coefficient 2.791; standard error 0.973; 95% CI 0.864 to 4.717; P = .005). In addition, decreased accuracy on the ISLT was associated with higher scores on the DASS depression subscale (coefficient −0.273; standard error 0.103; 95% CI −0.478 to −0.068; P = .009) and the GDS (coefficient −0.495; standard error 0.225; 95% CI −0.941 to −0.048; P = .03).
Discussion
Results of this study support our first hypothesis that lower PRMQ scores would be associated with better cognitive test scores. Additionally, higher PRMQ scores were related to poorer performance on memory and executive function tasks. Our second hypothesis was that SMCs would be associated with negative emotional states (eg, anxiety and depression), personality traits (eg, neuroticism and conscientiousness), stress, and the elements of the meaning-in-life. Higher scores on SMCs were associated with the personality trait of neuroticism, subclinical levels of anxiety and depression, greater levels of stress, destructive coping styles, perceiving stress as unmanageable, and more frequent negative interpersonal interactions. Fewer SMCs were associated with the personality traits of extroversion and conscientiousness and certain elements contributing to meaning-in-life (eg, being reconciled with the past and clear goals). Our findings are concordant with previous work involving older adults, which report more SMCs in participants with stress, anxiety, and depression. 37 –39 To the best of our knowledge, this is the first investigation examining the relationship between SMCs, meaning-in-life, and personality traits.
Further, understanding of the variables associated with SMCs may guide early identification of cognitive change and the institution of interventions for maintaining cognitive resilience. Such interventions might include (1) cognitive fitness training; (2) stress management for destructive coping styles and developing realistic perceptions; and (3) cognitive behavioral therapy focused on issues of adults in late life (eg, establishing clear goals, reconciling with the past, subclinical anxiety, and depression). Researchers have identified effective strategies for cognitive training. The Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study examined the impact of cognitive training (memory, reasoning, and processing speed) in healthy older individuals and found persisting benefits, especially on reasoning, an executive function. 33 Cognitive exercises were effective when computer based and administered at home.
In general, older adults do not seek help for SMCs. 40 Those seeking help may be turned away by health providers when formal neurocognitive tests report no impairment. In either case, older adults have a reduced opportunity to receive early intervention. We argue that measures used in this study would help in the identification of preclinical MCI individuals, particularly a self-report scale measuring SMCs in conjunction with brief measures of cognition, mood, and meaning-in-life.
The strength of this research is that it reports baseline data of an ongoing longitudinal study of community-dwelling adults in late life that continues into its third year. The focus is on personality, psychological distress, and mood that promote cognitive and functional resilience. It establishes and extends our knowledge of the associations of SMCs with personality traits and meaning-in-life. It highlights the significance of SMCs with respect to cognitive performance and general quality of life.
Some limitations should be considered in interpreting our results as well. This is a relatively small sample of well-educated, professionally successful, reasonably healthy participants with a greater involvement of woman and caucasians. The problem with generalizability was compensated for by nonrestrictive eligibility criteria and statistical adjustment for potential confounders. Selection bias is another potential limitation because the sample consisted of those who agreed to participate and had complete information. However, there was a low level of loss to follow-up, which was nondifferential across sites observed as the study continued.
In sum, SMCs were found to be associated with cognitive function (episodic memory and executive function), personality traits (neuroticism, extraversion, and conscientiousness), psychological stress (ie, stress perceived as unmanageable and negative coping style), mood (subclinical depression and anxiety), and meaning-in-life (ie, clear goals and reconciled with the past). These findings suggest the utility of a self-report scale measuring SMCs in conjunction with brief measures of cognition, mood, and meaning-in-life. This approach, neither costly nor labor intensive, will permit health care professionals to identify seniors vulnerable to changes in cognitive performance. Older adults could be assisted in instituting lifestyle changes (eg, cognitive training exercises, stress management, and brief cognitive behavior therapy focused on issues of adults in late life). For such benefits to be derived, however, an effort to increase awareness of the value of measuring SMCs among both practitioners and patients will be required.
Appendix A
Pearson’s Correlation and P values for Continuous Variables.
Footnotes
Authors’ Note: Susanne I. Steinberg and Selamawit Negash are the cofirst authors. The article was previously presented at the Alzheimer’s Association International Conference(Predictors of Resilient Cognitive Aging: Baseline Characteristics); Hawaii, USA; July 16-21, 2011 by Susanne I. Steinberg, Melissa G. Livney, Mitch A. Kling, Hannah McCoubrey, Stephanie Yuen, Carol Edwards, Natalia Louneva, Sharon Xie, and Steven E. Arnold; and at the Alzheimer’s Association International Conference (Factors Associated with Cognitive Resilience in Late Life: A Three Sample Comparison); Paris, France; July 14-19, 2012 by Susanne I. Steinberg, Mary D. Sammel, Melissa G. Livney, Mitch A. Kling, Hannah McCoubrey, Stephanie Yuen, and Steven E. Arnold.
