Abstract
Background
The differences in the incidence of heart failure (HF) by race/ethnicity as well as the potential mechanisms for these differences are largely unexplored in women.
Methods and Results
155,335 post menopausal women free of self-reported HF enrolled from 1993-1998 at 40 clinical centers throughout the United States as part of the Women’s Health Initiative and were followed until 2005, for an average of 7.7 years for incident hospitalized heart failure. Incident rates, hazard’s ratios and 95% CI were determined using Cox-proportional hazard’s model comparing racial/ethnic groups and population attributable risk percentages were calculated for each racial/ethnic group. African Americans had the highest age-adjusted incidence of HF (405/100,000 person-years) followed by whites (283) Hispanics (191) and Asian/Pacific Islanders (102). The excess risk in African Americans compared to whites (age-adjusted HR= 1.47) was significantly attenuated by adjustment for household income (HR=0.99) and diabetes mellitus (HR=0.92) but the lower risk in Hispanics (age-adjusted HR=0.76) and Asian/Pacific Islanders (age-adjusted HR=0.40) remained despite adjustment for traditional risk factors, socioeconomic status, lifestyle and access to care variables. The effect of adjustment for interim CHD on non-white versus white hazard ratios for heart failure differed by race/ethnic group.
Conclusions
Asian/Pacific Islander and Hispanic women have a lower incidence of heart failure while African American women have higher rates of heart failure compared to white women. The excess risk of incident heart failure in African American women is largely explained by adjustment for lower household incomes and diabetes in African American women while the lower rates of heart failure in Asian/Pacific Islanders and Hispanics are largely unexplained by the risk factors measured in this study.
Clinical Trial Registration Information
http://www.clinicaltrials.gov; Unique Identifier: NCT00000611
Keywords: heart failure, incidence, population, race/ethnicity
Introduction
Heart Failure (HF) is recognized by a constellation of signs and symptoms and a neuro-humoral response to cardiac dysfunction. HF develops as a consequence of many forms of cardiovascular disease and is not a single pathologic entity. Rates of HF are reaching epidemic proportions, affecting with more than five million people in the US with over 500,000 newly diagnosed cases each year1. Both the prevalence and morbidity associated with HF is increasing in the United States with racial and ethnic disparities noted. Despite advances in therapy and improvement in the five year survival rate, the prognosis is still relatively poor.2,3 HF also imposes considerable economic impact on health services due to the need for long-term, multi-pharmaceutical treatment, use of implantable defibrillators, and frequent hospitalizations.4 Most previous work related to racial/ethnic differences in the prevalence of heart failure have suggested that differences may be attributable to the relative importance of different risk factors or access to care issues.4-11 However such prevalence studies are prone to bias and lack temporality. A few recent studies have examined racial/ethnic differences in incident heart failure but had limited numbers incident cases of HF and with limited numbers of racial/ethnic groups for comparison.12,13 Also of interest are the gender differences in heart failure both in rates and risk factors, as most studies of HF have included a limited number of women. Previous research suggests that women have more hypertension, and valvular disease and less underlying coronary disease or dilated cardiomyopathy compared to men as potential risk factors for HF but again are limited to prevalence studies.11,14
These limitations emphasize the need for larger prospective epidemiologic studies clarifying the incidence and risk factors associated with HF in a multi-racial cohort in post-menopausal women. We address the following research questions in a large, diverse nation-wide cohort of post-menopausal women: Are there differences in the incidence of HF by race/ethnicity in post-menopausal women? If so, what socio-demographic, lifestyle, access to care and traditional risk factors explain these differences? Which modifiable risk factors contribute to the burden of heart failure in different race/ethnic groups in post-menopausal women?
Methods
Study Population
The Women’s Health Initiative (WHI) recruited women nationwide in 40 clinical centers between 1993-1998.15-18 Study participants were women age 50-79 at baseline. Women were excluded if they did not plan to reside in the area for at least 3 years, had medical conditions predictive of less than 3 years of survival or had complicating conditions such as alcoholism, mental illness, or dementia. Those eligible for either the clinical trials or observational arm completed baseline assessments including several self-administered questionnaires of socio-demographic characteristics, medical history, reproductive and menstrual history, health behavior including physical activity and diet, and family history of selected diseases. Trained staff obtained anthropometric measures including height, weight, and waist circumference. For blood pressure, after women sat quietly for five minutes, blood pressure was measured with a mercury manometer twice, 30 seconds apart, and the average was used in this analysis.
Medication use at baseline was ascertained by having the participants bring all the containers for medications taken for the 2 weeks prior to the baseline visit. Interviewers entered each medication into a central database, which assigned drug codes using Medi-Span software. Information was recorded on duration of use but not dose. White blood cell count and hemoglobin levels were measured via standardized automated technique on fresh samples at each local WHI site.
A standardized written protocol, centralized training of local clinical staff, local quality control, and periodic quality assurance visits by the Clinical Coordinating Center were used to maintain uniform data collection procedures at all study sites. Reproducibility of WHI questionnaire data was evaluated in a random sub-sample at 10 weeks with good to excellent reproducibility (weighted kappa- 0.77 to 0.99).15
Covariates
Race was self-reported as American Indian or Alaskan Native, Asian or Pacific Islander, Black or African-American, Hispanic/Latino, white (not of Hispanic origin), or Other.
For analytic purposes, age was categorized by age groups <50-59, 60-69,70-79+; education was categorized as less than high school or more than high school; income was categorized as <20K, 20-35K, 35-50K, 50-75K, 75K+ dollars per year; cigarette smoking was categorized as current, past and never; hormone status was categorized as current, past and never. Hyperlipidemia was defined as taking cholesterol lowering medication. Hypertension defined by self report and taking anti-hypertensive medications or systolic blood pressure ≥140 or diastolic BP ≥90 mmHg. Uncontrolled systolic BP was defined as systolic BP >150 mmHg and taking anti-hypertensive medications. Diabetes mellitus defined by self-report of physician diagnosis and taking hypoglycemic medications. Atrial fibrillation was based upon self-report and not medication use.
