Abstract
Purpose
Religion and spirituality (R/S) are patient-centered factors and often resources for managing the emotional sequelae of the cancer experience. Studies investigating the relationship between R/S (e.g., beliefs, experiences, coping) and mental health (e.g., depression, anxiety, well-being) in cancer have used very heterogeneous measures, with correspondingly inconsistent results. A meaningful synthesis of these findings has been lacking; thus, the purpose of this study was to conduct a meta-analysis of the research on R/S and mental health.
Methods
Four electronic databases were systematically reviewed and 2,073 abstracts met initial selection criteria. Reviewer pairs applied standardized coding schemes to extract correlational indices of the relationship between R/S and mental health. A total of 617 effect sizes from 148 eligible studies were synthesized using meta-analytic generalized estimating equations; subgroup analyses were performed to examine moderators of effects.
Results
The estimated mean correlation (Fisher z) was 0.19 (95% CI 0.16–0.23), which varied as a function of R/S dimension: affective, z=0.38 (95% CI 0.33-0.43); behavioral, z=0.03 (95% CI -0.02-0.08); cognitive, z=0.10 (95% CI 0.06-0.14); and ‘other,’ z=0.08 (95% CI 0.03-0.13). Aggregate, study-level demographic and clinical factors were not predictive of the relationship between R/S and mental health. There was little indication of publication or reporting biases.
Conclusions
The relationship between R/S and mental health is generally a positive one. The strength of that relationship is modest and varies as a function of R/S dimensions and mental health domains assessed. Identification of optimal R/S measures and more sophisticated methodological approaches are needed to advance research.
Keywords: Religion, Spirituality, Cancer, Meta-Analysis, Quality of Life, Anxiety, Depression, Distress
Introduction
Numerous studies have examined the relationship between religion and spirituality (R/S) and mental health. Reviews of this literature have concluded R/S has a favorable association with mental health, although there is some heterogeneity in study findings.1, 2 A growing part of this literature has examined the relationship between R/S and mental health among cancer patients and survivors. In the context of cancer, R/S may provide intra- and inter-personal resources to manage distress and enhance healthy adaptation. Park has suggested religion is a meaning system that helps individuals cope with significant life stressors and enhance mental health by fostering meaning-making coping, stress-related growth, and improved psychological well-being.3 As the literature on this topic continues to develop, meta-analytic efforts are needed to synthesize disparate findings and focus future investigation. This report describes the first meta-analysis of the literature on R/S and mental health in patients with cancer.
Although R/S generally has demonstrated a salutary relationship with mental health in the context of cancer, results vary. For example, in a large study of cancer survivors, aspects of spiritual well-being that include having a sense of meaning and peace were strongly associated with less depression and anxiety, but drawing comfort from one's faith was weakly associated with greater depression and anxiety.4 The relationship between R/S coping and mental health has yielded mixed findings, with negative5, null6, and positive relationships7 found in patients with cancer. In addition, certain types of R/S problem-solving and less negative religious coping have been associated with less cancer-specific distress in some but not all studies.8-10 Altogether, these results can be difficult to interpret because the significance and strength of the relationships between R/S and mental health appear to vary somewhat depending on the particular R/S dimensions and mental health domains examined. Further contributing to the ambiguity in findings between R/S and mental health is the overlap in content between measures of spiritual well-being and emotional well-being which may ensure and artificially inflate the relationship between R/S and mental health.11-13
Consequently, to provide a comprehensive summary of the relationship between R/S and mental health and to quantify and synthesize a large and frequently heterogeneous research literature, we sought to: 1) identify the R/S and mental health associations that have been the most and least studied; 2) describe the strength and direction of the R/S and mental health associations; 3) examine the differences in R/S and mental health associations as a function of different R/S (including with and without spiritual well-being) and different mental health variables; and 4) explore the degree to which moderator variables may account for variations in the relationship between R/S and mental health outcomes. This is one in a series of three meta-analyses, designed to summarize and synthesize the associations between R/S and patient-reported physical,14 mental, and social health outcomes.15
Methods
Definition of terms
R/S was conceptualized a priori as composed of affective, behavioral, and cognitive dimensions. Measures of affective R/S assessed constructs such as spiritual well-being, spiritual distress, and spiritual experiences (e.g., “I feel deep inner peace or harmony”). Measures of behavioral R/S assessed public and private religious activities as well as positive religious coping. Measures of cognitive R/S assessed specific beliefs or R/S perceptions. Measures assessing unique or multiple dimensions of R/S were categorized as ‘other’ R/S and included general religiousness, religious affiliation, and religious social support. See Salsman et al.16 for a more detailed discussion of R/S dimensions.
Mental health was defined a priori as the thoughts and feelings that comprise an individual's level of psychological well-being. Mental health may be reflected by functioning on both negative and positive domains. For example, thoughts or cognitions may include ruminative worries such as fears of recurrence or conversely, appreciation for life. Affect and mood may be negative (e.g., anxiety, depression) or positive (e.g., happiness, gratitude).
