Abstract
OBJECTIVES
To describe a case from 1908 of apparent brain death after operative intervention by Harvey Cushing at the Johns Hopkins Hospital.
METHODS
After institutional review board approval, which waived the requirement of informed consent from patients, and through the courtesy of the Alan Mason Chesney Archives, we reviewed the Johns Hopkins Hospital surgical files from 1896 to 1912.
RESULTS
We selected a single adult patient operated upon by Cushing, whose respirations ceased in the operating room and who was maintained by the use of artificial respiration via a tracheostomy during a 36-hour period, whereas further surgical interventions were performed in an attempt to improve his condition. The patient’s condition remained unimproved; artificial respirations were discontinued and the “cessation of all cardiac activity” was observed.
CONCLUSIONS
Brain death is a concept that presents unique challenges to the practicing physician. Although recent advances have allowed for better diagnosis of brain death, the topic remains fraught with controversy. The case described here documents Harvey Cushing’s struggles with the ethics of maintaining vital organ function with artificial respiration, despite clear evidence of irreversible ischemic brain damage. This case predates the earliest descriptions of brain death by more than 50 years and illustrates the dilemmas facing clinicians at the turn of the twentieth century.
Keywords: Artificial respiration, Brain death, Harvey Cushing
INTRODUCTION
Clinical death, historically, was defined as the permanent cessation of function of the heart and lungs (3). With the advent of mechanical life support technology, vital functions such breathing and heartbeat can be sustained regardless of brain function. The invention of the artificial respirator by Bjorn Ibsen in the early 1950s ushered in a new era of debate over the definition of “death” (12).
French neurologists Mollaret and Goulon introduced in 1959 a series of 23 patients with coma dépassé, or irreversible coma, and are credited with the first descriptions of brain death (5). These patients exhibited flat electroencephalogram (EEG) tracings along with permanent loss of consciousness, brainstem reflexes, and respirations (5, 9). In 1968, an ad hoc committee at Harvard Medical School established the first set of guidelines to diagnose brain death (2). This landmark report defined irreversible coma as a new criterion for death and listed steps to be taken by physicians to diagnose this condition. In 1971, Mohandas and Chou (4) reported that brainstem damage was a critical component of irreversible brain damage and diagnosis of brain death could be made through clinical examination of cranial nerve reflexes.
The Uniform Determination of Death Act of 1981 issued by the President’s Commission confirmed the legal standing of brain death, stating: “an individual who has sustained an irreversible cessation of all function of the entire brain, including the brain stem, is dead” (8). Since then, the criteria for its diagnosis have been expanded, culminating in the recent release of the latest guidelines from the American Academy of Neurology (11). Despite these advances, controversy continues to exist over the medico-legal and ethical implications of brain death.
Here we report a case from 1908, which predates the development of modern artificial respirators, of a 30-year-old man who underwent neurosurgical intervention by Dr. Harvey Cushing at the Johns Hopkins Hospital and was subsequently maintained by the use of manual artificial respiration for a period of 36 hours.
CASE REPORT
On September 8, 1908, a 30-year-old African-American man presented to the Johns Hopkins Hospital complaining of a “severe headache” that prevented him from sleeping. Two years previously, the patient had sustained an unspecified head trauma. The patient had been otherwise well until June of 1908, when he “just suddenly fell from chair and had a convulsion.” The patient continued to have intermittent, less severe, convulsions.
The patient was described as having a slow thought process and dull personality. He had difficulty maintaining a conversation, writing his name, and remembering his address but did not have aphasia or sensory/motor disturbances. According to Cushing’s notes, the patient had “frontal headaches and great mental confusion.”
An exploratory craniotomy was performed in the left frontal region on September 12, but “nothing pathological was found.” Postoperative notes indicated the patient was able to carry on conversation normally, a “thing which was impossible before operation.” The patient stated he had no headaches after the operation. He was discharged on September 20, 1908, because “he was very anxious to go home.”
Within a few days of discharge, the headaches returned, and gradually worsened. The patient was readmitted on November 24, 1908. He complained of “ringing in his ears” and that his “eyes hurt all times, especially when used.” Furthermore, the wife stated that the patient was irritable and several times had thrown “fits of rage” so violent that she was afraid to stay with him.
Cushing and Dr. George Heuer brought him to the operating room on December 8, 1908, for a left subtemporal decompression:
The operation presented no difficulties and was easily carried through to what promised to be a successful termination. There was a large temporal muscle, which allowed of an easy exposure of the subtemporal part of the cranium [. . .] The tension, however, of the exposed dura was so great that it seemed inadvisable to open it without . . . a lumbar puncture. This was done by Dr. Cushing, and fluid spurted from the needle under unusual tension; so much so in fact that it was feared that the growth might possibly be subtentorially situated and that a foraminal hernia, with its disturbing medullary effects, might have been occasioned. [. . .]