Prevalent coronary heart disease (CHD) was defined as self-reporting at baseline as having been hospitalized for a heart attack (myocardial infarction), coronary angioplasty (PTCA) or stent, coronary artery bypass graft (CABG) surgery, or angina (chest pains from heart problems).
Physical activity was ascertained using a series of questions related to walking and exercise at strenuous levels and physical activity at moderate and low-intensity levels. A composite variable was constructed imputing the mid-point of the range of frequency and duration of walking, strenuous exercise, and moderate and low- intensity physical activity to determine the hours of activity per week for each type of physical activity. A metabolic equivalent (MET) value was assigned to each level of activity and a total physical activity score (MET-hours/week) was computed for each participant.17 Alcohol intake was ascertained by asking participants to estimate over the past three months the average frequency and quantity of drinking, beer wine or liquor. Servings per week were estimated based upon 12 ounces of beer equivalent to 6 ounces of wine and 1.5 ounces of liquor for each participant.
Outcomes
Incident hospitalized HF was ascertained yearly in WHI by medical record abstraction of self-report hospitalizations and classified by trained adjudicators using the standardized methodology as previously described.18 Hospitalized HF requiring and/or occurring during hospitalization required physician diagnosis of new-onset or worsened congestive HF on the reported hospital admission and 1 or more of the following 4 criteria: HF diagnosed by physician and receiving medical treatment for HF, symptoms plus documentation in the current medical record of a history of an imaging procedure showing impaired left ventricular (LV) systolic or diastolic LV function, pulmonary edema/congestion on chest x-ray on the current admission, dilated ventricle(s) or “poor” LV or right ventricular (RV) function by echocardiography, radionuclide ventriculography, or other contrast ventriculography, or evidence of LV diastolic dysfunction. This method was found to have an excellent 79% agreement rate (kappa) comparing central adjudicated HF to local adjudication.18
Interim CHD was defined by adjudicated hospitalization for myocardial infarction, PTCA, CABG, or angina after baseline and prior to the HF hospitalization.18
Statistical Methods
The frequency distribution of the variables of interest was inspected to rule out anomalies and outliers due to measurement artifacts. Correlations among covariates were examined to evaluate collinearity. Differences in covariates by race/ethnicity and by developing incident HF were performed to look for potential confounding relationship using ANOVA and chi-square testing for continuous and categorical variables.
Women with self-reported HF at baseline (N= 2868) were excluded from the cohort, as were those with missing race or other race (N=2914) and those with missing covariate data (N= 691). Age-specific and age-adjusted rates using 2000 Census data for direct adjustment by race/ethnicity were calculated. Proportional hazards models were developed for incident hospitalized HF adjusting for potential confounders based upon the clinical literature as well inclusion of other potential confounders found in the univariate analysis that differed by race and by incident heart failure at P<.10. Because the entry criteria and time of observation were different between the observational study and clinical trials cohorts, we performed stratified analysis by cohort assignment and pooled the estimate of effect for each risk factor using the STRATA statement in proc PHREG in SAS.9.2. A C-statistic or area under the receiver operating characteristic curve which compares the sensitivity to the 1- specificity is presented to demonstrate how well the heart failure models discriminate cases of heart failure from non-cases.
Population attributable risk percentages were calculated to evaluate the potential impact of risk factor reduction from the public health perspective using the formula PAR=[p(r-1)]/[p(r-1) +1] × 100% where p is the proportion of the population with the risk factor and r is the relative risk estimate (hazard’s ratio) for the risk factor.
Results
The baseline cohort included 155,335 post-menopausal women free of self-reported HF and with complete data on confounders was analyzed of which 84.4% were white, 9% African American, 4% Hispanic and 2.6% Asian / Pacific Islanders. Table 1 shows the characteristics of the cohort by race/ethnicity. Significant differences between racial/ethnic groups were noted for socio-demographic factors such as age, education, income; access to care and medication issues such as insurance status, hysterectomy, hormone treatment; traditional risk factors for heart failure including obesity, history of coronary heart disease, diabetes; lifestyle factors such as alcohol servings per week, and Vitamin D intake.