Search strategy
Four electronic databases (PubMed, PsycInfo, CINAHL, and Cochrane Library) were systematically reviewed using standardized search strategies and controlled vocabulary terms for R/S (e.g., religio*, spiritual*), cancer (e.g., neoplasms, cancer, leukemia), and health outcomes (e.g., measure, scale, outcome*). Details regarding the search strategy are presented in the supplementary material. The searches included studies published in English from the earliest date available in each database through December 20, 2013. We requested unpublished studies via professional listservs of the American Psychosocial Oncology Society (Cancer Survivorship Special Interest Group), Society of Behavioral Medicine (Cancer Special Interest Group), and the American Psychological Association, Divisions 36 (Religion and Spirituality) and 38 (Health Psychology).
Inclusion criteria
Studies were included if they: (1) had an adult sample (≥18 years old) with a current or past diagnosis of cancer; (2) assessed an R/S variable; (3) assessed a mental health variable as described by our a priori definition; and (4) reported an effect size measuring the bivariate association between R/S and health. Data from intervention studies were included (e.g., baseline, pre-intervention effect sizes) except when the relationship between the R/S and health outcomes was potentially confounded with intervention effects. Descriptive and measure development/validation studies were included if they otherwise met study inclusion criteria. Excluded studies were: (1) caregiver or pediatric samples; (2) needs assessments of R/S or health; (3) qualitative assessments of R/S or health; and (4) R/S intervention studies in which the intervention was the only index of R/S.
Screening procedures
Four rater pairs reviewed abstracts to determine which articles merited full review. All abstracts were randomly assigned and reviewed independently by a senior scientist (GF, CP, TM, AS, or SD) and an early career scientist (JS, HJ) or an advanced graduate student (LG, AM). Discrepancies were resolved by rater-pair consensus. Studies meeting or possibly meeting (i.e., unable to determine based on the abstract) all criteria underwent full-text review. Four rater pairs independently reviewed the full-text articles and entered data abstracted from the studies. As described above, R/S measures were categorized as affective, behavioral, cognitive, or ‘other’, and outcome measures were categorized as physical, social, mental, or other. Data from subscale scores, if available, were used in lieu of total scores to maximize analytic flexibility and improve interpretability of study findings. Discrepancies were resolved by rater-pair consensus. When articles provided insufficient data, we attempted to contact authors for the required details.
Effect size measures
This meta-analysis was limited to studies reporting measures of bivariate association between R/S and mental health. Thus, the following types of effect size statistics were included: Pearson product-moment or Spearman rank correlation coefficients, standardized mean differences between groups, and odds ratios based on dichotomizing two continuous variables. If an effect size estimate was not directly reported, we attempted to calculate it based on information provided in the article. Multivariable measures of association, such as regression coefficients or partial correlation coefficients, were excluded because they are not directly comparable to measures of bivariate association and present considerable analytic complications.17
Effect sizes were coded in a standard way such that a positive relationship between an R/S dimension and mental health domain reflected more R/S and better mental health. For purposes of meta-analysis, all reported effect sizes were converted to the Fisher z scale, a non-linear transformation of Pearson's correlation measure. The Fisher z scale was chosen because it normalizes and stabilizes the sampling variance of Pearson correlation coefficients that constitute the majority of effect size measures in the meta-analysis and because it has an unbounded range.18 Transformation to the z-scale has very little effect in the range of correlations found in the present analysis (-0.4 < z < 0.4); consequently, the z-scale estimates reported below are nearly equivalent to the corresponding values on the scale of Pearson's r.
Moderator variables
We also coded the articles to examine the degree to which various demographic and clinical characteristics moderate the relationships between R/S and mental health. Sample-level average demographic characteristics included: gender, age, race, and geographic origin. Clinical characteristics of the samples included: cancer type, stage, and phase in the disease and survivor trajectory (diagnosis/treatment, post-treatment survivorship, end-of-life, and mixed).
Meta-analytic procedures
Many studies meeting inclusion criteria provided effect size data for multiple measures of R/S, multiple measures of mental health outcomes, or both, all based on a common sample of participants. When assessing the extent of past research using different combinations of R/S dimensions and mental health outcome measures, we focused on the number of unique samples (i.e., from different studies) rather than the number of unique effect size estimates, because estimates based on a common sample of participants are inter-correlated, rather than independent. In order to address the dependence of effect size estimates drawn from common studies, a generalized estimating equation (GEE) approach was used to estimate average effect sizes and meta-regressions, in conjunction with robust variance estimation procedures. This method produces valid inferences even when effect size estimates drawn from common studies are not independent, but are instead correlated to an unknown or mis-specified degree.19 For comparisons between two categories of effect sizes and tests of one-variable moderators, we employed robust t-tests involving small-sample corrections proposed by Tipton.20 For simultaneous comparisons among several categories (e.g., for testing differences across categories of R/S measures) and simultaneous tests of multiple moderators, we used robust Wald test statistics that follow chi-square reference distributions when the number of independent studies is large. Weights for the GEE analysis were determined based on a hierarchical model containing between-study and within-study random effects.
