Abstract
Background
With increased survival of perinatally HIV - infected adolescents due to antiretroviral therapy (ART), the focus of HIV care has shifted to health-related quality of life (HRQoL) as a measure of disease progression, effects of ART co-morbidity and prognosis. We assessed factors associated with better HRQoL in perinatally HIV -infected adolescents in Uganda by determining the associations between sexual and reproductive health (SRH) or lifestyle experiences on HRQoL.
Methods
In a cross-sectional study, data on SRH, lifestyle experiences, socio demographic factors, communication with parents on sexuality and satisfaction of SRH services in ART clinics were collected from 614 HIV perinatally infected adolescents aged 10–19 using an interviewer-administered survey questionnaire. HRQoL data were collected using the Medical Outcomes Study HIV Health Survey instrument (MOS-HIV). Factors associated with better HRQoL were analysed using multiple logistic regression.
Results
The mean age was 16.2 ± 2.1 years, 362 (58.8 %) were females and 210 (34.2 %) were sexually active. Adolescents on ART were twice likely to present with better physical health (AOR = 2.07, 95 % CI: 1.24–3.46) and four times more likely to present with better mental health (AOR = 3.9, 95 % CI: 2.22–6.92) than those who were not on ART. There were no statistically significant associations between SRH (ever had sex, ever been pregnant, condom use, contraceptive use) or life style factors and physical health or mental health. Those with secondary or tertiary education were more likely to present with a better mental health (AOR = 5.3, 95 % CI: 1.86–15.41) compared those who had attained primary or no education. Participants who desired to have a child in future more likely (AOR 1.7, 95 % CI: 1.05–3.00) to present with a better mental health. Lack of communication with guardians on sexuality (AOR = 0.6, 95 % CI: 0.40–0.89), or dissatisfaction with SRH services (AOR 0.34, 95 % CI: 0.18–0.62) were associated with poorer mental health.
Conclusion
Among perinatally HIV-infected adolescents in Uganda, being on ART was associated with better physical and mental health while lack of communication with guardians on sexuality or dissatisfaction with SRH services was associated with poor mental health. Adolescents with pregnancy intentions were more likely to have a better mental health.
Keywords: HIV, Health related quality of life, Sexual and reproductive health, Adolescents
Background
Globally, it is estimated that about 2.1 million adolescents aged 10–19 years are HIV positive [1]. The majority of these adolescents acquired HIV perinatally from their HIV infected mothers during pregnancy or birth or when they were breastfed. Nearly 2 million of these adolescents live in sub-Saharan Africa, 70 % of whom live in South Africa, Nigeria, Kenya, Tanzania, Uganda, Zimbabwe, Mozambique, Zambia, Ethiopia and Malawi [1]. In the year 2012, about 260,000 new HIV infections occurred in children worldwide [2]. With improved access to antiretroviral therapy (ART), most of these children will soon reach adolescence. In Uganda, the overall HIV prevalence among adolescents aged 15–19 years increased from 1.5 % in 2004–2005 to 2.4 % in 2011, while the overall national prevalence increased from 6.4 to 7.3 % [3]. In 2012, an estimated 110,000 adolescents were living with HIV in the country [4].
In general, quality of life (QOL) is the perceived quality of an individual’s daily life assessment of their well-being or lack thereof. QOL includes all emotional, social, and physical aspects of the individual’s life. In health care, health-related quality of life (HRQoL) is an assessment of how the individual’s well-being may be affected over time by a disease, a disability, or a disorder [5]. People living with HIV have significantly lower HRQoL than the general population, despite being virologically and immunologically stable [6].
The challenges that perinatally HIV-infected adolescents must deal with include; living in constant fear of having their serostatus being found out by peers [7–10], resentment and anger towards their parents, uncertainty about living a normal life and having a family in the future, treatment fatigue, as well as potential presence of feelings of powerlessness, hopelessness, depression and in extreme cases, suicidal ideation [11, 12]. These may affect their HRQoL. Many perinatally HIV-infected adolescents face the problem of orphan hood by having lost their parents or guardians, thereafter taking responsibility for welfare of younger siblings or other ill family members, stigma and discrimination, the fear of being viewed as abnormal, and being confronted with fear of death and an uncertain future [13, 14]. These may affect their HRQoL. Other challenges include living with an incurable chronic disease, lifelong medication dependence and adherence issues, drug-related toxicity and unwanted effects [11, 15–19]. All these may also affect the HRQoL. Consequently, some adolescents will have mental problems due to their HIV status or the treatment for HIV [16, 20, 21]. This, in turn, have potential implications related to their willingness to seek medical care, and motivation to adhere to therapy and ultimately influence health outcomes [22].
Several factors have been shown associated with HRQoL in patients with HIV, these include; Physical manifestations, antiretroviral therapy, psychological well-being, social support systems, coping strategies, spiritual well-being, and psychiatric comorbidities [23, 24]. Perinatally HIV-infected adolescents, like other adolescents form relationships, and become sexually active [25, 26]. Some relationships could be positive and supportive which may improve HRQoL. Yet, other relationships may be negative which negatively affect HRQoL. With increased survival due to ART, there is increasing survival of children (with a slowly progressive HIV infection) who are now reaching physiological and psychological maturation. As a consequence, they are at risk of becoming pregnant or causing a pregnancy, acquiring sexually transmitted infections and transmitting HIV [27]. Pregnancy and acquisition of an STI may also affect their HRQoL. Pregnancy related and STI comorbidities and associated physical symptoms may affect HRQoL. Disclosure of unwanted pregnancy may lead to denial from the partner which may affect the mental health of these adolescents [28, 29]. On the other hand, a pregnancy may be positive and acceptable by partner or their family, which improves the quality of life of the adolescents [30]. Additionally, adolescents living in constant fear of death may view pregnancy as a way of living a successor [31]. In addition to physical morbidity, STIs may lead to suspicion and mistrust in the relationships [32], thus leading to potential effect on quality of life. Lastly, ART treatment may improve immunity and reduce risk of co-morbidity from opportunistic infections, thus improving quality of life [17]. However, side-effects of ART may worsen quality of life [33].
With effective treatment available, the focus of HIV care has shifted to HRQoL, as a measure of disease progression, effects of ART and co-morbidity and prognosis [34, 35]. Focus should therefore be on assessment of HRQoL among HIV infected adults as well as adolescents in daily care [18, 34, 35]. A routine assessment of HRQoL in persons with HIV infection has the potential to improve care by assessing and monitoring treatment effects, enhancing communication between patient and provider, and tracking changes in functional status over time. There is limited information on association between sexual and reproductive health (SRH) or life style factors and HRQoL among Ugandan adolescents. Therefore, the aims of the present study were to describe HRQoL and to assess the association between SRH or lifestyle experiences and HRQoL among perinatally HIV infected adolescents in Uganda.