Table 1.
Description of WHI Cohort Free of HF at Baseline by Race/ethnicity
| Variable | Asian/Pacific Islander | African American | Hispanic | White | p-value* | ||||
|---|---|---|---|---|---|---|---|---|---|
| n=4,108 | n=14,103 | n=6,213 | n=130,911 | ||||||
| n | % | n | % | n | % | n | % | ||
| SOCIO-DEMOGRAPHIC | |||||||||
|
| |||||||||
| Age | |||||||||
| <50-59 | 1449 | 35.3 | 5898 | 41.8 | 3124 | 50.3 | 41080 | 31.4 | |
| 60-69 | 1723 | 41.9 | 6014 | 42.6 | 2426 | 39 | 59575 | 45.5 | |
| 70-79+ | 936 | 22.8 | 2191 | 15.5 | 663 | 10.7 | 30256 | 23.1 | <0.01 |
| Education | |||||||||
| Less than high school | 207 | 5.1 | 1657 | 11.9 | 1652 | 27.1 | 4445 | 3.4 | |
| High school or higher | 1231 | 30.2 | 3658 | 26.3 | 1751 | 28.69 | 35452 | 27.3 | |
| Some College | 830 | 20.4 | 3690 | 26.5 | 1418 | 23.2 | 36755 | 28.3 | |
| College or higher | 1809 | 44.4 | 4920 | 35.3 | 1283 | 21.0 | 53413 | 41.1 | <0.01 |
| Income | |||||||||
| <$20K | 468 | 12.2 | 3923 | 30.1 | 2126 | 38.5 | 17324 | 14.1 | |
| $20K-<$35K | 731 | 19.0 | 3179 | 24.4 | 1309 | 23.7 | 29931 | 24.4 | |
| $35K-<$50K | 733 | 19.0 | 2355 | 18.1 | 906 | 16.4 | 25827 | 21.1 | |
| $50K-<$75K | 931 | 24.2 | 2193 | 16.8 | 709 | 12.8 | 25135 | 20.5 | |
| $75K+ | 986 | 25.6 | 1372 | 10.5 | 474 | 8.6 | 24387 | 19.9 | <0.01 |
| ACCESS TO CARE and MEDICATIONS | |||||||||
|
| |||||||||
| Insurance Status | |||||||||
| No Ins. | 191 | 4.7 | 682 | 4.9 | 350 | 5.7 | 5897 | 4.6 | <0.01 |
| Medicare | 1512 | 37.2 | 5086 | 36.6 | 2264 | 36.9 | 48378 | 37.3 | 0.33 |
| Private Ins. | 3541 | 87.0 | 12030 | 8604 | 5318 | 86.6 | 113057 | 87.2 | 0.06 |
| Medications | |||||||||
| Aspirin | 908 | 22.4 | 2985 | 21.5 | 1321 | 21.5 | 27735 | 21.5 | 0.58 |
| Angiotensin Receptor Blockers | 32 | 0.8 | 93 | 0.7 | 47 | 0.8 | 919 | 0.7 | 0.81 |
| Beta-blocker | 347 | 8.6 | 1132 | 8.2 | 539 | 8.8 | 11005 | 8.5 | 0.39 |
| Multivitamin | 1629 | 39.7 | 5305 | 37.6 | 2363 | 38.0 | 51292 | 39.2 | <0.01 |
| Hormone Therapy | |||||||||
| Never | 1144 | 28.2 | 6565 | 47.3 | 2448 | 40.4 | 40106 | 31.6 | |
| Past | 843 | 20.8 | 3460 | 25 | 1336 | 22.1 | 29252 | 23.1 | |
| Current | 2075 | 51.1 | 3841 | 27.7 | 2270 | 37.5 | 57524 | 45.3 | <0.01 |
| Medical Condition Hysterectomy | 1436 | 35.0 | 7813 | 55.4 | 2781 | 44.8 | 52669 | 40.2 | <0.01 |
| TRADITIONAL RISK FACTORS | |||||||||
|
| |||||||||
| Hyperlipidemia | 524 | 13.5 | 1853 | 14 | 812 | 13.9 | 17209 | 14 | 0.86 |
| Hypertension | 1332 | 32.4 | 4520 | 32.0 | 1930 | 31.1 | 41715 | 31.9 | 0.35 |
| Obese | 1146 | 28.2 | 4232 | 30.3 | 1863 | 30.3 | 39151 | 30.2 | 0.05 |
| Previous Coronary Heart Disease | 288 | 7.0 | 1231 | 8.7 | 416 | 6.7 | 10052 | 7.7 | <0.01 |
| Atrial Fibrillation | 163 | 4.0 | 601 | 4.3 | 275 | 4.5 | 5407 | 4.2 | 0.53 |
| Diabetes | 237 | 5.8 | 1663 | 11.8 | 435 | 7.0 | 4234 | 3.2 | <0.01 |
| Cigarette Smoking | |||||||||
| Never | 2084 | 51.3 | 7126 | 51.2 | 3162 | 51.6 | 65819 | 51 | |
| Past | 1674 | 41.2 | 5823 | 41.8 | 2537 | 41.4 | 54386 | 42.1 | |
| Current | 301 | 7.4 | 969 | 7 | 432 | 7 | 8974 | 6.9 | 0.75 |
| LIFESTYLE | mean | SD | mean | SD | mean | SD | mean | SD | p-value** |
|
| |||||||||
| Physical Activity (MET – hour/week) | 11.9 | (12.9) | 12.6 | (13.9) | 12.4 | (13.7) | 12.4 | (13.8) | 0.06 |
| Alcohol (servings per week) | 2.3 | 4.8 | 2.3 | 4.7 | 2.3 | 4.6 | 2.4 | 4.9 | 0.03 |
| Vitamin D Intake (mcg/day) | 4.94 | 6.19 | 4.69 | 5.94 | 4.75 | 6.04 | 4.93 | 6.22 | <0.01 |
| PHYSIOLOGY | |||||||||
|
| |||||||||
| Systolic Blood Pressure (mmHg) | 128 | 17.9 | 127 | 17.8 | 127 | 17.5 | 127 | 17.7 | 0.67 |
| Diastolic Blood Pressure (mmHg) | 75 | 9.4 | 75 | 9.3 | 75 | 9.2 | 75 | 9.3 | 0.86 |
| Waist Hip Ratio | 0.81 | 0.08 | 0.81 | 0.08 | 0.81 | 0.08 | 0.81 | 0.08 | 0.43 |
| Waist Circumference (cm) | 86.0 | 13.6 | 86.5 | 13.8 | 86.5 | 13.6 | 86.5 | 13.9 | 0.24 |
| Hemoglobin (g/dL) | 13.5 | 1.0 | 13.5 | 1.1 | 13.5 | 1.1 | 13.5 | 1.1 | 0.81 |
| White Blood Cell (103/ml) | 6.4 | 16.7 | 6.1 | 7.2 | 6.1 | 8.3 | 6.2 | 12.2 | 0.32 |
SD – Standard Deviation
p-values obtained from Chi Square test statistic using categorical variables
p-values obtained using analysis of variance (ANOVA) for the continuous variable by race/ethnicity
Incident hospitalized HF developed in an average of 7.7 years of follow-up in 3,101 whites, 415 African Americans, 81 Hispanics and 36 Asian/Pacific Islanders. Age-specific and age-adjusted rates demonstrated differences by race with African Americans having the highest age-adjusted rate of incident hospitalized HF.(Figure 1A, Table 2) This higher rate was greatest in the under 60 age group. After multiple variable adjustments for other risk factors, Whites and African Americans had similar rates for HF while Hispanics and Asian/Pacific Islanders had persistently lower rates of HF. (Figure 1B and Table 3). The C-statistic for the full multivariate model was C=0.80 (95% CI: 0.79-0.81).
Figure 1.