Results
Study Selection
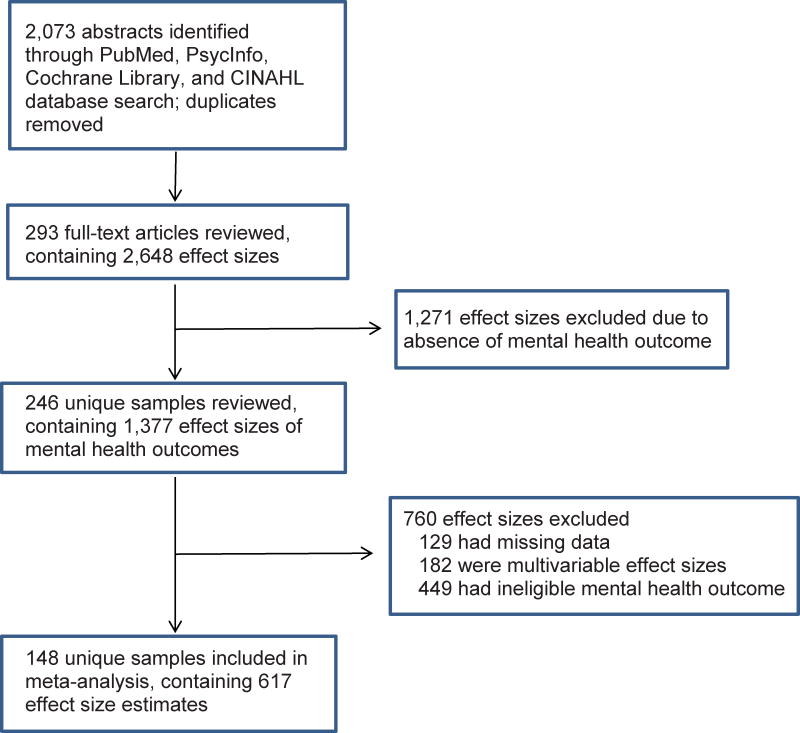
A total of 2,073 abstracts were identified through electronic databases. Full text articles were retrieved for 293 studies, covering 2,648 unique effect sizes. After excluding studies that did not have an eligible mental health outcome, had missing data, or did not report measures of bivariate association, 617 effect sizes from 148 unique samples were included for this study. Among excluded effect sizes were 182 multivariable measures of effect from 45 unique samples; however, bivariate measures of association from 4 of these samples were available and retained for analysis. Figure 1 provides a flow chart of the selection of studies, and characteristics of included studies are described in the supplementary material.
Figure 1. Flow Chart of Selection of Studies.
Study Participants
The combined samples included in our analyses comprised over 39,000 cancer patients with a mean number of 265 (SD=755) patients per sample. Across all included samples, the mean patient age was 57.1 years (SD=7.3), and the mean percentage of female patients was 69 (SD=28). Sixty-one percent of samples came from North America; of these, the mean percentage of Caucasian patients was 71 (SD = 32). Across all included samples, 22% focused on the diagnosis and treatment phase of the cancer continuum, 26% on the post-treatment survivorship phase, 9% on end-of-life phase, and 43% on multiple phases. Regarding cancer type, 29% of samples focused exclusively on breast cancer, 20% focused exclusively on another cancer (e.g., prostate, lung), and 51% were mixed-diagnosis cancer samples. Regarding stage at diagnosis, 9% focused on patients with early-stage disease (i.e., in situ or local), 16% on advanced stage disease (i.e., regional or metastatic), 40% were mixed, and 34% did not report disease stage.
R/S and Health Combinations
The R/S and mental health associations that have received the most attention are spiritual well-being (an affective construct) with emotional well-being (33 studies), depression (17 studies), and cancer-specific distress (15 studies). Within the behavioral R/S dimension, correlations of R/S coping with emotional well-being (17 studies) and depression (14 studies) have been frequently studied. Within the cognitive R/S dimension, spiritual growth and depression (6 studies) and God-image and emotional well-being (6 studies) have been examined most frequently. For the ‘other’ R/S dimension, composite R/S indices and emotional well-being (11 studies) were most frequently studied. Few studies have employed cognitive R/S constructs. For example, the relationships between R/S locus of control, religious orientation, and spiritual decline with any mental health outcomes have been examined in 3, 4, and 3 studies, respectively.
Meta-analyses
GEE analysis was conducted to determine the average effect size between R/S and mental health, pooling across all dimensions of R/S. Results are displayed in Table 1. R/S was significantly associated with mental health (z=.194). Additional analyses were conducted to determine whether the average effect sizes between R/S and mental health differed by R/S dimension. Dimensions significantly associated with mental health were affective (z=.380), cognitive (z=.102), and ‘other’ R/S (z=.080) but not behavioral R/S (z=.028). The association between mental health and affective R/S was significantly different from the association of mental health with the other three R/S dimensions (all Ps <.01); associations of behavioral R/S and cognitive R/S with mental health were significantly different from each other (P<.01). After accounting for sampling error in the effect size estimates, differences between R/S dimensions accounted for 38% of the overall variation in the strength of association between R/S and mental health, including 60% of the between-study variation. In light of observations about item overlap in measures of spiritual and emotional well-being, we repeated the analyses of overall R/S with the mental health domain and subdomains, as well as affective R/S with the mental health domain and subdomains, after omitting all measures of spiritual well-being. As shown in Table 1, excluding spiritual well-being measures from the analysis reduced the association between the overall average association between R/S and mental health to z=.085 and between affective R/S and mental health to z=.290; both estimates remained significant.