Methods
Study setting and sampling of clinics
This cross sectional study was conducted in the eastern, western and northern regions of Uganda. Twelve health facilities that provide ART were selected (four public and nonprofit private health facilities from each region). A multi-stage random sampling method was employed. Using the Ministry of Health (MOH) documents (2011), all health units with ≥50 clients aged 0–15 years were included in the sampling frame. This is because the MOH data is captured using 0–15 years and 15 years and above. The regions were purposively selected because the majority of the area is rural, whereas the previous studies [25, 36] on perinatally HIV infected adolescents were performed in the central region. Three facilities were selected by simple random sampling and one regional hospital was purposively selected since it is the referral hospital of the region. Each of the clinics provides ART and counseling regarding drug adherence, and general care.
Participants
Perinatally HIV-infected adolescents aged 10–19 years were recruited between September 2013 and March 2014. The sample size was calculated using Kish Leslie formula [37]. We assumed probability of poor HRQoL of 50 %, an acceptable error of 5 %, and Z value of 1.96 and a design effect of two. To obtain a final estimated sample size of 672, the goal was to recruit 56 participants consecutively from each health facility.
Data collection methods
Data were collected using interviewer-administered questionnaires that included questions about socio-demographic characteristics, sexuality, disclosure of HIV sero-status, sexually transmitted infections, contraception, pregnancy and procreation intentions, parental communication and sex education, peer influence and access and utilization of SRH services. To measure HRQoL, the Medical Outcomes Study HIV Health Survey instrument (MOS-HIV) was used [38]. We used an English version which has been culturally adapted, translated and validated in Uganda [39]. This English version was translated to four major languages (Lusoga, Ateso, Luo and Runyakitara) where the adolescents were recruited. The participants who were able to speak English responded in English (Majority) and those who did not know English responded in their respective languages. These languages are spoken widely in the areas where the data was collected. The tool includes 35 questions that assess eleven dimensions of health including; General Health Perceptions (GHP), Pain (P), Physical Functioning (PF), Role Functioning (RF), Social Functioning (SF), Mental Health (MH), Energy/Fatigue (EF), Health Distress (HD), Cognitive Function (CF), Quality of Life (QL) and Health Transition (HT). All items are answered on a scale of two, three, five or six response options. The MOS-HIV subscales are scored as summated rating scales and transformed on a 0–100 scale where higher scores indicate better health. Furthermore, a Physical Health Summary score (PHSS) and a Mental Health Summary score (MHSS), both on a 0–100 scale, can be generated by standardizing the scores using the weighting coefficients estimated in a previous study and provided by the author of the questionnaire [40, 41]. The data was not normally distributed, so we used the median instead of mean as a cut off for better and poorer HRQoL in the PHS and MHS (Fig. 1). Both scores were dichotomized at their respective medians yielding ordinal binary better and poorer HRQoL.
Fig. 1.
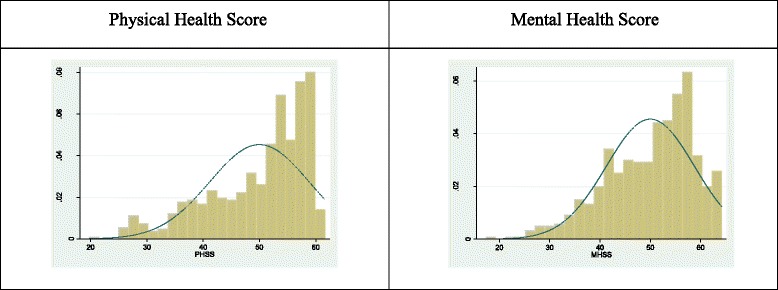
Distribution of physical and mental scores after Principal Component Analysis
Data analysis
Demographics characteristics were sumararised in frequency and percentage. Participant’s age was grouped into 10–14 years and 15–19 years. Education status was grouped into in school and out of school and education level was grouped into three categories: no education, primary and secondary. Occupation was grouped into three categories: students, unemployed and volunteers (employed). Living with parents was grouped into; one parent-means staying with at least one parent and not staying with a parent means not staying with any parent.
The outcome variable was better HRQoL as measured by the MOS-HIV instrument. The independent variables were socio-demographic characteristics (age, sex, education status, level of education hoped to complete and distance to clinic), medical factors (ART, disclosure of HIV status and comorbidities) SRH (ever had sex, pregnancy, condom use, contraceptive use, utilization of SRH services and parent communication on sexuality) and life style factors (smoking and alcohol use). To determine factors associated with better HRQoL on the PHSS and MHSS, we used the median as a cut-off as described previously. The outcome was defined as 1 if scores were greater or equal to the median and 0 if scores were below the median. Bivariate logistic regression analysis was carried out to determine associations between the outcome variable (HRQoL) and the independent factors. After checking for collinearity, all variables with a P value of ≤0.2 at the bivariate analysis were included in the multiple logistic regression models. During model development, all predictor variables with a p-value of ≤0.2 [42] at bivariate analysis were considered for inclusion in the multivariate logistic regression model. We used the likelihood ratio test to check for model fit by dropping insignificant variables first and refit the model until we got the best fit. Collinearity was assessed using a correlation matrix and cross-checked by the use of variance inflation factor which was set at ten [43]. In case two variables were associated (P <0.05), the variable explaining the largest variability (smaller p value at univariate analysis) was retained. Significance was set at 0.05 and all of the analyses were two tailed. Analyses were done using STATA®12.
Ethical consideration
Ethical approval was obtained from the Higher Degrees and Research Ethics committee, College of Health Sciences, Makerere University and Uganda National Council for Science and Technology (REC REF 2012-085). Administrative clearance and permissions were obtained from the management of the health facilities. Both written and verbal consents were obtained from adolescents above 18 years. For adolescents below 18 years, assent as well as consent from parents or guardians was obtained. Participation was voluntary and all the interviews were conducted in privacy and participant’s confidentiality was maintained throughout the study by giving an identification number on the questionnaire.
Results
Table 1 summarizes the characteristics of 614 participants. Of these 361(58.8 %) were males. The mean, standard deviation (SD) and median, interquartile range (IQR) age for the participants were 16.2 (2.06) and 16 (15–18) years respectively. For males, the mean age was 15.9 (SD 2.3) and for females 16.4 (SD 1.8) years. Overall, 500 (81.4 %) were aged 15–19 years, 455 (74.1 %) were enrolled in school and 374 (60.9 %) hoped to complete tertiary education; and 269 (43.8 %) had lost both parents. The median PHSS was 52.9 (IQR 44.6–57.4) and MHSS was 51.5 (IQR 44.0–56.9) for the whole sample. Figure 2 shows median PHSS and MHSS for the whole sample, males and females and different age groups. The difference between males and females and age groups with respect to summary scores was not statistically significant.