The tension did not greatly diminish by the above procedure, but sufficiently so to allow of an easy incision of the dura. [. . .] The extravasation, however, from these points was not sufficient to make it necessary to put on clips or to ligate the small branches of the meningeal [artery].
As Cushing completed the operation, disaster struck:
The wound was closed in the usual fashion in layers, some difficulty being experienced by the operator in closing the fascia. The ether was discontinued, a dressing was applied, and the patient seemed in excellent condition, when suddenly there was a cessation of respiration.
Artificial arm-and-chest respiration was kept up for some time and was followed by the insertion of a tracheotomy tube with inflation with bellows.
Cushing decided to reopen the wound, only to be met with further difficulties:
The subtemporal wound was then reopened without disclosing any reason for the pressure which had led to the bulbar palsy. The brain, however, was found to be protruding into the defect in unusual degree. The cortex was pale and its circulation entirely cut off, the picture being exactly what which is observed experimentally in fatal conditions of compression through the ‘cranial window.’ The blood pressure had fallen to a very low level, at which it could not be raised with the Rivirochi [Riva-Rocci] apparatus. Crile’s pneumatic suit was applied, and this brought about a sufficient rise in pressure to enable pulse to be readily palpated and pressured to be estimated.
The patient was unable to regain autonomic respirations, and all efforts were given to maintain his vital organs for an attempt at another craniotomy:
Artificial respiration was continued during the night and the next day. On the afternoon of this second day it seemed possible that by performing a craniotomy and stimulating the cortex it could be determined whether the circulation had been so shut off from the cerebrum that any possible restoration of function could not occur. It was thought possible also that a wide craniotomy might so allow the brain to dislocate upward as to relieve the bulbar centres, though it was rather late for such an event to occur.
Without anaesthsia of course a large flap was turned down from the right hemisphere. The . . . dura was opened and the perfectly anaemic brain protruded far into the dural defect. The brain was of a gray, colorless appearance, broken only by the black, greatly distended veins. [. . .] An even larger flap was turned down on the left side and a similar observation made. [. . .]
Stimulation of the motor cortex with the full strength of the faradic current gave no response whatsoever [. . .] the osteoplastic flaps were removed and the scalp resutured in position.
Finally, Cushing stated in his operative notes (Figure 1) that
[t]he patient’s condition was absolutely unaffected by these procedures, and it was evident that his heart was running simple as an isolated organ.
Artificial respiration was continued until late in the evening of this second day, when an attempt was made to so raise the pressure by an intravenous injection of adrenolin that the bulbar centres might possibly again be reactivated, undesirable as the accomplishment of this purpose might have been. There was apparently a temporary marked rise in pressure with some convulsive movements of the body, and a very prompt cessation of all cardiac activity.
Figure 1.
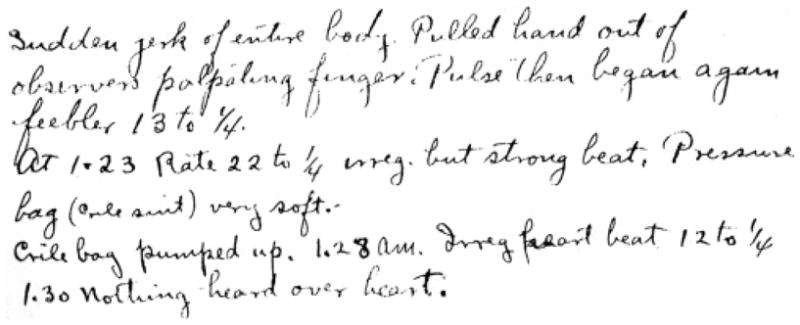
Handwritten note documenting attempts to resuscitate patient with adrenaline: “Sudden jerk of entire body. Pulled hand out of observers palpating finger. Pulse then began again feebler 13 to ¼. At 1.23 rate 22 to ¼ irreg. but strong beat. Pressure bag (crile suit) very soft. Crile bag pumped up. 1.28 am irreg heart beat 12 to ¼ 1.30 nothing heard over heart.”
Postmortem examination of the brain (Figure 2) demonstrated a left temporal lobe lesion.
Figure 2.