Table 1. Estimated Associations between Religion/Spirituality and Overall Mental Health.
| Religion/Spirituality Dimension | Estimate (SE) | 95% CI | Studies | Effect sizes |
|---|---|---|---|---|
| All | .194 (.019)*** | .156-.231 | 148 | 617 |
| All (SpWB excluded) | .085 (.013)*** | .059-.112 | 108 | 433 |
| Affective | .380 (.025)*** | .330-.431 | 68 | 234 |
| Affective (SpWB excluded) | .290 (.055)*** | .174-.406 | 20 | 50 |
| Behavioral | .028 (.026) | -.024-.080 | 43 | 133 |
| Cognitive | .102 (.018)*** | .065-.138 | 41 | 160 |
| ‘Other’ | .080 (.024)** | .031-.128 | 43 | 90 |
Note: Estimates are z-scale effect sizes. SE = standard error. CI = confidence interval. SpWB = spiritual well-being.
p<.01,
p<.001
Differential associations with mental health constructs
Further analyses were conducted to determine if the R/S and mental health associations varied across different mental health outcomes (i.e., emotional well-being, depression, anxiety, general distress, and cancer-specific distress). Table 2 shows the estimated effect sizes between R/S dimensions and mental health constructs. For R/S overall, the association with anxiety and cancer-specific distress were weaker than those for depression and emotional well-being (P<.05). Affective and cognitive R/S were significantly associated with all five categories of mental health outcomes (z=.269 to .424 and z=.088 to .124, respectively); ‘other’ R/S was significantly associated with depression and emotional well-being (z=.134 and z=.124, respectively). Differences were detected in the strength with which the mental health outcome categories were associated with affective R/S (P < .001) and ‘other’ R/S (P < .001); within the behavioral and cognitive dimensions, differences among the mental health outcome categories could not be distinguished (P=.70 and P=.95, respectively).
Table 2. Estimated Associations Between Religion/Spirituality and Mental Health Subdomains.
| Religion/ Spirituality Dimension |
Emotional Well-Being | General Distress | Depression | Anxiety | Cancer-Specific Distress | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est (SE) |
Studies | Effect sizes |
Est (SE) |
Studies | Effect sizes |
Est (SE) |
Studies | Effect sizes |
Est (SE) |
Studies | Effect sizes |
Est (SE) |
Studies | Effect sizes |
|
| All | 0.224 (.023)*** | 70 | 203 | 0.189 (.030)*** | 44 | 116 | 0.211 (.026)*** | 57 | 125 | 0.158 (.030)*** | 39 | 69 | 0.136 (.023) *** | 34 | 104 |
| All (SpWB excluded) | .096 (.015) *** | 46 | 144 | .072 (.022) ** | 35 | 91 | .096 (.024) *** | 45 | 93 | .063 (.035) | 31 | 51 | .080 (.021) ** | 21 | 54 |
| Affective | 0.411 (.035)*** | 40 | 79 | .401 (.038)*** | 15 | 32 | .424 (.035)*** | 25 | 43 | .340 (.040)*** | 16 | 25 | .269 (.041)*** | 17 | 55 |
| Affective (SpWB excluded) | .324 (.069)** | 11 | 20 | .318 (.063)** | 5 | 7 | .278 (.091)* | 9 | 11 | .146 (.124) | 6 | 7 | .321 (.207) | 3 | 5 |
| Behavioral | .026 (.032) | 23 | 48 | .059 (.048) | 13 | 22 | .032 (.037) | 18 | 31 | -.011 (.037) | 12 | 15 | .019 (.085) | 7 | 17 |
| Cognitive | .099 (.017)*** | 16 | 55 | .124 (.037)*** | 12 | 33 | .094 (.037)* | 17 | 33 | .088 (.035)* | 10 | 17 | .098 (.026)** | 12 | 22 |
| ‘Other’ | .124 (.027)*** | 18 | 21 | .028 (.033) | 17 | 29 | .134 (.026)** | 15 | 18 | .092 (.080) | 11 | 12 | .003 (.040) | 6 | 10 |
Note: A positive relationship between an R/S and mental health outcome reflects more R/S and better mental health (i.e., more emotional well-being and less general distress, depression, anxiety, and cancer-specific distress). Estimates are z-scale effect sizes. SE = standard error. SpWB = spiritual well-being.
p<.05,
p<.01,
p<.001
Affective R/S
To gain a better understanding of which R/S measures accounted for the significant relationships with mental health outcomes, additional analyses were conducted with the most frequently used R/S measures within the affective, cognitive, and ‘other’ R/S dimensions. For the affective R/S dimension, spiritual well-being and spiritual distress were the most common R/S subdimensions, used in 53 and 18 different studies, respectively. Spiritual well-being was significantly associated with each of the five categories of mental health outcomes (z=.272 to .482), and its average correlation with mental health outcomes differed by category (P<.001); specifically, the association with cancer-specific distress was significantly lower than the association with the other four mental health outcomes. Spiritual distress was significantly associated with emotional well-being, general distress, and depression (all Ps<.01), but not with anxiety or cancer specific distress; however, it should be noted that <5 independent studies contributed to the estimated associations with the latter categories. Differential associations across mental health outcomes could not be distinguished (P=.22).