Table 1.
Descriptive statistics on the sample of HIV perinatally infected adolescents (n = 614)
| Variables | Frequency | Percentage | |
|---|---|---|---|
| Sex | Male | 253 | 41.2 |
| Female | 361 | 58.8 | |
| Age groups | 10 – 14 years | 114 | 18.6 |
| 15 – 19 years | 500 | 81.4 | |
| Religion | Catholic | 257 | 41.9 |
| Protestant | 247 | 40.2 | |
| Others | 110 | 17.9 | |
| Education status | Out of school | 159 | 25.9 |
| In school | 455 | 74.1 | |
| Highest Level of education attained | None | 29 | 4.7 |
| Primary level | 355 | 57.2 | |
| Secondary level | 230 | 37.5 | |
| Highest level of education hoped to complete | Primary | 63 | 10.3 |
| Secondary | 106 | 17.3 | |
| Tertiary | 374 | 60.9 | |
| Don’t know | 71 | 11.6 | |
| Occupation | Students | 455 | 74.1 |
| Volunteers | 49 | 8 | |
| Stays home | 110 | 17.9 | |
| Region | Western | 229 | 37.3 |
| Eastern | 172 | 28 | |
| Northern | 213 | 34.7 | |
| Distance to clinic | Within 5 km | 193 | 31.4 |
| More than 5 km | 421 | 68.6 | |
| Living with parents | Both parents | 103 | 16.8 |
| One parent | 243 | 39.4 | |
| Not staying with any parents | 268 | 43.6 |
Fig. 2.
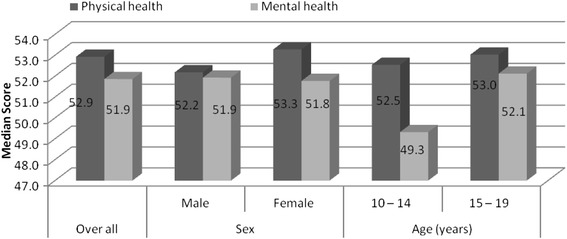
Median scores for PHS and MHS of the sample of HIV perinatally infected adolescents (n = 614)
Table 2 shows unadjusted association between socio demographics characteristics and PHSS and MHSS. Adolescents in school were more likely (OR: 1.53, 95 % CI 1.06–2.20) to present with better mental health than those out of school. Adolescents in secondary level of education were 9 times (OR: 9.44, 95 % CI 3. 28.04) and 5 times (OR: 5.48, 95 % CI 2.15–13.99) more likely to present with a better mental health and physical health respectively compared to those adolescents with no formal education. Adolescents who were unemployed were less likely to present with better mental health (OR: 0.46, 95 % CI 0.29–0.74) than those adolescents who were employed.
Table 2.
Unadjusted odds ratios of socio-demographics factors associated with PHS and MHS
| Physical health | Mental health | ||||||
|---|---|---|---|---|---|---|---|
| Crude OR | 95 % CI | P | Crude OR | 95 % CI | P | ||
| Sex | Male | Ref | |||||
| Female | 1.22 | 0.89 –1.69 | 0.219 | 0.99 | 0.72 – 1.36 | 0.94 | |
| Age groups | 10 – 14 years | Ref | |||||
| 15 – 19 years | 1.04 | 0.70 – 1.57 | 0.836 | 1.35 | 0.90 – 2.04 | 0.15 | |
| Religion | Catholic | Ref | |||||
| Protestant | 1.30 | 0.91 – 1.84 | 0.15 | 1.38 | 0.97 – 1.96 | 0.07 | |
| Others | 1.39 | 0.87 – 2.19 | 0.15 | 1.44 | 1.91 – 2.26 | 0.12 | |
| Education status | Out of school | Ref | |||||
| In school | 1.38 | 0.96 – 1.99 | 0.081 | 1.53 | 1.06 – 2.20 | 0.02 | |
| Level of education | None | Ref | |||||
| Primary level | 3.38 | 1.34 – 8.51 | 0.01 | 5.27 | 1.79 – 15.45 | 0.00 | |
| Secondary level | 5.48 | 2.15 – 13.99 | 0.00 | 9.44 | 3.18 – 28.04 | 0.00 | |
| Occupation | Students | Ref | |||||
| Volunteers | 0.82 | 0.45 – 1.49 | 0.509 | 1.21 | 0.66 – 2.22 | 0.54 | |
| Stays home | 0.82 | 0.52 – 1.31 | 0.416 | 0.46 | 0.29 – 0.75 | 0.00 | |
| Region | Western | Ref | |||||
| Eastern | 0.26 | 0.17 – 0.39 | 0.00 | 0.69 | 0.47 – 1.03 | 0.07 | |
| Northern | 1.1 | 0.76 – 1.62 | 0.595 | 0.61 | 0.42 – 0.89 | 0.01 | |
| Distance to clinic | Within 5 km | Ref | |||||
| More than 5 km | 0.68 | 0.49 – 0.96 | 0.03 | 0.90 | 0.64 – 1.26 | 0.52 | |
| α Living with parents | Both parents | Ref | |||||
| One parent | 1.09 | 0.69 – 1.74 | 0.69 | 0.96 | 0.61 – 1.53 | 0.88 | |
| Not staying with a parent | 1.46 | 0.87 – 2.16 | 0.17 | 0.90 | 0.63 – 1.56 | 0.96 | |
α Living with parents (whether the adolescent is living with parent) - One parent-means staying with at least one parent and Not staying with a parent means not staying with any parent
Table 3 shows unadjusted association between medical, SRH characteristics with PHSS and MHSS. Adolescents on ARV were twice more likely to present with better physical health (OR: 2.3, 95 % CI 1.47–4.11) and four times more likely to present with better mental health (OR: 4.11, 95 % CI 2.50–6.77) as compared to those not on ARV. The adolescents who had one sexual partner were more likely to present with better mental health (OR: 1.94, 95 % CI 1.00–3.74) compared to those with two or more sexual partners. Adolescents who were not communicating with their guardians on sexuality issues were less likely (OR: 0.69, 95 % CI 0.50–0.97) to present with better mental health compared to those who talked with their guardians about sexuality issues. The adolescents who were not smoking were nearly twice likely (OR 1.7, 95 % CI: 1.09–2.74) present with better physical health than those adolescents who were smoking.
Table 3.