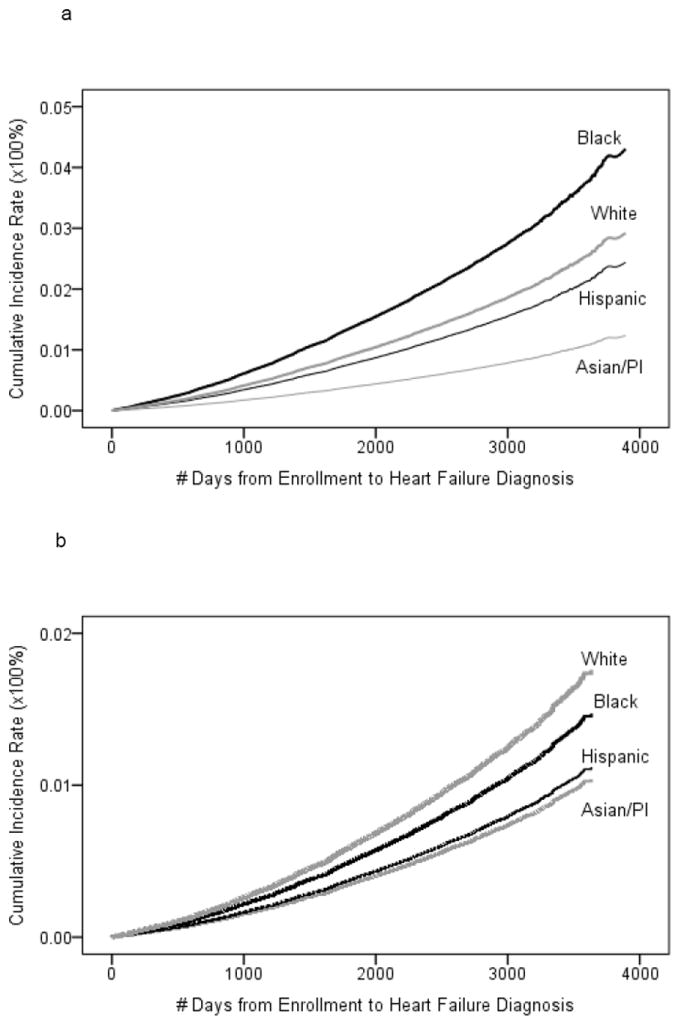
a: Age-adjusted Cumulative Incidence of Heart Failure in WHI Cohort by Race. b: Multivariate* Adjusted Cumulative Incidence of Heart Failure in WHI Cohort by Race. *adjusted for age, income, education, insurance status, alcohol consumption, physical activity, current medical conditions (hypertension, diabetes, high cholesterol, CHD, atrial fibrillation, history of hysterectomy) and medication use (hormone replacement therapy, multi-vitamins, aspirin, ARB, beta-blockers)
Table 2.
Crude, Age-adjusted and Age-specific Rates of Hospitalized HF by Race/Ethnicity (per 100,000 person-years).
| Race | White | African Americans | Hispanic | Asian/Pacific Islander | Total |
|---|---|---|---|---|---|
| Crude | 303.1 | 388.6 | 176.1 | 115.9 | 301.0 |
| Age-adjusted | 283.0 | 404.7 | 191.4 | 101.7 | 280.7 |
| <50-59 years | 93.1 | 217.0 | 114.3 | 35.5 | 106.5 |
| 60-69 years | 268.1 | 434.7 | 180.3 | 100.2 | 275.1 |
| 70-79+ years | 693.0 | 768.2 | 476.1 | 278.6 | 682.4 |
Table 3.
Nested models predicting Incident Heart Failure in Post Menopausal Women.
| Hazard Ratio (95% Confidence Interval)a | |||||
|---|---|---|---|---|---|
| Racial/Ethnic Group | Model 1: Age | Model 2: Age + SESb | Model 3: Age, SESb, Established Risk Factorsc | Model 4: Age, SESb, Established Risk Factorsc, Interim CHD | Model 5: Age, SESb, Established Risk Factorsc, Interim CHD, Additional Factorsd |
| White | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| Asian/Pacific Islander | 0.40 (0.28-0.57) | 0.41 (0.29-0.59) | 0.36 (0.25-0.52) | 0.42 (0.29-0.60) | 0.43 (0.29-0.62) |
| African American | 1.47 (1.31-1.66) | 1.20 (1.07-1.35) | 0.94 (0.83-1.06) | 1.04 (0.92-1.17) | 0.97 (0.86-1.11) |
| Hispanic | 0.76 (0.59-0.99) | 0.56 (0.43-0.73) | 0.52 (0.40-0.68) | 0.59 (0.46-0.77) | 0.59 (0.45-0.78) |
Abbreviations: SES, socioeconomic status; CHD, coronary heart disease
Boldface type indicates statistical significance at p<0.05
Income and education level
Hypertension, diabetes, obesity, dyslipidemia, smoking status, and CHD at baseline
Hysterectomy, atrial fibrillation, any health insurance, medication use (HRT, aspirin, ARB, beta blockers, multivitamin), physical activity level, alcohol consumption
To better understand which risk factors might explain the racial/ethnic differences in the incidence of heart failure, we performed nested models (Tables 3 and 4) comparing each race/ethnicity group to white women regarding their risk of Heart Failure. As shown in table 3, a model adjusting for age, income and education had a modest effect on explaining differences between African American women and whites had no effect on Asian/Pacific Islanders and the made more apparent the lower risk of heart failure in Hispanics. Adjusting for established risk factors for HF to the model, removed the excess risk in African American women compared to Whites and made more apparent the lower risk of Heart Failure in Asian/Pacific Islanders and Hispanic compared to Whites. Adjusting for interim CHD in addition to age, SES, and traditional risk factors had a modest effect on the inverse relationship between Hispanic and Asian/Pacific Islander race for incident HF compared to whites. For African American women, this adjustment lead to a non-significant excess risk in African American women compared to whites. Further adjusting for all potential confounders including access to care, medications and other medical conditions to the model, reversed the modest excess risk associated with adjusting for interim CHD in African American women and had minimal effect on the point estimates of risk for the Hispanic or Asian/Pacific Islanders.
Table 4.