Again, in light of observations about item overlap in measures of spiritual and emotional well-being, we repeated the analyses of affective R/S with the mental health subdomains, after omitting all measures of spiritual well-being. Omitting measures of spiritual well-being reduced the associations between R/S overall and each mental health subdomain by between .056 (for cancer-specific distress) and .128 (for emotional well-being); all estimates except for anxiety remained statistically significant (Table 2). After omitting measures of spiritual well-being, affective R/S remained significantly associated with emotional well-being, general distress, and depression, but not with anxiety or cancer-specific distress. Notably, the estimated association between affective R/S and anxiety was greatly reduced, from z=.340 to.146 (Table 2).
Cognitive R/S
In the cognitive R/S dimension, the most common construct was spiritual growth (e.g., spiritual change subscale of the Posttraumatic Growth Inventory), used in 11 studies. The average level of association between spiritual growth and mental health outcomes was small (z=.079) and did not differ across mental health outcome categories (P=.14).
Other R/S
For the ‘other’ R/S dimension, composite measures of R/S were used in 20 distinct samples. Their average level of association with mental health outcomes was low (z=.092), but differed by mental health outcome category (P<.001). Composite indices were significantly associated with depression (z=.127), emotional well-being (z=.147), and general distress (z=.108), but not with anxiety (P=0.87) or cancer-specific distress (P=0.77).
Moderator analyses
We examined study-level averages of socio-demographic (i.e., age, gender, geographic origin of study, race) and clinical variables (cancer type, stage, and phase in the continuum from treatment through survivorship) as potential moderators of the magnitude of effect size between R/S dimensions and mental health outcomes. No moderators were statistically significant (Ps>.09).
Reporting bias
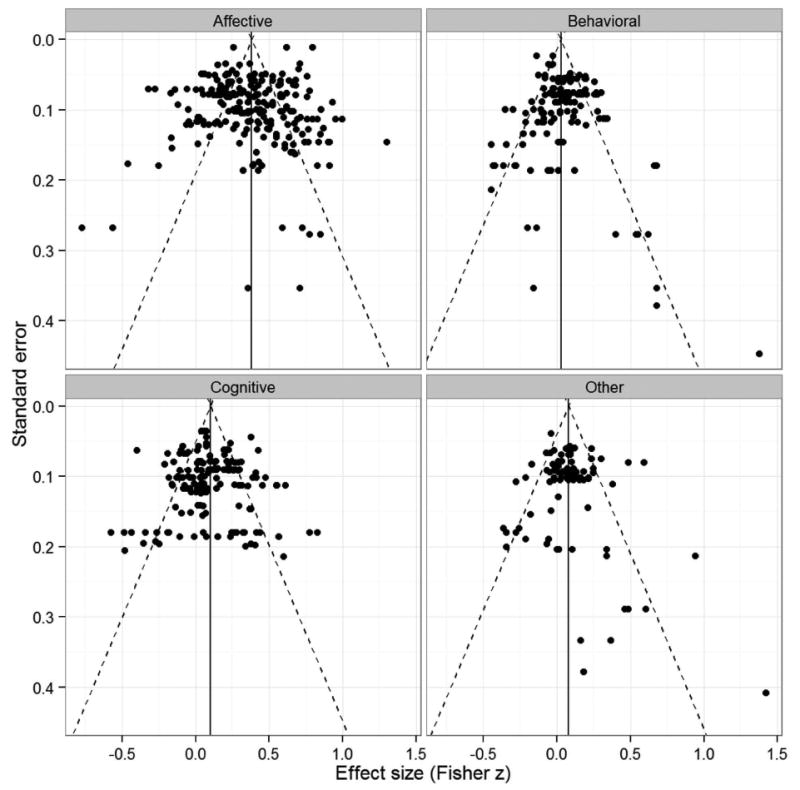
A pervasive concern in meta-analysis is the possibility that published or reported effect sizes are not representative of the results of all completed studies.21 Such reporting bias can arise if studies describing statistically significant results are most likely to be published, or if authors selectively report specific results based on their statistical significance (which can occur even if the full study is published). We consider it implausible that entire studies would go unreported based on the statistical insignificance of the bivariate association between R/S and mental health outcome variables, particularly because these associations were not the central focus of most studies. However, censoring of individual effect sizes is a plausible concern, and could affect the results of a meta-analysis by artificially inflating estimates of the average association between R/S measures and mental health outcomes. We assessed the threat of reporting bias through visual inspection of funnel plots and sensitivity analysis.
Figure 2 presents funnel plots of the reported effect size estimates within each R/S dimension. The plots do not display noticeable asymmetry that would indicate reporting bias, with the possible exception of the ‘other’ R/S dimension. A cluster-robust variant of Egger's test did not detect reporting bias (P=.24).22 The plots do make apparent the marked heterogeneity of effects within each R/S dimension.
Figure 2. Funnel plots of effect sizes versus standard errors for each R/S dimension.
We conducted a sensitivity analysis by identifying effect sizes not included in the main analysis due to missing data, but where it was noted that the effect size was statistically insignificant. The search process identified 44 effect sizes (from 7 studies) meeting this criterion, indicating a censoring rate of 6.7%. We tested the sensitivity of the results by imputing a value of zero for each of these missing effect sizes, then re-running all the analyses. Most previously reported results were insensitive to the inclusion of the imputed effect sizes. The most notable changes were that the average effect size in the behavioral R/S dimension increased to .063 (95% CI -.001-.136) and the average effect size in the ‘other’ R/S dimension decreased to .045 (95% CI -.039-.129) and was no longer statistically distinguishable from zero. However, the ‘other’ R/S dimension remained significantly associated with depression and emotional well-being.