Unadjusted odds ratios of SRH and life style factors associated with PHS and MHS
| PHS | MHS | ||||||
|---|---|---|---|---|---|---|---|
| Crude OR | 95 % CI | P | Crude OR | 95 % CI | P | ||
| Currently on ARVs | No | Ref | 1.47–3.62 | 0.00 | 4.11 | 2.50–6.77 | 0.00 |
| Yes | 2.3 | ||||||
| Ever had sex | No | Ref | 0.62–1.20 | 0.395 | 0.92 | 0.65–1.28 | 0.61 |
| Yes | 0.87 | ||||||
| Age at first sex | <16 years | 0.95 | 0.54–1.64 | 0.851 | 0.82 | 0.47–1.42 | 0.48 |
| ≥16 years | |||||||
| Number of sexual partners | None | Ref | 1.00–3.74 | 0.05 | |||
| One | 1.26 | 0.66–2.40 | 0.48 | 1.9 | 0.71–4.06 | 0.20 | |
| >1 more | 1.52 | 0.64–3.59 | 0.34 | 1.7 | |||
| Ever been married | No | Ref | |||||
| Yes | 1.79 | 0.93–3.45 | 0.084 | 0.6 | 0.31–1.18 | 0.14 | |
| Ever disclosed HIV status | No | Ref | |||||
| Yes | 1.06 | 0.67–1.68 | 0.802 | 1.25 | 0.79–1.9 | 0.34 | |
| Ever been treated for an STD/STI | No | 1 | 0.52–1.23 | 0.324 | 1.14 | 0.74–1.75 | 0.56 |
| Yes | 0.8 | ||||||
| Using family planning | No | Ref | 0.57–1.18 | 0.287 | 1.19 | 0.83–1.71 | 0.33 |
| Yes | 1.07 | ||||||
| Ever been pregnant | No | Ref | 0.65–1.74 | 0.8 | 0.78 | 0.48–1.28 | 0.33 |
| Yes | 1.07 | ||||||
| Wants to have child in the future | No | Ref | 0.52–1.24 | 0.327 | 1.51 | 0.97–2.34 | 0.06 |
| Yes | 0.8 | ||||||
| Parent adolescent communication on sexuality. | Yes | Ref | 0.55–1.06 | 0.106 | 0.69 | 0.50–0.97 | 0.03 |
| No | 0.76 | ||||||
| Ever smoked cigarette | No | Ref | 1.09–2.74 | 0.02 | 2.05 | 0.76–5.52 | 0.15 |
| Yes | 1.7 | ||||||
| Ever drunk alcohol | No | Ref | 0.41–1.07 | 0.10 | 1.75 | 0.76–2.02 | 0.34 |
| Yes | 0.67 | ||||||
| Having a friend who is smoker | No | Ref | 0.96–1.94 | 0.08 | 0.71 | 0.45–1.11 | 0.14 |
| Yes | 1.3 | ||||||
| Having friend who is drinking alcohol | No | Ref | |||||
| Yes | 0.73 | 0.52–1.03 | 0.081 | 1.02 | 0.69–1.38 | 0.88 | |
| Satisfied with the SRH service | Yes | Ref | 0.28–0.73 | 0.00 | 0.26 | 0.15–0.44 | |
| No | 0.46 | 0.00 | |||||
Table 4 shows the adjusted association of the independent variables and PHSS. Adolescents on ART were twice as likely to present with better physical health (AOR 2.07, 95 % CI: 1.24–3.46) compared to those who were not on ARVs. Furthermore, adolescents who had friends who smoked were less likely (AOR 0.48, 95 % CI: 0.29–0.80) to present with better physical health than those who did not have a friend who smoked. Adolescents recruited from the Northern region were less likely to present with better mental health (AOR 0.25, 95 % CI: 0.16–0.42) compared to adolescents from other regions.
Table 4.
Adjusted odds ratios of SRH, life style factors and socio-demographic factors associated with PHS
| Variables | PHSS | |||
|---|---|---|---|---|
| No (%) | AOR | 95 % CI | P | |
| Highest level of education hoped to complete | ||||
| Primary | 63(10.3) | Ref | ||
| Secondary | 106((17.3) | 0.41 | 0.20–0.85 | 0.01 |
| Tertiary | 374(60.9) | 1.01 | 0.55–1.88 | 0.56 |
| Don’t know | 71(11.6) | 0.67 | 0.31–1.50 | 0.34 |
| Region | ||||
| Western | 229(37.2) | Ref | ||
| Eastern | 172(28.0) | 1.13 | 0.73–1.75 | 0.57 |
| Northern | 213(34.7) | 0.25 | 0.16–0.42 | <0.001 |
| Distance to clinic | ||||
| Within 5 km | 193(34.7) | Ref | ||
| Within 20 km | 421(68.6) | 0.69 | 0.38–1.26 | 0.23 |
| Currently on ARVs | ||||
| No | 100 | Ref | ||
| Yes | 513 | 2.07 | 1.24–3.36 | Ref |
| Parent adolescent communication on sexuality | ||||
| No | 224 | Ref | ||
| Yes | 386 | 0.87 | 0.59–1.27 | 0.47 |
| Has a friend who is smoking cigarette | ||||
| No | 91 | Ref | ||
| Yes | 520 | 0.48 | 0.29–0.80 | <0.001 |
| Satisfied with the SRH service | ||||
| No | 88 | Ref | ||
| Yes | 521 | 0.69 | 0.41–1.16 | 0.17 |
AOR adjusted odds ratio, adjusted for variables included in the model
Table 5 shows the adjusted association of the independent variables and MHSS. Adolescents in secondary school were five times more likely to present with better mental health than those who did not have any form of education (AOR 5.3, 95 % CI: 1.86–15.41). Adolescents recruited from the Northern region were less likely (AOR 0.50, 95 % CI: 0.32–0.78) to present with better mental health than those recruited from other regions. Adolescents on ART were four time more likely to present with a better mental health (AOR 3.9, 95 % CI: 2.22–6.9). Participants who desired to have a child in future were two times more likely (AOR 1.7, 95 % CI: 1.05–3.00) to present with a better mental health than those who never intended to have children in the future. Adolescents who never discussed with their guardians on sexuality issues were less likely (AOR 0.6, 95 % CI: 0.40–0.89), to present with a better mental health compared to those who discussed with their guardians. Adolescents who had friends who smoked were less likely (AOR 0.57, 95 % CI: 0.35–0.98) to present with a better mental health. Adolescents who were not satisfied with SRH services were less likely (AOR 0.34, 95 % CI: 0.18–0.62) to present with a better mental health.
Table 5.