Nested Models of Heart Failure adding each risk factor individually comparing each Racial/Ethnic group to White Postmenopausal Women.
| Racial/Ethnic Group, Hazard Ratio (95% Confidence Interval) | |||||
|---|---|---|---|---|---|
| Model | Asian/Pacific Islander | African American | Hispanic | White | p-value for added covariate |
| Unadjusted Model (Model 1) | 0.38 (0.27-0.55) | 1.23 (1.10-1.38) | 0.56 (0.43-0.72) | 1.00 [Reference] | <0.001 |
| Established Risk Factors | |||||
| Model 1 + age | 0.40 (0.28-0.57) | 1.47 (1.31-1.66) | 0.76 (0.59-0.99) | 1.00 [Reference] | <0.001 |
| Model 1 + hypertension | 0.38 (0.27-0.55) | 1.23 (1.10-1.38) | 0.56 (0.43-0.72) | 1.00 [Reference] | 0.35 |
| Model 1 + uncontrolled sbp | 0.38 (0.27-0.55) | 1.23 (1.10-1.38) | 0.56 (0.43-0.72) | 1.00 [Reference] | 0.03 |
| Model 1 + diabetes | 0.35 (0.24-0.50) | 0.92 (0.81-1.03) | 0.49 (0.38-0.63) | 1.00 [Reference] | <0.001 |
| Model 1 + obesity (BMI ≥ 30) | 0.38 (0.27-0.55) | 1.23 (1.10-1.39) | 0.56 (0.43-0.72) | 1.00 [Reference] | <0.05 |
| Model 1 + smoking status | 0.37 (0.26-0.54) | 1.23 (1.10-1.38) | 0.56 (0.43-0.72) | 1.00 [Reference] | 0.77 |
| Model 1 + dyslipidemia | 0.37 (0.26-0.54) | 1.23 (1.10-1.38) | 0.56 (0.43-0.72) | 1.00 [Reference] | 0.77 |
| Model 1 + previous CHD | 0.38 (0.26-0.54) | 1.22 (1.09-1.37) | 0.56 (0.43-0.73) | 1.00 [Reference] | <0.001 |
| Socioeconomic Factors | |||||
| Model 1 + household income | 0.41 (0.29-0.59) | 0.99 (0.89-1.12) | 0.41 (0.32-0.53) | 1.00 [Reference] | <0.001 |
| Model 1 + education level | 0.37 (0.26-0.53) | 1.14 (1.01-1.28) | 0.44 (0.34-0.57) | 1.00 [Reference] | <0.001 |
| Other Medical Issues | |||||
| Model 1 + atrial fibrillation | 0.37 (0.26-0.54) | 1.23 (1.10-1.38) | 0.56 (0.43-0.72) | 1.00 [Reference] | 0.84 |
| Model 1 + hysterectomy | 0.38 (0.27-0.55) | 1.17 (1.04-1.31) | 0.55 (0.42-0.71) | 1.00 [Reference] | <0.001 |
| Access to Health Care and Medication Use | |||||
| Model 1 + any health insurance | 0.37 (0.25-0.53) | 1.23 (1.09-1.38) | 0.55 (0.43-0.72) | 1.00 [Reference] | 0.46 |
| Model 1 + ARB use | 0.38 (0.26-0.55) | 1.22 (1.09-1.37) | 0.56 (0.43-0.73) | 1.00 [Reference] | 0.61 |
| Model 1 + aspirin use | 0.38 (0.26-0.55) | 1.22 (1.09-1.37) | 0.56 (0.43-0.73) | 1.00 [Reference] | 0.75 |
| Model 1 + beta blocker use | 0.38 (0.26-0.55) | 1.22 (1.09-1.37) | 0.56 (0.43-0.73) | 1.00 [Reference] | 0.98 |
| Model 1 + HRT use | 0.38 (0.26-0.55) | 1.12 (1.00-1.26) | 0.53 (0.41-0.69) | 1.00 [Reference] | <0.001 |
| Model 1 + multivitamin use | 0.37 (0.25-0.53) | 1.23 (1.09-1.38) | 0.55 (0.43-0.72) | 1.00 [Reference] | 0.10 |
| Lifestyle Factors | |||||
| Model 1 + alcohol consumption | 0.38 (0.26-0.54) | 1.24 (1.10-1.39) | 0.56 (0.43-0.72) | 1.00 [Reference] | 0.80 |
| Model 1 + physical activity level | 0.38 (0.26-0.55) | 1.24 (1.10-1.39) | 0.55 (0.42-0.72) | 1.00 [Reference] | 0.43 |
| Proximal Risk Factors | |||||
| Model 1 + interim CHD | 0.44 (0.31-0.64) | 1.24 (1.10-1.39) | 0.62 (0.48-0.81) | 1.00 [Reference] | <0.001 |
P-values reflect the effect of adding the risk factor on predicting HF in the Cox-proportional hazard’s model, not differential effect across race/ethnicity gradient
To further explore the risk attenuation of HF in African American women compared to white women and the independent contribution of prevalent and interim CHD as well as other potential risk factors, we evaluated risk factor specific models (Table 4). For African American women adjusting for age made more apparent the excess risk of heart failure compared to whites whereas adjusting for diabetes mellitus, household income, education level, hysterectomy, HRT use lowered the excess risk of heart failure compared to whites. Of note, adjusting for diabetes mellitus and household income removed the excess risk of HF completely in African American women while hypertension, obesity, and prevalent or interim CHD had no effect. For Hispanic women, adjusting for the confounding effects of age and interim CHD for heart failure lead to point estimates of risk closer to the null compared to baseline risk levels whereas adjusting for diabetes, household income, education, lead to point estimates of a lower risk of HF for Hispanics compared to whites suggesting potential mechanisms for differences in rates of incident heart failure for Hispanics. For Asian/Pacific Islander women, adjusting for household income, and interim CHD had a modest effect on point estimates of the lower risk for HF compared to whites.
Population attributable percentages (PAR%) for heart failure attributed to diabetes and interim CHD are shown in Figure 2. This measure of the public health impact of these risk factors which accounts for both the prevalence of a risk factor and its relative risk shows that diabetes has its greatest impact on Hispanic and African American women and to a lesser extent Asian/Pacific Islander and white post menopausal women. Interim CHD shows a greater overall impact on the modifiable risk of Heart Failure, with its greatest effect on Hispanics, followed by Asian/Pacific Islanders, whites and then African Americans.
Figure 2.