Discussion
This study is the first meta-analysis of the relationships between R/S and mental health outcomes within the context of cancer. Based on 617 effect sizes from 148 independent studies and over 39,000 patients at various stages of the cancer care continuum, we found R/S overall had a positive association with mental health. This positive association remained even after removing the studies that used spiritual well-being as an R/S predictor variable. The strength of the relationship between R/S and mental health was relatively modest and varied as a function of type of R/S dimension (affective, behavioral, cognitive, ‘other’) and type of mental health outcomes (emotional well-being, general distress, cancer-specific distress, depression, and anxiety). Demographic and clinical variables were not significant moderators of the associations between the R/S dimensions and mental health outcomes.
Among the R/S dimensions, affective R/S was the most robust predictor of mental health outcomes emotional well-being, general distress and depression even when measures of spiritual well-being were omitted from the analyses. Criticism about item overlap between predictor and outcome measures in research about R/S and mental health11-13 has raised questions about how these findings should be interpreted, especially because it appeared that this criticism applied to more than a few studies. The present analyses confirmed that the concern applied to a large portion of the literature; omitting measures of spiritual well-being reduced the number of studies and number of effect sizes of all R/S and mental health by 27% and 30% and of affective R/S by 71% and 79%, respectively. In light of this criticism, the findings of a significant association between the various mental health outcomes and R/S overall and affective R/S when measures of spiritual well-being were excluded is an important contribution to the research. Spiritual well-being is an important outcome but adds little value to our understanding of the role of R/S and mental health when used as a predictor variable.
As further evidence that the relationship between R/S and mental health is not simply due to the confounding presence of spiritual well-being, both cognitive and ‘other’ R/S dimensions were significantly, albeit less strongly, related to mental health outcomes. Cognitive R/S was associated with all mental health outcomes – emotional well-being, general distress, cancer-specific distress, depression, and anxiety – whereas ‘other’ R/S was associated with emotional well-being and depression. For cognitive R/S constructs, the perception of positive changes in one's spiritual life co-occurred with reports of better mental health. While spiritual growth following a cancer diagnosis and treatment can easily be understood as a byproduct of higher levels of emotional well-being or even a mental health outcome, reports of positive psychosocial change following a cancer diagnosis often yield mixed associations with mental health.23 Accordingly, the presence of a significant relationship across all mental health outcomes is worth noting. Further research is needed to determine whether perceived spiritual growth affects mental health or vice versa.
Within the ‘other’ R/S dimension, composite indices of R/S that assess general religiousness or assess combinations of affective, behavioral, or cognitive R/S are somewhat common and related to better emotional well-being and less depression and general distress. Although it is difficult to parse out which dimensions of R/S within composite measures may be accounting for the relationships with mental health outcomes, there may be some shared variance common to all dimensions of R/S that essentially comprises a general factor, or R/S “g factor.” However, as the field of R/S and health research has evolved and there is greater interest in more focused questions about how specific aspects of R/S influence health and for whom, R/S composite measures have limited utility.
In light of the consistent associations in the general population of behavioral R/S measures, such as frequency of worship attendance, and outcomes such as emotional well-being24, the lack of any association with mental health outcomes in our analysis is surprising. Several factors may have contributed to this. Prayer is one of the most common R/S behaviors among patients with cancer25 but, as other investigators have described26, there may be at least two different associations between frequency of prayer and emotional well-being. Among patients for whom frequent prayer is a well-established practice, there may be an inverse association with emotional distress; that is more frequent prayer is associated with less distress. However, if distressed patients use prayer to seek comfort, cross-sectional studies will reveal a positive association; that is more frequent prayer is associated with more distress. These two different effects may dilute or negate an association between this common R/S behavior and mental health outcomes.
At first glance, the absence of moderation in our analyses is striking. However, it should be remembered that although differential involvement in R/S for demographic subgroups such as older adults, women, and racial-ethnic minorities is well-established in both community and clinical samples27-29, the evidence of the differential impact of R/S on health-related outcomes for those subgroups is more limited (e.g., Musick et al. 1998,30 Sternthal et al. 201231). It should also be noted that while we tested a number of potential demographic and clinical moderators, we were able to do so only using study-level aggregate information. A key limitation of this analysis is aggregation may conceal variation at the patient level, greatly reducing sensitivity relative to tests based on patient-level characteristics. Thus, our finding does not rule out the possibility of differences in the effects of R/S for specific mental health outcomes for one or more demographic or clinical subgroups.
A common concern in meta-analysis is that results may be skewed by publishing or reporting bias caused when studies with significant findings are more likely to be published than those with non-significant findings. Our analyses revealed little indication of publication or reporting bias. Given that our selection strategy included R/S and mental health outcomes based on descriptive or secondary outcomes and not simply those that were primary outcomes, we consider our findings robust to potential reporting biases.