Adjusted odds ratios of SRH, life style, and socio demographic factors associated MHS
| MHSS | ||||
|---|---|---|---|---|
| AOR | 95 % CI | |||
| Religion | ||||
| Catholic | 257(41.9) | Ref | ||
| Protestant | 246(40.2) | 1.2 | 0.77–1.76 | 0.46 |
| Others | 110(17.6) | 1.7 | 0.93–4.74 | 0.25 |
| Level of education. | ||||
| None | 29(4.7) | Ref | ||
| Primary | 355(57.2) | 3.3 | 1.18–9.38 | 0.02 |
| Secondary | 230(37.5) | 5.3 | 1.86–15.41 | <0.00 |
| Region | ||||
| Western | 229(37.30 | Ref | ||
| Eastern | 172(28.0 %) | 0.78 | 0.4–1.24 | 0.29 |
| Northern | 213(34.7 %) | 0.50 | 0.32–0.78 | <0.001 |
| Distance to clinic | ||||
| <5 km | 193(34.7) | Ref | ||
| >5 km | 421(68.6) | 0.63 | 0.38–1.05 | 0.08 |
| Living with parents | ||||
| Both parents | 103(16.8) | Ref | ||
| One parent | 243(39.4) | 0.85 | 0.50–1.44 | 0.54 |
| Not staying with a parent | 268(43.6) | 0.87 | 0.51–1.48 | 0.61 |
| Currently on ARVs | ||||
| No | 100(16.3) | Ref | ||
| Yes | 513(83.7) | 3.9 | 2.22–6.92 | <0.001 |
| Wants to have a child in the future | ||||
| No | 97(16..3) | Ref | ||
| Yes | 498(83.7) | 1.7 | 1.05–3.00 | 0.03 |
| Parent and adolescent communicating on sexuality issues. | ||||
| Yes | 224(36.7) | Ref | ||
| No | 386(63.3) | 0.6 | 0.40–0.89 | 0.01 |
| Friend who is smoking | ||||
| No | 91 (14.9) | Ref | ||
| Yes | 520(85.1) | 0.57 | 0.34–0.98 | 0.04 |
| Satisfied with the SRH service | ||||
| Yes | 92(15.0) | Ref | ||
| No | 521(85.0) | 0.34 | 0.18–0.62 | <0.00 |
AOR adjusted odds ratio, adjusted for variables included in the model
Discussion
There were no associations between SRH (ever had sex, ever been pregnant, condom use, contraceptive use) or lifestyle factors and physical health. However, adolescents on ARV were twice more likely to present with a better physical and four times more likely to present with better mental health as compared to those not on ARV and adolescents living in the Northern region or who had a friend who smoked were more likely to present with a worse physical or mental health compared to those living in the Western region or who did not have a friend who smoked. Adolescents who wanted to present with children in the future were more likely to have a better mental health. Not communicate with guardians about sexuality or who were dissatisfied with SRH services was associated with poorer mental health.
ART is effective in improving the self-rated HRQoL by improving the immune status of the patients [44, 45]. Our study shows perinatally -infected adolescents on ART had better physical and mental health compared to those who were not on treatment. This is in line with other studies that show that people on ART have better HRQoL [17, 46, 47]. There is thus a critical need to provide ART for adolescents who acquire HIV perinatally since treatment improves both the physical and mental domains of HRQOL.
Life style factors were not associated with HRQoL. Smoking increases the risks of developing serious illnesses like chronic obstructive pulmonary diseases or non-compliance to HIV treatment plan [48, 49]. Although there was no association between smoking and HRQoL in the current study, the adolescents who had a friend who was smoking were less likely to have better physical or mental health. Second hand smoke exposure in studies with adults been shown to be associated with reduced HRQoL [50, 51] and causes cardiovascular diseases and lung cancer [52, 53]. This may not be any different from adolescents.
SRH experiences may be associated with HRQoL, with effects that may be positive or negative. Because adolescents who want to have a family have something positive they look forward to, they are more likely to have a better mental health [54, 55], especially if they conceive. This study showed that adolescents who wanted to have children in the future were more likely to present with a better mental health. However, HIV positive pregnant women may experience increased health distress and worse health transition during the antenatal period compared to HIV negative pregnant women, mainly because of decreased social support and concern of the physical health of their children [56, 57]. Some HIV positive women become pregnant to avoid the stigma associated with childlessness and being identified as being HIV positive in their communities [58]. Yet others who get pregnant or are sexually active face criticism from the community because of potential transmission of HIV to their children or transmission to other community members [59]. These issues may influence HRQoL.
Parent communication on sexuality issues influences young people’s sexual behavior, which in turn affects HRQoL [60]. In this study, adolescents who communicated less with their parents were less likely to present with better mental health. Parent communication is highly influential in adolescents’ behavior as it could help them to develop positive individual values and make sexually healthy decisions, thus translating into an influence on HRQoL. Studies in Tanzania and elsewhere have found that parental communication improves outcomes of SRH and HIV prevention [61–63], which may translate into better HRQoL. There is a need for interventions such as parenting skills building that might enable parents to improve their relationships with their maturing children. This would equip parents with the appropriate skills for positive guidance and communication of their children and enhance safe sexual behaviors and SRH outcomes.
The study showed that participants recruited from northern region of the country reported poorer physical and mental health. This may be due to the northern region is being a post conflict area and studies have shown that people in general have higher rates of depression [64, 65]. This may affect the health related quality of life.
The study had several limitations. Due to the fact that sexual behaviour was self-reported, there was a potential of recall bias or under-reporting of sexual behaviour. Participants may have forgotten or may be embarrassed to reveal information on their sexual activity, especially for the females, and males may have exaggerated on issues on sexuality [66]. There could be a selection bias because of the way units were selected, as only health units with large numbers were selected. The results of the study may only be generalizable to the study population or other similar settings. We did not stratify the findings depending on clinic attended; this may affect the health related quality of life due to the differences in quality of services or care offered in the individual ART clinic. However, additionally, the strength of this study was the large sample size of perinatally HIV-infected adolescents. Furthermore, this study attempted to link SRH and life style factors with HRQoL. Secondly, the study used a standardised tool (MOS-HIV) that has been culturally adapted. Thirdly, data was collected in three regions of the country and from referral hospitals that are fairly representative of the general population in Uganda.
In our study gender was not associated with quality of life. However studies have shown that gender affects health transition, perceived HRQoL, health distress, social functioning and role functioning in the adult population [67–69]. Future research on gender and age differences (and their interaction) may provide potentially useful information for planning interventions to improve QoL and mental health among people infected with HIV/AIDS especially in perinatally HIV-infected adolescents. In addition, this was a cross sectional study which cannot evaluate causal relationships. There is need to study the effect of SRH and life style factors on HRQoL in a prospective or retrospective longitudinal study so that we can understand the cause-and-effect relationship between SRH, life style factors and HRQoL. Such studies could assess the effect of HRQoL on SRH and life style factors. Furthermore, this study did not assess the effect clustering due to belonging to a particular ART clinic yet quality of services offered may affect HRQoL. Future studies should assess the effect of clustering on HRQoL.