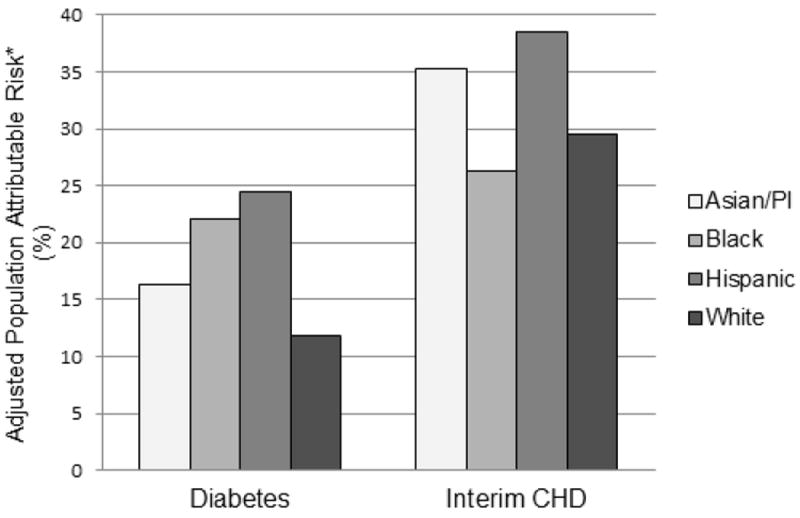
Population Attributable Risk Percentage of Diabetes and interim Coronary Heart Disease for Incident Heart Failure by Race/Ethnic group in Post Menopausal Women. *Relative Risk estimates adjusted for age, income and education
Discussion
This analysis of a large prospective cohort of racially and ethnically diverse post menopausal women revealed that African American women especially at or below the age of 60 years are at higher risk of incident hospitalized HF than their white counterparts, whereas Asian/Pacific Islanders and Hispanic women had lower risks of incident hospitalized HF than White postmenopausal women. Adjusting for age, socioeconomic status, and known risk factors for heart failure removed the excess risk for African American women but did not significantly attenuate the lower risk of HF found in the Asian/Pacific Islanders and Hispanic women compared to white women. For African American women, the higher risk of heart failure compared to Whites was largely explained by adjustment for diabetes mellitus and lower income levels. Population attributable risk percentages showed the greatest public health impact for interim CHD and diabetes mellitus, with differences by race/ethnicity on their relative attributable burden on incident heart failure.
Our age-adjusted incidence of hospitalized heart failure (280.7/100,000 person-years) is similar to that found in the Olmsted County study19 which had an age-adjusted incidence of 289/100,000 person-years in women, and the crude incidence rate of 310/100,000 in the MESA study12 but differs from the Cardiovascular Health Study (CHS)20 which had a crude incidence rate of 2,460/100,000 person-years and Health ABC21 which had a crude incidence rate of 1,170/100,000 person-years. The higher rates of incident HF in Health ABC and CHS are probably due to the older age of CHS and Health ABC cohorts, combining of men and women in the CHS estimates, differences in racial mix, geographic variation and diagnostic criteria utilized.
There are a limited number of studies have evaluated the incidence of hospitalized heart failure in different race/ethnic groups of women. Alexander et al,22 calculated the population based age-adjusted incidence of heart failure in California using administrative data in 1991, and found rates of 265/100,000 person years for white women, 454/100,000 person years for African American women, 237/100,000 for Hispanic women, and 206/100,000 very similar to our results. Bahrami et al using the Multi-ethnic Study of Atherosclerosis cohort (MESA)12, calculated rates of 240/100,000 for whites, 460/100,000 for African Americans, 350/100,000 for Hispanics and 100/100,000 for Asian/Pacific Islanders, however their estimates combined men and women and was based upon only 79 incident cases of HF. These rates from MESA are comparable to the 60-69 age-specific rates in our study for whites, African Americans, and Asian/Pacific Islanders in WHI but are much higher than those found for Hispanic women (180/100,000) in the WHI cohort. Bibbins-Domingo et al13 using the CARDIA cohort estimated early heart failure rates in African American women prior to age 50 of 55/100,000 person-years which is less than the 50-59 year old age-specific rate of 217/100,000 person-years found in WHI. These differences may well be explained by the difference in rates of heart failure in pre-menopausal compared to post-menopausal women. In addition, while comparing incidence rates of heart failure, how heart failure was defined including both hospitalized and outpatient diagnosis versus only hospitalized heart failure differed by study. For example in MESA12, of the 79 cases of incident heart failure approximately 18% were based upon outpatient diagnoses, whereas in CHS20, Health ABC21, and CARDIA13, all relied upon hospitalized heart failure or death similar to the WHI study. Not including outpatient diagnoses of heart failure, may have underestimated mild or transient cases of heart failure (viral associated cardiomyopathies) but given the large number of cases in whites and African Americans probably had little effect on overall incident rates, whereas in Hispanics and Asian Pacific Islander with much fewer incident cases, the impact of misclassification might be greater and tend to underestimate rates. However, the misclassification bias of not including outpatient heart failure diagnoses by risk factor is likely random, and therefore would bias towards the null, leading to underestimation of risk factor associations by race/ethnicity.