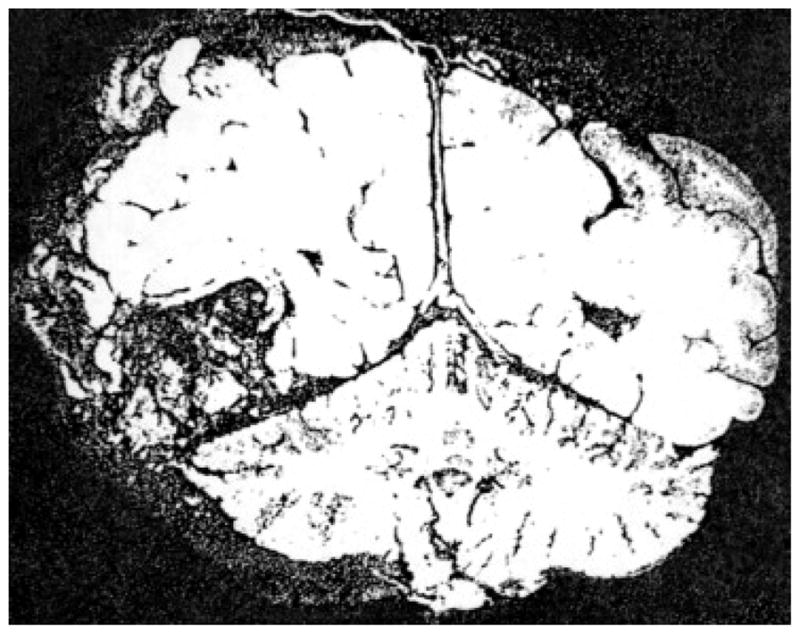
Postmortem coronal brain section demonstrating lesion in the left hemisphere shows relation of lesion to cerebellum.
DISCUSSION
Here we report a case from 1908 in which a patient was sustained with artificial respirations while surgical interventions were attempted to improve his condition. This case predates the earliest descriptions of brain death by more than half a century and touches upon key points in the contemporary debate over this medico-legal concept.
Medical standards and diagnostic criteria for brain death have been subject to debate. The most accepted parameters are from the American Academy of Neurology, which published a report in 1995 and updated the guidelines in 2010 to delineate the medical standard of practice to determine brain death (6, 11). These guidelines stipulate that the neurological assessment is the most important and definitive criteria for establishing a diagnosis of brain death, whereas confirmatory ancillary tests are optional but frequently used.
Although Cushing did not have access to the various optional ancillary tests often included in contemporary evaluations, after the required clinical diagnostic criteria are met, such as EEG, nuclear imaging, magnetic resonance imaging, or cerebral angiography, his notes from the case documented basic findings consistent with a contemporary diagnosis of brain death. First, the patient was unresponsive; it can be inferred from the operative note that the most likely cause was increased intracranial pressure and a “foraminal hernia.” A catastrophic herniation of the brain into the foramen magnum may lead to severe compression of the lower brainstem.
Indeed, even when his original craniotomy was reopened and a second bilateral craniectomy was performed without the use of anesthesia, no sensory or motor response was documented. Because Cushing’s operative notes in other cases documented discomfort and movement, it may be concluded that this patient exhibited a complete lack of response to noxious stimuli, one of the contemporary criteria for brain death. Although Cushing did not have the benefit of cerebral angiography to document decreased blood flow or nuclear imaging to map areas of necrotic brain (1), his operative note after reopening the wound described the cortex as “pale” and “its circulation entirely cut off, the picture being exactly what which is observed experimentally in fatal conditions of compression.” Cushing’s description of the brain provides an image of pathological hypoperfusion and necrosis. After a day and a half of artificial respiration, Cushing planned to use a craniotomy to reevaluate the status of the brain:
it seemed possible that by performing a craniotomy and stimulating the cortex it could be determined whether the circulation had been so shut off from the cerebrum that any possible restoration of function could not occur.
Cushing’s operative note from the attempted bilateral craniectomy offers further evidence of severe brain damage:
the perfectly anaemic brain protruded far into the dural defect. The brain was of a gray, colorless appearance, broken only by the black, greatly distended veins.
Even though these observations are subjective, rather than quantitative, it is undeniable that the patient had sustained tremendous ischemic brain damage; however, recent studies have documented that neuropathologic findings are not independently diagnostic of brain death (10).
Although EEG technology was not available at the time (7), Cushing performed Faradic stimulation of the cortex, resulting in “no response whatsoever.” This result strongly suggests an absence of electrical activity within the brain, although even modern EEG technology is not an accurate predictor of brain death. However, Cushing’s notation documents “a temporary marked rise in pressure with some convulsive movements of the body,” which may indicate some residual cortical function, despite other signs of brain death. Although Cushing did not document a neurological examination once artificial respirations were begun, he did document that the patient had “bulbar palsy,” suggesting bilateral impairment of cranial nerves IX, X, XI, and XII.
Despite the limitations of technology in the early 20th century, and the absence of some critical criteria used in the contemporary definition of brain death, the evidence presented in Cushing’s notes suggests the patient experienced irreversible brain damage, whereas his heart remained functional and respirations were continued through artificial means.