Conclusion
There was no association between SRH (ever had sex, ever been pregnant, condom use, contraceptive use) or life style factors and physical health. Adolescents on ARV were twice more likely to present with a better physical and four times more likely to present with mental health as compared to those not on ARV. Adolescents who wanted to present with children in the future were more likely to present with a better mental health . Poor mental health outcomes were associated with not having communication with guardians about sexuality or with their dissatisfaction with SRH services. There is need to design and integrate age appropriate and culturally valid screening and management of mental health in SRH services for perinatally HIV-infected adolescents.
Acknowledgements
The authors extend their gratitude and appreciation to all the participants who participated in the study, the staff of health facilities where the study was carried out. Doctoral committee members and field coordinator Ninsiima Gloria.
The work was supported by Grant Number 5R24TW008886 supported by OGAC, NIH and HRSA. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the supporting offices.
This research was partially supported by the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Wellcome Trust (UK) (Grant No: 087547/Z/08/Z), the Department for International Development (DfID) under the Development Partnerships in Higher Education (DelPHE), the Carnegie Corporation of New York (Grant No: B 8606), the Ford Foundation (Grant No: 1100–0399), Google.Org (Grant No: 191994), Sida (Grant No: 54100029) and MacArthur Foundation (Grant No: 10-95915-000-INP).
Footnotes
Competing interests
The authors declare that they have no competing interests
Authors’ contributions
SNM designed the study, collected and analyzed the data, drafted the paper NK designed the study and reviewed the paper. LEE designed the study and reviewed the paper and DK designed the study, analysed the data and reviewed the paper. All the authors approved the final draft of the paper.
Contributor Information
Scovia Nalugo Mbalinda, Email: snmbalinda@gmail.com.
Noah Kiwanuka, Email: nkiwanuka@gmail.com.
Dan K. Kaye, Email: dankkaye@yahoo.com
Lars E. Eriksson, Email: Lars.Eriksson@ki.se
References
- 1.Joint United Nations Programme on HIV/AIDS . Report on the Global AIDS Epidemic. 2013. [Google Scholar]
- 2.Joint United Nations Programme on HIV/AIDS . Global fact sheet. 2013. [Google Scholar]
- 3.Uganda Ministry of Health and ICF International . 2011 Uganda AIDS Indicator Survey: Key Findings. Calverton, Maryland, USA: MOH and ICF International; 2012. [Google Scholar]
- 4.Fund UNCs . Children and AIDS sixth stocktaking report. 2013. [Google Scholar]
- 5.Kaplan RM, Ries AL. Quality of life: concept and definition. Copd. 2007;4:263–271. doi: 10.1080/15412550701480356. [DOI] [PubMed] [Google Scholar]
- 6.Miners A, Phillips A, Kreif N, Rodger A, Speakman A, Fisher M, et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV. 2014;1:e32–e40. doi: 10.1016/S2352-3018(14)70018-9. [DOI] [PubMed] [Google Scholar]
- 7.Mburu G, Ram M, Oxenham D, Haamujompa C, Iorpenda K, Ferguson L. Responding to adolescents living with HIV in Zambia: a social–ecological approach. Child Youth Serv Rev. 2014;45:9–17. doi: 10.1016/j.childyouth.2014.03.033. [DOI] [Google Scholar]
- 8.Kang E, Mellins CA, Ng WYK, Robinson L-G, Abrams EJ. Standing between two worlds in Harlem: a developmental psychopathology perspective of perinatally acquired human immunodeficiency virus and adolescence. J Appl Dev Psychol. 2008;29:227–237. doi: 10.1016/j.appdev.2008.02.001. [DOI] [Google Scholar]
- 9.Rydstrom LL, Ygge BM, Tingberg B, Naver L, Eriksson LE. Experiences of young adults growing up with innate or early acquired HIV infection—a qualitative study. J Adv Nurs. 2013;69:1357–1365. doi: 10.1111/j.1365-2648.2012.06127.x. [DOI] [PubMed] [Google Scholar]
- 10.Wiklander M, Rydstrom LL, Ygge BM, Naver L, Wettergren L, Eriksson LE. Psychometric properties of a short version of the HIV stigma scale, adapted for children with HIV infection. Health Qual Life Outcomes. 2013;11:1477–7525. doi: 10.1186/1477-7525-11-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Domek GJ. Social consequences of antiretroviral therapy: preparing for the unexpected futures of HIV-positive children. Lancet. 2006;367:1367–1369. doi: 10.1016/S0140-6736(06)68584-X. [DOI] [PubMed] [Google Scholar]
- 12.Lafort Y, Geelhoed D, Cumba L, Lazaro C, Delva W, Luchters S, et al. Reproductive health services for populations at high risk of HIV: performance of a night clinic in Tete province, Mozambique. BMC Health Serv Res. 2010;10:1472–6963. doi: 10.1186/1472-6963-10-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nyamukapa CA, Gregson S, Lopman B, Saito S, Watts HJ, Monasch R, et al. HIV-associated orphanhood and children’s psychosocial distress: theoretical framework tested with data from Zimbabwe. Am J Public Health. 2008;98:133–141. doi: 10.2105/AJPH.2007.116038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petersen I, Bhana A, Myeza N, Alicea S, John S, Holst H, et al. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: a qualitative investigation. AIDS Care. 2010;22:970–978. doi: 10.1080/09540121003623693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bush-Parker T. Perinatal HIV: children with HIV grow up. Focus. 2000;15:1–4. [PubMed] [Google Scholar]
- 16.Foster C, Waelbrouck A, Peltier A. Adolescents and HIV infection. Curr Opin HIV AIDS. 2007;2:431–436. doi: 10.1097/COH.0b013e3282ced150. [DOI] [PubMed] [Google Scholar]
- 17.Alibhai A, Martin LJ, Kipp W, Konde-Lule J, Saunders LD, Rubaale T, et al. Quality of life of HIV patients in a rural area of western Uganda: impact of a community-based antiretroviral treatment program. Curr HIV Res. 2010;8:370–378. doi: 10.2174/157016210791330400. [DOI] [PubMed] [Google Scholar]
- 18.Jelsma J, Maclean E, Hughes J, Tinise X, Darder M. An investigation into the health-related quality of life of individuals living with HIV who are receiving HAART. AIDS Care. 2005;17:579–588. doi: 10.1080/09540120412331319714. [DOI] [PubMed] [Google Scholar]