A study in the United Kingdom,8 evaluating southeast Asian women mainly from the Indian subcontinent compared to white women, found minimally higher rates of hospitalized heart failure southeast Asians (430/100,000) compared to white women (410/100,000) contrary to the protective effects found in our study and in the California study which is probably related to differences in Indo-Asian compared to Asians/Pacific Islanders found in the WHI and other US cohorts. The WHI had only a small number of women from the Indian subcontinent. Contrary to our findings and those of Alexander et al, Thomas et al9 recently published data from selected hospitals suggesting that Hispanics had greater risks HF than whites. This cross-sectional analysis combined both men and women, and similar to many previous studies4-8,10,11 on the ethnic differences in heart failure is limited in terms of determining true differences in rates due to its cross-sectional nature and concerns about prevalence-incidence bias, temporal bias and incomplete adjustment for confounding bias. Also contrary to our findings, Bahrami et al12 in the MESA study found higher rates of incident HF in Hispanics compared to whites, but this risk did not reach statistical significance presumably related to sample size issues. Of interest is the fact that in MESA this increased risk in Hispanics was attenuated by household income and LV mass index and to a lesser extent by hypertension suggesting potential mechanisms important to Hispanic population. In WHI Hispanic women adjustment for higher household incomes lead to lower risk estimates of heart failure whereas development of interim CHD lead to higher estimates of heart failure compared to whites and hypertension had no confounding effect. The explanation for the differences in risk of HF in Hispanics between the different studies is unclear but may be related to different countries of origin in Hispanics (Caribbean, Central American, South American) and the degree of acculturation in the different studies.9, 12, 22
Why Hispanic and Asian women have lower rates of heart failure even after adjusting for age, socioeconomic status, and known cardiac risk factors than whites in our study remains unclear. A recent paper on racial and ethnic differences in subclinical myocardial function in a population cohort free of cardiovascular disease using cardiac MRI with tissue tagging found that Chinese-Americans had the greatest magnitude of peak systolic strain and strain rates consistent with the highest rate of systolic contraction while African-Americans had the lowest rates of peak systolic strain in the majority of wall regions and Hispanics had the lowest rate of contractility in all wall regions.23 These regional differences in LV systolic function may provide a clue into explaining the differential rates of heart failure by race and ethnicity.23
Risk factors for hospitalized HF found in this analysis are similar to those found in other prospective studies including older age, lower educational attainment, lower income, diabetes and CHD.2,4,12,19 Hysterectomy was found to be a risk factor in this study which had previously been reported as a risk factor for heart failure in the observational cohort of WHI.24 While we found hormone therapy and multivitamin use (borderline significant) to be protective, we believe these results may be confounded by past versus present use as well as markers for overall good health. We did not find hypertension to be a risk factor for heart failure in our analysis whereas it has been found to be a risk factor in most other studies of heart failure.2,4,12,19,25 We explored this anomaly using differing definitions of hypertension in the WHI dataset and found that uncontrolled systolic blood pressure (systolic BP > 150 mm Hg and on anti-hypertensive medication) did have a modest effect in predicting heart failure (Table 4) but no differential effect by race, we therefore chose to use the more standard definition of hypertension for our nested model (Table 3) to be comparable to other studies.
The strengths of this study are that it is prospective, has an adequate sample size to evaluate racial and ethnic differences with reasonable power, and has over 7.7 years of follow-up. Its limitations include the fact that while HF was a physician adjudicated outcome utilizing consistent clinical criteria, it was not a primary outcome of the WHI study and thus its definition relied upon clinical criteria that didn’t capture uniform quantitative assessment of systolic function or diastolic left ventricular function, valvular pathology or separate categorization for right HF. In addition, BNP and other biomarkers of HF were not routinely assessed. Still, this measurement error would be non-differential across race/ethnicity groups and thus would bias our results towards the null. While dietary factors were measured in this cohort they are not reported here as they are the focus of another paper. Serum creatinine and cystatin C are not currently available to assess the role of chronic kidney disease in the etiology of heart failure in WHI. Hemoglobin levels to evaluate anemia and WBC as measures of inflammation were available for analysis but did not show an association with heart failure in the univariate analysis and therefore we not evaluated as confounding risk factors.
We did not evaluate Native Americans (0.44%) of WHI study due to small numbers and therefore unstable estimates of any potential findings. Missing data was limited to < 1% of the sample and thus would have negligible effect on our findings.
In summary, race and ethnicity appear to play an important role in the epidemiology of incident HF with much lower rates found in Asian/Pacific Islanders and Hispanic post-menopausal women compared to white women. Confirming the results of previous studies, African American women have the highest rates of HF especially under the age of 60. However these differences are completely explained by effects of income and diabetes mellitus and not by hypertension or CHD in this cohort. Different risk factors have different effects on the incidence of heart failure for each racial/ethnic group providing some insight into potential different mechanisms explaining the differential rates of incident heart failure. Interim CHD and diabetes have the greatest modifiable public health impact on the incidence of heart failure and are variable in their attribution to the incidence of heart failure by race/ethnicity. The mechanism of the differential attribution of risk factors by race/ethnicity need to be explored in more depth in future cohort studies with appropriate genomic and environmental exposure data.
Supplementary Material
Clinical summary.
Heart Failure is increasing in prevalence especially in older women with differences noted by race/ethnicity. However limited information is available on differences by race/ethnicity on the incidence of heart failure which may differ from previous studies due the small number of cases of incident heart failure in racial/ethnic minorities and the incomplete assessment of potential biases. In addition, the potential mechanisms for these differences including the role of traditional risk factors, lifestyle, socioeconomic status and access to care issues in women are not well explored. This study confirmed previous studies findings that African American women had the highest rates of heart failure especially at younger ages, but also demonstrated that this increased risk was completely abated when household income or diabetes was taken into account. Hispanic and Asian/Pacific Islander women not from the Indian subcontinent had lower rates of heart failure compared to Whites, and this protective effect persisted when all the above risk factors were adjusted for. Future research on better understanding the genetic and environmental interactions that lead to the differential rate of heart failure by race/ethnicity and the risk factors involved may lead to improved targeted preventive therapies.
Acknowledgments
We thank the WHI investigators, staff and study participants for their outstanding dedication and commitment. A full listing of Women’s Health Initiative can be found in the supplement.