In addition to documenting criteria consistent with brain death, Cushing’s notes also reflected his insight into heart and lung function, as well as his ethical dilemma in attempting to sustain “life” without apparent brain function. After a day and a half of artificial respiration, and two surgical interventions that failed to produce clinical improvement, Cushing noted “it was evident that his heart was running simple as an isolated organ.” This single sentence documented an early understanding that cardiac function might continue even when higher brain and autonomic respiratory functions have ceased. At the end of the second day of artificial respiration, when adrenaline was injected in an attempt to improve the patient’s condition, Cushing briefly reflected on whether it was worthwhile to pursue such avenues: “the bulbar centres might possibly again be reactivated, undesirable as the accomplishment of this purpose might have been.” The reluctance to successfully reverse the patient’s condition may have been predicated more on the significant equipment and staff required to provide manual respirations, rather than on a concern for the patient’s long-term outcome after the neurological insult. This reflection illuminates the ethical conundrum facing contemporary clinicians, whose practice must balance what modern technology can accomplish with what modern technology should accomplish.
As Cushing pioneered neuro-oncology and neurosurgery, in this report, we provide support of Cushing’s trailblazing role in what may be a first report of a situation that resembles the activity in a modern day neurocritical care unit. The use of artificial respiration in this patient was not an endeavor undertaken lightly; without modern mechanical ventilators, the task was completed manually, with a hospital staff member using arm-and-chest and bellow inflation techniques for 36 hours. A tremendous amount of effort was expended to maintain function of the body’s vital organs while Cushing attempted to repair the brain herniation and perhaps even struggled to grasp the concept of brain death and its dilemmas during the dawn of neurosurgery.
Abbreviations and Acronyms
- EEG
Electroencephalogram
Footnotes
Conflict of interest statement: Dr. Courtney Pendleton is supported by a HHMI-Ivy Student Research Training Grant. Alfredo Quinones-Hinojosa is funded by the KO8 NIH grant and an HHMI grant. Figures were provided courtesy of the Alan Mason Chesney Archives.
References
- 1.Bonetti MG, Ciritella P, Valle G, Perrone E. 99mTc HM-PAO brain perfusion SPECT in brain death. Neuroradiology. 1995;37:365–369. doi: 10.1007/BF00588013. [DOI] [PubMed] [Google Scholar]
- 2.Harvard Medical School. A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA. 1968;205:337–340. [PubMed] [Google Scholar]
- 3.Laureys S, Fins JJ. Are we equal in death? Avoiding diagnostic error in brain death. Neurology. 2008;70:e14–e15. doi: 10.1212/01.wnl.0000303264.66049.c1. [DOI] [PubMed] [Google Scholar]
- 4.Mohandas A, Chou SN. Brain death. A clinical and pathological study. J Neurosurg. 1971;35:211–218. doi: 10.3171/jns.1971.35.2.0211. [DOI] [PubMed] [Google Scholar]
- 5.Mollaret P, Goulon M. Le coma dépassé (mémoire préliminaire) Rev Neurol (Paris) 1959;101:3–5. [PubMed] [Google Scholar]
- 6.Practice parameters for determining brain death in adults (summary statement) The Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1995;45:1012–1014. doi: 10.1212/wnl.45.5.1012. [DOI] [PubMed] [Google Scholar]
- 7.Swartz BE, Goldensohn ES. Timeline of the history of EEG and associated fields. Electroencephalogr Clin Neurophysiol. 1998;106(2):173–176. [PubMed] [Google Scholar]
- 8.Uniform Determination of Death Act. vol 12 Uniform Laws Annotated (U.L.A.) 589 (West 1993 and West Supp. 1997). Chicago: National Conference of Commissioners on Uniform State Laws; 1980.
- 9.Wijdicks EF. The diagnosis of brain death. N Engl J Med. 2001;344:1215–1221. doi: 10.1056/NEJM200104193441606. [DOI] [PubMed] [Google Scholar]
- 10.Wijdicks EF, Pfeifer EA. Neuropathology of brain death in the modern transplant era. Neurology. 2008;70:1234–1237. doi: 10.1212/01.wnl.0000289762.50376.b6. [DOI] [PubMed] [Google Scholar]
- 11.Wijdicks EF, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1911–1918. doi: 10.1212/WNL.0b013e3181e242a8. [DOI] [PubMed] [Google Scholar]
- 12.Zorab J. The resuscitation greats. Bjorn Ibsen Resuscitation. 2003;57:3–9. doi: 10.1016/s0300-9572(03)00040-6. [DOI] [PubMed] [Google Scholar]