This meta-analysis is not without limitations. There may be concerns a meta-analysis of R/S and cancer obscures important individual differences. Cohen suggested religion can be considered a type of culture32, and similar to other cultural dimensions, there may be more within- than between-culture variation for certain types of R/S.33 For example, we did not account for the effects of religious affiliation or associated variations in commitment. Consequently, salient group characteristics may be obscured when aggregated with data from more heterogeneous samples. Unfortunately, most studies did not provide sufficient descriptive characteristics to code for homogeneity/heterogeneity of religious affiliation. An additional limitation was that studies reporting only multivariable measures of association (e.g., partial correlations, regression coefficients) were excluded due to the lack of comparability of multivariable- and bivariate effect sizes. The multivariable effect sizes differed from the retained effect sizes in terms of the distribution of R/S measures and mental health outcome measures, suggesting that a separate synthesis of these effect sizes is warranted. Finally, the prevalence of cross-sectional data hinders our ability to infer causality from these data. The possible bi-directional relationship between R/S dimensions and mental health cannot be examined, nor can such studies shed light on whether a common factor contributes to both R/S and mental health. These are important areas for future research about the contributions of affective R/S to the mental health of cancer patients.
In summary, this meta-analysis is the first to examine the relationships between R/S dimensions and mental health outcomes within the context of cancer. Findings underscore the modest but positive relationships between various aspects of R/S and mental health. From a population perspective, modest associations can account for substantial effects. Accordingly, given the large number of patients who describe R/S as one of the, if not the, most important factor(s) in coping with their illness, it is possible that R/S is serving a beneficial role in the mental health of a substantial number of patients with cancer. This meta-analysis has a number of strengths, including the breadth of the literature reviewed, the categorization of R/S dimensions (affective, behavioral, cognitive, ‘other’) and mental health outcomes (emotional well-being, anxiety, depression, general distress, cancer-specific distress), the inclusion of potential clinical and demographic moderating variables, and the analyses of publication bias.
Although this meta-analysis is an important step toward synthesizing and understanding the complex relationships between R/S and mental health, future research should focus on delineating these differential effects. Specifically, the mechanisms accounting for R/S and mental health are poorly understood and merit greater attention. The investigation of pathways between R/S and mental health would be aided by the increased use of psychometrically strong R/S measures. In a number of studies in this meta-analysis, investigators used psychometrically poor measures of R/S specifically designed for their study, making clear categorization of measures and thus comparisons of relationships challenging. Finally, to move the field forward, more rigorously designed studies and longitudinal approaches are needed to better understand what types of R/S are most beneficial and for which groups of patients. This information can then be used to provide better patient-centered care, reduce adverse emotional sequelae of the cancer experience, and promote greater well-being.
Supplementary Material
Acknowledgments
Funding Source: Research reported in this publication was supported by the National Cancer Institute of the NIH under award number K07CA158008. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
The authors have no financial disclosures or conflicts of interest to report.
References
- 1.Koenig HG. Research on religion, spirituality, and mental health: a review. Canadian Journal of Psychiatry. 2009;54:283–291. doi: 10.1177/070674370905400502. [DOI] [PubMed] [Google Scholar]
- 2.Lee BY, Newberg AB. Religion and Health: A Review and Critical Analysis. Zygon. 2005;40:443–468. [Google Scholar]
- 3.Park CL. Religion as a meaning-making framework in coping with life stress. Journal of Social Issues. 2005;61:707–729. [Google Scholar]
- 4.Canada AL, Murphy PE, Fitchett G, Peterman AH, Schover LR. A 3-factor model for the FACIT-Sp. Psycho-Oncology. 2008;17:908. doi: 10.1002/pon.1307. [DOI] [PubMed] [Google Scholar]
- 5.Derks W, de Leeuw JRJ, Hordijk GJ, Winnubst JAM. Differences in coping style and locus of control between older and younger patients with head and neck cancer. Clinical Otolaryngology. 2005;30:186–192. doi: 10.1111/j.1365-2273.2004.00938.x. [DOI] [PubMed] [Google Scholar]
- 6.Jim HS, Richardson SA, Golden-Kreutz DM, Andersen BL. Strategies used in coping with a cancer diagnosis predict meaning in life for survivors. Health Psychology. 2006;25:753–761. doi: 10.1037/0278-6133.25.6.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Travado L, Grassi L, Gil F, Martins C, Ventura C, Bairradas J. Do spirituality and faith make a difference? Report from the Southern European Psycho-Oncology Study Group. Palliative and Supportive Care. 2010;8:405–413. doi: 10.1017/S147895151000026X. [DOI] [PubMed] [Google Scholar]
- 8.Nairn RC, Merluzzi TV. The role of religious coping in adjustment to cancer. Psycho-Oncology. 2003;12:428–441. doi: 10.1002/pon.654. [DOI] [PubMed] [Google Scholar]