Funding Sources:
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts N01WH22110, 24152, 32100-2, 32105-6, 32108-9, 32111-13, 32115, 32118-32119, 32122, 42107-26, 42129-32, and 44221.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.American Heart Association. Heart disease and stroke statistics-2008 Update. Dallas (Tex): American Heart Association; 2008. [Google Scholar]
- 2.Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5:167–173. doi: 10.1023/A:1009884820941. [DOI] [PubMed] [Google Scholar]
- 3.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long-term trends in the incidence and survival with heart failure. N Engl J Med. 2002;347:1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 4.Young JB. The global epidemiology of heart failure. Med Clin North Am. 2004;88:1135–1143. doi: 10.1016/j.mcna.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Kamath S, Drazner M, Wynne J, Fanarow G, Yancy C. Characteristics and Outcomes in African American Patients with Decompensated Heart Failure. Arch Intern Med. 2008;168:1152–1158. doi: 10.1001/archinte.168.11.1152. [DOI] [PubMed] [Google Scholar]
- 6.Auble T, Hsieh M, Yealy D. Differences in initial severity of illness between black and white emergency department patients hospitalized with heart failure. Am Heart J. 2009;157:306–311. doi: 10.1016/j.ahj.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 7.Shroff G, Taylor A, Colvin-Adams M. Race-related differences in heart failure therapies: Simply black and white or shades of grey? Curr Cardiol Rep. 2007;9:178–181. doi: 10.1007/BF02938347. [DOI] [PubMed] [Google Scholar]
- 8.Blackledge H, Newton J, Squire I. Prognosis for South Asian and White Patients Newly Admitted to Hospital with Heart Failure in the United Kingdom: Historical Cohort Study. BMJ. 2003;327:526–531. doi: 10.1136/bmj.327.7414.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas K, Hernandez A, Dai D, Heidenreich P, Fonarow G, Peterson E, Yancy C. Association of Race/Ethnicity with Clinical Risk Factors, Quality of Care, and Acute Outcomes in Patients Hospitalized with Heart Failure. Am Heart J. 2011;161:764–754. doi: 10.1016/j.ahj.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Moe G, Tu J. Heart Failure in the Ethnic Minorities. Curr Opin Cardiol. 2010;25:124–130. doi: 10.1097/HCO.0b013e328335fea4. [DOI] [PubMed] [Google Scholar]
- 11.Mosterd A, Hoes AW, de Bruyne MC, Deckers JW, Linker DT, Hofman A, Grobbee DE. Prevalence of heart failure and left ventricular dysfunction in the general population. The Rotterdam Study. Eur Heart J. 1999;20:447–455. [PubMed] [Google Scholar]
- 12.Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K, Burke GL, Lima JAC. Differences in the Incidence of Congestive Heart Failure by Ethnicity; The Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:2138–2145. doi: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial Differences in Incident Heart Failure among Young Adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niemen MS, Veli-Pekka H, Hochadel M, Drexler H, Komajda M, Brutsaert D, Dickstein K, Ponikowski P, Tavazzi L, Follath F, Lopez-Sendon JL. Gender related differences in patients presenting with acute heart failure. Results from EuroHeart Failure Survey II. Eur J Heart Fail. 2008;10:140–148. doi: 10.1016/j.ejheart.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 15.Langer R, White E, Lewis C, Kotchen J, Hendrix S, Trevisan M. The Women’s Health Initiative observational study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol. 2003;13:S107–121. doi: 10.1016/s1047-2797(03)00047-4. [DOI] [PubMed] [Google Scholar]
- 16.The Women’s Health Initiative Study Group. Design of the Women’s Health Initiative Clinical Trial and Observational Study. Controlled Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 17.McTiernan A, Kooperberg C, White E, Wilcox S, Coates R, Adams-Campbell LL, Woods N, Ockene J Women’s Health Initiative Cohort Study. Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women’s Health Initiative Cohort Study. JAMA. 2003;290:1331–1336. doi: 10.1001/jama.290.10.1331. [DOI] [PubMed] [Google Scholar]
- 18.Heckbert SR, Kooperberg C, Safford MM, Psaty BM, Hsia J, McTiernan A, Gaziano JM, Frishman WH, Curb JD. Comparison of Self-Report, Hospital Discharge Codes, and Adjudication of Cardiovascular Events in the Women’s Health Initiative. Am J Epidemiol. 2004;160:1152–1158. doi: 10.1093/aje/kwh314. [DOI] [PubMed] [Google Scholar]
- 19.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJl. Trends in Heart Failure Incidence and Survival in a Community-based Population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 20.Schellenbaum GD, Rea TD, Heckbert SR, Smith NL, Lumley T, Roger VL, Kitzman DW, Taylor HA, Levy D, Psaty BM. Survival Associated with Two Sets of Diagnostic Criteria for Congestive Heart Failure. Am J Epidemiol. 2004;160:628–635. doi: 10.1093/aje/kwh268. [DOI] [PubMed] [Google Scholar]
- 21.Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, Psaty BM, Smith NL, Newman AB, Rodondi N, Satterfield S, Bauer DC, Bibbins-Domingo K, Smith AL, Wilson PW, Vasan RS, Harris TB, Butler J. Epidemiology of Incident Heart Failure in a Contemporary Elderly Cohort. The Health, Aging and Body Composition Study. Arch Intern Med. 2009;169:708–715. doi: 10.1001/archinternmed.2009.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexander M, Grumbach K, Remy L, Rowell R, Massie B. Congestive Heart Failure Hospitalizations and Survival in California: Patterns According to Race/Ethnicity. Am Heart J. 1999;137:919–927. doi: 10.1016/s0002-8703(99)70417-5. [DOI] [PubMed] [Google Scholar]
- 23.Rolim V, Fernandes S, Cheng S, Cheng YJ, Rosen B, Agarwal S, McClelland R, Bluemke D, Lima J. Racial and Ethnic Differences in Subclinical Myocardial Function: the Multi-Ethnic Study of Atherosclerosis. Heart. 2011;97:405–410. doi: 10.1136/hrt.2010.209452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howard BV, Kuller L, Langer R, Manson JE, Allen C, Assaf A, Cochrane BB, Larson JC, Lasser N, Rainford M, Van Horn L, Stefanick ML, Trevisan M Women’s Health Initiative. Risk of cardiovascular disease by hysterectomy status, with and without oopherectomy: The Women’s Health Initiative Observation Study. Circulation. 2005;111:1462–1470. doi: 10.1161/01.CIR.0000159344.21672.FD. [DOI] [PubMed] [Google Scholar]
- 25.Bibbins-Domingo K, Lin F, Vittinghoff E, Barrett-Connor E, Hulley SB, Grady D, Shlipak MG. Predictors of Heart Failure Among Women With Coronary Disease. Circulation. 2004;110:1424–1430. doi: 10.1161/01.CIR.0000141726.01302.83. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