- 19.Flicker S, Skinner H, Read S, Veinot T, McClelland A, Saulnier P, et al. Falling through the cracks of the big cities: who is meeting the needs of HIV-positive youth? Can J Public Health. 2005;96:308–312. doi: 10.1007/BF03405172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Domek GJ. Facing adolescence and adulthood: the importance of mental health care in the global pediatric AIDS epidemic. J Dev Behav Pediatr. 2009;30:147–150. doi: 10.1097/DBP.0b013e318196b0cc. [DOI] [PubMed] [Google Scholar]
- 21.Wood SM, Shah SS, Steenhoff AP, Rutstein RM. The impact of AIDS diagnoses on long-term neurocognitive and psychiatric outcomes of surviving adolescents with perinatally acquired HIV. AIDS. 2009;23:1859–1865. doi: 10.1097/QAD.0b013e32832d924f. [DOI] [PubMed] [Google Scholar]
- 22.Aranda-Naranjo B. Quality of life in the HIV-positive patient: implications and consequences. J Assoc Nurses AIDS Care. 2004;15:20S–27S. doi: 10.1177/1055329004269183. [DOI] [PubMed] [Google Scholar]
- 23.Douaihy A, Singh N. Factors affecting quality of life in patients with HIV infection. AIDS Read. 2001;11:450–454. [PubMed] [Google Scholar]
- 24.Ogbuji QC, Oke AE. Quality of life among persons living with HIV infection in Ibadan, Nigeria. Afr J Med Med Sci. 2010;39:127–135. [PubMed] [Google Scholar]
- 25.Bakeera-Kitaka S, Nabukeera-Barungi N, Nostlinger C, Addy K, Colebunders R. Sexual risk reduction needs of adolescents living with HIV in a clinical care setting. AIDS Care. 2008;20:426–433. doi: 10.1080/09540120701867099. [DOI] [PubMed] [Google Scholar]
- 26.Brogly SB, Watts DH, Ylitalo N, Franco EL, Seage GR, 3rd, Oleske J, et al. Reproductive health of adolescent girls perinatally infected with HIV. Am J Public Health. 2007;97:1047–1052. doi: 10.2105/AJPH.2005.071910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organisation . Strengthening the health sector response to adolescent health and development. Geneva: (CAH) DoCaAHaD ed; 2009. [Google Scholar]
- 28.Hill LM, Maman S, Groves AK, Moodley D. Social support among HIV-positive and HIV-negative adolescents in Umlazi, South Africa: changes in family and partner relationships during pregnancy and the postpartum period. BMC Pregnancy Childbirth. 2015;15:015–0542. doi: 10.1186/s12884-015-0542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nzioka C. Dealing with the risks of unwanted pregnancy and sexually transmitted infections among adolescents: some experiences from Kenya. Afr J Reprod Health. 2001;5:132–149. doi: 10.2307/3583331. [DOI] [PubMed] [Google Scholar]
- 30.Birungi H, Mugisha JF, Nyombi J, FOHEH N. Sexual and reproductive health needs of adolescents perinatally infected with HIV in Uganda. 2008. [Google Scholar]
- 31.Kanniappan S, Jeyapaul MJ, Kalyanwala S. Desire for motherhood: exploring HIV-positive women’s desires, intentions and decision-making in attaining motherhood. AIDS Care. 2008;20:625–630. doi: 10.1080/09540120701660361. [DOI] [PubMed] [Google Scholar]
- 32.Hattori MK, Longfield K. Sexual role expectations, mistrust, and sexual violence among young people in East and Southern Africa: implications for HIV prevention. Washington: Population Services International; 2008. [Google Scholar]
- 33.Chen WT, Shiu CS, Yang JP, Simoni JM, Fredriksen-Goldsen KI, Lee TS, et al. Antiretroviral Therapy (ART) side effect impacted on quality of life, and depressive symptomatology: a mixed-method study. J AIDS Clin Res. 2013;4:218. doi: 10.4172/2155-6113.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Basavaraj KH, Navya MA, Rashmi R. Quality of life in HIV/AIDS. Indian J Sex Transm Dis. 2010;31:75–80. doi: 10.4103/0253-7184.74971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hays RD, Cunningham WE, Sherbourne CD, Wilson IB, Wu AW, Cleary PD, et al. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV Cost and Services Utilization Study. Am J Med. 2000;108:714–722. doi: 10.1016/S0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- 36.Birungi H, Mugisha JF, Obare F, Nyombi JK. Sexual behavior and desires among adolescents perinatally infected with human immunodeficiency virus in Uganda: implications for programming. J Adolesc Health. 2009;44:184–187. doi: 10.1016/j.jadohealth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Kish L (Ed.). survey sampling. New York: John Wiley and Sons; 1965.
- 38.Wu AW, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV) Qual Life Res. 1997;6:481–493. doi: 10.1023/A:1018451930750. [DOI] [PubMed] [Google Scholar]
- 39.Mast TC, Kigozi G, Wabwire-Mangen F, Black R, Sewankambo N, Serwadda D, et al. Measuring quality of life among HIV-infected women using a culturally adapted questionnaire in Rakai district, Uganda. AIDS Care. 2004;16:81–94. doi: 10.1080/09540120310001633994. [DOI] [PubMed] [Google Scholar]
- 40.Grossman HA, Sullivan PS, Wu AW. Quality of life and HIV: current assessment tools and future directions for clinical practice. AIDS Read. 2003;13:583–590. [PubMed] [Google Scholar]
- 41.Wu AW, Hays RD, Kelly S, Malitz F, Bozzette SA. Applications of the Medical Outcomes Study health-related quality of life measures in HIV/AIDS. Qual Life Res. 1997;6:531–554. doi: 10.1023/A:1018460132567. [DOI] [PubMed] [Google Scholar]
- 42.Hosmer DW, Lemeshow S. Applied logistic regression analysis. New York: Wiley; 2000. [Google Scholar]
- 43.Kutner MH, Nachtsheim CJ, Neter J. Applied linear regression models. Fourth edn. New York: McGraw-Hill Irwin; 2004. [Google Scholar]
- 44.Nglazi MD, West SJ, Dave JA, Levitt NS, Lambert EV. Quality of life in individuals living with HIV/AIDS attending a public sector antiretroviral service in Cape Town, South Africa. BMC Public Health. 2014;14:1471–2458. doi: 10.1186/1471-2458-14-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burgoyne RW, Tan DH. Prolongation and quality of life for HIV-infected adults treated with highly active antiretroviral therapy (HAART): a balancing act. J Antimicrob Chemother. 2008;61:469–473. doi: 10.1093/jac/dkm499. [DOI] [PubMed] [Google Scholar]