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Steven E. Arnold has board memberships with Teva and Bristol Myers Squibb. He presently does consultancy work for Pain Therapeutics. He has also received payment for lectures including service on speaker’s bureaus for Rush University Medical Center, Trinitas Regional Medical Center, and University of Puerto Rico. Brian Harel is a full-time employee of CogState, the company that provided the cognitive tests used in the study. Mary Sammel provided consultant services for Swiss Precision Diagnostics GmbH.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Steven E. Arnold, MD, has grant funding paid to the University of Pennsylvania from NIH for R01AG03947802, ADC NIH/NIA P30-AG010124, American Health Assistance Foundation for A2012116, University of Southern California-San Diego for UCSDCT and 22 UPENN-RES and Marian S. Ware Alzheimer's Program as well as Bristol Myers Squibb, Eli Lilly, Neuronetrix, Merck, Pfizer, and Johnson & Johnson. Susanne Steinberg, MD, MSCE, had a NRSA Postdoctoral Fellowship (217703) from the training grant NIH T32-MH019931.
References
- 1. Jessen F, Wiese B, Bachmann C, et al. Prediction of dementia by subjective memory impairment effects of severity and temporal association with cognitive impairment. Arch Gen Psychiatry. 2010;67(4):414–422. [DOI] [PubMed] [Google Scholar]
- 2. Stewart R, Godin O, Crivello F, et al. Longitudinal neuroimaging correlates of subjective memory impairment: 4-year prospective community study. Br J Psychiatry. 2011;198(3):199–205. [DOI] [PubMed] [Google Scholar]
- 3. Glodzik-Sobanska L, Reisberg B, De Santi S, et al. Subjective memory complaints: presence, severity and future outcome in normal older subjects. Dement Geriatr Cogn Disord. 2007;24(3):177–184. [DOI] [PubMed] [Google Scholar]
- 4. Dickerson BC, Sperling RA, Hyman BT, Albert MS, Blacker D. Clinical prediction of Alzheimer disease dementia across the spectrum of mild cognitive impairment. Arch Gen Psychiatry. 2007;64(12):1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saykin AJ, Wishart HA, Rabin LA, et al. Older adults with cognitive complaints show brain atrophy similar to that of amnestic MCI. Neurology. 2006;67(5):834–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tepest R, Wang L, Csernansky JG, et al. Hippocampal surface analysis in subjective memory impairment, mild cognitive impairment and Alzheimer's dementia. Dement Geriatr Cogn Disord. 2008;26(4):323–329. [DOI] [PubMed] [Google Scholar]
- 7. Striepens N, Scheef L, Wind A, et al. Volume loss of the medial temporal lobe structures in subjective memory impairment. Dement Geriatr Cogn Disord. 2010;29(1):75–81. [DOI] [PubMed] [Google Scholar]
- 8. Stewart R, Dufouil C, Godin O, et al. Neuroimaging correlates of subjective memory deficits in a community population. Neurology. 2008;70(18):1601–1607. [DOI] [PubMed] [Google Scholar]
- 9. Mosconi L, De Santi S, Brys M, et al. Hypometabolism and altered cerebrospinal fluid markers in normal apolipoprotein E E4 carriers with subjective memory complaints. Biol Psychiatry. 2008;63(6):609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Visser PJ, Verhey F, Knol DL, et al. Prevalence and prognostic value of CSF markers of Alzheimer's disease pathology in patients with subjective cognitive impairment or mild cognitive impairment in the DESCRIPA study: a prospective cohort study. Lancet Neurol. 2009;8(7):619–627. [DOI] [PubMed] [Google Scholar]
- 11. Barnes LL, Schneider JA, Boyle PA, Bienias JL, Bennett DA. Memory complaints are related to Alzheimer disease pathology in older persons. Neurology. 2006;67(9):1581–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Knopman DS, Caselli RJ. Appraisal of cognition in preclinical Alzheimer's disease: a conceptual review. Neurodegener Dis Manag. 2012;2(2):183–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tractenberg RE, Pietrzak RH. Intra-individual variability in Alzheimer's disease and cognitive aging: definitions, context, and effect sizes. PLoS ONE. 2011;6(4):e16973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Auriacombe S, Helmer C, Amieva H, Berr C, Dubois B, Dartigues JF. Validity of the free and cued selective reminding test in predicting dementia: the 3C study. Neurology. 2010;74(22):1760–1767. [DOI] [PubMed] [Google Scholar]
- 15. Mohs RC, Knopman D, Petersen RC, et al. Development of cognitive instruments for use in clinical trials of antidementia drugs: additions to the Alzheimer's Disease Assessment Scale that broaden its scope. The Alzheimer's Disease Cooperative Study. Alzheimer Dis Assoc Disord. 1997;11(suppl 2):S13–S21. [PubMed] [Google Scholar]
- 16. van Oijen M, de Jong FJ, Hofman A, Koudstaal PJ, Breteler MM. Subjective memory complaints, education, and risk of Alzheimer's disease. Alzheimers Dement. 2007;3(2):92–97. [DOI] [PubMed] [Google Scholar]