- 9.Trevino K, Archambault E, Schuster J, Richardson P, Moye J. Religious Coping and Psychological Distress in Military Veteran Cancer Survivors. Journal of Religion and Health. 2012;51:87–98. doi: 10.1007/s10943-011-9526-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yanez B, Edmondson D, Stanton AL, et al. Facets of Spirituality as Predictors of Adjustment to Cancer: Relative Contributions of Having Faith and Finding Meaning. Journal of Consulting and Clinical Psychology. 2009;77:730–741. doi: 10.1037/a0015820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koenig HG. Concerns About Measuring “Spirituality” in Research. The Journal of Nervous and Mental Disease. 2008;196:349–355. doi: 10.1097/NMD.0b013e31816ff796. [DOI] [PubMed] [Google Scholar]
- 12.Sherman AC, Simonton S. Assessment of religiousness and spirituality in health research. In: Plante TG, C SA, editors. Faith and health : psychological perspectives. New York: Guilford Press; 2001. pp. 139–163. [Google Scholar]
- 13.Visser A, Garssen B, Vingerhoets A. Spirituality and well-being in cancer patients: a review. Psycho-Oncology. 2010;19:565–572. doi: 10.1002/pon.1626. [DOI] [PubMed] [Google Scholar]
- 14.Jim HSL, Pustejovsky JE, Park CL, et al. Religion, spirituality, and physical health in cancer patients: a meta-analysis. Manuscript submitted for publication. 2014 doi: 10.1002/cncr.29353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherman AC, Merluzzi TV, Pustejovsky JE, et al. A meta-analytic review of religious or spiritual involvement and social health among cancer patients. Manuscript submitted for publication. 2014 doi: 10.1002/cncr.29352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salsman JM, Fitchett G, Merluzzi TV, Sherman AC, Park CL. Religion, spirituality, and health outcomes in cancer: A case for a meta-analytic investigation. Manuscript submitted for publication. 2014 doi: 10.1002/cncr.29349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Becker BJ, Wu MJ. The Synthesis of Regression Slopes in Meta-Analysis. Statistical Science. 2007;22:414–429. [Google Scholar]
- 18.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis Chichester. United Kingdom: Wiley; 2009. [Google Scholar]
- 19.Hedges LV, Tipton E, Johnson MC. Robust variance estimation in meta-regression with dependent effect size estimates. Research Synthesis Methods. 2010;1:39–65. doi: 10.1002/jrsm.5. [DOI] [PubMed] [Google Scholar]
- 20.Tipton E. Small sample adjustments for robust variance estimation with meta-regression Psychological Methods. 2014 doi: 10.1037/met0000011. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Rothstein HR, Sutton AJ, Borenstein M. Publication bias in meta-analysis. In: Rothstein H, Sutton AJ, Borenstein M, editors. Publication bias in meta-analysis : prevention, assessment and adjustments. Chichester, England; Hoboken, NJ: Wiley; 2005. pp. 1–10. [Google Scholar]
- 22.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical Research Ed) 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of Posttraumatic Growth: Research and Practice. Mahwah: Lawrence Erlbaum Associates, Inc; 2006. pp. 138–175. [Google Scholar]
- 24.McCullough ME, Larson DB. Religion and depression: a review of the literature. Twin Research (2000) 1999;2:126–136. doi: 10.1375/136905299320565997. [DOI] [PubMed] [Google Scholar]
- 25.Yates J, Mustian K, Morrow G, et al. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Supportive Care in Cancer. 2005;13:806–811. doi: 10.1007/s00520-004-0770-7. [DOI] [PubMed] [Google Scholar]
- 26.Park C. Religiousness/Spirituality and Health: A Meaning Systems Perspective. Journal of Behavioral Medicine. 2007;30:319–328. doi: 10.1007/s10865-007-9111-x. [DOI] [PubMed] [Google Scholar]
- 27.Canada A, Fitchett G, Murphy P, et al. Racial/ethnic differences in spiritual well-being among cancer survivors. Journal of Behavioral Medicine. 2013;36:441–453. doi: 10.1007/s10865-012-9439-8. [DOI] [PubMed] [Google Scholar]
- 28.Idler EL, Musick MA, Ellison CG, et al. Measuring Multiple Dimensions of Religion and Spirituality for Health Research: Conceptual Background and Findings from the 1998 General Social Survey. Research on Aging. 2003;25:327–365. [Google Scholar]
- 29.Taylor RJ, Chatters LM, Jackson JS. Religious and Spiritual Involvement Among Older African Americans, Caribbean Blacks, and Non-Hispanic Whites: Findings From the National Survey of American Life. Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2007;62:S238–S250. doi: 10.1093/geronb/62.4.s238. [DOI] [PubMed] [Google Scholar]
- 30.Musick MA, Koenig HG, Hays JC, Cohen HJ. Religious activity and depression among community-dwelling elderly persons with cancer: the moderating effect of race. Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 1998;53:218–227. doi: 10.1093/geronb/53b.4.s218. [DOI] [PubMed] [Google Scholar]
- 31.Sternthal MJ, Williams DR, Musick MA, Buck AC. Religious practices, beliefs, and mental health: variations across ethnicity. Ethnicity and Health. 2012;17:171–185. doi: 10.1080/13557858.2012.655264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen AB. Many forms of culture. American Psychologist. 2009;64:194–204. doi: 10.1037/a0015308. [DOI] [PubMed] [Google Scholar]
- 33.Adams G, Markus HR. Toward a conception of culture suitable for a social psychology of culture. In: Schaller M, Crandall CS, editors. The psychological foundations of culture. Mahwah, N.J: Lawrence Erlbaum; 2004. pp. 335–360. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.