- 46.Bomba M, Nacinovich R, Oggiano S, Cassani M, Baushi L, Bertulli C, et al. Poor health-related quality of life and abnormal psychosocial adjustment in Italian children with perinatal HIV infection receiving highly active antiretroviral treatment. AIDS Care. 2010;22:858–865. doi: 10.1080/09540120903483018. [DOI] [PubMed] [Google Scholar]
- 47.Dorz S, Lazzarini L, Cattelan A, Meneghetti F, Novara C, Concia E, et al. Evaluation of adherence to antiretroviral therapy in Italian HIV patients. AIDS Patient Care STDS. 2003;17:33–41. doi: 10.1089/108729103321042890. [DOI] [PubMed] [Google Scholar]
- 48.Hodgson I, Ross J, Haamujompa C, Gitau-Mburu D. Living as an adolescent with HIV in Zambia — lived experiences, sexual health and reproductive needs. AIDS Care. 2012;24:1204–1210. doi: 10.1080/09540121.2012.658755. [DOI] [PubMed] [Google Scholar]
- 49.Helleberg M, Afzal S, Kronborg G, Larsen CS, Pedersen G, Pedersen C, et al. Mortality attributable to smoking among HIV-1-infected individuals: a nationwide, population-based cohort study. Clin Infect Dis. 2013;56:727–734. doi: 10.1093/cid/cis933. [DOI] [PubMed] [Google Scholar]
- 50.Bridevaux PO, Cornuz J, Gaspoz JM, Burnand B, Ackermann-Liebrich U, Schindler C, et al. Secondhand smoke and health-related quality of life in never smokers: results from the SAPALDIA cohort study 2. Arch Intern Med. 2007;167:2516–2523. doi: 10.1001/archinte.167.22.2516. [DOI] [PubMed] [Google Scholar]
- 51.Weeks SG, Glantz SA, De Marco T, Rosen AB, Fleischmann KE. Secondhand smoke exposure and quality of life in patients with heart failure. Arch Intern Med. 2011;171:1887–1893. doi: 10.1001/archinternmed.2011.518. [DOI] [PubMed] [Google Scholar]
- 52.Services. USDoHaH . A report of the surgeon general: how tobacco smoke causes disease: what it means to you. Atlanta: Department of Health and Human Services CfDCaP, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health ed; 2010. [Google Scholar]
- 53.Services. USDoHaH . The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta: Department of Health and Human Services CfDCaP, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health ed; 2014. [Google Scholar]
- 54.Awiti Ujiji O, Ekstrom AM, Ilako F, Indalo D, Rubenson B. I will not let my HIV status stand in the way. Decisions on motherhood among women on ART in a slum in Kenya- a qualitative study. BMC Womens Health. 2010;10:1472–6874. doi: 10.1186/1472-6874-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kwalombota M. The effect of pregnancy in HIV-infected women. AIDS Care. 2002;14:431–433. doi: 10.1080/09540120220123829. [DOI] [PubMed] [Google Scholar]
- 56.Larrabee KD, Monga M, Eriksen N, Helfgott A. Quality of life assessment in pregnant women with the human immunodeficiency virus. Obstet Gynecol. 1996;88:1016–1020. doi: 10.1016/S0029-7844(96)00332-8. [DOI] [PubMed] [Google Scholar]
- 57.Turan B, Stringer KL, Onono M, Bukusi EA, Weiser SD, Cohen CR, et al. Linkage to HIV care, postpartum depression, and HIV-related stigma in newly diagnosed pregnant women living with HIV in Kenya: a longitudinal observational study. BMC Pregnancy Childbirth. 2014;14:400. doi: 10.1186/s12884-014-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hea A-D-A. Issues surrounding reproductive choice for women lying with HIV in Abidjan, Côte d’Ivoire. Reprod Health Matters. 1999;7:20–29. doi: 10.1016/S0968-8080(99)90108-8. [DOI] [Google Scholar]
- 59.Feldman R, Maposhere C. Safer sex and reproductive choice: findings from “positive women: voices and choices” in Zimbabwe. Reprod Health Matters. 2003;11:162–173. doi: 10.1016/S0968-8080(03)02284-5. [DOI] [PubMed] [Google Scholar]
- 60.Wamoyi J, Fenwick A, Urassa M, Zaba B, Stones W. Parental control and monitoring of young people’s sexual behaviour in rural North-Western Tanzania: Implications for sexual and reproductive health interventions. BMC Public Health. 2011;11:106. doi: 10.1186/1471-2458-11-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wamoyi J, Fenwick A, Urassa M, Zaba B, Stones W. Parent–child communication about sexual and reproductive health in rural Tanzania: implications for young people’s sexual health interventions. Reprod Health. 2010;7:6. doi: 10.1186/1742-4755-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Biddlecom A, Awusabo-Asare K, Bankole A. Role of parents in adolescent sexual activity and contraceptive use in four African countries. Int Perspect Sex Reprod Health. 2009;35:72–81. doi: 10.1363/3507209. [DOI] [PubMed] [Google Scholar]
- 63.Opara PI, Eke GK, Akani NA. Mothers perception of sexuality education for children. Niger J Med. 2010;19:168–172. doi: 10.4314/njm.v19i2.56513. [DOI] [PubMed] [Google Scholar]
- 64.Pfeiffer A, Elbert T. PTSD, depression and anxiety among former abductees in Northern Uganda. Confl Health. 2011;5:1752–1505. doi: 10.1186/1752-1505-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Roberts B, Damundu EY, Lomoro O, Sondorp E. Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba, Southern Sudan. BMC Psychiatry. 2009;9:9–7. doi: 10.1186/1471-244X-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mhalu A, Leyna GH, Mmbaga EJ. Risky behaviours among young people living with HIV attending care and treatment clinics in Dar Es Salaam, Tanzania: implications for prevention with a positive approach. J Int AIDS Soc. 2013;16:17342. doi: 10.7448/IAS.16.1.17342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vigneshwaran E, Padmanabhareddy Y, Devanna N, Alvarez-Uria G. Gender differences in health related quality of life of people living with HIV/AIDS in the Era of highly active antiretroviral therapy. N Am J Med Sci. 2013;5:102–107. doi: 10.4103/1947-2714.107526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pereira M, Canavarro MC. Gender and age differences in quality of life and the impact of psychopathological symptoms among HIV-infected patients. AIDS Behav. 2011;15:1857–1869. doi: 10.1007/s10461-011-9928-8. [DOI] [PubMed] [Google Scholar]
- 69.Tesfay A, Gebremariam A, Gerbaba M, Abrha H. Gender differences in health related quality of life among people living with HIV on highly active antiretroviral therapy in Mekelle Town, Northern Ethiopia. Biomed Res Int. 2015;516369:6. doi: 10.1155/2015/516369. [DOI] [PMC free article] [PubMed] [Google Scholar]