- 17. Slavin MJ, Brodaty H, Kochan NA, et al. Prevalence and predictors of “subjective cognitive complaints” in the Sydney Memory and Ageing Study. Am J Geriatr Psychiatry. 2010;18(8):701–710. [DOI] [PubMed] [Google Scholar]
- 18. Derouesne C, Alperovitch A, Arvay N, et al. Memory complaints in the elderly: a study of 367 community-dwelling individuals from 50 to 80 years old. Arch Gerontol Geriatr Suppl. 1989;1:151–163. [PubMed] [Google Scholar]
- 19. Hanninen T, Reinikainen KJ, Helkala EL, et al. Subjective memory complaints and personality traits in normal elderly subjects. J Am Geriatr Soc. 1994;42(1):1–4. [DOI] [PubMed] [Google Scholar]
- 20. Potvin O, Bergua V, Meillon C, et al. State anxiety and cognitive functioning in older adults. Am J Geriatr Psychiatry. 2013;21(9):915–924. [DOI] [PubMed] [Google Scholar]
- 21. Maruff P, Thomas E, Cysique L, et al. Validity of the CogState brief battery: relationship to standardized tests and sensitivity to cognitive impairment in mild traumatic brain injury, schizophrenia and AIDS dementia complex. Arch Clin Neuropsychol. 2009;24(2):165–178. [DOI] [PubMed] [Google Scholar]
- 22. Papp KV, Snyder PJ, Maruff P, Bartkowiak J, Pietrzak RH. Detecting subtle changes in visuospatial executive function and learning in the amnestic variant of mild cognitive impairment. PLoS ONE. 2011;6(7):e21688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thompson TA, Wilson PH, Snyder PJ, et al. Sensitivity and test–retest reliability of the international shopping list test in assessing verbal learning and memory in mild Alzheimer's disease. Arch Clin Neuropsychol. 2011;26(5):412–424. [DOI] [PubMed] [Google Scholar]
- 24. Lim Y, Ellis K, Harrington K, et al. Use of the CogState brief battery in the assessment of Alzheimer's disease related cognitive impairment in the Australian imaging, biomarkers and lifestyle (AIBL) study J Clin Exp Neuropsychol. 2012:34(4):345–358. [DOI] [PubMed] [Google Scholar]
- 25. Nasreddine ZS, Phillips NA, Bedirian V, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. [DOI] [PubMed] [Google Scholar]
- 26. Brandt J, Spencer M, Folstein M. The Telephone Interview for Cognitive Status Neuropsychiatry. Neuropsychol Behav Neurol. 1988;1:111–117. [Google Scholar]
- 27. Crawford J, Smith G, Maylor E, Sala S, Logie R. The prospective retrospective memory questionnaire normative data and latent structure in a large non clinical sample. Memory. 2003;11(3):261–275. [DOI] [PubMed] [Google Scholar]
- 28. Crawford JR, Henry JD, Ward AL, Blake J. The Prospective and Retrospective Memory Questionnaire (PRMQ): latent structure, normative data and discrepancy analysis for proxy-ratings. Br J Clin Psychol. 2006;45(1):83–104. [DOI] [PubMed] [Google Scholar]
- 29. Costa PT, McRae RR. NEO-PI-R Professional Manual: Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI). Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- 30. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–343. [DOI] [PubMed] [Google Scholar]
- 31. Carver C. You want to measure coping but your protocol is too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. [DOI] [PubMed] [Google Scholar]
- 32. Cohen S, Williamson GM. Perceived Stress in a Probability Sample in the United States. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 33. Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288(18):2271–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17(1):37–49. [DOI] [PubMed] [Google Scholar]
- 35. Krause N. Traumatic events and meaning in life: exploring variations in three age cohorts. Ageing Soc. 2005;25(4):501–524. [Google Scholar]
- 36. Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry. 2010;67(3):304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Snitz BE, Yu L, Crane PK, Chang CC, Hughes TF, Ganguli M. Subjective cognitive complaints of older adults at the population level: an item response theory analysis. Alzheimer Dis Assoc Disord. 2012;26(4):344–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bartley M, Bokde AL, Ewers M, et al. Subjective memory complaints in community dwelling healthy older people: the influence of brain and psychopathology. Int J Geriatr Psychiatry. 2012;27(8):836–843. [DOI] [PubMed] [Google Scholar]
- 39. Elfgren C, Gustafson L, Vestberg S, Passant U. Subjective memory complaints, neuropsychological performance and psychiatric variables in memory clinic attendees: a 3-year follow-up study. Arch Gerontol Geriatr. 2010;51(3):e110–e114. [DOI] [PubMed] [Google Scholar]
- 40. Hurt CS, Burns A, Brown RG, Barrowclough C. Why don't older adults with subjective memory complaints seek help? Int J Geriatr Psychiatry. 2012;27(4):394–400. [DOI] [PubMed] [Google Scholar]